Abstract
Morphologically atypical Fusarium verticillioides causing a nasal abscess in a severely immunosuppressed child was successfully treated with repeated surgical intervention and liposomal amphotericin B, despite amphotericin B resistance in vitro. Definitive identification was achieved by sequencing the translation elongation factor α gene after ribosomal sequencing proved inadequate.
CASE REPORT
A 9-year-old boy diagnosed with chronic myelogenous leukemia in September 2001 had been treated with imatinib (STI 571) for 9 months and achieved hematologic and cytogenetic remission. After allogeneic bone marrow transplantation in June 2002, he developed severe chronic graft-versus-host disease (GvHD) involving the skin, the liver, and the gastrointestinal tract. GvHD was accompanied by dryness of the eyes, nose, and mouth, which frequently made the patient feel compelled to pick his nose despite moistening measures. Under immunosuppression with cyclosporine, mycophenolate mofetil, prednisolone, and budesonide, the patient required repeated courses of antiviral treatment for the reactivation of cytomegalovirus (CMV), human herpesvirus 6, and Epstein-Barr virus, revealed by PCR in his blood. He experienced several febrile episodes, most of which responded to broad-spectrum antibacterial agents, except for one episode which required the addition of antifungal treatment with liposomal amphotericin B (LAMB). While receiving antimicrobial prophylaxis with oral penicillin V (for functional hyposplenia) and intravenous caspofungin, the patient became febrile again on day 579 after bone marrow transplant and exhibited a slight increase of C-reactive protein (CRP) and leukocytosis (18,600/μl) with a marked left shift. An intranasal tumor protruding through both nostrils was observed. Ear, nose, and throat evaluation revealed a fluctuant mass on both sides of the cartilaginous nasal septum, with partial destruction of the cartilage shown by computed tomography (CT) imaging (Fig. 1). Hemorrhagic and purulent fluid was aspirated, and antibiotic treatment with piperacillin and tazobactam was started. A cytologic examination revealed no signs of malignancy nor the presence of microorganisms. The patient remained febrile, and CRP increased to a maximum of 58 mg/liter. When the microbiology lab reported the growth of a fungal species 2 days after abscess drainage, caspofungin was replaced by LAMB at a dose of 6 mg kg of body weight−1 day−1. Culture on Sabouraud glucose agar and microscopy revealed features suggestive of Fusarium spp. In the following days, the patient, still under immunosuppressive treatment with cyclosporine, mycophenolate mofetil, and corticosteroids, markedly improved, with defervescence as well as normalization of CRP and granulocyte counts. One week after the operation, his nasal respiration gradually deteriorated again, and bilateral swelling at the anterior nasal septum required another drainage 13 days after the first surgical intervention. Debridement of the fungal focus was not performed in order to avoid disfigurement and functional impairment. From the drainage fluid, the same fungus was cultured again, while bacterial cultures remained sterile.
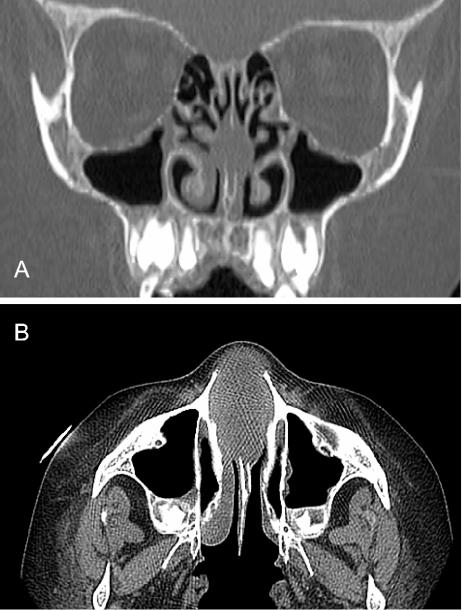
FIG. 1.
Cranial CT scan showing mucosal abscess formation with partial destruction of the cartilaginous nasal septum and complete obstruction of the anterior nasal cavity. (A) Frontal view; (B) horizontal view.
Since clinical improvement occurred in our patient after the second abscess drainage, antifungal treatment with high-dose LAMB (6 mg kg−1 day−1) was continued for 32 days (22 days beyond the surgical cure) and was supplemented by local instillation of povidone iodine in a 1:8 dilution via an intranasal cotton tampon until its removal 1 week after the operation. We avoided voriconazole use out of concern about additional hepatotoxicity and possible effects of drug interactions with cyclosporine.
No further reactivation of Fusarium infection was observed, despite continuing signs (and treatment) of chronic GvHD. Follow-up nasal swabs revealed a normal flora without fungal growth. Nine days after its cessation, LAMB and broad-spectrum antibiotics were restarted due to respiratory symptoms, the recurrence of fever, an increase in CRP to 142 mg/liter, repeatedly positive Aspergillus galactomannan antigen tests, several subpleurally located nodular lesions revealed by CT, and transient neutropenia that had started 2 weeks earlier. Sadly, after 3 more weeks, the patient died from interstitial pneumonia. An autopsy confirmed CMV as the cause of pneumonia with additional granulomatous pleural lesions growing Aspergillus fumigatus but not Fusarium. The nasal septum was macroscopically unremarkable; a histologic examination was not performed.
Mycological studies and diagnosis.
Material from the nasal lesions was inoculated repeatedly on Sabouraud glucose agar containing gentamicin and chloramphenicol (bioMérieux, Marcy l'Etoile, France) and on a chromogenic medium for the identification of Candida species (Can2 agar; bioMérieux).
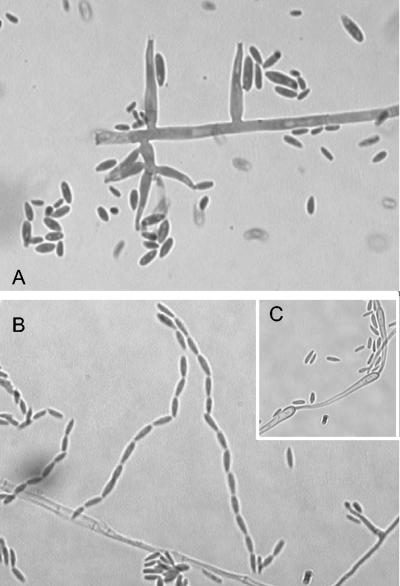
After 48 h of incubation at both 30 and 37°C, numerous colonies were observed. They became ochraceous to pinkish with abundant white aerial mycelia and brownish-to-orange reverse coloration. Microscopy of subcultured isolates showed hyaline septate hyphae with sessile, entirely monophialidic conidiophores (Fig. 2A) producing microconidia in long chains (Fig. 2B). Microconidia were 6 to 10 μm long by 2.5 to 3.5 μm wide and were mostly aseptate or, rarely, had one or two septa; in shape, they were clavate, cylindrical, or slightly curved with a tapered, truncate base. Neither macroconidia nor chlamydospores were observed on the above-mentioned media or on potato dextrose and synthetic nutrient-poor agar, media used for Fusarium identification (12). These criteria suggested Fusarium verticillioides (Sacc.) Nirenberg. Nevertheless, it was not possible to rule out the similar opportunistic pathogen Fusarium napiforme based on morphology alone. F. napiforme is stated to produce a proportion of distinctive pyriform microconidia (13), but these may be uncommon, induced only under special conditions, or even not seen in some isolates (see Fig. 80 in a work by Summerbell [23]). F. napiforme also differs by producing chlamydospores, but these are scarce, and F. verticillioides may produce similar structures, referred to as inflated cells with thickened walls (8) that differ from true chlamydospores only by being emptier in appearance. Even more confusing was the fact that the strain produced abundant racquet hyphae (Fig. 2C), structures observed elsewhere in the genus Fusarium but not mentioned in descriptions of F. verticillioides (4, 6, 8).
FIG. 2.
Microphotographs of the F. verticillioides case isolate. (A) Hyaline septate hyphae with sessile monophialidic conidiophores; (B) microconidia in long chains; (C) racquet hyphae.
Shortly after the isolation of the fungus, when its morphological identification was still at a preliminary phase, we performed a PCR of the ribosomal internal transcribed spacers (ITS) with the fungus-specific primers ITS1f and ITS5 (3). The amplicon was sequenced using the ABI PRISM BigDye Terminator cycle sequencing kit (Applied Biosystems, Foster City, Calif.). This procedure is sufficient to identify an increasing number of medically important fungi (18), provided compatible morphology is ascertained in a control study.
Comparison of the sequence obtained with reference sequences in GenBank resulted in near matches with several members of the Fusarium subgenus Liseola, including Fusarium sacchari (in GenBank under the corresponding teleomorph name Gibberella sacchari), F. napiforme, Fusarium subglutinans, F. verticillioides, and Fusarium fujikuroi (Gibberella fujikuroi). Species identity could not be confirmed. ITS analysis is considered unreliable for the identification of strains in the Fusarium subgenus Liseola, partly because its resolution level is low (4, 16) and partly because all strains in this group contain two paralogous, discrepant ITS sequence types, a potential source of confusion (15). Therefore, we employed primers EF-1 and EF-2 for translation elongation factor α (EF) amplification and sequencing as recommended by O'Donnell et al. (16). Sequencing of EF yielded a distinctive homology of 99.8% (one nucleotide difference among 540 nucleotides) to GenBank sequences of Gibberella moniliformis, which is F. verticillioides by its teleomorph name. F. napiforme and other Fusarium species could be omitted because they had similarities of ≤95%.
Antifungal susceptibility testing.
Susceptibility of the case strain to amphotericin B (AMB), voriconazole (VRC), fluconazole (FLC), itraconazole (ITC), and 5-flucytosine was tested using the Etest (AB Biodisk, Solna, Sweden). Broth microdilution antifungal tests for AMB, ITC, and VRC were also carried out (11).
Etest results showed that the strain was resistant to 5-flucytosine and FLC (Table 1). The universal resistance of Fusarium species to these drugs is abundantly documented (19); therefore, microdilution tests for these substances were not carried out. The results for ITC and VRC correlated with the MICs obtained with the microdilution method, as shown in Table 1. In contrast, great discrepancies between results from the two methods were found for AMB, as Etest MICs were 10-fold higher than those obtained with microdilution. Similar data were found by Espinel-Ingroff for Fusarium solani (7). However, no breakpoints have been established for F. verticillioides.
TABLE 1.
Antifungal susceptibilities of the F. verticillioides case isolate
| Drug | MIC (μg/ml) as determined by:
|
|
|---|---|---|
| Etest | Microdilution testa | |
| Amphotericin B | 24 | 2.5 |
| 5-Flucytosine | >32 | ND |
| Fluconazole | >256 | ND |
| Voriconazole | 0.25 | 1.0 |
| Itraconazole | 1.0 | 2.0 |
Microdilution tests were performed according to the NCCLS M38-A standard. ND, not determined.
Conclusions.
Although F. verticillioides elements were not seen in direct specimen microscopy in this case, the fungus was extensively isolated on two occasions from otherwise sterile abscess drainage specimens. Fluids from filamentous fungal abscesses often lack microscopically recognizable fungal elements, and tissue biopsy samples must be taken to demonstrate these elements (23). In the present case, to avoid possible complications, biopsy was not done, but the repeated heavy outgrowth, the complete lack of mucosal surface contaminants in culture, and the antifungal drug response resulting in clinical cure of the abscess all signal that the isolated fungus was causal.
Antifungal prophylaxis with caspofungin was used in our patient in order to take advantage of its low toxicity combined with broadened coverage relative to that of FLC. However, this case report provides clinical evidence that echinocandins cannot prevent infection with in vitro-resistant filamentous fungi, such as Fusarium spp.
Fusarium species are common plant pathogens or saprobes on decaying plant material (6). In immunocompetent patients, Fusarium species cause local infection; posttraumatic keratitis is the most common infection type seen (2, 23, 24). In contrast, immunocompromised and particularly hematological patients suffer severe infections, presenting with refractory fever in more than 90% of cases, with typical ecthyma-like skin lesions or sino-pulmonary infections occurring in approximately 75%. Fusarium infection is the second-most-common mold infection in immunosuppressed patients and results in mortality rates ranging from 50 to 80% (5, 20). F. verticillioides is relatively commonly involved in such cases (9). It differs epidemiologically from the more common F. solani and Fusarium oxysporum in forming microconidia not in wet, mucoid masses but instead in dry chains. The formation of conidia in dry chains is a feature ecologically connected to airborne dispersal (22). This species may thus be relatively likely to infect immunocompromised patients via the airways (17). This likelihood may have been a factor in the nasal site of our patient's infection. Fusarium species with mucoid conidia pose a significant indoor air hazard to immunocompromised patients only when water from contaminated plumbing systems is forcibly aerosolized, e.g., via shower facilities (1).
As pointed out by Guarro et al. (9), Fusarium spp. can exhibit considerable interspecies variability in pathogenicity. F. verticillioides is among the more aggressive species and frequently disseminates (9). Our patient carried several risk factors for disseminated Fusarium infection, including immunosuppression, tissue damage, and receipt of a graft from an unrelated donor. Absence of neutropenia, tapering of immunosuppressive therapy, and reduction of fungal load by local treatment with povidone iodine may have prevented dissemination and even made healing possible. In contrast, the patient's immune function did not suffice to overcome CMV reactivation or to prevent pulmonary growth of A. fumigatus, a fungus generally considered more virulent than any Fusarium sp. (22).
To date, few cases of nasal fusarial involvement in immunocompromised patients have been published (10, 21), although infection via the sinuses is not uncommon (5, 14). In one nasal case (10), F. solani was involved and disseminated. Notably, however, a limited F. chlamydosporum infection of a nasal turbinate in a neutropenic U.S. patient was cured with debridement and LAMB (21). F. chlamydosporum is a relatively weak pathogen not known to cause disseminated infection (23). In general, however, such nasal Fusarium infections may be controllable except in the most severely neutropenic patients affected with relatively virulent Fusarium species. The unusual accessibility of the involved tissue for surgical intervention or topical therapy may be a contributing factor in this controllability.
The ability to identify many pathogenic fungi rapidly and cheaply by means of ITS sequencing (18) has led to increasingly common adoption of this technique. With Fusarium pathogens of the subgenus Liseola, this procedure may not be adequate, and molecular diagnostic laboratories working with invasive fungal diseases should consider having the relevant EF primers available.
Nucleotide sequence accession numbers.
The strain was deposited at the Centraalbureau voor Schimmelcultures in Utrecht, The Netherlands, as CBS 114579. The ITS and EF sequences were submitted to GenBank under accession numbers AY533376 and AY611386, respectively.
REFERENCES
- 1.Anaissie, E. J., R. T. Kuchar, J. H. Rex, A. Francesconi, M. Kasai, F. M. Muller, M. Lozano-Chiu, R. C. Summerbell, M. C. Dignani, S. J. Chanock, and T. J. Walsh. 2001. Fusariosis associated with pathogenic Fusarium species colonization of a hospital water system: a new paradigm for the epidemiology of opportunistic mold infections. Clin. Infect. Dis. 33:1871-1878. [DOI] [PubMed] [Google Scholar]
- 2.Boutati, E. I., and F. J. Anaissie. 1997. Fusarium, a significant emerging pathogen in patients with hematologic malignancy: ten years' experience at a cancer center and implications for management. Blood 90:999-1008. [PubMed] [Google Scholar]
- 3.Buzina, W., H. Braun, K. Freudenschuss, A. Lackner, W. Habermann, and H. Stammberger. 2003. Fungal biodiversity—as found in nasal mucus. Med. Mycol. 41:149-161. [DOI] [PubMed] [Google Scholar]
- 4.De Hoog, G. S., J. Guarro, J. Gené, and M. J. Figueras. 2000. Atlas of clinical fungi, 2nd ed. Centraalbureau voor Schimmelcultures, Utrecht, The Netherlands.
- 5.Dignani, M. C., and E. Anaissie. 2004. Human fusariosis. Clin. Microbiol. Infect. 10(Suppl. 1):67-75. [DOI] [PubMed] [Google Scholar]
- 6.Domsch, K.-H., W. Gams, and T.-H. Anderson. 1993. Compendium of soil fungi. IHW Verlag, Eching, Germany.
- 7.Espinel-Ingroff, A. 2001. In vitro fungicidal activities of voriconazole, itraconazole, and amphotericin B against opportunistic moniliaceous and dematiaceous fungi. J. Clin. Microbiol. 39:954-958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gerlach, W., and H. Nirenberg. 1982. The genus Fusarium—a pictorial atlas. Mitt. Biol. Bundesanst. Land- Forstwirtsch. 209:1-406. [Google Scholar]
- 9.Guarro, J., M. Nucci, T. Akiti, J. Gené, M. D. G. C. Barreiro, and R. T. Gonçalves. 2000. Fungemia due to Fusarium sacchari in an immunosuppressed patient. J. Clin. Microbiol. 38:419-421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lopes, J. O., E. S. de Mello, and C. Klock. 1995. Mixed intranasal infection caused by Fusarium solani and a zygomycete in a leukaemic patient. Mycoses 38:281-284. [DOI] [PubMed] [Google Scholar]
- 11.National Committee for Clinical Laboratory Standards. 2002. Reference method for broth dilution antifungal susceptibility testing of filamentous fungi. Approved standard M38-A. National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 12.Nirenberg, H. I. 1976. Untersuchungen über die morphologische und biologische Differenzierung in der Fusarium-Sektion Liseola. Mitt. Biol. Bundesanst. Land- Forstwirtsch. 119:1-117. [Google Scholar]
- 13.Nirenberg, H. I., and K. O'Donnell. 1998. New Fusarium species and combinations within the Gibberella fujikuroi species complex. Mycologia 90:434-458. [Google Scholar]
- 14.Nucci, M., K. A. Marr, F. Queiroz-Telles, C. A. Martins, P. Trabasso, S. Costa, J. C. Voltarelli, A. L. Colombo, A. Imhof, R. Pasquini, A. Maiolino, C. A. Souza, and E. Anaissie. 2004. Fusarium infection in hematopoietic stem cell transplant recipients. Clin. Infect. Dis. 38:1237-1242. [DOI] [PubMed] [Google Scholar]
- 15.O'Donnell, K., and E. Cigelnik. 1997. Two divergent intragenomic rDNA ITS2 types within a monophyletic lineage of the fungus Fusarium are nonorthologous. Mol. Phylogenet. Evol. 7:103-116. [DOI] [PubMed] [Google Scholar]
- 16.O'Donnell, K., E. Cigelnik, and H. I. Nirenberg. 1998. Molecular systematics and phylogeography of the Gibberella fujikuroi species complex. Mycologia 90:465-493. [Google Scholar]
- 17.Okada, H., S. Hamatani, M. Kondo, T. Imai, S. Itoh, K. Isobe, and S. Onishi. 2000. Successful treatment of disseminated Fusarium infection in an infant with leukemia. Int. J. Hematol. 72:494-498. [PubMed] [Google Scholar]
- 18.Pryce, T. M., S. Palladino, I. D. Kay, and G. W. Coombs. 2003. Rapid identification of fungi by sequencing the ITS1 and ITS2 regions using an automated capillary electrophoresis system. Med. Mycol. 41:369-381. [DOI] [PubMed] [Google Scholar]
- 19.Pujol, I., J. Guarro, J. Gene, and J. Sala. 1997. In-vitro antifungal susceptibility of clinical and environmental Fusarium spp. strains. J. Antimicrob. Chemother. 39:163-167. [DOI] [PubMed] [Google Scholar]
- 20.Richardson, S. E., R. M. Bannatyne, R. C. Summerbell, J. Milliken, R. Gold, and S. S. Weitzman. 1988. Disseminated fusarial infection in the immunocompromised host. Rev. Infect. Dis. 10:1171-1181. [DOI] [PubMed] [Google Scholar]
- 21.Segal, B. H., T. J. Walsh, J. M. Liu, J. D. Wilson, and K. J. Kwon-Chung. 1998. Invasive infection with Fusarium chlamydosporum in a patient with aplastic anemia. J. Clin. Microbiol. 36:1772-1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Summerbell, R. C. 2001. Respiratory tract infections caused by indoor fungi, p. 195-215. In B. Flannigan, R. A. Samson, and J. D. Miller (ed.), Microorganisms in home and indoor work environments. Taylor and Francis Press, London, England.
- 23.Summerbell, R. C. 2003. Aspergillus, Fusarium, Sporothrix, Piedraia and their relatives, p. 237-498. In D. H. Howard (ed.), Pathogenic fungi in humans and animals, 2nd ed. Marcel Dekker Press, New York, N.Y.
- 24.Zapater, R. C. 1986. Opportunistic fungal infections—Fusarium infections—keratomycosis by Fusarium. Jpn. J. Med. Mycol. 27:68-69. [Google Scholar]