Abstract
Simple Summary
The dynamic change in gene expression during follicular development is essential for oocyte maturation and ovulation. The genes encoding for estrogen receptor (ESR2) and follicle-stimulating hormone receptor (FSHR) play crucial roles in ovarian follicular development. Gene expression is subjected to different regulatory mechanisms, including microRNAs, which have been demonstrated to regulate specific target genes. No information is currently available on the expression of miRNAs in canine ovarian follicles; therefore, the objective of this study was to evaluate the expression of miRNAs cfa-miR-34a and cfa-let-7c predicted against FSHR and ESR2, respectively, related to their target gene expression in follicular cells throughout the estrous cycle in this species. The genes and miRNAs were evaluated using quantitative PCR analyses. Each miRNA and its target genes were expressed in all estrous phases. A tendency for an inverse relationship was observed between the expression of miR-34a and FSHR only in anestrus, while an inverse correlation was found between miR-let-7c and ESR2 during the entire cycle. The differential expression profile of miR-34a and miR-let-7c and their predicted target genes in canine ovarian follicles obtained in the present study suggests a role of these miRNAs in the negative regulation of FSHR and ESR2 genes throughout the ovarian cycle.
Abstract
The genes encoding for estrogen receptor (ESR2) and follicle-stimulating hormone receptor (FSHR) play crucial roles in ovarian follicular development. This study aimed to determine the expression levels of miRNAs predicted against FSHR and ESR2 mRNAs in follicular cells related to their target genes during the estrous cycle in canines. Antral follicles were dissected from 72 ovaries following ovariohysterectomies. MiRNAs regulating FSHR and ESR2 genes were selected from miRNA databases, and mature miRNA and mRNA expression profiling was performed using real-time polymerase chain reaction (PCR). The best miRNA for each target gene was selected considering the quantitative PCR (qPCR) performance and target prediction probability, selecting only miRNAs with a binding p-value of 1.0, and choosing cfa-miR-34a and cfa-let-7c for FSHR and ESR2, respectively. The expression levels comparing the different phases of the estrous cycle were evaluated using ANOVA. Pearson correlations between the expression pattern of each miRNA and their target genes were performed. Each miRNA and its target genes were expressed in the granulosa cells in all estrous phases. FSHR remained low in anestrus and proestrus, increased (p < 0.05) to the highest level in estrus, and decreased (p < 0.05) in diestrus. ESR2 showed the same trend as FSHR, with the highest (p < 0.05) expression in estrus and the lowest (p < 0.05) in anestrus and proestrus. A tendency for an inverse relationship was observed between the expression of miR-34a and FSHR only in the anestrus phase, while an inverse correlation (r = −0.8) was found between miRNA-7c and ESR2 (p < 0.01). The expression profile of miR-34a and miR-let-7c and their predicted target genes of dog ovarian follicles throughout the estrous cycle observed in this study suggest a role in the transcriptional regulation of FSHR and ESR2, which is the first evidence of the involvement of these miRNAs in the canine follicular function.
Keywords: dog, gene expression, ovarian cycle
1. Introduction
Ovarian follicular development is controlled by complex interactions between hormones produced in the hypothalamus, pituitary gland, and ovaries. Follicle-stimulating hormone (FSH) is secreted by gonadotrophs of the anterior pituitary gland in response to gonadotropin-releasing hormone (GnRH) [1] and acts upon its receptor follicle-stimulating hormone receptor (FSHR), which is a member of the rhodopsin receptor family of G protein-coupled receptors [2], stimulating follicular cells to produce steroids [3]. FSHR activation is necessary for the hormonal functioning of FSH and thus, it is crucial for follicular development. This receptor is encoded by the FSHR gene, and its expression has been reported in follicles of different species [4,5], including canines [6,7,8]. Although fluctuations in FSH circulating levels display temporal patterns, the changes in FSHR expression throughout the estrous cycle has not been previously described in canines.
On the other hand, estrogens (E2), which are produced by follicle cells, act directly by binding with estrogen receptors alpha (ERα) and beta (ERβ), which are ligand-activated transcription factors, and indirectly by activating plasma membrane-associated E R intracellular signaling [9,10]. Estrogen receptors alpha and beta subtypes are encoded by ESR1 and ESR2 genes, respectively. Predominantly expressed by granulosa cells [11], ERβ is associated with follicle growth and ovarian responsiveness in canines [12]. This receptor is essential for gonadotropin-induced steroidogenesis and gametogenesis [13,14]. In addition, ERβ regulates gonadotropin secretion acting in GnRH neurons [15].
Endocrine regulation of ovarian function involving FSH and E2 defines the follicular phase before ovulation [16]. The actions of both hormones depend on their receptor expression to perform their functions. At the same time, receptor mRNA expression strongly depends on the post-transcriptional modifications to which they are subjected [2]. Increasing evidence corroborates that miRNAs regulate ovarian function through their actions in ovarian cells, such as granulosa and cumulus cells [17,18], and oocytes [19]. MicroRNAs are the most abundant class of small RNAs in the ovary [20]. They are short, non-coding RNA molecules of approximately 17–22 nucleotides that have emerged as critical post-transcriptional regulatory RNA molecules [21]. MicroRNAs regulate the gene expression of target genes by binding to the 3′-untranslated regions (3′-UTR) of mRNAs, inhibiting their translation and/or causing their degradation [22,23], or, in minor proportion, by enhancing translation at the post-translation stage [24]. The effects of FSH on ovarian cell proliferation and estrogen levels could be mediated by several ovarian miRNAs [25,26]. Some studies have reported differences in miRNA expression during different ovarian stages; thus, dynamic changes in the profiles of different miRNAs have been described during follicle development in mice [27] as in other species [28,29]. Therefore, several follicular functions could be developmentally regulated by miRNAs throughout the estrous cycle. The understanding of the mRNA–miRNA relationship will provide insights into the mechanisms of normal follicle development, further providing the possibility of new reproductive techniques and treatments in canids. However, no information is currently available on the expression of miRNAs in canine ovarian follicles. Studies on other species are only sometimes homologous to dogs because the canine estrous cycle is not comparable to the cycles of other mammals due to its length and many peculiarities. Therefore, this preliminary study aimed to evaluate the expression of miRNAs predicted against FSHR and ESR2, related to their target genes in follicular cells, comparing different phases of the estrous cycle in canines.
2. Materials and Methods
2.1. Animals
Ovaries were collected from 36 non-pregnant mixed-breed canine females (aged 1–4 years) after routine ovariohysterectomies at veterinary centers. The phases of the estrous cycle were confirmed based on the progesterone measurement of blood samples obtained during neutering.
Animal procedures were performed following the guidelines established by the Animal Care Committee at the University of Chile and the Chilean National Agency for Research and Development (ANID), Ministry of Sciences and Technology (Number 21485—VET—UCH). Informed consent was obtained from the dog tutors.
2.2. Ovaries Processing and Follicles Isolation
The ovaries were kept in saline solution (NaCl 0.9%) at 4 °C and transported to the laboratory within 20–30 min. Each ovary was rinsed in saline solution thrice, and the adipose and connective tissues were removed and placed in Petri dishes (Falcon; Becton Drive, Biosciences. Franklin Lakes, NJ, USA), in PBS, pH 7.4, supplemented with 5% (v/v) heat-inactivated fetal calf serum (FCS) [30].
Ovaries without any visual abnormalities or cystic formation were selected for the experiments and classified in each estrous phase based on ovarian structures on the surface (follicles and corpus luteum) [31] and serum progesterone concentrations using the Minireader for Canine Progesterone (Minitube, Tiefenbach, Germany), and the specific test kit for progesterone (#219001110; Minitube). The values of progesterone for each stage of the cycle were based on previous studies. Proestrus, 0.2–2 ng/mL; estrus 2–18 ng/mL; diestrus > 20 ng/mL and anestrus < 0.19 ng/mL [31,32].
Individual antral follicles free of ovarian tissue were dissected using stereomicroscopes. Follicular cells from each antral follicle were retrieved manually using a 1 mL-gauge needle and a fine-tipped glass pipette after a puncture to release the intra-follicular contents. The method used to isolate granulosa cells was described in our previous studies [32,33]. In brief, the cumulus–oocyte complexes were discarded, and the aspirated granulosa cells and the follicular fluid were transferred to a conical tube and washed three times in PBS by centrifugation at 300× g for 10 min using an Eppendorf Centrifuge 5415 D (Eppendorf, Hamburg, Germany) at 22 °C.
The follicular cell pellets were transferred to RNAlater (Invitrogen, Carlsbad, CA, USA) in tubes and kept in pools. The classification of the estrous phase (anestrus, proestrus, estrus, and diestrus) of each sample was recorded prior to pooling and subsequently stored at −20 °C until total RNA extraction. Three different cell pools were used for each estrous phase, each containing granulosa cells from around 40–60 antral follicles.
2.3. microRNA Selection
As one miRNA could regulate more than one mRNA through miRNA–mRNA interactions, and one mRNA could be regulated by several miRNAs [34], we selected and tested specific miRNAs for the target genes. Thus, miRNAs regulating FSHR mRNA (cfa-miR-8900; cfa-miR-34c; cfa-miR-34a) and ESR2 (cfa-miR-8881; cfa-miR-8837; cfa-let-7c) were selected from the Canis familiaris miRNAs databases available in the public microRNA databases miRbase [35] and miRWalk [36] (Table 1). The selection was based on the binding site-predicted targets available in the databases, based on the TarPmiR algorithm. From the predicted miRNAs targeting FSHR and ESR2, we considered the predicted probability of miRNAs and target mRNA considering the binding p-value (higher values represent a higher probability of being the target site) by evaluating three candidate miRNAs per target gene.
Table 1.
List of miRNA Primers sequences for RT-qPCR.
| Target Gene | miRNA | Primer |
|---|---|---|
| ESR2 | cfa-miR-8881 | UUUGUUUUCUCUGGUUCUGUACC |
| cfa-miR-8837 | UUCUUGCUGGAGUCCGGUUGUCU | |
| cfa-let-7c | UGAGGUAGUAGGUUGUAUGGUU *** | |
| FSH-R | cfa-miR-8900 | UAGGACUUUAAUGGCUGGAGAGA |
| cfa-miR-34c | AGGCAGUGUAGUUAGCUGAUUGC | |
| cfa-miR-34a | UGGCAGUGUCUUAGCUGGUUGU. *** | |
| ref miRNAs | cfa-miR-16 | 5′-UAGCAGCACGUAAAUAUUGGCG-3′ |
| ref miRNAs | cfa-miR-26 | 5′-UUCAAGUAAUCCAGGAUAGGCU-3′ |
*** Selected miRNA considering qPCR performance and target predicted probability with binding p-value of 1.0.
2.4. RNA Isolation, Primers, and qPCR Analysis
For miRNA and mRNA expression assessment, total RNA was extracted using the Gene JET RNA Purification Kit (#K0731, Thermo Scientific, Eugene, OR, USA), according to the manufacturer’s instructions. The concentration and purity of the total RNA were determined using an Epoch spectrophotometer (Epoch, Biotek Industries, Highland Park, IL, USA). The total RNA was stored at −80 °C.
The synthesis of cDNA from miRNA was performed using the Affinity Script qPCR cDNA synthesis kit (Agilent Technologies, Santa Clara, CA, USA) following manufacturer’s instructions. The cDNA concentration was assessed using the Epoch spectrophotometer (Epoch, Biotek Industries, Biotek Instrument, Winooski, VT, USA). We selected reference miRNAs previously validated in Canis familiaris to perform the miRNA expression analysis. Six miRNA-specific forward and universal reverse primers were used to amplify the mature miRNAs. Two reference miRNAs cfa-miR-16 [37] and cfa-miR-26a [38] (Table 1) were the most stable reference miRNAs and were selected as normalizers for relative quantification of miRNA expression levels. Primers for amplifying canine miRNAs were designed using available sequences from previously described databases, or from publications regarding reference genes.
For FSHR mRNA, canine-specific primers were designed under standard procedures using information from GenBank sequences to Canis familiaris. For ESR2, canine-specific primers were used according to Goncalves et al. [39]. β-actin (ACTB) and H2A histone (H2A) were used as normalized reference genes, consistent with previous studies [31,40] (Table 2).
Table 2.
Sequences of primers for references genes used in this study and FSH-R, ESR2 genes evaluated for qRT-PCR analysis.
| Gene | Sequence 5′-3′ | Accession Number | Amplicon | Tm °C | Efficence |
|---|---|---|---|---|---|
| ACTB | F:ATTGTCATGGACTCTGGGGATG | AF021873.2 | 191 bp | 56.7 | 1.99 |
| R:TCCTTGATGTCACGCACGAT | |||||
| H2A | F:AGTACCTGACGGCCGAGAT | XM545419.4 | 245 bp | 59.6 | 1.97 |
| R:AGGGCAAATCAATCCAGAGA | |||||
| ESR2 | F: TTCTATAGCCCTGCTGTGATGAAT | AF389885.1 | 204 bp | 60.0 | 2.01 |
| R: ATTATGTCCTTGAATGCTTCTTT | |||||
| FSH-R | F:AACTCATTTGGCCATCCTTG | NC051814.1 | 212 bp | 60.0 | 1.98 |
| R:TGACTGCACCTTAGGCAGTG |
Abbreviation: FSHR, follicle-stimulating hormone gene receptor. ESR2, Estrogen gene receptor beta. ACTB, β-actin and H2A, histone genes.
Quantitative expressions of miRNAs and mRNA were assessed with an Eco Real-Time PCR System Model EC-100-1001 (Illumina®, San Diego, CA, USA) using qPCR miRNA Master Mix (Agilent Technologies, Santa Clara, CA, USA) following the manufacturer’s protocols. For mRNA assessment, cDNA was obtained using the enzyme conjugate Affinity Script cDNA Synthesis Kit (Agilent Technologies, Santa Clara, CA, USA) and the cDNA concentration was determined using an Epoch spectrophotometer (Epoch, Biotek Industries). For mRNA and miRNA analysis, control samples, without reverse transcriptase, 10 ng of cDNA template, or primers, were included in duplicate in each plate. Data were analyzed using the ΔΔCT method of relative quantification.
2.5. Statistical Analysis
Multiple comparisons of the relative expression levels of miRNA and mRNAs in follicular cells and reproductive stage were analyzed by ANOVA using the InfoStat Professional Program, Version 2018, Cordoba, Argentina. The data were transformed into a normal distribution before applying the analysis. Significant differences among means were evaluated using the Duncan’s test.
The possible association between the expression pattern of each miRNAs and its target genes throughout the follicular development was evaluated using Pearson’s correlation coefficient.
All values were considered significantly different for p ≤ 0.05.
3. Results
The best miRNA for each target gene (ESR2 and FSHR) was selected considering qPCR performance (low ct value and specific melt curve), and target prediction probability, selecting only miRNAs with a binding p-value of 1.0, with cfa-miR-34a, targeting the coding sequence in the position 1390 to 1438 of the FSHR gene, and cfa-let-7c (lethal-7), targeting the 3′ UTR sequence in the position 1915 to 1933 of the ESR2 gene.
The expression of each miRNA and its target genes was observed in the granulosa cells at all reproductive cycle stages, confirming their presence in canine follicles. The relative abundance of FSHR and ESR2 transcripts and the miRNAs cfa-miR-34a and cfa-let-7c exhibited specific-stage variations in follicular cells.
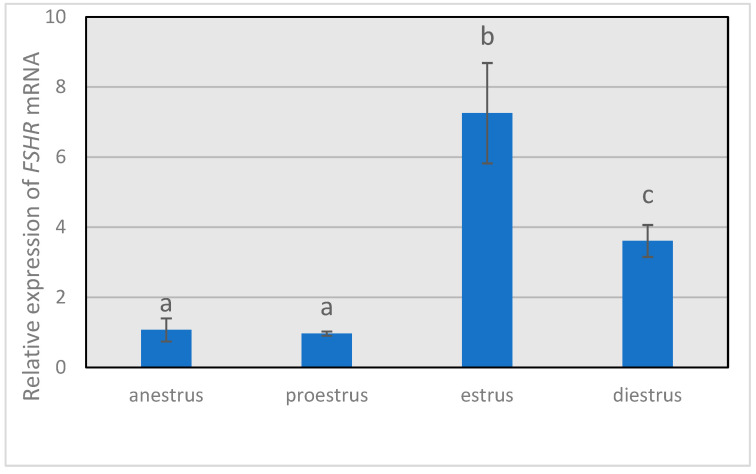
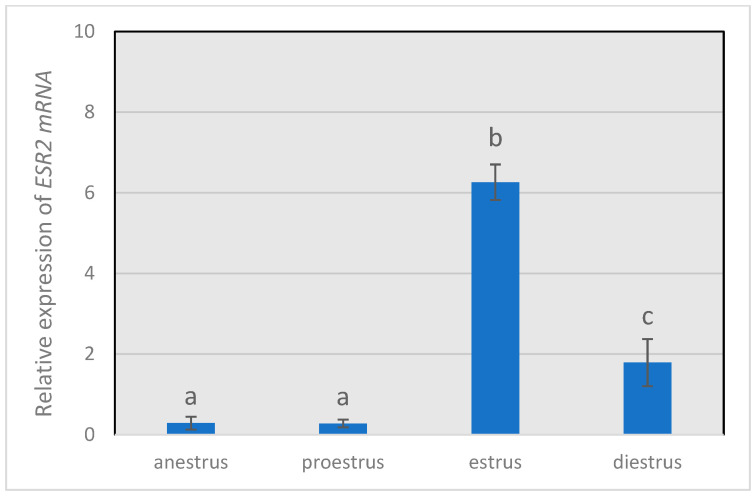
The relative expression of FSHR (Figure 1) remained low during anestrus and proestrus, increasing (p < 0.05) to the highest value in the estrus phase and decreasing (p < 0.05) during diestrus, but with a higher (p < 0.05) expression level than that observed in anestrus or proestrus. The same trend was shown by ESR2 transcript (Figure 2), with the highest (p < 0.05) relative abundance in estrus and the lowest values (p < 0.05) in granulosa cells from anestrus and proestrus.
Figure 1.
Gene expression levels of FSHR throughout the different phases of the estrous cycle. FSHR mRNA expression levels relative to the housekeeping genes β-actin RNA (ACTB) and histone H2A (H2A). Different letters above the bars indicate significant differences (p < 0.05).
Figure 2.
Gene expression levels of ESR2 throughout the different phases of the estrous cycle. Gene expression levels of ESR2 relative to those of the housekeeping genes β-actin RNA (ACTB) and histone H2A (H2A). Different letters above the bars indicate significant differences (p < 0.05).
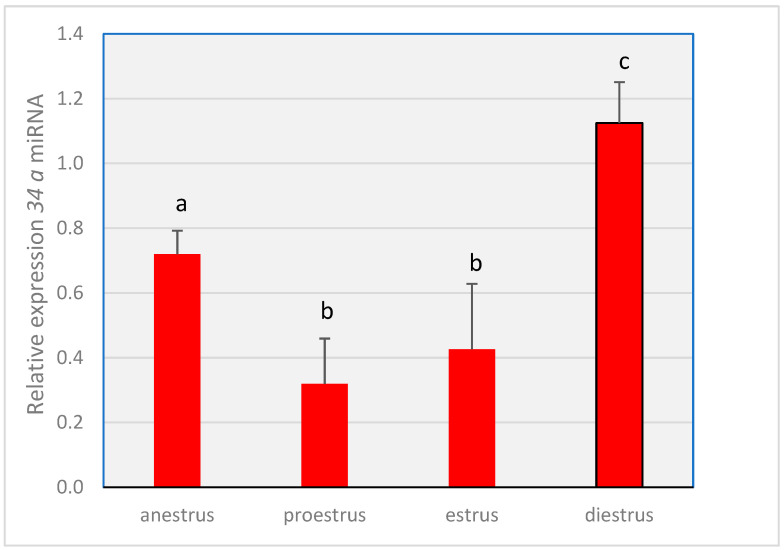
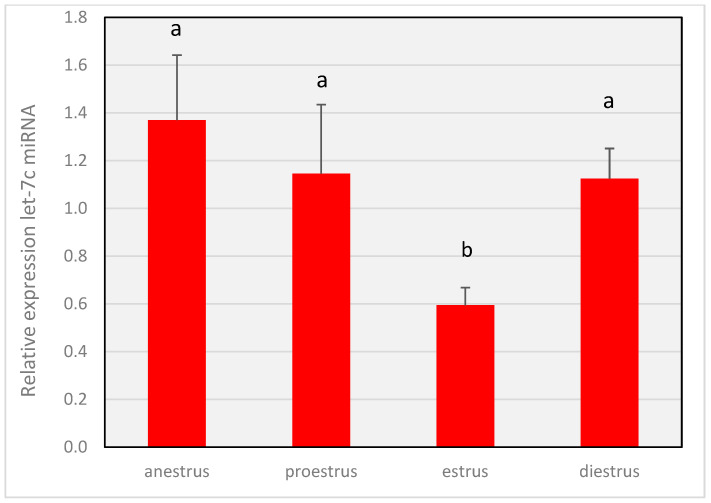
Differences (p < 0.05) were observed in the expression of both miRNA-34a (Figure 3) and MiR-let-7c (Figure 4) throughout the cycle. The expression level of miR-34a in proestrus and estrus was lower (p < 0.05) compared to that in anestrus and diestrus, with the highest values (p < 0.05) observed in the diestrus phase. MiR-let-7c showed a decrease (p < 0.05) in relative expression during the estrus phase compared to the other three stages, where the relative abundance was similar (p > 0.05).
Figure 3.
Gene expression levels of 34a miRNA throughout the different phases of the estrous cycle. The miRNA expression of miR-34a relative to those of the reference miRNAs cfa-miR-16 and cfa-miR-26a. Different letters above the bars indicate significant differences (p < 0.05).
Figure 4.
Gene expression levels of miR-let-7c throughout the different phases of the estrous cycle. The miRNA expression of miR-let-7c relative to those of the reference miRNAs cfa-miR-16 and cfa-miR-26a. Different letters above the bars indicate significant differences (p < 0.05).
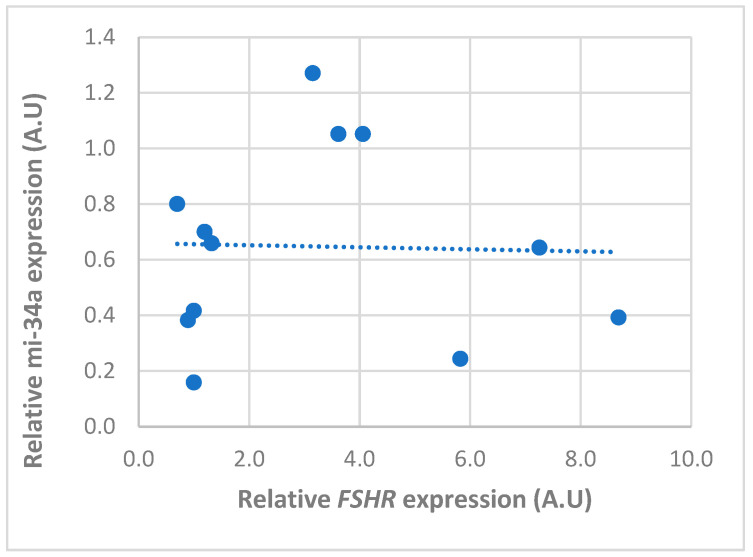
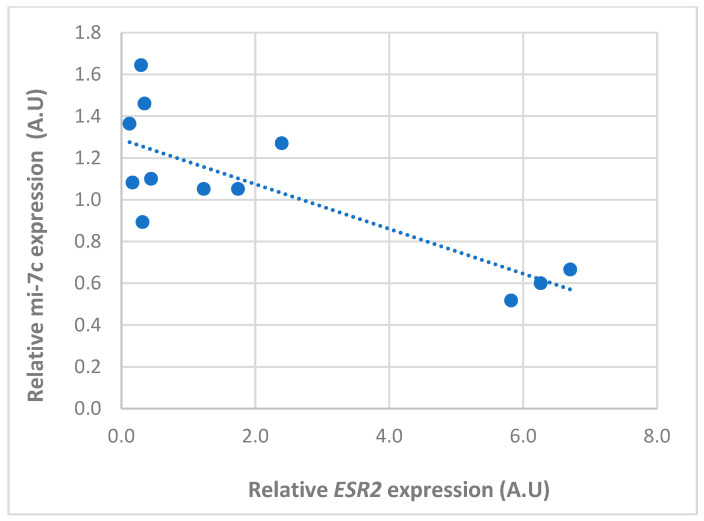
There was a tendency for an inverse relationship between the expression of miR-34a and its target gene (FSHR) only in the anestrus phase (Figure 5). However, no significant correlation was observed throughout the whole cycle (r = −0.06), whereas an inverse and significative correlation (r = −0.8) was found between miRNA-7c and ESR2 (Figure 6; p < 0.01).
Figure 5.
Pearson correlation between the relative expression of miR-34a and FSHR mRNA in follicular cells obtained from follicles in different phases of the canine estrous cycle. Dots represents the normalized expression level of each gene in A.U (arbitrary unit) and dotted line represent the trend line. No significant correlation was observed throughout the whole cycle (r = −0.06).
Figure 6.
Pearson correlation between the relative expression of miR-let-7c and ESR2 mRNA in follicular cells obtained from follicles in different phases of the canine estrous cycle. Dots represents the normalized expression level of each gene in A.U (arbitrary unit) and dotted line represent the trend line for correlation. An inverse and significative correlation (r = −0.8) was found between miRNA-7c and ESR2 throughout the estrus cycle.
4. Discussion
This study demonstrated for the first time the expression of two miRNAs predicted against two essential genes, FSHR and ESR2, involved in follicular and oocyte development and their temporal abundance concerning their target genes in ovarian follicular cells in canines.
Although FSHR and its encoded receptors have been reported in canine granulosa cells [6,41], its variation throughout the estrous cycle has not been previously described in this species. The different FSHR expression patterns found during the estrous phases in the present study showed cyclic changes in growing follicles, implying that FSHR expression could be developmentally and hormonally regulated in dogs, like in other species [2,42]. Notably, the lowest FSHR mRNA expression levels were observed during the anestrus and proestrus phases. During the anestrus, the concentration of circulating FSH is the highest in the dog estrous cycle [43], although, without changes in the expression of its receptor (FSHR) [7]. Coincidentally, it has been demonstrated that FSH stimulation can inhibit FSHR transcription in Sertoli cells [44], involving self-regulation between hormone levels and the gene expression of its receptor. However, FSHR expression involves various other regulatory mechanisms that affect its stability and translation efficiency [42]. The FSHR is a target gene of different miRNAs, as demonstrated for miRNA-125 in porcine granulosa cells [29], and miRNA-3 and miRNA-143 in bovine granulosa cells [26]. We analyzed the expression pattern of cfa-miRNA-34a (miR-34a) in canine granulosa cells, which was predicted to regulate canine FSHR. The expression of miR-34a was higher in the anestrus and diestrus phases than in the other phases, which was consistent with the low level of FSHR relative expression in anestrus, when FSH concentration is high, but not in the diestrus stage, when the circulating FSH is low. MicroRNA 34a, as a member of the miR-34 family (miR-34a/b/c, miR-34s) [45], has been proposed to control essential ovarian functions and negatively regulate the local translation of FSHR. In porcine ovarian cells, FSH promotes the expression of miR-34a [46], indicating that miR-34a may be involved in controlling ovarian functions; as both, miR-34a and FSH are synergists in their actions on follicular cell activity. Therefore, the influence of miR-34a on FSHR may depend on FSH levels which are high during canine anestrus. This could explain the trend towards an inverse relationship between cfa-miRNA-34a and its target gene only in anestrus, and the lack of significance in the correlation between cfa-miRNA-34a and FSHR abundance throughout the other phases of the estrous cycle.
Granulosa cells express mainly ERβ [47], and the ovary is the primary site associated with the highest level of ERβ [48]. Therefore, ERβ seems to be a critical mediator of estradiol signaling in granulosa cells orchestrating folliculogenesis. In a mouse model, ESR2 mRNA expression has been associated with ovarian responsiveness to gonadotropins [49]. The present findings showed that ESR2 mRNA was highly expressed in follicular cells during the estrus period, with very low transcript abundance prior to this stage. In other species, ESR2 in follicles is mainly expressed during the follicular phase [50] and is possibly involved in regulating the ovulation process during the estrus stage. In ESR2-knockout mice, luteinizing hormone receptors become insufficient for ovulation [45]. Furthermore, it has been reported that the pre-ovulatory estradiol surge in dogs probably triggers the pre-ovulatory peak in LH [33,51]. Therefore, estradiol could influence the ovulation process via ERβ-ESR2 mediation [12]. However, the precise mechanisms by which ESR2 regulates the estrous cycle and ovulation mechanisms are not yet fully understood.
MicroRNAs have been involved in the regulation of estrogen production in granulosa cells [52]. MiR-let-7c is one of the earliest identified miRNAs [53], and its family members are highly conserved across species and the most abundant miRNAs in the ovary [54,55], suggesting that they have fundamental roles in reproductive physiology. Here, miR-let-7c was observed during all phases of the canine estrous cycle, which agrees with the presence of miR-let-7c in the ovine [56] and caprine [57] granulosa cells. The lowest miR-let-7c expression level was observed in the estrus phase, while the relative gene expression of ESR2, the predicted target of miR-let-7c, was the highest. In contrast, in other phases of the cycle, the expression of miR-let-7c was higher, whereas that of the ESR2 gene was lower. Therefore, miR-let-7c was inversely related to ESR2 expression, consistent with previous studies on breast cancer stem cells [58]. MiR-let-7c can regulate ERβ presence by directly targeting its mRNA ESR2, decreasing its expression [58], or affecting signaling pathways involved in ESR2 expression [58]. Further research is necessary to decipher the complex regulatory mechanisms underlying ESR2 and miR-let-7c expression and their roles in reproductive physiological processes in canines.
5. Conclusions
The differential expression profile of miR-34a and miR-let-7c and their predicted target genes in canine ovarian follicles throughout the estrous cycle obtained in the present study suggest a role in the transcriptional regulation of FSHR and ESR2 genes, which represents the first evidence of the involvement of these miRNAs in the canine follicular function, opening the possibility of investigating their future use in different reproductive treatments in this species. Advanced research on miRNAs in the canine ovary will help to understand the mechanisms and regulation involved.
Acknowledgments
We thank the veterinary staff of the La Pintana and Peñalolen Veterinary Clinical Centers for providing canine ovaries.
Author Contributions
M.D.l.R. Conceptualization, investigation, writing. P.D. Conceptualization, investigation, formal analysis. J.P. Methodology, formal analysis, O.A.P. Methodology, formal analysis. A.V. Methodology. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The animal study protocol was approved by the Institutional Ethics Committee of University of Chile (CICUA) (protocol code 21485, 28 July 2021).
Informed Consent Statement
Written informed consent was obtained from the owners of the animals.
Data Availability Statement
The data of this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This study was financed by the National Foundation for Scientific and Technological Research (FONDECYT. Grant 1211285), from the National Research and Development Agency (ANID). Ministry of Sciences and Technology.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Bosch E., Alviggi C.M., Conforti A., Hanyaloglu A.C., Chuderland D., Simoni M., Raine-Fenning N., Crépieux P., Kol S., Rochira V., et al. Reduced FSH and LH action: Implications for medically assisted reproduction. Hum. Reprod. 2021;36:1469–1480. doi: 10.1093/humrep/deab065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.George J., Dille E.A., Heckert L.L. Current Concepts of Follicle-Stimulating Hormone Receptor Gene Regulation. Biol. Reprod. 2011;84:7–17. doi: 10.1095/biolreprod.110.085043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McDonald R., Sadler C., Kumar T.R. Gain–of–Function Genetic Models to Study FSH Action. Front. Endocrinol. 2019;10:28. doi: 10.3389/fendo.2019.00028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tisdall D.J., Watanabe N.L., Hudson P., McNatty K.P. FSH receptor gene expression during ovarian follicle development in sheep. J. Mol. Endocrinol. 1995;15:273–281. doi: 10.1677/jme.0.0150273. [DOI] [PubMed] [Google Scholar]
- 5.Wandji S.A., Eppig J.J., Fortune J.E. FSH and growth factors affect the growth and endocrine function in vitro of granulosa cells of bovine preantral follicles. Theriogenology. 1996;45:817–832. doi: 10.1016/0093-691X(96)00011-8. [DOI] [PubMed] [Google Scholar]
- 6.De Cock H., Ducatelle R., Logghe J.P. Immunohistochemical localization of estrogen receptor in the normal canine female genital tract. Dom. Anim. Endocrinol. 1997;14:133–147. doi: 10.1016/S0739-7240(97)00001-5. [DOI] [PubMed] [Google Scholar]
- 7.McBride M.W., Aughey E., O’Shaughnessy P.J., Jeffcoate I.A. Ovarian function and FSH receptor characteristics during canine anoestrus. J. Reprod. Fertil. Suppl. 2001;57:3–10. [PubMed] [Google Scholar]
- 8.Saint-Dizier M., Jaffré N., Reynaud K., Remy B., Thoumire S., Chastant-Maillard S. Expression of follicle-stimulating hormone and luteinising hormone binding sites in the bitch ovary during the follicular phase. Reprod. Fertil. Dev. 2008;20:925–934. doi: 10.1071/RD08119. [DOI] [PubMed] [Google Scholar]
- 9.Klinge C.M. Estrogen Regulation of MicroRNA Expression. Curr. Genom. 2009;10:169–183. doi: 10.2174/138920209788185289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O’Lone R., Frith M.C., Karlsson E.K., Hansen U. Genomic Targets of Nuclear Estrogen Receptors. Mol. Endocrinol. 2004;18:1859–1875. doi: 10.1210/me.2003-0044. [DOI] [PubMed] [Google Scholar]
- 11.Tang Z.R., Zhang R., Lian Z.X., Deng S.L., Yu K. Estrogen-Receptor Expression and Function in Female Reproductive Disease. Cells. 2019;8:1123. doi: 10.3390/cells8101123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hatoya S., Torii R., Kumagai D., Sugiura K., Kawate N., Tamada H., Sawada T., Inaba T. Expression of estrogen receptor a and b genes in the medio basal hypothalamus, pituitary and ovary during the canine estrous cycle. Neurosci. Let. 2003;347:131–135. doi: 10.1016/S0304-3940(03)00639-6. [DOI] [PubMed] [Google Scholar]
- 13.Lee E.B., Chakravarthi V.P., Wolfe M.W., Rumi M.A. ERβ Regulation of Gonadotropin Responses during Folliculogenesis. Int. J. Mol. Sci. 2021;22:10348. doi: 10.3390/ijms221910348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Emori C., Kanke T., Ito H., Akimoto Y., Fujii W., Naito K., Sugiura K. Expression and regulation of estrogen receptor 2 and its coregulators in mouse granulosa cells. J. Reprod. Dev. 2022;68:137–143. doi: 10.1262/jrd.2021-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Couse J.F., Yates M.M., Deroo B.J., Korach K.S. Estrogen receptor-beta is critical to granulosa cell differentiation and the ovulatory response to gonadotropins. Endocrinology. 2005;146:3247–3262. doi: 10.1210/en.2005-0213. [DOI] [PubMed] [Google Scholar]
- 16.Toms D., Pan B., Li J. Endocrine Regulation in the Ovary by MicroRNA during the Estrous Cycle. Front. Endocrinol. 2018;8:378. doi: 10.3389/fendo.2017.00378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang S., Wang S., Luo A., Ding T., Lai Z., Shen W. Expression patterns and regulatory functions of microRNAs during the initiation of primordial follicle development in the neonatal mouse ovary. Biol. Reprod. 2013;89:126. doi: 10.1095/biolreprod.113.107730. [DOI] [PubMed] [Google Scholar]
- 18.Sen A., Prizant H., Light A., Biswas A., Hayes E., Lee H.J., Barad D., Gleicher N., Hammes S.R. Androgens regulate ovarian follicular development by increasing follicle stimulating hormone receptor and microRNA-125b expression. Proc. Natl. Acad. Sci. USA. 2014;111:3008–3013. doi: 10.1073/pnas.1318978111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dehghan Z., Mohammadi-Yeganeh S., Rezaee D., Salehi M. MicroRNA-21 is involved in oocyte maturation, blastocyst formation, and pre-implantation embryo development. Dev. Biol. 2021;480:69–77. doi: 10.1016/j.ydbio.2021.08.008. [DOI] [PubMed] [Google Scholar]
- 20.Ro S., Song R., Park C., Zheng H., Sanders K.M., Yan W. Cloning and expression profiling of small RNAs expressed in the mouse ovary. RNA. 2007;13:2366–2380. doi: 10.1261/rna.754207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tesfaye D., Gebremedhn S., Salilew-Wondim D., Hailay T., Hoelker M., Grosse-Brinkhaus C., Schellander K. MicroRNAs: Tiny molecules with a significant role in mammalian follicular and oocyte development. Reproduction. 2018;155:R121–R135. doi: 10.1530/REP-17-0428. [DOI] [PubMed] [Google Scholar]
- 22.Ambros V. MicroRNAs: Tiny regulators with great potential. Cell. 2001;107:823–826. doi: 10.1016/S0092-8674(01)00616-X. [DOI] [PubMed] [Google Scholar]
- 23.O’Brien J., Hayder H., Zayed Y., Peng C. Overview of MicroRNA Biogenesis, Mechanisms of Actions, and Circulation. Front. Endocrinol. 2018;9:402. doi: 10.3389/fendo.2018.00402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vasudevan S., Tong Y.C., Steitz J.A. Switching from repression to activation: microRNAs can up-regulate translation. Science. 2007;318:1931–1934. doi: 10.1126/science.1149460. [DOI] [PubMed] [Google Scholar]
- 25.Yin M., Wang X., Yao G. Transactivation of micrornA-320 by microRNA-383 regulates granulosa cell functions by targeting E2F1 and SF-1 proteins. J. Biol. Chem. 2014;289:18239–18257. doi: 10.1074/jbc.M113.546044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang Z., Chen C.Z., Xu M.Q., Zhang L.Q., Liu J.B., Gao Y., Jiang H., Yuan B., Zhang J.B. MiR-31 and miR-143 affect steroid hormone synthesis and inhibit cell apoptosis in bovine granulosa cells through FSHR. Theriogenology. 2018;123:45–53. doi: 10.1016/j.theriogenology.2018.09.020. [DOI] [PubMed] [Google Scholar]
- 27.Yin M., Lu M., Yao G., Tian H., Lian J., Liu L., Liang M., Wang Y., Sun F. Transactivation of microRNA-383 by steroidogenic factor-1 promotes estradiol release from mouse ovarian granulosa cells by targeting RBMS1. Mol. Endocrinol. 2012;26:1129–1143. doi: 10.1210/me.2011-1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Donadeu F.X., Schauer S.N., Sontakke S.D. Involvement of miRNAs in ovarian follicular and luteal development. J. Endocrinol. 2012;215:323–334. doi: 10.1530/JOE-12-0252. [DOI] [PubMed] [Google Scholar]
- 29.Fabová Z., Loncová B., Sirotkin A.V. MicroRNA miR-125b can suppress ovarian granulosa cell functions: Interrelationships with FSH. Cell Biochem. Funct. 2022;41:177–188. doi: 10.1002/cbf.3771. [DOI] [PubMed] [Google Scholar]
- 30.De Los Reyes M., Palomino J., Araujo A., Flores J., Ramirez G., Parraguez V.H., Aspee K. Cyclooxygenase 2 messenger RNA levels in canine follicular cells: Interrelationship with GDF- 9, BMP-15 and progesterone. Dom. Anim. Endocrinol. 2021;74:106529. doi: 10.1016/j.domaniend.2020.106529. [DOI] [PubMed] [Google Scholar]
- 31.Ramirez G., Palomino J., Aspee K., De los Reyes M. GDF-9 and BMP-15 mRNA levels in canine cumulus cells related to cumulus expansion and the maturation process. Animals. 2020;10:462. doi: 10.3390/ani10030462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fernandez T., Palomino J., Parraguez V.H., Peralta O.A., De los Reyes M. Differential expression of GDF-9 and BMP- 15 during follicular development in canine ovaries evaluated by flow cytometry. Anim. Reprod. Sci. 2016;167:59–67. doi: 10.1016/j.anireprosci.2016.02.005. [DOI] [PubMed] [Google Scholar]
- 33.De los Reyes M., Palomino J., Parraguez V.H., Ramírez F. Analysis of LH receptor in canine ovarian follicles throughout the estrous cycle. Theriogenology. 2017;93:71–77. doi: 10.1016/j.theriogenology.2017.01.029. [DOI] [PubMed] [Google Scholar]
- 34.Kozomara A., Birgaoanu M., Griffiths-Jones S. miRBase: From microRNA sequences to function. Nucleic Acids Res. 2019;47:55–62. doi: 10.1093/nar/gky1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sticht C., De La Torre C., Parveen A., Gretz N. miRWalk: An online resource for prediction of microRNA binding sites. PLoS ONE. 2018;13:0206239. doi: 10.1371/journal.pone.0206239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Riolo G., Cantara S., Marzocchi C., Ricci C. miRNA Targets: From Prediction Tools to Experimental Validation. Methods Protoc. 2021;4:1. doi: 10.3390/mps4010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Craig K.K., Wood G.A., Keller S., Mutsaers A.J., Wood R.D. MicroRNA profiling in canine multicentric lymphoma. PLoS ONE. 2019;14:e0226357. doi: 10.1371/journal.pone.0226357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Narita M., Nishida H., Asahina R., Nakata K., Yano H., Ueda T., Inden M., Akiyoshi H., Maeda S., Kamishina H. Identification of reference genes for microRNAs of extracellular vesicles isolated from plasma samples of healthy dogs by ultracentrifugation, precipitation, and membrane affinity chromatography methods. Am. J. Vet. Res. 2019;80:449–454. doi: 10.2460/ajvr.80.5.449. [DOI] [PubMed] [Google Scholar]
- 39.Goncalves J.S.A., Vannucchi C.I., Braga F.C., Paula-Lopes F.F., Milazzotto M.P., Assumpcao M.E.O.A., Visintin J.A. Oestrogen and Progesterone receptor gene expression in canine oocytes and cumulus cells throughout the oestrous cycle. Reprod. Dom. Anim. 2009;44((Suppl. S2)):239–242. doi: 10.1111/j.1439-0531.2009.01422.x. [DOI] [PubMed] [Google Scholar]
- 40.Palomino J., De los Reyes M. Temporal expression of GDF-9 and BMP-15 mRNAs in canine ovarian follicles. Theriogenology. 2016;86:1541–1549. doi: 10.1016/j.theriogenology.2016.05.013. [DOI] [PubMed] [Google Scholar]
- 41.Nagashima J.B., Wildt D.E., Alexander T.J., Songsasen N. Activin Promotes Growth and Antral Cavity Expansion in the Dog Ovarian Follicle. Theriogenology. 2019;15:168–177. doi: 10.1016/j.theriogenology.2019.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kishi H., Kitahara Y., Imai F., Nakao K., Suwa H. Expression of the gonadotropin receptors during follicular development. Reprod. Med. Biol. 2018;17:11–19. doi: 10.1002/rmb2.12075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Concannon P.W. Research challenges in endocrine aspects of canine ovarian cycles. Reprod. Dom. Anim. 2012;47((Suppl. S6)):6–12. doi: 10.1111/rda.12121. [DOI] [PubMed] [Google Scholar]
- 44.Viswanathan P., Wood M.A., Walker W.H. Follicle-stimulating hormone (FSH) transiently blocks FSH receptor transcription by increasing inhibitor of deoxyribonucleic acid binding/differentiation-2 and decreasing upstream stimulatory factor expression in rat Sertoli cells. Endocrinology. 2009;150:3783–3791. doi: 10.1210/en.2008-1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Imani S., Wu R.C., Fu J. MicroRNA-34 family in breast cancer: From research to therapeutic potential. J. Cancer. 2018;9:3765–3775. doi: 10.7150/jca.25576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fabová Z., Loncová B., Bauer M., Sirotkin A.V. Interrelationships Between miR-34a and FSH in the Control of Porcine Ovarian Cell Functions. Reprod. Sci. 2023;30:1789–1807. doi: 10.1007/s43032-022-01127-2. [DOI] [PubMed] [Google Scholar]
- 47.Jefferson W.N., Couse J.F., Banks E.P., Korach K.S., Newbold R.R. Expression of estrogen receptor beta is developmentally regulated in reproductive tissues of male and female mice. Biol. Reprod. 2000;62:310–317. doi: 10.1095/biolreprod62.2.310. [DOI] [PubMed] [Google Scholar]
- 48.Drummond A.E., Fuller P.J. The importance of ERbeta signalling in the ovary. J. Endocrinol. 2010;205:15–23. doi: 10.1677/JOE-09-0379. [DOI] [PubMed] [Google Scholar]
- 49.Rumi M.A.K., Singh P., Roby K.F., Zhao X., Iqbal K., Ratri A., Lei T., Cui W., Borosha S., Dhakal P., et al. Defining the Role of Estrogen Receptor β in the Regulation of Female Fertility. Endocrinology. 2017;158:2330–2343. doi: 10.1210/en.2016-1916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bao B., Kumar N., Karp R.M., Garverick H.A., Sundaram K. Estrogen receptor-beta expression in relation to the expression of luteinizing hormone receptor and cytochrome P450 enzymes in rat ovarian follicles. Biol. Reprod. 2000;63:1747–1755. doi: 10.1095/biolreprod63.6.1747. [DOI] [PubMed] [Google Scholar]
- 51.Wildt D.E., Panko W.B., Chakraborty P.K., Seager S.W.J. Relationship of serum estrone, estradiol-17b and progesterone to LH, sexual behavior, and time of ovulation in the bitch. Biol. Reprod. 1979;20:648–658. doi: 10.1095/biolreprod20.3.648. [DOI] [PubMed] [Google Scholar]
- 52.Pan B., Zhan X., Li J. MicroRNA-574 Impacts Granulosa Cell Estradiol Production via Targeting TIMP3 and ERK1/2 Signaling Pathway. Front. Endocrinol. 2022;13:2127. doi: 10.3389/fendo.2022.852127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Søkilde R., Persson H., Ehinger A., Pirona A.C., Fernö M., Hegardt C., Larsson C., Loman N., Malmberg M., Rydén L., et al. Refinement of breast cancer molecular classification by miRNA expression profiles. BMC Genom. 2019;20:503. doi: 10.1186/s12864-019-5887-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Roush S., Slack F.J. The let-7 family of microRNAs. Trends Cell Biol. 2008;18:505–516. doi: 10.1016/j.tcb.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 55.Xu X., Shen H.R., Yu M., Du M.R., Li X.L. MicroRNA let-7i inhibits granulosa-luteal cell proliferation and oestradiol biosynthesis by directly targeting IMP2. RBMO. 2022;44:803–816. doi: 10.1016/j.rbmo.2022.01.016. [DOI] [PubMed] [Google Scholar]
- 56.Dai T., Kang X., Yang C., Mei S., Wei S., Guo X., Ma Z., Shi Y., Chu Y., Dan X. Integrative Analysis of miRNA-mRNA in Ovarian Granulosa Cells Treated with Kisspeptin in Tan Sheep. Animals. 2022;12:2989. doi: 10.3390/ani12212989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhang X.D., Zhang Y.H., Ling Y.H., Liu Y., Cao H.G., Yin Z.-J., Ding J.P., Zhang X.R. Characterization and differential expression of microRNAs in the ovaries of pregnant and non-pregnant goats (Capra hircus) [(accessed on 1 November 2023)];BMC Genom. 2013 14:157. doi: 10.1186/1471-2164-14-157. Available online: http://www.biomedcentral.com/1471-2164/14/157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sun X., Xu C., Tang S.C., Wang J., Wang H., Wang P., Du N., Qin S., Li G., Xu S., et al. Let-7c blocks estrogen-activated Wnt signaling in induction of self-renewal of breast cancer stem cells. Cancer Gene Ther. 2016;23:83–89. doi: 10.1038/cgt.2016.3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data of this study are available on request from the corresponding author.