Abstract
Objectives
The purpose of this study was to evaluate the effects of oral trazodone on echocardiographic variables, heart rate (HR) and blood pressure (BP) in healthy cats.
Methods
Client-owned domestic cats between 2 and 8 years of age were recruited. Cats were considered healthy based on physical examination, complete blood count, blood chemistry profile, urinalysis, total thyroxine concentration, non-invasive BP measurement by Doppler method and a screening transthoracic echocardiogram with simultaneous electrocardiogram. Echocardiographic variables assessed pre-trazodone and 90–120 mins post-trazodone (50 mg PO) included left ventricular internal diameter in systole and diastole, interventricular septal and left ventricular free-wall thickness in systole and diastole, left atrial size, left auricular function and left ventricular diastolic function assessed by spectral Doppler transmitral and pulmonary venous flow velocities, and tissue Doppler profiles. Mean echocardiographic and hemodynamic variables were calculated for pre- and post-trazodone examinations for each cat. Pre- and post-trazodone variables were analyzed with a paired t-test with significance set at P <0.05.
Results
Twelve healthy cats were evaluated. Trazodone was administered to all cats and a sedative effect was observed. There were no clinically significant differences in any echocardiographic variables post-trazodone administration. Systolic BP was significantly decreased after trazodone (P = 0.001) with no significant change in HR.
Conclusions and relevance
Trazodone did not alter echocardiographic variables, in a clinically relevant manner, in this group of healthy cats. Trazodone may aid in obtaining transthoracic echocardiograms without affecting HR or echocardiographic variables but may significantly lower BP in healthy cats.
Keywords: Blood pressure, cardiac, echocardiogram, sedation, ultrasound
Introduction
Stress and transportation for veterinary visits can affect comprehensive evaluations of cats. 1 Oral anxiolytic drugs are available by prescription; however, all have disadvantages, limiting their clinical utility.2,3 Without the ability to reliably decrease anxiety in cats via oral at-home drugs, veterinarians often rely on parenterally administered sedative drugs. While these drugs can facilitate advanced diagnostics, including echocardiography, their dose-dependent effects on hemodynamic and echocardiographic variables can be profound.4–8
Trazodone hydrochloride, an oral serotonin antagonist and reuptake inhibitor, has been shown to decrease anxiety in cats when administered prior to veterinary visits and is well tolerated. 9 Identifying a safe, at-home administrable sedative/anxiolytic that does not significantly affect cardiovascular function is ideal for cats, particularly if their cardiovascular health status in unknown. Trazodone is a promising drug for alleviating anxiety in cats. Trazodone has been reported to produce adrenergic receptor blocking effects, suggesting that it may affect the cardiovascular system. Nevertheless, its effects on echocardiographic and hemodynamic variables in cats have not been reported. The purpose of this study was to evaluate the effects of oral trazodone on echocardiographic variables, heart rate (HR) and blood pressure (BP) in healthy cats. We hypothesized that oral trazodone would affect echocardiographic and hemodynamic variables in healthy cats.
Materials and methods
Animals
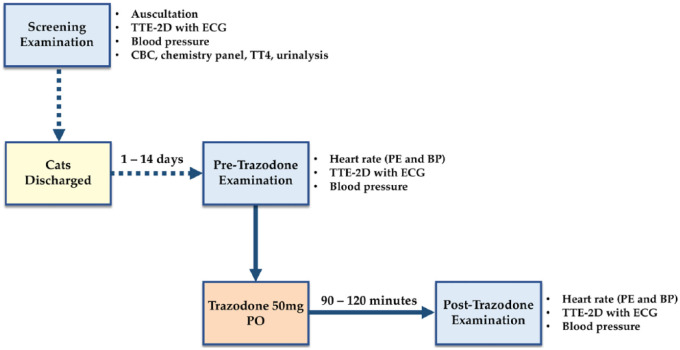
This study was approved by the Institutional Animal Care and Use Committee at the University of Illinois Urbana-Champaign. Twelve adult cats, between 2 and 8 years of age, were recruited and client consent was obtained for all cats prior to enrollment. A summary of the study protocol is outlined in Figure 1. Each cat was deemed healthy based on physical examination, complete blood count, blood chemistry profile, urinalysis, total thyroxine concentration and non-invasive BP measurement by the Doppler method. Additionally, a non-sedated transthoracic two-dimensional echocardiographic (TTE-2D) examination, with a simultaneous electrocardiogram (ECG), was performed. Cats were excluded from the study if they had any structural or functional abnormalities noted on TTE-2D examination, ECG or abnormalities on the screening tests. Cats that met the inclusion criteria returned for a separate visit 1–14 days later. At this later visit, cats were admitted to hospital through the cardiology service and housed in a quiet dedicated ward prior to obtaining a baseline TTE-2D examination.
Figure 1.
Summary of study events in chronological order. BP = blood pressure; ECG = electrocardiogram; CBC = complete blood count; PE = physical examination; TT4 = total thyroxine concentration; TTE-2D = transthoracic two-dimensional echocardiogram
Echocardiogram
All TTE-2D examinations were performed by a single investigator (RCF), using a GE Vivid E9 ultrasonographic scanner, equipped with a 12 MHz phased-array transducer with simultaneous ECG monitoring. Cats were positioned in right, then left lateral recumbency on a raised table with a central opening. All images and cine loops were digitally stored and transferred to a separate EchoPAC workstation equipped with BT13 software for offline analysis. Each echocardiographic study was analyzed by the same observer (RCF) in random order. Each measurement was repeated five times and the mean values were used for statistical analysis.
Assessment of left ventricular (LV) size and function was performed using standard right parasternal short-axis and long-axis views, and a left apical parasternal long-axis view. 10 Variables measured included LV internal dimensions at end-diastole (LVIDd) and end-systole (LVIDs), LV free-wall thickness at end diastole and end systole, and interventricular septal thickness at end diastole and end systole. The LV luminal area at end diastole (LVAd) and end-systole (LVAs) were measured from the right parasternal short-axis images at the level of the chordae tendineae. The LV fractional shortening (LV – FS = [LVIDd–LVIDs]/LVIDd × 100%) and LV fractional area change (LV – FAC = [LVAd–LVAs]/LVAd × 100%) were calculated.
Assessment of left atrial (LA) size was performed from standard right parasternal long-axis and short-axis views. Variables measured included LA diameter (LASAX) and aortic diameter (Ao) in diastole measured from a right parasternal short-axis view and the ratio between LASAX to Ao (LA:Ao) was calculated. Additionally, the maximum LA septal-to-free-wall dimension (LADMax) was measured from the right parasternal long-axis four-chamber view. LA appendage velocities, emptying (LAA emptying) and filling (LAA filling), were recorded using pulsed-wave Doppler from the left cranial short-axis view.
Transmitral and pulmonary venous flow velocities were recorded using pulsed-wave Doppler from a left apical parasternal long-axis view. Variables measured included isovolumic relaxation time, peak velocity of early diastolic transmitral flow (E), deceleration time of early diastolic transmitral flow, peak velocity of late diastolic transmitral flow (A), peak velocity of pulmonary vein systolic flow, peak velocity of pulmonary vein diastolic flow, peak velocity of pulmonary vein reversal flow at atrial contraction (PVA) and duration of pulmonary vein reversal flow at atrial contraction. Ratio between Peak E to Peak A (E:A) was calculated.
Tissue Doppler imaging was performed with the highest available transducer frequency to record the velocity of lateral mitral annular motion from the left apical parasternal long-axis view. The following variables were measured: peak early diastolic velocity, peak late diastolic velocity and peak systolic velocity.
BP
All cats had an indirect systemic BP evaluated via the Doppler method using a previously reported protocol. 11 Blood pressure was obtained halfway through the echocardiographic examinations, prior to switching lateral recumbency, during pre- and post-trazodone examinations to maintain consistency. Patients were positioned in right lateral recumbency using gentle manual restraint. An appropriately sized cuff, 30–40% of the circumference of the antebrachium, was used on the left forelimb and secured with a Velcro fastener. Three consecutive measurements, with <5 mmHg variance, were obtained and recorded.
Trazodone administration
Baseline echocardiograms were performed for each cat without sedation. Subsequently, each cat was administered one 50 mg tablet of trazodone PO and placed in a quiet room. Cats were re-imaged 90–120 mins after sedation, based on the previously reported peak sedative effect of orally administered trazodone. 12
Sedative effect
The degree of sedation caused by trazodone was subjectively evaluated by the same observer (RCF). Subjective assessment of post-trazodone behavior, compliance with restraint and spontaneous mobility was compared with baseline (pre-trazodone) parameters.
Statistical analysis
Statistical analysis was performed with commercially available software and SAS version 9.4. Means were calculated for each cat by examination. Distribution of variables was tested for normality using Shapiro–Wilk and Anderson–Darling tests at the alpha = 0.05 level. Data were evaluated using a paired t-test and a Wilcoxon signed-rank test of the null hypothesis and significance level was set at P <0.05.
Results
Thirteen cats were initially recruited. One cat was excluded during the screening TTE-2D examination owing to poor compliance and aggressive behavior. The remaining 12 cats were healthy, domestic cats (seven spayed females, five castrated males) with a median age of 3.3 years (range 2–7 years), mean ± SD body weight of 4.7 ± 1.0 kg (range 3.0–6.3 kg) and median body condition score of 5 (range 4–7). The median time from screening examination to pre- and post-trazodone examinations was 7.5 days (range 1–12 days). The mean dose of trazodone was 11.2 ± 2.8 mg/kg (range 7.9–16.6) and the mean time to post-trazodone examination was 96.3 ± 3.9 mins (range 92–105 mins). Although not objectively quantified in our study, a mild-to-moderate sedative effect was observed in all cats post-trazodone facilitating restraint for TTE-2D, ECG and BP evaluation.
Results for variables of LV size and LV systolic function, LA size and LAA function and LV diastolic function are displayed in Tables 1, 2 and 3, respectively. The only significant differences between pre- and post-trazodone variables (paired t-test) were mean LASAX measured in the right parasternal short-axis view, mean E:A and mean PVA. The mean increase in LASAX after trazodone administration was 0.06 cm (P = 0.035), whereas LA:Ao in right parasternal short-axis view and LADMax measured from the right parasternal long-axis view were not significantly different post-trazodone. Mean E:A was increased by 0.15 (P = 0.046) post-trazodone, whereas peak E and A velocities were not statistically different and reduced by 0.03 m/s (P = 0.447) and 0.06 m/s (P = 0.068), respectively. Mean PVA was increased by 0.05 m/s (P = 0.019), whereas all other pulmonary venous Doppler flows were not statistically different.
Table 1.
Echocardiographic variables of left ventricular size and systolic function pre- and post-trazodone in 12 healthy cats
| Variable | Pre-trazodone | Post-trazodone | P value |
|---|---|---|---|
| LVIDd (mm) | 15.3 ± 1.1 | 15.6 ± 1.7 | 0.403 |
| LVIDs (mm) | 7.8 ± 1.2 | 7.5 ± 1.2 | 0.353 |
| LV-FS (%) | 48.6 ± 8.1 | 51.4 ± 7.7 | 0.265 |
| LVAd (cm2) | 2.3 ± 0.3 | 2.4 ± 0.4 | 0.230 |
| LVAs (cm2) | 0.7 ± 0.2 | 0.63 ± 0.2 | 0.093 |
| LV-FAC (%) | 69.4 ± 6.3 | 73.0 ± 6.8 | 0.066 |
| IVSd (mm) | 4.1 ± 0.7 | 4.2 ± 0.6 | 0.204 |
| IVSs (mm) | 6.4 ± 0.8 | 6.6 ± 1.0 | 0.083 |
| LVFWd (mm) | 4.3 ± 0.7 | 4.4 ± 0.7 | 0.082 |
| LVFWs (mm) | 7.0 ± 0.8 | 7.1 ± 0.7 | 0.331 |
| AV max (m/s) | 0.90 ± 0.18 | 0.90 ± 0.14 | 0.994 |
| S′ (m/s) | 0.06 ± 0.01 | 0.06 ± 0.01 | 0.331 |
Data are mean ± SD
LVIDd = left ventricular internal dimension in diastole; LVIDs = left ventricular internal dimension in systole; LV-FS = left ventricular fractional shortening; LVAd = left ventricular internal area in diastole; LVAs = left ventricular internal area in systole; LV-FAC = left ventricular fractional area change; IVSd = interventricular septal thickness in diastole; IVSs = interventricular septal thickness in systole; LVFWd = left ventricular free-wall thickness in diastole; LVFWs = left ventricular free-wall thickness in systole; AV max = peak aortic flow velocity; S’ = peak systolic velocity of lateral mitral annulus
Table 2.
Echocardiographic variables of left atrial size and left auricular function pre- and post-trazodone in 12 healthy cats
| Variable | Pre-trazodone | Post-trazodone | P value |
|---|---|---|---|
| LADMax (mm) | 13.5 ± 1.0 | 13.6 ± 1.0 | 0.798 |
| LASAX (cm) | 1.19 ± 0.07 | 1.25 ± 0.06 | 0.024* |
| Ao (cm) | 0.93 ± 0.09 | 0.95 ± 0.08 | 0.411 |
| LA:Ao | 1.28 ± 0.13 | 1.33 ± 0.12 | 0.294 |
| LAA emptying (m/s) | 0.48 ± 0.09 | 0.45 ± 0.09 | 0.297 |
| LAA filling (m/s) | 0.47 ± 0.10 | 0.45 ± 0.07 | 0.526 |
Data are mean ± SD
Difference between pre- and post-trazodone was statistically significant
LADMax = maximum left atrial septal-to-free wall dimension in right parasternal long-axis four-chamber view; LASAX = left atrium short-axis diameter in diastole; Ao = aortic short-axis dimension in diastole; LA:Ao = ratio between LASAX and Ao; LAA emptying = peak velocity blood flow leaving the left auricular appendage during atrial contraction; LAA filling = peak velocity of blood flow entering the left auricular appendage after atrial contraction
Table 3.
Echocardiographic variables of left ventricular diastolic function pre- and post-trazodone in 12 healthy cats
| Variable | Pre-trazodone | Post-trazodone | P value |
|---|---|---|---|
| E (m/s) | 0.69 ± 0.14 | 0.66 ± 0.14 | 0.447 |
| A (m/s) | 0.53 ± 0.09 | 0.47 ± 0.12 | 0.068 |
| E:A | 1.32 ± 0.25 | 1.47 ± 0.31 | 0.046* |
| DTE (m/s) | 79.0 ± 14.0 | 74.5 ± 13.9 | 0.247 |
| DTE slope (m/s2) | 9.3 ± 2.6 | 9.3 ± 3.5 | 0.962 |
| E’ (m/s) | 0.08 ± 0.02 | 0.09 ± 0.01 | 0.199 |
| A’ (m/s) | 0.05 ± 0.01 | 0.49 ± 0.01 | 0.221 |
| IVRT (ms) | 51.5 ± 7.0 | 52.8 ± 6.5 | 0.655 |
| PVS (m/s) | 0.51 ± 0.10 | 0.51 ± 0.13 | 0.788 |
| PVD (m/s) | 0.41 ± 0.08 | 0.43 ± 0.09 | 0.318 |
| PVA (m/s) | 0.23 ± 0.04 | 0.28 ± 0.07 | 0.019* |
| PVAdur (ms) | 53.4 ± 6.4 | 50.5 ± 9.4 | 0.287 |
Data are mean ± SD
Difference between pre- and post-trazodone was statistically significant
E = peak velocity of early diastolic transmitral flow; A = peak velocity of late diastolic transmitral flow; E:A = ratio between E and A; DTE = deceleration time of early diastolic transmitral flow; DTE slope = slope of DTE; E’ = peak early diastolic velocity of lateral mitral annulus; A’ = peak late diastolic velocity of lateral mitral annulus; IVRT = isovolumetric relaxation time; PVS = peak velocity of pulmonary vein systolic flow; PVD = peak velocity of pulmonary vein diastolic flow; PVA = peak velocity of pulmonary vein atrial reversal flow; PVAdur = duration of the PVA
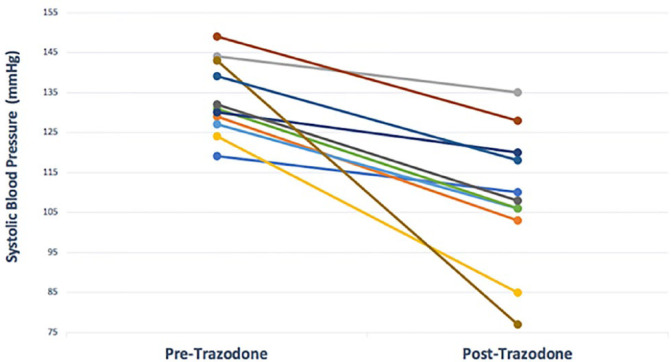
Results for HR and BP variables are displayed in Table 4. HR, obtained during the physical examination and during BP measurement, was not significantly decreased after trazodone administration. Trazodone decreased systolic BP in all cats and the overall effect was significant (P = 0.001). The mean ± SD reduction in systolic BP post-trazodone was 25 ± 16 mmHg (range 9–66 mmHg). BP was inadvertently not recorded for one cat post-trazodone and this cat has been censored from the data. Figure 2 displays the individual changes in BP for the remaining 11 cats.
Table 4.
Hemodynamic variables pre- and post-trazodone in 11 healthy cats
| Variable | Baseline | Post-trazodone | P value |
|---|---|---|---|
| HR PE | 195 ± 30 | 187 ± 24 | 0.356 |
| HR BP | 176 ± 23 | 165 ± 27 | 0.162 |
| BP | 131 ± 11 | 107 ± 17 | 0.001* |
Data are mean ± SD
Difference between pre- and post-trazodone was statistically significant
HR PE = heart rate auscultated during physical examination; HR BP = heart rate obtained during Doppler blood pressure examination; BP = systolic blood pressure obtained via Doppler method
Figure 2.
Change in systolic blood pressure pre- and post-trazodone administration in 11 healthy cats
Discussion
This study did not observe differences of clinical relevance for echocardiographic variables after oral trazodone in healthy cats. While three variables were statistically different, their magnitude of change is considered clinically insignificant. The LASAX was statistically different after trazodone administration. In a previous study evaluating LA size in cats, the LASAX had a SD of 0.1 cm and a coefficient of variation of 9.0%. 13 In our study, the difference between baseline and post-trazodone was 0.06 cm. This difference is considered clinically acceptable and likely represents normal variability of this measurement in healthy cats. Additionally, all other variables used to assess LA size (LA:Ao and LADMax) were not statistically different post-trazodone. Diastolic function was also considered to be unaffected by trazodone. Two indices of diastolic function (E:A and PVA) were statistically different post-trazodone; however, previous studies indicate that in normal cats mean E:A is 1.5 ± 0.3 and mean PVA is 0.23 ± 0.06 m/s.14,15 In our study, the differences post-trazodone for E:A and PVA were 0.15 and 0.05 m/s, respectively, supporting normal variability in healthy cats. We therefore conclude that trazodone had no clinically relevant effect on any of the echocardiographic variables assessed in this group of healthy cats.
A statistically and clinically significant decrease in systolic BP post-trazodone was observed for all cats in this study (Figure 2). In humans, trazodone is reported to cause hypotension and exacerbate postural hypotension.16–18 Trazodone is a serotonin2 receptor antagonist, but its active metabolite, m-chlorophenylpiperazine, is a serotonin receptor agonist. Trazodone also blocks postsynaptic α1-adrenoceptors, which gives it a distinct sedation profile; however, the α1-adrenoceptor antagonism properties of trazodone lowers BP. In our study, the mean ± SD reduction in systolic BP post-trazodone was 25 ± 16 mmHg (range 9–66 mmHg). Even when excluding the cats with the highest and lowest reductions in BP, a clinically and statistically significant reduction in mean BP (n = 9; pre-trazodone 131 ± 9 mmHg; post-trazodone 109 ± 12 mmHg) was still observed (P = 0.006). BP is the product of systemic vascular resistance (SVR) and cardiac output, which is the product of HR and stroke volume (SV). Thus: BP = SVR × HR × SV. In our study, no cats had clinically or statistically significant changes in HR or SV after trazodone administration. Therefore, the observed reduction in BP in our study is best explained by a decrease in SVR, likely from the α1-adrenoceptor antagonism properties of trazodone. Previous studies evaluating trazodone in cats either did not evaluate BP 12 or reported no change after trazodone administration. 9 No BP values or time of BP measurement post-trazodone were reported in the latter paper. Additionally, that report stated BP was always the last diagnostic test performed and was assessed via the tail using the Doppler method. 9 It has been reported that forelimb measurements are best suited for Doppler evaluation while high-definition oscillometry measurements are best utilized on the tail in cats.11,19 A single 50 mg dose and a minimum 90 min wait time was selected based on a previous report evaluating the greatest sedative effect in cats. 12 By waiting a minimum of 90 mins, the post-trazodone echocardiographic and BP examinations would be completed during the reported peak effect of trazodone. While the previous study and our study both utilized the Doppler method, a direct comparison of our data cannot be made. The potential vasodilatory effects of trazodone in cats should be explored further.
There are several limitations to this study. First, this study evaluated a small number of healthy cats and therefore it cannot be assumed that the lack of effects of trazodone on echocardiographic variables will be similar in cats with cardiac disease. Secondly, the operator (RCF) who performed all echocardiographic examinations was not blinded to the treatment administration because there was no placebo group. However, this observer was blinded to patient information and study number when making measurements to reduce motivational bias. Finally, this was a single-dose study and the conclusions may differ with varying or repeated dosing.
Conclusions
Trazodone did not alter echocardiographic variables, in a clinically relevant manner, in this group of healthy cats. Trazodone may aid in obtaining transthoracic echocardiograms without affecting HR or echocardiographic variables but may significantly lower BP in healthy cats.
Acknowledgments
We would like to thank Kathryn McConnell, CVT, for her technical assistance.
Footnotes
Accepted: 31 October 2018
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Ryan C Fries  https://orcid.org/0000-0001-9682-7755
https://orcid.org/0000-0001-9682-7755
References
- 1. Quimby JM, Smith ML, Lunn KF. Evaluation of the effects of hospital visit stress on physiologic parameters in the cat. J Feline Med Surg 2011; 13: 733–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hughes D, Moreau RE, Overall KL, et al. Acute hepatic necrosis and liver failure associated with benzodiazepine therapy in six cats, 1986–1995. J Vet Emerg Crit Care 2007; 6: 13–20. [Google Scholar]
- 3. Levy JK, Cullen JM, Bunch SE, et al. Adverse reaction to diazepam in cats. J Am Vet Med Assoc 1994; 205: 156–157. [PubMed] [Google Scholar]
- 4. Fox PR, Bond BR, Peterson ME. Echocardiographic reference values in healthy cats sedated with ketamine hydrochloride. Am J Vet Res 1985; 46: 1479–1484. [PubMed] [Google Scholar]
- 5. Jacobs G, Knight DH. Change in M-mode echocardiographic values in cats given ketamine. Am J Vet Res 1985; 46: 1712–1713. [PubMed] [Google Scholar]
- 6. Moise NS, Horne WA, Flanders JA, et al. Repeatability of the M-mode echocardiogram and the effects of acute changes in heart rate, cardiac contractility, and preload in healthy cats sedated with ketamine hydrochloride and acepromazine. Cornell Vet 1986; 76: 241–258. [PubMed] [Google Scholar]
- 7. Ribas T, Bublot I, Junot S, et al. Effects of intramuscular sedation with alfaxalone and butorphanol on echocardiographic measurements in healthy cats. J Feline Med Surg 2015; 17: 530–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ward JL, Schober KE, Fuentes VL, et al. Effects of sedation on echocardiographic variables of left atrial and left ventricular function in healthy cats. J Feline Med Surg 2012; 14: 678–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Stevens BJ, Frantz EM, Orlando JM, et al. Efficacy of a single dose of trazodone hydrochloride given to cats prior to veterinary visits to reduce signs of transport- and examination-related anxiety. J Am Vet Med Assoc 2016; 249: 202–207. [DOI] [PubMed] [Google Scholar]
- 10. Thomas WP, Gaber CE, Jacobs GJ, et al. Recommendations for standards in transthoracic two-dimensional echocardiography in the dog and cat. Echocardiography Committee of the Specialty of Cardiology, American College of Veterinary Internal Medicine. J Vet Intern Med 1993; 7: 247–252. [DOI] [PubMed] [Google Scholar]
- 11. Taylor SS, Sparkes AH, Briscoe K, et al. ISFM consensus guidelines on the diagnosis and management of hypertension in cats. J Feline Med Surg 2017; 19: 288–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Orlando JM, Case BC, Thomson AE, et al. Use of oral trazodone for sedation in cats: a pilot study. J Feline Med Surg 2016; 18: 476–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Abbott JA, MacLean HN. Two-dimensional echocardiographic assessment of the feline left atrium. J Vet Intern Med 2006; 20: 111–119. [DOI] [PubMed] [Google Scholar]
- 14. Disatian S, Bright JM, Boon J. Association of age and heart rate with pulsed-wave Doppler measurements in healthy, nonsedated cats. J Vet Intern Med 2008; 22: 351–356. [DOI] [PubMed] [Google Scholar]
- 15. Chetboul V, Sampedrano CC, Tissier R, et al. Quantitative assessment of velocities of the annulus of the left atrioventricular valve and left ventricular free wall in healthy cats by use of two-dimensional color tissue Doppler imaging. Am J Vet Res 2006; 67: 250–258. [DOI] [PubMed] [Google Scholar]
- 16. Khouzam HR. A review of trazodone use in psychiatric and medical conditions. Postgrad Med 2017; 129: 140–148. [DOI] [PubMed] [Google Scholar]
- 17. Cowen PJ. Psychopharmacology. In: Bellack AS, Hersen M. (eds). Comprehensive clinical psychology. Oxford: Pergamon, 1998, pp 135–161. [Google Scholar]
- 18. Poon IO, Braun U. High prevalence of orthostatic hypotension and its correlation with potentially causative medications among elderly veterans. J Clin Pharm Ther 2005; 30: 173–178. [DOI] [PubMed] [Google Scholar]
- 19. Cannon MJ, Brett J. Comparison of how well conscious cats tolerate blood pressure measurement from the radial and coccygeal arteries. J Feline Med Surg 2012; 14: 906–909. [DOI] [PMC free article] [PubMed] [Google Scholar]