Abstract
Axillary blockade of the brachial plexus (BP) is advocated in humans and dogs for surgical procedures carried out on the foot, carpus and elbow as it provides complete analgesia distally from above the elbow joint. The aim of this study was to develop an ultrasound (US)-guided approach to block the BP in cats. Two groups of 12 feline cadavers each were used to compare two different techniques to block the BP at the axillary level. The reliability of the techniques was assessed by anatomical and computed tomography (CT) studies. Cadavers of the first group were positioned in dorsal recumbency with the forelimb to be blocked adducted (thoracic limbs flexed and orientated caudally) (FAD technique). The second group was positioned in dorsal recumbency with the forelimb abducted 90° (FAB technique). The accuracy of the techniques was determined by US after injecting 1 ml blue ink along the BP nerves, and by CT after injecting 1 ml of an iodinated contrast medium. The anatomical and CT studies confirmed the accuracy of the US location of the BP nerves. Staining of the axillaris, musculocutaneous, radialis, medianus and ulnaris nerves was observed in 100% of cats using the FAB technique and in 66% of the cats using the FAD technique. Rate of complications was higher in the FAD technique. In conclusion, a US-guided axillary approach to the BP by the use of a FAB technique is a safe and feasible procedure to block the BP in the cat. Further studies are needed to ascertain whether the technique can be applied in a clinical setting.
Introduction
Peripheral nerve blocks have traditionally been performed using anatomical landmarks or nerve electrostimulation to locate the target nerves. 1 Ultrasound (US)-guided techniques are now gaining popularity to facilitate these blocks. Ultrasonographic guidance for locoregional anaesthesia offers several advantages when compared with electrolocation or blind techniques; direct visualisation of the target nerves may reduce the need for multiple needle passes, thus reducing tissue damage and risk of vascular laceration; in addition, blockade performance times may also decrease.2–4 However, when trained anaesthesiologists perform the blocks the onset times to achieve the blocks and the success rates are similar when electrolocation and US-guided techniques are compared. 5 In spite of this, direct visualisation of the spreading of local anaesthetic (LA) during injection, with the possibility of repositioning the needle in the case of misdistribution of LA, may increase the precision of the blockade, reducing the volume of LA necessary in comparison with blind or electrolocation techniques.6–8
Blockade of the brachial plexus (BP) has been recommended in dogs for surgical procedures carried out on the foot, carpus and elbow, as it produces complete analgesia distally from above the elbow joint.9–11
Axillary blockade of the BP can be performed at two different levels: either at the level of the scapulohumeral joint or cranial to the acromion.11–14 A more distal technique, RUMM block, has been described to desensitise the individual nerves that innervate the thoracic limb (radialis, ulnaris, medianus and musculocutaneous nerves) at the level of the mid-humerus. 15 The paravertebral BP blockade desensitises the spinal nerves forming the BP as they emerge from the spinal cord at the level of the intervertebral foramina.16–18
In cats, the normal ultrasonographic appearance of the BP has recently been reported. 19 However, to the authors’ knowledge, there are no descriptions of an US-guided technique to block the BP in the cat.
The aim of this study was to assess the feasibility of US-guided BP blockade in the cat. For this, two techniques to block the BP by US were compared, assessing the success of the nerve staining and the complication rates observed.
Materials and methods
Animals
The project was approved by the Local Animal Care and Ethics Committee of the University of Murcia. A total of 24 fresh intact adult cadaver cats with a body weight of 3.36 kg (range 2.85–4 kg) obtained from the Local Zoonoses and Public Health Service were employed. All the cats were humanely euthanased for reasons unrelated to this study. The studies were carried out within a period of 5 h after euthanasia. The animals were randomly divided into two groups to evaluate two different forelimb positions to block the BP. Only one forelimb was used on each cat; therefore, a total of 24 limbs were blocked. Nine animals of each group were employed in order to study the distribution of injectate in the BP by means of an anatomical study, and the remaining three animals were subjected to a computed tomographic (CT) study.
Procedures
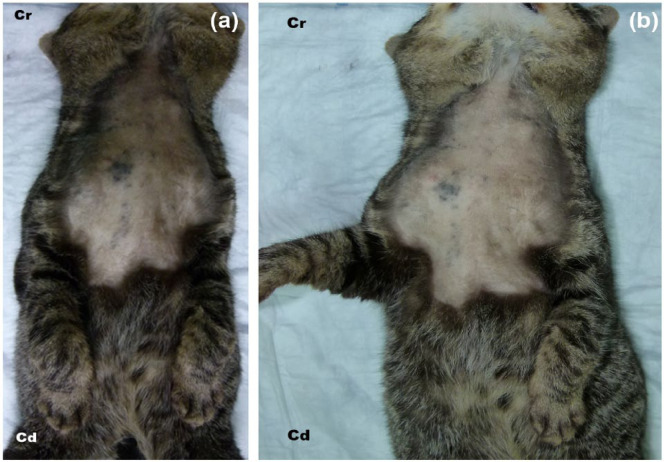
The hair was clipped and the skin cleaned from the occipital region to the last rib, including the forelimb, up to the elbow. The cats were placed in dorsal recumbency with both forelimbs adducted (thoracic limbs flexed and orientated caudally) (FAD technique) (Figure 1a) or with the forelimb to be blocked abducted 90° and the other one adducted to the side (FAB technique) (Figure 1b). The axillary area was scanned in all cases with the transducer positioned parallel to the spine and the orientation marker directed cranially. 18 A 4–13 MHz linear array transducer set at a frequency of 13 MHz (My Lab 70; Esaote) and at a depth of 2 cm was employed to perform these scans. Once the nerve roots of the BP were identified, a non-traumatic peripheral nerve block needle (Stimuplex D 0.71 × 40 mm 30°; B Braun Melsungen AG) was inserted craniomedial to the shoulder joint and then advanced in a cranial to caudal direction. The needle was inserted in-plane with respect to the ultrasound transducer. The tip of the needle was positioned in the most caudal aspect of the BP, and 1 ml of dye solution obtained from mixing 0.5 ml of blue ink and 0.5 ml of saline solution (1:1 ratio) was injected along to the medial aspect of the entire BP as the needle was being progressively withdrawn in a caudal to cranial direction. For the CT study, 1 ml of iodinated contrast medium (150 mg/ml) obtained by mixing iohexol 300 mg/ml (Omnitrast 300; Bayer) and saline solution (1:1 ratio) was injected as described above. The distribution of the solution around the nerve roots was observed in real time by US. The US-guided location of the BP and administration of injectate were always performed by the same investigators (AAn, AAg). These investigators have significant clinical experience in the blockade of peripheral nerves using US-guided techniques.
Figure 1.
Positioning of the forelimbs. (a) FAD technique: both forelimbs are adducted. (b) FAB technique: the forelimb to be blocked is abducted 90°. Cr = cranial; Cd = caudal
Anatomical study
Gross dissection of the BP
Twelve forelimbs were immediately dissected to study the distribution of the ink along the BP. The skin was reflected from the elbow to the sternum to expose the muscles of the axillary region. The overlying fascia was removed. The pectorales superficiales and pectoralis profundus muscles were detached from their insertion sites at the proximal epiphysis of the humerus. The scapula and humerus were then abducted to expose the nerves and blood vessels located in the axillary space.
The presence of ink staining the nerves of the BP confirmed the accuracy of the US nerve location. The variables recorded to assess the outcome of each technique included the deposition of the ink in relation to the roots of the BP, and the length of the dye observed along the target nerves. The deposition of the dye in relation to the BP (staining score) was scored on a two-point scale and recorded individually for each nerve. An injection score of 1 was given when the nerve was stained and 2 when the nerve was not stained. Complications of the BP axillary block, such as intraneural injection, staining of the phrenicus nerve, spreading of the ink out of the axillary space or trauma to vascular structures, were recorded.
Cryosections
Red latex was introduced through the thoracic aorta in six fresh feline cadavers. These specimens were frozen at −20°C for 24 h and then at −80°C for another 24 h. Transverse cryosections at the level of the axillary space were obtained using a high-speed band saw set at a thickness of 5 mm. The sections were immediately placed in acetone at −40°C to preserve them frozen. Photographs of both faces of each frozen anatomic slice were taken to perform a cross-sectional study of the distribution of ink around the roots of the BP.
The deposition of the dye in relation to the BP nerves was scored on a three-point scale and recorded individually for each nerve. An injection score of 1 was given when the nerve was stained (epineural) or 2 when the nerve was not stained but dye was found in the perineural tissues <5 mm away from the nerve (perineural). When dye was found >5 mm away from the nerve, an injection score of 3 was given (peripheral). Injection was considered successful when the nerve was stained (injection score 1). 20
Complications of the techniques, such as intraneural injection, staining of the phrenicus nerve, spreading of the ink outside of the axillary space or trauma to vascular structures, were also recorded.
CT study
Six cats were employed in this part of the study. The injection of contrast medium was performed using the US-guided technique described above. CT (High speed dual; General Electric) scans were performed after the introduction of the needle and then immediately after the deposition of the ink. The cadavers were placed for the CT scans in the position employed to perform the US-guided BP blockade. Transverse CT scans, at a thickness of 1 mm, were obtained from the occipital region to the last rib. Bone and standard algorithms were used. Reformatted images were obtained in both sagittal and dorsal planes. The images were reviewed using a picture archiving and computer system (PACS) workstation, using bone (window width [WW] = 2000, window level [WL] = 800) and soft tissue (WW = 360, WL = 60) windows display settings. The CT images were evaluated to assess the position of the needle and the distribution of contrast medium. The spreading of the contrast along the axillary space was also measured. Reformatted images were used to visualise and measure the longest spreading distances of contrast medium in cranial-to-caudal, dorsal-to-ventral and medial-to-lateral directions. The spreading of contrast medium out of the axillary space was considered a complication of the technique.
Results
The BP was correctly identified by US in all cases. The BP appeared as a cluster of small, round hypoechoic structures surrounded by a thin hyperechoic rim in a transverse plane. This was confirmed by observing the spreading of ink around the target nerves in the dissected cadavers, as well as in the transverse cryosections. The needle was easily inserted and visualised using a single insertion and an in-plane technique.
Anatomical study
Gross dissection of the BP
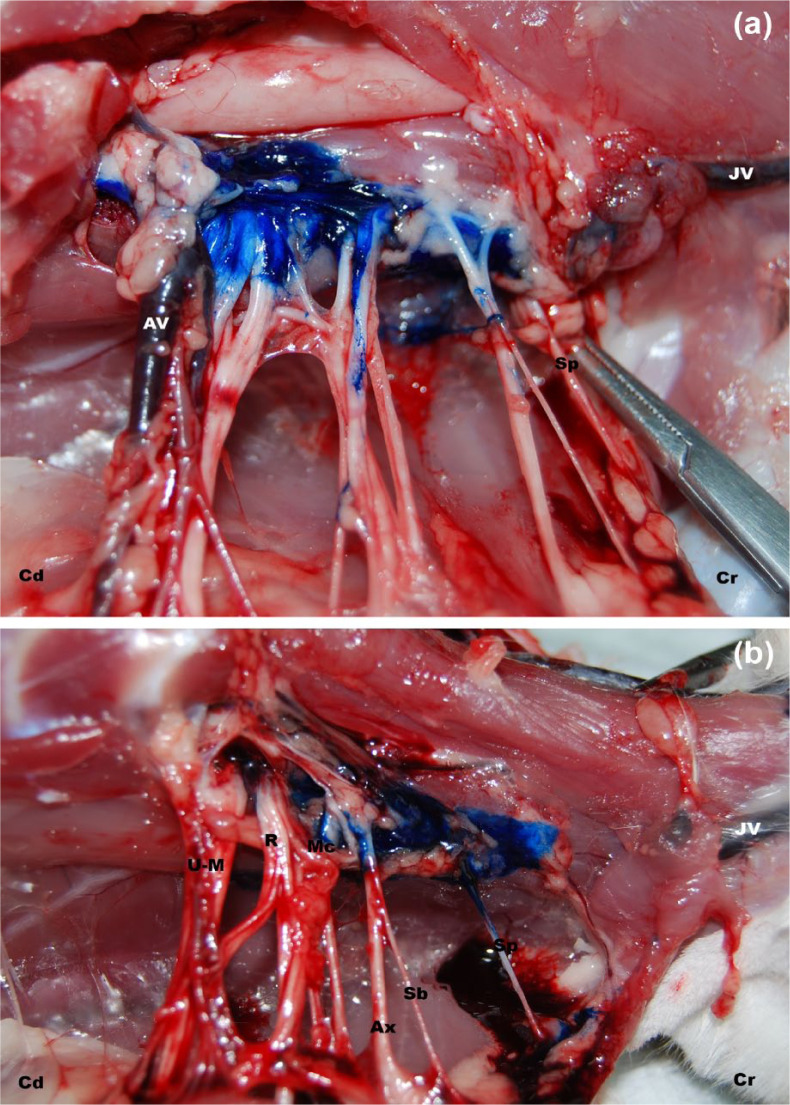
The number of the roots of the BP stained and their staining scores for the two studied techniques are summarised in Table 1. The suprascapularis nerve was not stained (staining score 2) in any case with the FAB technique; however, it was stained (staining score 1) in 3/6 cats when using the FAD technique. Subscapulares nerves were stained (staining score 1) in 3/6 cats when using the FAD technique and 2/6 using the FAB technique. The axillaris nerve was stained (staining score 1) in 3/6 cats when using the FAD, and in all cases (6/6) using the FAB technique. Musculocutaneous, radialis, medianus and ulnaris nerves were successfully stained (staining score 1) in all cases (6/6) using the FAB technique (Figure 2a). In the FAD group, staining (staining score 1) was observed for the musculocutaneous nerve in 3/6 cats, and for the radialis, medianus and ulnaris nerves in all cats (6/6) (Figure 2b).
Table 1.
Staining scores of the roots of the brachial plexus according to the position of the forelimb to be blocked
| Positioning of forelimbs | FAD | FAB | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cats | 1 | 2 | 3 | 4 | 5 | 6 | 1 | 2 | 3 | 4 | 5 | 6 |
| Nerves | ||||||||||||
| Suprascapularis N | 1 | 1 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Subscapularis N | 1 | 1 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 1 |
| Axillaris N | 1 | 1 | 1 | 2 | 2 | 2 | 1 | 1 | 1 | 1 | 1 | 1 |
| Musculocutaneous N | 1 | 1 | 1 | 2 | 2 | 2 | 1 | 1 | 1 | 1 | 1 | 1 |
| Radialis N | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Medianus N | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Ulnaris N | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
FAD = forelimbs adducted to the side; FAB = the forelimb to be blocked abducted 90° and the other one adducted to the side; 1 = nerve stained; 2 = nerve not stained
Figure 2.
Gross dissection of the brachial plexus (BP). (a) FAB technique: ink is observed staining all the roots of the BP nerves except the suprascapularis nerve (Sp). (b) FAD technique: ink is observed around the suprascapularis (Sp), subscapularis (Sb), axillaris (Ax) and musculocutaneous nerves (Mc). FAB technique = the forelimb to be blocked is abducted 90º; FAD technique = both forelimbs are adducted; Cr = cranial; Cd = caudal; JV = jugular vein; AV = axillary vein; U-M = ulnaris-medianus nerves; R = radialis nerve; Mc = musculocutaenous nerve; Ax = axillaris nerve; Sb = subscapularis nerve
The proportion of injections that achieved a staining score of 1 was highest for the FAB (32/42) when compared with the FAD technique (27/42).
Nerves of the BP were stained over a mean length of 0.41 cm (range 0.2–1) by the FAD technique. This mean was of 1.01 cm (range 0.3–2) for the FAB technique (Table 2). In the FAD group, all the nerves were stained for a minimum length of 0.3 cm with exception of the axillaris nerve (minimum length of 0.2 cm). The longest nerve staining length was observed for the ulnaris nerve (0.6 cm) in this group.
Table 2.
Staining length (cm) (mean [range]) over the target nerves of the brachial plexus according to the position of the forelimb to be blocked
| Positioning of forelimbs | FAD | FAB |
|---|---|---|
| Nerves | ||
| Suprascapularis N | 0.3 (0.3) | 0 |
| Subscapularis Nn | 0.3 (0.3) | 0.3 (0.3) |
| Axillaris N | 0.4 (0.2–0.5) | 1.3 (0.7–2) |
| Musculocutaneous N | 0.38 (0.3–0.4) | 1.43 (0.7–2) |
| Radialis N | 0.4 (0.3–0.5) | 1.65 (0.9–2) |
| Medianus N | 0.44 (0.3–0.5) | 1.8 (1–2) |
| Ulnaris N | 0.46 (0.3–0.6) | 1.8 (1–2) |
FAD = forelimbs adducted to the side; FAB = the forelimb to be blocked abducted 90° and the other one adducted to the side
The subscapulares nerves had a minimum staining length of 0.3 cm. The rest of the BP nerves were stained in length ranges of 0.7–2 cm. The longest nerve staining length observed for the FAB technique was 2 cm.
Staining of the phrenicus nerve was observed in 3/6 cats with the FAD technique. Evidence of trauma of the jugular vein (haematoma) was noted in two cats of the FAD group. Distribution of dye within the thorax was noted in two cats of the FAD group. No complications were observed in the FAB group.
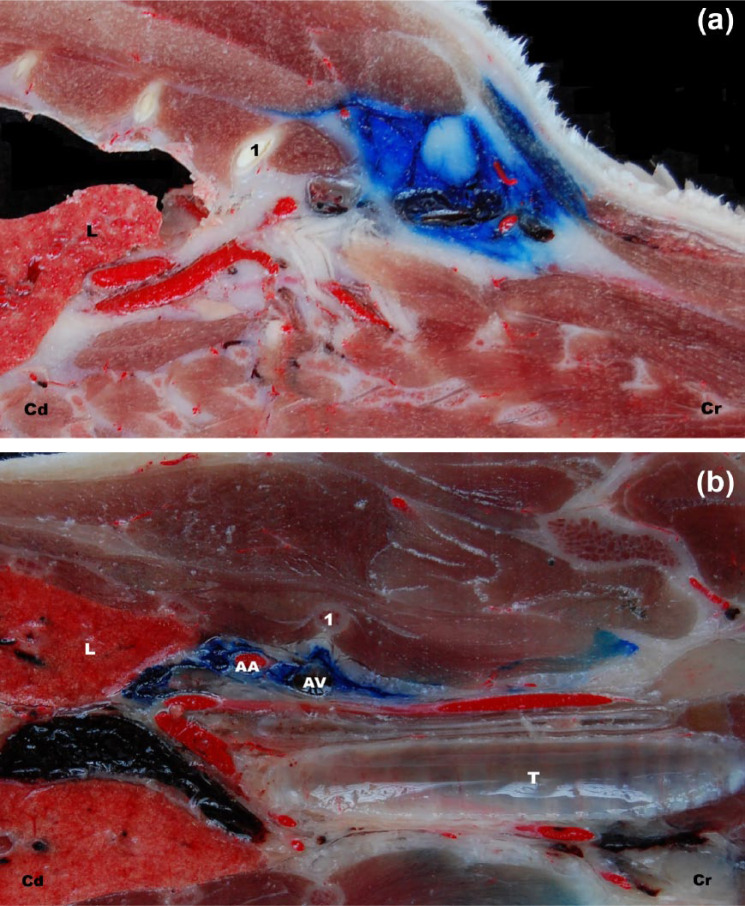
Cryosections
The scores for the deposition of the ink in relation to the nerves of the BP for the two studied approaches are summarised in Table 3. The suprascapularis nerve was not stained in any case with the FAB technique. This nerve was stained in 1/3 cats by the FAD approach. Subscapulares nerves were stained in all cases with the FAB approach and in 1/3 cats within the FAD group. Axillaris, musculocutaneous, radialis, medianus and ulnaris nerves were successfully stained in all cases by the use of the FAB technique (Figure 3a) and in 2/3 cats within the FAD group (Figure 3b).
Table 3.
Scores for the deposition of ink in relation to brachial plexus nerves according to the position of the forelimb to be blocked
| Positioning of forelimbs | FAD | FAB | ||||
|---|---|---|---|---|---|---|
| Cats | 1 | 2 | 3 | 1 | 2 | 3 |
| Nerves | ||||||
| Suprascapularis N | 3 | 2 | 1 | 3 | 3 | 2 |
| Subscapularis N | 3 | 2 | 1 | 1 | 1 | 1 |
| Axillaris N | 1 | 2 | 1 | 1 | 1 | 1 |
| Musculocutaneous N | 1 | 2 | 1 | 1 | 1 | 1 |
| Radialis N | 2 | 1 | 1 | 1 | 1 | 1 |
| Medianus N | 2 | 1 | 1 | 1 | 1 | 1 |
| Ulnaris N | 2 | 1 | 1 | 1 | 1 | 1 |
FAD = forelimbs adducted to the side; FAB = the forelimb to be blocked abducted 90° and the other one adducted to the side; 1 = epineural staining; 2 = perineural staining; 3 = peripheral staining
Figure 3.
Cryosection on dorsal plane. (a) FAB technique: notice the ink at the axillary space. (b) FAD technique: notice the ink within the thorax. FAB technique = the forelimb to be blocked is abducted 90º; FAD technique = both forelimbs are adducted; Cr = cranial; Cd = caudal; AA = axillary artery; AV = axillary vein; 1 = first rib; L = lung; T = trachea
The number of injections that achieved a staining score of 1 was higher in the FAB (18/21) than in the FAD group (12/21).
No evidence of intraneural injection was observed in any case. Evidence of trauma of the jugular vein (haematoma) was noted in one cat of the FAD group. There was presence of dye within the thorax in two cats of the FAD group. No complications were noted in the FAB group.
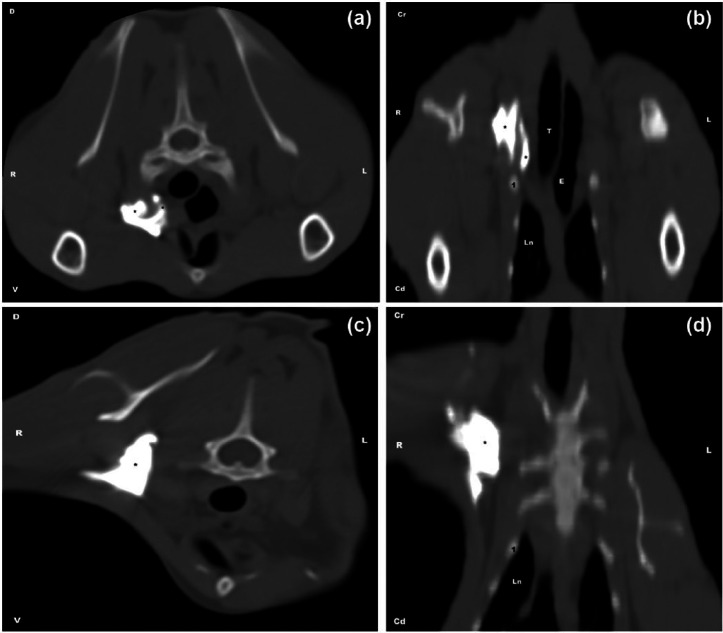
CT study
The CT scans demonstrated an accurate location of the needle tip within the axillary region cranial to the first rib in all cases. The spreading distances of contrast medium within the axillary region are summarised in Table 4. The spreading extent of contrast medium was greatest in the cranial-to-caudal direction for both techniques, and it was slightly greater for the FAD group. The spreading of contrast medium was similar between the two approaches in dorsal–ventral and medial–lateral directions. Spreading of contrast medium to other structures occurred in 2/3 cats in the FAD group (Figure 4a,b). Contrast medium was visualised in the thoracic inlet in one cat, and around the trachea, neck muscles and within the thorax in the other. No complications were observed in the FAB group (Figure 4c,d).
Table 4.
Spreading distances (cm) of contrast medium within the axillary region according to the position of the forelimb to be blocked
| Positioning of forelimbs | FAD | FAB | ||||||
|---|---|---|---|---|---|---|---|---|
| Cats | 1 | 2 | 3 | Mean | 1 | 2 | 3 | Mean |
| Direction of spread | ||||||||
| Cranial–caudal | 3.3 | 3.8 | 3.2 | 3.4 | 3.2 | 5.1 | 4.2 | 4.2 |
| Dorsal–ventral | 1.2 | 1.2 | 2.7 | 1.7 | 1.8 | 1.7 | 1.4 | 1.6 |
| Medial–lateral | 1.4 | 2 | 1.2 | 1.5 | 1.5 | 1.7 | 1.4 | 1.5 |
FAD = forelimbs adducted to the side; FAB = the forelimb to be blocked abducted 90° and the other one adducted to the side
Figure 4.
Pattern of the distribution of the injectate in the CT study. (a) FAD technique: transverse view; the contrast medium (*) is observed spreading at the axillary space and within the thorax. (b) FAD technique: dorsal view. (c) FAB technique: transverse view; the contrast medium (*) is observed spreading at the axillary space. (d) FAB technique: dorsal view.
FAD technique = both forelimbs are adducted; FAB technique = the forelimb to be blocked is abducted 90°; Cr = cranial; Cd = caudal; R = right; L = left; D = dorsal; V = ventral; Ln = lung; 1 = first rib; T = trachea; E = oesophagus
Discussion
The aim of this study was to validate an optimal US-guided technique to block the BP in the cat, studying its feasibility and accuracy by means of anatomical and CT studies. To our knowledge, this is the first study to investigate the use of US guidance to block the BP in the cat.
Blocking of the BP at the axillary approach is used for anaesthesia or analgesia during orthopaedic procedures of the elbow and distal parts of the forelimbs in dogs.9,10 US-guided BP blockade has been widely described in humans and more recently in dogs and calves.11,17,21
BP blockade in dogs has been reported at three levels: at the axillary space (axillary BP block), at the level of the mid-humerus (RUMM block) and at the level of the intervertebral foramina (paravertebral BP blockade). One study describes the appearance and approach to carry out a paravertebral BP block by US guidance. Paravertebral BP block is performed by US-guided injections in the vicinity of the spinal nerves that form the BP as they emerge from the spinal cord at the level of the intervertebral foramina, which provides analgesia for procedures of the structures proximal to the elbow. 17 A recent study describes success and complication rates for three techniques of paravertebral BP blockade in dogs. 18 Another study describes the US-guided technique for axillary BP block. Local anaesthesia of the BP at the level of the axillary space produces analgesia for procedures involving the elbow and regions distal to it. 11 In the latest study, dogs were placed in dorsal recumbency with the thoracic limbs naturally flexed and oriented caudally.
An infraclavicular nerve block described in humans for surgical procedures carried out below mid-humerus is similar to the axillary BP block described in dogs. 22 Most authors have described a technique in which the arm is adducted to the side and the puncture is made inferior to the coracoid process.23–25 Other authors described the technique with the arm abducted 90–110º.26,27 Another study reports that both techniques provided excellent analgesia, but the abducted technique allowed a faster, easier and safer block. 28
In the present study, for the development of a BP blocking technique in cats, the effect of two different positions of the extremities to block was compared. Cats were positioned in dorsal recumbency with both forelimbs adducted to the side (FAD technique) or with the forelimb to be blocked abducted 90° and the other one adducted to the side (FAB technique).
The FAD technique used in our study was similar to that described for dogs, 11 except that by using cadavers it was not possible to get a ‘naturally flexed’ position of the limb. The reason for investigating a different position (FAB technique) was that, in our experience, the FAD technique was difficult to perform in cats due to their smaller size, and, the increased difficulty may lead to a higher rate of complications.
The BP in the cat is formed by suprascapularis, subscapularis, axillaris, musculocutaneous, radialis, medianus and ulnaris nerves. Complete analgesia of the forelimb distally from above the elbow joint is achieved by the effective blockade of the axillaris, musculocutaneous, radialis, medianus and ulnaris nerves.12,29–31 In this study, the FAB technique achieved staining of the axillaris, musculocutaneous, radialis, medianus and ulnaris nerves in 100% of cats. However, the axillaris nerve was stained in 66% and musculocutaneous nerve in 83% of the cases by the use of the FAD technique. This may be due to the position of the forelimb adducted to the side, which could produce a reduced spreading of the dye between these nerve structures.
In this study, suprascapularis and subscapulares nerves were inconsistently stained with both techniques. These nerves primarily supply the muscles involving the shoulder joint so these results support the fact that BP blockade by an axillary approach cannot provide complete analgesia during procedures involving the shoulder. The incomplete success rate observed in this study may have been due to the large dimensions of the axillary space. Probably the volume of dye used in the present study was not enough to stain the more cranial nerves of the BP (suprascapularis and subscapulares nerves) since the dye was administered from a caudal-to-cranial injection. Previous studies support that desensitisation of the nerves innervating the humerus, shoulder and scapula requires administering LA at the level of the spinal nerve roots (paravertebral block). 17 However, it may be possible that by using a larger volume of dye, a complete block of the entire BP could be achieved, although this hypothesis requires further study.
Complications of BP blocks have been described in humans and also in dogs. Diaphragmatic hemiparesis secondary to a phrenicus nerve block has been reported in humans, and, while rarely of clinical significance, it can be the result of an aberrant spreading of anaesthetic agent outside the axillary space. 32 The phrenicus nerve runs medial to the BP in the dog, 33 and acute phrenicus nerve block does not seem to impair ventilation in awake or sleeping dogs if it is unilateral. However, it could potentially lead to hypoxia and respiratory distress, especially in patients with limited respiratory reserve, or if the block is bilateral, which results in a complete diaphragmatic paralysis.18, 34,35 In our study, the gross dissection of the BP showed that the phrenicus nerve was stained in 50% of the cats using the FAD technique. However, it was not observed in any cat within the FAB group.
In the present study, jugular puncture was found as a complication associated with the FAD technique. The jugular vein lies medial and in close proximity to the BP. There is an increased risk of accidental puncture of the jugular vein when the FAD technique is employed, as the long axis of the needle runs parallel to the jugular vein in this technique. No jugular puncture was observed in the FAB group, probably because the abducted 90° positioning of the forelimb to be blocked increases the distance between the target nerves of the BP and the jugular vein. This fact could explain the different incidences of jugular puncture observed in our study for the FAB and FAD techniques.
In our study, most of the contrast medium was observed by CT within the axillary space. However, some contrast medium was observed within the fascial planes of the neck as well as inside the thoracic cavity in cats of the FAD group. The presence of staining inside the thoracic cavity was also reported in a previous study conducted in dogs, although the clinical significance of this finding remains unclear. 18
Another complication of BP blockade is long-term nerve damage resulting from direct nerve trauma or high pressure related necrosis. 32 Because cadavers were used in this study, it was not possible to evaluate the potential for this complication.
The use of cadavers was also associated with other limitations. This cadaveric study allows us only to speculate on the clinical efficacy of the BP block by the observation of the extent of dye or contrast medium distributed along the BP and target nerves. The length of the nerve in contact with the LA is a major factor determining the success of a peripheral nerve blockade. 36 An in vitro study suggested that staining of ⩾2 cm along a peripheral nerve should be considered sufficient to produce a clinically effective nerve blockade.13,36 In the CT study, the length of nerves stained was within a range of 1.23–1.98 cm for the FAD technique and 1.4–1.7 cm for the FAB technique. These results are below the mentioned optimal threshold for an effective nerve blockade. In this study, both contrast medium and dye were progressively injected along to the medial aspect of the BP as the needle was being removed from caudal to cranial direction. This could explain the shorter extent of the dorsoventral distribution observed for the injectate. Previous studies showed that successful staining of nerves determined in cadavers was not related to the observed clinical efficacy because the spreading of the injectate may be reduced in live animals because of possible uptake of the LA by the lymphoid and blood circulations.17,18,37 Therefore, further clinical studies are needed to confirm our results and to establish optimal volume of LA for BP blockade in cats.
Conclusions
The results from this study show that the US-guided axillary approach to the BP by the use of a FAB technique is a safe and feasible procedure to block the BP in the cat. Further investigation is needed to ascertain whether the technique can be effectively applied in a clinical setting and to establish the optimal volume of LA.
Acknowledgments
The authors would like to thank Hill’s Pet Nutrition (Spain) for the scholarship granted to AAn for supporting her postgraduate training.
Footnotes
The authors do not have any potential conflicts of interest to declare.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Accepted: 29 July 2014
References
- 1. Marhofer P, Chan VW. Ultrasound-guided regional anesthesia: current concepts and future trends. Anesth Analg 2007; 104: 1265–1269. [DOI] [PubMed] [Google Scholar]
- 2. Sites BD, Brull R. Ultrasound guidance in peripheral regional anesthesia: philosophy, evidence-based medicine, and techniques. Curr Opin Anaesthesiol 2006; 19: 630–639. [DOI] [PubMed] [Google Scholar]
- 3. Gray AT. Ultrasound-guided regional anesthesia: current state of the art. Anesthesiology 2006; 104: 368–373. [DOI] [PubMed] [Google Scholar]
- 4. Williams SR, Chouinard P, Arcand G, et al. Ultrasound guidance speeds execution and improves the quality of supraclavicular block. Anesth Analg 2003; 97: 1518–1523. [DOI] [PubMed] [Google Scholar]
- 5. Meierhofer JT, Anetseder M, Roewer N, et al. Guidance of axillary multiple injection technique for plexus anesthesia: ultrasound versus nerve stimulation. Anaesthesist 2014; 7: 568–573. [DOI] [PubMed] [Google Scholar]
- 6. Sandhu NS, Bahniwal CS, Capan LM. Feasibility of an infraclavicular block with a reduced volume of lidocaine with sonographic guidance. J Ultrasound Med 2006; 25: 51–56. [DOI] [PubMed] [Google Scholar]
- 7. Casati A, Baciarello M, Di Cianni S, et al. Effects of ultrasound guidance on the minimum effective anaesthetic volume required to block the femoral nerve. Br J Anaesth 2007; 98: 823–827. [DOI] [PubMed] [Google Scholar]
- 8. Oberndorfer U, Marhofer P, Bosenberg A, et al. Ultrasonographic guidance for sciatic and femoral nerve blocks in children. Br J Anaesth 2007; 98: 797–801. [DOI] [PubMed] [Google Scholar]
- 9. Thurmon JC, Ko JCH. Anesthesia and chemical restraint. In: Greenough PR, Weaver AD. (eds). Lameness in cattle. 3rd ed. Philadelphia: WB Saunders, 1997, pp 41–55. [Google Scholar]
- 10. Skarda RT, Tranquilli WJ. Local anesthetics. In: Tranquilli WJ, Thurmon JC, Grim KA. (eds). Lumb Jones’ veterinary anesthesia and analgesia. 4th ed. Ames: Blackwell Publishing, 2007, pp 395–418. [Google Scholar]
- 11. Campoy L, Bezuidenhout AJ, Gleed RD, et al. Ultrasound-guided approach for axillary brachial plexus, femoral nerve, and sciatic nerve blocks in dogs. Vet Anaesth Analg 2010; 37: 144–153. [DOI] [PubMed] [Google Scholar]
- 12. Futema F, Tabacchi-Fantoni D, Auler JOC, Jr, et al. A new brachial plexus block technique in dogs. Vet Anesth Analg 2002; 29: 133–139. [DOI] [PubMed] [Google Scholar]
- 13. Campoy L, Martin-Flores M, Looney AL, et al. Distribution of a lidocaine-methylene blue solution staining in brachial plexus, lumbar plexus and sciatic nerve blocks in the dog. Vet Anaesth Analg 2008; 35: 348–354. [DOI] [PubMed] [Google Scholar]
- 14. Mahler SP, Adogwa AO. Anatomical and experimental studies of brachial plexus, sciatic, and femoral nerve location using peripheral nerve stimulation in the dog. Vet Anaesth Analg 2008; 35: 80–89. [DOI] [PubMed] [Google Scholar]
- 15. Trumpatori BJ, Carter JE, Hash J, et al. Evaluation of a midhumeral block of the radial, ulnar, musculocutaneous and median (RUMM block) nerves for analgesia of the distal aspect of the thoracic limb in dogs. Vet Surg 2010; 39: 785–796. [DOI] [PubMed] [Google Scholar]
- 16. Lemke KA, Dawson SD. Local and regional anesthesia. Vet Clin North Am Small Anim Pract 2000; 30: 839–857. [DOI] [PubMed] [Google Scholar]
- 17. Bagshaw HS, Larenza MP, Seiler GS. A technique for ultrasound-guided paravertebral brachial plexus injections in dogs. Vet Radiol Ultrasound 2009; 50: 649–654. [DOI] [PubMed] [Google Scholar]
- 18. Rioja E, Sinclair M, Chalmers H, et al. Comparison of three techniques for paravertebral brachial plexus blockade in dogs. Vet Anaesth Analg 2012; 39: 190–200. [DOI] [PubMed] [Google Scholar]
- 19. Ansón A, Gil F, Laredo FG, et al. A correlative ultrasound anatomy of the feline brachial plexus and major nerves of the thoracic limb. Vet Radiol Ultrasound 2013; 54: 185–193. [DOI] [PubMed] [Google Scholar]
- 20. De Vlamynck CA, Pille F, Hauspie S, et al. Evaluation of three approaches for performing ultrasonography-guided anesthetic blockade of the femoral nerve in calves. Am J Vet Res 2013; 74: 750–756. [DOI] [PubMed] [Google Scholar]
- 21. Iwamoto J, Yamagishi N, Sasaki K, et al. A novel technique of ultrasound-guided brachial plexus block in calves. Res Vet Sci 2012; 93: 1467–1471. [DOI] [PubMed] [Google Scholar]
- 22. Tran de QH, Clemente A, Tran DQ, et al. A comparison between ultrasound-guided infraclavicular block using the ‘double bubble’ sign and neurostimulation-guided axillary block. Anesth Analg 2008; 107: 1075–1078. [DOI] [PubMed] [Google Scholar]
- 23. Kapral S, Janrasits O, Schaberning C, et al. Lateral infraclavicular plexus block vs. axillary block for hand and forearm surgery. Acta Anaesthesiol Scand 1993; 43: 1047–1052. [DOI] [PubMed] [Google Scholar]
- 24. Kilka HG, Geiger P, Mehrkens HH. Infraclavicular plexus blockade. A new method for anaesthesia of the upper extremity. An anatomical and clinical study. Anaesthesist 1995; 44: 339–344. [DOI] [PubMed] [Google Scholar]
- 25. Greher M, Retzl G, Niel P, et al. Ultrasonographic assessment of topographic anatomy in volunteers suggests a modification of the infraclavicular brachial block. Br J Anaesth 2002; 88: 632–636. [DOI] [PubMed] [Google Scholar]
- 26. Raj PP, Montgomery SJ, Nettles D, et al. Infraclavicular brachial plexus block – a new approach. Anesth Analg 1973; 52: 897–904. [PubMed] [Google Scholar]
- 27. Borgeat A, Ekatodramis G, Dumont C. An evaluation of the infraclavicular block via a modified approach of the Raj technique. Anesth Analg 2001; 93: 436–441. [DOI] [PubMed] [Google Scholar]
- 28. Biegeleisen P, Wilson M. A comparison of two techniques for ultrasound guided infraclavicular block. Br J Anaesth 2006; 96: 502–507. [DOI] [PubMed] [Google Scholar]
- 29. Hofmeister EH, Kent M, Read MR. Paravertebral block for forelimb anesthesia in the dog – an anatomic study. Vet Anaesth Analg 2007; 34: 139–142. [DOI] [PubMed] [Google Scholar]
- 30. Skarda RD. Local and regional anesthesia in ruminants and swine. Vet Clin North Am 1996; 12: 579–626. [DOI] [PubMed] [Google Scholar]
- 31. Nutt P. Brachial plexus analgesia in the dog. Vet Rec 1962; 74: 874–876. [Google Scholar]
- 32. Ben-David B. Complications of peripheral blockade. Anesthesiol Clin 2002; 20: 695–707. [DOI] [PubMed] [Google Scholar]
- 33. Lemke KA, Creighton CM. Paravertebral blockade of the brachial plexus in dogs. Vet Clin North Am Small Anim Pract 2008; 8: 1231–1241. [DOI] [PubMed] [Google Scholar]
- 34. Stradling JR, Kozar LF, Dark J, et al. Effect of acute diaphragm paralysis on ventilation in awake and sleeping dogs. Am Rev Respir Dis 1987; 136: 633–637. [DOI] [PubMed] [Google Scholar]
- 35. Riazi S, Carmichael N, Awad I, et al. Effect of local anaesthetic volume (20 vs 5 ml) on the efficacy and respiratory consequences of ultrasound-guided interscalene brachial plexus block. Br J Anaesth 2008; 101: 549–556. [DOI] [PubMed] [Google Scholar]
- 36. Raymond SA, Steffensen SC, Gugino LD, et al. The role of length of nerve exposed to local anesthetics in impulse blocking action. Anesth Analg 1989; 68: 563–570. [PubMed] [Google Scholar]
- 37. Rasmussen LM, Lipowitz AJ, Graham LF. Development and verification of saphenous, tibial and common peroneal nerve block techniques for analgesia below the thigh in the nonchondrodystrophoid dog. Vet Anaesth Analg 2006; 33: 36–48. [DOI] [PubMed] [Google Scholar]