Abstract
We have evaluated the performance of two rapid, low-cost methods for the detection of ofloxacin (OFX) resistance with 95 Mycobacterium tuberculosis isolates from countries with high multidrug-resistant tuberculosis endemicity. Results obtained by nitrate reductase and resazurin assays showed 100% agreement with those of the proportion method on 7H11 agar using 2 μg of OFX/ml. We confirmed the resistance of all isolates found to be resistant to OFX by the Mycobacterium Growth Indicator Tube system, and complete agreement among all methods was observed. Nitrate reductase and resazurin assays are rapid, simple, low-cost methods and might become inexpensive alternative procedures for rapid detection of OFX resistance in low-resource countries.
The control of tuberculosis (TB) has become a problem particularly for patients with multidrug-resistant tuberculosis (MDR-TB), defined as TB showing resistance at least to isoniazid and rifampin. The treatment of MDR-TB is much more difficult and expensive, and the mortality rate is particularly high in developing countries. Some patients with MDR-TB do not respond to treatment with first-line drugs (isoniazid [INH], rifampin [RIF], ethambutol [EMB], pyrazinamide, and streptomycin [STR]) (7, 8, 10, 36). Consequently, the treatment of MDR-TB involves reserve drugs called “second-line drugs.” Several studies have shown that MDR-TB can be cured by a combination of second-line drugs under DOTS-plus, the treatment strategy proposed by the World Health Organization to address the management of MDR-TB in settings with good control programs (9, 11, 17, 22, 25, 36).
Fluoroquinolones are widely used for the treatment of bacterial infections and also have activity against Mycobacterium tuberculosis. Among these, ofloxacin (OFX) has been identified as a new agent in the treatment of TB due to its significant bactericidal activity against M. tuberculosis (3, 12). OFX has been shown to be well tolerated by patients, with a low toxicity. To preserve the efficacy of OFX in the treatment of TB, laboratories supporting TB services in areas where MDR-TB is endemic must therefore be able to provide prompt and reliable drug susceptibility testing (DST) for OFX and the other drugs used in the treatment of patients. However, it is well known that DST on Löwenstein Jensen (LJ) medium or Middlebrook agar is very slow, requiring at least 4 to 6 weeks to produce the first results (5, 6). The development of rapid DST that is simple to use and affordable for low-resource countries is a priority (20, 24), since there are already reports of OFX-resistant strains of M. tuberculosis or the creation of OFX resistance during treatment (14, 15, 16, 18, 31, 34, 38). Some efforts have already been made to perform second-line DST by the radiometric BACTEC TB-460 system (Becton Dickinson Diagnostic Instrument Systems, Sparks, Md.) (29), but this method requires heavy equipment and radioactivity, which is an inappropriate technology for low-resource countries. Among the new alternative phenotypic methods for DST, rapid colorimetric methods, employing oxidation-reduction indicators, have been demonstrated to be reliable for second-line drugs and are promising methods for implementation in low-resource countries (21, 23). Another recently described method is the nitrate reductase assay on LJ medium, which is based on the ability of M. tuberculosis to reduce nitrate to nitrite. The presence of nitrite can easily be detected with specific reagents that produce a change in color (1, 19). Until now, this method has not been applied to the study of second-line drugs.
The aim of this work is to evaluate these two novel, rapid, low-cost methods for performing DST for OFX on M. tuberculosis isolates originating from countries with high prevalences of MDR-TB. The previously described resazurin microplate assay (21) and the nitrate reductase assay on 7H11 medium were performed in parallel, and the results were compared to those obtained by the conventional proportion method (PM) on 7H11 agar. All isolates found resistant to OFX were tested twice by each method, and results were confirmed by a commercial nonradiometric method, the manual Mycobacterium Growth Indicator Tube (MGIT) (26).
MATERIALS AND METHODS
Bacterial isolates.
Ninety-five clinical isolates originating from different areas in Peru, Armenia, Azerbaijan, Georgia, and Kazakhstan with high prevalences of MDR-TB were studied. All isolates have known drug susceptibility profiles for first-line drugs (RIF, INH, EMB, STR). M. tuberculosis H37Rv (ATCC 27294) was used as the susceptible control. All strains were freshly subcultured on LJ medium before use and were tested by the different methods.
Drugs.
OFX was obtained from Sigma-Aldrich (Bornem, Belgium). The stock solution was prepared in advance at a concentration of 1 mg/ml in 0.1 N NaOH, filter sterilized. and kept at −20°C for no more than 1 month.
DST.
The PM was performed on 7H11 agar with the recommended critical concentration of OFX, 2 μg/ml (37).
Colorimetric reagents.
A stock solution of resazurin sodium salt powder (Acros Organics N.V., Geel, Belgium) was prepared at 0.01% in distilled water, filter sterilized, and kept at +4°C.
The resazurin microtiter assay.
The resazurin microtiter assay plate method was carried out as described by Palomino et al. (28). Briefly, the inoculum was prepared from fresh LJ medium in 7H9-S medium (consisting of Middlebrook 7H9 broth containing 0.1% Casitone and 0.5% glycerol and supplemented with oleic acid, albumin, dextrose, and catalase [OADC; Becton Dickinson]), adjusted to a no. 1 McFarland tube, and diluted 1:20; 100 μl was used as the inoculum. The OFX stock solution was thawed and diluted in 7H9-S medium to four times the highest final concentration tested. Serial twofold dilutions of OFX were prepared directly in a sterile 96-well flat-bottom microtiter plate (VWR, Merck Eurolab, Leuven, Belgium) by using 100 μl of 7H9-S. The range of concentrations tested for OFX was 0.25 to 8.0 μg/ml. A growth control containing no antibiotic and a sterile control without inoculation were also prepared on each plate. Two hundred microliters of sterile water was added to all perimeter wells to avoid evaporation during incubation. The plate was covered with its lid, replaced in the original bag, and incubated at 37°C under a normal atmosphere. After 7 days of incubation, 30 μl of resazurin solution was added to each well and the plate was reincubated overnight. Then, at day 8, a change in color from blue (oxidized state) to pink (reduced state) indicated the growth of bacteria, and the MIC was defined as the lowest concentration of drug that prevented this change in color.
Nitrate reduction assay.
The nitrate reduction assay is based on the ability of M. tuberculosis to reduce nitrate to nitrite, which is routinely used for biochemical identification of mycobacterial species. The presence of nitrite can easily be detected with specific reagents that produce a color change. When used as a drug susceptibility test, the nitrate reduction assay uses the detection of nitrite as an indication of growth. OFX was included in the 7H11 medium at concentrations of 2 and 4 μg/ml with 1 mg of potassium nitrate (KNO3)/ml. The inoculum turbidity was adjusted to a no. 1 McFarland tube, and the inoculum was diluted 1:10 in phosphate-buffered saline. The reagent mixture consisted of 1 part 50%-concentrated hydrochloric acid (HCl), 2 parts 0.2% sulfanilamide, and 2 parts 0.1% n-1-naphthylethylenediamine dihydrochloride. The assay was performed as described by Δngeby et al. (1). For each strain, 200 μl of the undiluted suspension was inoculated into the antibiotic tube, and 200 μl of the 1:10 dilution was inoculated into the drug-free tube. The tubes were incubated in a horizontal position for one night and then at 37°C in a vertical position. After 7 days, 500 μl of the reagent mixture was added to one drug-free tube. If any color appeared, all the tubes were developed with the reagent mixture; otherwise, the tubes were reincubated and the procedure was repeated at day 9 and day 14. A strain was considered resistant if there was a color change in the antibiotic tube greater than that in the 1:10-diluted growth control.
MGIT.
The MGIT test was carried out as described by Palomino et al. (27). Briefly, MGIT tubes were supplemented with 0.5 ml of OADC, and OFX was added to a final concentration of 2 μg/ml. A growth control tube was prepared without antibiotic. The inoculum was adjusted to a 0.5 McFarland standard and further diluted 1:5 with sterile saline. The tubes were inoculated with 0.5 ml of the inoculum diluted 1:5. A positive-control tube was prepared by adding 5 ml of a 0.4% sodium sulfite solution to an empty MGIT tube, and an uninoculated MGIT tube was used as a negative control. After 3 days of incubation at 37°C, the fluorescence of the MGIT tubes was read on a 365-nm UV transilluminator. The growth control tube was compared to the positive and negative controls. Positivity was indicated by bright orange fluorescence at the bottom of the tube and an orange reflection at the meniscus. Negative tubes showed very little or no fluorescence. The time when the fluorescence appeared on the growth control tube was considered day 0 for the interpretation of the drug-containing tube. A strain was considered susceptible if the drug tube did not fluoresce within 2 days of the positivity of the growth control. A strain was considered resistant if the drug tube was positive within 2 days of the positivity of the growth control.
Analysis of data.
A MedCalc Software (Mariakerke, Belgium) program was used to calculate the cutoff point for the best resolution of resistant and susceptible strains.
RESULTS
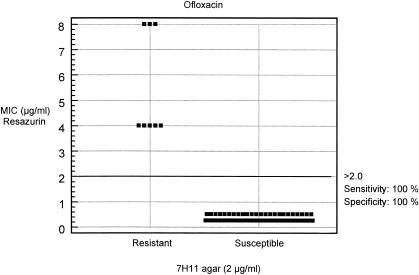
With the resazurin assay, colorimetric test results were available after an average of 8 days of incubation; results of the PM on 7H11 agar were available after 1 month. These results are presented in Table 1. For all M. tuberculosis isolates determined to be susceptible to OFX by the PM on 7H11 agar, the MIC was 0.5 μg/ml or lower. Eight out of 95 isolates were found to be resistant by the PM, and the MICs were equal to or higher than 4 μg/ml. All results were concordant. The correlation between MIC results obtained by the resazurin colorimetric method and results obtained by the 7H11 agar PM is shown in Fig. 1. The dot plot diagram, obtained with the MedCal Software program, allowed us to establish a cutoff point that distinguishes negative from positive results. The cutoff represents the “critical concentration” that defines susceptible and resistant strains based on the best fit of the colorimetric results with the conventional method. At 2 μg of OFX/ml, the specificity and sensitivity were both 100%.
TABLE 1.
MICs of OFX for 95 M. tuberculosis isolates determined by the resazurin assay compared to the PM
| PM result (no. of strains) | No. of isolates for which the OFX MIC (μg/ml) was:
|
|||||
|---|---|---|---|---|---|---|
| <0.25 | 0.5 | 1 | 2 | 4 | 8 | |
| OFX resistant (8) | 5 | 3 | ||||
| OFX susceptible (87) | 62 | 25 | ||||
FIG. 1.
Dot plot diagram of the susceptibilities of 95 isolates of M. tuberculosis to OFX by the 7H11 agar proportion method versus the colorimetric MIC resazurin assay.
With the nitrate reductase assay, results were obtained between 9 and 14 days, but the majority of results, for 75 out of 95 isolates (78.9%), were available at 9 days. These results are presented in Table 2. Complete agreement was found between the results of the nitrate reductase assay with two concentrations of OFX (2 and 4 μg/ml) and those obtained by the PM on 7H11 agar (2 μg/ml). Resistant results were tested at least twice for each method and confirmed by a third commercial method, the manual MGIT system. By the MGIT, results were obtained between 5 and 10 days. MGIT results agreed completely with those obtained for the resistant isolates by the PM, the resazurin assay, and the nitrate reductase assay.
TABLE 2.
Results for 95 M. tuberculosis isolates determined by the nitrate reductase assay compared to the PM
| PM result (no. of isolates) | Nitrate reductase assay result (no. of isolates)
|
|
|---|---|---|
| OFX resistant | OFX susceptible | |
| OFX resistant (8) | 8 | 0 |
| OFX susceptible (87) | 0 | 87 |
DISCUSSION
In low-income countries there is a great need for fast, reliable, and economical methods for testing the susceptibility of M. tuberculosis to first- and second-line drugs, due to the resurgence of MDR-TB strains and the appearance of the first reports of M. tuberculosis isolates resistant to fluoroquinolones (4). OFX is a fluoroquinolone active in the treatment of MDR-TB (36). Since human immunodeficiency virus has been associated with MDR-TB, OFX-containing drug regimens have been proven to be effective and safe for the treatment of MDR-TB in these patients (35). A trial conducted in Chennai, India, by the Tuberculosis Research Centre (33) showed promising results with several 4-month OFX-containing regimens for the treatment of sputum-positive pulmonary TB patients. As is known, the conventional PM is slow and laborious. The BACTEC TB-460 system, also used as a “gold standard,” reduces the time needed to obtain results, but the machine and the vials are expensive and generate radioactive waste. For these reasons, the BACTEC TB-460 system is used only in reference laboratories. Molecular genetic methods (32) are fast but too expensive to be used in most resource-poor settings, and in addition, not all the mechanisms of drug resistance are known (30). Fully automated commercial systems such as the BACTEC MGIT 960 (Becton Dickinson) or MB/BACT (Organon Teknika) are rapid and easy to use, but they require heavy equipment and high running costs.
The colorimetric resazurin assay was found to be an alternative low-cost and rapid method to detect resistance to OFX. The results obtained in this study are in complete agreement with those obtained by the PM. Our proposed cutoff value of 2 μg/ml fully agrees with the MIC of our previous study (21). The microplate format offers many advantages: many DSTs can be performed at the same time, and the method is cost-effective (including the reagents) and rapid and gives quantitative (MIC) results. One disadvantage of resazurin assays is the use of liquid media in a microplate format, which might be a biohazard, since aerosols could be generated.
The nitrate reductase assay, based on the ability of M. tuberculosis to reduce nitrate to nitrite, which is easily detectable with specific reagents, is another very interesting low-cost, rapid method. In this study, for the first time, testing of the susceptibility of M. tuberculosis to OFX by the nitrate reductase assay was evaluated. This method was recently evaluated for testing of first-line drugs (1). In this study, all results were concordant with those of the PM and the other methods tested. Results obtained with 2 and 4 μg of OFX/ml were the same. Therefore, we propose a concentration of 2 μg of OFX/ml for performing DST by the nitrate reductase assay; this is the same concentration used by the other methods (21, 26, 29). Since the critical drug concentrations for second-line drugs have not been completely established, this study helps to optimize the cutoff value and the ideal OFX concentration for DST. Nitrate reductase-negative strains of M. tuberculosis are very unusual. Our laboratory has tested the abilities of more than 200 clinical isolates originating from several countries, mainly located in Africa, to reduce nitrate and has found that 99% of these isolates were positive by this test (unpublished data). On the other hand, false results would be detected by the appropriate growth control included in the test. The great advantage of the nitrate reductase test is that it is performed on the classical 7H11, with nitrate incorporated into the medium. This is a very important factor, because laboratories do not have to change completely to another method. Adaptation to a novel technology is not always easy for laboratories involved in routine work. Moreover, biosafety problems are limited, because the medium is solid.
We performed a fourth test, with the commercial manual MGIT system, to confirm the resistance of the eight isolates found resistant to OFX by the conventional method, the resazurin assay, and the nitrate reductase assay. All these isolates were also found resistant by the MGIT system. This nonradiometric alternative method was easy to use, and results were obtained in 5 to 10 days. Until now, only two studies have used this technique to detect resistance to second-line drugs (OFX [26] and kanamycin [2]). This method requires no equipment, except for a UV lamp to enable reading of the tubes. The commercial manual MGIT system is reliable and less expensive than BACTEC TB-460 system and is not radioactive. The cost is the only factor precluding widespread use of this technique.
Among the eight isolates found resistant to OFX, six were resistant to the first-line drugs: INH, RIF, EMB, and STR. One isolate was resistant to INH, RIF, and EMB, and one was resistant only to EMB. Resistance to fluoroquinolones is not routinely assessed, particularly for isolates that are susceptible to current first-line drugs. In this study, we found one isolate resistant to OFX but susceptible to INH, RIF, and EMB. Since fluoroquinolones have been used widely for the treatment of bacterial infections, and for preventive therapy or empirical treatment of TB (13), resistance to fluoroquinolones should be rapidly detected in order to avoid the spread of strains resistant to OFX, and DST must not be difficult to perform because the lack of a reliable rapid method.
In summary, due to the high level of agreement of the resazurin and nitrate reductase assays with the gold-standard method, these methods seem to have the potential to provide rapid detection of OFX resistance. The results obtained with the nitrate reductase assay and the colorimetric resazurin method were available in an average of 10 days, as with the BACTEC TB-460 system. The use of OADC, when obtained from a commercial source, could represent an important cost. However, the use of a homemade OADC supplement can lower this cost, but the product should be quality controlled for adequate reproducibility and performance. The main disadvantage of the colorimetric resazurin assay versus the nitrate reductase assay is the use of liquid media. On the other hand, the resazurin assay is very practical in that many tests can be performed at the same time, which is a gain in time, due to the miniaturization of the microplate format. One disadvantage of the nitrate reductase assay is that the culture is killed by the mix reagent used to develop the assay. It is recommended that, if the culture is needed to perform other tests, one extra tube be used in parallel.
In conclusion, these assays represent a good option for testing of susceptibility to OFX by reliable, economical methods and have the potential to become interesting alternative methods, particularly in low-resource settings. Collaborative efforts will perform DST for the other second-line drugs with the nitrate reductase assay, which was not done until now. Early detection of MDR-TB and accurate DST for second-line drugs are essential for the successful control and treatment of MDR-TB around the world.
Acknowledgments
We thank Krista Fissette for excellent technical assistance.
This study was supported by the European Commission RDG (INCO-DEV Programme), projects ICA4-CT-2001-10087 and ICA-CT-2002-10057, and by the Damien Foundation, Brussels, Belgium.
REFERENCES
- 1.Δngeby, K. A., L. Klintz, and S. E. Hoffner. 2002. Rapid and inexpensive drug susceptibility testing of Mycobacterium tuberculosis with a nitrate reductase assay. J. Clin. Microbiol. 40:553-555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bastian, I., L. Rigouts, J. C. Palomino, and F. Portaels. 2001. Kanamycin susceptibility testing of Mycobacterium tuberculosis using Mycobacterium Growth Indicator Tube and a colorimetric method. Antimicrob. Agents Chemother. 45:1934-1936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berning, S. E. 2001. The role of fluoroquinolones in tuberculosis today. Drugs 61:9-10. [DOI] [PubMed] [Google Scholar]
- 4.Bryskier, A., and J. Lowther. 2002. Fluoroquinolones and tuberculosis. Expert Opin. Investig. Drugs 11:233-258. [DOI] [PubMed] [Google Scholar]
- 5.Canetti, G., F. Froman, J. Grosset, P. Hauduroy, M. Langerova, H. T. Mahler, G. Meissner, D. A. Mitchison, and L. Sula. 1963. Mycobacteria: laboratory methods for testing drug sensitivity and resistance. Bull. W. H. O. 29:565-578. [PMC free article] [PubMed] [Google Scholar]
- 6.Canetti, G., W. Fox, A. Khomenko, H. T. Mahler, N. K. Menon, D. A. Mitchison, N. Rist, and N. A. Smelev. 1969. Advances in techniques of testing mycobacterial drug sensitivity, and the use of sensitivity tests in tuberculosis control programmes. Bull. W. H. O. 41:21-43. [PMC free article] [PubMed] [Google Scholar]
- 7.Espinal, M. A. 2003. The global situation of MDR-TB. Tuberculosis (Edinburgh) 83:44-51. [DOI] [PubMed] [Google Scholar]
- 8.Espinal, M. A., A. Laszlo, L. Simonsen, F. Boulahbal, S. J. Kim, A. Reniero, S. Hoffner, H. L. Rieder, N. Binkin, C. Dye, R. Williams, M. C. Raviglione, et al. 2001. Global trends in resistance to antituberculosis drugs. N. Engl. J. Med. 344:1294-1303. [DOI] [PubMed] [Google Scholar]
- 9.Espinal, M. A., C. Dye, M. Raviglione, and A. Kochi. 1999. Rational ‘DOTS plus’ for the control of MDR-TB. Int. J. Tuberc. Lung Dis. 3:561-563. [PubMed] [Google Scholar]
- 10.Espinal, M. A., S. J. Kim, P. G. Suarez, K. M. Kam, A. G. Khomenko, G. B. Migliori, J. Baez, A. Kochi, C. Dye, and M. C. Raviglione. 2000. Standard short-course chemotherapy for drug-resistant tuberculosis: treatment outcomes in 6 countries. JAMA 283:2537-2545. [DOI] [PubMed] [Google Scholar]
- 11.Farmer, P., and J. Y. Kim. 1998. Community based approaches to the control of multidrug resistant tuberculosis: introducing “DOTS-plus.” Br. Med. J. 317:671-674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gillespie, S. H., and N. Kennedy. 1998. Fluoroquinolones: a new treatment for tuberculosis? Int. J. Tuberc. Lung Dis. 2:265-271. [PubMed] [Google Scholar]
- 13.Ginsburg, A. S., J. H. Grosset, and W. R. Bishai. 2003. Fluoroquinolones, tuberculosis, and resistance. Lancet Infect. Dis. 7:432-442. [DOI] [PubMed] [Google Scholar]
- 14.Ginsburg, A. S., N. Hooper, N. Parrish, K. E. Dooley, S. E. Dorman, J. Booth, M. Diener-West, W. G. Merz, W. R. Bishai, and T. R. Sterling. 2003. Fluoroquinolone resistance in patients with newly diagnosed tuberculosis. Clin. Infect. Dis. 11:1448-1452. [DOI] [PubMed] [Google Scholar]
- 15.Ginsburg, A. S., S. C. Woolwine, N. Hooper, W. H. Benjamin, Jr., W. R. Bishai, S. E. Dorman, and T. R. Sterling. 2003. The rapid development of fluoroquinolone resistance in M. tuberculosis. N. Engl. J. Med. 349:1977-1978. [DOI] [PubMed] [Google Scholar]
- 16.Grimaldo, E. R., T. E. Tupasi, A. B. Rivera, M. I. Quelapio, R. C. Cardano, J. O. Derilo, and V. A. Belen. 2001. Increased resistance to ciprofloxacin and ofloxacin in multidrug-resistant Mycobacterium tuberculosis isolates from patients seen at a tertiary hospital in the Philippines. Int. J. Tuberc. Lung Dis. 5:546-550. [PubMed] [Google Scholar]
- 17.Gupta, R., M. C. Raviglione, and M. A. Espinal. 2001. Should tuberculosis programmes invest in second-line treatments for multidrug-resistant tuberculosis (MDR-TB)? Int. J. Tuberc. Lung Dis. 5:1078-1079. [PubMed] [Google Scholar]
- 18.Lee, A. S., L. L. Tang, I. H. Lim, and S. Y. Wong. 2002. Characterization of pyrazinamide and ofloxacin resistance among drug resistant Mycobacterium tuberculosis isolates from Singapore. Int. J. Infect. Dis. 6:48-51. [DOI] [PubMed] [Google Scholar]
- 19.Lemus, D., A. Martin, E. Montoro, F. Portaels, and J. C. Palomino.2004. Rapid alternative methods for detection of rifampicin resistance in Mycobacterium tuberculosis. J. Antimicrob. Chemother. 54:130-133. [DOI] [PubMed] [Google Scholar]
- 20.Loddenkemper, R., D. Sagebiel, and A. Brendel. 2002. Strategies against multidrug-resistant tuberculosis. Eur. Respir. J. Suppl. 36:66s-77s. [DOI] [PubMed] [Google Scholar]
- 21.Martin, A., M. Camacho, F. Portaels, and J. C. Palomino. 2003. Resazurin microtiter assay plate testing of Mycobacterium tuberculosis susceptibilities to second-line drugs: rapid, simple, and inexpensive method. Antimicrob. Agents Chemother. 47:3616-3619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mitnick, C., J. Bayona, E. Palacios, S. Shin, J. Furin, F. Alcantara, E. Sanchez, M. Sarria, M. Becerra, M. C. Fawzi, S. Kapiga, D. Neuberg, J. H. Maguire, J. Y. Kim, and P. Farmer. 2003. Community-based therapy for multidrug-resistant tuberculosis in Lima, Peru. N. Engl. J. Med. 348:119-128. [DOI] [PubMed] [Google Scholar]
- 23.Morcillo, N., B. Di Giulio, B. Testani, M. Pontino, C. Chirico, and A. Dolmann. 2004. A microplate indicator-based method for determining drug-susceptibility of multidrug-resistant Mycobacterium tuberculosis to antimicrobial agents. Int. J. Tuberc. Lung Dis. 8:253-259. [PubMed] [Google Scholar]
- 24.Nachega, J. B., and R. E. Chaisson. 2003. Tuberculosis drug resistance: a global threat. Clin. Infect. Dis. 36:24-30. [DOI] [PubMed] [Google Scholar]
- 25.Pablos-Mendez, A., D. K. Gowda, and T. R. Frieden. 2002. Controlling multidrug-resistant tuberculosis and access to expensive drugs: a rational framework. Bull. W. H. O. 80:489-495. [PMC free article] [PubMed] [Google Scholar]
- 26.Palaci, M., S. Y. Ueki, D. N. Sato, M. A. Da Silva Telles, M. Curcio, and E. A. Silva. 1996. Evaluation of mycobacteria growth indicator tube for recovery and drug susceptibility testing of Mycobacterium tuberculosis isolates from respiratory specimens. J. Clin. Microbiol. 34:762-764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Palomino, J. C., H. Traore, K. Fissette, and F. Portaels. 1999. Evaluation of Mycobacteria Growth Indicator Tube (MGIT) for drug susceptibility testing of Mycobacterium tuberculosis. Int. J. Tuberc. Lung Dis. 3:344-348. [PubMed] [Google Scholar]
- 28.Palomino, J. C., A. Martin, M. Camacho, H. Guerra, J. Swings, and F. Portaels. 2002. Resazurin microtiter assay plate: simple and inexpensive method for detection of drug resistance in Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 46:2720-2722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pfyffer, G. E., D. A. Bonato, A. Ebrahimzadeh, W. Gross, J. Hotaling, J. Kornblum, A. Laszlo, G. Roberts, M. Salfinger, F. Wittwer, and S. Siddiqi. 1999. Multicenter laboratory validation of susceptibility testing of Mycobacterium tuberculosis against classical second-line and newer antimicrobial drugs by using the radiometric BACTEC 460 technique and the proportion method with solid media. J. Clin. Microbiol. 37:3179-3186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Siddiqi, N., M. Shamim, S. Hussain, R. K. Choudhary, N. Ahmed, Prachee, S. Banerjee, G. R. Savithri, M. Alam, N. Pathak, A. Amin, M. Hanief, V. M. Katoch, S. K. Sharma, and S. E. Hasnain. 2002. Molecular characterization of multidrug-resistant isolates of Mycobacterium tuberculosis from patients in North India. Antimicrob. Agents Chemother. 46:443-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sullivan, E. A., B. N. Kreiswirth, L. Palumbo, V. Kapur, J. M. Musser, A. Ebrahimzadeh, and T. R. Frieden. 1995. Emergence of fluoroquinolone-resistant tuberculosis in New York City. Lancet 345:1148-1150. [DOI] [PubMed] [Google Scholar]
- 32.Takiff, H. E., L. Salazar, C. Guerrero, W. Philipp, W. M. Huang, B. Kreiswirth, S. T. Cole, W. R. Jacobs, Jr., and A. Telenti. 1994. Cloning and nucleotide sequence of Mycobacterium tuberculosis gyrA and gyrB genes and detection of quinolone resistance mutations. Antimicrob. Agents Chemother. 38:773-780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tuberculosis Research Centre, Chennai. 2002. Shortening short course chemotherapy: a randomised clinical trial for treatment of smear positive pulmonary tuberculosis with regimens using ofloxacin in the intensive phase. Indian J. Tuberc. 49:27-38. [Google Scholar]
- 34.Van Deun, A., M. A. Hamid Salim, A. P. Kumar Das, I. Bastian, and F. Portaels. 2004. Results of a standardised regimen for multidrug-resistant tuberculosis in Bangladesh. Int. J. Tuberc. Lung Dis. 8:560-567. [PubMed] [Google Scholar]
- 35.Walwaikar, P. P., V. K. Morye, and A. S. Gawde. 2003. Ofloxacin in multidrug resistant tuberculosis. J. Indian Med. Assoc. 101:210-212. [PubMed] [Google Scholar]
- 36.World Health Organization. 2000. Guidelines for establishing DOTS-Plus pilot projects for the management of multidrug resistant tuberculosis (MDRTB). WHO/ODS/TB/2000.279. World Health Organization, Geneva, Switzerland.
- 37.World Health Organization. 2001. Guidelines for drug susceptibility testing for second-line anti-tuberculosis drugs for DOTS-plus. WHO/CDS/TB/2001.288. World Health Organization, Geneva, Switzerland.
- 38.Yu, M. C., J. Suo, T. P. Lin, and K. T. Luh. 1997. In vitro activity of ofloxacin against Mycobacterium tuberculosis. J. Formos. Med. Assoc. 96:13-16. [PubMed] [Google Scholar]