Abstract
Background
The health and well-being of volunteer donors is of critical concern for blood collection agencies responsible for ensuring a stable supply of blood products. However, lay understandings of the impact of donating blood on health remain poorly understood. As lay perceptions are likely to influence critical decisions about donation, understanding these perceptions is key for informing evidence-based approaches to donor retention and recruitment. As such, we conducted a systematic review of the blood donation literature to identify donors’ and non-donors’ perceptions of the short and longer-term physiological health effects of whole-blood and/or blood product donation.
Materials and methods
This review was conducted in line with PRISMA guidelines. Studies published from January 1995 to February 2021 were included. Perceptions were defined as both experiences and beliefs. Psychological effects were considered outside the scope of the review.
Results
A total of 247 studies were included. Most studies (89.5%) had donation-related health perceptions as a background rather than a central (10.5%) focus, and they were only assessed in relation to whole blood donation. More results focused on health-related beliefs than experiences (82 vs 18%), specific rather than general beliefs and experiences (80 vs 20%) and more frequently examined negative than positive beliefs and experiences (83 vs 17%). The most commonly studied and reported specific negative beliefs related to increased risk of infectious disease, reduced vitality, vasovagal reactions and low iron. Most studies examining specific negative beliefs were conducted in Asian countries.
Discussion
Findings reinforce that lay perspectives on how donation impacts health are under-researched, and it is difficult to know how important these are in informing critical decisions about donation for donors and non-donors. We suggest that further research with donation-related health beliefs and experiences as the central focus is needed to provide insights to inform communications with donors and the public.
Keywords: blood donors, health, systematic review, blood banks, attitude
INTRODUCTION
Blood Collection Agencies (BCAs) rely on volunteer donors to ensure a stable supply of blood products. Globally, BCAs struggle to maintain sufficient supply, with the trend of increasingly lower participation in blood donation exacerbated by COVID-191,2. As such, the health and well-being of volunteer donors is of critical concern, both for those who receive blood products and for the ongoing participation of these donors. While research has focused on acute reactions that occur around the time of donation3 (e.g., injuries, vasovagal reactions), or on the longer-term management of iron deficiency4,5,6, lay understandings of the impact donating blood may have on health remain poorly understood. This is problematic as such perceptions likely impact the decision to donate or not, the frequency at which donations are made, and the products donated7. As such, understanding lay perceptions of the impact donating has on health is key to informing evidence-based approaches to donor retention and recruitment.
While not an explicit health-seeking behavior, donating blood is associated with being healthy. Donors undergo health screening to be eligible to donate and may also receive health information such as blood pressure and hemoglobin readings through donating6. In turn, those who perceive themselves to be healthy tend to become, and remain donors8,9. BCAs also undertake activities that further build the association between blood donation and health, for example participating in population-based studies such as SARS-CoV-2 pandemic seroprevalence studies, inviting donors to be part of longitudinal studies of donor health, and establishing biobanks10–12. Further, some BCAs offer donors additional health information as incentives to donate13.
Despite this association between health and donating blood, there has been limited examination of how donors and non-donors perceive donation to be related to health, what informs their perceptions and how this impacts willingness to donate blood. Where these questions have been considered, most insights are elicited incidentally through studies on donor motivation7,14–21. In these, broad health perceptions are identified as both a deterrent to, and motivator of blood donation. For example, Charbonneau and colleagues (2016) surveyed continuing Canadian whole-blood donors on their motivations to donate and found that 27.0% indicated “other health reasons” were factors for reducing donation frequency or stopping donating altogether7. In contrast, Glynn et al. (2002) found 9.0% of respondents to a large-scale US-based survey17 identified the belief “donating is good for my health” as a motivator of blood donation. Outside of North America, 2.2% of respondents to a Swedish survey of donor motivations indicated that donation being “good for health” was the main reason for continuing donation21. There is some indication that health-related donation-related beliefs are culturally-specific, with research with donors and non-donors from ethnic minority backgrounds living in France22 and Australia23 identifying barriers related to fear of contracting infection and fear of losing strength as a result of donating blood.
However, in the above studies, the specific nature of the health belief, and how it motivates or deters blood donation, was not examined in-depth. For example, donors’ perceptions of their health may act as a deterrent due to a belief that they are ineligible to donate (e.g., to protect the safety of recipients), or, they may want to protect their own health from perceived negative effects of blood donation. Similarly, where health perceptions act as a motivator, the specifics of how donating is seen to be good for health or makes someone feel better have not been interrogated. One interview study with participants in the INTERVAL trial24,25 in which donors could be asked to donate blood more frequently, has explored understandings of blood and the body in relation to more frequent donation. In relation to health impacts, donors in this study perceived that their bodies naturally replenished lost blood, and felt that a general healthy lifestyle enabled them to donate blood regularly without implications for their health. As with earlier donor surveys20, it was common for interviewees in Lynch and Cohns’ study25 to raise both positive and negative health effects of blood donation. This study highlights the potential for research on donor health to generate findings that could be used to help BCAs encourage donors to give blood initially and more frequently.
Despite the potential usefulness of insights generated from these studies, we lack a comprehensive understanding of what perceived health effects of donating whole-blood and blood products have been identified in research. Having this information can help BCAs to communicate with donors and the public to better explain how blood donation affects health and to understand and address beliefs about donation and health that may prevent people from donating or encourage them to donate. This information is particularly important as BCAs continue to expand their participation in the health landscape.
Accordingly, our aims were to provide the first systematic review and integration of the blood donation literature to i. identify donors’ and non-donors’ perceptions (i.e., experiences and beliefs) regarding the short and longer-term physiological health effects of whole-blood and/or blood product donation; ii. identify the extent to which researchers have investigated health effects of whole-blood and/or blood product donation and; iii. explore differences in health perceptions of blood donation in different parts of the world.
MATERIALS AND METHODS
Full details regarding the search strategy and extraction plan are on the pre-registered Prospero record (CRD42021283396). This review was conducted in line with PRISMA guidelines26.
Search strategy
A systematic literature search of CINAHL, MEDLINE, PsycINFO, Web of Science, PubMed, Embase, ProQuest Dissertations, and Theses Global was completed in February 2021. The search strategy comprised terms related to the targeted population, their donation perceptions and donor health. A backward citation search of relevant review papers was also completed (see Prospero record for list).
The search was restricted to studies published from January 1995 to account for possible changes in blood donation populations, eligibility criteria, and procedures over time (e.g., in technology, machinery) which may impact donor perceptions. Where possible, the search was further limited to English and human participants. Finally, as the search returned a number of conference abstracts, for those deemed relevant, a supplementary search was completed to identify if a peer-reviewed full study version was available. In instances where this was the case, and the article not already captured by our search, the record was revised to reflect the full-text version.
Eligibility criteria
Following removal of duplicates, title and abstracts were screened for ineligibility by one author (SC) (i.e., not human, not in English, not about whole-blood/blood product donation, autologous and convalescent plasma donors, non-primary research articles). A second author (SK) screened 25% of records to ensure agreement (inter-rater reliability >0.80 acceptable; K=1.00). Full-text screening was then completed independently by two authors (SC and SK). Discussion between authors, including RT and BM, resolved disagreements. Table I outlines (in)eligibility criteria27.
Table I.
Eligibility criteria for the systematic review
| Inclusion criteria | Exclusion criteria |
|---|---|
| All published empirical study designs written in English a | Non-primary research articles (e.g., conference proceedings/ abstracts, editorials, commentary) |
| Theses and dissertations written in English | Multiple articles with identical samplesb |
| whole-blood, plasma, platelets, red blood cells donors | Convalescent plasma donors |
| Non-donors, first-time, repeat, deferred, and lapsed donors of all ages | Non-human donors |
| Related and non-related donors | Autologous donors |
| Remunerated and non-remunerated donors | Studies looking at perceptions of catching an illness by being in the donor centre, rather than by the donation itself (e.g., COVID, Masser et al., 2020b; Avian Influenza, Masser et al., 2011, see online supplementary content) |
While intervention studies were eligible, as examining the efficacy of interventions was not an aim, only studies with non-active control group/ pre-intervention data were included.
In such cases studies were merged and considered as a singular dataset.
Key definitions
Perceptions of health impacts of blood donation were defined as both experiences and beliefs, with each construct explored separately. Experiences referred to personally experienced consequences of donating (e.g., donating caused me to bruise), while beliefs included general understandings or opinions surrounding donation (e.g., donation affects immunity), and included third-party reports (e.g., health professionals’ opinion of patients’ health perceptions). As this study was concerned with longer-term health perceptions, rather than health events that happened during or immediately following donation, experiences were further limited to those occurring off-site and not as an immediate reaction to donation (e.g., citrate reactions during plasmapheresis donations). Consequently, experiences recorded during and/or after donation while still on-site, or recorded of f-site but in explicit reference to on-site experiences (e.g., how did you feel during donation) were considered ineligible. However, cases were permitted where it was unclear if the experience occurred on or off-site (e.g., I donated blood and felt weak) or participants reported both on and off-site experiences (e.g., which of the following symptoms did you experience during or after donation).
The term health was limited to negative and positive physiological(physicalstate, e.g., weakness, good for health) features. Psychological (mental/emotional state, e.g., well-being) effects were considered outside the scope of the review due to a lack of consistency and clarity between and within studies regarding definitions and measurement. In this review, health incorporated both specific and general consequences, which were assessed separately. Specific consequences focused on a single and explicit physical health effect (e.g., blood donation has a negative effect on fertility). General perceptions included statements of broader donation-related health effects. Importantly, such perceptions were only included if they contained a reference to self within the context of health (e.g., blood donation is good/harmful was excluded, however donation is good for my health/harmful to my body was permitted). General perceptions also included statements referring to multiple specific categories that could not be separated (e.g., donating affects fertility and immunity).
Studies that mentioned measuring health perceptions of donation as an aim were classified as central, while studies that measured health effects secondary to the aims of the study were classified as background.
DATA EXTRACTION
Two authors (SC, SK) completed 50% of data extraction and coding each. Discussions between authors occurred when there was uncertainty around inclusion/exclusion of information. The following data were extracted to provide a holistic picture of the extent to which this topic had been addressed in the literature:
study characteristics: country of origin, study design (quantitative vs qualitative), and interest in health perceptions (central, background);
participant characteristics: demographics (gender, age, education, ethnicity, and religion), and participant source (high school students, university students, blood donors at a clinic, general population, not specified, mixed);
donor characteristics: donation type (whole-blood, plasma, platelet, red blood cell, mixed) and donor type (donor, non-donor, first-time, repeat, lapsed);
health perception information: perception type (experience, belief), health effect type (specific, general), health effect direction (positive, negative), and whether the information was extractable (i.e., study included relevant methodology but not relevant results; yes, no [composite score, unusable statistics, not reported]); and
outcomes: percentage of studies that investigated each health perception and, where available, the percentage of participants that endorsed each health perception. If one study provided multiple percentages towards the same perception, the largest percentage was extracted. Percentages were averaged when one study reported multiple percentages from different samples (e.g., whole-blood vs plasma) relating to the same perception.
Insufficient data were available for extraction regarding donor remuneration status, donor relationship (related, non-related), or donor sub-group comparisons of outcomes (e.g., non-donor vs donor).
Risk of bias assessment
While the PRISMA checklist features an assessment of risk of bias, for this particular review, a quality assessment may serve as an inaccurate and invalid depiction of bias for three reasons28:
the purpose of this review is to gain insight into the current state of this literature, thus considering all studies, regardless of quality, is important;
in the majority of studies eligible for extraction, the perceived health effects were not a central focus of the study (see results for more detail), but rather a minor secondary mention; and
due to the inclusion of various study designs, different quality assessments were required which would prevent a standardized evaluation.
As such, a risk of bias assessment was not undertaken.
RESULTS
Search results
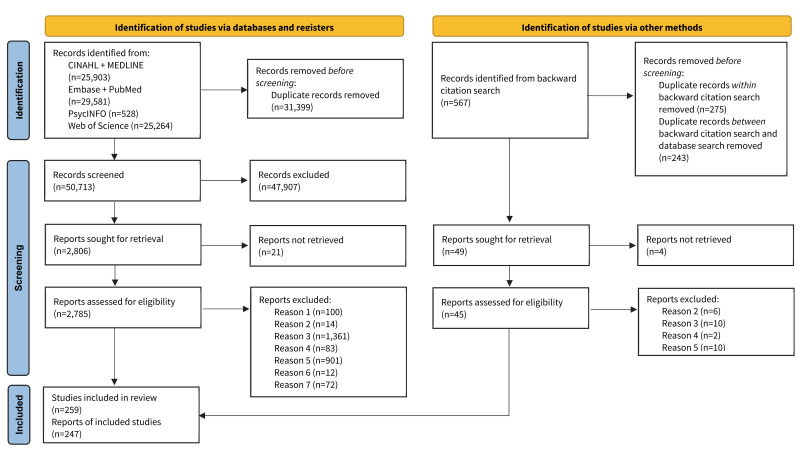
In total, 82,112 records were identified from database searches and 567 from backward citation searches. 31,917 duplicates were removed prior to screening, and 47,907 were excluded at title/abstract screening for ineligibility. 2,855 articles were sought for retrieval and of these 25 could not be retrieved, a further 100 were duplicates, 2,399 were excluded for ineligibility, and 72 included questions about donation-related health perceptions with unusable results (e.g., provided composite total scores only) and were excluded at the full-text screening stage (Figure 1). A total of 259 articles reporting on 247 unique datasets (referred to as studies below) were included in the review.
Figure 1.
PRISMA flowchart of study screening and selection procesess
Note. Reason 1 = additional manually-identified duplicates; 2 = not in English; Reason 3 = not primary data; Reason 4 = not regarding human whole blood/blood product donation; Reason 5 = donors’ perceptions of donation-related physiological health not discussed or discussed in relation to during or immediately following donation; Reason 6 = active control group and/or no pre-intervention data; Reason 7 = unusable data (e.g., total composite scale scores, included a relevant question but did not provide results).
Description of included studies
The 247 studies comprised 27 qualitative, 204 quantitative, and 16 mixed-design methods. Most studies (No.=221, 89.5%) had donation-related health perceptions as a background, rather than a central (No.=26, 10.5%), focus. Studies were published between 1995 and 2021, with 73.0% published from 2010 onwards. Over a third (39.3%) of studies originated in Asia, followed by North America (17.8%), Europe (17.0%), and Africa (16.6%). Whole-blood donation was examined most frequently (91.0%) and plasma (1.6%), platelet (0.4%), or a combination of donation types (7.0%), examined least.
Description of participants
Participants comprised either blood donors from a blood clinic/donor centre (34.0%), students (28.4%), or the general public (21.1%). Just over a third of studies included donors only (36.8%) and a third included a mix of donors and non-donors (36.0%), while 6.9% included non-donors only and 20.3% did not specify donor status. Of studies including donors (No.=180; 72.9%), the proportion of donors ranged from 2.4 to 100% (mean 65.9%, median 73.0%). In studies reporting donor experience, on average 38.0% were first-time donors (median 31.9%, range 1.6–100.0%).
Donor age was reported inconsistently as the mean, median, or proportions within age ranges. Where reported, donors were a mean age of 35.6 years (range 19.8–52.6), median 34 years (range 27–41), or most frequently within the 18–40-year age group. The mean proportion of female donors reported in studies was 38.0% (median 40.3%, range 0.0–100.0%). Studies originating in Asia (41.1%), North America (18.3%), and Europe (17.2%) most frequently included donors. Of studies including non-donors (No.=106), the mean proportion of non-donors was 65.6% (median 67.8%, range 18.4–97.6%). Non-donor age was reported in less than a quarter of studies, either as a mean or proportion within age ranges. Non-donors were aged a mean of 27.5 years (range 19.7–39.1) or were most frequently within the 18–30 years age group. The mean proportion of female non-donors reported in studies was 56.0% (median 54.3%, range 0.0–100.0%). Studies originating in Asia (52.8%) and Africa (21.7%) most frequently included non-donors.
Categories of specific health consequences
Table II shows a breakdown of the categories of specific consequences of donating blood (e.g., blood loss, vitality) which were developed after extraction and once an understanding of the literature was achieved. Specifically, two authors (SC, SK) met to discuss the overlap between the specific health-related beliefs and experiences extracted, resulting in the creation of 14 distinct categories. These categories were then examined and approved by remaining authors, before the extracted data was coded accordingly. The aim of this procedure was to meaningfully group consequences to allow for a more comprehensive and consistent comparison of the specific positive and negative health-related beliefs and experiences of donating blood.
Table II.
Categorisation of specific health consequences
| Category | Inclusion summary |
|---|---|
| Reproductive health | Fertility, menstruation, impotence |
| Immunity | Resistance to illness, getting/becoming sick, fever |
| Vitality | Energy, fitness, weakness, sleep, metabolism |
| Iron | Iron levels, anaemia, supplement use |
| Blood loss | Losing too much blood or inability to replenish blood supply |
| Infectious disease | HIV, AIDS, malaria etc. |
| Health risk/protective factors | Blood pressure, development of cancer, cardiac arrest, diabetes etc |
| Physical appearance | Weight gain/loss, acne |
| Improving blood | Filtering blood, reducing thickness, replenishing/purifying blood (removing old), increasing circulation |
| Headache | Headaches, migraines |
| Death | Dying, accelerated ageing/reduced lifespan |
| Adverse events: vasovagal reactions | Fainting, dizziness, vertigo, nausea/ feeling sick/being sick, blurred vision, extreme changes in body temperature |
| Adverse events: other physical | Bruising, nerve damage, tingling, convulsions, muscle spasms, allergic reactions, and other specific injuries |
| Adverse events: non-specific | General mention of adverse events, feeling unwell, combination of vasovagal and other physical adverse events |
Note: there were two exceptions to weakness being coded as vitality 1) when weakness in relation to anaemia, this was coded as iron; and 2) when weakness was raised in conjunction with other vasovagal reactions this was coded as adverse events: vasovagal reactions.
Beliefs and experiences
The 247 studies (Online Supplementary Content Table SI) included 568 reports of beliefs and/or experiences. Overall, more reports of health perceptions focused on beliefs than experiences (82.0 vs 18.0%), considered specific rather than general beliefs and experiences (80.0 vs 20.0%), and more frequently examined negative than positive beliefs and experiences (83.0 vs 17.0%) (Table III). In particular, reports most frequently comprised specific negative beliefs and specific negative experiences. Over 90.0% of reports of general and/or specific beliefs had health as a background rather than primary focus of the study, whereas approximately 50.0% of reports of general and/or specific experiences had health as a background focus (Table III).
Table III.
Beliefs and experiences, specificity, valence, and health focus (No.=568 reports of beliefs and/or experiences in studies)*
| General No. (%) Study reports | Specific No. (%) Study reports | ||
|---|---|---|---|
| Beliefs | Positive | 46/568 (8.1) | 45/568 (7.9) |
| Negative | 62/568 (10.9) | 313/568 (55.1) | |
| Beliefs – health focus | Background | Positive 46 (100.0) Negative 61 (98.4) |
Positive 38 (84.4) Negative 303 (96.8) |
| Central | Positive 0 (0.0) Negative 1 (1.6) |
Positive 7 (15.6) Negative 10 (3.2) |
|
| Experiences | Positive | 2/568 (0.4) | 4/568 (0.7) |
| Negative | 5/568 (0.9) | 91/568 (16.0) | |
| Experiences – health focus | Background | Positive 2 (100.0) Negative 2 (40.0) |
Positive 2 (50.0) Negative 48 (52.7) |
| Central | Positive 0 (0.0) Negative 3 (60.0) |
Positive 2 (50.0) Negative 43 (47.3) |
Five reports for specific beliefs in relation to weight loss or gain that could not be categorised as either positive or negative.
Beliefs general
Study reports of general positive beliefs (No.=46) comprised the beliefs that donation was good for health and/or that the beneficial health effects of donation motivated or were a reason for donation. On average, 40.1% of participants in these study reports mentioned general positive beliefs (e.g., “Donation is good for one’s health”) (Table IV). Over half of the reports for general positive beliefs occurred in studies conducted in Asia.
Table IV.
Study reports for general positive (No.=46) and general negative (No.=62) beliefs by continent
| Continent | General beliefs | |||||||
|---|---|---|---|---|---|---|---|---|
| Positive | Negative | |||||||
| No. (%) Study reports of beliefs | Range % participants reporting beliefs in studies | Mean % participants reporting beliefs in studies | Median% participants reporting beliefs in studies | No. (%) Study reports of beliefs | Range % participants reporting beliefs in studies | Mean % participants reporting beliefs in studies | Median % participants reporting beliefs in studies | |
| All | 46 (100.0) | 0.4–97.5 | 40.1 | 35.9 | 62 (100.0) | 0.6–76.7 | 22.2 | 17.5 |
| Africa | 6 (13.0) | 0.5–78.9 | 40.3 | 42.3 | 18 (29.0) | 2.0–76.7 | 32.0 | 29.0 |
| Asia | 25 (54.4) | 0.8–97.5 | 46.4 | 45.6 | 32 (51.6) | 0.6–67.0 | 19.8 | 15.0 |
| Europe | 8 (17.4) | 4.8–47.5 | 27.5 | 38.1 | 3 (4.8) | 4.4–26.5 | 15.4 | 15.4 |
| North America | 6 (13.0) | 0.4–50.0 | 25.6 | 30.0 | 5 (8.1) | 2.2–47.0 | 20.3 | 16.0 |
| Oceania | 0 | - | - | - | 3 (4.8) | 4.9 – 25.1 | 15.8 | 17.5 |
| Mixed (Asia, North America) | 1 (2.2) | 12.5–87.6 | 48.1 | 46.1 | 1 (1.6) | 0.9–10.2 | 4.3 | 3.2 |
Study reports of general negative beliefs (No.=62) related to donation posing a risk to health or causing ill health and/or donation-related health risks being a deterrent/ barrier to donation (e.g., “Donation is harmful to your health”). On average, 22.2% of participants in these study reports cited general negative beliefs (Table IV). Reports for general negative beliefs occurred in studies conducted most often in Asia (51.6%) and Africa (29.0%).
Beliefs specific
Specific positive beliefs (No.=45) that were reported in studies were coded into seven categories (see health consequences, Table II) and ranked in order of how frequently they were measured across studies: improving blood, health protective factors, physical appearance (weight loss, look younger), vitality (energy boost), headaches, immunity, and iron (decrease levels) (Table V). At least half of reports for the two most common beliefs originated in studies conducted in Asia only or Asia and South America.
Table V.
Study reports for specific positive beliefs overall and by continent (No.=45)
| Specific belief | Study reports of beliefs | Range % participants reporting beliefs in studies | Mean % participants reporting beliefs in studies | Median % participants reporting beliefs in studies | No. (%) Continent study reports occurred | ||
|---|---|---|---|---|---|---|---|
| Label | Qual No. | Quant No. | Total No. (%) | ||||
| Immunity | 1 | - | 1 (0.2) | - | - | - | 1 (100.0) North America |
| Vitality | 3 | 3 | 6 (13.3) | 3.2–4.0 | 3.7 | 4.0 | 1 (16.7) Asia 2 (33.3) Europe 3 (50.0) North America |
| Iron | - | 1 | 1 (0.2) | 1.2–1.2 | 1.2 | 1.2 | 1 (100.0) Asia |
| Health risk/protective factors | 3 | 7 | 10 (22.2) | 0.3–67.7 | 23.0 | 17.5 | 1 (10.0) Africa 5 (50.0) Asia 1 (10.0) Europe 1 (10.0) North America 1 (10.0) Oceania 1 (10.0) South America |
| Physical appearance | 3 | 6 | 9 (20.0) | 0.3–43.9 | 11.9 | 3.6 | 2 (22.2) Africa 5 (55.6) Asia 1 (11.1) Europe 1 (11.1) South America |
| Improving blood | 10 | 6 | 16 (35.6) | 1.2–74.9 | 23.9 | 7.7 | 2 (12.5) Africa 5 (31.3) Asia 3 (18.8) Europe 1 (6.2) North America 1 (6.2) Oceania 4 (25.0) South America |
| Headaches | - | 2 | 2 (0.4) | 1.0–31.5 | 16.3 | 16.3 | 1 (50.0) Asia 1 (50.0) Europe |
Reports of specific negative beliefs (No.=313) in studies were coded into 13 categories (Table II) and ranked in order of most frequent occurrence across studies: infectious disease, vitality (causes weakness), adverse events involving vasovagal reactions, iron, immunity, non-specific adverse events, reproductive health, adverse events involving other physical injury, physical appearance (weight gain), death, health risk factors (increase blood pressure), blood loss, and headaches (Table VI). Reports of these frequently occurring beliefs most commonly occurred in studies originating in Asia and Africa.
Table VI.
Study reports for specific negative beliefs overall and by continent (No.=313)
| Specific belief | Study reports of beliefs | Range % participants reporting beliefs in studies | Mean % participants reporting beliefs in studies | Median % participants reporting beliefs in studies | No. (%) Continent study reports occurred | ||
|---|---|---|---|---|---|---|---|
| Label | Qual No. | Quant No. | Total No. (%) | ||||
| Reproductive health | 2 | 12 | 14 (4.5) | 1.5–22.8 | 9.3 | 5.7 | 1 (7.1) Mixed 7 (50.0) Africa 6 (42.9) Asia |
| Immunity | 6 | 10 | 16 (5.1) | 3.1–50.0 | 13.8 | 8.7 | 7 (43.8) Africa 6 (37.5) Asia 1 (6.2) North America 2 (12.5) Oceania |
| Vitality | 5 | 33 | 38 (12.1) | 0.1–92.3 | 26.2 | 22.0 | 15 (39.5) Africa 17 (44.7) Asia 2 (5.3) Europe 4 (10.5) Oceania |
| Iron | 2 | 25 | 27 (8.6) | 4.2–83.9 | 27.3 | 19.2 | 7 (25.9) Africa 17 (63.0) Asia 1 (3.7) Europe 2 (7.4) North America |
| Blood loss | 4 | 3 | 7 (2.3) | 3.6–33.9 | 14.7 | 6.6 | 4 (57.1) Africa 2 (28.6) Europe 1 (14.3) Oceania |
| Infectious disease | 10 | 110 | 120 (38.3) | 0.2–93.6 | 30.9 | 25.5 | 27 (22.5) Africa 54 (45.0) Asia 11 (9.2) Europe 1 (0.8) Mixed 19 (15.8) North America 3 (2.5) Oceania 5 (4.2) South America |
| Health risk/protective factors | - | 7 | 7 (2.3) | 0.3–25.0 | 11.8 | 9.5 | 2 (28.6) Africa 3 (42.8) Asia 1 (14.3) Europe 1 (14.3) North America |
| Physical appearance | 2 | 8 | 10 (3.2) | 3.3–35.6 | 16.9 | 14.1 | 5 (50.0) Africa 5 (50.0) Asia |
| Headaches | - | 2 | 2 (0.6) | 2.6–11.5 | 7.1 | 7.1 | 2 (100.0) Africa |
| Death | - | 8 | 8 (2.6) | 2.1–32.2 | 9.4 | 8.0 | 6 (75.0) Africa 1 (12.5) Asia 1 (12.5) Oceania |
| Adverse events:non-specific | 3 | 12 | 15 (4.8) | 0.5–87.0 | 24.9 | 16.2 | 5 (33.3) Africa 4 (26.7) Asia 2 (13.3) Europe 2 (13.3) North America 1 (6.7) Oceania 1 (6.7) South America |
| Adverse events: vasovagal reactions | 4 | 34 | 38 (12.1) | 0.2–66.0 | 23.3 | 21.8 | 12 (31.6) Africa 14 (36.8) Asia 7 (18.4) Europe 2 (5.3) North America 2 (5.3) Oceania 1 (2.6) South America |
| Adverse events:other physical | 2 | 9 | 11 (3.5) | 1.5–24.0 | 14.9 | 16.4 | 5 (45.5) Africa 3 (27.3) Asia 2 (18.2) Europe 1 (9.0) Oceania |
Five reports of specific beliefs about weight loss or gain after whole-blood donation could not be categorized as positive or negative.
Experiences general
Two reports of general positive experiences (e.g., “I feel physically better after donating today”) and five reports of general negative experiences (e.g., “Persistent ongoing symptoms”) were included in studies (Table III). On average, general positive and negative experiences were mentioned by 30.8% and 19.7% of participants, respectively. Study reports of general positive experiences had health as a background focus and originated in Europe. Sixty percent of reports of general negative experiences had health as a central focus and originated in Europe.
Experiences specific
Studies included four reports of specific positive experiences and, of these reports, 3 were from qualitative studies that described improving blood as a result of donating, and specifically replenishment of blood leading to feelings of increased health. These reports were from studies originating in either South America or Asia (Table VII).
Table VII.
Study reports for specific positive experiences (No.=4) and specific negative experiences (No.=91)
| Specific experience | Study reports of experiences | Range % participants reporting experiences in studies | Mean % participants reporting experiences in studies | Median % participants reporting experiences in studies | No. (%) Continent study reports occurred | ||
|---|---|---|---|---|---|---|---|
| Label | Qual No. | Quant No. | Total No. (%) | ||||
| Positive experiences | |||||||
| Vitality | - | 1 | 1 (25.0) | 11.9 | 11.9 | - | 1 (100.0) Europe |
| Improving blood | 3 | - | 3 (75.0) | - | - | - | 1 (33.0) Asia 2 (67.0) South America |
| Negative experiences | |||||||
| Immunity | 1 | 2 | 3 (3.3) | 0.8–2.9 | 1.9 | 1.9% | 1 (33.0) Africa 2 (67.0) Asia |
| Vitality | 0 | 16 | 16 (17.6) | 0.9–52.6 | 12.2% | 7.7% | 1 (6.3) Africa 6 (37.5) Asia 4 (25.0) Europe 3 (18.8) North America 2 (12.5) Oceania |
| Iron | 1 | 1 | 2 (2.2) | 56.0 | 56.0 | 56.0 | 2 (100.0) Asia |
| Infectious disease | 0 | 1 | 1 (1.0) | 1.1 | 1.1 | 1.1 | 1 (100.0) Europe |
| Headaches | 0 | 2 | 2 (2.2) | 0.4–1.0 | 0.7 | 0.7 | 2 (100.0) Europe |
| Adverse events: non-specific | 0 | 21 | 21 (23.1) | 0.1–51.8 | 18.8 | 13.0 | 7 (33.3) Asia 5 (23.8) Europe 6 (28.6) North America 3 (14.3) Oceania |
| Adverse events: vasovagal reactions | 2 | 27 | 29 (31.9) | 0.0–32.1 | 9.6 | 7.2 | 1 (3.4) Africa 9 (31.0) Asia 9 (31.0) Europe 7 (24.1) North America 3 (10.3) Oceania |
| Adverse events: other physical | 1 | 16 | 17 (18.7) | 0.0–70.5 | 13.2 | 4.8 | 9 (52.9) Asia 2 (11.8) Europe 5 (29.4) North America 1 (5.9) Oceania |
Study reports of specific negative experiences (No.=91) were coded into eight categories (Table II). Study reports of negative experiences were ranked in order of most frequent occurrence across studies: adverse events vasovagal reactions, adverse events non-specific (feeling unwell), adverse events other physical (bruising), vitality (tiredness), immunity, iron, headaches, and infectious disease (Table VII). These frequently occurring experiences most often originated in study reports from Asia, Europe, and North America.
DISCUSSION
The aim of this review was to systematically integrate the literature on the perceived health effects of blood donation. Specifically, we identified donors’ and non-donors’ perceptions operationalized as personal experiences and broader beliefs of the short and longer-term physiological health effects of blood donation. We also sought to examine the extent to which health effects of whole-blood and/or blood product donation have been investigated and differences in health perceptions of blood donation in different parts of the world.
While a large number of studies assessed donation-related health perceptions, in the vast majority these perceptions were the background focus and only assessed in relation to whole-blood. Health was more often a central focus in results reporting experiences, possibly because these studies considered events occurring after donation. Further, health was almost exclusively a background focus when beliefs were considered.
These results could be interpreted as indicating that people do not generally have donation-related health perceptions, and this justifies the lack of focus within research. Alternatively, people may have a wide array of negative and positive donation-related health perceptions that have not yet been comprehensively mapped. The lack of focus on how donors perceive donating whole-blood, plasma, and platelets to impact their health means that the breadth, valence and level of endorsement of perceptions of health still remain largely unknown. Diversifying our focus away from whole-blood is particularly important given the worldwide expansion in plasma collection sites29. We know little of the short and long-term effects of donating plasma or on lay understandings of how plasma donation impacts health, and this work is needed to inform approaches to donor communications.
Accepting the limitations of existing research, clear asymmetries were observed. Specifically, most studies focused on beliefs rather than experiences, and on specific negative beliefs, rather than positive. In part this focus and frequent endorsement is explained by known risks of blood donation of vasovagal reactions, iron loss and other adverse events. Donors are routinely educated about these risks and are often encouraged to engage in behaviours during or after donating to mitigate risk and improve donor retention30. Negative impacts on vitality are another common-sense outcome of blood donation, likely related to understandings about physiological impacts of losing iron and blood volume25. However, and perhaps surprisingly, the most frequently endorsed specific negative belief around blood donation was in relation to infectious diseases. The belief that blood donation carries a risk of acquiring transfusion transmitted infections (TTIs) such as HIV has been documented in some settings22,31, and is a known deterrent to donation in these settings and by migrant groups. As this belief relates to trust in the system of blood collection, this finding suggests that it remains particularly important to research and address this with those who have connections to countries where such beliefs are more common22,31,32 and who may lack knowledge on or trust in the procedures to mitigate these risks in other countries33. Other specific negative beliefs identified, such as those relating to negative impacts on physical appearance and reproductive health appear context-specific, with most studies asking about these and reporting findings originating in Asian or African countries. This finding draws attention to the likelihood that ethnic minority groups living in Western countries will hold divergent understandings of the impacts of donation on their health. As BCAs in countries with growing migrant groups aim to improve representation of these groups in blood donor panels more research is needed to understand if, and how, beliefs about health impact willingness to donate blood in these groups.
Results for specific negative experiences most frequently mirrored beliefs, with a focus on vasovagal reactions, non-specific adverse events, and vitality. These were mostly reported in studies with blood donors. However, only one study reported infectious disease as an experience while this was commonly cited as a belief. Negative impacts on immunity and iron levels, and headaches were also mentioned by small numbers of participants. That frequent experiences differed from frequent beliefs is likely explained by studies reporting experiences drawing upon actual rather than anticipated donation.
Consistent with the risk mitigation focus of donor research, specific positive beliefs were only considered in 46 studies and specific positive experiences in four studies. The most frequently mentioned positive beliefs related to improving blood, health protective factors, such as lowering blood pressure, and physical appearance, such as weight loss. The belief that donating blood improves blood quality through removing excess or unclean blood and stimulating production of new blood has its origins in therapeutic bloodletting33. Beliefs relating to improving blood and health protective factors were more commonly mentioned in studies from Asia and South America, however few specific positive beliefs were endorsed by ≥20.0% of participants and it remains unclear how widespread these beliefs are. Notably, few studies included specific positive experiences, although most of those that did documented experiences related to improving blood through donation. The existence of positive perceptions that have no basis in fact are challenging for BCAs as they cannot be used to promote blood donation, yet addressing them may deter those motivated by these beliefs. One approach may be to conduct research to improve understanding of positive beliefs (e.g., improving blood) and how they relate to evidence (e.g., changes to iron metabolism and erythropoiesis that take place after donating blood).
CONCLUSIONS
While highlighting some key health perceptions that people have in relation to blood donation, overall, this review reinforces that lay perspectives on the health impacts of blood donation have not been comprehensively researched. Focusing only on physiological impacts due to the inconsistent quality of data on psychological impact, our analysis shows conclusively that health impacts have been treated as peripheral in research to date. Within analyses that have considered these perceived impacts there has been an asymmetrical focus on whole-blood and negative rather than positive impacts. For this reason, and despite inclusion of data from 247 studies in the review, it remains difficult to know how important health beliefs and experience are for donors and non-donors, and to what extent these experiences and beliefs impact critical decisions in the donation process. The discrepancy between reported beliefs and experiences provides an avenue for future research, for example to understand whether certain beliefs are more likely to be held by people who have not donated blood, and whether engaging in blood donation changes the types of beliefs reported. Research should also focus on understanding the cultural context of health beliefs, such as through a multi-continent study, and on developing standardized definitions for measuring psychological impacts of donation. Making donation-related health beliefs and experiences a central research focus, and comprehensively mapping how these relate to differences in donor characteristics and behaviour, geographical region, and products donated has potential to provide insights critical to appropriate education to ensure the ongoing sufficiency of the blood supply. Further, we believe that better understanding health beliefs and experiences, and how these shape blood donation behaviour in different settings, can make a valuable contribution to conceptualisations of blood donation as a reciprocal arrangement that considers benefits and risks to the donor as well as the recipient35. Such knowledge is particularly important given the salience of health to activities that BCAs are increasingly inviting donors to participate in, such as biobanks and other health-related research36. Having this knowledge could help inform the kind of health information donors value and would like to receive from BCAs, as well as health-related communication and education strategies.
Supplementary Information
Footnotes
AUTHORS’ CONTRIBUTIONS: RT, BM, TED: substantial contributions to the conception or design of the review; SPC, MKH, SPK: substantial contribution to the acquisition and analysis of data; RT, BM, MKH: interpretation of data for the review; RT, BM, SPC, MKH, SPK, TED: drafting the manuscript; MKH: revising the manuscript; RT, BM, SPC, MKH, SPK, TED: final approval of the manuscript.
The Authors declare no conflicts of interest.
Commented by doi 10.2450/BloodTransfus.625
FUNDING: Australian governments fund Australian Red Cross Lifeblood for the provision of blood, blood products, and services to the Australian community.
REFERENCES
- 1.Jones JM, Sapiano MRP, Mowla S, Bota D, Berger JJ, Basavaraju SV. Has the trend of declining blood transfusions in the United States ended? Findings of the 2019 National Blood Collection and Utilization Survey. Transfusion. 2021;61(Suppl 2):S1–S10. doi: 10.1111/trf.16449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sayers M. Donor motivation and psychosocial research. Transfusion. 2022;62:1912–1916. doi: 10.1111/trf.17024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.France CR, Ditto B, France JL, Himawan LK. Psychometric properties of the Blood Donation Reactions Inventory: a subjective measure of presyncopal reactions to blood donation. Transfusion. 2008;48:1820–1826. doi: 10.1111/j.1537-2995.2008.01831.x. [DOI] [PubMed] [Google Scholar]
- 4.Chueca M, Bouvet G, Duron-Martinaud S, Doyen M, Poirrier L, Martinaud C. Iron-deficiency among blood donors: Donors’ opinion on iron supplementation strategy. Transfusion Clinique et Biologique. 2020;27:218–221. doi: 10.1016/j.tracli.2020.08.004. [DOI] [PubMed] [Google Scholar]
- 5.Kiss JE, Vassallo RR. 2018 How do we manage iron deficiency after blood donation? Br J Haematol. 2018;181:590–603. doi: 10.1111/bjh.15136. [DOI] [PubMed] [Google Scholar]
- 6.France JL, France CR, Rebosa M, Shaz BH, Kessler DA. Promoting awareness of donation-related iron depletion among high risk blood donors. Transfusion. 2021;61:3353–3360. doi: 10.1111/trf.16694. [DOI] [PubMed] [Google Scholar]
- 7.Charbonneau J, Cloutier M-S, Carrier E. Why do blood donors lapse or reduce their donation’s frequency? Transfus Med Rev. 2016;30:1–5. doi: 10.1016/j.tmrv.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 8.Davey RJ. The blood centre as a community health resource. Vox Sang. 2006;91:206–213. doi: 10.1111/j.1423-0410.2006.00824.x. [DOI] [PubMed] [Google Scholar]
- 9.O’Brien SF, Drews SJ, Lewin A, Russell A, Davison K, Goldman M, et al. How do we decide how representative our donors are for public health surveillance. Transfusion. 2022;62:2431–2437. doi: 10.1111/trf.17140. [DOI] [PubMed] [Google Scholar]
- 10.Rigas AS, Skytthe A, Erikstrup C, Rostgaard K, Petersen MS, Hjalgrim H, et al. The healthy donor effect impacts self-reported physical andmental health-results from the Danish Blood Donor Study (DBDS) Transfus Med. 2019;29(Suppl 1):65–69. doi: 10.1111/tme.12478. [DOI] [PubMed] [Google Scholar]
- 11.Pedersen OB, Erikstrup C, Kotzé SR, Sorensen E, Petersen MS, Grau K, et al. The Danish blood donor study: a large, prospective cohort and biobank for medical research. Vox Sang. 2012;102:271. doi: 10.1111/j.1423-0410.2011.01553.x. [DOI] [PubMed] [Google Scholar]
- 12.Karki S, Gemelli CN, Davison TE, Masser BM, Marks DC, Bell K, et al. Willingness of blood donors in Australia to provide additional data and blood sample for health research. Transfusion. 2021;61:2855–2861. doi: 10.1111/trf.16629. [DOI] [PubMed] [Google Scholar]
- 13.Leipnitz S, de Vries M, Clement M, Mazar N. Providing health checks as incentives to retain blood donors - Evidence from two field experiments. IJRM. 2018;35:628–640. doi: 10.1016/j.ijresmar.2018.08.004. [DOI] [Google Scholar]
- 14.Bagot KL, Bove LL, Masser BM, Bednall TC, Buzza M. Perceived deterrents to being a plasmapheresis donor in a voluntary, nonremunerated environment. Transfusion. 2013;53:1108–1119. doi: 10.1111/j.1537-2995.2012.03891.x. [DOI] [PubMed] [Google Scholar]
- 15.Bagot KL, Masser BM, Starfelt LC, White KM. Building a flexible, voluntary donation panel: an exploration of donor willingness. Transfusion. 2016;56:186–194. doi: 10.1111/trf.13278. [DOI] [PubMed] [Google Scholar]
- 16.Bove LL, Bednall T, Masser B, Buzza M. Understanding the plasmapheresis donor in a voluntary, nonremunerated environment. Transfusion. 2011;51:2411–2424. doi: 10.1111/j.1537-2995.2011.03168.x. [DOI] [PubMed] [Google Scholar]
- 17.Glynn SA, Kleinman SH, Schreiber GB, et al. Motivations to donate blood: demographic comparisons. Transfusion. 2002;42:216–225. doi: 10.1046/j.1537-2995.2002.00008.x. [DOI] [PubMed] [Google Scholar]
- 18.Hinrichs A, Picker SM, Schneider A, Lefering R, Neugebauer EAM, Gathof BS. Effect of blood donation on well-being of blood donors. Transfus Med. 2008;18:40–48. doi: 10.1111/j.1365-3148.2007.00805.x. [DOI] [PubMed] [Google Scholar]
- 19.Nguyen DD, DeVita DA, Hirschler NV, Murphy EL. Blood donor satisfaction and intention of future donation. Transfusion. 2008;48:742–748. doi: 10.1111/j.1537-2995.2007.01600.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nilsson Sojka B, Sojka P. The blood-donation experience: perceived physical, psychological and social impact of blood donation on the donor. Vox Sang. 2003;84:120–128. doi: 10.1046/j.1423-0410.2003.00271.x. [DOI] [PubMed] [Google Scholar]
- 21.Sojka BN, Sojka P. The blood donation experience: self-reported motives and obstacles for donating blood. Vox Sang. 2008;94:56–63. doi: 10.1111/j.1423-0410.2007.00990.x. [DOI] [PubMed] [Google Scholar]
- 22.Grassineau D, Papa K, Ducourneau A, Duboz P, Boetsch G, Chiaroni J. Improving minority blood donation: anthropologic approach in a migrant community. Transfusion. 2007;47:402–409. doi: 10.1111/j.1537-2995.2007.01130.x. [DOI] [PubMed] [Google Scholar]
- 23.Gahan L, Masser B, Mwangi C, Thorpe R, Davison T. Motivators, facilitators, and barriers to blood donation in Australia by people from ethnic minority groups: perspectives of sub-Saharan African, East/ South-East Asian, and Melanesian/Polynesian blood donors. Journal of Sociology. 2022;58:95–112. doi: 10.1177/1440783321999462. [DOI] [Google Scholar]
- 24.Moore C, Sambrook J, Walker M, Tolkien Z, Kaptoge S, Allen D, et al. The INTERVAL trial to determine whether intervals between blood donations can be safely and acceptably decreased to optimise blood supply: study protocol for a randomised controlled trial. Trials. 2014;15:363. doi: 10.1186/1745-6215-15-363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lynch R, Cohn S. Donor understandings of blood and the body in relation to more frequent donation. Vox Sang. 2018;113:350–356. doi: 10.1111/vox.12641. [DOI] [PubMed] [Google Scholar]
- 26.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. PLOS Medicine. 2021;18:e1003583. doi: 10.1371/journal.pmed.1003583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implementation Sci. 2010;5:69. doi: 10.1186/1748-5908-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pham MT, Rajić A, Greig JD, Sargeant JM, Papadopoulos A, McEwen SA. A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Res Synth Methods. 2014;5:371–385. doi: 10.1002/jrsm.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Holloway K. Understanding the experiences of plasma donors in Canada›s new source plasma collection centres during COVID-19: a qualitative study. Vox Sang. 2022;117:1078–1084. doi: 10.1111/vox.13301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thijsen A, Thorpe R, Davison TE, Nguyen L, Masser B. The vasovagal reaction experience among blood donors: A qualitative study of factors that affect donor return. Soc Sci Med. 2021;282:114142. doi: 10.1016/j.socscimed.2021.114142. [DOI] [PubMed] [Google Scholar]
- 31.Olaiya MA, Alakija W, Ajala A, Olatunji RO. Knowledge, attitudes, beliefs and motivations towards blood donations among blood donors in Lagos, Nigeria. Transfus Med. 2004;14:13–7. doi: 10.1111/j.0958-7578.2004.00474.x. [DOI] [PubMed] [Google Scholar]
- 32.Hu H, Wang T, Fu Q. Psychological factors related to donation behaviour among Chinese adults: results from a longitudinal investigation. Transfus Med. 2017;27:335–341. doi: 10.1111/tme.12422. [DOI] [PubMed] [Google Scholar]
- 33.Polonsky MJ, Renzaho AMN, Brijnath B. Barriers to blood donation in African communities in Australia: the role of home and host country culture and experience. Transfusion. 2011;51:1809–1819. doi: 10.1111/j.1537-2995.2010.03053.x. [DOI] [PubMed] [Google Scholar]
- 34.Sanabria E. Alleviative bleeding: bloodletting, menstruation and the politics of ignorance in a Brazilian Blood Donation Centre. Body & Society. 2009;15:123–144. doi: 10.1177/1357034X09104112. [DOI] [Google Scholar]
- 35.Busby HW. Trust, nostalgia and narrative accounts of blood banking in England in the 21st century. Health. 2010;14:369–382. doi: 10.1177/1363459309359717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rigas AS, Pedersen OB, Burgdorf KS, Bruun MT, Sørensen E, Erikstrup C, et al. Tools and challenges in creating a biobank in a modern blood bank: experience from the Danish Blood Donor Study (DBDS) ISBT Sci Series. 2016;11(Suppl 1):182–187. doi: 10.1111/voxs.12231. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.