Abstract
In this study, we applied the Dilator-Dotter technique, a catheter-based angioplasty, to cross through severely stenotic or occluded vertebral arteries during mechanical thrombectomy, and we explored its efficacy and safety in treating tandem lesions of posterior circulation. We performed a retrospective analysis of patients with acute stroke caused by tandem lesions of posterior circulation treated with the Dilator-Dotter technique and thrombectomy between July 2017 and December 2021. In addition to collecting clinical, radiographic, and procedural data from patient records, we also collected information about surgical complications and outcome. We enrolled 9 patients for this study. In all cases, the vertebral artery (VA) on the affected side was crossed through via the Dilator-Dotter technique, and mechanical thrombectomy was successfully performed. The average time from groin puncture to revascularization (TICI 2B–3) was 26 minutes (range 16–50 minutes). Eight patients (89%) achieved complete recanalization with TICI 3, and only 1 patient suffered from thrombus escape to the posterior cerebral artery. Eight patients underwent VA stenting, while the remaining patient was excluded from this procedure because a postoperative brain CT scan recorded obvious staining of the contrast medium within the infarcted area. Five patients had modified Rankin Scale scores ≤ 3 at the 3-month follow-up examination, and 2 patients died due to postoperative cerebral hemorrhage and severe ischemia. The Dilator-Dotter technique may represent a safe and effective treatment for tandem lesions of posterior circulation. Using this method, the lesions can be rapidly recanalized and treated.
Keywords: acute ischemic stroke, basilar artery occlusion, mechanical thrombectomy, tandem, vertebral artery occlusion
1. Introduction
Acute basilar artery occlusion is a fatal disease with a high rate of mortality and disability. Although mechanical thrombectomy has been considered to be the most effective treatment for basilar artery occlusion in recent years, the associated methods and prognostic guidelines differ depending on the specific etiology. Tandem disease of posterior circulation is a rare etiology involving occlusion of the extracranial vertebral artery (VA) or severe stenosis with secondary thrombus occlusion of the basilar artery[1] (BA). In comparison with pure embolization of the BA, tandem vertebrobasilar occlusion may result in longer operative time and worse clinical outcomes.[2,3] Exploring new surgical methods for rapid recanalization may improve patient prognosis.
The Dotter technique, a well-known catheter angioplasty, was first used in peripheral vascular occlusive disease.[4] A modified Dotter technique, called the Dilator-Dotter technique, has been successfully applied to tandem lesions of anterior circulation and has led to faster recanalization times.[5] To our knowledge, there is only 1 published case report on the application of the Dilator-Dotter technique to tandem lesions of posterior circulation.[6] In our study, we examine 9 patients with such lesions treated using the Dilator-Dotter technique, and further illustrate the operational advantages associated with this technology.
2. Materials and methods
We performed a retrospective analysis of medical records from patients with acute ischemic stroke (AIS) who underwent endovascular thrombectomy between July 2017 and December 2021. These records include patients with severe stenosis or occlusion of the VA and occlusion of the BA. We excluded patients with AIS of the anterior circulation, and stroke caused by occlusion of the perforating vessels associated with the posterior circulation system. We also excluded cases in which the VA was first treated with balloon angioplasty or stenting.
All patients in our sample reached the hospital within 24 hours of manifesting pathological symptoms. If the patient reached the hospital within 4.5 hours, we first performed intravenous thrombolysis. The 2 inclusion criteria were: 1) presence of extremely severe stenosis or occlusion of the VA combined with intracranial BA occlusion, established via computer tomography angiography, magnetic resonance angiography, or digital subtraction angiography; 2) endovascular treatment within 24 hours of the onset of symptoms, with no intracerebral hemorrhage confirmed by cranial CT scan.
We recorded the following clinical and surgical data: age, sex, preoperative the National Institutes of Health Stroke Scale (NIHSS), surgical approach, groin to recanalization time, successful recanalization, severity of pre- and postoperative stenosis or occlusion, postoperative symptomatic intracranial hemorrhage alongside other surgical complications, and modified Rankin Scale at 90-day follow-up examination. Successful recanalization was defined as TICI grade 2b–3, and good prognosis was defined as modified Rankin Scale ≥ 3 at 90 days after operation.
3. Technical procedures
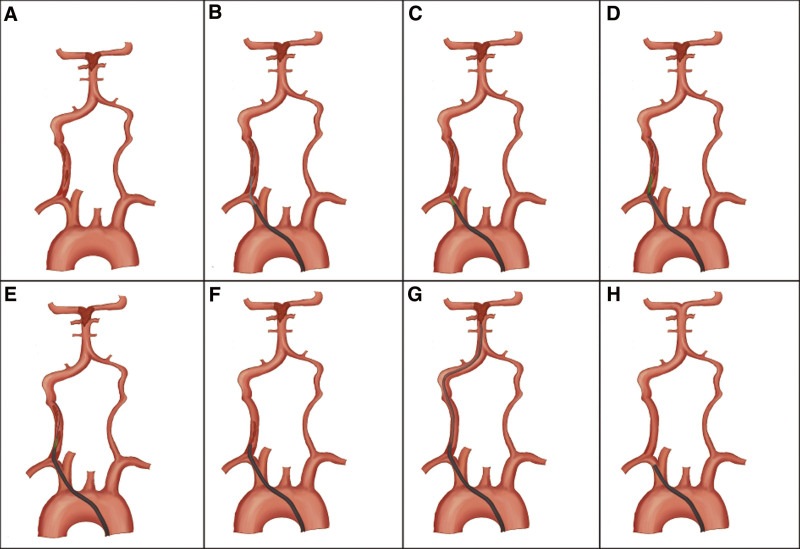
All lesions in this study were accessed through the right common femoral artery. Local anesthesia was used for patients who cooperated with the treatment, and general anesthesia was used for patients who did not cooperate or needed airway protection. We used a 4F MPA catheter (Cordia, Miami Lakee), a 0.035-inch guide wire, and a straight 6F 90-cm Neuron MAX 088 guiding catheter (Penumbra, CA) to select the subclavian artery on the affected side. The prepackaged Neuron MAX 088 inner dilator was inserted into the guiding catheter together with the guide wire. The guide wire went over the occlusion segment, and then guided the inner dilator to cross through the segment. The Neuron MAX 088 guiding catheter was subsequently advanced over the inner dilator, through the occluded segment, and into the VA. For some patients with tortuous blood vessels, we first used the guide wire to cross through the occlusion segment, followed by the 4F MPA catheter; we then removed the guide wire, inserted a 300-cm 0.035-inch Super Core 35 wire (Abbott Vascular, Santa Clara, USA), and withdrew the 4F MPA catheter. The inner dilator went through the occluded segment along the Super Core 35 wire. Once the guiding catheter had crossed the occluded segment, it was used to perform suction (Fig. 1).
Figure 1.
(Schematic diagram.). (A) Acute occlusion of the origin of the right vertebral artery, secondary thrombus occlusion of the basilar artery. (B, C) The guidewire was passed through the vertebral artery occlusion and the Neuron MAX 088 inner dilator was exchanged to the proximal vertebral artery occlusion. (D, E) The Neuron MAX 088 inner dilator passed along a guidewire through occluded vertebral arteries, and the Neuron MAX 088 guiding catheter was subsequently advanced over the inner dilator, through the occluded segment. (F, G, H) Firstly, negative pressure suction was performed on the Neuron MAX 088 guiding catheter, followed by a suction catheter up to the basilar artery occlusion to extract the thrombus. After the vertebral artery recanalization, the residual stenosis of the occluded segment was observed to determine whether to undergo stenting.
Following the above procedures, we started treatment of the intracranial thrombus using the direct aspiration first-pass technique whenever possible. If thrombectomy failed, we used a Solitaire FR stent (Medtronic, CA, USA) combined with a Sofia 5F or 6F aspiration catheter (MicroVention, CA, USA). Intracranial thrombectomy was determined to be successful if treatment resulted in recanalization of TICI 2b–3. After restoration of intracranial blood flow, we withdrew the Neuron MAX 088 guiding catheter until it was proximal to the occluded segment of the VA, while retaining the guide wire inside the VA. For most patients, we chose to perform VA stenting because of unstable plaque at the lesion site, or the possibility of re-occlusion caused by elastic retraction of the vessel. We did not perform VA stenting in patients who presented larger infarct size and higher risk of postoperative hemorrhagic transformation (Figs. 1-3).
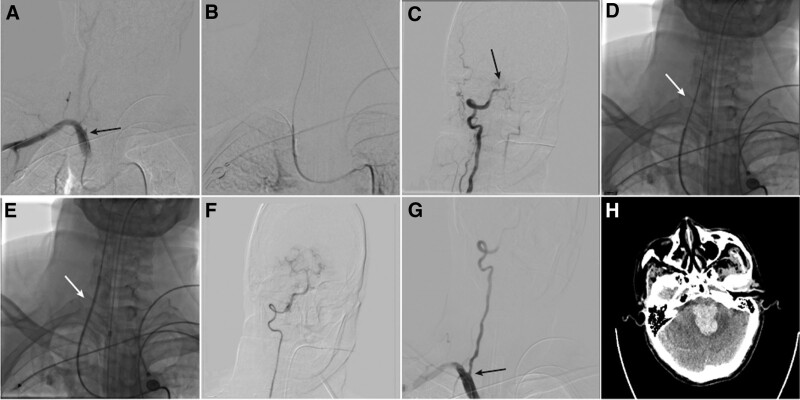
Figure 3.
(Patient 7). (A) Right vertebral artery angiography showed the stump of right vertebral artery with tortuous aortic arch (black arrow). (B) Guide wire selected into the occluded right vertebral artery. (C) 4F MPA angiography showed occlusion at the junction of vertebral artery and basilar artery (black arrow). (D) In order to enhance the support force, after replacing the Super core guide 35 wire, the inner dilator tracked over the wire and across the occlusion. (E) The Neuron MAX 088 guide catheter tracked over the inner dilator and across the occlusion (white arrow). (F) Angiography showed intracranial thrombus removal and recanalization. (G) Angioplasty at the ostial of vertebral artery with 5 * 15 mm balloon expandable stent. (H) Six h after surgery, cranial CT showed brainstem hemorrhage.
4. Results
From July 2017 to December 2021, 236 patients with posterior circulation AIS underwent endovascular thrombectomy at our institution. We excluded 210 patients because they did not present subtotal occlusion or occlusion of the proximal VA. We excluded an additional 17 patients who underwent balloon angioplasty prior to intracranial thrombectomy. We included the remaining 9 patients, who presented with severe ostial stenosis or occlusion of the VA and tandem occlusion of the BA. All patients were treated with the Dilator-Dotter technique applied to the origin of the VA.
The mean age of the included patients was 66 years old (range 51–78), with 6 males (67%) and 3 females (33%). The preoperative NIHSS score was 28 (range 20–36). Three patients (33%) received intravenous tPA before the procedure (Table 1).
Table 1.
Patient demographics, procedural-related data, and outcome.
| Case | Age | Sex | IV tPA |
NIHSS preop | Groin to recanalization time (min) | Stenosis preop (%) | Stenosis postop (%) | Intracranial arterial treatment | Acute re-occlusion | Emergency vertebral artery stenting | TICI | sICH | mRS at 90 d |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 51 | M | N | 23 | 22 | 100 | 50 | ADAPT | N | Y | 3 | N | 3 |
| 2 | 74 | M | N | 29 | 20 | 100 | 60 | Aspiration + SR | N | Y | 3 | N | 3 |
| 3 | 53 | M | Y | 32 | 18 | 100 | 70 | ADAPT | N | Y | 2b | N | 4 |
| 4 | 54 | M | N | 24 | 23 | 100 | 50 | ADAPT | N | N | 3 | N | 2 |
| 5 | 78 | F | Y | 20 | 15 | 100 | 60 | ADPTA | N | Y | 3 | N | 2 |
| 6 | 71 | M | N | 32 | 45 | 100 | 80 | ADAPT | N | Y | 3 | N | 6 |
| 7 | 74 | M | N | 36 | 50 | 100 | 80 | Aspiration + SR | N | Y | 3 | Y | 6 |
| 8 | 77 | F | N | 27 | 26 | 100 | 70 | Aspiration + SR | Y | Y | 3 | N | 4 |
| 9 | 65 | F | Y | 26 | 16 | 95 | 60 | ADAPT | N | Y | 3 | N | 3 |
ADAPT = direct aspiration first-pass technique, mRS = modified Rankin score, NIHSS = National institutes of health stroke score, sICH = symptomatic intracranial hemorrhage, SR = stent retriever, TICI = thrombolyisis in cerebral infarction, tPA = tissue plasminogen activator.
5. Procedural results
The average time from groin puncture to final intracranial revascularization (TICI 2B–3) was 26 minutes (range 16–50 minutes). Thrombectomy was performed using a combination of aspiration catheter and stent retriever in 3 patients, while direct aspiration alone (direct aspiration first-pass technique) was used in 6 patients. Successful intracranial revascularization (TICI 2b–3) was achieved in all patients: 8 patients (89%) achieved complete recanalization with TICI 3, and 1 patient experienced thrombus escape to the posterior cerebral artery.
Before surgery, the origin of the VA was occluded in all patients except for one, who presented severe stenosis (stenosis rate of about 95%). The Dilator-Dotter technique was successfully carried out in all patients and provided good access for intracranial thrombectomy. Stenosis at the origin of the VA was reduced to 64% (range 50%–80%) after application of the Dilator-Dotter technique. Considering the high risk of VA restenosis, 8 of the 9 patients underwent emergency VA stenting. The remaining patient did not undergo stenting because postoperative brain CT scans showed obvious staining by the contrast medium within the infarcted area. There were no iatrogenic dissections or other surgical complications.
6. Clinical outcome
One patient developed brainstem hemorrhage 2 days after operation (case 7) and was discharged after declining further treatment. Two patients suffered from asymptomatic hemorrhage that was spotting at the infarct site. In case 6, the preoperative NIHSS score was 32. Although vascular recanalization was successfully achieved, the patient showed no significant improvement. Brain CT scans recorded severe brainstem infarction, so the patient could not resume spontaneous breathing and could not be treated further. None of the other patients in our group underwent decompressive craniectomy caused by severe brain edema. All patients were followed up within 90 days of discharge, and no re-occlusion occurred. In-stent restenosis occurred in 2 patients, but both cases involved moderate stenosis. We recommended administration of dual antiplatelet drugs until half a year after discharge.
7. Discussion
In this report, we describe a group of patients with severe acute vertebrobasilar stroke caused by tandem VA-BA occlusion, and we suggest a novel surgical approach. Ecker et al[7] published the first report on 6 patients who had undergone vertebral angioplasty prior to BA thrombectomy. There was, however, no consensus on the optimal technique for such cases. All of our patients were treated with the Dilator-Dotter technique applied to the affected side of the VA to establish endovascular access for BA thrombectomy, and all operations were successful.
There is ongoing controversy over surgical strategies for tandem lesions of both anterior and posterior circulatory systems. The main area of contention relates to the sequence of treatment for proximal or distal lesions. In particular, it is debated whether emergency VA angioplasty should be performed, and whether the BA thrombectomy route should pass through the clean-road pathway or the dirty-road pathway. The advantage of the retrograde/reverse approach is that it prioritizes the critical step of intracranial thrombectomy, thus allowing for quick restoration of cerebral blood flow. The relative advantage of proximal recanalization is that it can prevent proximal thrombus shedding, and collateral restoration can be achieved.[8,9] In addition, if the stent is released, dual antiplatelet therapy may be required, thereby increasing the risk of intracranial hemorrhage.[10]
As a result of the anatomical characteristics of the posterior circulatory vessels, surgical paths can be divided into dirty-road pathways and clean-road pathways. Current research on optimal surgical approaches has not conclusively weighed in favor of one over the other.[1,7,11] In our study, we consistently chose the dirty-road strategy because presence of a contralateral VA in our patients was either non-dominant or non-existent. In fact, even if a contralateral VA is present, we nevertheless recommend the dirty-road pathway for surgery when the affected VA is identified as the injured vessel. This recommendation is based on the notion that the occluded VA may form VA stump syndrome, and BA occlusion will then re-occur.[12,13]
In 1965, Dr Charles Dotter described percutaneous transluminal catheter angioplasty (Dotter technique), a method that uses a coaxial system of rigid polyethylene catheters to recanalize an occluded popliteal artery.[14] Since then, this technique has been widely adopted in the field of neurointervention, making it possible to quickly recanalize occluded carotid arteries, greatly reduce reperfusion time, and thus improve patient prognosis.[15] Woodward et al[15] described the insertion of a 6F diagnostic catheter through the ICA occluded segment, and dilation with the catheter followed by an upthrust of the 6F Shuttle Sheath through the stenosis. However, several factors can hamper catheter placement, including hardness of plaque, extent and length of stenosis, and degree of vessel tortuosity. Forcing the catheter through the stenosis when the catheter does not match the size of the guide wire can lead to arterial dissection, vessel rupture, and spasms.
The Neuron MAX 088 catheter contains a tapered inner dilator shaft made of high-density polyethylene polymer, with an inner diameter of 0.035 inches. A step effect will not occur if there is no gap between the guide wire and the inner dilator. Compared with the traditional Dotter angioplasty, the design of the tapered tip can greatly reduce trauma to the vessel wall and occurrence of surgical complications. In a slight departure from the Dilator-Dotter technique,[5] we first tried to pass the guide wire through the occluded segment when using the 4F 125-cm MPA catheter to select the subclavian artery, because the Neuron MAX 088 catheter is not selective. If the passage was successful, the 4F MPA catheter was made to cross through the occluded segment along the guide wire. This operation has 2 advantages: first, the catheter is positioned within the true lumen of the vessel via MPA catheter angiography and the location of intracranial thrombus is identified, so as to set the stage for the next surgical plan; second, replacement with a stiffer guide wire can provide stronger support, especially in cases of tortuous right VA occlusion. None of our patients suffered from arterial perforation, dissection, or thrombus escape.
In our study, 55.6% (5/9) of the patients had a good prognosis, and 2 patients died (patient 6 and patient 7). Of these 2, 1 (patient 7) died due to symptomatic intracranial hemorrhage. Endovascular treatment of VA-BA tandem lesions is rarely reported, and the overall incidence of postoperative symptomatic intracranial hemorrhage is uncertain.[2] Emergency stenting of tandem lesions to the anterior circulation may increase the risk of intracranial hemorrhage, possibly as a consequence of hyperperfusion syndrome and postoperative use of dual antiplatelet drugs.[16] In our study, 88.9% of patients underwent emergency VA stent vascular maturation. Despite observing only moderate residual stenosis after application of the Dilator-Dotter technique, we still performed stenting in some patients because plaque elastic recoil was more common after VA angioplasty, and the risk of re-occlusion was high. The fatal intracranial hemorrhage in patient 7 may be attributed to the large size of the infarcted region, and severe residual stenosis of the VA after mechanical thrombectomy. Furthermore, emergency stenting was performed on this patient and antiplatelet drugs were administered after surgery.
The Dilator-Dotter technique can significantly reduce operation time for tandem lesions of the posterior circulation. The average recanalization time in this study was 26 minutes (range 16–50 minutes), which is significantly shorter than previously reported.[1,11,17,18] In addition, the Dilator-Dotter technique can temporarily block VA blood flow during surgery, preventing further thrombus in the VA from escaping to the intracranial artery. However, the Dilator-Dotter technique presents some limitations. It can only be used for VA disease caused by atherosclerosis but is unsuitable for VA dissection. Furthermore, currently, the Neuron MAX 088 catheter is the only one that can be used for this operation, so the technique cannot be extended to other manufacturers. Because this study relied on a relatively small sample size, the safety and effectiveness of the Dilator-Dotter technique will require further assessment with larger samples in future studies.
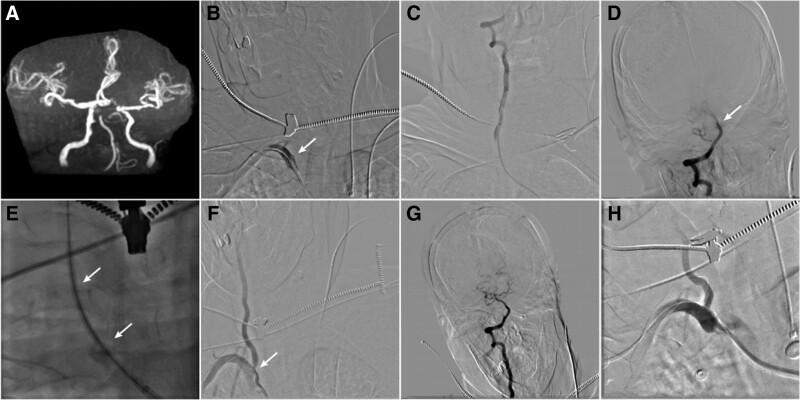
Figure 2.
(Patient 5). (A) cranial MRA showed occlusion of the basilar apex. (B) Right subclavian artery angiography showing the right vertebral artery stump (white arrow). (C and D) 4F MPA catheter angiography showed unobstructed blood flow in the distal vertebral artery with embolization of the basilar artery tip (white arrow). (E) a conical inner dilator passed through the occluded vertebral artery (double white arrow). (F and G) After mechanical thrombectomy, angiography showed stenosis of the right vertebral artery, with a stenosis rate of about 60% (white arrow); the thrombus at the tip of basilar artery had been removed. (H) angioplasty at the ostial of vertebral artery with 4 * 15 mm balloon expandable stent. MRA = magnetic resonance angiography.
Author contributions
Conceptualization: Hebo Wang.
Data curation: Ning Han, Liang Ma, Lei Zhao, Guodong Xu, Yangjuan Jia, Hebo Wang.
Investigation: Ning Han, Liang Ma, Lei Zhao, Guodong Xu, Yangjuan Jia.
Methodology: Ning Han, Liang Ma, Lei Zhao, Guodong Xu, Yangjuan Jia.
Abbreviations:
- AIS
- acute ischemic stroke
- BA
- basilar artery
- NIHSS
- the National Institutes of Health Stroke Scale
- VA
- vertebral artery
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
The authors have no conflicts of interest to disclose.
Ethical approval was waived by the local ethics committees in view of the retrospective nature of the study. All the procedures being performed were part of the routine care and were in accordance to the 1964 Helsinki Declaration.
Supported by Hebei Natural Science Foundation (grant No. H2020307041).
How to cite this article: Han N, Ma L, Zhao L, Xu G, Jia Y, Wang H. The Dilator-Dotter technique can successfully treat tandem lesions of posterior circulation. Medicine 2024;103:4(e37044).
Contributor Information
Ning Han, Email: hanning_happy@163.com.
Liang Ma, Email: 61553635@163.com.
Lei Zhao, Email: 434652678@qq.com.
Guodong Xu, Email: hbghsjjrk@163.com.
Yangjuan Jia, Email: jiayangjuan@sina.cn.
References
- [1].Cohen JE, Leker RR, Gomori JM, et al. Emergent revascularization of acute tandem vertebrobasilar occlusions: endovascular approaches and technical considerations-confirming the role of vertebral artery ostium stenosis as a cause of vertebrobasilar stroke. J Clin Neurosci. 2016;34:70–6. [DOI] [PubMed] [Google Scholar]
- [2].Baik SH, Park HJ, Kim JH, et al. Mechanical thrombectomy in subtypes of basilar artery occlusion: relationship to recanalization rate and clinical outcome. Radiology. 2019;291:730–7. [DOI] [PubMed] [Google Scholar]
- [3].Compter A, van der Hoeven EJ, van der Worp HB, et al. Vertebral artery stenosis in the Basilar Artery International Cooperation Study (BASICS): prevalence and outcome. J Neurol. 2015;262:410–7. [DOI] [PubMed] [Google Scholar]
- [4].Brillu C, Picquet J, Villapadierna F, et al. Percutaneous transluminal angioplasty for management of critical ischemia in arteries below the knee. Ann Vasc Surg. 2001;15:175–81. [DOI] [PubMed] [Google Scholar]
- [5].Amuluru K, Sahlein D, Al-Mufti F, et al. The Dilator-Dotter technique: a modified method of rapid internal carotid artery revascularization in acute ischemic stroke. AJNR Am J Neuroradiol. 2020;41:1863–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Cox M, Layton K, Hise J. Dilator-Dotter technique for acute ischemic stroke: further applications in the vertebral arteries. AJNR Am J Neuroradiol. 2022;43:E7–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Ecker RD, Tsujiura CA, Baker CB, et al. Endovascular reconstruction of vertebral artery occlusion prior to basilar thrombectomy in a series of six patients presenting with acute symptomatic basilar thrombosis. J Neurointerv Surg. 2014;6:379–83. [DOI] [PubMed] [Google Scholar]
- [8].Rangel-Castilla L, Rajah GB, Shakir HJ, et al. Management of acute ischemic stroke due to tandem occlusion: should endovascular recanalization of the extracranial or intracranial occlusive lesion be done first? Neurosurg Focus. 2017;42:E16. [DOI] [PubMed] [Google Scholar]
- [9].Mpotsaris A, Bussmeyer M, Buchner H, et al. Clinical outcome of neurointerventional emergency treatment of extra- or intracranial tandem occlusions in acute major stroke: antegrade approach with Wallstent and Solitaire stent retriever. Clin Neuroradiol. 2013;23:207–15. [DOI] [PubMed] [Google Scholar]
- [10].Amuluru K, Al-Mufti F, Romero CE. Acute ischemic stroke due to common carotid ostial disease with tandem intracranial occlusions treated with thrombectomy and staged retrograde stenting. Interv Neurol. 2018;7:445–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Piechowiak EI, Kaesmacher J, Zibold F, et al. Endovascular treatment of tandem occlusions in vertebrobasilar stroke: technical aspects and outcome compared with isolated basilar artery occlusion. J Neurointerv Surg. 2020;12:25–9. [DOI] [PubMed] [Google Scholar]
- [12].Maeoka R, Nakagawa I, Ohnishi H, et al. A thread of hope for successful revascularization for acute embolic basilar artery occlusion due to miserable vertebral artery stump syndrome. A technical report. J Clin Neurosci. 2020;73:299–303. [DOI] [PubMed] [Google Scholar]
- [13].Zhang W, Wang S, Li C, et al. A case series and literature review of vertebral artery stump syndrome. Front Neurol. 2022;12:770845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Dotter CT, Judkins MP. Percutaneous transluminal treatment of arteriosclerotic obstruction. Radiology. 1965;84:631–43. [DOI] [PubMed] [Google Scholar]
- [15].Woodward K, Wegryn S, Staruk C, et al. The Dotter method revisited: early experience with a novel method of rapid internal carotidartery revascularization in the setting of acute ischemic stroke. J Neurointerv Surg. 2016;8:360–6. [DOI] [PubMed] [Google Scholar]
- [16].Dorado L, Castano C, Millan M, et al. Hemorrhagic risk of emergent endovascular treatment plus stenting in patients with acute ischemic stroke. J Stroke Cerebrovasc Dis. 2013;22:1326–31. [DOI] [PubMed] [Google Scholar]
- [17].Elhorany M, Boulouis G, Hassen WB, et al. Outcome and recanalization rate of tandem basilar artery occlusion treated by mechanical thrombectomy. J Neuroradiol. 2020;47:404–9. [DOI] [PubMed] [Google Scholar]
- [18].Baik SH, Jung C, Kim BM, et al. Mechanical thrombectomy for tandem vertebrobasilar stroke: characteristics and treatment outcome. Stroke. 2020;51:1883–5. [DOI] [PubMed] [Google Scholar]