Abstract
Cryptosporidium parvum is an important cause of diarrhea in humans and several animal species. Prostaglandins play a central role in regulating intestinal fluid secretion in animal models of cryptosporidiosis, but their cellular sources and mechanisms of induction are unclear. Here, we show that C. parvum infection directly activates prostaglandin H synthase 2 expression and prostaglandin E2 and F2α production in human intestinal epithelial cells.
Cryptosporidium parvum is an important cause of diarrhea in both immunocompetent and immunosuppressed hosts and is responsible for 1 to 2% of deaths in patients with acquired immunodeficiency syndrome (21). The mechanisms underlying C. parvum-induced diarrhea in humans are poorly understood. The presence of an enterotoxic activity released by the parasite has been previously reported (8), but these findings are controversial (20). In a porcine model of cryptosporidiosis, diarrhea results from a combination of secretory diarrhea and sodium-glucose malabsorption due to villous atrophy and epithelial cell damage (3). The former is controlled by prostaglandin E2 (PGE2) and prostacyclin (PGI2), which appear to act either directly on intestinal epithelial cell functions or indirectly by activating cholinergic and VIPergic neuronal pathways (1). However, neither the cellular source of PGE2 and PGI2 in this model, nor the mechanisms leading to their induction are known. Inflammatory cells in the mucosa, such as macrophages, can produce high levels of prostaglandins and may be important for prostaglandin production after C. parvum infection, since infection is often accompanied by some degree of inflammation (7, 17). However, significant diarrhea associated with C. parvum infection has been reported in the absence of overt histopathological changes in the gut (14, 18), suggesting that cells normally present in the uninfected mucosa, e.g., epithelial cells or fibroblasts, produce increased prostaglandin levels after infection. Our previous studies suggested that intestinal epithelial cells, which are the predominant host cells infected with C. parvum (15), can act as sensors of infection and provide early signals for the initiation of the mucosal inflammatory response by releasing chemoattractant cytokines (12). Furthermore, other studies have shown that infection of epithelial cells with invasive bacteria upregulates prostaglandin production (5). Based on these findings, the present studies tested the hypothesis that intestinal epithelial cells respond to infection with C. parvum with increased prostaglandin production.
C. parvum, which was initially isolated from an infected child, was maintained in calves at the Institut National de la Recherche Agronomique, Nouzilly, France, and C. parvum oocysts were purified by filtration and diethyl ether sedimentation as described previously (12). The human adenocarcinoma cell lines HCT-8 (ATCC CCL 244) and HT-29 (ATCC HTB 38) were maintained in RPMI 1640 medium–10% heat-inactivated fetal bovine serum (FBS)–2 mM l-glutamine–50 U of penicillin G per ml–50 μg of streptomycin per ml. Infections were performed as described previously (12). Briefly, cells were seeded into six-well Costar tissue culture plates at 2 × 106 cells/well and grown for 24 h. Infections with oocysts were done in a supplemented medium as described by Upton et al. (24). After a 5-h infection period, monolayers were washed, and fresh supplemented medium was added. This time is referred to as 0 h for all experiments. To determine the levels of prostaglandin production, cultures were washed and incubated for 15 min in 1 ml of RPMI 1640 medium per well–10 mM HEPES–2 mg of bovine serum albumin per ml–20 μM arachidonic acid. Levels of the prostaglandins PGE2 and PGF2α were determined by enzyme immunoassay (Cayman Chemical, Ann Arbor, Mich.). These prostaglandins were chosen for the present studies based on our previous finding that they were the major prostaglandins produced by human intestinal epithelial cell lines (5). To correct for cell loss due to lysis of parasite-infected cells, prostaglandin levels were divided for each culture by the amount of total protein present in the culture at each time point (i.e., the time of the assay). Total protein contents were determined by lysing the monolayers in lysis buffer (150 mM NaCl, 20 mM Tris [pH 7.5], 0.1% Triton X-100, 1 mM phenylmethylsulfonyl fluoride (PMSF), 10 μg of aprotinin per ml) and by assaying the protein concentrations by the Bradford method (Bio-Rad Laboratories, Hercules, Calif.). The lysates were subsequently used for immunoblot analysis of prostaglandin H synthase 1 (PGHS-1), PGHS-2, and actin expression by using previously published protocols and antibodies (5). Levels of PGHS-2 and β-actin mRNA were determined by quantitative reverse transcription (RT)-PCR with standard RNAs as we described before (5, 10).
The human intestinal xenograft model used in the present studies has been described in detail before (12, 19). Briefly, human fetal intestines were transplanted onto the backs of SCID mice and allowed to develop for 10 to 15 weeks. At this time, a differentiated epithelial layer of entirely human origin has developed (19). Xenografts were infected by injecting 108 C. parvum oocysts in 200 μl of phosphate-buffered saline (PBS) into the lumen. Control xenografts were injected with 200 μl of PBS (sham infection). Tissues were collected 5 days after infection, since this time point was shown in a rabbit intestinal xenograft model to be the earliest after C. parvum infection at which there was consistent and widespread epithelial infection (23). Successful infection was confirmed on paraffin sections stained with hematoxylin and eosin and by transmission electron microscopy as reported previously (12). Total RNA was extracted from mucosal scrapings, and mRNA levels for PGHS-2 and β-actin and levels of 28S rRNA were determined by quantitative RT-PCR (5). The RT-PCR of PGHS-2 and β-actin was specific for the respective human mRNAs, since amplification of mouse spleen RNA or DNA did not yield any PCR products (5). The xenograft studies were performed at the Babraham Institute, Cambridge, United Kingdom, with full approval from the Cambridge Local Ethics Committee and in accordance with the Home Office guidelines specified in the Polkinghorne Report (19).
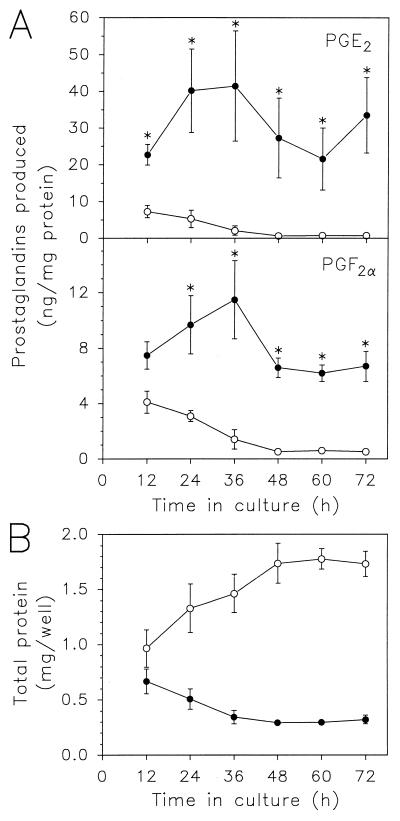
Infection of HCT-8 cells with C. parvum increased PGE2 production by as much as 50-fold (Fig. 1). The increase was first observed at 12 h after infection, was maximal by 36 h, and was sustained until the end of the observation period (72 h). Production of PGF2α also increased after C. parvum infection with a kinetics similar to that of PGE2 production, although the absolute levels produced and the relative increases after infection were ∼5-fold less than those for PGE2 (Fig. 1). Similarly, C. parvum infection of another human intestinal epithelial cell line, HT-29, increased PGE2 and PGF2α production by >6-fold (controls, <30 pg of PGE2/mg of total protein and 9 ± 1 pg of PGF2α/mg of protein; 36 h after C. parvum infection, 204 ± 47 pg of PGE2/mg of protein and 171 ± 82 pg of PGF2α/mg of protein; values are means ± standard errors of the means [SEM] of the results of three independent experiments). In contrast to infection with live C. parvum cells, exposure of HCT-8 cells to heat-inactivated C. parvum (57°C for 1 h) did not affect PGE2 or PGF2α production (data not shown).
FIG. 1.
Time course of increased prostaglandin production after C. parvum infection of HCT-8 cells. HCT-8 monolayers in six-well plates were infected with 107 oocysts/well (•), of which 40 to 60% were found to excyst, as determined in parallel experiments. Uninfected monolayers were used as a control (○). The amounts of PGE2 and PGF2α produced (A) were determined after a 15-min incubation period with 20 μM arachidonic acid at the indicated times after infection. Subsequently, monolayers were lysed and the amounts of total protein/well were determined (B). Data are means ± SEM of three to four independent experiments. Asterisks, values that were significantly increased relative to those in the respective uninfected controls (P ≤ 0.05), as determined by the t test.
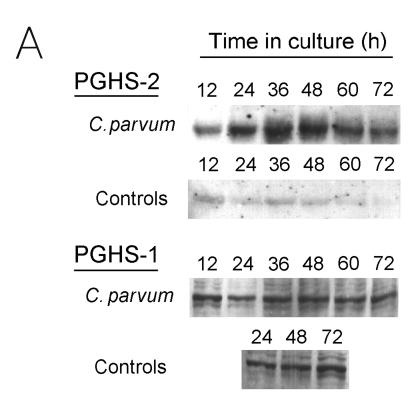
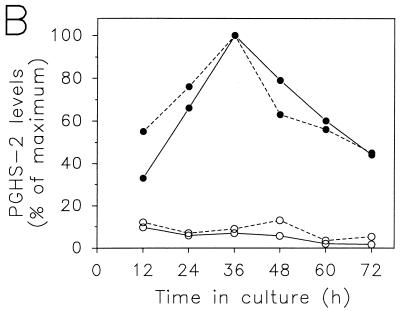
Prostaglandin production is controlled by the levels of the key enzyme PGHS, which exists in two isoforms, PGHS-1 and PGHS-2. Although both isoforms catalyze the same biosynthetic step, they display considerable differences in regulation and tissue-specific expression and have overlapping as well as unique physiologic functions (25). Both isoforms are expressed in intestinal epithelial cells (5). To define their role in the C. parvum-induced increase in PGE2 and PGF2α production, two PGHS inhibitors were used, i.e., indomethacin and NS-398. Indomethacin, which inhibits both PGHS isoforms, and NS-398, which is a highly specific inhibitor of PGHS-2 (6), completely blocked increased production of PGE2 (Table 1) and PGF2α (data not shown) after C. parvum infection of HCT-8 cells. These data indicate that PGHS-2 was mostly responsible for the increase in PGE2 and PGF2α production after C. parvum infection. In agreement with this, PGHS-2 levels increased after C. parvum infection of HCT-8 cells (Fig. 2), with time course and relative extent paralleling those of the increase in PGE2 production (Fig. 1). In contrast, levels of PGHS-1 (Fig. 2) and actin were minimally affected by C. parvum infection of HCT-8 cells (the ratios of the levels in infected relative to control cells were 1.3, 1.3, and 0.8 for PGHS-1 at 24, 48, and 72 h after infection, respectively, and 1.3 and 0.8 for actin at 48 and 72 h after infection, respectively, as determined by scanning densitometry of immunoblots). Furthermore, the increase in PGHS-2 protein levels was paralleled by an increase in PGHS-2 mRNA levels in C. parvum-infected HCT-8 cells (Fig. 3), although the relative increase in PGHS-2 mRNA levels was less than that of PGHS-2 protein levels (Fig. 2).
TABLE 1.
Effect of PGHS inhibitors on C. parvum-induced PGE2 production by HCT-8 intestinal epithelial cellsa
| Expt and inhibitor added | Amt of PGE2 produced (ng/mg of cellular protein)
|
|
|---|---|---|
| Control | With C. parvum | |
| 1 | ||
| None | 1.7 ± 0.1 | 22.4 ± 0.3 |
| Indomethacin | <0.1b | 0.2 ± 0.1b |
| NS-398 | <0.1b | 0.2 ± 0.1b |
| 2 | ||
| None | 1.0 ± 0.2 | 125.0 ± 20.5 |
| Indomethacin | 0.4 ± 0.1b | 0.5 ± 0.1b |
| NS-398 | <0.1b | 0.6 ± 0.1b |
Confluent monolayers of HCT-8 cells in six-well plates were infected with 8 × 106 C. parvum oocysts and incubated for 40 h. The PGHS inhibitors indomethacin (10 μM) and NS-398 (10 μM) were added for 1 h, and the amounts of PGE2 produced were determined after addition of 20 μM arachidonic acid for 15 min. Data are means ± SEM of triplicate cultures.
Significantly different (P < 0.01) from values for parallel cultures not treated with a PGHS inhibitor, as determined by the t test.
FIG. 2.
Immunoblot analysis of PGHS-2 and PGHS-1 expression after C. parvum infection of HCT-8 cells. HCT-8 monolayers in six-well plates were infected with 107 C. parvum oocysts/well or were left uninfected (controls). Cultures were incubated for the indicated periods of time, and cell lysates were prepared, size fractionated, and blotted onto a nitrocellulose membrane. PGHS-2 and PGHS-1 were detected with rabbit anti-human PGHS-2 and PGHS-1 (Oxford Biomedical), respectively, and the ECL system (Amersham). (A) Examples of immunoblots for PGHS-2 and PGHS-1. Scans were obtained with a Bio-Rad GS-670 scanning densitometer and PhotoFinish imaging software. (B) Quantitative densitometric analysis of the PGHS-2 immunoblot shown in panel A (continuous lines), along with data from an additional experiment (dashed lines). PGHS-2 levels were expressed as percentages of the maximum value observed for any of the samples in each experiment (i.e., 36 h after C. parvum infection in both experiments). •, C. parvum infected; ○, uninfected controls.
FIG. 3.
Increased PGHS-2 mRNA expression in C. parvum-infected HCT-8 cells. HCT-8 monolayers in six-well plates were infected with 107 oocysts. Levels of mRNAs for PGHS-2 (•) and β-actin (▾) were determined by quantitative RT-PCR with standard RNAs and were expressed as ratios of the values for infected cells to those for controls. Data are the means ± SEM of the results from three independent experiments. Mean mRNA levels in controls were 2.2 × 105 transcripts/μg of total RNA for PGHS-2 and 2.5 × 107 transcripts/μg of RNA for β-actin. Asterisks indicate that values are significantly increased relative to those in the respective uninfected controls (P ≤ 0.05), as determined by the t test.
To confirm the cell line findings in vivo, we used a human intestinal xenograft model (19). This model has the advantage that normal human intestinal epithelial cells can be infected with C. parvum under controlled conditions in the absence of potentially confounding coinfections, which are commonly encountered when samples from C. parvum-infected patients are used. We showed previously that the intestinal xenograft model can be successfully infected with C. parvum and can be used to characterize cytokine responses to infection (12). As shown in Table 2, levels of human PGHS-2 mRNA increased by 10-fold when they were assayed 5 days after C. parvum infection of intestinal xenografts. As a control, levels of 28S rRNA and β-actin mRNA changed by <2-fold after infection. Intestinal epithelial cells are the most abundant human cell type in the xenografts (19) and are likely the only cells in this model that become infected with C. parvum (12). Moreover, the RT-PCR used in these studies is specific for human PGHS-2 mRNA (5). Together, these findings indicate that intestinal epithelial cells most likely are responsible for the increase in PGHS-2 mRNA levels after C. parvum infection in the intestinal xenograft model.
TABLE 2.
Increased expression of human PGHS-2 mRNA in C. parvum-infected human intestinal xenograftsa
| RNA species | No. of RNA transcripts/ μg of total RNA
|
Ratio of infected/ control | |
|---|---|---|---|
| Control | With C. parvum | ||
| PGHS-2 | 1.3 × 104 | 1.3 × 105 | 10.0 |
| 28S rRNA | 4.4 × 108 | 8.0 × 108 | 1.8 |
Human intestinal xenografts were infected with 108 C. parvum oocysts in PBS by transcutaneous injection. Controls were injected with PBS alone (i.e., sham infected). Tissues were collected 5 days later, and total RNA was extracted from mucosal scrapings of each individual xenograft. Equal amounts of RNA were pooled from five to eight different xenografts in each group, and levels for PGHS-2 mRNA and 28S rRNA were determined by quantitative RT-PCR. mRNA levels for β-actin that changed by <2-fold after infection (12) are not shown.
Intestinal epithelial cells respond to C. parvum infection, as shown here, with increased PGHS-2 expression and PGE2 and PGF2α production. This epithelial response can provide a partial explanation for the observation that PGHS products, and PGE2 in particular, are important for regulating increased fluid secretion in response to C. parvum infection, as shown in piglets (2). Nonetheless, it is difficult at present to assess the relative contributions of epithelial cells and other cells, such as macrophages and subepithelial fibroblasts, to C. parvum-induced mucosal PGE2 production at different stages of the infection. In the normal unstimulated state, epithelial PGE2 production represents only a relatively small fraction of total mucosal PGE2 production in the rabbit colon (4, 13). However, based on the present findings, the epithelial contribution appears to increase substantially after infection. Regardless of the absolute amount of PGE2 produced by intestinal epithelial cells after C. parvum infection, epithelial cell-derived PGE2 is likely to be more efficient than PGE2 produced by cells in the underlying mucosa in affecting epithelial functions in a paracrine or autocrine manner, due to reduced diffusion distances. In contrast to PGE2, epithelial production of PGF2α is relatively high compared with total mucosal PGF2α production in the normal rabbit colon, even in the unstimulated state (4, 13). However, PGF2α may be less important than PGE2 in controlling epithelial ion transport, since it was shown to be much less effective in inducing chloride secretion by polarized human intestinal epithelial cell monolayers (5).
Increased epithelial PGHS-2 expression and PGE2 production after C. parvum infection may have functions other than regulating epithelial chloride and, concomitantly, fluid secretion. For example, PGE2 upregulates epithelial mucin expression (16). Increased mucus production is observed after C. parvum infection of suckling mice (9), which may be a protective host response against further infection by the extracellular stages of the parasite (22). PGE2 has also been shown to downregulate inflammatory cytokine production by activated macrophages (11), which could explain why, in some cases, diarrhea can develop after C. parvum infection in the apparent absence of mucosal inflammation.
Acknowledgments
We thank Roselyne Mancassola for expert technical help.
This work was supported by National Institutes of Health grant DK35108, a fellowship from the DRI of the Institut National de la Recherche Agronomique, France (F.L.), and a Career Development award from the Crohn’s and Colitis Foundation of America (L.E.).
REFERENCES
- 1.Argenzio R A, Armstrong M, Rhoads J M. Role of the enteric nervous system in piglet cryptosporidiosis. J Pharmacol Exp Ther. 1996;279:1109–1115. [PubMed] [Google Scholar]
- 2.Argenzio R A, Lecce J, Powell D W. Prostanoids inhibit intestinal NaCl absorption in experimental porcine cryptosporidiosis. Gastroenterology. 1993;104:440–447. doi: 10.1016/0016-5085(93)90412-6. [DOI] [PubMed] [Google Scholar]
- 3.Argenzio R A, Liacos J A, Levy M L, Meuten D J, Lecce J G, Powell D W. Villous atrophy, crypt hyperplasia, cellular infiltration, and impaired glucose-Na absorption in enteric cryptosporidiosis of pigs. Gastroenterology. 1990;98:1129–1140. doi: 10.1016/0016-5085(90)90325-u. [DOI] [PubMed] [Google Scholar]
- 4.Craven P A, DeRubertis F R. Profiles of eicosanoid production by superficial and proliferative colonic epithelial cells and sub-epithelial colonic tissue. Prostaglandins. 1986;32:387–399. doi: 10.1016/0090-6980(86)90007-9. [DOI] [PubMed] [Google Scholar]
- 5.Eckmann L, Stenson W F, Savidge T C, Lowe D C, Barrett K E, Fierer J, Smith J R, Kagnoff M F. Role of intestinal epithelial cells in the host secretory response to infection by invasive bacteria. Bacterial entry induces epithelial prostaglandin H synthase-2 expression and prostaglandin E2 and F2α production. J Clin Invest. 1997;100:296–309. doi: 10.1172/JCI119535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Futaki N, Takahashi S, Yokoyama M, Arai I, Higuchi S, Otomo S. NS-398, a new anti-inflammatory agent, selectively inhibits prostaglandin G/H synthase/cyclooxygenase (COX-2) activity in vitro. Prostaglandins. 1994;47:55–59. doi: 10.1016/0090-6980(94)90074-4. [DOI] [PubMed] [Google Scholar]
- 7.Genta R M, Chappell C L, White A C, Kimball K T, Goodgame R W. Duodenal morphology and intensity of infection in AIDS-related intestinal cryptosporidiosis. Gastroenterology. 1993;105:1769–1775. doi: 10.1016/0016-5085(93)91075-s. [DOI] [PubMed] [Google Scholar]
- 8.Guarino A, Canani R B, Casola A, Pozio E, Russo R, Bruzzese E, Fontana M, Rubino A. Human intestinal cryptosporidiosis: secretory diarrhea and enterotoxic activity in Caco-2 cells. J Infect Dis. 1995;171:976–983. doi: 10.1093/infdis/171.4.976. [DOI] [PubMed] [Google Scholar]
- 9.Hill B D, Blewett D A, Dawson A M, Wright S. Cryptosporidium parvum: investigation of sporozoite excystation in vivo and the association of merozoites with intestinal mucus. Res Vet Sci. 1991;51:264–267. doi: 10.1016/0034-5288(91)90075-y. [DOI] [PubMed] [Google Scholar]
- 10.Jung H C, Eckmann L, Yang S K, Panja A, Fierer J, Morzycka-Wroblewska E, Kagnoff M F. A distinct array of proinflammatory cytokines is expressed in human colon epithelial cells in response to bacterial invasion. J Clin Invest. 1995;95:55–65. doi: 10.1172/JCI117676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Knudsen P J, Dinarello C A, Strom T B. Prostaglandins posttranscriptionally inhibit monocyte expression of interleukin 1 activity by increasing intracellular cyclic adenosine monophosphate. J Immunol. 1986;137:3189–3194. [PubMed] [Google Scholar]
- 12.Laurent F, Eckmann L, Savidge T C, Morgan G, Theodos C, Naciri M, Kagnoff M F. Cryptosporidium parvum infection of human intestinal epithelial cells induces the polarized secretion of C-X-C chemokines. Infect Immun. 1997;65:5067–5073. doi: 10.1128/iai.65.12.5067-5073.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lawson L D, Powell D W. Bradykinin-stimulated eicosanoid synthesis and secretion by rabbit ileal components. Am J Physiol. 1987;252:G783–G790. doi: 10.1152/ajpgi.1987.252.6.G783. [DOI] [PubMed] [Google Scholar]
- 14.Lefkowitch J H, Krumholz S, Feng-Chen K C, Griffin P, Despommier D, Brasitus T A. Cryptosporidiosis of the human small intestine: a light and electron microscopic study. Hum Pathol. 1984;15:746–752. doi: 10.1016/s0046-8177(84)80165-3. [DOI] [PubMed] [Google Scholar]
- 15.Marcial M A, Madara J L. Cryptosporidium: cellular localization, structural analysis of absorptive cell-parasite membrane-membrane interactions in guinea pigs, and suggestion of protozoan transport by M cells. Gastroenterology. 1986;90:583–594. doi: 10.1016/0016-5085(86)91112-1. [DOI] [PubMed] [Google Scholar]
- 16.McCool D J, Marcon M A, Forstner J F, Forstner G G. The T84 human colonic adenocarcinoma cell line produces mucin in culture and releases it in response to various secretagogues. Biochem J. 1990;267:491–500. doi: 10.1042/bj2670491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Meisel J L, Perera D R, Meligro C, Rubin C E. Overwhelming watery diarrhea associated with a Cryptosporidium in an immunosuppressed patient. Gastroenterology. 1976;70:1156–1160. [PubMed] [Google Scholar]
- 18.Modigliani R, Bories C, Le Charpentier Y, Salmeron M, Messing B, Galian A, Rambaud J C, Lavergne A, Cochand-Priollet B, Desportes I. Diarrhoea and malabsorption in acquired immune deficiency syndrome: a study of four cases with special emphasis on opportunistic protozoan infestations. Gut. 1985;26:179–187. doi: 10.1136/gut.26.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Savidge T C, Morey A L, Ferguson D J, Fleming K A, Shmakov A N, Phillips A D. Human intestinal development in a severe-combined immunodeficient xenograft model. Differentiation. 1995;58:361–371. doi: 10.1046/j.1432-0436.1995.5850361.x. [DOI] [PubMed] [Google Scholar]
- 20.Sears C L, Guerrant R L. Cryptosporidiosis: the complexity of intestinal pathophysiology. Gastroenterology. 1994;106:252–254. doi: 10.1016/s0016-5085(94)95891-2. [DOI] [PubMed] [Google Scholar]
- 21.Selik R M, Chu S Y, Ward J W. Trends in infectious diseases and cancers among persons dying of HIV infection in the United States from 1987 to 1992. Ann Intern Med. 1995;123:933–936. doi: 10.7326/0003-4819-123-12-199512150-00006. [DOI] [PubMed] [Google Scholar]
- 22.Thea D M, Pereira M E, Kotler D, Sterling C R, Keusch G T. Identification and partial purification of a lectin on the surface of the sporozoite of Cryptosporidium parvum. J Parasitol. 1992;78:886–893. [PubMed] [Google Scholar]
- 23.Thulin J D, Kuhlenschmidt M S, Rolsma M D, Current W L, Gelberg H B. An intestinal xenograft model for Cryptosporidium parvum infection. Infect Immun. 1994;62:329–331. doi: 10.1128/iai.62.1.329-331.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Upton S J, Tilley M, Brillhart D B. Effects of select medium supplements on in vitro development of Cryptosporidium parvum in HCT-8 cells. J Clin Microbiol. 1995;33:371–375. doi: 10.1128/jcm.33.2.371-375.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Williams C S, DuBois R N. Prostaglandin endoperoxide synthase: why two isoforms? Am J Physiol. 1996;270:G393–G400. doi: 10.1152/ajpgi.1996.270.3.G393. [DOI] [PubMed] [Google Scholar]