Abstract
Objectives
The aim of this study was to describe and evaluate the configurations and management of feline skull fractures and concurrent injuries following head trauma.
Methods
Medical records and CT images were reviewed for cats with skull fractures confirmed by CT that were managed conservatively or with surgery. Details of signalment, presentation, skull fracture configuration, management, re-examination, and complications or mortality were recorded and analysed.
Results
Seventy-five cats (53 males, 22 females) with a mean age of 4.8 ± 3 years met the inclusion criteria. Eighty-nine percent of cats had fractures in multiple bones of the skull, with the mandible, upper jaw (maxilla, incisive and nasal bones) and craniofacial regions most commonly affected. Temporomandibular joint injury occurred in 56% of cats. Road traffic accidents (RTAs) were the most common cause of skull fractures, occurring in 89% of cats, and caused fractures of multiple regions of the skull. RTAs were also associated with high levels of concurrent injuries, particularly ophthalmic, neurological and thoracic injuries. A more limited distribution of injuries was seen in non-RTA cats. Equal numbers of cats were managed conservatively or surgically (47%). Mortality rate was 8% and complications were reported in 22% of cats. Increasing age at presentation and presence of internal upper jaw fractures were risk factors for development of complications. No risk factors were identified for mortality.
Conclusions and relevance
RTAs were the most common cause of feline skull fractures and resulted in fractures in multiple regions of the skull and concurrent injuries occurred frequently. Problems with dental occlusion were uncommon post-treatment. An increased risk of implant loosening and malocclusion was seen with palatine and pterygoid bone fractures and hard palate injuries. This study provides useful additional information regarding feline skull fractures, concurrent injuries and management techniques following head trauma.
Keywords: Skull fracture, head trauma, surgery, conservative, complications, CT, computed tomography
Introduction
Trauma is a common cause of injury in cats, with the head being one of the most frequently injured areas.1,2 Fractures of various bones of the skull are reported following head trauma, with up to 27% of trauma-related fractures affecting the skull.3–5 Road traffic accidents (RTAs) are the most common cause;6–8 however, skull fractures can also be caused by falling from a height or fighting.9–14
Skull fractures in cats may be managed conservatively or surgically. Reported surgical techniques include mandibular cerclage, interfragmentary wiring, interarcuate stabilisation with dental acrylic, bignathic encircling and retaining device (BEARD), external skeletal fixation (ESF), mini-plate fixation and mandibulectomy.15–19 For temporomandibular joint (TMJ) injuries, conservative management, maxillomandibular fixation, closed or open reduction of luxations, and condylectomy have all resulted in a successful functional outcome. 13 Morbidity associated with skull fractures and potentially their management include inability to eat, malocclusion of the dental arcade, TMJ ankylosis, soft tissue swelling, implant failure, damage to tooth roots and neurovascular structures, and regurgitation.13,16,17,19 Depending on the severity of the fractures and the type of fixation, feeding tubes may also be placed. 20
The current literature regarding skull fractures caused by head trauma in cats is limited and predominantly relates to management of specific fracture types, particularly of the mandible.7,17,19,21 CT is more sensitive than plain radiography for the identification of skull fractures in dogs and cats due to the complex anatomy of the skull and the lack of superimposition of structures and superior resolution achieved with CT.22,23 The additional information gained from these images regarding fracture configuration may be used to direct treatment planning.3,22 The aim of this study was to categorise skull fractures and concurrent injuries following head trauma in cats based on CT imaging and to describe their management.
Materials and methods
Ethical approval was obtained from the ethical review board at our institution (reference SR2017-1230). Medical records for cats admitted following head trauma between January 2010 and June 2017 were identified. Inclusion criteria were the presence of a fracture of any part of the skull, managed either conservatively or surgically, where CT imaging was used in their diagnosis (0.75 mm thick slices, 16-slice scanner [Mx8000 IDT; Philips]).
CT scans were evaluated by a board-certified radio-logist and surgeon. Medical records and CT images were reviewed for patient signalment, time from injury to presentation, type of traumatic event, location and configuration of skull fractures, concurrent injuries (including any dental trauma), management of skull fractures, whether a feeding tube was placed, length of hospitalisation, re-examination, complications and mortality. Traumatic events were classified as RTAs (including those witnessed and when cats were found by the road), bites, falling from a height and being shot. Evaluation of CT images was performed using DICOM imaging software (Osirix version 4.1 64-bit open-source DICOM viewer; Osirix Imaging Software). Skull fractures were classified as mandibular (body and ramus), mandibular symphyseal, external upper jaw (maxilla, incisive and nasal bones), internal upper jaw (palatine and pterygoid bones, hard and soft palate injuries), TMJ, craniofacial (frontal, orbital, temporal and zygomatic bones) and caudal skull (calvarium, parietal, occipital, presphenoid and basisphenoid bones). Concurrent injuries were classified as ophthalmic, soft tissue (wounds), orthopaedic, neurological and intrathoracic.
Statistical analysis was performed using standard computer software (SPSS version 24.0; IBM). Normality of data distribution was assessed and descriptive statistics performed as appropriate. To assess the relationship between risk factors and mortality or development of complications, univariable binary logistic regression was performed for each variable. Any variables with a P value <0.1 were put forward into multivariable logistic regression analysis with backwards elimination. Statistical significance was set at P <0.05.
Results
Signalment and presentation
Seventy-five cats (mean age 4.8 ± 3 years) met the inclusion criteria. Fifty-three cats (71%) were male (50 neutered, three entire) and 22 were female (21 neutered, one entire). Domestic shorthair (n = 52; 69%), domestic longhair (n = 7; 10%) and 10 other pedigree breeds (21%) were represented. Bengal cats (n = 3; 4%) were the most common pedigree breed. Cats were either presented directly to the first-opinion emergency service (n = 15; 20%) or were referred from other primary care practices (n = 60; 80%). Median time between the initial injury and presentation to our centre was 1 day (range 0–30 days). The majority of skull fractures occurred following RTAs (n = 67; 89%), with the others caused by dog or cat bites (n = 5; 7%), falls (n = 2; 3%) and being shot (n = 1; 1%).
Skull fractures
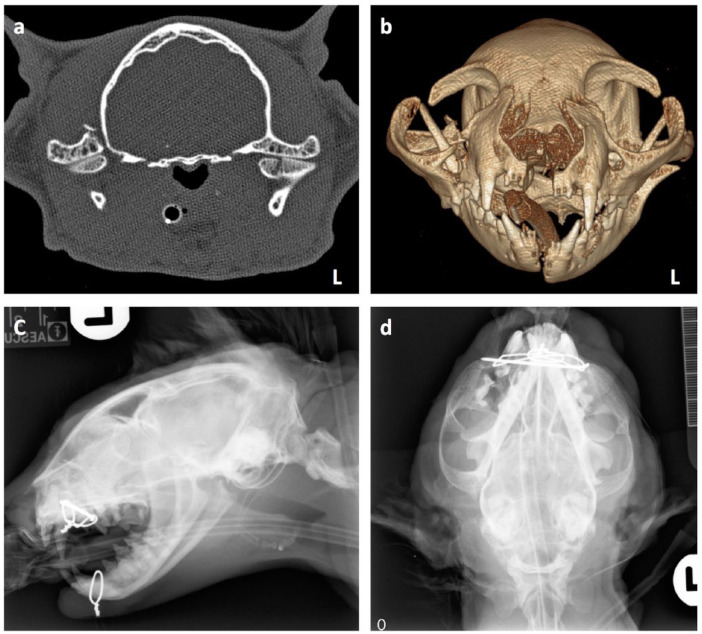
Fractures were seen in a single bone of the skull in eight cats (11%) and in multiple bones in 67 cats (89%) (Figure 1a,b). The frequency and configuration of fractures are outlined in Table 1. Fractures of the mandibular (body and symphysis), upper jaw (internal and external) and craniofacial regions each occurred in approximately 70% of cats, with caudal skull fractures less frequently seen (n = 7; 9%). Eighty percent of mandibular fractures and 81% of TMJ injuries were unilateral, whereas the majority of upper jaw fractures were bilateral (64%). TMJ injuries were categorised as luxations (n = 10; 24%) and fractures (n = 27; 64%) (Figure 1a), with both luxation and fracture seen in five cats with TMJ injuries (12%). Hard palate defects occurred in 34 cats (45%) with an additional soft palate defect in one cat (1%).
Figure 1.
(a) Transverse 0.75 mm CT slice at the level of the temporomandibular joints. There is fracture of the temporal process of zygoma on the right and a left mandibular condyle (vertical fracture, medial one-third). (b) Three-dimensional volume-rendered CT shows mandibular and maxillary symphyseal separations, bilateral maxillary fractures, right temporal process of the zygoma fracture, bilateral frontal-maxillary suture interface fracture and right fracture of the orbital lamella of frontal bone, with fracture through the maxillary arcade. (c) Lateral projection and (d) ventrodorsal skull radiographs postoperatively showing placement of cerclage wire around the mandible caudal to the canine teeth, K-wire placed across the maxillary bones and the maxilla further stabilised with a figure-of-eight tension band wire. The right zygomatic arch is fractured and there is widening of the maxillary incisors, compatible with the fractures identified on CT. Left mandibular condyle is absent; the mandibular fossa is empty and the retroarticular process is clearly visible
Table 1.
Skull fracture classification, indicating the number of cats with each fracture type and fracture configuration, and showing the number of each fracture type by location
| Total | Bilateral | Left | Right | Midline | |
|---|---|---|---|---|---|
| Mandibular | 54 (72) | 11 (20) | 18 (33) | 25 (46) | NA |
| Mandibular symphysis | 53 (71) | NA | NA | NA | 53 (100) |
| External upper jaw | 55 (73) | 35 (64) | 8 (15) | 7 (13) | 25 (45) |
| Internal upper jaw | 53 (71) | 24 (45) | 9 (17) | 6 (11) | 41 (77) |
| TMJ | 42 (56) | 8 (19) | 13 (31) | 21 (50) | NA |
| Craniofacial | 57 (76) | 38 (67) | 11 (19) | 8 (14) | 0 (0) |
| Caudal skull | 7 (9) | NA | NA | NA | 7 (100) |
Data are n (%)
TMJ = temporomandibular joint; NA = not applicable
The fracture configurations seen with each type of trauma are detailed in Table 2. RTAs caused fractures of multiple regions, with mandibular, upper jaw and craniofacial fractures occurring most frequently. Bites also caused fractures in multiple regions, whereas falling from a height only affected the mandibular body and internal upper jaw. In those cats with gun-shot injuries, only mandibular and symphyseal fractures were reported.
Table 2.
Skull fracture aetiology, showing the number of fractures seen with each trauma type
| RTA | Fall | Bite | Shot | |
|---|---|---|---|---|
| Mandibular | 47 (70) | 2 (100) | 4 (80) | 1 (100) |
| Mandibular symphysis | 49 (73) | 0 (0) | 3 (60) | 1 (100) |
| External upper jaw | 53 (79) | 0 (0) | 2 (40) | 0 (0) |
| Internal upper jaw | 51 (76) | 2 (100) | 1 (20) | 0 (0) |
| TMJ | 40 (60) | 0 (0) | 2 (40) | 0 (0) |
| Craniofacial | 56 (84) | 0 (0) | 1 (20) | 0 (0) |
| Caudal skull | 6 (9) | 0 (0) | 1 (20) | 0 (0) |
Data are n (%)
RTA = road traffic accident; TMJ = temporomandibular joint
A variety of techniques were used for management of skull fractures. Three cats (4%) were euthanased before treatment of the skull fractures was performed; two owing to the severity of their concurrent injuries; and one developed congestive heart failure and pleural effusion following general anaesthesia for CT. Of the 53 cats with mandibular symphyseal separations, 44 (83%) were stabilised with cerclage wire (n = 36; 82%) (Figure 1c,d) or an encircling polydioxanone suture (n = 8; 18%). Thirty-five (47%) cats with fractures affecting the other regions of the skull were conservatively managed and surgery was performed in the other 35 cats. Surgical fixation included maxillomandibular (n = 10; 29%), maxillary (n = 1; 3%) or mandibular (n = 3; 9%) ESF, BEARD (n = 2; 6%), reconstruction of fragments with pins, screws and wire (n = 4; 11%), hard palate reconstruction (n = 11; 31%), and management of TMJ fractures or luxations (n = 8; 23%).
Table 3 shows the management of fractures of each region of the skull. Cranial and caudal skull fractures were all managed conservatively, although surgery was performed in some, when in combination with other skull fractures. Maxillomandibular ESFs and BEARDs were used for caudal mandibular fractures and TMJ injuries to provide stability between the mandible and the maxilla during healing. Mandibular ESFs were used in three cats with bilateral mandibular fractures and a maxillary ESF was used in one cat with bilateral maxilla fractures and a left TMJ fracture. Hard palate reconstruction was performed in 27% of the 41 cats with hard palate defects, using transmaxillary K-wire and tension band (four cats) (Figure 1c,d) or polydioxanone sutures (seven cats), with the remainder managed conservatively.
Table 3.
Management of skull fractures, showing the number of each fracture configuration treated with particular techniques
| Conservative | ESF | BEARD | Reconstruction (pins/screws/K-wires/suture) | |
|---|---|---|---|---|
| Mandibular | 34 (67) | 13 (25) | 1 (2) | 4 (8) |
| External upper jaw | 43 (82) | 9 (17) | 0 (0) | 0 (0) |
| Internal upper jaw | 28 (56) | 11 (22) | 0 (0) | 11 (22) |
| Craniofacial | 54 (100) | 0 (0) | 0 (0) | 0 (0) |
| Caudal skull | 6 (100) | 0 (0) | 0 (0) | 0 (0) |
Data are n (%)
ESF = external skeletal fixation; BEARD = bignathic encircling and retaining device
TMJ fracture luxations were managed surgically in eight cats (19%) by either open surgical reduction (n = 4; 50%) or excision arthroplasty (n = 4; 50%) (Figure 1c,d). A maxillomandibular ESF was applied in seven of these cats and a BEARD in the other. An oesophagostomy tube was placed in 48 cats (64%).
Concurrent injuries
Concurrent injuries were seen in 57 cats (76%), with 30 of these (53%) experiencing multiple injuries. Cats suffered ophthalmological (n = 30; 40%), soft tissue (n = 12; 16%), orthopaedic (n = 9; 12%), neurological (n = 22; 29%) and intrathoracic (n = 22; 29%) injuries. Concurrent orthopaedic injuries included elbow and radiocarpal luxation (one cat), scapular fractures (two cats), coxofemoral luxation (one cat), pelvic fractures including sacroiliac luxation, acetabular, pubic and ischial fractures (five cats), and femoral head fracture (one cat). Dental trauma, including displacement and fracture of teeth, occurred in 16 cats (21%).
RTAs were the only cause of multiple concurrent injuries. No concurrent injuries occurred in the cat that was shot, or in the three cats that were bitten (60%), or one of the two cats that fell from a height (50%). Of the 57 cats with concurrent injuries, 26 (46%) were managed conservatively. Two cats (3.5%) were euthanased owing to the severity of their injuries; one had severe traumatic brain injury and the other had an extensive tongue laceration alongside multiple bilateral fractures of all regions of the skull. Surgical treatment was performed in the other 27 cats (47%) and medical management in two cats (3%); one had thoracocentesis for bilateral pneumothorax and pleural effusion, and the other had increased intracranial pressure, which was treated with mannitol.
Follow-up, complications and mortality
Median hospitalisation time was 5 days (range 0–17 days). Six cats died prior to discharge (8%): two were euthanased owing to the severity of their injuries; one developed congestive heart failure and pleural effusion following general anaesthesia; two suffered respiratory arrest on recovery from general anaesthesia for surgical management of skull fractures; and one suffered respiratory arrest following carotid artery laceration and ligation during placement of an oesophagostomy tube. This last cat was excluded from statistical analysis as its death was secondary to an iatrogenic injury rather than the original trauma. No variables were found to be associated with a change in mortality rate.
Of the 69 cats that survived to discharge, 34 (49%) were re-examined at our institution, with repeat skull imaging in 14. Median follow-up was 37 days (range 7–64 days). In cats with mandibular cerclage, 21 (48%) were removed at our institution (20 wires [56% of cerclage wires placed] and one PDS suture [13% of cerclage sutures]), with a median time to removal of 51 days (range 29–76 days).
Complications related to management were reported in 16 cats (21%), including implant loosening or failure (n = 6; 8%), mild non-clinical malocclusion (n = 4; 5%), anaesthetic complications (n = 4; 5%), carotid artery laceration during oesophagostomy tube placement (n = 1; 1%) and postoperative vomiting requiring BEARD removal to reduce risk of aspiration (n = 1; 1%). Aspiration pneumonia was identified on CT at re-examination in one cat, although no associated clinical signs were noted. This cat was treated with amoxicillin-clavulanate (20 mg/kg q12h PO) for 2 weeks. All anaesthetic complications resulted in cardiopulmonary arrest or euthanasia. Both cats that had a BEARD placed developed complications; in one, the BEARD failed to maintain jaw alignment so was replaced with a maxillomandibular ESF, and the other developed vomiting 2 days postoperatively, so the BEARD was removed to reduce the risk of aspiration and subsequently replaced once vomiting resolved. No other complications required additional treatment or a change in fracture management technique.
Age at presentation (P = 0.03) and the presence of internal upper jaw fractures (P = 0.03), concurrent injuries (P = 0.04) and ophthalmological injuries (P = 0.04) were the only variables with a P value <0.1 after the univariable logistic regression analysis, so these were entered into the multivariable analysis. Following multivariable logistic regression analysis with backwards elimination, increasing age (P = 0.04) and the presence of internal upper jaw fractures (P = 0.03) were found to be significantly associated with the overall complication rate.
Discussion
This is the first study to describe skull fractures and concurrent injuries following head trauma in a large number of cats and to evaluate their management. The mean age of the cats was 4.8 years, consistent with previous reports, and males were over-represented,9,11,13 although a recent study showed that cats between 7 months and 2 years old have the highest risk of RTAs. 24 RTAs were the most common cause of head trauma, with fewer falls and bite wounds observed than reported previously.6–8 Falling from a height occurred less frequently as a cause of head trauma in our study than previously described,8,13,14 possibly due to high-rise housing of indoor cats being uncommon in the UK. Also, some cats that suffered a fall from a height may only have a mandibular symphyseal separation 9 and hence they may have been managed without performing CT, although the routine approach is to give them a CT them for occult injuries at this institution.
Mandibular, upper jaw (internal and external) and craniofacial fractures all occurred in 70–75% cats, with TMJ injuries being common and caudal skull fractures being uncommon (9% cats), consistent with a recent study categorising feline craniomaxillofacial fractures following trauma. 23 Following RTAs, fractures were observed in similar numbers across multiple regions of the skull. Bites and gunshots would be expected to affect different regions of the skull depending on the area targeted, although there were too few cats affected by these trauma types in our study to draw definitive conclusions about fracture configuration. Falls from a height often affect the mandible, palate and TMJ, as cats tend to rotate in falls so as to land on their paws, and hence the mandible may impact on the ground as they land.9–11,13 The two cats that suffered a fall in our study both had injuries to the mandible and palate, although neither had TMJ injury.
Concurrent injuries were more likely with RTAs and ophthalmic injuries were most common, followed by intrathoracic and neurological injuries. This is consistent with high-energy RTAs and the pattern suggests cats being ‘clipped’ at their front, rather than at their hind, with associated pelvic fracture patterns and soft tissue injuries. 25 Importantly, this demonstrates the need to make careful ophthalmic, neurological and thoracic reviews in cats presenting with head trauma. Only two of the cats with concurrent injuries were euthanased as a direct result of the severity of these injuries. Of those remaining, 53% required surgical or medical management of their concurrent injuries in addition to management of the skull fractures, whereas 47% could be conservatively managed. These factors are important to consider when discussing recovery time, postoperative care, cost and overall prognosis with clients in these cases.
The majority of mandibular symphyseal separations were managed surgically. For all other fractures, there was an equal split between conservative and surgical management. For most cats managed surgically, the objective was to provide indirect fracture stabilisation and maintenance of dental occlusion during fracture healing. Open reduction and internal fixation is reported for some skull fractures in cats, 21 but the small fragments involved makes the technique challenging, and there is a high risk of damage to tooth roots and neurovascular structures.14,26 Application of a maxillomandibular ESF also requires careful pin positioning to avoid damage to tooth roots and bone resorption secondary to heat necrosis. This study was unable to assess whether implants interfered with tooth roots as postoperative radiographs were not assessed. Interdental bonding and composite splints could be an alternative that avoids the risk of tooth root or neurovascular damage14,18 but may provide weaker fixation than ESFs. 27
The degree of opening at the rostral mouth is important with maxillomandibular ESFs, as it can affect the ability to lap postoperatively, and, as with BEARDs, there is a risk of respiratory obstruction or aspiration if regurgitation or vomiting occurs.17,19 Two cats were affected by this in our study; one cat with a BEARD developed vomiting postoperatively, so the BEARD was removed and replaced when it resolved, and aspiration pneumonia was identified on CT at re-examination in another cat with a maxillomandibular ESF, although without clinical signs.
TMJ injuries were observed in 56% of the cats in this study, and were usually unilateral, which is consistent with the prevalence of TMJ injury previously reported in cats with maxillofacial trauma.13,23 All TMJ luxations were managed with closed reduction under sedation or general anaesthesia. TMJ ankylosis has been reported as a potential complication following intra-articular TMJ lesions if managed conservatively, which then requires excision arthroplasty.13,18 In our study any cats with comminuted, intra-articular fractures or those severely affecting joint function were treated with excision arthroplasty at the time of diagnosis, instead of pursuing conservative management initially. This appeared to be well tolerated by these cats, consistent with previous findings. 13 TMJ ankylosis was not identified in any cats in this population, although more cases may have been identified with a longer follow-up period.
Previously reported complications associated with jaw fractures include dental trauma, malocclusion, oronasal fistulas, osteomyelitis, delayed or non-union, implant failure, soft tissue swelling, inability to eat, and abnormalities in dental eruption and development.14,16,17,19 The complications related to skull fractures in our study were loosening of implants (cerclage wires, BEARD or ESF pins), mild malocclusion and vomiting requiring removal of maxillomandibular fixation to minimise the risk of aspiration. Not all cats had repeated skull imaging, so delayed or non-union of fractures may have occurred but not been detected, although if present these did not cause any clinically apparent problems. General anaesthetic complications resulting in cardiopulmonary arrest or euthanasia occurred in three cats. This is unexpectedly high and may relate to brain injury associated with head trauma and the loss of protective mechanisms maintaining intracranial blood flow during periods of hypotension under general anaesthesia; 28 however, no particular risk factors were identified here.
Overall, older cats were found to be at greater risk of developing complications, which may relate to the severity of concurrent injuries, or the presence of other unidentified comorbidities. Full haematology and biochemistry panels were not available for all of these cats, but a limited trauma panel (including blood gases, electrolytes, creatinine and total bilirubin) was run at initial presentation with no significant abnormalities detected. Internal upper jaw fractures were also associated with an increased risk of complications. This may be because fractures of the palatine bone and midline hard palate separations cause jaw instability with changes to the position of the dental arcade and are therefore more likely to result in malocclusion.
The retrospective nature of the study introduces potential bias, particularly regarding data recording at the time of presentation and surgery and for clinical follow-up; not all cats were re-examined at our institution, so some complications may be under-reported. However, the epidemiology of these fractures as reported from CT represents the most accurate analysis to date. Long-term follow-up was not performed, so no conclusions can be made about long-term outcome and prognosis. Detailed analysis of individual techniques for treatment of each fracture type is beyond the scope of this study, so further research is required to determine the most appropriate management options for fractures in different regions of the skull.
Conclusions
RTAs are the most common cause of skull fractures in cats, and this type of trauma causes fractures in multiple areas of the skull. It is important to be aware of the high level of concurrent injuries in RTA head trauma cats, particularly ophthalmic, neurological and thoracic pathology. Mandibular fractures and, notably, symphyseal separations were the most common injuries seen, but usually in combination with other skull fractures. Craniofacial and upper jaw fractures were most commonly bilateral in their configurations, whereas TMJ injuries were more likely to be unilateral, and caudal skull fractures were not very common. An increased risk of complications, such as implant loosening and malocclusion, was seen with fractures of the internal upper jaw, although the reason for this could not be identified in this study. Further research is needed to direct treatment recommendations for different fracture types.
Footnotes
Accepted: 23 November 2018
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Richard L Meeson  https://orcid.org/0000-0002-8972-7067
https://orcid.org/0000-0002-8972-7067
References
- 1. Rochlitz I. Study of factors that may predispose domestic cats to road traffic accidents: part 2. Vet Rec 2003; 153: 585–588. [DOI] [PubMed] [Google Scholar]
- 2. Kolata RJ. Trauma in dogs and cats: an overview. Vet Clin North Am Small Anim Pract 1980; 10: 515–522. [DOI] [PubMed] [Google Scholar]
- 3. Wunderlin N, Amort K, Wigger A, et al. Computed tomography in cats with craniofacial trauma with regard to maxillary and orbital fractures. Tierarztl Prax Ausg K Kleintiere Heimtiere 2012; 40: 341–349. [PubMed] [Google Scholar]
- 4. Wong WT. A survey of fractures in the dog and cat in Malaysia. Vet Rec 1984; 115: 273–274. [DOI] [PubMed] [Google Scholar]
- 5. Phillips IR. A survey of fractures in the dog and cat. J Small Anim Pract 1979; 20: 661–674. [DOI] [PubMed] [Google Scholar]
- 6. Rockar RA, Drobatz KS, Shofer FS. Development of a scoring system for the veterinary trauma patient. J Vet Emerg Crit Care 1994; 4: 77–83. [Google Scholar]
- 7. Umphlet RC, Johnson AL. Mandibular fractures in the cat. A retrospective study. Vet Surg 1988; 17: 333–337. [DOI] [PubMed] [Google Scholar]
- 8. Battier B, Montavon PM. A retrospective clinical study of the fractures and luxations of the mandible in the cat [article in French]. Schweiz Arch Tierheilkd 1989; 131: 77–80, 87–94. [PubMed] [Google Scholar]
- 9. Vnuk D, Pirkić B, Matićić D, et al. Feline high-rise syndrome: 119 cases (1998–2001). J Feline Med Surg 2004; 6: 305–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Whitney WO, Mehlhaff CJ. High-rise syndrome in cats. J Am Vet Med Assoc 1987; 191: 1399–1403. [PubMed] [Google Scholar]
- 11. Bonner SE, Reiter AM, Lewis JR. Orofacial manifestations of high-rise syndrome in cats: a retrospective study of 84 cases. J Vet Dent 2012; 29: 10–18. [DOI] [PubMed] [Google Scholar]
- 12. Kuo KW, Bacek LM, Taylor AR. Head trauma. Vet Clin North Am Small Anim Pract 2018; 48: 111–128. [DOI] [PubMed] [Google Scholar]
- 13. Çetinkaya MA. Temporomandibular joint injuries and ankylosis in the cat. Vet Comp Orthop Traumatol 2012; 25: 366–374. [DOI] [PubMed] [Google Scholar]
- 14. Legendre L. Maxillofacial fracture repairs. Vet Clin North Am Small Anim Pract 2005; 35: 985–1008. [DOI] [PubMed] [Google Scholar]
- 15. Woodbridge N, Owen M. Feline mandibular fractures. J Feline Med Surg 2013; 15: 211–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zacher AM, Marretta SM. Oral and maxillofacial surgery in dogs and cats. Vet Clin North Am Small Anim Pract 2013; 43: 609–649. [DOI] [PubMed] [Google Scholar]
- 17. Moores AP. Maxillomandibular external skeletal fixation in five cats with caudal jaw trauma. J Small Anim Pract 2011; 52: 38–41. [DOI] [PubMed] [Google Scholar]
- 18. Soukup JW, Snyder CJ. Traumatic dentoalveolar and maxillofacial injuries in cats. J Feline Med Surg 2014; 16: 915–927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nicholson I, Wyatt J, Radke H, et al. Treatment of caudal mandibular fracture and temporomandibular joint fracture-luxation using a bi-gnathic encircling and retaining device. Vet Comp Orthop Traumatol 2010; 23: 102–108. [DOI] [PubMed] [Google Scholar]
- 20. Adamantos S, Garosi L. Head trauma in the cat: 1. Assessment and management of craniofacial injury. J Feline Med Surg 2011; 13: 806–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bilgili H, Kurum B. Treatment of fractures of the mandible and maxilla by mini titanium plate fixation systems in dogs and cats. Aust Vet J 2003; 81: 671–673. [DOI] [PubMed] [Google Scholar]
- 22. Bar-Am Y, Pollard RE, Kass PH, et al. The diagnostic yield of conventional radiographs and computed tomography in dogs and cats with maxillofacial trauma. Vet Surg 2008; 37: 294–299. [DOI] [PubMed] [Google Scholar]
- 23. Tundo I, Southerden P, Perry A, et al. Location and distribution of craniomaxillofacial fractures in 45 cats presented for the treatment of head trauma. J Feline Med Surg 2019; 21: 322–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rochlitz I. Study of factors that may predispose domestic cats to road traffic accidents: part 1. Vet Rec 2003; 153: 549–553. [DOI] [PubMed] [Google Scholar]
- 25. Meeson RL, Geddes AT. Management and long-term outcome of pelvic fractures: a retrospective study of 43 cats. J Feline Med Surg 2017; 19: 36–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kern DA, Smith MM, Stevenson S, et al. Evaluation of three fixation techniques for repair of mandibular fractures in dogs. J Am Vet Med Assoc 1995; 206: 1883–1890. [PubMed] [Google Scholar]
- 27. Bennett JW, Kapatkin AS, Marretta SM. Dental composite for the fixation of mandibular fractures and luxations in 11 cats and 6 dogs. Vet Surg 1994; 23: 190–194. [DOI] [PubMed] [Google Scholar]
- 28. Armitage-Chan EA, Wetmore LA, Chan DL. Anesthetic management of the head trauma patient. J Vet Emerg Crit Care 2007; 17: 5–14. [Google Scholar]