Abstract
Practical relevance
Diseases of the biliary tree and gallbladder are more common in cats than diseases of the liver parenchyma. The parenchyma is usually affected secondarily to systemic illnesses, while the biliary system is the prime target for infectious agents (eg, bacteria and flukes) and non-infectious conditions (eg, neoplasia and cysts).
Clinical approaches
Cats with biliary disease are evaluated because of common feline clinical signs such as anorexia, nausea, vomiting and lethargy. Icterus may or may not be obvious. Biopsies for histological evaluation, and bile aspirates for culture and cytological evaluation are helpful diagnostically. Antibiotics and immunosuppressive drugs have been used successfully. Hepatosupportive drugs may help in liquefying thick bile and protecting hepatic tissue from damage. Ultrasound is a noninvasive diagnostic tool that may help in identifying dilated bile ducts, liver cysts and choleliths. It is also used to guide percutaneous bile aspiration.
Audience
This review, written for all veterinarians who treat cats, describes the various conditions that can affect the feline biliary tree and gallbladder. Treatment options are discussed, and brief summaries provided of surgical techniques and diagnostic approaches.
Evidence base
The veterinary literature pertaining to feline biliary disease is comprehensively reviewed. When appropriate, data on dogs and humans has been included to provide background information. Based on the available literature, more research into feline biliary diseases is needed.
The healthy liver
The first embryonic function of the liver is haematopoiesis. 1 Upon maturation, the liver has critical functions in metabolism and detoxification, including synthesis of proteins such as albumin and blood clotting factors, maintenance of glucose homeostasis, lipid metabolism, conjugation and excretion of endogenous and exogenous toxins and drugs, and excretion of bile.2,3
The feline liver is the largest internal organ, corresponding to approximately 3–4% of total body weight.4,5 Parenchymal liver diseases include lipidosis, amyloidosis and feline infectious peritonitis (FIP). In these diseases, the liver parenchyma is not the primary target, but is affected as part of the systemic disease. In cats, it is the biliary system rather than the liver parenchyma that is the primary target of disease.
Feline bile (pH 5.9–7.8) is a fluid consisting of various (non-)sulphated bile acids and cholesterol.6,7 Taurine is the only nutrient used by cats to conjugate bile acids and, because cats have limited taurine production capacity, it is considered an essential dietary component for cats.6,8 Thus taurine availability can also be considered a limiting factor in the production of conjugated bile acids.
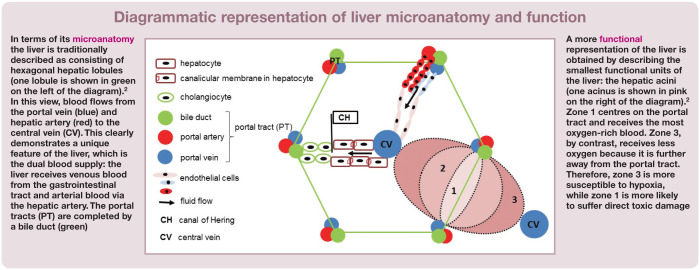
Bile salts are excreted into specialised regions of the canalicular membrane between hepatocytes: the bile canaliculi (see diagram on page 515). The bile canaliculi drain into the canals of Hering, which merge to create interlobular bile ducts, and later fuse into intrahepatic bile ducts. These join to form hepatic ducts and, ultimately, the common bile duct (CBD). Together with the cystic duct, this network is considered to be the biliary tree. The biliary tree and gallbladder constitute the biliary system. At Vater’s papilla, the CBD enters the duodenum.9–11 In cats, the major pancreatic duct usually joins the CBD before it enters the duodenum; only 20% of cats are estimated to have an accessory pancreatic duct with its own separate opening into the duodenum. 12
The hepatic ducts transport bile into the gallbladder, where the fluid is stored and concentrated during fasting. The duodenal mucosa produces cholecystokinin when food enters the intestines, the hormone that stimulates the gallbladder to contract. Bile enters the duodenum via the CBD and mixes with food. Bile acids aid in digestion and absorption of lipids and fat-soluble vitamins. Bile is also used to eliminate many waste and toxic products, which are subsequently excreted in the faeces. About 90% of bile acids are reabsorbed in the enterohepatic circulation. 7
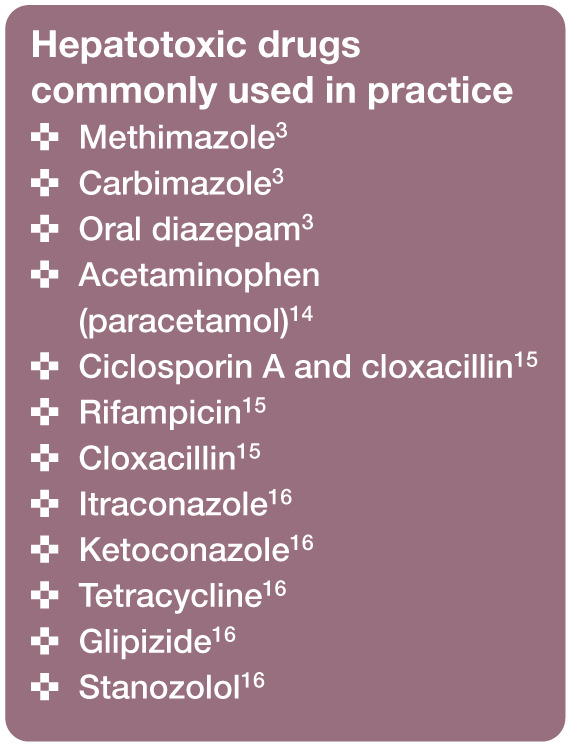
Felids have a low capacity for glucuronide conjugation of drugs and toxins, limiting their conversion to water-soluble substances that can be excreted into urine or bile. 13 This makes cats more prone to suffer hepatotoxic effects when exposed to certain drugs and toxins (see box above for commonly used drugs that are hepatotoxic to cats).
A detailed report, almost a century ago, by Boyden showed that over 12% of cats have some sort of accessory gallbladder (see later). 17 However, biliary disease and gallbladder anomalies are infrequently reported together, which suggests that there is no association between the two. 18
Cholestasis
An important clinical syndrome associated with biliary disease is cholestasis, which is defined as impaired bile flow. 19 Cholestasis is not a disease per se, but a pathophysiological phenomenon associated with dysfunction of the biliary system. Two forms are commonly distinguished – intrahepatic and extrahepatic.
Intrahepatic cholestasis occurs predominantly at the level of hepatocytes, bile canaliculi or bile ductuli in zone 1 (see diagram above). In cats, intrahepatic cholestasis is linked to the destruction of bile ductuli and hepatic fibrosis secondary to cholangitis. 18 Some cholestatic drugs (eg, methimazole, ciclosporin, rifampicin and cloxacillin) have been associated with reduced bile flow at the canalicular level.3,15 In all species, dogs and humans included, endotoxins represent a major cause of intrahepatic cholestasis by impairment of the canalicular bile flow. 20
Extrahepatic cholestasis is caused by obstruction of the CBD.
Extrahepatic bile duct obstruction
Aetiology
Bile sludge and choleliths, associated with cholangitis, cholecystitis and impaired contractility of the gallbladder, have been implicated as the most common causes of extrahepatic bile duct obstruction (EHBDO).21–23 Other causes include pancreatitis,12,22 biliary neoplasia, 22 foreign bodies,21,24 biliary mucoceles 18 and gastrointestinal disease. 23
Clinical signs
Clinical signs appear to be non-specific in relation to the cause of cholestasis and include abdominal pain, vomiting, dehydration, nausea, anorexia, weight loss, lethargy, pyrexia, icterus (Figure 1), diarrhoea and polyuria/ polydipsia.12,18,21–24 Although acholic faeces have consistently been seen after experimental ligation of the CBD, this finding is not encountered in clinical practice. 12
Figure 1.
Icterus observed (a) in the ear and (b) on the skin of the ventral neck. Images courtesy of (a) Dr Robert Favier, Utrecht University, and (b) Marleen Assink
Diagnosis
Increased activity of liver enzymes, especially the short-lived alkaline phosphatase, may indicate cholestasis (see Table 1).7,14 Elevations in total bilirubin and bile acids are also commonly seen.7,12,23
Table 1.
| Parameter | Anatomical distribution | Increases in response to: | t1/2 | Increases observed: | Decreases observed: | Especially useful in: | Findings in biliary and gallbladder diseases (with supporting references) |
|---|---|---|---|---|---|---|---|
| Alanine aminotransferase* (ALT) | Cytosol of hepatocytes, cardiac muscle, kidney | Hepatocellular necrosis, inflammation, acetaminophen toxicosis | 3.5 h | In first 5 days after injury (within 24 h in acetaminophen toxicosis) | 2–3 weeks after recovery (within 72 h in acetaminophen toxicosis) | – | |
| Aspartate aminotransferase† (AST) | Cytosol and mitochondria of hepatocytes, skeletal muscle, heart, kidney, brain, small intestine, spleen | – | 1.5 h | In first 3 days after injury | 2–3 weeks after recovery | Hepatic necrosis, cholangitis, chronic bile duct obstruction | |
| Alkaline phosphatase‡ (ALP) | Membrane of hepatocytes, bone, intestine, kidney, placenta | Neonates (colostrum), young animals (bone growth), hyperthyroidism, inflammation and neoplasia, late pregnancy, lipidosis | 6 h | Within 2 days of EHBDO | 2–3 weeks after recovery | Cholestasis | |
| γ-glutamyltransferase (γGT) | Kidney, pancreas, intestine, gallbladder, membrane of cholangiocytes | – | – | Within 3 days of EHBDO | – | Cholestasis (interpret together with ALP) | |
| Lactate dehydrogenase§ (LDH) | Skeletal muscle, heart, kidney, intestine, cytosol of hepatocytes, lung, pancreas | Diffuse severe hepatic necrosis or inflammation; young animals (higher in kittens than adults) | – | – | – | – | – |
| Arginase | Cytosol of hepatocytes and mitochondria | – | – | – | – | – | – |
| Sorbitol dehydrogenase§ (SDH) | Cytosol of hepatocytes | – | – | – | – | – | – |
| γ-globulins | – | – | – | – | – | – | |
| Bile acids | – | Loss of functional hepatic mass | – | – | – | – | |
| Cholesterol | – | – | – | – | – | – | |
| Bilirubin | – | – | – | – | – | – |
Mostly periportal in location
Mostly periacinar in location
Does not increase in cats treated with glucocorticoids
Not used routinely
LC = lymphocytic cholangitis; AD-PKD = autosomal dominant polycystic kidney disease; EHBDO = extrahepatic bile duct obstruction; CBD = common bile duct; LFC = cholangitis due to liver flukes; NC = neutrophilic cholangitis; t1/2 = half-life in the circulation
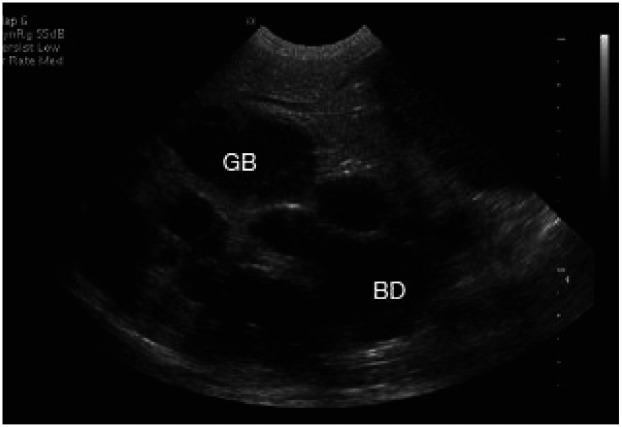
EHBDO can often be diagnosed with ultrasound. In normal cats, intrahepatic and extrahepatic ducts are not visible; thus, any duct visible on ultrasonography is considered dilated. 22 The diameter of the CBD is a useful parameter in diagnosing EHBDO since it is greater than 5 mm in 97% of affected cats; the upper limit for healthy cats has been established at 4 mm.21,22
In contrast, gallbladder dilatation is not a reliable sign of EHBDO in clinical practice, although it is invariably seen after experimental bile duct ligation. 22
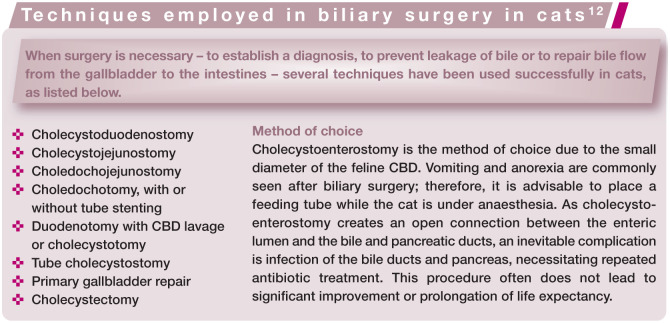
Treatment
Treatment depends on the cause of the obstruction, and may involve the use of choleretics such as ursodeoxycholic acid (UDCA) (bile sludge), surgery (choleliths, foreign body, mucocele), praziquantel (liver flukes), prednisolone (cholangitis, gastrointestinal disease), antibiotics (suppurative cholangitis, gastrointestinal disease), and a low fat diet, antiemetics and supportive fluids (pancreatitis).
Prognosis
Many of the above-mentioned therapies can be very successful in relieving cholestasis, though the prognosis is heavily dependent on the underlying cause.
Inflammation of the biliary system
Inflammatory bile duct diseases are among the most common types of hepatopathy in cats.11,43 Feline cholangitis may be accompanied by pancreatitis, inflammatory bowel disease and cholecystitis.36,44
Neutrophilic cholangitis
Aetiology
Enteric bacteria have been implicated in inflammatory liver disease, with translocation across the mucosal barrier being the most likely source of infection.26,35,44 Neutrophilic cholangitis (NC) may also be caused by ascending bacterial infection from the gut or haematogenous dissemination of enteric bacteria.26,45,46 In healthy cats, transient bacterobilia exists although the biliary tract is considered to be sterile. 47
In cats, NC is accompanied by cholecystitis. 26 In fact, these are likely not distinct entities in cats.
Clinical signs
The most promient clinical signs of NC are nausea, vomiting, anorexia and fever. Icterus is present in a minority of cases.
Diagnosis
Examination of a sample of bile is the most likely route to a diagnosis (Figure 2).26,48 Bile samples can be obtained by cholecystocentesis with a 22 G needle under ultrasound guidance (see box below). Ultrasonography usually reveals no abnormalities of the gallbladder, although oedema of the gallbladder wall may be seen in acute, severe cases. Cytology of bile will reveal neutrophils and sometimes bacteria. Culture will determine the bacterial species present, and their antimicrobial susceptibility. A biochemical profile is often within normal limits or may show increased activity of alanine aminotransferase, while the most common finding on a complete blood count is leukocytosis.
Figure 2.
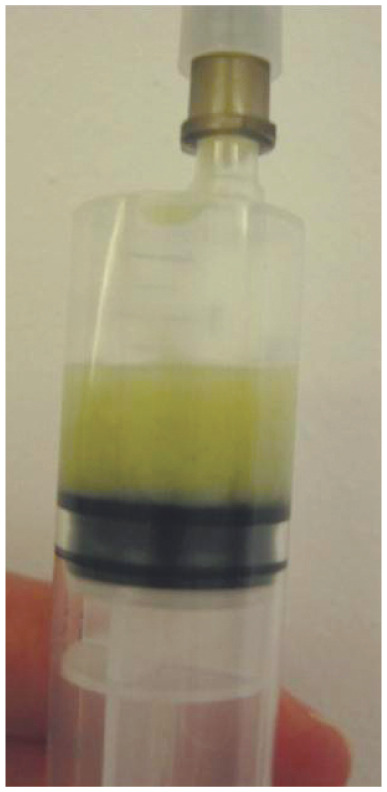
Bile sample from a cat with neutrophilic cholangitis. The bile is yellow and turbid due to the presence of pus
Treatment
Amoxicillin/clavulanate and ticarcillin/clavulanate for at least 4 weeks have been used successfully in the treatment of NC,26,28 and are the first-choice treatment (Table 2). other antibiotics, such as chloramphenicol, fluoroquinolones and metronidazole, are well excreted in bile, have good anaerobic activity and may be considered.7,35 It is recommended that susceptibility testing is performed routinely to allow selection of the best antibiotic. Long-term treatment is essential to prevent recurrence.
Table 2.
Reported use of medical therapies for feline biliary disease
| Disease | Therapy |
|---|---|
| NC 27 | Metronidazole 30 mg/kg q24h PO and amoxicillin 10 mg/kg q12h PO for 2 months |
| NC26,28 | Amoxicillin/clavulanate 45 mg q12h SC initially, then 50 mg PO q12h for 4 weeks in total (cat body weight 2.85 kg), or ticarcillin/clavulanate PO for at least 4 weeks |
| NC 26 | UDCA 50 mg q24h PO and vitamin K1 6 mg q24h PO |
| NC and cholecystitis 26 | Enrofloxacin 2.5 mg/kg q12h SC |
| NC and cholecystitis 26 | Amoxicillin/clavulanate 100 mg q8h IV, ciprofloxacin 30 mg q24h PO and UDCA 30 mg q24h PO (cat body weight 2.3 kg) for 2 weeks |
| NC and cholecystitis 26 | Amoxicillin 70 mg q12h SC |
| NC and cholecystitis 26 | Doxycycline 50 mg q12h PO and cephalexin IV for 7 days, then 112.5 mg q12h PO for 4 weeks in total |
| Cholecystitis 52 | NSAIDs |
| Cholecystitis7,35 | Chloramphenicol Fluoroquinolones Amoxicillin/clavulanate Metronidazole |
| Gallbladder rupture, NC and cholecystitis 26 | Cefoxitin 120 mg q8h IM and amoxicillin 100 mg q12h PO |
| Choledochal cyst 30 | Pre-surgery (and continued for 3 days): amoxicillin/clavulanate 60 mg q8h IV and metronidazole 30 mg q12h IV Post-surgery: amoxicillin/clavulanate 50 mg q12h PO, metronidazole 33.3 mg q12h PO, UDCA 37.5 mg q24h PO, S-adenosylmethionine 50 mg q24h PO, vitamin E 10 mg q24h PO and vitamin K 0.05 mg q24h PO |
| EHBDO 24 | 4 week course of potentiated amoxicillin 15 mg/kg q12h PO, metronidazole 15 mg/kg q24h PO, and Samylin* 1 g sachet q24h PO |
| LC 53 | Prednisolone 1–2 mg/kg q24h PO for 4–6 weeks, followed by gradual dose tapering |
| LC,53 mucocele, choleliths, cholestasis18,39 | UDCA 15 mg/kg q24h PO |
| LC 29 | Prednisolone (up to 4 mg/kg PO) for an initial period of 3 weeks, followed by gradual dose tapering over 6–8 weeks |
| EHBDO 32 | Amoxicillin/clavulanate 20 mg/kg q8h IV, metronidazole 10 mg/kg q12h IV, buprenorphine 30 mg/kg q8h IM, and vitamin K1 0.5 mg/kg q12h SC (for 3 days); followed by cephalexin 15 mg/kg q12h PO, metronidazole 10 mg/kg q12h PO and UDCA 10 mg/kg PO q24h (antibiotics for a total duration of 4 weeks) |
| Lipidosis 39 | Metaclopramide 0.05 mg/kg/h IV and ranitidine 1.5 mg/kg q12h IV |
| Hepatic encephalopathy 39 | Lactulose 1 ml q8h PO |
S-adenosyl L-methionine/silybin/vitamin E liver supplement (VetPlus)
NC = neutrophilic cholangitis; UDCA = ursodeoxycholic acid; EHBDO = extrahepatic bile duct obstruction; LC = lymphocytic cholangitis; NSAIDs = non-steroidal anti-inflammatory drugs; PO = orally; IV = intravenously; SC = subcutaneously; IM = intramuscularly
Increased levels of cyclooxygenase were detected in inflamed mucosa of feline gallbladders in one experimental study, 54 suggesting a role for non-steroidal anti-inflammatory drugs (NSAIDs) in the treatment of cholecystitis. 52
Adjunctive therapies used for NC have included UDCA and vitamin K. 26 However, there is no evidence for their beneficial effect and, in the authors‘ opinion, treatments for NC should be limited to long-term use of antibiotics, as discussed above. 55
Prognosis
The only study that reports on prognosis for feline NC states that most cats regained their previous health after receiving the appropriate antibiotics. 26 However, if treatment is too late or unsuccessful the disease is often fatal. 36
Lymphocytic cholangitis
Aetiology
Bacterial as well as immunological aetiologies have been suggested for lymphocytic cholangitis (LC).29,56–60 Hypothetically, an infectious agent could initiate inflammation, which could then be sustained as an immune-mediated disease after the infectious agent has been eliminated. This would suggest that LC could be a chronic sequela to NC. However, no such connection has ever been confirmed. LC and NC are presently considered to be two separate, unconnected diseases. Additionally, LC has been diagnosed secondarily to bile duct obstruction by choleliths. 32 To date, however, no definite aetiology has been established.
Clinical signs
Nausea, chronic vomiting, diarrhoea, anorexia and icterus are seen in LC, as are polyphagia and weight loss.27,30 The course of the disease is often protracted, spanning months to years. Icterus, if present, usually indicates advanced disease. Male cats appear to be affected more frequently than females. 53
Diagnosis
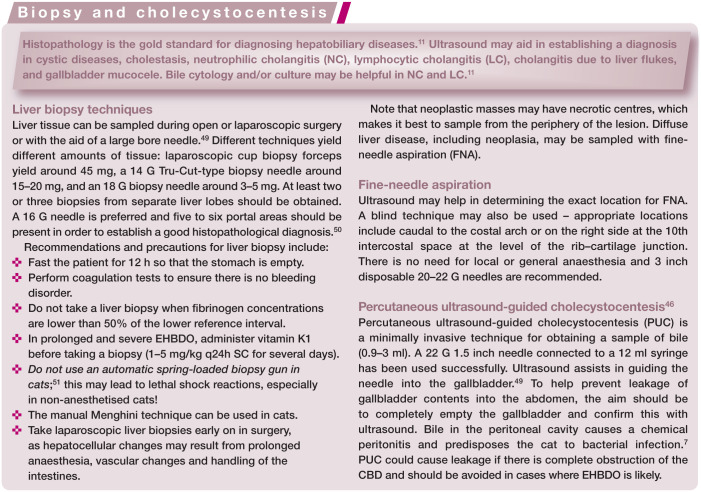
Hypergammaglobulinaemia is the most consistent abnormality on the biochemical profile.28,29 This, together with the chronicity of the disease, often leads to a misdiagnosis of FIP. 61 Ultrasonographically, dilated intra- and extrahepatic bile ducts are frequently seen (Figure 3), although not all cases of LC have ultrasonographic changes in the bile ducts. Dilatation of the bile ducts excludes FIP. It is not possible to distinguish between NC and LC based on these findings. 36 Furthermore, ultrasound has limited sensitivity for detecting infiltrative liver diseases. 22
Figure 3.
Distended bile ducts in a cat. GB = gallbladder; BD = bile duct. Reproduced from the WSAVA Standards for Clinical and Histological Diagnosis of Canine and Feline Liver Diseases, 11 with permission of Dr George Voorhout
FNA is not diagnostic. Cytology may show lymphocytes and may lead to a misdiagnosis of malignant lymphoma.62–65 The portal distribution of lesions in cats with LC cannot be identified with FNA cytology and there is a discrepancy between histology and cytology in 55% of cases.66,67
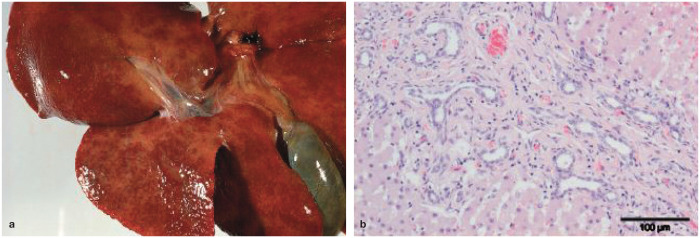
Histology is the gold standard for diagnosing LC (Figure 4). Either surgical or laparoscopic wedge biopsy procedures may be used, or alternatively larger needle biopsy techniques (see box on page 518) that obtain at least five portal triads – the sample size that is considered representative in humans. 50 In a study comparing needle and wedge biopsies, only 2/13 cats and dogs received the same histological diagnosis; 50 this is likely due to the small needle diameter used for liver sampling. In the authors’ experience, the diagnosis of LC can be accurately made with Tru-Cut liver biopsies of sufficient size. This is achieved using a 16 G needle in a semi-automatic biopsy gun (see box on page 518). Thinner needles lead to diagnostic inaccuracy; surgical wedge biopsies should be pursued in preference.
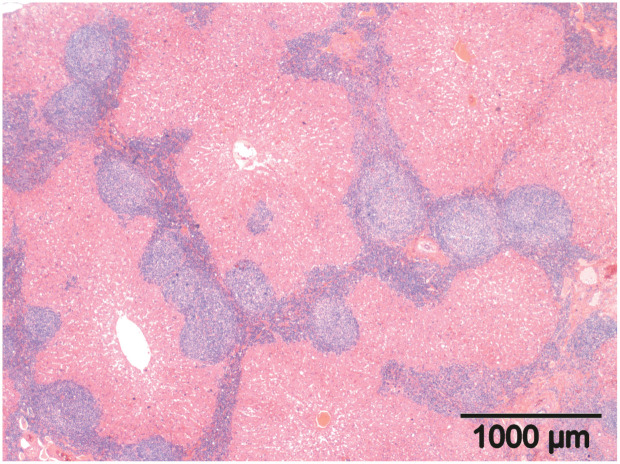
Figure 4.
Histology of a liver biopsy sample from a cat with lymphocytic cholangitis. Dense infiltrates of small lymphocytes are present in portal areas, extending to portal–portal bridging. Haematoxylin and eosin
Typical histological lesions are lymphocytic inflammation of the biliary tree with fibrosis surrounding the bile ducts (an expression of the chronicity of the process). Lymphocytes are present inside the lumen and wall, and around the bile ducts in the portal triads. In cats with LC, the biliary system is prone to infection, leading to a mixed lymphocytic and neutrophilic inflammation.
Treatment
Corticosteroids, such as prednisolone (1–2 mg/kg q24h), and UDCA (15 mg/kg q24h) have been used as treatments for LC.29,53,60 If there is secondary bacterial infection, treatment should also include appropriate antibiotics for 4–5 weeks. The best sample for cytological identification of bacteria and culture for sensitivity testing is bile, obtained by ultrasound-guided aspiration of the gallbladder.
Prognosis
Data from 23 cats showed that 70% survived for more than 1 year, with a mean survival time of 51.8 months. 43 In a separate study, cats treated with prednisolone had better survival rates than cats treated with UDCA; overall survival rates for 1, 2 and 3 years were 74%, 56% and 35%, respectively, with a median overall survival of 795 days (~26 months). 53
Cholangitis due to liver flukes
Aetiology
Liver flukes that cause feline cholangitis are members of the opisthorchiidae or Dicrocoeliidae families; Platynosomum species are most common in (sub)tropical regions.11,37,68 Snails and lizards carry the liver fluke and cats become infected when they ingest these prey items.11,68 Adult flukes reside in the bile ducts and gallbladder of affected animals, and this may lead to cholestasis (Figure 5).7,68
Figure 5.
Cholangitis due to liver fluke infection. Reprinted with permission from the WSAVA Standards for Clinical and Histological Diagnosis of Canine and Feline Liver Diseases. 11 Image courtesy of the Society of Comparative Hepatology
Clinical signs
Cats with cholangitis due to liver flukes (LFC) show clinical signs such as lethargy, weight loss, decreased appetite, abdominal pain and vomiting.37,38 Icterus may be observed and is associated with cholestasis due to high numbers of parasites. 68
Diagnosis
Microscopic examination of liver biopsies, bile or faeces may sometimes reveal liver fluke eggs.38,69 Eosinophilic inflammation in the portal areas on liver histology is suggestive of LFC. 38 Chronic LFC leads to dilatation and fibrosis of bile ducts, which can be seen on ultrasound. 68 These imaging findings are very similar to those of chronic LC. A blood smear or complete blood count sometimes reveals eosinophilia, which is never seen in cats with LC.
Treatment
Liver flukes can be treated adequately with praziquantel (20 mg/kg q24h PO for 3 days). 37
Prognosis
With the correct therapy the prognosis is excellent. 70 Changes to the biliary tree, such as dilatations, will persist and will increase the patient’s sensitivity to ascending bacterial infections from the intestines. 28
Cholecystitis
Aetiology
Experimentally, feline cholecystitis has been induced by platelet activating factor, Escherichia coli lipopolysaccharide and xenotransplantation of human gallstones into feline gallbladders.52,54 Furthermore, cytolytic agents in bile cause severe inflammation in cholestasis, 27 and bile salts cause tissue necrosis, aiding in bacterial colonisation. 7 These bacteria may either be blood-borne or originate from the intestines.7,44 In cats, cholecystitis may be accompanied by NC. 26 Bile peritonitis has never been reported as a sequela to cholecystitis in cats. 71
As discussed, there are no indications that cholecystitis and NC are distinctly different entities in the cat.
Clinical signs
Reported clinical signs include inappetence, lethargy, vomiting, anorexia, diarrhoea, jaundice, cranial abdominal pain, weight loss, pyrexia, anaemia and mild hyperbilirubinaemia.26,40
Diagnosis
Ultrasound may demonstrate a thick, doublerimmed, oedematous gallbladder wall in acute forms of cholecystitis, and a thinner, single-layered wall in chronic or mild inflammation. 72 In one study of six cats, cholecystocentesis yielded bacteria (E coli, Streptococcus species, Clostridium species and Salmonella enterica), as well as degenerate inflammatory cells in most cases. 26 Histology of the gallbladder wall shows neutrophils in the epithelium and/or wall. 11
Treatment
Increased levels of cyclooxygenase have been detected in inflamed mucosa of feline gallbladders, 54 suggesting a role for NSAIDs in the treatment of cholecystitis. 52 Antibiotics such as chloramphenicol, fluoroquinolones, amoxicillin/clavulanate and metronidazole concentrate in bile and have good anaerobic activity.7,35
Prognosis
Based on the only published study, the prognosis is good when the right antibiotic has been determined and administered. 26
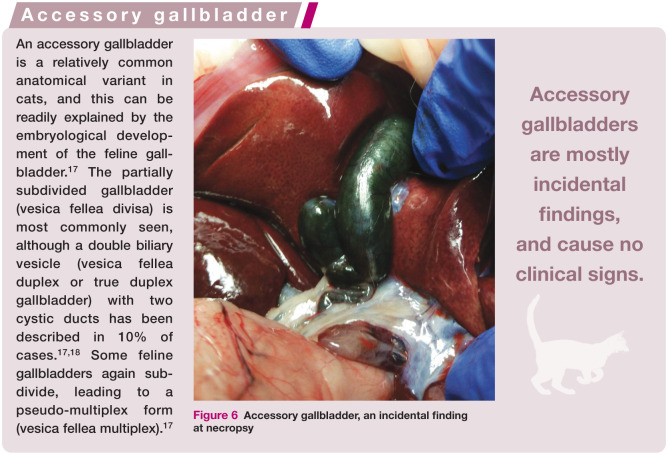
Diseases of the gallbladder
Anomalies in gallbladder shape are frequently seen on ultrasound examination and over 12% of cats have some form of accessory gallbladder (see box above).17,72 Most of the diagnosed aberrant gallbladders are incidental findings during ultrasound examination, surgery or at necropsy (Figure 6) and cause no clinical signs. Cholecystectomy can be performed if removal of the aberrant gallbladder is necessary.
Figure 6.
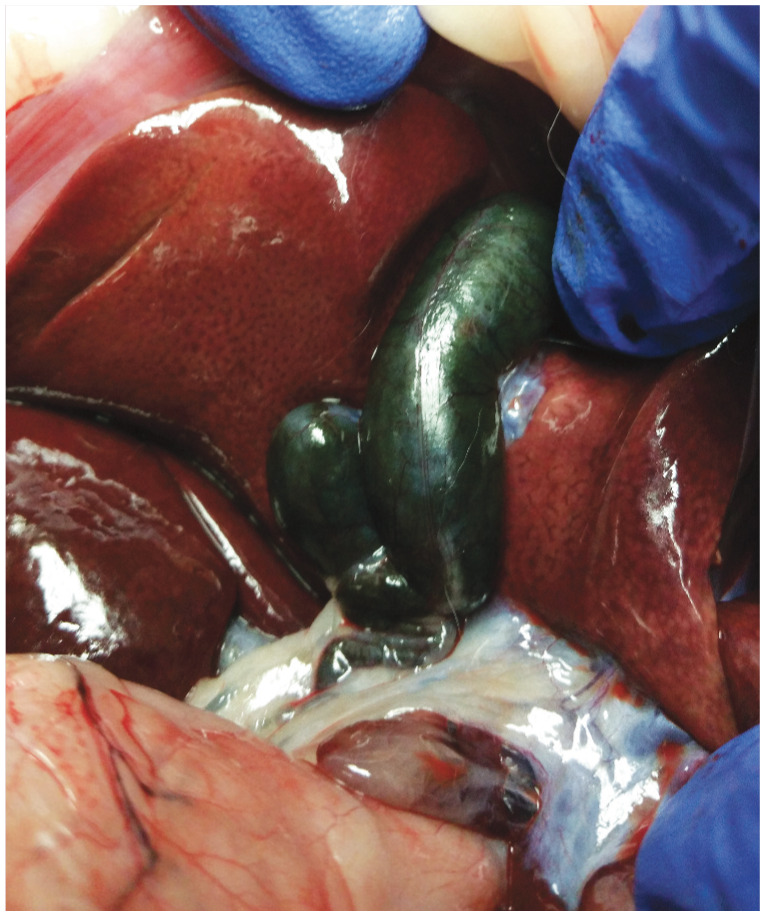
Accessory gallbladder, an incidental finding at necropsy
Cholelithiasis
Aetiology
Choleliths (gallstones) are encountered infrequently, accounting for fewer than 1% of canine and feline cases of liver disease combined. 7 They are much more common in humans. The majority of human gallstones are predominantly comprised of cholesterol, with pigment stones being much rarer. 33 Based on what is known about the pathogenesis of choleliths in man and prairie dogs, a number of contributing factors can be proposed (see right).
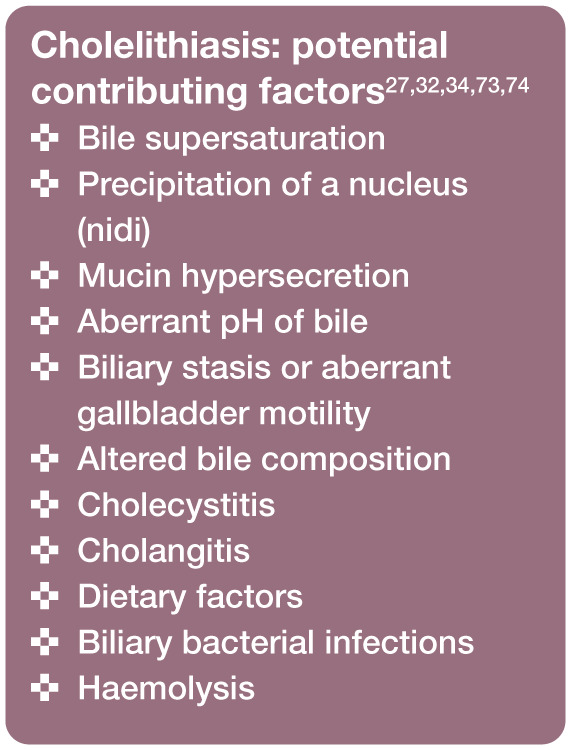
Choleliths are sometimes encountered in cases of EHBDO. 22 They consist of calcium carbonate or palmitate, and amorphous plugs of bile salts and cholesterol. 22 other studies have identified stones composed of a combination of: bilirubin, 32 calcium carbonate, oxalate, phosphate and magnesium;12,40 calcium carbonate and calcium bilirubinate;27,33 cholesterol, bilirubin derivatives and calcium salts; 7 and calcium carbonate, calcium bilirubinate and cholesterol. 34 Based on their composition, most feline stones are classified as black (bilirubin) or brown (bacterial degradation of biliary matter), also known as pigment gallstones. 74
Altered gallbladder motility, mucin hypersecretion and ascending bacterial infection might have contributed to stone formation in a case reported by Elwood and colleagues. 33
No definitive causal relationship has been determined between the presence of gallbladder sludge and the formation of stones. 23
Clinical signs
Symptomatic cholelithiasis is not encountered frequently in the cat, 7 and clinical signs might be associated with the cause or consequence of cholelithiasis rather than the choleliths themselves. 33 Vomiting has been reported, as well as dehydration, anorexia, icterus and lethargy.27,32,34 Interestingly, most cats with choleliths are male. 34
Diagnosis
Bile can be examined cytologically for cells, crystals and bacteria. 33 Radiographs, ultrasound and cholecystography with contrast can be used to visualise gallstones.7,33,34
Treatment
Litholytic and choleretic agents, such as UDCA, are used in treating asymptomatic cholesterol gallstones in humans. UDCA has been used safely in cats at a dosage of 15 mg/kg body weight q24h Po. 53 In contrast, pigment stones in humans are removed surgically; surgical removal of the gallbladder has been shown to prevent recurrence of stone formation.33,73 In cats, surgery has been used successfully to remove stones or the gallbladder itself, as well as to divert the biliary tract (see box above for commonly used surgical techniques).22,32–34
Prognosis
The prognosis is guarded since choleliths may be the cause or the consequence of disease. The underlying or resultant disease will ultimately determine the outcome. When cats survive surgery and recuperate well, the prognosis can be favourable.
Gallbladder mucocele
Aetiology
Mucous glands in the epithelium of the gallbladder protect against the deleterious effects of bile acids. Cats have fewer mucous glands than dogs, which may explain why mucoceles have been reported less frequently in cats than in dogs. 72 In total, three feline cases have been described.18,22,39 In dogs, mucoceles have a distinct striated pattern, but no such pattern was reported for the three cats. 11 Mucous gland hyperplasia was described in one feline case. 72
In a case report by Bennett and colleagues, concurrent hepatic lipidosis was diagnosed. 39 Dyslipidaemias, possibly induced by excessive glucocorticoid use, have been implicated in the formation of canine gallbladder mucoceles. 75 Certain breeds (Shetland Sheepdog), gene mutations and endocrinopathies (hypothyroidism and hypercortisolism) have been associated with canine gallbladder mucoceles.75,76
Clinical signs
Reported clinical signs have included vomiting, anorexia, lethargy, weight loss and icterus.18,39 Conceivably, these could have been associated with concurrent diseases, such as EHBDO, hepatic lipidosis and cholestasis, and not with the mucocele per se.
Diagnosis
Gallbladder mucoceles can been seen with abdominal ultrasound. Cholecystocentesis usually does not yield any fluid because of the thick, inspissated bile. 39 Histology of the gallbladder wall would show cystic mucinous hyperplasia.11,39
Treatment
Surgical removal of the gallbladder was described by Woods et al. 18 Other treatment approches have included cholecystojejunostomy, 39 and the use of choleretic drugs such as UDCA. 18 The prevailing opinion is that, for dogs, cholecystectomy is the most effective treatment. 77
Prognosis
Two of the three cats reported in the literature did well.18,39 Possible complications include rupture of the gallbladder and recurrence. The prognosis is guarded in cases of feline EHBDO and hepatic lipidosis. High mortality rates have been reported with biliary diversion surgery in cats. 12
Gallbladder infarctions
Aetiology
Thrombosis of the cystic artery, a branch of the hepatic artery and the sole arterial blood supply to the gallbladder, may cause gallbladder infarcts. 11 Theoretically, torsion of the gallbladder may also cause arterial occlusion and infarction. The fundus of the gallbladder has been specified as being the site most prone to rupture as a sequela to ischaemia. 71 While necrotic areas and ischaemia have been observed in the gallbladders of cats, the authors of that study linked these findings to anaerobic bacterial infection. 26 Gallbladder infarcts have been described in a series of dogs, but not in cats. 78
The bile peritonitis that is expected to follow gallbladder infarction and necrosis is rarely encountered in feline practice, and was reported only once (0.3%) in 396 cases studied. 79 This might be due to the biliary epithelium exhibiting excellent regenerative properties, as has been recognised in dogs. 39
Clinical signs
Clinical signs (in dogs) have included vomiting, icterus, anorexia, pyrexia and diarrhoea. 78 Bile peritonitis in two cats was associated with anorexia and vomiting. 71
Diagnosis
Ultrasound can help in identifying abnormalities in the gallbladder, as well as in showing poor abdominal detail suggestive of abdominal effusion.71,78 In a review of 12 canine cases, surgery confirmed ruptured and distended gallbladders, but no torsions were encountered. 78 Histology of the gallbladder wall shows necrosis and thrombosis of the artery. 11
Cytology of abdominal effusion in bile peritonitis has revealed predominantly neutrophils and macrophages, with golden to greenish-brown material in the cytoplasm of macrophages or in the background. 79 Bile leakage was shown to be diagnosed effectively by a greater than two-fold increase in the bilirubin concentration of the effusion compared with serum. 71
Treatment
Damaged gallbladders must be surgically removed and trauma causing bile peritonitis must be surgically repaired. Supportive therapies, such as fluid therapy and assisted feeding, might be required to assure the patient‘s recovery.
Prognosis
Conjecturing from the scant information available, a guarded prognosis is anticipated. Thrombosis might be caused by vascular problems, which may have a far greater impact on the cat than gallbladder infarction. Biliary disease in cats is associated with nausea, vomiting and anorexia, which predisposes the patient to hepatic lipidosis. Bile salts are toxic to tissues, leading to tissue necrosis and the growth of bacteria. 7 A further consideration is that biliary diversion surgery has been shown to be associated with high mortality rates.12,80
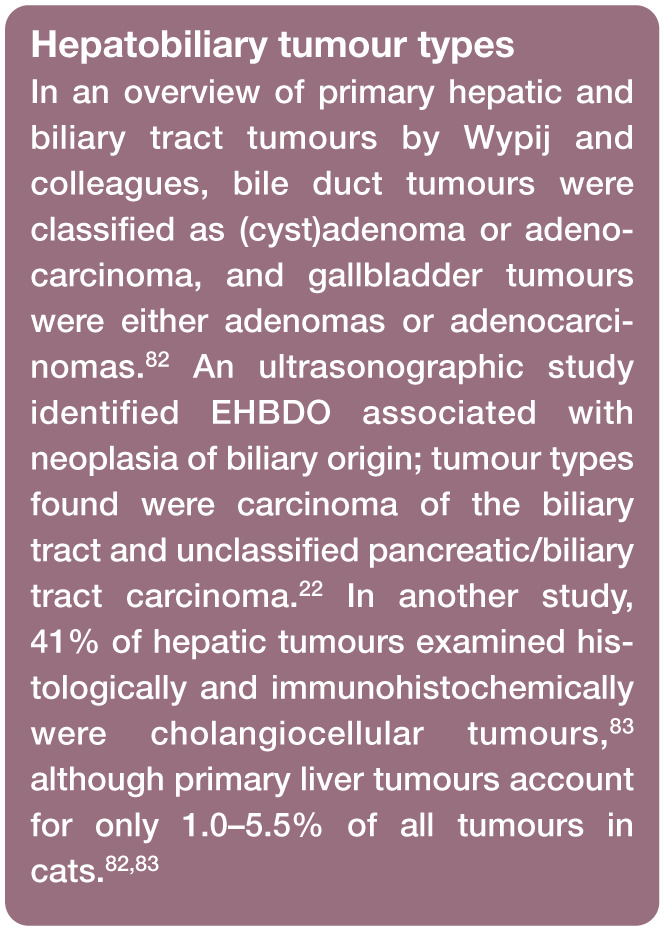
Neoplasia
Aetiology
In cats, neoplasms of the biliary system occur more frequently than neoplasms of hepatic cell origin. 81 A brief summary of primary tumour types that have been identified is given in the box on the left.
Cholangitis was present concurrently in 3/25 cats suffering from cholangiocellular tumours, while another three cats had concurrent auto - somal dominant polycystic kidney disease (AD-PKD). 83 It has been proposed that cholangitis may be involved in the aetiology of cholangiocellular feline tumours. 83
Bile duct adenomas have been found to be associated with bile duct adenocarcinomas, suggesting that adenoma, metaplasia and dysplasia may be viewed as precursor lesions in cats. 81 This same study found no choleliths in the cats with either gallbladder carcinoma or bile duct adenocarcinomas. 81
Lymphoma and mast cell tumours were most frequently found as concurrent neoplasms, although lymphoma of the gallbladder is extremely rare.65,81 There is a single case report of urinary bladder lymphoma associated with concurrent involvement of the gallbladder. 84 Feline neuroendocrine epithelial tumours have been reported, possibly the result of a malignant transformation of hepatic stem cells.81,82
Clinical signs
Male cats are overrepresented for biliary adenocarcinomas and cystadenocarcinomas, with up to 38% of cats being asymptomatic. 82 In symptomatic cases, clinical signs are similar to those seen in other hepatobiliary disorders, and include icterus. 82 Paraneoplastic alopecia has been reported in two cats with hepatocellular carcinoma and bile duct carcinoma.41,42
Diagnosis
Severe thickening of the gallbladder wall or CBD has been observed on ultrasound.22,84 Radiography, cytology and tissue biopsy may all be helpful in identifying neoplastic lesions. 82
Treatment
A large part of the liver can be surgically resected without impairing hepatic function, so surgical removal of focal lesions seems to be the best option. Systemic chemotherapy is relatively ineffective.82,85
Prognosis
Up to 65% of primary hepatobiliary tumours in cats are reported to be benign. 82 However, malignant biliary tumours have been found to have higher metastatic rates than hepatocellular carcinomas. 81
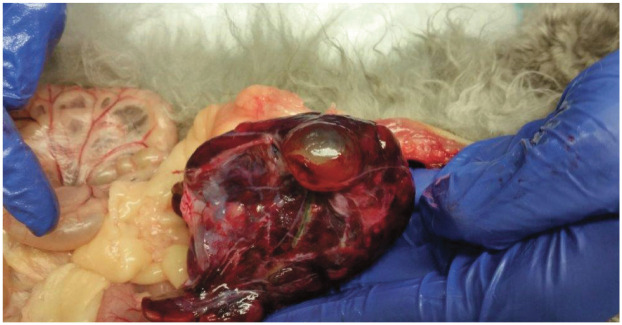
Cystic diseases
Cysts in the liver (Figure 7) always arise from the bile system, and are therefore also considered a biliary disease.
Figure 7.
Liver cyst, an incidental finding at necropsy. Courtesy of Marleen Assink
Solitary biliary cysts
Case reports have documented biliary cysts in cougars, lions and leopards, as well as in domestic cats.27,30,86,87
Aetiology
Extrahepatic solitary cysts of the biliary system are found occasionally in cats. 30 To the authors’ knowledge, no aetiology has been suggested.
In humans, where the condition is also encountered, several aetiological mechanisms have been proposed: 88
Differences in epithelial cell proliferation, causing the area with faster proliferation rates to distend;
Reflux of pancreatic enzymes into the cystic duct due to a defect in the pancreaticobiliary sphincter;
Localised weakness in the wall of the biliary duct.
Experimentally, biliary cysts have been created in puppies, but not in adult dogs, by scraping the mucosa of the bile duct followed by CBD ligation. 88
Biliary cystadenomas, an uncommon benign liver tumour of older cats, may be encountered as a focal or multifocal cystic lesion. 89 While the tissue of origin is still unknown, the cysts are speculated to arise from ‘small retention cysts associated with embryologic bile ducts that do not connect to the main biliary tree’. 89
Clinical signs
Clinical signs in a domestic shorthair cat with a cyst arising from the CBD included polyphagia, weight loss, nervousness, and urinating in the house due to increased pressure on the bladder by the cyst. 30 Chronic vomiting and anorexia were reported in another case, although this cat also suffered from suppurative cholangitis which could have caused these clinical signs. 27
Hepatobiliary cysts have been found as intrapericardial lesions following diaphragmatic herniation, and were the cause of progressive exercise intolerance and coughing. 87
Biliary cystadenomas were reported to be associated with anorexia, lethargy, weight loss, occasional vomiting and weakness, but no abdominal pain or discomfort. 89
Diagnosis
Large cysts have been found during clinical examination.30,89 Diagnostic imaging might be helpful in locating biliary cysts, and some are found at necropsy (Figure 8).86,89 Clinical laboratory data may be normal, but elevations in liver enzymes (eg, alanine aminotransferase and alkaline phosphatase) and bilirubin have been reported.30,89 Clotting times were found to be within normal reference intervals, 30 and fluid analysis revealed high protein content and limited mixed bacterial growth. 30 True cysts usually contain bile.27,89
Figure 8.

Biliary cyst. Reprinted with permission from the WSAVA Standards for Clinical and Histological Diagnosis of Canine and Feline Liver Diseases. 11 Image courtesy of the Society of Comparative Hepatology
Treatment
Complete or partial surgical resection is the treatment of choice when the cyst needs to be removed because of mechanical compression on adjacent structures.30,89
Prognosis
The prognosis for cats with biliary cystadenomas is good, due to the benign nature of these cysts. 89 However, as the cause of solitary biliary cysts is usually unknown, recurrence might occur and the long-term outcome is uncertain. 30
Congenital biliary cystic disease
Aetiology
Feline cystic liver disease is most often multifocal and has been found in 68% of cats with polycystic kidney disease (PKD).30,31 Persian cats inherit PKD as an autosomal dominant trait. Besides hepatic cysts, liver fibrosis is also commonly seen in cats with PKD (Figure 9). 31
Figure 9.
Juvenile biliary cystic disease with hepatic fibrosis – (a) macroscopy, (b) microscopy. Reprinted with permission from the WSAVA Standards for Clinical and Histological Diagnosis of Canine and Feline Liver Diseases. 11 Images courtesy of the Society of Comparative Hepatology
Increased epithelial proliferation is involved in the formation of renal cysts in Persian cats. This occurs intermittently and in the early stages of cyst formation. 90
Clinical signs
PKD in Persian cats is clinically similar to human AD-PKD.11,90 Clinical signs are mostly a result of the renal disease, and not the hepatic cysts.
Diagnosis
Both renal and hepatic cysts may be visualised ultrasonographically. Hepatic lesions comprising cystic malformation and fibrosis are identified on liver histology.
Treatment
There is no treatment for PKD. Breeding programmes and genetic screening have contributed to a reduction in the number of affected cats over the years.
Prognosis
The prognosis for PKD is fair, since most cats only start showing clinical signs at an advanced age.
Key Points
Biliary disease is more common in cats than disease of the hepatic parenchyma.
Due to limited capacity for glucuronide conjugation of drugs and toxins, cats are prone to hepatotoxic injury. A number of frequently used veterinary drugs can be toxic to cats.
Enteric bacteria have been implicated in inflammatory liver disease.
Changes to the biliary tree, such as dilatations, will persist and will increase the patient’s sensitivity to ascending bacterial infection from the intestines.
One in eight cats have some form of accessory gallbladder. Usually, there are no clinical signs and these anomalies are found incidentally on ultrasound examination or at necropsy.
Most cats with choleliths, lymphocytic cholangitis and neoplasia are male.
The gallbladder has only a single artery supplying blood, but infarcts have never been described in cats.
Biliary cysts are encountered in many felids, not just domestic cats. In domestic cats, liver cysts are linked to polycystic kidney disease.
Histology, cytology and culture are valuable diagnostic tools in feline biliary disease.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The authors received no financial support for the research, authorship and/or publication of this article.
References
- 1. Larsen WJ. Human embryology. 3rd ed. Philadelphia: Churchill Livingstone, 2001. [Google Scholar]
- 2. Young B, Heath JW. Wheater’s functional histology. 4th ed. Philadelphia: Churchill Livingstone, 2000. [Google Scholar]
- 3. Trepanier LA. Idiosyncratic drug toxicity affecting the liver, skin, and bone marrow in dogs and cats. Vet Clin North Am Small Anim Pract 2013; 43: 1055–1066. [DOI] [PubMed] [Google Scholar]
- 4. Cullen JM. Pathologic basis of veterinary disease. 4th ed. St Louis, MO: Mosby, 2007. [Google Scholar]
- 5. Dyce KM, Sack WO, Wensing CJG. Textbook of veterinary anatomy. 3rd ed. Elsevier Health, 2002. [Google Scholar]
- 6. Taylor W. The bile acid composition of rabbit and cat gallbladder bile. J Steroid Biochem 1977; 8: 1077–1084. [DOI] [PubMed] [Google Scholar]
- 7. Neer TM. A review of disorders of the gallbladder and extrahepatic biliary tract in the dog and cat. J Vet Intern Med 1992; 6: 186–192. [DOI] [PubMed] [Google Scholar]
- 8. Markwell PJ, Earle KE. Taurine: an essential nutrient for the cat. A brief review of the biochemistry of its requirement and the clinical consequences of deficiency. Nutr Res 1995; 15: 53–58. [Google Scholar]
- 9. Center SA. Diseases of the gallbladder and biliary tree. Vet Clin North Am Small Anim Pract 2009; 39: 543–598. [DOI] [PubMed] [Google Scholar]
- 10. Vakili K, Pomfret EA. Biliary anatomy and embryology. Surg Clin North Am 2008; 88: 1159–1174. [DOI] [PubMed] [Google Scholar]
- 11. WSAVA Liver Standardization Group. WSAVA Standards for Clinical and Histological Diagnosis of Canine and Feline Liver Diseases. Philadelphia: Saunders, Elsevier, 2006. Also available as an e-book at http://www.vetvisuals.com/home-society-of-comparative-hepatology/sch (accessed May 29, 2016). [Google Scholar]
- 12. Bacon NJ, White RA. Extrahepatic biliary tract surgery in the cat: a case series and review. J Small Anim Pract 2003; 44: 231–235. [DOI] [PubMed] [Google Scholar]
- 13. van Beusekom CD, Fink-Gremmels J, Schrickx JA. Comparing the glucuronidation capacity of the feline liver with substrate-specific glucuronidation in dogs. J Vet Pharmacol Ther 2014; 37: 18–24. [DOI] [PubMed] [Google Scholar]
- 14. Center SA. Interpretation of liver enzymes. Vet Clin North Am Small Anim Pract 2007; 37: 297–333. [DOI] [PubMed] [Google Scholar]
- 15. van Beusekom CD, van den Heuvel JJ, Koenderink JB, et al. The feline bile salt export pump: a structural and functional comparison with canine and human Bsep/BSEP. BMC Vet Res 2013; 9: 259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Washabau RJ, Day MJ. Liver. Canine and feline gastroenterology. St Louis, MO: Elsevier Saunders, 2013, pp 849–957. [Google Scholar]
- 17. Boyden EA. The accessory gall-bladder – an embryological and comparative study of aberrant biliary vesicles occurring in man and the domestic mammals. Am J Anat 1926; 38: 177–231. [Google Scholar]
- 18. Woods KS, Brisson BA, Defarges AM, et al. Congenital duplex gallbladder and biliary mucocele associated with partial hepatic cholestasis and cholelithiasis in a cat. Can Vet J 2012; 53: 269–273. [PMC free article] [PubMed] [Google Scholar]
- 19. Rothuizen J. Important clinical syndromes associated with liver disease. Vet Clin North Am Small Anim Pract 2009; 39: 419–437. [DOI] [PubMed] [Google Scholar]
- 20. Center SA. Chronic liver disease: current concepts of disease mechanisms. J Small Anim Pract 1999; 40: 106–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Leveille R, Biller DS, Shiroma JT. Sonographic evaluation of the common bile duct in cats. J Vet Intern Med 1996; 10: 296–299. [DOI] [PubMed] [Google Scholar]
- 22. Gaillot HA, Penninck DG, Webster CR, et al. Ultrasonographic features of extrahepatic biliary obstruction in 30 cats. Vet Radiol Ultrasound 2007; 48: 439–447. [DOI] [PubMed] [Google Scholar]
- 23. Harran N, d’Anjou MA, Dunn M, et al. Gallbladder sludge on ultrasound is predictive of increased liver enzymes and total bilirubin in cats. Can Vet J 2011; 52: 999–1003. [PMC free article] [PubMed] [Google Scholar]
- 24. Brioschi V, Rousset N, Ladlow JF. Imaging diagnosis – extrahepatic biliary tract obstruction secondary to a biliary foreign body in a cat. Vet Radiol Ultrasound 2014; 55: 628–631. [DOI] [PubMed] [Google Scholar]
- 25. Chapman SE, Hostutler RA. A laboratory diagnostic approach to hepatobiliary disease in small animals. Vet Clin North Am Small Anim Pract 2013; 43: 1209–1225. [DOI] [PubMed] [Google Scholar]
- 26. Brain PH, Barrs VR, Martin P, et al. Feline cholecystitis and acute neutrophilic cholangitis: clinical findings, bacterial isolates and response to treatment in six cases. J Feline Med Surg 2006; 8: 91–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lecoindre P, Chevallier M. Extrahepatic biliary tract diseases in cats. Case reports and bibliographic synthesis. Revue Méd Vét 2004; 155: 591–597. [Google Scholar]
- 28. Rothuizen J, Boomkens SY, van den Ingh TSGAM. Introduction: cholangitis in cats. Infectious causes of hepatitis in dogs and cholangitis in cats. Utrecht: Utrecht University, 2005. [Google Scholar]
- 29. Lucke VM, Davies JD. Progressive lymphocytic cholangitis in the cat. J Small Anim Pract 1984; 25: 249–260. [Google Scholar]
- 30. Best EJ, Bush DJ, Dye C. Suspected choledochal cyst in a domestic shorthair cat. J Feline Med Surg 2010; 12: 814–817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bosje JT, van den Ingh TS, van der Linde-Sipman JS. Polycystic kidney and liver disease in cats. Vet Q 1998; 20: 136–139. [DOI] [PubMed] [Google Scholar]
- 32. Harvey AM, Holt PE, Barr FJ, et al. Treatment and long-term follow-up of extrahepatic biliary obstruction with bilirubin cholelithiasis in a Somali cat with pyruvate kinase deficiency. J Feline Med Surg 2007; 9: 424–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Elwood CM, White RN, Freeman K, et al. Cholelithiasis and hyperthyroidism in a cat. J Feline Med Surg 2001; 3: 247–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Eich CS, Ludwig LL. The surgical treatment of cholelithiasis in cats: a study of nine cases. J Am Anim Hosp Assoc 2002; 38: 290–296. [DOI] [PubMed] [Google Scholar]
- 35. Wagner KA, Hartmann FA, Trepanier LA. Bacterial culture results from liver, gallbladder, or bile in 248 dogs and cats evaluated for hepatobiliary disease: 1998–2003. J Vet Intern Med 2007; 21: 417–424. [DOI] [PubMed] [Google Scholar]
- 36. Callahan Clark JE, Haddad JL, Brown DC, et al. Feline cholangitis: a necropsy study of 44 cats (1986–2008). J Feline Med Surg 2011; 13: 570–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Xavier FG, Morato GS, Righi DA, et al. Cystic liver disease related to high Platynosomum fastosum infection in a domestic cat. J Feline Med Surg 2007; 9: 51–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Haney DR, Christiansen JS, Toll J. Severe cholestatic liver disease secondary to liver fluke (Platynosomum concinnum) infection in three cats. J Am Anim Hosp Assoc 2006; 42: 234–237. [DOI] [PubMed] [Google Scholar]
- 39. Bennett SL, Milne M, Slocombe RF, et al. Gallbladder mucocoele and concurrent hepatic lipidosis in a cat. Aust Vet J 2007; 85: 397–400. [DOI] [PubMed] [Google Scholar]
- 40. Moores AL, Gregory SP. Duplex gall bladder associated with choledocholithiasis, cholecystitis, gall bladder rupture and septic peritonitis in a cat. J Small Anim Pract 2007; 48: 404–409. [DOI] [PubMed] [Google Scholar]
- 41. Marconato L, Albanese F, Viacava P, et al. Paraneoplastic alopecia associated with hepatocellular carcinoma in a cat. Vet Dermatol 2007; 18: 267–271. [DOI] [PubMed] [Google Scholar]
- 42. Pascal-Tenorio A, Olivry T, Gross TL, et al. Paraneoplastic alopecia associated with internal malignancies in the cat. Vet Dermatol 1997; 8: 47–52. [DOI] [PubMed] [Google Scholar]
- 43. Weiss DJ, Armstrong PJ, Gagne J. Inflammatory liver disease. Semin Vet Med Surg (Small Anim) 1997; 12: 22–27. [DOI] [PubMed] [Google Scholar]
- 44. Twedt DC, Cullen J, McCord K, et al. Evaluation of fluorescence in situ hybridization for the detection of bacteria in feline inflammatory liver disease. J Feline Med Surg 2014; 16: 109–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Gagne JM, Weiss DJ, Armstrong PJ. Histopathologic evaluation of feline inflammatory liver disease. Vet Pathol 1996; 33: 521–526. [DOI] [PubMed] [Google Scholar]
- 46. Savary-Bataille KC, Bunch SE, Spaulding KA, et al. Percutaneous ultrasound-guided cholecystocentesis in healthy cats. J Vet Intern Med 2003; 17: 298–303. [DOI] [PubMed] [Google Scholar]
- 47. Sung JY, Leung JW, Olson ME, et al. Demonstration of transient bacterobilia by foreign body implantation in feline biliary tract. Dig Dis Sci 1991; 36: 943–948. [DOI] [PubMed] [Google Scholar]
- 48. Marolf AJ, Leach L, Gibbons DS, et al. Ultrasonographic findings of feline cholangitis. J Am Anim Hosp Assoc 2012; 48: 36–42. [DOI] [PubMed] [Google Scholar]
- 49. Rothuizen J, Twedt DC. Liver biopsy techniques. Vet Clin North Am Small Anim Pract 2009; 39: 469–480. [DOI] [PubMed] [Google Scholar]
- 50. Cole TL, Center SA, Flood SN, et al. Diagnostic comparison of needle and wedge biopsy specimens of the liver in dogs and cats. J Am Vet Med Assoc 2002; 220: 1483–1490. [DOI] [PubMed] [Google Scholar]
- 51. Proot SJ, Rothuizen J. High complication rate of an automatic Tru-Cut biopsy gun device for liver biopsy in cats. J Vet Intern Med 2006; 20: 1327–1333. [DOI] [PubMed] [Google Scholar]
- 52. Kaminski DL, Feinstein WK, Deshpande YG. The production of experimental cholecystitis by endotoxin. Prostaglandins 1994; 47: 233–245. [DOI] [PubMed] [Google Scholar]
- 53. Otte CM, Penning LC, Rothuizen J, et al. Retrospective comparison of prednisolone and ursodeoxycholic acid for the treatment of feline lymphocytic cholangitis. Vet J 2013; 195: 205–209. [DOI] [PubMed] [Google Scholar]
- 54. Nilsson B, Delbro D, Hedin L, et al. Role of cyclooxygenase-2 for fluid secretion by the inflamed gallbladder mucosa. J Gastrointest Surg 1998; 2: 269–277. [DOI] [PubMed] [Google Scholar]
- 55. Mayumi T, Someya K, Ootubo H, et al. Progression of Tokyo Guidelines and Japanese Guidelines for management of acute cholangitis and cholecystitis. J UOEH 2013; 35: 249–257. [DOI] [PubMed] [Google Scholar]
- 56. Boomkens SY, Kusters JG, Hoffmann G, et al. Detection of Helicobacter pylori in bile of cats. FEMS Immunol Med Microbiol 2004; 42: 307–311. [DOI] [PubMed] [Google Scholar]
- 57. Greiter-Wilke A, Scanziani E, Soldati S, et al. Association of Helicobacter with cholangiohepatitis in cats. J Vet Intern Med 2006; 20: 822–827. [DOI] [PubMed] [Google Scholar]
- 58. Kordick DL, Brown TT, Shin K, et al. Clinical and pathologic evaluation of chronic Bartonella henselae or Bartonella clarridgeiae infection in cats. J Clin Microbiol 1999; 37: 1536–1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Otte CM, Gutierrez OP, Favier RP, et al. Detection of bacterial DNA in bile of cats with lymphocytic cholangitis. Vet Microbiol 2012; 156: 217–221. [DOI] [PubMed] [Google Scholar]
- 60. Day MJ. Immunohistochemical characterization of the lesions of feline progressive lymphocytic cholangitis/cholangiohepatitis. J Comp Pathol 1998; 119: 135–147. [DOI] [PubMed] [Google Scholar]
- 61. Addie D, Belak S, Boucraut-Baralon C, et al. Feline infectious peritonitis. ABCD guidelines on prevention and management. J Feline Med Surg 2009; 11: 594–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Gruffydd-Jones T. Inflammatory liver disease. Permanente educatie gezelschapsdieren: Cats with non specific signs. Departement geneeskunde van gezelschapsdieren te Utrecht, 2009. [Google Scholar]
- 63. Raskin RE. Cytology of the liver: review of basic changes. International Congress of the Italian Association of Companion Animal Veterinarians. Rimini, Italy, 2006, pp 92–93. [Google Scholar]
- 64. Wilson HM. Feline alimentary lymphoma: demystifying the enigma. Top Companion Anim Med 2008; 23: 177–184. [DOI] [PubMed] [Google Scholar]
- 65. Baxter KJ, Hill RC, Parfitt SL, et al. Gastrointestinal small-cell lymphoma with gall bladder involvement in a cat. J Feline Med Surg 2012; 14: 267–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Roth L. Comparison of liver cytology and biopsy diagnoses in dogs and cats: 56 cases. Vet Clin Pathol 2001; 30: 35–38. [DOI] [PubMed] [Google Scholar]
- 67. Wang KY, Panciera DL, Al-Rukibat RK, et al. Accuracy of ultrasound-guided fine-needle aspiration of the liver and cytologic findings in dogs and cats: 97 cases (1990–2000). J Am Vet Med Assoc 2004; 224: 75–78. [DOI] [PubMed] [Google Scholar]
- 68. Salomao M, Souza-Dantas LM, Mendes-de-Almeida F, et al. Ultrasonography in hepatobiliary evaluation of domestic cats (Felis catus, L., 1758) infected by Platynosomum Looss, 1907. Int J Appl Res Vet Med 2005; 3: 271–279. [Google Scholar]
- 69. Senior K. Time to end our neglect of liver flukes. Lancet Infect Dis 2009; 9: 276. [Google Scholar]
- 70. Marcos LA, Terashima A, Gotuzzo E. Update on hepatobiliary flukes: fascioliasis, opisthorchiasis and clonorchiasis. Curr Opin Infect Dis 2008; 21: 523–530. [DOI] [PubMed] [Google Scholar]
- 71. Ludwig LL, McLoughlin MA, Graves TK, et al. Surgical treatment of bile peritonitis in 24 dogs and 2 cats: a retrospective study (1987–1994). Vet Surg 1997; 26: 90–98. [DOI] [PubMed] [Google Scholar]
- 72. Hittmair KM, Vielgrader HD, Loupal G. Ultrasonographic evaluation of gallbladder wall thickness in cats. Vet Radiol Ultrasound 2001; 42: 149–155. [DOI] [PubMed] [Google Scholar]
- 73. Ko CW, Lee SP. Gallstone formation. Local factors. Gastroenterol Clin North Am 1999; 28: 99–115. [DOI] [PubMed] [Google Scholar]
- 74. Soloway RD, Trotman BW, Ostrow JD. Pigment gallstones. Gastroenterology 1977; 72: 167–182. [PubMed] [Google Scholar]
- 75. Aguirre AL, Center SA, Randolph JF, et al. Gallbladder disease in Shetland Sheepdogs: 38 cases (1995–2005). J Am Vet Med Assoc 2007; 231: 79–88. [DOI] [PubMed] [Google Scholar]
- 76. Cullen JM, Willson CJ, Minch JD, et al. Lack of association of ABCB4 insertion mutation with gallbladder mucoceles in dogs. J Vet Diagn Invest 2014; 26: 434–436. [DOI] [PubMed] [Google Scholar]
- 77. Walter R, Dunn ME, d’Anjou MA, et al. Nonsurgical resolution of gallbladder mucocele in two dogs. J Am Vet Med Assoc 2008; 232: 1688–1693. [DOI] [PubMed] [Google Scholar]
- 78. Holt DE, Mehler S, Mayhew PD, et al. Canine gallbladder infarction: 12 cases (1993–2003). Vet Pathol 2004; 41: 416–418. [DOI] [PubMed] [Google Scholar]
- 79. Gavazza A, Turinelli V, Lubas G. Effusion in the cat: classification of 396 fluids according to a problem-oriented scheme. Comp Clin Pathol 2013; 22: 517–521. [Google Scholar]
- 80. Monticelli P, Stathopoulou TR, Lee K, et al. Life-threatening perianaesthetic complications in five cats undergoing biliary tract surgery: case series and literature review. J Feline Med Surg. Epub ahead of print 20 April 2016. DOI: 1098612X16646152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Patnaik AK. A morphologic and immunocytochemical study of hepatic neoplasms in cats. Vet Pathol 1992; 29: 405–415. [DOI] [PubMed] [Google Scholar]
- 82. Wypij J, Fan TM, de Lorimier L-P. Primary hepatic and biliary tract tumors in dogs and cats: an overview. Vet Med 2006; 101: 384–394. [Google Scholar]
- 83. van Sprundel RG, van den Ingh TS, Guscetti F, et al. Classification of primary hepatic tumours in the cat. Vet J 2014; 202: 255–266. [DOI] [PubMed] [Google Scholar]
- 84. Geigy CA, Dandrieux J, Miclard J, et al. Extranodal B-cell lymphoma in the urinary bladder with cytological evidence of concurrent involvement of the gall bladder in a cat. J Small Anim Pract 2010; 51: 280–287. [DOI] [PubMed] [Google Scholar]
- 85. Balkman C. Hepatobiliary neoplasia in dogs and cats. Vet Clin North Am Small Anim Pract 2009; 39: 617–625. [DOI] [PubMed] [Google Scholar]
- 86. Bernard JM, Newkirk KM, McRee AE, et al. Hepatic lesions in 90 captive nondomestic felids presented for autopsy. Vet Pathol 2015; 52: 369–376. [DOI] [PubMed] [Google Scholar]
- 87. Scruggs SM, Bright JM. Chronic cardiac tamponade in a cat caused by an intrapericardial biliary cyst. J Feline Med Surg 2010; 12: 338–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Flanigan DP. Biliary cysts. Ann Surg 1975; 182: 635–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Nyland TG, Koblik PD, Tellyer SE. Ultrasonographic evaluation of biliary cystadenomas in cats. Vet Radiol Ultrasound 1999; 40: 300–306. [DOI] [PubMed] [Google Scholar]
- 90. Eaton KA, Biller DS, DiBartola SP, et al. Autosomal dominant polycystic kidney disease in Persian and Persian-cross cats. Vet Pathol 1997; 34: 117–126. [DOI] [PubMed] [Google Scholar]