Abstract
We developed a 16S PCR-based assay for the rapid detection of Nocardia spp. directly from human clinical samples. The applicability of the assay was confirmed by using 18 samples from patients with nocardiosis as diagnosed by conventional cultures and 20 clinical samples from patients with confirmed tuberculosis used as negative controls.
Nocardia spp. have been isolated worldwide from the environment and induce serious infections in humans, occurring most frequently in immunosuppressed patients. The common clinical forms of Nocardia infections are pulmonary, cerebral, cutaneous, subcutaneous, and lymphocutaneous infections and mycetoma (5, 7, 19, 21). Most of the cases are not correctly and rapidly recognized, due to the absence of pathognomonic clinical signs. The diagnosis of nocardiosis, currently based on direct examination and conventional cultures, is difficult, long, and time-consuming. The need for new methods allowing identification of Nocardia infections is crucial. We reported and validated a PCR approach combined with hybridization to perform a diagnosis directly from clinical specimens such as skin biopsy samples, pus from abscesses, sputa, or bronchoalveolar liquid (BAL).
Tested samples contained 250 μl of sterile water (molecular biology-grade water; Eurobio, Courtaboeuf, France) plus 100-μl pus samples, 100-μl seeded specimens, or 100-mg tissue biopsy specimens. These mixtures were incubated for 3 h at 55°C with proteinase K at 20 mg/ml (Sigma Aldrich, Saint Quentin Fallavier, France) and inactivated for 15 min at 95°C. Then, nocardial DNA was extracted with an MTB respiratory specimen preparation kit (Roche, Meylan, France), according to the manufacturer's instructions. Primers NG1 (5′-ACCGACCACAAGGGGG-3′) and NG2 (5′-GGTTGTAAACCTCTTTCGA-3′) (0.5 μM final concentration) were used to amplify a Nocardia genus-specific 590-bp fragment of 16S rRNA, as previously described (17). Primers PC04 (5′-CAACTTCATCCACGTTCACC-3′) and GH20 (5′-GAAGAGCCAAGGACAGGTAC-3′) were used to amplify a 268-bp fragment of the human β-globin gene selected as a control gene to monitor specimen processing and DNA extraction, as previously described (11). Amplification was carried out using packaged PCR tubes (Ready-to-Go PCR beads; Amersham Biosciences, Orsay, France) after reconstituted final volumes of 25 and 10 μl of extracted DNA were added to the PCR mixture. Twelve microliters of each amplification reaction mixture was analyzed by electrophoresis performed with a 1% (wt/vol) agarose gel stained with ethidium bromide (0.7 μg/ml). After migration, the 16S amplified fragments were transferred under a vacuum onto positive nylon membranes (Hybond-N+; Amersham Biosciences) by Southern blotting. The fragments were then dried and fixed under UV for 3 min. Hybridization with a chemiluminescent 16S probe (prepared by PCR using the reference strain Nocardia asteroides ATCC 19247T, according to the protocol described above) and detection were then achieved as previously described (16).
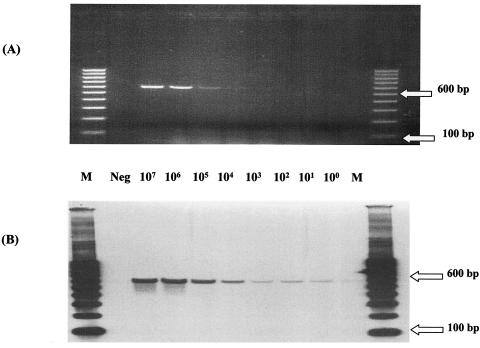
To evaluate the analytical sensitivity of the assay, we used clinical specimens seeded with 108 to 101 cells per ml from N. asteroides strain ATCC 19247T. In the BAL specimens, 103 CFU/reaction mixture was visually detected after agarose gel electrophoresis, whereas as little as 1 CFU/reaction mixture was detected by Southern blotting and chemiluminescent hybridization (Fig. 1). The same results were obtained with seeded skin biopsy and cerebral abscess specimens. These data indicate that the sensitivity of hybridization was 1,000 times higher than that of the single electrophoresis performed with an agarose gel stained with ethidium bromide. Moreover, the hybridization step allowed confirmation of the specificity of the amplified fragments (Fig. 1 and 2).
FIG. 1.
Analytical sensitivity of PCR protocol determined with clinical BAL sample seeded with Nocardia inocula of various sizes (shown as number of CFU per reaction mixture for each lane). (A) After electrophoresis in 1% agarose gel; (B) after Southern blot hybridization with a 16S probe. Lanes: M, molecular size markers (100-bp ladder); Neg, unseeded BAL sample (negative control).
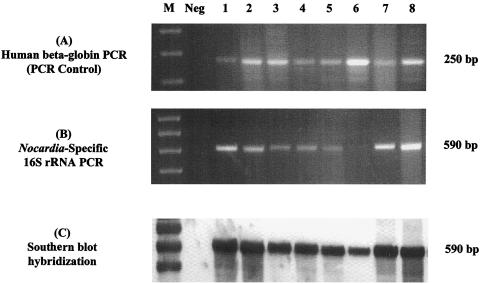
FIG. 2.
Agarose gel electrophoresis and Southern blot hybridization of PCR products obtained from clinical samples from patients with confirmed nocardiosis. (A) β-Globin amplified products in 1% agarose gel; (B) Nocardia-specific 16S rRNA amplified products in 1% agarose gel; (C) Southern blot hybridization with chemiluminescent 16S probe. Lanes: M, molecular size markers (100-bp ladder); Neg, distilled water; 1 to 8, clinical samples.
Eighteen samples (four BAL, two sputum, two pleural liquid, six pus, and four biopsy samples) from patients with different forms of nocardiosis were tested to demonstrate the applicability of this protocol in a clinical setting. For all specimens, the presence of Nocardia was confirmed by culture. All isolates were identified at the species level by hsp65 PCR restriction analysis and were distributed as follows: N. asteroides (n = 3), N. brasiliensis (n = 2), N. farcinica (n = 4), N. nova (n = 6), and N. otitidiscaviarum (n = 3).
For all specimens, amplifications were positive (Fig. 2). The intensity of amplified DNA in agarose gel was variable: sometimes weak, but always detectable. Conversely, a sharp chemiluminescent signal was observed for each sample after hybridization, confirming the specificity of the 590-bp amplified fragments and facilitating interpretation of the samples with weak intensive bands in the agarose gel. The assay described herein enabled us to detect Nocardia DNA in various tissue samples that are representative of specimens classically used in the diagnosis of Nocardia infections (BAL, sputum, biopsy, and pus specimens).
Twenty samples (2 BAL, 3 biopsy, 3 pus, and 12 sputum samples) from patients hospitalized in the Hospices Civils de Lyon (Lyon, France) were used as controls. For each of the 20 patients, a diagnosis of tuberculosis was confirmed by culture and PCR (AMPLICOR MTB; Roche) according to the sample used in our study. No visible amplified fragments were observed, either in the agarose gel or after the hybridization of transferred membranes (data not shown). These results highlighted the specificity of the primers and PCR protocol, since these samples contained mycobacteria that are closely related to Nocardia spp.
Human β-globin, selected as a control gene to monitor specimen processing and DNA extraction, was correctly amplified from the 65 human specimens tested (27 seeded samples [data not shown] and 38 clinical samples [examples in Fig. 2]). These results demonstrated the absence of PCR inhibitors in extracts and validated the 16S PCR results and Southern blot analysis. The DNA extraction method was chosen according to the common characteristics of cell wall composition for Mycobacterium and Nocardia organisms, because of the extensive validation of the MTB respiratory specimen preparation kit (Roche) for extraction of Mycobacterium tuberculosis DNA from clinical samples (6, 9, 18, 24, 25). The results obtained demonstrate that this protocol is effective in liberating nocardial DNA and preventing PCR inhibitors.
In addition to being sensitive, specific, and rapid, the assay developed can overcome several problems associated with the microbiological diagnosis of nocardiosis. Due to time-consuming phenotypic methods, nocardiosis is sometimes diagnosed after the dissemination of the strain to other organs or after the patient has died (15, 20, 23). Therefore, it is difficult to institute an adapted therapy at the early stages of the disease. However, early initiation of appropriate antibiotherapy is paramount in reducing the high mortality rates of patients with nocardiosis and is dependent on early detection of the nocardial infection. Until now, a confirmed diagnosis required the isolation of the organism from specimens. This “gold standard” is believed to lack sensitivity (21). Whereas Nocardia strains can grow on a large variety of media, their isolation from the complex mixed flora of clinical specimens (especially pulmonary samples) has been problematic, due to the slower growth of Nocardia spp. relative to that of other contaminating bacteria and fungi. These other organisms can hide and/or prevent growth of Nocardia isolates. The molecular approach abolishes these problems by the specific amplification of nocardial DNA, even if several other contaminating or colonizing bacteria are present in human specimens. Empirical antibiotherapy instituted before sampling can also prevent or delay growth of bacteria, especially in cerebral or skin abscesses. Molecular approaches were not affected by the viability of bacteria and allowed the detection of bacteria even after the initiation of active chemotherapy.
Our PCR protocol can also help to answer several academic questions concerning Nocardia and nocardiosis. Combined with specific DNA extraction from soil, the protocol may facilitate the high-throughput screening of ecological niches of Nocardia and allow us to replace the use of uncommon selective media. It may allow a large-scale screening of human nocardial carriage and mild clinical infections in humans that have been described in the literature but never clearly demonstrated. Finally, several works support the concept that cell wall-deficient forms of Nocardia spp. play a significant role in both the pathogenesis and the latency of disease, as well as the recurrence of infections after apparently successful chemotherapy (1, 2, 3, 4, 14). Recent data suggest that such forms of Nocardia spp. could be implicated in symptoms similar to those of Parkinson's disease (8, 10, 26). It is necessary to develop methods capable of detecting these Nocardia spp. in order to discover, understand, and monitor accurately their effects on the environment and on patients. Molecular techniques like the PCR protocol presented here represent one of the specific approaches that may contribute to such studies (12, 13, 22, 27).
In conclusion, we have developed a highly sensitive and specific PCR assay for the detection of Nocardia bacteria in tissue samples. Further studies are necessary to prospectively evaluate this assay within a larger clinical population. Nevertheless, this assay could improve the speed of diagnosis of nocardiosis, which could lead to a favorable course of treatment and prognosis for patients (in terms of mortality, relapse, and side effects). Techniques such as the PCR assay described here may benefit reference laboratories and leading university laboratories with clinics serving numerous patients at risk for nocardiosis.
Acknowledgments
We are grateful to the following individuals in France who sent clinical Nocardia-positive samples to our laboratory: F. Batguzere (Centre Hospitalier de Pau, Pau), H. Biessy (Hôpital Saint Louis, La Rochelle), S. Bourdon (Centre Hospitalier d'Angers, Angers), S. Dekeyser (Centre Hospitalier de Béthune, Béthune), F. Girard-Pipau (Centre Hospitalo-Universitaire de l'Archet, Nice), F. Hamdad-Douadi (Centre Hospitalo-Universitaire d'Amiens, Amiens), H. Lelièvre (Laboratoire Marcel Mérieux, Lyon), M.-N. Letouzey (Centre Hospitalier de Villefranche, Villefranche sur Saône), L. Maisonneuve (Hôpital Intercommunal Robert Ballanger, Aulnay-sous-Bois), H. de Montclos (Centre Hospitalier de Fleyriat, Bourg-en-Bresse), C. Pradon (Hôpital Américain de Paris, Neuilly sur Seine), and B. Pron (Hôpital Raymond Poincarré, Garches).
REFERENCES
- 1.Beaman, B. L. 1981. The possible role of L-phase variants of Nocardia in chronic infections. Zentbl. Bakteriol. Mikrobiol. Hyg. Abt. Suppl. 11:221-227. [Google Scholar]
- 2.Beaman, B. L. 1982. Nocardiosis: role of the cell deficient state of Nocardia, p. 231-255. In G. J. Domingue (ed.), Cell wall defective bacteria: basic principles and clinical significance. Addison-Wesley Publishing Co., Inc., Reading, Mass.
- 3.Beaman, B. L. 1984. The cell wall as a determinant of pathogenicity in Nocardia: the role of L-forms in pathogenesis, p. 89-104. In L. Ortiz-Ortiz, L. F. Bojalil, and V. Yakoleff (ed.), Biological, biochemical and biomedical aspects of actinomycetes. Academic Press, Orlando, Fla.
- 4.Beaman, B. L., J. Burnside, B. Edwards, and W. Causey. 1976. Nocardial infections in the United States, 1972-1974. J. Infect. Dis. 134:286-289. [DOI] [PubMed] [Google Scholar]
- 5.Beaman, B. L., M. A. Saubolle, and R. J. Wallace. 1995. Nocardia, Rhodococcus, Streptomyces, Oerskovia, and other aerobic actinomycetes of medical importance, p. 379-399. In P. R. Murray, E. J. Baron, M. A. Pfaller, F. C. Tenover, and R. H. Yolken (ed.), Manual of clinical microbiology, 6th ed. American Society for Microbiology, Washington, D.C.
- 6.Bergmann, J. S., and G. L. Woods. 1996. Clinical evaluation of the Roche AMPLICOR PCR Mycobacterium tuberculosis test for detection of M. tuberculosis in respiratory specimens. J. Clin. Microbiol. 34:1083-1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boiron, P., F. Provost, G. Chevrier, and B. Dupont. 1992. Review of nocardial infections in France 1987 to 1990. Eur. J. Clin. Microbiol. Infect. Dis. 11:709-714. [DOI] [PubMed] [Google Scholar]
- 8.Chapman, G., B. L. Beaman, D. A. Loeffler, D. M. Camp, E. F. Domino, D. W. Dickson, W. G. Ellis, I. Chen, S. E. Bachus, and P. A. Le Witt. 2003. In situ hybridization for detection of nocardial 16S rRNA: reactivity within intracellular inclusions in experimentally infected cynomolgus monkeys and in Lewy body-containing human brain specimens. Exp. Neurol. 184:715-725. [DOI] [PubMed] [Google Scholar]
- 9.D'Amato, R. F., A. A. Wallman, L. H. Hochstein, P. M. Colaninno, M. Scardamaglia, E. Ardila, M. Ghouri, K. Kim, R. C. Patel, and A. Miller. 1995. Rapid diagnosis of pulmonary tuberculosis by using Roche AMPLICOR Mycobacterium tuberculosis PCR test. J. Clin. Microbiol. 33:1832-1834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Diaz-Corrales, F. J., C. Colasante, Q. Contreras, M. Puig, J. A. Serrano, L. Hernandez, and B. L. Beaman. 2004. Nocardia otitidiscaviarum (GAM-5) induces parkinsonian-like alterations in mouse. Braz. J. Med. Biol. Res. 37:539-548. [DOI] [PubMed] [Google Scholar]
- 11.Gauduchon, V., L. Chalabreysse, J. Etienne, M. Cĺard, Y. Benito, H. Lepidi, F. Thivolet-Bj́ui, and F. Vandenesch. 2003. Molecular diagnosis of infective endocarditis by PCR amplification and direct sequencing of DNA from valve tissue. J. Clin. Microbiol. 41:763-766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harper-Owen, R., D. Dymock, V. Booth, A. J. Weightman, and W. G. Wade. 1999. Detection of unculturable bacteria in periodontal health and disease by PCR. J. Clin. Microbiol. 37:1469-1473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Josephson, K. L., C. P. Gerba, and I. L. Pepper. 1993. Polymerase chain reaction detection of nonviable bacterial pathogens. Appl. Environ. Microbiol. 59:3513-3515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khobata, S. 1998. Tinctorial properties of spherical bodies in broth cultures of Nocardia asteroides GUH-2. Microbiol. Immunol. 42:151-157. [DOI] [PubMed] [Google Scholar]
- 15.Koffi, N., E. Aka-Danguy, A. Ngom, B. Kouassi, B. A. Yaya, and M. Dosso. 1998. Prevalence of nocardiosis in an area of endemic tuberculosis. Rev. Mal. Respir. 15:643-647. [PubMed] [Google Scholar]
- 16.Laurent, F., A. Carlotti, P. Boiron, J. Villard, and J. Freney. 1996. Ribotyping: a tool for taxonomy and identification of the Nocardia asteroides complex species. J. Clin. Microbiol. 34:1079-1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Laurent, F. J., F. Provost, and P. Boiron. 1999. Rapid identification of clinically relevant Nocardia species to genus level by 16S rRNA gene PCR. J. Clin. Microbiol. 37:99-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Levidiotou, S., G. Vrioni, E. Galanakis, E. Gesouli, C. Pappa, and D. Stefanou. 2003. Four-year experience of use of the Cobas Amplicor system for rapid detection of Mycobacterium tuberculosis complex in respiratory and nonrespiratory specimens in Greece. Eur. J. Clin. Microbiol. Infect. Dis. 22:349-356. [DOI] [PubMed] [Google Scholar]
- 19.Lopez Martinez, R., L. J. Mendez Tovar, P. Lavalle, O. Welsh, A. Saul, and E. Macotela Ruiz. 1992. Epidemiology of mycetoma in Mexico: study of 2105 cases. Gac. Med. Mex. 128:477-481. [PubMed] [Google Scholar]
- 20.Lucas, S. B., A. Hounnoun, C. Peacock, A. Beaumel, A. Kadio, and K. M. De Cock. 1994. Nocardiosis in HIV-positive patients: an autopsy study in West Africa. Tuber. Lung Dis. 75:301-307. [DOI] [PubMed] [Google Scholar]
- 21.McNeil, M. M., and J. M. Brown. 1994. The medically important aerobic actinomycetes: epidemiology and microbiology. Clin. Microbiol. Rev. 7:357-417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Palmu, A. A., P. A. Saukkoriipi, M. I. Lahdenkari, L. K. Kuisma, P. H. Makela, T. M. Kilpi, and M. Leinomen. 2004. Does the presence of pneumococcal DNA in middle-ear fluid indicate pneumococcal etiology in acute otitis media? J. Infect. Dis. 189:775-784. [DOI] [PubMed] [Google Scholar]
- 23.Reis, M. A., R. S. Costa, and A. S. Ferraz. 1995. Causes of death in renal transplant recipients: a study of 102 autopsies from 1968 to 1991. J. R. Soc. Med. 88:24-27. [PMC free article] [PubMed] [Google Scholar]
- 24.Scarparo, C., P. Piccoli, A. Rigon, G. Ruggiero, M. Scagnelli, and C. Piersimoni. 2000. Comparison of enhanced Mycobacterium tuberculosis amplified direct test with COBAS AMPLICOR Mycobacterium tuberculosis assay for direct detection of Mycobacterium tuberculosis complex in respiratory and extrapulmonary specimens. J. Clin. Microbiol. 38:1559-1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shah, S., A. Miller, A. Mastellone, K. Kim, P. Colaninno, L. Hochstein, and R. D'Amato. 1998. Rapid diagnosis of tuberculosis in various biopsy and body fluid specimens by the AMPLICOR Mycobacterium tuberculosis polymerase chain reaction test. Chest 113:1190-1194. [DOI] [PubMed] [Google Scholar]
- 26.Tam, S., D. P. Barry, L. Beaman, and B. L. Beaman. Neuroinvasive Nocardia asteroides GUH-2 induces apoptosis in the substantia nigra in vivo and dopaminergic cells in vitro. Exp. Neurol. 177:453-460. [DOI] [PubMed]
- 27.Wang, H., and Z. Chen. 2001. Observations of properties of the L-forms of Mycobacterium tuberculosis induced by the antituberculosis drugs. Zhonghua Jiehe He Huxi Zazhi 24:52-55. [PubMed] [Google Scholar]