Abstract
Objectives
The aim of the present study was to report clinical findings, surgical complications and outcomes for previously hoarded cats treated surgically for otitis media-interna (OMI) and to investigate the risk factors for complications and poor outcomes.
Methods
A retrospective study was conducted of 58 cats from an institutional hoarding environment that underwent ventral bulla osteotomy (VBO).
Results
Inappetence was uncommon at presentation (9/58, 16%) compared with pruritus/alopecia (50%), nasopharyngeal signs (45%), otitis externa (OE) (79%) and otitis interna (OI) (ataxia ± head tilt/head excursions) in 40%. Purulent aural discharge occurred in 36% and polyps in 26%. The tympanic bulla wall was moderately or severely thickened radiographically in 38/108 (35%) ears. Cultures were positive for Streptococcus equi subspecies zooepidemicus in 26/48 (54%) cats. Of the 58 cats, 40 (69%) had complications after the first VBO and 19/30 (63%) after the second. Of 101 complications, 56 (55%), from 27/88 (31%) surgeries, were considered serious, including life-threatening perioperative complications in seven, OI in eight, prolonged anorexia in six and worsening of pruritus/alopecia in nine cases. Three cats developed xerostomia (dry mouth) after the second VBO. Pruritus/alopecia, nasopharyngeal signs, OE and purulent aural discharge resolved in a statistically significant proportion of cats but persisted in some. Full resolution of OI was uncommon. OI preoperatively, and surgery performed by a generalist (vs specialist) surgeon, were risk factors for OE at recheck (OI: odds ratio [OR] 4.35; 95% confidence interval [CI] 1.21–15.70; P = 0.02; surgery: OR 3.64; 95% CI 1.03–12.87; P = 0.045). No other prognostic indicators were identified. No variables tested were significantly associated with risk of serious complications or euthanasia.
Conclusions and relevance
Surgical management of chronic OMI was successful in most cases but was not benign and not always beneficial. The analysis was unable to identify clinically helpful outcome predictors. Optimal management of chronic feline OMI remains a challenge, particularly for animal shelters. Less invasive approaches and chronic medical management require further investigation.
Keywords: Otitis media, otitis interna, ventral bulla osteotomy, surgery, animal hoarding, complications, outcomes, Streptococcus equi subspecies zooepidemicus
Introduction
Feline otitis media (OM) can be a challenging diagnosis because it lacks specific clinical signs and often manifests as upper respiratory disease or otitis externa (OE).1,2 It is most often associated with ascending infection from the nasopharynx through the auditory (Eustachian) tube1,3 and may extend to cause otitis interna (OI).1,4,5 This causes the classic signs of peripheral vestibular disease (PVD) (nystagmus, head tilt/excursions and ataxia)2,4 that are likely to trigger suspicion of OM.
Stress and overcrowding predispose to upper respiratory infection (URI) in cats.6,7 Hoarding environments are high risk for chronic upper respiratory disease complex,8 –10 which can involve the nasal passages, nasopharynx, auditory tubes, paranasal sinuses and middle ear (for reference, see https://fankhauserblog.files.wordpress.com/1993/04/cat_head_xs_p4183384lbd.jpg and https://teachmeanatomy.info/head/organs/the-nose/paranasal-sinuses/). 11 Undiagnosed otitis media-interna (OMI) is common in cats with rhinitis,11,12 and concurrent sinonasal disease1,11,13,14 complicates the management of chronic OMI.
Surgical management has been reported for polyps,15,16 failed medical therapy,17,18 opacity in the tympanic cavity, thickening of the bulla wall and chronic OM. 5 , 19 When surgery is deemed necessary, ventral bulla osteotomy (VBO) is the surgery of choice in cats. This requires advanced surgical expertise, is expensive and time-consuming, and can be associated with significant complications.15–17,19–22
Chronic feline OMI is a Pandora’s box (‘a source of great and unexpected troubles’) for animal shelters. Failure to identify OMI has implications for both cats and adopters, but overdiagnosis is also a risk, and clinical management is problematic. There are no evidence-based guidelines for feline case management, nor are reliable prognostic indicators available.
It was the authors’ hope that this study would help resolve some of the decision-making dilemmas associated with chronic OMI. The aims of the present study were to report presenting signs, postoperative complications and outcomes in 58 previously hoarded cats treated surgically for OMI, and to identify the risk factors for complications and poor outcomes.
Materials and methods
Animals and study design
This retrospective observational study examined the records of cats from a single institutional hoarding environment (IHE)10,23 that were transferred to Toronto Humane Society (THS) between February 2017 and April 2019. THS is a large urban shelter, with a fully equipped veterinary hospital. Routine intake procedures included core vaccination, Wood’s lamp screening retroviral screening and treatment with selamectin and pyrantel.
OMI associated with Streptococcus equi suspecies zooepidemicus (SEZ) had previously been encountered in cats from another IHE. The index of suspicion was therefore high, and intake procedures included careful assessment for OMI. Shelter protocols for OMI and polyps were followed for suspected cases and included general anesthesia, otoscopic examination, examination of the nasopharynx for a polyp and radiographs of the tympanic bullae. CT was performed at a referral hospital on a case-by-case basis. Cultures were performed at the veterinarian’s discretion.
Cats were included if they originated from the same IHE, had been diagnosed with OMI and met the following retrospective confirmatory criteria: (1) clinical findings consistent with OMI; (2) diagnosis by a shelter veterinarian; and (3) bulla disease identified by either CT scan and/or radiographs interpreted by a boarded veterinary radiologist (SM), and/or visual confirmation at the time of VBO.
Case management
Initial therapy for all cases consisted of a broad-spectrum oral antibiotic and tris-EDTA-enrofloxacin-dexamethasone eardrops compounded in-house (tris-EDTA 9.8 ml, enrofloxacin [50 mg/ml]; 1.66 ml, dexamethasone phosphate [5 mg/ml] 0.32 ml). Prednisolone was prescribed as recommended for polyps, 20 and case by case at the clinician’s discretion for cats without polyps. Dexamethasone was administered perioperatively in selected cases. This was initially to help manage airway edema and subsequently to attempt to prevent it. There were no fixed criteria, and administration was based on the surgeon’s risk assessment. VBO surgeries were initially performed in-house, and subsequently by boarded surgeons at referral facilities. A protocolized veterinary examination (see file 1 in the supplementary material) was performed, typically under sedation, to assess the result of each VBO surgery. Results were recorded for the recheck time point as close as possible to 4 weeks after the final VBO.
Clinical findings and outcome measures
Preoperative findings were retrospectively classified (Table 1; see file 2 in the supplementary material for criteria). The case definition for OI/PVD was presence of head tilt/excursions and/or ataxia. Tympanic bulla wall thickening was scored by a boarded radiologist (SM). Surgical complications were classified based on a study by Smeak. 21 Complications were classified as serious if they were life-threatening, had functional consequences, and/or required intensive or prolonged care. Poor surgical outcomes were euthanasia, serious surgical complications and/or moderate/severe nasopharyngeal (NP) signs, moderate/severe OE or presence of OI at the postoperative recheck.
Table 1.
Clinical features of otitis media-interna before ventral bulla osteotomy surgery in 58 cats transferred from an institutional hoarding environment
| Variable | Classification | n (%) |
|---|---|---|
| Inappetence | Mild/moderate | 5 (8.6) |
| Severe | 4 (6.9) | |
| Pruritus/alopecia | Localized | 12 (21) |
| Generalized | 17 (29) | |
| Nasopharyngeal signs* | Moderate | 25 (43) |
| Severe | 1 (1.7) | |
| Otitis externa* | Moderate | 35 (60) |
| Severe | 11 (19) | |
| Aural discharge type | Dark/ceruminous | 30 (52) |
| Purulent | 21 (36) | |
| Tympanic membrane † | Bulging, inflamed | 13 (11) |
| Ruptured | 20 (17) | |
| Not visualized | 35 (30) | |
| Polyp ‡ | Aural | 6 (10) |
| Nasopharyngeal | 6 (10) | |
| Both aural and nasopharyngeal | 3 (5.2) | |
| Radiographic bulla wall thickening § | Moderate | 27 (25) |
| Severe | 11 (10) | |
| Horner’s syndrome | 1 (1.7) | |
| Nystagmus | 1 (1.7) | |
| Otitis interna (peripheral vestibular signs) | Head tilt/excursions | 22 (38) |
| Ataxia | 1 (1.7) | |
| Meningoencephalitis | 1 (1.7) |
For outcomes analysis, mild changes were grouped with normal findings for these variables
n = 116 ears
Polyps were found in the bulla at surgery in an additional three cats
n = 108 ears (four cats had CT only)
Data analysis
Data analysis used Microsoft Excel and MedCalc (https://www.medcalc.org/calc/odds_ratio.php). To create dichotomous variables for statistical analysis, mild NP signs, OE and bulla wall thickening were grouped with normal findings, and other abnormal categories were grouped together (for example, moderate and severe NP signs) (see file 2 in the supplementary material). McNemar’s test was used to test the null hypothesis that VBO did not result in resolution of clinical signs. ORs were used to quantify univariable relationships between factors relevant to clinical decision-making and outcomes/complications and were tested for significance using the Pearson c2 test. Significance was set at P <0.05.
Results
Study population
In total, 669 cats were transferred from the IHE during the study period. OMI was suspected in 95 (14%) cats and confirmed in 70. Nineteen cats with unconfirmed OMI were euthanized before confirmation, and six did not meet the case definition. Of the 70 cases, 59 were treated surgically and 11 medically. One was excluded because of surgical complications unrelated to OMI, leaving 58. The time from intake to surgery varied, but all cats received medical treatment before surgery.
Presenting signs and clinical findings
Of the 58 cats, 18 (31%) were feline immunodeficiency virus (FIV)-positive on point-of-care testing. Ear mites were suspected in 20/58 (34%) because of the nature of the aural exudate. The exudate from seven cats was examined microscopically and was positive for Otodectes mites in two. Mites were visualized on otoscopic examination in one cat.
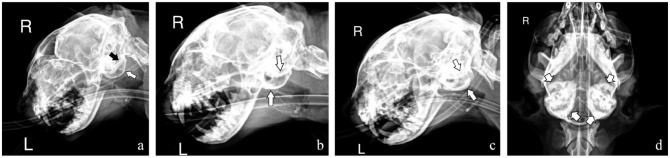
Nine cats (16%) exhibited inappetence (Table 1). Half had pruritus and/or alopecia, which extended beyond the head and neck in 17 (‘generalized’). In total, 26 (45%) cats had moderate/severe NP signs. Moderate/severe OE was common (46/58, 79%), with purulent discharge in 21 (36%) cats. Polyps were found in 15 (26%) cats. The tympanic membranes (TMs) were bulging/inflamed in 13/116 (11%) ears and ruptured in 20 (17%). Radiographically, there was increased opacity in one or both compartments of the tympanic cavity in 99/108 (92%) ears. The bulla wall was thickened in 98 (91%) ears. Thickening was mild in 60 (56%) ears, moderate in 27 (25%) and severe in 11 (10%) (Figure 1). Horner’s syndrome and nystagmus were uncommon (1/58 each, 1.7%). OI was present in 23 (40%) cats, of which 22 had head tilt/excursions.
Figure 1.
Radiographic images showing otitis media in previously hoarded cats. (a) Cat 10: left dorsal-right ventral oblique radiograph of the skull, showing mild bony thickening of the left tympanic bulla (white arrow) and severe bony thickening of the right tympanic bulla (black arrow) superimposed on the skull. (b) Cat 63: left dorsal-right ventral oblique radiograph of the skull, showing moderate bony thickening of both tympanic bullae (white arrows). (c) Cat 18: left dorsal-right ventral oblique radiograph of the skull, showing severe bony thickening of both tympanic bullae (white arrows). (d) Cat 58: ventrodorsal radiograph of the skull, showing severe bony thickening of both tympanic bullae (white arrows)
A total of 81 bacterial cultures were performed for 48 cats (15 ear canal, nine nasal, two pharyngeal, 33 from the bulla at the first VBO, 20 from the bulla at the second VBO and two from the bulla at revision surgery) (manuscript in preparation). Of 48 cats, 26 (54%) had at least one SEZ-positive culture and 8/48 (17%) had cultures that were exclusively positive for other species. There was no growth for 14/48 (29%) cats.
Surgical complications
Two of three cats that underwent simultaneous bilateral VBOs developed postoperative airway obstruction. One had multiple subsequent complications (wound abscess, aspiration pneumonia and prolonged anorexia) and the other developed prolonged anorexia. Both cats ultimately recovered. All subsequent bilateral VBOs were staged and performed at least 2 weeks apart.
Unilateral VBO was performed in 25/58 (43%) cats, staged bilateral in 30 (52%) cats and simultaneous bilateral in three (5.2%) cats. In total, 26 surgeries were performed by shelter veterinarians and 62 by specialist surgeons. Of the 58 cats, 40 (69%) had 65 complications after the first VBO and 19/30 (63%) had 36 complications after the second (Table 2). Of 101 complications, 56 (55%), from 27/88 surgeries (31%), were serious. The most frequent serious neurological complication was OI, in eight (14%) cats. Horner’s syndrome occurred in 41 (71%) cats and 52/88 (59%) surgeries and occurred after both VBOs in 11 cats.
Table 2.
Surgical complications after 88 ventral bulla osteotomies in 58 cats with otitis media-interna, transferred from an institutional hoarding environment
| Complication | Considered serious? | After first surgery (n = 58) | After second surgery (n = 30) |
|---|---|---|---|
| None | 18 (31) | 11 (37) | |
| Any complication | 40 (69) | 19 (63) | |
| Serious complication | 17 (29) | 10 (33) | |
| Life-threatening perioperative complications | |||
| Cardiac arrest | Y | 3 (5.2) | 0 |
| Dyspnea/upper airway obstruction – no tracheostomy/ventilation | Y | 2 (3.4) | 1 (3.3) |
| Dyspnea/upper airway obstruction – tracheostomy/ventilation | Y | 1 (1.7) | 0 |
| Severe hemorrhage | Y | 0 | 0 |
| Early postoperative complications (within 2 weeks)* | |||
| Acute wound infection | N | 1 (1.7) | 0 |
| Aspiration pneumonia | Y | 2 (3.4) | 0 |
| Congestion/cough/wheeze | Y | 2 (3.4) | 1 (3.3) |
| Nystagmus | N | 1 (1.7) | 1 (3.3) |
| Horner's syndrome | N | 35 (60) | 17 (57) |
| Otitis interna | Y | 5 (8.6) | 3 (10) |
| Head tilt/excursions | 4 (6.9) | 3 (10) | |
| Ataxia | 4 (6.9) | 3 (10) | |
| Meningoencephalitis † | Y | 1 ‡ (1.7) | 0 |
| Prolonged complications (persisted >2 weeks postoperatively a | |||
| Alopecia/pruritus* | Y | 6 (10) | 3 (10) |
| Chronic wound infection | Y | 0 | 0 |
| New anorexia (>1 week duration) | Y | 2 (3.4) | 4 (13) |
| Xerostomia, ‘brown tongue’ | Y | 0 | 3 (10) |
| Number of complications | 65 | 36 | |
| Number of serious complications | 34 | 22 | |
Data are n (%)
New or markedly worse
An additional cat developed presumed meningoencephalitis 2 months postoperatively (see text)
Based on a retrospective case review, was likely to have been present before surgery
Other than new anorexia
Life-threatening perioperative complications occurred in six cats at the first VBO and one at the second VBO (7/88 surgeries; 8%). One was euthanized after cardiac arrest. A second cat that arrested developed Horner’s syndrome and OI but improved and survived to adoption. One cat required an emergency tracheostomy but survived to adoption. Presumptive meningoencephalitis (ME) occurred in two cats: acutely in one cat 2 weeks after VBO; and 2 months after VBO in the other. Both were euthanized. In the first case, ME was probably present before surgery and may have been acutely exacerbated.
Six cats developed prolonged anorexia postoperatively. These cats sometimes showed interest in food, with initial prehension but subsequent dropping of the food. Three of the six cats developed brown discoloration of the tongue (Figure 2). Diagnostics were performed in one of these three, and showed neutrophilic inflammation with multiple organisms, including pigmented fungi, and a Candida-positive culture. The tongue discoloration was suspected to be secondary to xerostomia (dry mouth) and yeast overgrowth. The three affected cats were treated with oral itraconazole, topical pilocarpine and oral rinses of chlorhexidine or povidone-iodine, as well as esophagostomy tube feeding in two cats. The tongue discoloration resolved in all three cats, but subsequently recurred in one. This cat was euthanized after a complicated and prolonged clinical course.
Figure 2.

Xerostomia and brown discoloration of the tongue, gingiva and mucosa overlying the hard palate after ventral bulla osteotomy in a cat. Note the dry appearance of the oral cavity
Severe, generalized pruritus occurred in nine cats postoperatively. At the postoperative recheck, this had resolved in four cats (at intake, alopecia/pruritus was absent in three and localized in one of these four), improved in two cats (localized alopecia/pruritus was present at intake and recheck in both) and persisted in three cats (at intake, alopecia/pruritus was absent in two and localized in one of these three).
In total, 53 (91%) cats were adopted, and five (8.6%) cats were euthanized for serious surgical complications (n = 3), delayed-onset ME (n = 1) and failure to improve postoperatively, polyp regrowth and FIV-positive status (n = 1).
Outcome analysis
A statistically significant proportion of cats showed resolution of pruritus/alopecia (P = 0.001), moderate/severe NP signs (P = 0.002), moderate/severe OE (P <0.001) and purulent aural discharge (P = 0.002) (Table 3). At recheck, postoperative Horner’s syndrome had persisted in 26/41 (63%) affected cats (P <0.001) and resolved in 11/41 (27%) cats. Data were not available for 4/41 (10%) cats. There was no significant change for inappetence or presence of OI.
Table 3.
Resolution of clinical abnormalities at the veterinary recheck approximately 4 weeks after the final VBO, in 58 cats with otitis media-interna, transferred from an institutional hoarding environment
| Before VBO | Recheck after VBO | P value | n | ||
|---|---|---|---|---|---|
| Absent | Present | ||||
| Inappetence | Absent | 46 (81) | 4 (7.0) | 0.50 | 57 |
| Present | 6 (11) | 3 (5.3) | |||
| Pruritus/alopecia | Absent | 24 (43) | 3 (5.4) | 0.001 | 56 |
| Present | 19 (34) | 10 (18) | |||
| Moderate/severe nasopharyngeal signs | Absent | 29 (53) | 2 (3.6) | 0.002 | 55 |
| Present | 16 (29) | 8 (15) | |||
| Moderate/severe otitis externa | Absent | 9 (16) | 2 (3.6) | <0.001 | 55 |
| Present | 32 (58) | 12 (22) | |||
| Purulent aural discharge |
Absent | 33 (60) | 2 (3.6) | 0.002 | 55 |
| Present | 16 (29) | 4 (7.3) | |||
| Horner’s syndrome | Absent | 26 (49) | 26 (49) | <0.001 | 53 |
| Present | 1 (1.9) | 0 | |||
| Otitis interna | Absent | 27 (50) | 4 (7.4) | 1.00 | 54 |
| Present | 5 (9.3) | 18 (33) | |||
| Head tilt/excursions | Absent | 30 (54) | 4 (7.1) | 1.00 | 56 |
| Present | 3 (5.4) | 19 (34) | |||
| Ataxia | Absent | 52 (93) | 3 (5.4) | Discordant cells too small | 56 |
| Present | 1 (1.8) | 0 | |||
Data are n (%). Data in cells shaded green (Present-Absent) and yellow (Absent-Present) were used in the McNemar test. Statistically significant P values are shown in bold type.
Green = resolved after VBO; orange (Present-Present) = did not resolve; VBO = ventral bulla osteotomy; yellow = developed after VBO
OI before VBO was associated with a significantly greater risk for moderate/severe OE at recheck (OR 4.35; 95% CI 1.21–15.70; P = 0.02) (Table 4). Surgery perfomed by a generalist was also associated with higher risk for moderate/severe OE (OR 3.64; 95% CI 1.03–12.87; P = 0.045). No other associations with negative outcomes were identified (Tables 4 and 5).
Table 4.
OR* risk analysis for key negative outcomes, approximately 4 weeks after final VBO, in 58 cats with otitis media-interna, transferred from an institutional hoarding environment
| Moderate/severe nasopharyngeal signs at recheck | Moderate/severe otitis externa at recheck | Clinical signs of otitis interna at recheck |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | OR | 95% CI | P value | n | OR | 95% CI | P value | n | OR | 95% CI | P value | |
| Preoperative variables | ||||||||||||
| FIV-positive | 55 | 2.75 | 0.67–11.2 | 0.16 | 55 | 2.05 | 0.58–7.24 | 0.27 | 54 | 0.49 | 0.14–1.67 | 0.25 |
| Moderate/severe nasopharyngeal signs | – | – | – | – | 55 | 1.41 | 0.42–4.77 | 0.58 | 53 | 0.54 | 0.18–1.64 | 0.27 |
| Moderate/severe otitis externa | 55 | 0.50 | 0.11–2.39 | 0.39 | – | – | – | – | 54 | 0.78 | 0.11–2.98 | 0.72 |
| Purulent aural discharge | 55 | 0.71 | 0.16–3.10 | 0.64 | 55 | 2.15 | 0.63–7.42 | 0.22 | 54 | 0.29 | 0.08–1.04 | 0.06 |
| Ruptured tympanic membrane | 33 | 0.18 | 0.02–1.71 | 0.14 | 33 | 1.60 | 0.33–7.65 | 0.56 | 32 | 2.10 | 0.49–9.00 | 0.32 |
| Polyp | 55 | 0.86 | 0.19–3.79 | 0.84 | 55 | 0.47 | 0.11–1.97 | 0.30 | 54 | 2.50 | 0.78–7.97 | 0.12 |
| Moderate/severe bulla wall thickening | 51 | 0.77 | 0.19–3.15 | 0.72 | 51 | 1.31 | 0.38–4.50 | 0.67 | 50 | 0.38 | 0.11–1.24 | 0.12 |
| Otitis interna | 55 | 0.64 | 0.15–2.82 | 0.56 | 55 | 4.35 | 1.21–15.70 | 0.02 | – | – | – | – |
| SEZ cultured | 47 | 1.80 | 0.39–8.27 | 0.45 | 47 | 2.67 | 0.61–11.70 | 0.19 | 46 | 1.08 | 0.33–3.56 | 0.90 |
| Surgical variables | ||||||||||||
| Two VBO surgeries | 55 | 10.29 | 1.20–88.07 | 0.07 | 55 | 0.86 | 0.26–2.91 | 0.81 | 54 | 1.06 | 0.36–3.15 | 0.92 |
| Generalist surgeon | 55 | 3.69 | 0.89–15.27 | 0.07 | 55 | 3.64 | 1.03–12.87 | 0.045 | 54 | 1.77 | 0.56–5.57 | 0.44 |
Odds ratios reflect risk of the outcomes listed compared with absence of these outcomes. Values in bold are statistically significant.
CI = confidence interval; OR = odds ratio; FIV = feline immunodeficiency virus; SEZ = Streptococcus equi suspecies zooepidemicus; VBO = ventral bulla osteotomy
Table 5.
OR* risk analysis for serious complications and euthanasia after VBO in cats with otitis media-interna, transferred from an institutional hoarding environment
| Serious complications | Euthanasia | |||||||
|---|---|---|---|---|---|---|---|---|
| n | OR | 95% CI | P value | n | OR | 95% CI | P value | |
| Preoperative variables | ||||||||
| FIV-positive | 58 | 0.75 | 0.23–6.80 | 0.63 | 58 | 1.54 | 0.23–10.13 | 0.65 |
| Nasopharyngeal disease | 57 | 2.77 | 0.92-8.32 | 0.07 | 57 | 0.84 | 0.13–5.46 | 0.86 |
| Otitis externa | 58 | 2.11 | 0.50–8.84 | 0.31 | 58 | 1.05 | 0.11–10.34 | 0.97 |
| Purulent aural discharge | 58 | 1.38 | 0.46–4.15 | 0.56 | 58 | 2.92 | 0.45–19.06 | 0.26 |
| Ruptured tympanic membrane | 35 | 1.09 | 0.27–4.50 | 0.90 | 35 | 0.53 | 0.05–5.68 | 0.60 |
| Polyp | 58 | 0.83 | 0.27–2.55 | 0.74 | 58 | 3.18 | 0.48–20.81 | 0.23 |
| Moderate/severe bulla wall thickening | 54 | 0.67 | 0.22–2.04 | 0.48 | 54 | 0.75 | 0.12–4.91 | 0.77 |
| Otitis interna | 58 | 0.42 | 0.13–1.32 | 0.14 | 58 | 0.35 | 0.04–3.37 | 0.37 |
| SEZ cultured | 48 | 3.40 | 0.97–11.98 | 0.06 | – | – | – | – |
| Surgical variables | ||||||||
| Two VBO surgeries | 58 | 2.19 | 0.74–6.50 | 0.16 | 58 | 0.60 | 0.09–3.86 | 0.59 |
| Generalist surgeon | 58 | 0.83 | 0.27–2.55 | 0.74 | 58 | 1.30 | 0.20–8.47 | 0.79 |
Odds ratios reflect risk of serious complications or euthanasia, compared with their absence
CI = confidence interval; OR = odds ratio; FIV = feline immunodeficiency virus; SEZ = Streptococcus equi suspecies zooepidemicus; VBO = ventral bulla osteotomy
Discussion
These results indicate that the risks of VBO in chronic OMI cannot confidently be balanced by an assurance that clinical problems will resolve after surgery. A significant proportion of cats showed resolution of NP signs, OE, purulent aural discharge and pruritus/alopecia, demonstrating clinical benefit. However, clinical signs did not resolve in a sizeable minority of cats. This might have been owing to chronic turbinate damage in some cats, as well as irreversible changes in the external, middle and inner ear.
Our analysis did not identify viable predictors of complications or negative outcomes. The association of OI with persistent OE, but not other outcomes, is of limited value. Although generalists had worse outcomes for persistent OE compared with specialists, outcomes for other variables were similar. This suggests that this surgery can be successfully performed by a skilled generalist.
Feline OM may be underdiagnosed. 17 The most obvious signs are head tilt and polyps, which were absent in more than half of the cats in our study. It was striking that most cats showed no inappetence at presentation, despite clinical rhinitis. This contrasts with the typical presentation of acute URI, in which lethargy and inappetence are common. 24 OMI should be considered a differential in cats with rhinitis and normal appetite, particularly if there is little response to an appropriate first-line antibiotic.
OE is generally uncommon in cats compared with dogs,25 –27 but was common in cats with OMI in our study and others. 13 OE is likely to be secondary to OMI in cats, while the opposite is the case in dogs. 1 While few cats were tested for ear mites because of routine use of selamectin, only 3/7 were positive. Dark, crumbly exudate ‘typical’ for ear mites can be a presenting sign of OM. 1 Routine in-house microscopy should be performed on all cats presenting with OE. Negative results should increase suspicion of OMI.
Cytology and culture of myringotomy samples are useful diagnostic tools in middle-ear disease, but the primary diagnosis of otitis media is based on otoscopic examination and imaging.2,28 Confirmation in our study relied heavily on radiographs. This may have biased case selection toward more severe cases. Radiography has lower sensitivity for diagnosis of OM compared with CT or MRI,29–33 but radiographic diagnosis is feasible in chronic cases, in which changes can be striking (Figure 1). Bulla wall thickening is the most readily identifiable change. In our study, a scoring system using wall thickness, asymmetry and tympanic cavity opacity (data not shown) did not offer advantages over scoring bulla wall thickening alone. Correct positioning and interpretation of bulla radiographs are essential and require appropriate training.
Prolonged anorexia occurred after six surgeries and was associated with xerostomia and brown discoloration of the tongue in three cats that had bilateral VBOs. The most likely mechanism is hyposalivation and altered taste sensation through iatrogenic damage to the chorda tympani nerve. 34 Bilateral nerve damage would explain the occurrence of xerostomia only after the second surgery, as unilateral nerve function would presumably have been adequate after a single surgery. People report loss of taste, loss of taste acuity, or an unusual or bitter taste after chorda tympani damage, 34 and this might have contributed to anorexia after the first VBO in two cats. Dysbiosis secondary to xerostomia and antibiotics was suspected to have caused yeast overgrowth and brown discoloration of the tongue in three cats.
Although stress, allergic skin disease or parasites might have caused pruritus/alopecia, generalized pruritus was observed in this group of cats to a greater extent than is typically seen in this shelter and occurred in the face of broad-spectrum parasiticide products. Local discomfort probably caused pruritus in some cats, while generalized pruritus may have been owing to undiagnosed allergic skin disease in others. In OMI cases with persistent and generalized pruritus, feline hyperesthesia syndrome could be considered if an allergy work-up is negative. This has been reported in a cat with OMI and ME. 35
The decision to proceed with surgical management was typically based on a lack of response to medical management, as well as the assumption that moderate/severe bulla wall thickening would not respond adequately to medical treatment. This assumption remains untested. Additional reasons for pursuing surgery were previous experience with chronic OMI and concern for progression to ME. ME was rare in our study, and occurred as a postoperative complication, suggesting that surgery is not always protective. In the shelter setting, barriers to adoption, adopter expectations and future financial burden are also key considerations. However, given that VBOs did not always result in substantial clinical improvement, the prevalence of serious surgical complications is concerning.
Life-threatening perioperative complications, as also reported elsewhere,19,21,22 indicate that particular attention must be paid to anesthetic and postoperative airway management. Preoperative dexamethasone may reduce airway swelling, 22 and is advisable in the absence of contraindications. Staging of bilateral VBOs appears to be safer for severe and chronic OMI, but substantially adds to the cost and duration of treatment.
OI did not resolve in most cats. Improvement was noted at some postoperative rechecks, but the data were not uniform enough to allow analysis. In previous reports, neurological improvement was reported in three-quarters of cats treated medically and all cats treated surgically, 18 but OI did not fully resolve in any cat. 16 Postoperative OI occurred in eight cats. This complication has been reported previously,16,17,19 and results from damage to sensitive structures and, possibly, extension of infection after surgical manipulation. More conservative osteotomy could be considered, but in the authors’ experience (CP, PR), this may be insufficient and require revision, as occurred in three early cases in this series.
Concurrent FIV-positive status was not a negative prognostic indicator. This is important, because both FIV and OMI prevalences are high in some groups of hoarded cats. 10 Bilateral disease requiring bilateral VBO was expected to be associated with worse outcomes, but this was not the case. Clinical SEZ infection in cats is associated with animal hoarding and can cause chronic upper and lower respiratory tract infection, OMI and ME.8,35–37 Surprisingly, a positive SEZ culture had no significant association with negative outcomes. This suggests that inflammatory changes, dysbiosis 38 and chronicity may play a greater role than the specific organism identified.
Middle-ear infection is, in effect, an abscess in an inaccessible site, and this limits the value of systemic medications. Therapeutic myringotomy, flushing and topical therapy have been recommended.1,2,26 Despite cautions to the contrary, 3 myringotomy may be feasible without specialized equipment, but requires skill and can result in complications. There is no primary peer-reviewed literature to support the effectiveness of therapeutic myringotomy and flushing in chronic feline OMI. Inflammatory tissue, chronic infection and the bony septum that greatly restricts access to the medioventral compartment of the feline tympanic cavity are likely to reduce the effectiveness of flushing and topical medication in chronic cases. Even if effective, multiple treatments might be required. Myringotomy was not attempted in our setting, primarily because of lack of confidence that these cases could be successfully treated in this way. In a recent study, medical management with a single myringotomy and flush, glucocorticoids and antibiotics was successful in 17/24 cats with OM. 39 However, severity, chronicity and criteria for success were not addressed in this preliminary report.
Could chronic medical management be reasonable in chronic OMI? Cats in our study typically had no obvious evidence of discomfort. Cats with OI were generally mobile and active, with disabling ataxia or head tilt being uncommon. It might be feasible to manage such cases conservatively, with treatment goals of avoiding progression and managing problematic NP signs and OE. One motivation for surgical management of OMI is the risk of extension of infection to the brainstem. Although ME was common in an older case series, 40 it is no longer a frequently reported complication,35,41 and may be amenable to medical treatment.35,41,42 Chronic rhinosinusitis (RSS) can be managed medically, 43 and this could form a blueprint for chronic OMI. Surgical management could be reserved for cases with quality-of-life concerns that might reasonably be expected to be alleviated by surgery.
This study was limited by its retrospective nature and the extraordinary difficulties of managing complex individual cases within a large group setting. The extent of improvement of ataxia and head tilt was not codified, and these would have been useful data. The assessment of the clinical success of VBO was limited by perpetuating factors for OE in a few cats and presumed, or CT-confirmed, RSS in a greater number. This reflects the reality that chronic RSS is part of the feline chronic upper respiratory disease complex.
Studies directly comparing different treatment approaches to chronic feline OMI would be of immense value. Groups of hoarded cats with OMI would present an ideal opportunity to compare medical and surgical approaches to OMI, with potentially lifesaving, resource-sparing results. However, such studies would be complex and expensive.
Conclusions
The surgical management of chronic OMI was successful in many cases, but it was not benign, and not always beneficial. The improvement of signs of OI is a reasonable treatment goal, while full resolution is less likely. Serious complications, including some that were life-threatening and others that compromised welfare and were highly resource-intensive, were quite frequent. No viable predictors of surgical and overall outcomes could be identified. Conservative medical management of OMI could be considered, with surgery reserved for cases in which there are quality of life concerns that might reasonably be expected to be ameliorated by VBO.
Supplemental Material
Supplemental material, sj-docx-1-jfm-10.1177_1098612X231197089 for A Pandora’s box in feline medicine: presenting signs and surgical outcomes in 58 previously hoarded cats with chronic otitis media-interna by Linda S Jacobson, Kyrsten J Janke, Sasha K Kennedy, Gina A Lockwood, Shawn D Mackenzie, Carl D Porter and Patrick B Ringwood in Journal of Feline Medicine and Surgery
Supplemental material, sj-docx-2-jfm-10.1177_1098612X231197089 for A Pandora’s box in feline medicine: presenting signs and surgical outcomes in 58 previously hoarded cats with chronic otitis media-interna by Linda S Jacobson, Kyrsten J Janke, Sasha K Kennedy, Gina A Lockwood, Shawn D Mackenzie, Carl D Porter and Patrick B Ringwood in Journal of Feline Medicine and Surgery
Acknowledgments
We thank PetSmart Charities Canada, Toronto Veterinary Emergency Hospital, Veterinary Emergency Clinic, IDEXX Laboratories, Dr Zeny Feng and Dr Tim Nuttall for their assistance. Thanks are also extended to the staff, management and Board of Toronto Humane Society for their dedication and support.
Footnotes
Correction (September 2023): The paper was updated to correct a sentence in the Conclusions: “Conservative medical management of OMI could be considered, with surgery reserved for cases in which there are quality of life concerns that might reasonably be expected to be ameliorated by VBO.”
Accepted: 2 August 2023
Supplementary material The following files are available as supplementary material: File 1: Examination template for cats following ventral bulla osteotomy,
File 2: Classification of clinical features of otitis media-interna, and dichotomous groupings used for statistical analysis.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: The work described in this manuscript involved the use of non-experimental (owned or unowned) animals. Established internationally recognized high standards (‘best practice’) of veterinary clinical care for the individual patient were always followed and/or this work included the use of cadavers. Ethical approval from a committee was therefore not specifically required for publication in JFMS. Although not required, where ethical approval was still obtained, it is stated in the manuscript.
Informed consent: Informed consent (verbal or written) was obtained from the owner or legal custodian of all animal(s) described in this work (experimental or non-experimental animals, including cadavers) for all procedure(s) undertaken (prospective or retrospective studies). No animals or people are identifiable within this publication, and therefore additional informed consent for publication was not required.
ORCID iD: Linda S Jacobson  https://orcid.org/0000-0001-9704-8737
https://orcid.org/0000-0001-9704-8737
Sasha K Kennedy  https://orcid.org/0009-0009-2738-1003
https://orcid.org/0009-0009-2738-1003
References
- 1. Gotthelf LN. Diagnosis and treatment of otitis media in dogs and cats. Vet Clin North Am Small Anim Pract 2004; 34: 469–487. [DOI] [PubMed] [Google Scholar]
- 2. Grace SF. Otitis media and interna. In: Norsworthy GD. (ed). The feline patient (5th ed.) New Jersey, USA: Wiley-Blackwell, 2018, pp 448–450. [Google Scholar]
- 3. Paterson S. Conditions of the middle ear. In: Paterson S, Tobias K. (eds). Atlas of ear diseases of the dog and cat. Chicester: Wiley-Blackwell, 2013, pp 107–123. [Google Scholar]
- 4. LeCouteur R, Vernau K. Feline vestibular disorders. Part I: anatomy and clinical signs. J Feline Med Surg 1999; 1: 71–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rosychuk R, Bloom P. Otitis media: how common and how important? In: DeBoer DJ, Affolter VK, Hill PB. (eds). Proceedings of the Sixth World Congress of Veterinary Dermatology 2008. Hong Kong: Wiley-Blackwell, 2010, pp 345–352. [Google Scholar]
- 6. Tanaka A, Wagner DC, Kass PH, et al. Associations among weight loss, stress and upper respiratory tract infection in shelter cats. J Am Vet Med Assoc 2012; 240: 570–576. [DOI] [PubMed] [Google Scholar]
- 7. Wagner DC, Kass PH, Hurley KF. Cage size, movement in and out of housing during daily care, and other environmental and population health risk factors for feline upper respiratory disease in nine North American animal shelters. PLoS One 2018; 13. DOI: 10.1371/journal.pone.0190140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Polak KC, Levy JK, Crawford PC, et al. Infectious diseases in large-scale cat hoarding investigations. Vet J 2014; 201: 189–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Strong S, Federico J, Banks R, et al. A collaborative model for managing animal hoarding cases. J Appl Anim Welf Sci 2018; 19: 267–278. [DOI] [PubMed] [Google Scholar]
- 10. Jacobson L, Giacinti J, Robertson J. Medical conditions and outcomes in 371 hoarded cats from 14 sources: a retrospective study (2011–2014). J Feline Med Surg 2019; 22: 484–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Detweiler DA, Johnson LR, Kass PH, et al. Computed tomographic evidence of bulla effusion in cats with sinonasal disease : 2001–2004. J Vet Intern Med 2006; 20: 1080–1084. [DOI] [PubMed] [Google Scholar]
- 12. Shanaman M, Seiler G, Holt D. Prevalence of clinical and subclinical middle ear disease in cats undergoing computed tomographic scans of the head. Vet Radiol Ultrasound 2012; 53: 76–79. [DOI] [PubMed] [Google Scholar]
- 13. Swales N, Foster A, Barnard N. Retrospective study of the presentation, diagnosis and management of 16 cats with otitis media not due to nasopharyngeal polyp. J Feline Med Surg 2018; 20: 1082–1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Schlicksup MD, Van Winkle TJ, Holt DE. Prevalence of clinical abnormalities in cats found to have nonneoplastic middle ear disease at necropsy: 59 cases (1991–2007). J Am Vet Med Assoc 2009; 235: 841–843. [DOI] [PubMed] [Google Scholar]
- 15. Tillson DM, Donnelly KE. Feline inflammatory polyps and ventral bulla osteotomy. Compend Contin Educ Vet 2004; 26: 446–454. https://www.vetfolio.com/learn/article/feline-inflammatory-polyps-and-ventral-bulla-osteotomy (accessed 24 March 2021). [Google Scholar]
- 16. Faulkner J, Budsberg S. Results of ventral bulla osteotomy for treatment of middle ear polyps in cats. J Am Anim Hosp Assoc 1990; 26: 496–499. [Google Scholar]
- 17. Trevor PB, Martin RA. Tympanic bulla osteotomy for treatment of middle-ear disease in cats: 19 cases (1984–1991). J Am Vet Med Assoc 1993; 202: 123–128. [PubMed] [Google Scholar]
- 18. Dutil GF, Guevar J, Schweizer D, et al. Otitis media and interna with or without polyps in cats: association between meningeal enhancement on postcontrast MRI, cerebrospinal fluid abnormalities, and clinician treatment choice and outcome. J Feline Med Surg 2022; 24: e481–e489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kapatkin AS, Matthiesen DT, Noone KE, et al. Results of surgery and long-term follow-up in 31 cats with nasopharyngeal polyps. J Am Anim Hosp Assoc 1990; 26: 387–392. [Google Scholar]
- 20. Anderson DM, Robinson RK, White RAS. Management of inflammatory polyps in 37 cats. Vet Rec 2000; 147: 684–687. [PubMed] [Google Scholar]
- 21. Smeak DD. Management of complications associated with total ear canal ablation and bulla osteotomy in dogs and cats. Vet Clin North Am Small Anim Pract 2011; 41: 981–994. [DOI] [PubMed] [Google Scholar]
- 22. De Gennaro C, Vettorato E, Corletto F. Severe upper airway obstruction following bilateral ventral bulla osteotomy in a cat. Can Vet J 2017; 58: 1313–1316. [PMC free article] [PubMed] [Google Scholar]
- 23. Patronek GJ. Hoarding of animals: an under-recognized public health problem in a difficult-to-study population. Public Health Rep 1999; 114: 81–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kennedy M, Little SE. Viral diseases. In: Little SE. (ed). The cat: clinical medicine and management. Philadelphia, PA: Elsevier Saunders, 2012, pp 1029–1070. [Google Scholar]
- 25. Bollez A, De Rooster H, Furcas A, et al. Prevalence of external ear disorders in Belgian stray cats. J Feline Med Surg 2018; 20: 149–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Brame B, Cain C. Chronic otitis in cats: clinical management of primary, predisposing and perpetuating factors. J Feline Med Surg 2021; 23: 433–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Nuttall T. Otitis. In: Noli C, Colombo S. (eds). Feline dermatology. New York City, USA: Springer, 2020, pp 175–209. [Google Scholar]
- 28. Vernau KM, LeCouteur RA. Feline vestibular disorders. Part II: Diagnostic approach and differential diagnosis. J Feline Med Surg 1999; 1: 81–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rohleder JJ, Jones JC, Duncan RB, et al. Comparative performance of radiography and computed tomography in the diagnosis of middle ear disease in 31 dogs. Vet Radiol Ultrasound 2006; 47: 45–52. [DOI] [PubMed] [Google Scholar]
- 30. Allgoewer I, Lucas S, Schmitz S. Magnetic resonance imaging of the normal and diseased feline middle ear. Vet Radiol Ultrasound 2000; 41: 413–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Benigni L, Lamb C. Diagnostic imaging of ear disease. In Pract 2006; 28: 122–130. [Google Scholar]
- 32. Garosi LS, Dennis R, Schwarz T. Review of diagnostic imaging of ear diseases in the dog and cat. Vet Radiol Ultrasound 2003; 44: 137–146. [DOI] [PubMed] [Google Scholar]
- 33. Dickie AM, Doust R, Cromarty L, et al. Comparison of ultrasonography, radiography and a single computed tomography slice for the identification of fluid within the canine tympanic bulla. Res Vet Sci 2003; 75: 209–216. [DOI] [PubMed] [Google Scholar]
- 34. Mandel L. Hyposalivation after undergoing stapedectomy. J Am Dent Assoc 2012; 143: 39–42. [DOI] [PubMed] [Google Scholar]
- 35. Martin-Vaquero P, da Costa RRC, Daniels JJB. Presumptive meningoencephalitis secondary to extension of otitis media/interna caused by Streptococcus equi subspecies zooepidemicus in a cat. J Feline Med Surg 2011; 13: 606–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Blum S, Elad D, Zukin N, et al. Outbreak of Streptococcus equi subsp. zooepidemicus infections in cats. Vet Microbiol 2010; 144: 236–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Britton AP, Davies JL. Rhinitis and meningitis in two shelter cats caused by Streptococcus equi subspecies zooepidemicus. J Comp Pathol 2010; 143: 70–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Bordin A, Sidjabat HE, Cottrell K, et al. Chronic rhinosinusitis: a microbiome in dysbiosis and the search for alternative treatment options. Microbiol Aust 2016; 37: 149. [Google Scholar]
- 39. Deleporte S, Prélaud P. Single myringotomy for the treatment of otitis media in cats: a retrospective study [abstract]. Vet Dermatol 2021; 32: 421. [Google Scholar]
- 40. Lawson DD. Otitis media in the cat. Vet Rec 1957; 643–647. [Google Scholar]
- 41. Moore SA, Bentley RT, Carrera-Justiz S, et al. Clinical features and short-term outcome of presumptive intracranial complications associated with otitis media/interna: a multi-center retrospective study of 19 cats (2009–2017). J Feline Med Surg 2018; 21: 148–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Negrin A, Cherubini GB, Lamb C, et al. Clinical signs, magnetic resonance imaging findings and outcome in 77 cats with vestibular disease: a retrospective study. J Feline Med Surg 2010; 12: 291–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Scherk M. Snots and snuffles. Rational approach to chronic feline upper respiratory syndromes. J Feline Med Surg 2010; 12: 548–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-jfm-10.1177_1098612X231197089 for A Pandora’s box in feline medicine: presenting signs and surgical outcomes in 58 previously hoarded cats with chronic otitis media-interna by Linda S Jacobson, Kyrsten J Janke, Sasha K Kennedy, Gina A Lockwood, Shawn D Mackenzie, Carl D Porter and Patrick B Ringwood in Journal of Feline Medicine and Surgery
Supplemental material, sj-docx-2-jfm-10.1177_1098612X231197089 for A Pandora’s box in feline medicine: presenting signs and surgical outcomes in 58 previously hoarded cats with chronic otitis media-interna by Linda S Jacobson, Kyrsten J Janke, Sasha K Kennedy, Gina A Lockwood, Shawn D Mackenzie, Carl D Porter and Patrick B Ringwood in Journal of Feline Medicine and Surgery