Summary Statement
Prospective head-to-head comparison of coronary calcium scores between standard CT and photon-counting CT show no significant differences, while photon-counting CT administers substantially lower radiation dose.
Brief Introduction
Coronary artery calcium (CAC) is a robust tool for risk prediction of cardiovascular events1. Standard computed-tomography (CT) technology uses detectors that measure the total energy across multiple photons simultaneously2. In contrast, photon-counting computed tomography (PCCT) is a new technology with detectors, which discriminate the energy of individual photons in the x-ray beam. PCCT can convert detected individual photons directly into electric signals3, increasing spatial resolution and reducing electronic noise4.
The impact of this new generation CT on the evaluation of coronary artery calcium is not yet known. The purpose of this study is to assess the performance of a PCCT system for the evaluation of CAC.
Methods
In this HIPAA-compliant, IRB approved, prospective study, all patients who received a clinical non-contrast CT CAC exam were invited to have a second scan on the PCCT system (NAEOTOM Alpha, Siemens Healthineers, Forchheim, Germany) on the same day.
Patients underwent non-contrast ECG-gated CT examination using a standard CAC protocol on a dual-source CT scanner (FORCE, Siemens Healthineers). A same-day scan on the PCCT used protocol parameters matched to standard dual-source CT for image acquisition and reconstruction (120 kVp, automated tube current modulation (reference mAs: 55, same process as in current clinical standard CT), 3 mm slice thickness, filtered-back projection (FBP) in EID/FBP at 70 keV reconstruction in PCCT, 1.5 mm increments, kernel: Qr36, IQ level PCCT: 10). Calcium measurements (calcium volume, mass and Agatston Score (0=no risk, 1–10=minimal risk, 11–100=mild risk, 101–400=moderate risk, >400=severe risk5)) were calculated using Syngo.Via (Siemens Healthineers), mean plaque densities using TeraRecon (TeraRecon, Inc, Durham, NC), and radiation dose measurements (volumetric CT Dose-Index, CTDIvol; Dose-Length-Product, DLP) were recorded. Contrast-to-noise ratio (CNR) and signal-to-noise ratio (SNR) were calculated. Comparisons were made using paired, two-tailed t-tests (RStudio).
Results
Of the ten patients, eight were male (age: 65 ± 9 years, BMI: 27.3 ± 8.0 kg/m2). The median calcium volume, calcium mass and Agatston score (range: 0–4056) was comparable on standard CT and on PCCT (Table 1). Agatston scores with standard CT and PCCT resulted in the same coronary artery disease risk stratification (3 patients=no risk, 3=mild risk, 1=moderate risk, 3=severe risk). Evaluated plaque was limited to calcified plaque and mean calcium densities were not significantly different between standard CT and PCCT for the left main artery (Table 1), the left anterior descending artery, the right coronary artery or the circumflex artery (Figure 1A). Image quality, as assessed by CNR (standard CT: 9.1 ± vs PCCT: 7.8 ±) and SNR (standard: 3.1 ± vs PCCT 3.2 ± ) were similar. Radiation dose was lower for PCCT than standard CT (CTDIvol clinical: 4.5 ± 3.9 vs PCCT: 2.1 ± 0.9, (P=0.06) (Figure 1B); DLP clinical: 74.8 ± 56.1 vs PCCT: 38.7 ± 10.8, (P=0.05)).
Table 1:
Measurements comparing standard clinical CT and photon-counting CT.
| Standard CT | Photon-counting CT | P-value | |
|---|---|---|---|
| Median Calcium Volume | 41 [IQR: 409] | 60 [IQR: 407] | 0.22 |
| Median Calcium Mass | 9 [IQR: 100] | 11 [IQR: 88] | 0.16 |
| Median Agatston Score | 44 [IQR: 88] | 62 [IQR: 431] | 0.26 |
| Mean Ca Density LM (SD) | 263 (106) | 241 (94) | 0.6 |
| Mean Ca Density LAD (SD) | 254 (40) | 242 (41) | 0.45 |
| Mean Ca Density RCA (SD) | 269 (53) | 253 (84) | 0.54 |
| Mean Ca Density CX (SD) | 172 (0)* | 185 (0)* | /* |
Ca=Calcium, LM=Left Main Artery, LAD=Left Anterior Descending Artery, RCA=Right Coronary Artery, CX=Circumflex Artery, SD=Standard Deviation
only one patient had calcifications in the CX.
Figure 1: Comparisons of calcium scores, mean plaque densities, and radiation doses between standard CT and photon-counting CT (PCCT).
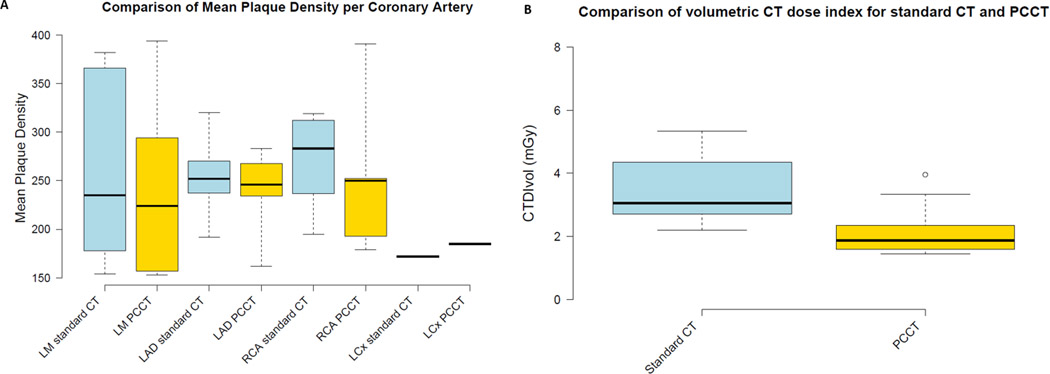
A shows the mean plaque densities were compared on a per vessel basis and showed no significant intra-individual differences between standard clinical CT and PCCT. B, the volumetric CT dose index (CTDIvol) trended lower for PCCT in comparison with standard clinical CT (P=0.06).
Comment
This early experience with PCCT demonstrates calcium volume and mass measurements, Agatston scores, and mean plaque densities are comparable with standard CT. We incorporated different ways of measuring coronary calcium to ensure that this was representative of different clinical practices across the US and worldwide. The Agatston score has a large body of research robustly supporting it as a clinical risk predictor of cardiovascular events. However, criticism of the Agatston score includes that it was established when CT imaging was not as advanced as it is presently and artificially reduces quality of CT images, as highly standardized reconstructions are needed, which do not reflect the capabilities of current scanner generations. The calcium volume score takes into account all pixels with an HU value of >130 and is a generally robust method for coronary risk prediction, though it is more susceptible to partial volume artifacts than the Agatston score. The calcium mass score was established to determine absolute coronary calcium mass and has been shown to have higher sensitivity and precision than the Agatston score, though its measurement is less common in clinical practice, in part because it has to be calibrated for body size. Slightly higher Agatston scores in PCCT are explained by the fact that PCCT used a fixed monoenergetic reconstruction value of 70 keV, while standard CT used 120kVp (mean energy of the spectrum depends on patient size ~70 keV to 77 keV). The observed difference was lower than expected differences across manufacturers6, and did not alter overall clinical risk classification.
Radiation dose was lower for PCCT compared with standard CT. Although this is a small, single-center study, this head-to-head comparison of calcium quantification with PCCT and standard CT aligns with pre-clinical studies performed on a prototype scanner model in a phantom and ex-vivo hearts7, who reported improved image quality and lower radiation dose for calcium scoring performed with a PCCT prototype.
In conclusion, this early evidence suggests comparable calcium quantification capabilities and similar image quality with potential for lower radiation exposure with PCCT.
Footnotes
Disclosure Statement
Author JC Ramirez-Giraldo is an employee of Siemens Healthineers. The other authors have no relevant disclosures.
Contributor Information
Fides Regina Schwartz, Duke University Health System, Department of Radiology.
Melissa A. Daubert, Duke University Health System, Department of Cardiology.
Lior Molvin, Duke University Health System, Department of Radiology.
Juan Carlos Ramirez-Giraldo, Research and Development, Siemens Healthineers.
Ehsan Samei, Duke University Health System, Department of Radiology.
Daniele Marin, Duke University Health System, Department of Radiology.
Tina D. Tailor, Duke University Health System, Department of Radiology.
References
- 1.Pletcher MJ, Tice JA, Pignone M, Browner WS. Using the Coronary Artery Calcium Score to Predict Coronary Heart Disease Events: A Systematic Review and Meta-analysis. Archives of Internal Medicine. 2004;164:1285–1292. [DOI] [PubMed] [Google Scholar]
- 2.McCollough CH, Leng S, Yu L, Fletcher JG. Dual- and Multi-Energy CT: Principles, Technical Approaches, and Clinical Applications. Radiology. 2015;276:637–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Flohr T, Petersilka M, Henning A, Ulzheimer S, Ferda J, Schmidt B. Photon-counting CT review. Physica Medica. 2020;79:126–136. [DOI] [PubMed] [Google Scholar]
- 4.Willemink MJ, Persson M, Pourmorteza A, Pelc NJ, Fleischmann D. Photon-counting CT: Technical Principles and Clinical Prospects. Radiology. 2018;289:293–312. [DOI] [PubMed] [Google Scholar]
- 5.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990. Mar 15;15(4):827–32. doi: 10.1016/0735-1097(90)90282-t. PMID: 2407762. [DOI] [PubMed] [Google Scholar]
- 6.Willemink MJ, Vliegenthart R, Takx RAP, et al. Coronary Artery Calcification Scoring with State-of-the-Art CT Scanners from Different Vendors Has Substantial Effect on Risk Classification. Radiology. 2014;273:695–702. [DOI] [PubMed] [Google Scholar]
- 7.Symons R, Sandfort V, Mallek M, Ulzheimer S, Pourmorteza A. Coronary artery calcium scoring with photon-counting CT: first in vivo human experience. Int J Cardiovasc Imaging. 2019;35:733–739. [DOI] [PubMed] [Google Scholar]


