Abstract
Enterotoxigenic strains of Bacteroides fragilis produce an extracellular metalloprotease toxin (termed fragilysin) which is cytopathic to intestinal epithelial cells and induces fluid secretion and tissue damage in ligated intestinal loops. We report here that the fragilysin gene is contained within a small genetic element termed the fragilysin pathogenicity islet. The pathogenicity islet of B. fragilis VPI 13784 was defined as 6,033 bp in length and contained nearly perfect 12-bp direct repeats near its ends. Sequencing across the ends of the pathogenicity islet from two additional enterotoxigenic strains, along with PCR analysis of 20 additional enterotoxigenic strains, revealed that the islet is inserted at a specific site on the B. fragilis chromosome. The site of integration in three nontoxigenic strains contained a 17-bp GC-rich sequence which was not present in toxigenic strains and may represent a target sequence for chromosomal integration. In addition to the fragilysin gene, we identified an open reading frame encoding a predicted protein with a size and structural features similar to those of fragilysin. The deduced amino acid sequence was 28.5% identical and 56.3% similar to fragilysin and contained a nearly identical zinc-binding motif and methionine-turn region.
Bacteroides fragilis inhabits the colons of humans and animals and in humans comprises about 1% of the normal gut flora (23). Although abundant, at approximately 109 organisms/g of human feces, it is less prevalent than a number of other anaerobes in the intestine, some of which are present at more than 1010 organisms/g of feces. B. fragilis is, however, by far the anaerobe most commonly isolated from clinical specimens and has been associated with a number of diseases, including soft tissue infections, abscesses, and bacteremias (14, 36). Its prevalence in infections caused by anaerobic organisms has been attributed in large part to its complex carbohydrate capsule, which has been shown to cause abscesses in the absence of the organism itself (43). An outer membrane protein involved in heme uptake has also been implicated in virulence (33). Little else, however, is known about factors contributing to B. fragilis infections.
In 1984 Myers et al. implicated strains of B. fragilis as a cause of diarrhea in newborn lambs (24). They showed that the supernatant of these strains caused a fluid response in lamb ligated intestinal loops, suggesting the presence of an enterotoxin. These strains, termed enterotoxigenic B. fragilis strains, were also found to cause intestinal disease in calves, piglets, foals, and rabbits (4, 5, 7, 25, 26, 28–30). More recently, enterotoxigenic B. fragilis has been implicated in human diarrheal disease (27, 34, 36, 38, 41). In 1992, Weikel et al. showed that supernatants of enterotoxigenic B. fragilis caused rapid morphological changes in human colon carcinoma cell lines, particularly HT-29 cells (45; see also references 6 and 39). Our laboratory used the cytopathic effect to assay for toxin activity and purified a single 20-kDa polypeptide which induced rounding of HT-29 cells and caused fluid secretion in intestinal-loop assays (44). We subsequently cloned a portion of the enterotoxin gene using single-specific-primer PCR with a degenerate primer based on the N-terminal sequence of the secreted enterotoxin (22). Sequencing revealed the toxin contained a zinc-binding motif (HEXXHXXGXXH) characteristic of metalloproteases from the metzincin family (3, 42). Biochemical analysis confirmed that the enterotoxin was indeed a zinc metalloprotease. Furthermore, specific inhibitors of metalloproteases inhibited cytotoxicity and prevented fluid secretion and tissue damage caused by the toxin in vivo, suggesting that its toxic properties are due to the protease activity (32). We also showed that the toxin (now termed fragilysin) disrupts the paracellular barrier of cultured epithelial cell monolayers (31). Monolayers treated with fragilysin showed a time- and dose-dependent loss of the tight-junction protein ZO-1 and a concomitant decrease in electrical resistance. Furthermore, the effect appeared to be dependent on proteolytic activity outside the cell, as inhibitors of cell-mediated endocytosis did not prevent the toxin’s effect. Together, these data suggest that the enterotoxic activity of fragilysin is due to disruption of the paracellular barrier of the intestinal epithelium, possibly by proteolytic degradation of the tight-junction proteins.
We recently reported cloning and sequencing of the fragilysin toxin gene from a cosmid library of enterotoxigenic B. fragilis strain VPI 13784 (18). The toxin gene encodes a preprotoxin of 44 kDa. The preprotoxin contains a potential N-terminal signal peptide characteristic of bacterial lipoproteins and a 22-kDa prosequence (46). The protoxin is cleaved at an Arg-Ala site to release the 20-kDa extracellular metalloprotease.
In recent years it has emerged that virulence genes of pathogenic bacteria are often clustered within definable genetic elements termed pathogenicity islands (8, 10–12, 19). We were, therefore, interested in whether the fragilysin gene is associated with other virulence genes in a pathogenicity island.
Definition of the pathogenicity islet and analysis of the site of integration.
In order to determine if the fragilysin gene of enterotoxigenic B. fragilis strain VPI 13784 was contained on a pathogenicity island, we began sequencing DNA flanking the gene in cosmid clone 2c1, which we isolated in our previous study (18). To determine if we were still using DNA found only in enterotoxigenic strains, we periodically performed PCRs on the nontoxigenic B. fragilis strain VPI 2553 with primers facing inward with respect to the fragilysin gene. Eventually, with primers LO1 (5′ CCACCGTGCCAATGTCAGATA) and RO1 (5′ CTGAAGAACGAGGCGGTATC) we observed a PCR product of approximately 350 bp, suggesting we had sequenced past the ends of an element. From this analysis we were able to predict that the fragilysin gene was contained in an element of approximately 6 kb, which we termed the fragilysin pathogenicity islet (Fig. 1).
FIG. 1.
Schematic of the fragilysin pathogenicity islet. ORFs are represented by thick arrows. Small arrows at the ends represent direct repeats. Open boxes at the ends represent DNA outside the islet, which is also present in nontoxigenic B. fragilis. Restriction sites are BamHI (B), EcoRI (E), PstI (P), SacI (Sc), SmaI (Sm), XmnI (X), HindIII (H), and NdeI (N).
In order to define the ends of the pathogenicity islet, we sequenced the PCR product generated from nontoxigenic strain VPI 2553. The precise ends were then determined by comparison of the sequence from the nontoxigenic strain with the sequence from enterotoxigenic strain VPI 13784 near the predicted ends of the element (Fig. 2). Alignment of the sequences revealed the presence of a 17-bp sequence from the nontoxigenic strain that did not match any portion of the DNA sequence from the toxigenic strain. The sequences flanking the 17-bp sequence, however, aligned nearly perfectly with DNA flanking the element, allowing precise definition of the ends of the pathogenicity islet. Based on this alignment, we defined the pathogenicity islet of VPI 13784 as 6,033 bp in length. The islet contained nearly perfect direct repeats of 12 bp close to its ends.
FIG. 2.
Nucleotide sequences used to define the ends of the fragilysin pathogenicity islet. The nontoxigenic sequence was from B. fragilis VPI 2553. Toxigenic sequences across the left and right ends of the pathogenicity islet were from enterotoxigenic B. fragilis strain VPI 13784. Lowercase letters represent where the sequence from the nontoxigenic strain varied from the sequence flanking the ends of the islet. A 17-bp sequence present only in DNA from the nontoxigenic strain is boxed. Arrows indicate the ends of the islet and corresponding nucleotide number. Direct repeats (DR) are underlined.
In order to compare the pathogenicity islet ends and site of insertion in other strains, we sequenced PCR products across the islet ends of two additional enterotoxigenic B. fragilis strains, 86-5443-2-2 and VPI 4932. Primer pairs LO1-LI1 (5′ GGCCAAGGATGGTGTTC) and RI1 (5′ ATACTTATCCCATTTGTCC)-RO1 were used to generate DNA for the sequencing reactions. The sequence of each strain across these regions was identical to the sequence of VPI 13784.
To further determine if the fragilysin pathogenicity islet is integrated at the same position on the chromosome, we screened 20 additional enterotoxigenic strains with primer pairs LO1-LI2 (5′ GCACTTGGGATTCCGGTA) and RI1-RO1, flanking the left and right ends of the islet, respectively. The expected lengths for the PCR products were 1,485 bp for the left-end reaction and 1,229 bp for the right-end reaction. PCRs with all 20 strains produced identical products of the predicted length for each primer pair tested. Enterotoxigenic B. fragilis strains used were as follows: from the Virginia Polytechnic Institute Anaerobe Collection, VPI 2554, 2633, 13760, 13784, 13785, 13919, 13920, 14317, 14315, 14318, 43858, 43859, and 43860; from Johns Hopkins, JH 1912, 2330, 2333, 2326, 5-2, and 5-200; from Gifu Anaerobic Institute, GAI 10-1-5, 20422, and 20283; and from the Veterinary Research Laboratory, Montana State University, strain 86-5443-2-2.
To determine if the site of integration in other nontoxigenic strains was similar to that in VPI 2553, we sequenced PCR products of the same region of the chromosome from two additional B. fragilis strains, VPI 3156 and VPI 6815. Primers LO1 and RO1 were used to generate DNA for sequencing. The sequence of each nontoxigenic strain was identical to the sequence of the PCR product from VPI 2553.
Sequence of a putative second metalloprotease (MP II) and comparison to fragilysin.
An open reading frame (ORF) of 1,188 bp encoding a predicted protein of 396 amino acids was located 1,676 bp upstream of the fragilysin gene (Fig. 3). The predicted protein had a calculated molecular weight of 44,396 and a pI of 5.26, compared to a calculated molecular weight of 44,402 and pI of 5.08 for fragilysin. Furthermore, the deduced amino acid sequence contained a zinc-binding motif and methionine-turn characteristic of the metzincins (3). The N terminus contained an 18-amino-acid hydrophobic sequence similar to signal peptides found in bacterial lipoproteins, a feature also observed for fragilysin (9, 18, 46). An Arg-Ala site was located near the middle of the predicted protein, in a position similar to the processing site of fragilysin. If processed at this site the released product would be a 183-residue protein (Mr, 20,446) with a pI of 5.49; by comparison, extracellular fragilysin is a 186-residue protein (Mr, 20,680) with a pI of 4.71.
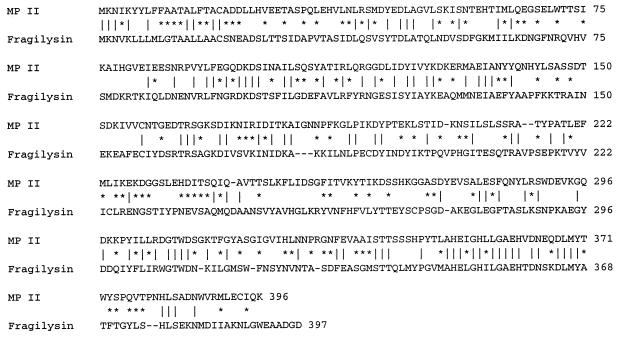
FIG. 3.
Alignment of the predicted amino acid sequences of MP II and fragilysin. |, identical residues; *, conserved substitutions.
A search of the protein data banks revealed that the predicted amino acid sequence of the MP II ORF contained significant homology to a number of metalloproteases, including mammalian matrixins, snake venom proteases, and fragilysin. Alignment of the amino acid sequences of MP II and fragilysin revealed 28.5% identity and 56.3% similarity, when conserved substitutions are considered. Of note, one of the nonconserved residues was at the position immediately following the third histidine of the zinc-binding motif. In fragilysin there is a threonine at this position, while MP II contains a valine. This residue has been used to group other metzincins into families (42).
Primers from divergent regions of the putative MP II and fragilysin genes were used to screen the 23 enterotoxigenic B. fragilis strains used in this study. The expected PCR products were 548 bp for the ORF of MP II with primer pair M1 (5′ GAGGGCTCTGAACTATGGACAAC)-M2 (5′ AAAGAAGTGGTGACAGCCTGAA) and 859 bp for the fragilysin gene with primer pair F1 (5′ TGGGAGATGAGTTCGCAGTATTA-F2 (5′ CCAACCGAGATTTTTAGCGATTAT). All 23 strains contained the MP II and fragilysin genes by this criterion. Several nontoxigenic strains were tested and showed no reaction product with either set of primers.
ORF1, located near the 5′ end of the fragilysin gene, encoded a predicted protein with homology to a snake cytotoxin and was reported in our previous study (18). Apart from this ORF, the MP II ORF, and the fragilysin gene, no other ORFs of over 200 nucleotides were present in the pathogenicity islet. The noncoding regions of the pathogenicity islet contained limited homology to the long genome of the Saccharomyces cerevisiae mitochondria within a region of clustered tRNA genes (47). The homology, however, was in noncoding regions, and homology to structural tRNA genes was not found. The islet of VPI 13784 had a GC content of 35%, compared with 53 and 47% for the 400 bp flanking the left and right ends of the islet, respectively, and an estimated 43% for the genome of B. fragilis (15). The regions flanking the islet did not reveal significant homology to any entries in the databases.
Pathogenicity islands contain a number of distinguishing features which have been outlined in recent reviews (8, 10–12, 19). In the case of smaller elements, containing only one or a few genes, they have been referred to as pathogenicity islets (11). The pathogenicity islet of enterotoxigenic B. fragilis has a number of features common to pathogenicity islands from other gram-negative pathogens. It represents a distinct genetic unit which contains the fragilysin toxin gene and the gene for a second potential virulence-associated metalloprotease. It has a lower GC content than the rest of the chromosome. Furthermore, it is flanked by direct repeats, although the repeats are not located at the exact ends of the element and may not be functionally or evolutionarily equivalent to those found in other pathogenicity islands. Finally, it is located at a specific position on the B. fragilis chromosome. The fragilysin pathogenicity islet, therefore, joins a growing list of defined virulence-associated genetic elements which pathogenic bacteria have acquired by horizontal gene transfer during microbial evolution.
Our sequence analysis of the chromosome at the site of integration in nontoxigenic strains revealed the presence of a GC-rich 17-bp segment which was not present in enterotoxigenic strains. The 17-bp sequence may be a target site for the integration of the fragilysin pathogenicity islet. Nontoxigenic strains of Clostridium difficile contain a 127-bp sequence which is not found in toxigenic strains (13). The sequence has been proposed as a target for integration of the C. difficile toxigenic element, which contains the genes for toxins A and B, as well as the txeR gene, which regulates production of the toxins (13, 21).
While we may think of the element containing the fragilysin gene in terms of pathogenicity, there may be another aspect to consider. The human gut flora is composed of more than 400 species of bacteria, making it an exceedingly complex environment. Accordingly, there is intense competition for nutrients. Microorganisms which survive in the gut, therefore, must have effective means of obtaining nutrients that are in short supply. In this regard, the acquisition of metalloprotease genes may provide a nutritional advantage to enterotoxigenic strains of B. fragilis, due to increased access to essential peptides or amino acids. Thus, the pathogenicity islet could also be thought of as a nutritional islet, the presence of which coincidentally confers on B. fragilis the ability to disrupt the paracellular barrier and cause diarrhea.
Enterotoxigenic B. fragilis has been isolated from both healthy and symptomatic individuals and appears to be common and widespread (2, 16, 17, 20, 27, 34, 35, 37, 38). While there is evidence that it causes diarrhea in children aged 1 to 5, its role as a causative agent of diarrhea in adults remains unclear. With regard to nonintestinal disease caused by B. fragilis, Kato et al. showed an increased association of enterotoxigenic B. fragilis with extraintestinal infections, including bacteremias (16, 17). More recently, Aucher et al. described a case of neonatal meningitis caused by enterotoxigenic B. fragilis (2). Of note, the convalescent-phase sera of the patient reacted strongly with a ca. 45-kDa protein which appeared to be unique to the toxigenic strain. The role, however, of enterotoxigenic B. fragilis metalloproteases in extraintestinal infections, if any, remains to be determined.
Franco et al. cloned and characterized a B. fragilis metalloprotease toxin gene from strain 86-5443-2-2 (9). The reported sequence was 92% identical and 95.4% similar to the deduced amino acid sequence of the fragilysin toxin gene from VPI 13784 (18). The authors proposed the existence of two alleles, bft-1 (VPI 13784) and bft-2 (86-5443-2-2), based on hybridization of enterotoxigenic strains of B. fragilis with oligonucleotide probes from a divergent region of the two toxin genes. Of 139 enterotoxigenic strains screened, 49% hybridized with the bft-1 probe and 51% hybridized with the bft-2 probe. None of the strains hybridized with both probes. We should emphasize that the sequence of the putative second metalloprotease, identified in this study, is only 28.5% identical to fragilysin. Therefore, the 86-5443-2-2 toxin described by Franco et al. is clearly a variant of fragilysin and not the second metalloprotease.
The presence of the putative second metalloprotease gene in the pathogenicity islet raises a number of intriguing questions. Does enterotoxigenic B. fragilis express a second metalloprotease similar to fragilysin? If so, does the second metalloprotease have toxic properties similar to fragilysin? Do the two metalloproteases act synergistically in vivo? Our future research will focus on answering these questions.
Cosmid clone 2c1 used for sequencing was isolated by the alkaline lysis method followed by CsCl gradient purification (40). All other sequence data were determined by direct sequencing of PCR products. Sequencing was performed by fluorescent automated DNA sequence analysis at Commonwealth Biotechnologies, Richmond, Va., and the University of Iowa DNA facility, Iowa City. All nucleotide and protein sequence data were compiled and analyzed with the software package Lasergene (DNAStar, Inc., Madison, Wis.). Additional analysis of sequence data was performed with a basic local alignment search tool (1).
Nucleotide sequence accession numbers.
The GenBank accession numbers of the B. fragilis VPI 13784 pathogenicity islet sequence and the integration site of nontoxigenic VPI 2553 are AF038459 and AF038460, respectively.
Acknowledgments
This work was supported by Public Health Service grant AI322940 from the National Institute of Allergy and Infectious Diseases.
The JH and GAI B. fragilis strains were kindly provided by Cynthia Sears of Johns Hopkins University and Naoki Kato of the Gifu Anaerobic Institute. Strain 86-5443-2-2 was a generous gift from Lyle L. Myers, Montana State University. We thank Phillip Schwartz for technical assistance.
REFERENCES
- 1.Altschul S F, Gish W, Miller W, Myers G W, Lipman D J. Basic local alignment search tool. J Mol Biol. 1991;215:403–410. doi: 10.1016/S0022-2836(05)80360-2. [DOI] [PubMed] [Google Scholar]
- 2.Aucher P, Saunier J P, Grollier G, Sebald M, Fauchere F L. Meningitis due to enterotoxigenic Bacteroides fragilis. Eur J Clin Microbiol Infect Dis. 1996;15:820–823. doi: 10.1007/BF01701527. [DOI] [PubMed] [Google Scholar]
- 3.Bode W, Gomis-Ruth F, Stockler W. Astacins, serralysins, snake venom and matrix metalloproteses exhibit identical zinc-binding environments (HEXXHXXGXXH and met-turn) and topologies and should be grouped into a common family, ‘the metzincins.‘. FEBS Lett. 1993;331:134–140. doi: 10.1016/0014-5793(93)80312-i. [DOI] [PubMed] [Google Scholar]
- 4.Border M, Firehammer B D, Shoop D S, Myers L L. Isolation of Bacteroides fragilis from feces of diarrheic calves and lambs. J Clin Microbiol. 1985;21:472–473. doi: 10.1128/jcm.21.3.472-473.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Collins J E, Bergeland M E, Myers L L, Shoop D S. Exfoliating colitis associated with enterotoxigenic Bacteroides fragilis in a piglet. J Vet Diagn Invest. 1989;1:349–351. doi: 10.1177/104063878900100413. [DOI] [PubMed] [Google Scholar]
- 6.Donelli G, Fabbri A, Fiorentini C. Bacteroides fragilis enterotoxin induces cytoskeletal changes and surface blebbing in HT-29 cells. Infect Immun. 1996;64:113–119. doi: 10.1128/iai.64.1.113-119.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Duimstra J R, Myers L L, Collins J E, Benfield D A, Shoop D S, Bradbury W C. Enterovirulence of enterotoxigenic Bacteroides fragilis in gnotobiotic pigs. Vet Pathol. 1991;28:514–518. doi: 10.1177/030098589102800608. [DOI] [PubMed] [Google Scholar]
- 8.Finlay B B, Falkow S. Common themes in microbial pathogenicity revisited. Microbiol Mol Biol Rev. 1997;61:136–169. doi: 10.1128/mmbr.61.2.136-169.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Franco A A, Mundy L M, Trucksis M, Wu S, Kaper J B, Sears C L. Cloning and characterization of the Bacteroides fragilis metalloprotease toxin gene. Infect Immun. 1997;65:1007–1013. doi: 10.1128/iai.65.3.1007-1013.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Groisman E A, Ochman H. Pathogenicity islands: bacterial evolution in quantum leaps. Cell. 1996;87:791–794. doi: 10.1016/s0092-8674(00)81985-6. [DOI] [PubMed] [Google Scholar]
- 11.Groisman E A, Ochman H. How Salmonella became a pathogen. Trends Microbiol. 1997;5:343–349. doi: 10.1016/S0966-842X(97)01099-8. [DOI] [PubMed] [Google Scholar]
- 12.Hacker J, Blum-Oehler G, Muhldorfer I, Tschape H. Pathogenicity islands of virulent bacteria: structure, function and impact on microbial evolution. Mol Microbiol. 1997;23:1089–1097. doi: 10.1046/j.1365-2958.1997.3101672.x. [DOI] [PubMed] [Google Scholar]
- 13.Hammond, G. A., and J. L. Johnson. The toxigenic element of Clostridium difficile strain VPI 10463. Microb. Pathog. 19:203–213. [DOI] [PubMed]
- 14.Hofstad T. Virulence factors in anaerobic bacteria. Eur J Clin Microbiol Infect Dis. 1992;11:1044. doi: 10.1007/BF01967797. [DOI] [PubMed] [Google Scholar]
- 15.Holdeman L V, Kelley R W, Moore W E C. Genus I. Bacteroides, Castellani and Cholmers 1919, 959AL. In: Krieg N R, Holt J G, editors. Bergey’s manual of systematic bacteriology. Vol. 1. Baltimore, Md: The Williams & Wilkins Co.; 1984. pp. 604–631. [Google Scholar]
- 16.Kato, N., A. Karuniawati, R. Jotwani, H. Kato, K. Watanabe, and K. Ueno. 1995. Isolation of enterotoxigenic Bacteroides fragilis from extraintestinal sites by cell culture assay. Clin. Infect. Dis. 20(Suppl. 2):S41. [DOI] [PubMed]
- 17.Kato, N., H. Kato, K. Watanabe, and K. Ueno. 1996. Association of enterotoxigenic Bacteroides fragilis with bacteremia. Clin. Infect. Dis. 23(Suppl.):S83–S86. [DOI] [PubMed]
- 18.Kling J J, Wright R L, Moncrief J S, Wilkins T D. Cloning and characterization of the gene for the metalloprotease enterotoxin of Bacteroides fragilis. FEMS Microbiol Lett. 1997;146:279–284. doi: 10.1016/s0378-1097(96)00488-0. [DOI] [PubMed] [Google Scholar]
- 19.Mecsas J J, Strauss E J. Molecular mechanisms of bacterial pathogenesis: type III secretion systems and pathogenicity islands. Emerg Infect Dis. 1996;2:270–288. doi: 10.3201/eid0204.960403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Meisel-Mikulajczyk F, Sebald M, Torbicka E, Rafalowska K, Zielinska U. Isolation of enterotoxigenic Bacteroides fragilis strains in Poland. Acta Microbiol Pol. 1994;43:389–392. [PubMed] [Google Scholar]
- 21.Moncrief J S, Barroso L A, Wilkins T D. Positive regulation of Clostridium difficile toxins. Infect Immun. 1997;65:1105–1108. doi: 10.1128/iai.65.3.1105-1108.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moncrief J S, Obiso R, Jr, Barroso L A, Kling J J, Wright R L, Van Tassell R L, Lyerly D W, Wilkins T D. The enterotoxin of Bacteroides fragilis is a metalloprotease. Infect Immun. 1995;63:175–181. doi: 10.1128/iai.63.1.175-181.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moore W E C, Cato E P, Holdeman L V. Some current concepts in intestinal bacteriology. Am J Clin Nutr. 1978;31:S33–S42. doi: 10.1093/ajcn/31.10.S33. [DOI] [PubMed] [Google Scholar]
- 24.Myers L L, Firehammer B D, Shoop D S, Border M M. Bacteroides fragilis: a possible cause of acute diarrheal disease in newborn lambs. Infect Immun. 1984;44:241–244. doi: 10.1128/iai.44.2.241-244.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Myers L L, Shoop D S. Association of enterotoxigenic Bacteroides fragilis with diarrheal disease in young piglets. Am J Vet Res. 1987;48:774–775. [PubMed] [Google Scholar]
- 26.Myers L L, Shoop D S, Byars T B. Diarrhea associated with enterotoxigenic Bacteroides fragilis in foals. Am J Vet Res. 1987;48:1565–1567. [PubMed] [Google Scholar]
- 27.Myers L L, Shoop D S, Stackhouse L L, Newman F S, Flaherty R J, Letson G W, Sack R B. Isolation of enterotoxigenic Bacteroides fragilis from humans with diarrhea. J Infect Dis. 1987;152:1344–1347. doi: 10.1128/jcm.25.12.2330-2333.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Myers L L, Shoop D S, Collins J E, Bradbury W C. Diarrheal disease caused by enterotoxigenic Bacteroides fragilis in infant rabbits. J Clin Microbiol. 1989;27:2025–2030. doi: 10.1128/jcm.27.9.2025-2030.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Myers L L, Shoop D S, Collins J E. Rabbit model to evaluate enterovirulence of Bacteroides fragilis. J Clin Microbiol. 1990;28:1658–1660. doi: 10.1128/jcm.28.7.1658-1660.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Myers L L, Collins J E, Shoop D S. Ultrastructural lesions of enterotoxigenic Bacteroides fragilis. Vet Pathol. 1991;28:336–338. doi: 10.1177/030098589102800411. [DOI] [PubMed] [Google Scholar]
- 31.Obiso R J, Jr, Azghani A O, Wilkins T D. The Bacteroides fragilis toxin fragilysin disrupts the paracellular barrier of epithelial cells. Infect Immun. 1997;65:1431–1439. doi: 10.1128/iai.65.4.1431-1439.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Obiso R J, Jr, Lyerly D M, Van Tassell R L, Wilkins T D. Proteolytic activity of the Bacteroides fragilis enterotoxin causes fluid secretion and intestinal damage in vivo. Infect Immun. 1995;63:3820–3826. doi: 10.1128/iai.63.10.3820-3826.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Otto B R, Sparrius M, Verweij-van Vught A M J J, MacLaren D M. Iron-regulated outer membrane protein of Bacteroides fragilis involved in heme uptake. Infect Immun. 1990;58:3954–3958. doi: 10.1128/iai.58.12.3954-3958.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pantosti A, Piersimoni C, Perissi G. Detection of Bacteroides fragilis enterotoxin in the feces of a child with diarrhea. J Clin Dis. 1994;19:809–810. doi: 10.1093/clinids/19.4.809. [DOI] [PubMed] [Google Scholar]
- 35.Pantosti A, Cerquetti M, Colongel R, D’Ambrosio F. Detection of intestinal and extraintestinal strains of enterotoxigenic Bacteroides fragilis by the HT-29 cytotoxicity assay. J Med Microbiol. 1994;41:191–196. doi: 10.1099/00222615-41-3-191. [DOI] [PubMed] [Google Scholar]
- 36.Polk B F, Kasper D L. Bacteroides fragilis subspecies in clinical isolates. Ann Intern Med. 1977;86:569–571. doi: 10.7326/0003-4819-86-5-569. [DOI] [PubMed] [Google Scholar]
- 37.Sack R B, Albert M J, Alam K, Neogi P K B, Akbar M S. Isolation of enterotoxigenic Bacteroides fragilis from Bangladeshi children with diarrhea: a controlled study. J Clin Microbiol. 1994;32:960–963. doi: 10.1128/jcm.32.4.960-963.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sack R B, Myers L L, Aleido-Hill J, Shoop D S, Bradbury W C, Reidand R, Santasham M. Enterotoxigenic Bacteroides fragilis: epidemiological studies of its role as a human pathogen. J Diarrhoeal Dis Res. 1992;10:4–9. [PubMed] [Google Scholar]
- 39.Saidi R F, Sears C L. Bacteroides fragilis toxin rapidly intoxicates human intestinal epithelial cells (HT29/C1) in vitro. Infect Immun. 1996;64:5029–5034. doi: 10.1128/iai.64.12.5029-5034.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sambrook J, Fritsch E F, Maniatis T. Molecular cloning: a laboratory manual. 2nd ed. Cold Spring Harbor, N.Y: Cold Spring Harbor Laboratory Press; 1989. [Google Scholar]
- 41.San Joaquin V H, Griffis J C, Lee C, Sears C L. Association of Bacteroides fragilis with childhood diarrhea. Scand J Infect Dis. 1995;27:211–215. doi: 10.3109/00365549509019011. [DOI] [PubMed] [Google Scholar]
- 42.Stocker W L, Grams F, Bauman U, Reiner P, Gomis-Ruth F X, McKay D B, Bode W. The metzincins—topological and sequential relations between the astacins, adamalysins, serralysins, and matrixins (collagenases) define a superfamily of zinc peptidases. Protein Sci. 1995;4:823–840. doi: 10.1002/pro.5560040502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tzianabos A O, Onderdonk A B, Smith R S, Kasper D L. Structure-function relationships for polysaccharide-induced intra-abdominal abscesses. Infect Immun. 1994;62:3590–3593. doi: 10.1128/iai.62.8.3590-3593.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Van Tassell R L, Lyerly D M, Wilkins T D. Purification and characterization of an enterotoxin from Bacteroides fragilis. Infect Immun. 1992;60:1343–1350. doi: 10.1128/iai.60.4.1343-1350.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Weikel C S, Grieco F D, Reuben J, Myers L L, Sack R B. Human colonic epithelial cells, HT29/C1, treated with crude Bacteroides fragilis enterotoxin dramatically alter their morphology. Infect Immun. 1992;60:321–327. doi: 10.1128/iai.60.2.321-327.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wu H C, Tokunaga M. Biogenesis of lipoproteins in bacteria. Curr Top Microbiol Immunol. 1986;125:127–157. doi: 10.1007/978-3-642-71251-7_9. [DOI] [PubMed] [Google Scholar]
- 47.Zamaroczy M, Bernardi G. The primary structure of the mitochondrial genome of Saccharomyces cerevisiae—a review. Gene. 1986;47:155–177. doi: 10.1016/0378-1119(86)90060-0. [DOI] [PubMed] [Google Scholar]