Abstract
Choking (or foreign body airway obstruction) is a widespread phenomenon with serious consequences of morbidity and mortality. Choking (often also called suffocation) can be caused by food or inedible objects and leads to various degrees of asphyxiation or lack of oxygen in the blood stream. The incidence is very high in both young children and adults, especially seniors. However, since not all choking episodes end up in the emergency room or become fatalities, they often escape statistics. Although episodes of choking from non-edible bodies are infrequent, they affect mostly young children. Three of the most common risks for choking in general are neurological disorders, dysphagia and dental issues (few or no teeth, unstable or unsuitable prosthesis or orthodontic appliances). The purpose of this study was to evaluate the risk factors of choking and ways to reduce/avoid this event. We reported data on a series of 138 patients admitted to the emergency department following a choking event, at a hospital in Rome, Italy. The age group of the analyzed population ranged from 1 to 88 years, with the most represented age group of these between 40 and 59, with a similar distribution between males and females. The types of foods on which people choked reflected the seasonal, traditional and local foods: 67% of patients reported choking on fish bones followed by meat bones (9%) and artichokes (3%). Three relevant non-food choking elements reported were: orthodontic items, toothpicks and pins (one occurrence each). We also reported on two clinical cases of patients choking on meat and a chicken bone. In conclusion, choking awareness and prevention are essential for implementing potential life-saving precautions. Prevention is the first tool to reduce the occurrence of this event, therefore it is necessary to analyze the risk factors and educate the population to eliminate them. Proper chewing and oral manipulation are paramount functions in preventing choking, along with meal-time supervision if little children and elderly. Then, it behooves the healthcare professionals to disseminate knowledge of emergency maneuvers (e.g., Heimlich maneuver) to be implemented in the event of choking.
Key Words: choking, foreign body, food, chewing, airway obstruction, prevention, Heimlich maneuver, children, adults
Ethical Publication Statement
We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Choking, also defined as foreign body airway obstruction (FBAO), is a phenomenon that occurs when a foreign body (food, little hard objects, candies, etc.) prevents the air passage in the respiratory tract.1 Technically, choking usually occurs when a person is eating (internal obstruction of the airways), as opposed to drowning in water, or suffocating (external obstruction of the airways) with a plastic bag or a pillow, or strangulation (external compression of the airways) with a sting or a scarf.2 An obstruction that prevents oxygen from entering the lungs results in oxygen deprivation (asphyxia), that often leads to life-long neurological consequences and death if not quickly solved. See Tables 1 and 2.
Table 1.
Strategies to prevent food choking.
| Babies-Toddlers-Children | • Breastfeed as long as possible • Introduce different textures and flavors during weaning, under supervision • Adopt the Baby-Led Weaning strategy when appropriate • Teach children the correct consistency of food well chewed: similar to a blended veggie soup • Cut grapes, olives and cherry tomatoes in half, lengthwise • Teach children it’s ok to spit out pits, seeds, bone fragments etc. • Teach children not to talk with their mouth full • Teach children not to run, laugh, stuff their mouths or play while eating • Provide a quiet, unhurried, environment during meals • Prevent distractions during meals, such as computer games • Be a model for your child: always eat something crunchy to promote better chewing and oral detection of foreign objects • Safety 1st Small Objects Choking Tester, is a simple device to determine how small is too small. Designed by the CPSC, Consumer Product Safety Commission. If an object fits entirely inside this Choking Tester, then it's a choking hazard to a child. |
| Adults and Elderly | • Eat slowly and let the saliva soak the food until the bolus has a soupy consistency • Practice mindful chewing to identify small changes in texture (seeds, dirt, plastic fragments etc.) • Cut the meat in small bites and chew them thoroughly • Avoid distractions and physical movements during meals (no TV, computers, walking or talking) • Cut hotdogs and sausages lengthwise and not in round thick slices. • Be mindful that dentures reduce the oral sensitivity to find smaller items such as little bones or veggies hard fibers • Excessive alcohol may impair oral sensitivity and motor performance • Chew well foods that are sticky: rice, wafers, peanut butter and avoid hard candies, especially round ones • Supervise the meals of anybody with neurological, psychiatric or neuromuscular issues • Don’t try to answer quickly and avoid laughing with your mouth full |
Approximately 66 to 77 children younger than 10 years die from choking on food each year in the United States. More than 10,000 ER visits annually can be attributed to choking on food among children aged 14 years and younger.3 Canada saw an increase in children’s choking death in 2006-2012 compared to past decades.4 In the USA, of over 76,000 deaths from choking, in adults over 65 years of age, 6.5% of deaths were classified ad food choking.5 A study conducted in San Diego County, indicated that many choking deaths were due to meat and 45% of choking episodes happened at home.6 According to the National Safety Council (NSC), in the US, choking is the 4th leading cause of unintentional deaths, with two-thirds of choking deaths happening in people over 75. The Office for UK National Statistics reported 289 deaths in 2016 because of choking, with a 17% increase from the year before, with 85% of those deaths being caused by food and with about 91% of all choking deaths happening to adults over 45 years of age. The extra-hospital mortality rate is about 36.4%. The in-hospital mortality rate for airway foreign bodies is between 0.26% and 13.6% after complications due to delayed hypoxia, a severe laryngeal edema or bronchospasm requiring a tracheotomy or re-intubation, pneumothorax, pneumomediastinum, cardiac arrest, tracheal or bronchial laceration, and hypoxic brain damage.7 Although these statistics are worrisome, anecdotally, the number of chocking episodes not resulting in ER visits and death certificates is much higher and almost anybody will experience some degree of choking episodes during a lifetime.
Table 2.
Strategies to prevent non-food choking.
| Babies-Toddlers-Children | • Keep small items away from children: marbles, balloons, hard candies, pebbles, buttons, small coins • Check for labels on little toys and toy parts. • Keep away objects that smell like food: eraser, toys, large pills • Avoid foods with little toys or inedible items inside • Learn the Abdominal Thrust (also known as the Heimlich Maneuver, see Figure 1) for babies and toddlers |
| Adults and Elderly | • Supervise and remove small items from anybody with neurological, psychiatric or neuromuscular disorders • Ensure better stability of the dentures and better dental occlusion • Improve saliva production • Beware of hard candies, especially round ones • Learn to perform the Abdominal Thrust (also known as the Heimlich Maneuver, see Figure 1) |
Causes and risk factors of choking deaths involving food are often related to traditional foods and cultural circumstances:
Eating some foods at birthday parties;8
Eating mochi rice cake in Japan;9
Eating nuts and seeds for “Autumn day” in Spain;10
Eating hot dogs in the USA;11
Eating at home more that at the restaurant;6
Choking tends to occur during eating due to the specific properties of some food (hot dogs, cut meat, hard candies, peanut butter, popcorn, chewing gum, marshmallows), especially in young children, whose choking may also be caused by inedible objects such as, coins, beads, balloons, little toys or parts of toys.
Consistency, texture and shape of the food bite can also be risk factors,12 such as pieces of food too big to be manipulated within the oral cavity (like a chunk of an apple), round and slippery foods (some hard gelatins), cylindrical foods or foods cut into rounds (hot dogs, carrots), hard foods (candies, some fruits), sticky foods (peanut butter, some candies, potatoes), fibrous foods (meat, celery) or compressible foods (cakes, bread).13
The risk depends not only on the type of food and its size, but also on the person's age, the amount taken and proper salivation. Indeed nuts, seeds, dry fruits are more dangerous in childhood (younger than 4) and in excessive amount (a pinch of them as opposed to a single one at the time). Air-way size foods: grapes, cherry tomatoes, apple chunks, carrots are only dangerous when they are too big to be chewed or not chewed properly. Saliva is of paramount importance in food bolus oral manipulation and formation and therefore in choking and yet we still don’t have good data on the impact of xerostomia (qualitative and quantitative changes in saliva) as well as the proper amount of saliva required to create a cohesive food bolus, easy to manipulate orally and swallow safely.14 The differences in risk between adults and children are also due to the different anatomy of the respiratory tract. The upper and lower airways of infants and children are smaller in diameter than in adults. They are shorter and positioned more anteriorly in the neck. The tongue is very thick in relation to the oropharynx. The trachea is very short and has little cartilaginous support. Mild edema or limited obstruction can reduce the diameter of the airways and determine a respiratory insufficiency. Moreover, children have an intense metabolic activity, the oxygen consumption in infants is twice that of adults, consequently, hypoxia develops more rapidly in the presence of respiratory insufficiency.
Especially in the adult patient, there are many risk factors that increase the risk of suffocation:
Fig 1.
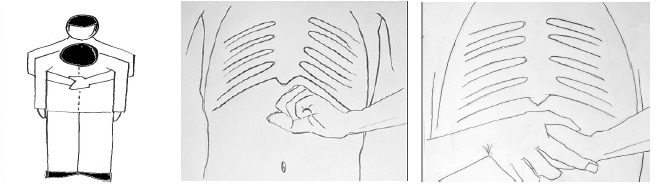
The Heimlich maneuver can be a life-saving rescue technique, but it should only be used if the person can’t breathe and is conscious (Panels left, central, right). It can be used on adults and children but isn’t recommended for infants, for whom a different maneuver needs to be implemented. (Image realized by Dr. Samuele Mafucci Orlandini).
Neurological, neuromuscular or psychiatric diseases (Dementia, Alzheimer’s, Parkinson’s, ALS, MS, Schizophrenia, ADHD, etc. (https://www.dhs.state.il.us/page.aspx?item=73374)24
Dysphagia (which can be both a risk factor or a consequence)
Lung/breathing diseases or conditions (Emphysema, COPD, Asthma etc)
Chronic obstructive sleep apnea
Allergic reactions that cause swelling of the throat
Excessive use of alcohol and/or drugs
Risky behaviors (eating contests, dares, bravado)
Use of certain medications that impact consciousness, alertness, sensory-motor coordination and that increase fatigue
Surgery that compromised the integrity of the oro-pharyngolaryngeal complex
In particular, individuals with developmental disabilities, but also some institutionalized elderly people, can have increased choking risk because of:
Decreased or absent protective airway reflexes.17
Decreased or disordered breathing/swallowing
Poor coordination and oral stage dysphagia
Poor or underdeveloped oral motor skills
Gastro-esophageal reflux disorder (GERD)
Epileptic seizures
Inability to swallow certain fluid consistencies and/or food textures
-Medication side effects
Dental or skeletal malocclusion
Impaired mobility
Often need for feeding assistance
Often inability to communicate problems in chewing, swallowing or protective mechanisms
Dental health has an impact of on choking too,18 due to teeth or muscle-related factors such as: orofacial/TMJ pain, denture instability, total dentures (upper and lower), severe malocclusion, edentulism or missing several teeth. For example, tooth loss or loose teeth is a chronic disability, which makes it difficult for patients to perform essential tasks such as chewing properly while eating.18 Dentures that cover the palate, impacting the lingual-palatal neurosensory interface, can make it difficult to sense whether the food is fully chewed before it is swallowed. If dentures fit poorly or hurt, individuals might not wear them, thus being unable to properly chew their food. In adults and in the elderly it is possible that some items get lodged at the laryngeal level, for example parts of dental prostheses. Small unfit temporary prosthesis may get dislodged during eating and get lodged instead in the upper airways often not closing them completely but causing distressing choking sensation.19
Materials and Methods
Between the years 2017-2018, we retrospectively assessed the records of 138 patients from the San Filippo Neri hospital in Rome, which is not specifically a pediatric hospital, with the purpose of finding a possible association between:
Patients’ age and type of foreign body causing a choking event
Patients’ gender and choking events
Presence of malocclusion and choking events
Presence of orthodontic devices, dentures and choking events
The data reported here belongs to patients admitted to the emergency room for instances of choking, later anonymized for statistical purposes (See Supplemental materials Figure 1,2,3,4,5). All patients included in this study self reported or were deemed to be healthy, with no known disease, neurological pathology or anatomical malformation. The study was conducted in accordance with the Declaration of Helsinki.
The limit for statistical significance was always considered p<0.05.
Results
The population analyzed ranged from 1 to 88 years of age, with the age of a segment (12%) of the sample not specified; 52% of the sample was female and 48% male, therefore the distribution is almost homogeneous. In this study, although a significant percentage of case files (13%) did not indicate the cause of the choking episode, the highest percentage (67%) of a foreign body responsible for choking was reportedly fish bones followed by meat bones (9%) and artichokes (3%), reflecting the choices of seasonal and traditional foods in the local area, while choking on fruit seeds, vegetables, popcorn was more unusual. Episodes of choking from inedible bodies were also reported, affecting one patient each: orthodontic devices, coins, tooth picks, pins and needles were indicated as a source of choking, with homogeneous frequency between males and females. Regarding the age of the patients reported to the ER for chocking, although 12% is not specified, children age from 1 to 19 represented 18% of the sample, 19% was between age 20 and 39, 31% was between age 40 and 59, and 20% was between age 60 and 88.
We also report two clinical cases which are not related to the previously sample, but describe typical cases.
Clinical Case 1
Female, 61 years. Total denture on upper jaw and partial denture on lower jaw. Reportedly she choked with a big bite of steak. She was saved thanks to the Abdominal Thrust Maneuver (also called the Heimlich Maneuver). Although the exact reasons why she had that choking episode were not clear, possible circumstances could have been: being in a hurry, total upper denture and partial lower denture which may reduce the sensory input (stereognosis) during chewing and swallowing, a possibly unstable set of dentures or worn out occlusal surfaces, or she did not chew the meat enough to reduce the size of the meat particles in the bolus (comminution). See Supplemental materials Figure 6.
Clinical Case 2
Female, 67-year-old, complete upper denture. She partially choked with a chicken bone, requiring ER intervention to dislodge the bone. Again, although the circumstances of the choking episode were not reported, it’s possible that the patient experienced lack of sensory input due to the upper denture, was eating in a hurry or did not chew the food adequately to allow the discrimination between the bolus ready to be swallowed and the little bone. See Supplemental materials Figure 7.
Discussion
The aspiration of a foreign body is a life-threatening emergency due to the accidental lodging of objects in the respiratory tract and represents a significant public health problem, sometimes resulting in fatal outcomes. To prevent injury, especially in the pediatric population, the vigilant supervision of young children during eating is essential. In fact, most choking episodes occur during meals and generally occur even in the presence of adults.21 The risk, in children, is related to the type of food ingested, its shape, consistency and quantity, and they should eat appropriate types of food according to their age. The first step to reduce cases of suffocation is prevention: in particular it is possible to focus attention on the correct chewing of the food. Chewing contributes to swallow initiation because sufficient food comminution leads to optimal cohesion with saliva, which is necessary for adequate food bolus formation, with a quick and safe passage through the pharynx into the esophagus, while bypassing the airway.22 Chewing and swallowing are different in newborns, in children, in different stages of life, all the way to the end of it. This means that adult chewing and adult swallowing are achieved by developing organs, functions, experiences and skills. In fact, age-related anatomy and function changes affect bolus formation and therefore swallowing.23
From 0 to 3 years of age, choking prevention can be also performed through breastfeeding on the first year, as breastfeeding primes the neuromuscular mechanics for future chewing. Also, the food should be natural, healthy, properly prepared, varied in textures and not only well-mashed or pureed. Training should be implemented as early as possible to allow children to detect and spit out small non-food items (bones, pits, large fibers etc.). In the age range of 4 to 12 years, proper chewing and prevention of choking should aim to improve muscles activity (respiration, swallowing, eating different type of food) and it is important to intercept malocclusion, which can affect and be affected by oro-nasal functions.
In children it is important to pay attention to orthodontic devices, while in adults particular attention must be paid to prostheses, by ensuring their integrity, stability and function. Anybody, not just healthcare practitioners, should learn to practice the Heimlich maneuver (abdominal thrust) on people experiencing a choking episode. The abdominal thrust maneuver can be performed in babies, children and adults by way of different techniques. One of the risk factors for FBAO (foreign body airway obstruction) in children is a lack of knowledge by caregivers, therefore prevention should include public education, including meal supervision and training of abdominal thrust techniques and cardiopulmonary resuscitation maneuvers in worst cases. Adults should pay attention to their own eating habits, the context in which they eat (restaurant, home, being in a hurry or distracted) and their way of taking, chewing and orally analyzing the food bolus, to avoid accidental aspiration.
Chocking is a frequently unreported phenomenon, affecting all ages, without much gender difference. This study confirmed the influence of food choices, mostly reflecting local cultural and seasonal foods. Because choking often leads to hospitalization and even death, prevention and awareness of this phenomenon are essential to reduce mortality. Prevention is the first tool to reduce the occurrence of this event, therefore it is necessary to analyze the risk factors and educate the population to eliminate them. Proper chewing and oral manipulation are paramount functions in preventing choking, along with meal-time supervision if little children and elderly. Oral and dental health, along with monitoring prostheses and orthodontic items are an essential aspect of preventing choking. Then, it behooves the healthcare professionals to disseminate knowledge of emergency maneuvers (e.g., Heimlich maneuver) to be implemented in the event of choking.
Acknowledgments
The authors are grateful to the partecipants for their kind cooperation and to Alessandro Molinello, Mario Toller and Danny D’Agostini for generous scientific assistance.
List of acronyms
- FBAO
Foreign body airway obstruction
- NSC
National Safety Council
- COPD
Disorder cronic obstructive polmonar
- CPSC
Consumer Product Safety Commission
- ADHD
Attention Deficit Hyperactivity Disorder
- ER
Emergency Rate
- GERD
Gastro-esophageal reflux disorder
Funding Statement
Funding: This research received no external funding.
Contributor Information
Stefano Saran, Email: ssaran@studenti.uninsubria.it.
Licia Coceani Paskay, Email: lcpaskay@gmail.com.
Martina De Luca, Email: martina.deluca97@hotmail.com.
Augusto Tricerri, Email: augusto.tricerri@aslroma1.it.
Samuele Mafucci Orlandini, Email: samuele.mafucciorlandini@policlinicogemelli.it.
Francesca Greco, Email: francescagreco.1@alice.it.
Giuseppe Messina, Email: giuseppe.messina@uniroma5.it.
References
- 1.Simpson E. How to manage a choking adult. Nurs Stand. 2016. Sep 14;31(3):42-46. doi: 10.7748/ns.2016.e10542. PMID: 27745052. [DOI] [PubMed] [Google Scholar]
- 2.Cyr C; Canadian Paediatric Society Injury Prevention Committee. Preventing choking and suffocation in children. Paediatr Child Health. 2012. Feb;17(2):91-4. doi: 10.1093/pch/17.2.91. PMID: 23372401; PMCID: PMC3299355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Friedman ML, Nitu ME. Acute Respiratory Failure in Children. Pediatr Ann. 2018. Jul 1;47(7):e268-e273. doi: 10.3928/19382359-20180625-01. PMID: 30001440. [DOI] [PubMed] [Google Scholar]
- 4.Wu WS, Sung KC, Cheng TJ, Lu TH. Associations between chronic diseases and choking deaths among older adults in the USA: a cross-sectional study using multiple cause mortality data from 2009 to 2013. BMJ Open. 2015. Nov 12;5(11):e009464. doi: 10.1136/bmjopen-2015-009464. PMID:26563213; PMCID: PMC4654350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dolkas L, Stanley C, Smith AM, Vilke GM. Deaths associated with choking in San Diego county. J Forensic Sci. 2007. Jan;52(1):176-9. doi: 10.1111/j.1556-4029.2006.00297.x. PMID: 17209932. [DOI] [PubMed] [Google Scholar]
- 6.Montana A, Salerno M, Feola A, Asmundo A, Di Nunno N, Casella F, Manno E, Colosimo F, Serra R, Di Mizio G. Risk Management and Recommendations for the Prevention of Fatal Foreign Body Aspiration: Four Cases Aged 1.5 to 3 Years and Mini-Review of the Literature. Int J Environ Res Public Health. 2020. Jun 30;17(13):4700. doi: 10.3390/ijerph17134700. PMID: 32629891; PMCID: PMC7369691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Matsubayashi T, Ueda M. Suicides and accidents on birthdays: Evidence from Japan. Soc Sci Med. 2016. Jun;159:61-72. doi: 10.1016/j.socscimed.2016.04.034. Epub 2016 Apr 29. PMID: 27173742. [DOI] [PubMed] [Google Scholar]
- 8.Kiyohara K, Sakai T, Nishiyama C, Nishiuchi T, Hayashi Y, Iwami T, Kitamura T. Epidemiology of Out-of-Hospital Cardiac Arrest Due to Suffocation Focusing on Suffocation Due to Japanese Rice Cake: A Population-Based Observational Study From the Utstein Osaka Project. J Epidemiol. 2018. Feb 5;28(2):67-74. doi: 10.2188/jea.JE20160179. Epub 2017 Oct 28. PMID: 29093354; PMCID: PMC5792229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lluna J, Olabarri M, Domènech A, Rubio B, Yagüe F, Benítez MT, Esparza MJ, Mintegi S; en representación del Comité de Seguridad y Prevención de Lesiones No Intencionadas en la Infancia de la Asociación Española de Pediatría. Recomendaciones sobre la prevención de aspiraciones de cuerpos extraños [Recommendations for the prevention of foreign body aspiration]. An Pediatr (Barc). 2017. Jan;86(1):50.e1-50.e6. Spanish. doi: 10.1016/j.anpedi.2016.04.013. Epub 2016 May 24. PMID: 27234822. [DOI] [PubMed] [Google Scholar]
- 10.American Academy of Pediatrics Committee on Child Health Financing. Medicaid policy statement. Pediatrics. 2005. Jul;116(1):274-80. doi: 10.1542/peds.2005-0891. Epub 2005 May 16. PMID: 15897340. [PubMed] [Google Scholar]
- 11.Levrini L, Bocchieri S, Mauceri F, Saran S, Carganico A, Zecca PA, Segù M. Chewing Efficiency Test in Subjects with Clear Aligners. Dent J (Basel). 2023. Mar 1;11(3):68. doi: 10.3390/dj11030068. PMID: 36975565; PMCID: PMC10047352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sahin A, Meteroglu F, Eren S, Celik Y. Inhalation of foreign bodies in children: experience of 22 years. J Trauma Acute Care Surg. 2013. Feb;74(2):658-63. doi: 10.1097/TA.0b013e3182789520. PMID: 23354266. [DOI] [PubMed] [Google Scholar]
- 13.Saccomanno S, Saran S, De Luca M, Fioretti P, Gallusi G. Prevention of malocclusion and the importance of early diagnosis in the Italian young population. Eur J Paediatr Dent. 2022. Sep;23(3):178-182. doi: 10.23804/ejpd.2022.23.03.02. PMID: 36172913. [DOI] [PubMed] [Google Scholar]
- 14.van der Bilt A, Engelen L, Pereira LJ, van der Glas HW, Abbink JH. Oral physiology and mastication. Physiol Behav. 2006. Aug 30;89(1):22-7. doi: 10.1016/j.physbeh.2006.01.025. Epub 2006 Mar 29. PMID: 16564557. [DOI] [PubMed] [Google Scholar]
- 15.Boyd KL, Saccomanno S, Coceani Paskay Hv L, Quinzi V, Marzo G. Maldevelopment of the cranio-facial-respiratory complex: A Darwinian perspective. Eur J Paediatr Dent. 2021. Sep;22(3):225-229. doi: 10.23804/ejpd.2021.22.03.9. PMID: 34544252. [DOI] [PubMed] [Google Scholar]
- 16.Gelb M, Montrose J, Paglia L, Saccomanno S, Quinzi V, Marzo G. Myofunctional therapy Part 2: Prevention of dentofacial disorders. Eur J Paediatr Dent. 2021. Jun;22(2):163-167. doi: 10.23804/ejpd.2021.22.02.15. PMID: 34238010. [DOI] [PubMed] [Google Scholar]
- 17.Kohyama K, Mioche L, Bourdiol P. Influence of age and dental status on chewing behaviour studied by EMG recordings during consumption of various food samples. Gerodontology. 2003. Jul;20(1):15-23. doi: 10.1111/j.1741-2358.2003.00015.x. PMID: 12926747. [DOI] [PubMed] [Google Scholar]
- 18.Xie Q, Ding T, Yang G. Rehabilitation of oral function with removable dentures--still an option? J Oral Rehabil. 2015. Mar;42(3):234-42. doi: 10.1111/joor.12246. Epub 2014 Oct 18. PMID: 25327636. [DOI] [PubMed] [Google Scholar]
- 19.Köse A, Kostak D, Aramagan E, Durak A, Seçkin NS, Dönmez SS, Melek H. Tracheobronchial foreign body aspiration: dental prosthesis. Case Rep Pulmonol. 2014;2014:465856. doi: 10.1155/2014/465856. Epub 2014 Aug 4. PMID: 25165606; PMCID: PMC4137749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sidell DR, Kim IA, Coker TR, Moreno C, Shapiro NL. Food choking hazards in children. Int J Pediatr Otorhinolaryngol. 2013. Dec;77(12):1940-6. doi: 10.1016/j.ijporl.2013.09.005. Epub 2013 Sep 12. PMID: 24113156. [DOI] [PubMed] [Google Scholar]
- 21.Chik KK, Miu TY, Chan CW. Foreign body aspiration in Hong Kong Chinese children. Hong Kong Med J. 2009. Feb;15(1):6-11. PMID: 19197090. [PubMed] [Google Scholar]
- 22.Saitoh E, Shibata S, Matsuo K, Baba M, Fujii W, Palmer JB. Chewing and food consistency: effects on bolus transport and swallow initiation. Dysphagia. 2007. Apr;22(2):100-7. doi: 10.1007/s00455-006-9060-5. Epub 2007 Feb 14. PMID: 17347905. [DOI] [PubMed] [Google Scholar]
- 23.Prinz JF, Lucas PW. An optimization model for mastication and swallowing in mammals. Proc Biol Sci. 1997. Dec 22;264(1389):1715-21. doi: 10.1098/rspb.1997.0238. PMID: 9447729; PMCID: PMC1688744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.IDHS Illinois Department of Human Services. JB Pritzker, Governor, Grace B. Hou, Secretary. https://www.dhs.state.il.us/page.aspx?item=73374 [Google Scholar]


