Abstract
Nitric oxide (NO) is a labile inorganic free radical produced by NO synthase from the substrate l-arginine in various cells and tissues including endothelial cells. A substantial elevation of nitrite levels indicative of NO production occurred in cultures of Cowdria ruminantium-infected bovine pulmonary endothelial cells (BPEC) incubated in medium alone. Exposure of the infected cultures to recombinant bovine gamma interferon (BorIFN-γ) resulted in more rapid production of NO, reduced viability of C. ruminantium, and induction of endothelial cell death. Significant inhibition of NO production was noted after addition of the NO synthase inhibitor N-monomethyl-l-arginine (l-NMMA), indicating that the increase in production occurred via the inducible NO synthase pathway. Reduction in the infectivity of C. ruminantium elementary bodies (EBs) occurred in a dose-dependent manner after incubation with the NO donor molecule S-nitroso-N-acetyl-dl-penicillamine (SNAP) prior to infection of endothelial cells. The level of infection in cultures maintained in SNAP was reduced in a dose-dependent manner with significant negative correlation between the final level of infection on day 7 and the level of SNAP (r = −0.96). It was established that pretreatment and cultivation of C. ruminantium EBs with the NO donor molecule SNAP reduced infectivity to cultures and viability of EBs with the implication that release of NO in vivo following infection of endothelial cells may have an effect upon the multiplication of the agent in the host animal and may be involved in the pathogenesis of heartwater through the effect of this molecule upon circulation.
Heartwater is an important infectious tick-borne disease of domestic and wild ruminants that is caused by an intracellular rickettsial organism, Cowdria ruminantium, which infects and multiplies in the cytoplasm of endothelial cells (9, 14). The clinical manifestations and severity of the disease are associated mainly with severe respiratory, cardiac, and nervous embarrassment due to increased capillary permeability, leading to edema (8). While increased capillary permeability may explain the marked fall in blood and plasma volume which occurs prior to death from heartwater infection (8), the cause of such alterations remains obscure. The work reported here was designed to investigate the role of the association between C. ruminantium and endothelial cells in the pathogenesis of heartwater and the development of host resistance to this infection.
The approach was prompted by reports that nitric oxide (NO), a powerful vasodilator generated by the endothelium, is intimately related to mechanisms of edema formation and hyperemia (10, 22, 23); that NO is both microbicidal (1, 2, 4) and cytotoxic (27); and that interferons (IFNs) may play an important role in resistance to intracellular viruses and rickettsias, such as C. ruminantium (30), possibly by elevating NO production. This work was therefore designed to monitor NO production in cultures of bovine pulmonary endothelial cells (BPEC) infected with C. ruminantium, to assess the effect of gamma interferon (IFN-γ) on NO production by BPEC and its effect on C. ruminantium and the endothelial cells, and to assess the effect of NO on the viability and infectivity of C. ruminantium to BPEC in vitro.
MATERIALS AND METHODS
Endothelial cells.
A BPEC cell line was prepared from vascular tissues, obtained from abattoir-slaughtered cattle, by a modification of the method described by Byrom et al. (7). In brief, short segments of the pulmonary artery were immersed in phosphate-buffered saline containing antibiotics (PBS-A). Collagenase solution at 1 mg/ml in PBS-A was used to detach the cells, which were then cultured in Glasgow minimal essential medium (Gibco Laboratories, Glasgow, United Kingdom) supplemented with 20% heat-inactivated fetal calf serum, 200 mM l-glutamine, 100 IU of penicillin G per ml, and 100 μg of streptomycin per ml.
C. ruminantium isolate.
The Gardel isolate of C. ruminantium isolated in Guadeloupe (31) was maintained in endothelial cell cultures by using Glasgow minimal essential medium fortified with 10% bovine serum, 20 mM HEPES, 10% tryptose phosphate broth, 20 mM l-glutamine, 100 IU of penicillin G per ml, and 100 μg of streptomycin per ml by previously described protocols (7).
Endothelial cell infection.
Glass coverslips of about 13 mm in diameter were sterilized in absolute ethanol for 10 min and then rinsed in sterile PBS before being inserted in four 24-well culture plates (Gibco) with sterile forceps. BPEC were seeded in the plates and incubated at 37°C in 5% CO2. At confluence, the cells were infected with C. ruminantium elementary bodies (EBs) obtained from the supernatant of an infected BPEC culture. The supernatant was centrifuged at 1,500 × g to separate endothelial cells and then at 15,000 × g to pellet the EBs. The EBs were then resuspended in complete medium, and this was used as the inoculum to infect the cells. The plates were then incubated at 37°C for 4 h, after which all the medium was removed and fresh medium containing 0, 25, 50, 75, or 100 U of bovine recombinant IFN-γ (BorIFN-γ; Novartis Animal Health Inc., Basel, Switzerland) per ml was added to the cells. The effect of the NO synthase inhibitor N-monomethyl-l-arginine (l-NMMA) (Sigma, Poole, United Kingdom) at 1 mM was also assessed by culturing infected endothelial cells with or without BorIFN-γ. Twelve replicates were used for each treatment. The other wells were left as uninfected control wells.
Detection of NO generation by C. ruminantium-infected BPEC.
NO reacts with water in culture medium to produce a stable and quantifiable product, nitrite (NO2−), whose concentration can be taken as a measure of NO production by cultured endothelial cells (19). NO2− levels were assayed in culture supernatants daily up to day 7 postinfection by the Griess assay method (19, 33). A 100-μl volume of the test sample was mixed with an equal volume of the Griess reagent (0.1% naphthylethylene diamine · 2HCl and 1% sulfanilamide in 5% phosphoric acid) and incubated at room temperature for 10 min. The optical density value was read at 492 nm on a microplate reader. A standard curve was generated by using doubling dilutions within a range of 0 to 100 μM of sodium nitrite in culture medium. All the reagents, unless otherwise stated, were from Sigma. Samples were tested in triplicate, and the results are expressed as means ± standard deviation. The basal level of NO2− in cell-free medium was determined for each assay and deducted from the level in the test samples.
Assay for viable C. ruminantium EBs.
The viability of C. ruminantium EBs was quantified by the fluorescein diacetate staining method. Fluorescein diacetate is taken in by all cells but is hydrolyzed within live cells to produce green fluorescence (28). The culture supernatants were centrifuged at low speed (1,000 × g) for 5 min to pellet the endothelial cells before staining. A 90-μl volume of medium from the test plates was mixed with 10 μl of diluted fluorescein diacetate (1:50 in PBS), and the mixture was incubated for 15 min at room temperature in the dark. The mean number of viable EBs was counted by fluorescence microscopy in 10 fields at a magnification of ×1,000, and viability was defined as the count expressed as a proportion of the total Cowdria count × 100%.
Assay for viable endothelial cells.
The endothelial cell monolayer was examined microscopically daily for any cytopathic changes. On day 7 the medium from the cultures was removed and the cell monolayer on coverslips was stained in Diff Quik (Baxter Diagnostics) by the standard procedure described by the manufacturer, with acridine orange to identify and quantify viable and nonviable endothelial cells. For the acridine orange staining, a modification of a previously described method (25) was used. Briefly, the slides were fixed in 70% ethanol for 10 min, stained with acridine orange (3 μg/ml) for 3 h at room temperature, and viewed under a fluorescence microscope. Apoptotic cells were identified morphologically by condensation of chromatin, nuclear fragmentation, blebbing of the nuclear membrane, and presence of membrane-bound bodies (25). Nonviable cells were counted in five fields at a magnification of ×1,000 and expressed as a mean percentage ± standard deviation.
Assay for the effect of NO pretreatment of C. ruminantium.
The effect of NO on C. ruminantium was assessed by infecting BPEC with EBs pretreated with different concentrations of the NO donor molecule S-nitroso-N-acetyl-dl-penicillamine (SNAP) (Affiniti U.K.). C. ruminantium EBs were pretreated for 2 h at 37°C with 0, 25, 50, and 100 μM SNAP dissolved in culture medium. The NO level for each concentration of SNAP was determined by the Griess assay method described above. The viability count of the treated EBs was performed before infection by using the fluorescein diacetate staining method as described above. The EBs were then centrifuged at 15,000 × g for 20 min and washed in fresh medium before being resuspended in complete medium and used to infect confluent cell monolayers in 24-well culture plates containing coverslips prepared as described above. The plates were incubated at 37°C in 5% CO2 for 4 h to allow infection of the cells, after which the inoculum was removed from all the wells and replaced with fresh medium. To assess the level and rate of infection, the number of fluorescent foci (colonies) per coverslip and the percentage of infected endothelial cells were determined on days 2 and 4 postinfection by the indirect fluorescent-antibody test and Giemsa staining of endothelial cells on coverslips, respectively. Briefly for the indirect fluorescent-antibody test, the coverslips were fixed in 20% acetone for 10 min. An anti-Cowdria 32-kDa monoclonal antibody at 1:200 in PBS was added to the cells on the coverslips and incubated in a humidified chamber at room temperature for 1 h. After three 5-min washes in PBS, the cells were incubated with a biotin-labelled anti-mouse antibody at a dilution of 1:250, incubated for 1 h at room temperature in a humidified chamber, and given another wash. A further 1-h incubation followed the addition of streptavidin-fluorescein isothiocyanate at a 1:300 dilution. The cells were viewed under a fluorescence microscope, and the number of fluorescent foci of infection on the total area of the coverslip was estimated. The infection rate in Giemsa-stained coverslips was assessed, and the number of infected cells per field was expressed as a percentage of the total cell count. Counts were made on four coverslips per treatment, and the mean value was recorded.
Assay for the effect of coculturing NO in C. ruminantium-infected cultures.
The effect of incubating infected cultures with different concentrations of SNAP on viability and multiplication was assessed. BPEC were cultured on coverslips as described above and infected at confluence with C. ruminantium EBs in medium containing 0, 25, 50, and 100 μM SNAP, which was left in the cultures throughout the experiment. The viability of C. ruminantium EBs in these cultures was determined on days 1, 2, 4, and 7 postinfection. This was done by taking aliquots from four wells for each treatment, which were then centrifuged at low speed (1,000 × g) for 5 min to separate the endothelial cells, and the viability of EBs in the supernatant was determined by the fluorescein diacetate staining method as described above. To estimate the level of infection in cultures at the end of the experiment, cytospin smears were prepared on day 7 postinfection from each of these treatments and stained with Giemsa and a mean estimate of the number of organisms per field was assessed for each treatment. This was taken as a reflection of the multiplication rate of the infectious agent in these cultures.
Data analysis.
Student’s t test, the Mann-Whitney test, the chi-square test, and the correlation coefficient test were used for statistical data analysis as appropriate and depending on the distribution of the data, at 95% confidence intervals.
RESULTS
NO production by C. ruminantium-infected BPEC.
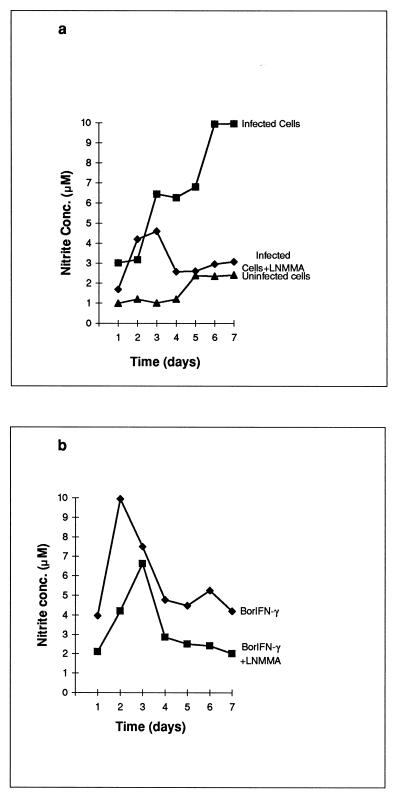
NO levels measured at 24-h intervals revealed a gradual cumulative increase in the number of BPEC infected with C. ruminantium and incubated in medium alone (Fig. 1a). The highest levels were noted on day 7 postinfection. The highest NO concentration coincided with the period when the degree of infection was highest, as observed in cytospin preparations. Treatment of C. ruminantium-infected cultures with BorIFN-γ resulted in increased NO production, with peak levels being recorded at 2 days posttreatment (Fig. 1b). In the cultures supplemented with the l-arginine analog l-NMMA, significant inhibition (P < 0.05) of NO production was recorded in the absence or presence of BorIFN-γ (Fig. 1).
FIG. 1.
NO production by C. ruminantium-infected BPEC. Nitrite levels indicative of NO were measured daily for 7 days in BPEC cultures infected with C. ruminantium in medium alone or supplemented with BorIFN-γ and/or l-NMMA. (a) A significant increase in NO levels was recorded in infected BPEC cultures incubated with medium alone (▪) compared to uninfected cells (▴). A significant inhibition of NO production was recorded in cultures supplemented with l-NMMA (⧫). (b) In infected BPEC cultures supplemented with BorIFN-γ, a more rapid increase in NO levels was recorded, with peak levels being attained 48 h after exposure (⧫). NO production was significantly suppressed in cultures exposed to both BorIFN-γ and l-NMMA (▪).
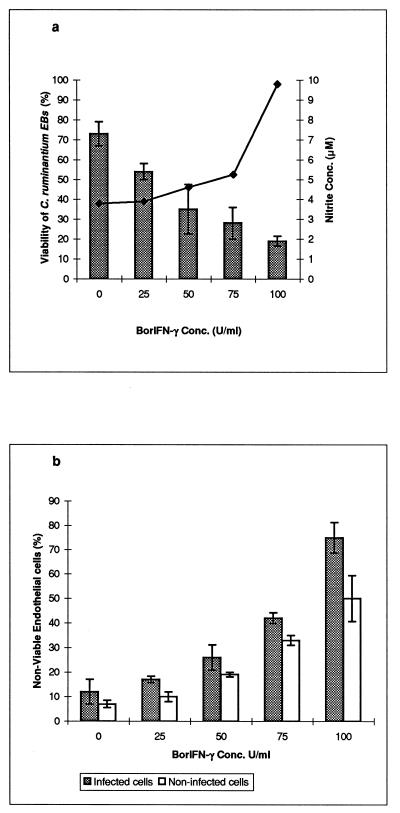
Effect of BorIFN-γ on C. ruminantium viability.
The proportion of viable EBs of C. ruminantium in cultures treated with different concentrations of BorIFN-γ was analyzed at the end of the experiment. The percentage of viable EBs was significantly lower (P < 0.05) in the presence of 100, 75, 50, and 25 U of BorIFN-γ per ml than in the unexposed cultures. The reduced viability was dose dependent, with a much lower viability being recorded at the higher concentrations of BorIFN-γ (Fig. 2a).
FIG. 2.
Effect of BorIFN-γ on C. ruminantium and endothelial-cell viability. The proportion of viable C. ruminantium EBs in BPEC cultures exposed to different concentrations of BorIFN-γ was assessed on day 7 postinfection by a fluorescein diacetate staining method. (a) A significant reduction in viable EBs was recorded in cultures supplemented with BorIFN-γ, in a dose-dependent manner, with the decrease in viability corresponding to nitrite levels. The bars indicate the mean viability of EBs: lines indicate peak NO levels (at 48 h postinfection). (b) Addition of BorIFN-γ to BPEC cultures induced apoptotic cell death in a dose-dependent fashion. This was assessed morphologically on day 7 postinfection in acridine orange- and Diff Quik-stained cells, and the numbers of nonviable cells were recorded as a percentage. Increased cell death was recorded in infected cells compared to noninfected cells.
Effect of BorIFN-γ on endothelial-cell viability.
It was noted that BorIFN-γ caused pronounced changes in the endothelial cells, with the effect being more evident in cells infected with C. ruminantium. Significant cellular changes were noted visually within 48 h after exposure to BorIFN-γ (P < 0.05) (Fig. 2b). These cytopathic changes increased in a dose-dependent fashion. The cells were observed to be rounding up and detaching from the culture plate when the cell monolayer was examined under dark-field microscopy. Apoptotic cell death was morphologically identified in acridine orange- and Diff Quik-stained cells. The cells revealed nuclear fragmentation, chromatin condensation, indiscernible nuclear organelles, blebbing of the nuclear membrane, and presence of dark-staining membrane-bound bodies. There was more evidence of apoptotic cell death in the infected BorIFN-γ-exposed cultures (75%) than in the uninfected BorIFN-γ-treated cultures (50%), whereas in the absence of BorIFN-γ, there was an increase of only 5% in the percentage of nonviable cells in infected (12%) compared to noninfected (7%) cultures.
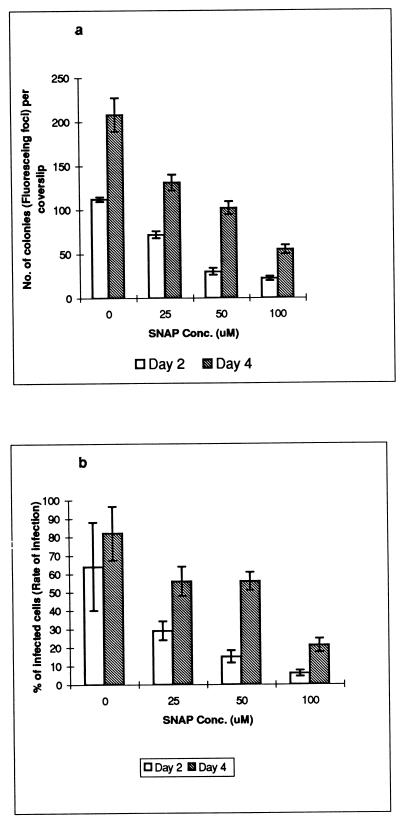
Effect of pretreatment of C. ruminantium EBs with SNAP-generated NO on infectivity.
Significant differences (P < 0.05) were noted in the number of C. ruminantium colonies and the infection rate of endothelial cells on days 2 and 4 postinfection in cultures infected with SNAP-pretreated EBs compared with cultures infected with nontreated EBs (Fig. 3). The number of fluorescing colonies in cultures which had been infected with SNAP-pretreated EBs was smaller than that in the nontreated controls. This reduction occurred in a dose-dependent manner, with smaller numbers of fluorescing colonies being recorded in cultures treated with higher concentrations of SNAP (Fig. 3a). Larger numbers of colonies were recorded on day 4 than on day 2 postinfection, indicating little or no effect of pretreatment of EBs on the subsequent multiplication rate of the viable organisms in the cells (Fig. 3a). The ratio of the number of fluorescing colonies on day 4 to that on day 2 had a range of 2 to 3.4 in all treatments, indicating that almost similar rates of multiplication had occurred after cell entry (Fig. 3a). The rate of infection, defined as the percentage of infected endothelial cells, was closely related to the number of fluorescing colonies, with a higher proportion of infected cells being recorded in cultures infected with EBs not treated with SNAP-generated NO and a higher proportion being found on day 4 compared to day 2 postinfection (Fig. 3b). The organisms were noticeable by day 2 as small, blue-staining, closely packed morulae in Giemsa-stained cells, and the morulae were noted to have increased in size and number from day 2 to day 4.
FIG. 3.
Effect of pretreatment with SNAP-generated NO on infectivity of C. ruminantium EBs. (a) The mean number of fluorescing colonies per coverslip was assessed in cultures infected with SNAP-pretreated EBs on days 2 and 4 postinfection on stained indirect fluorescent-antibody test coverslips. This number, which was a reflection of the infectivity of the pretreated EBs, was found to be inversely related to the SNAP concentration. The number was approximately doubled from day 2 to day 4 irrespective of the SNAP concentration used to treat the EBs, indicating similar multiplication rates of the organism once entry into endothelial cell was gained. (b) The rate of infection (percentage of infected cells) was assessed on days 2 and 4 postinfection in Giemsa-stained cultures infected with SNAP-pretreated EBs. There was an increased rate of infection between days 2 and 4 postinfection in both cultures infected with SNAP-pretreated EBs and the controls.
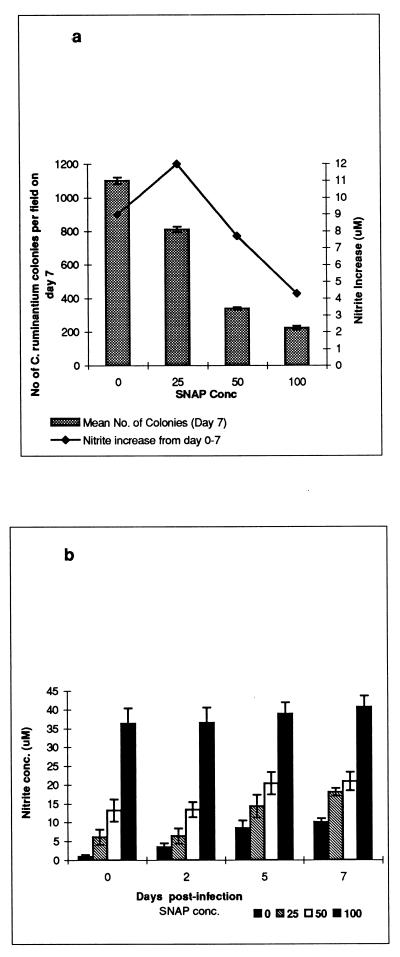
Effect of coculturing SNAP with C. ruminantium-infected cells on the rickettsial viability and growth.
Viability counts were assessed on days 1, 2, 4, and 7 postinfection in all the cultures. In the cultures incubated in the presence of SNAP, significantly reduced viability counts of C. ruminantium EBs were recorded compared with those in untreated control cultures (Table 1). The viability was dose related, with the highest viability counts being recorded in the control cultures without SNAP and the lowest counts being recorded in cultures treated with 100 μM SNAP, with similar trends being recorded for all the days assessed (Table 1). Cytospin smears prepared on day 7 postinfection showed that the number of C. ruminantium colonies per field was negatively correlated with the level of SNAP (r = −0.96) but was more or less a reflection of the viability counts, with a very high correlation coefficient (r = 0.97) (Fig. 4a). The concentration of NO in the culture medium did not decline during the experiment but, rather, increased during the period of infection (Fig. 4b). Although the SNAP-containing cultures had higher cumulative final nitrite levels as a result of the NO released by this molecule, the rate of increase in the nitrite level during the period of infection was higher in heavily infected cultures, i.e., those which had been incubated without SNAP or with low levels of SNAP, than in lightly infected ones (Fig. 4a).
TABLE 1.
Effect of coculturing SNAP with C. ruminantium-infected cells on the viability of extracellular rickettsiae
| SNAP concn (μM) | % Viability (mean ± SD) on day:
|
|||
|---|---|---|---|---|
| 1 | 2 | 4 | 7 | |
| 0 | 90 ± 8 | 82 ± 4 | 75 ± 4.5 | 82.5 ± 14 |
| 25 | 79 ± 3 | 68 ± 5 | 52 ± 4 | 57.9 ± 7 |
| 50 | 56 ± 7 | 45 ± 3 | 28 ± 2.5 | 25.5 ± 4.2 |
| 100 | 38 ± 5 | 37 ± 4 | 20 ± 3 | 5.4 ± 1 |
Mean viability counts of C. ruminantium EBs in the culture medium were assessed on days 1, 2, 4, and 7 postinfection in cultures incubated with different concentrations of SNAP. The viability was inversely related to the concentration of SNAP and consequently to the NO levels (r = −0.96) but was highly correlated with the number of colonies per coverslip (r = 0.97) on day 7 postinfection.
FIG. 4.
Effect of coculturing SNAP with C. ruminantium-infected cells on rickettsial viability and growth. (a) Cytospin smears were prepared on day 7 postinfection for each treatment, and the mean number of C. ruminantium organisms per field was estimated. The count was dose related, with significantly lower counts recorded for 100 and 50 μM SNAP than for 25 μM SNAP and the control. (b) Nitrite levels were measured on days 0, 2, 5, and 7 postinfection for each treatment in cultures in which SNAP was retained throughout the experiment. Nitrite levels increased more in cultures without SNAP than in those containing SNAP, indicating induction of NO production by the infection. The infectious yield in these cultures, a reflection of its growth, was positively related to the increase of nitrite levels, indicating induction of NO production by the organism.
DISCUSSION
Previous observations have indicated strongly that the IFN system, and probably other cytokines as well, plays a key role in natural resistance to C. ruminantium infections (18, 30). This study looked for the production of NO by cultures of resting or BorIFN-γ-activated BPEC infected with C. ruminantium, as well as the effect of the cytokine on the viability of C. ruminantium and BPEC in vitro. The effect of SNAP as an exogenous source of NO on the viability and infectivity of C. ruminantium to BPEC was also examined.
The results of this study demonstrated that infection of resting BPEC with C. ruminantium resulted in induction of NO production compared to that in uninfected cells. Addition of BorIFN-γ to these cultures resulted in enhancement of the NO production in a dose-dependent fashion. Suppression of NO production in both resting and BorIFN-γ-stimulated BPEC by the l-arginine analog l-NMMA implied involvement of the inducible NO synthase pathway in these responses, as reported for other bovine systems (3, 33). Both the viability and infectivity of C. ruminantium EBs were markedly reduced in a dose-dependent fashion when they were incubated with the NO donor molecule SNAP prior to infection of endothelial cells. The study also demonstrated induction of apoptotic cell death of infected cells, seen as alterations in the morphology and viability of the BorIFN-γ-treated endothelial cells. The decreased viability of the infectious agent may have been associated with the apoptosis of endothelial cells in BorIFN-γ-treated cultures or may have resulted from other effects including increased NO production. However, the maximal NO level induced in cultures exposed to 100 U of BorIFN-γ per ml was 10 μM (Fig. 2a), which was much lower than that recorded in 100 μM SNAP in culture medium (35 μM) (Fig. 4b), yet the rickettsial viability was lower in the BorIFN-γ-treated cultures than in the SNAP-treated cultures (Fig. 2a and 4a). The inhibition of Cowdria growth by IFN-γ in concanavalin A-stimulated T-cell supernatants without detectable increases in NO production has been reported (18). However, the activity of IFN-γ was detected by neutralization and may have been lower than that used in this study. Our findings were consistent with the up-regulation of NO generation with bovine IFN-γ reported for bovine macrophages (15, 33). Tumor necrosis factor alpha has also been reported to induce NO synthesis in bovine endothelial cells (32), in contrast to bovine macrophages (15). NO synthesis in bovine macrophages is suppressed by interleukin-4 but unchanged by interleukin-10 or transforming growth factor β (15), whereas the latter is reported to increase NO production in bovine aortic endothelial cells (13). Regulation of NO synthesis would therefore appear to differ between bovine endothelial cells and macrophages, but the up-regulation by a Th1 cytokine (IFN-γ) in both cell types is of interest. Apoptosis in infected-cell cultures occurred at a higher rate than in uninfected cells in response to BorIFN-γ. It is possible this was associated with NO synthesis, since apoptosis in tumor cells by bovine endothelium-derived NO has been reported (32). However, cytotoxicity of IFN-γ to cells has been reported to occur on exposure to the cytokine alone or in combination with a second signal, including intracellular infectious agents (12, 20). We are suggesting here that the killing of C. ruminantium in the BorIFN-γ-treated cultures was also associated with the apoptotic event. Similar findings were reported by Molloy et al. (20) on the viability of intracellular Mycobacterium bovis in monocytes in vitro. They reported that toxic mediators that killed the monocytes by necrosis had no effect on the viability of the organism while those that killed the cells by apoptosis reduced the viability of the organism by 60 to 70%. It has been suggested that since apoptosis is accompanied by nuclear fragmentation of the cells, the integrity of the genetic material of the intracellular organism may be compromised, leading to its killing (20).
The reduced infectivity of C. ruminantium in cultures maintained in medium containing SNAP was attributed mainly to the effects of NO upon the organism prior to infection, since the incubation of EBs with SNAP prior to infection reduced the infectivity in a dose-dependent manner. However, the infection increased at a similar rate irrespective of prior SNAP treatment after first appearance of infected endothelial cells on day 2 (Fig. 3). There was no apparent reduction of infection as a result of maintaining the cultures in SNAP; the ratio of the number of organisms per field in the control cultures to that in the cultures maintained in medium containing SNAP (Fig. 4a) was not significantly different from that obtained when EBs were treated with the same levels of SNAP prior to infection (Fig. 3a). Since the EBs were allowed to infect cell cultures in the presence of SNAP, the dose-dependent reduction of infection in SNAP-maintained cultures can be attributed to the inactivation during infection of the cultures, with no significant increase in the effect of the SNAP during the 7-day period of experiment. Indeed, the high correlation (r = 0.97) between viability counts of EBs remaining in the medium on day 1 and the level of subsequent Cowdria infection in these cultures suggests that the principal effect of SNAP was upon the infectivity of the extracellular organisms. Release of fresh EBs into culture medium, from day 6, is expected from the approximately 6-day cycle of C. ruminantium infection in vitro and may explain the increased viability of extracellular EBs on day 7 in cultures maintained in low concentrations of SNAP (25 μM or below [Table 1]). Therefore, SNAP treatment reduced initial infection rates in the cells, but the level of infection increased at much the same rate irrespective of initial SNAP concentration in culture medium.
The induction of inducible NO synthase by IFN-γ may contribute to the anti-Cowdria activity manifested in IFN-treated cultures of C. ruminantium-infected BPEC. The NO level induced by infection of BPEC without any treatment was approximately 10 μM on day 7, with similar levels being recorded after 48 h in cultures treated with 100 U of IFN-γ per ml. This level of NO is intermediate between the 5 and 13 μM produced by 25 and 50 μM SNAP, respectively. Since the last two treatments significantly reduced the infection level, it can be concluded that the level of NO released in culture by infection alone or by IFN-γ induction may have an effect on the infectivity of released EBs and may thereby indicate a role of NO in the protective responses to heartwater infection. This study reports for the first time that NO is capable of reducing both the viability and infectivity of C. ruminantium in BPEC in vitro, indicating that NO released by endothelial cells or by other cells such as monocytes may play a role in reducing the infectivity of extracellular EBs and thereby in reducing the spread of infection. If release of NO during endothelial cell infection occurs in vivo, this can be expected to reduce the viability of the agent for other endothelial cells and potentially for the arthropod vector; furthermore, in late-stage clinical disease, when a high proportion of endothelial cells are infected, release of endothelial-cell NO would not be expected to affect the development of these infections but would have other, possibly pathogenic consequences. The anti-Cowdria effect of BorIFN-γ may involve NO as well as other pathways involving additional factors, since the NO concentration generated by cells exposed to IFN-γ was not as high as that generated by 100 μM SNAP yet the reduction in viability was higher in the cultures treated with IFN-γ. The study shows that C. ruminantium organisms are killed by events involving activities on IFN-γ and NO in vitro. The findings reported here are comparable with the findings of a study of IFN-γ- and tumor necrosis factor alpha-stimulated mouse endothelial cells, where it was demonstrated that endothelial cells were capable of killing Rickettsia conorii through a mechanism involving NO synthesis (34).
Several biological roles of NO have been described by different authors. NO-dependent nonspecific immunity is now accepted as a general phenomenon involving the reticuloendothelial systems (21) and as a primary defense mechanism against tumor cells (35) and several microbial pathogens and a potent agent in nonspecific defense mechanisms by up-regulating the release of inflammatory mediators (17). NO production by macrophages and monocytes during the response to infection has been correlated with resistance to a wide variety of pathogens in vivo, including M. bovis (20), Listeria monocytogenes (4), Schistosoma mansoni (24, 36), Theileria annulata (33), Plasmodium berghei (29), and Histoplasma capsulatum (16). In contrast, NO mediation of immunosuppression has been suggested to occur in cattle infected with the rickettsia Anaplasma marginale, where treatment with an NO inhibitor, aminoguanidine, resulted in lower levels of the parasite (11). This was thought to be due to the immunosuppressive effects of NO, since its neutralization was beneficial to the host and since the inhibition of NO synthase by aminoguanidine was postulated to increase immune system effectiveness. The inhibition of peripheral T-cell proliferation by NO in mice has also been reported (5). C. ruminantium resides in endothelial cells, an association which leads to increased vascular permeability. The underlying cause of this permeability remains obscure, but mediators rather than structural changes have been more strongly implicated in the pathogenesis of the disease. Not only may excessive NO production by endothelial cells in vivo, which are in continuous contact with the bloodstream, constitute an important role in phenomena such as changes in vascular wall integrity, leading to increased vascular permeability, but also, under other circumstances, NO produced by activated endothelial cells may act as a toxic effector molecule, altering the physiology of endothelial cells, inhibiting various metabolic functions of cells, and leading to death of pathogens such as the schistomula of Schistosoma mansoni (24). NO also precipitates the loss of intracellular iron, resulting in inhibition of certain of the vital enzymes involved in mitochondrial respiration (6). This finding suggests that NO may contribute to the mitochondrial changes observed in the alveolar endothelial cells infected with C. ruminantium (26).
This study has shown that NO produced endogenously or from exogenous sources kills C. ruminantium in a dose-dependent fashion. Although lack of knowledge limits discussion of the potential role of NO in C. ruminantium pathogenesis and immunity, these findings point to a role for NO in resistance to C. ruminantium infections and in the pathology of the disease. Toxic mediators have been suggested to be responsible for some unexplained pathology of the disease, including increased vascular permeability leading to edema and also to vascular collapse in terminal cases of the disease, consistent with effects of NO production upon the vascular system. In a recent study (unpublished data), we noted that infection of previously exposed African breeds of sheep resulted in higher levels of nitrite in plasma during the clinical response. The induction of NO synthesis by IFN-γ may be an important determinant of the outcome of C. ruminantium infection. This is supported by the following sequence of events: rickettsemia occurs 3 to 6 days before the onset of fever and pathology, but terminal collapse, reduced blood pressure, and peak pulmonary edema occur only a few days after the first immune responses are detectable and when rickettsemia has declined but endothelial-cell infection is highest (unpublished data). On the basis of our results and those cited previously, it is becoming clear that NO may be an important component of the immune response to intracellular infections and the pathophysiology of heartwater infection.
ACKNOWLEDGMENTS
We acknowledge R. F. Steiger, Novartis Animal Health Inc., Basel, Switzerland, for providing us with the BorIFN-γ and F. Jongejan, Utrecht, The Netherlands, for providing us with the 32-kDa anti-Cowdria monoclonal antibody.
REFERENCES
- 1.Adams L B, Hibbs J B, Jr, Taintor R R, Krahenbuhl J L. Microbiostatic effect of murine activated macrophages for Toxoplasma gondii: role of synthesis of inorganic nitrogen oxides from l-arginine. J Immunol. 1990;144:2725–2729. [PubMed] [Google Scholar]
- 2.Adams L B, Franzblau S G, Vavrin Z, Hibbs J B, Jr, Krahenbuhl J L. l-Arginine-dependent macrophage effector functions inhibit metabolic activity of Mycobacterium leprae. J Immunol. 1991;147:1642–1646. [PubMed] [Google Scholar]
- 3.Adler H, French B, Thorny M, Pfister H, Peterhans E, Jungi T W. Inducible nitric oxide synthase in cattle. J Immunol. 1995;154:4710–4718. [PubMed] [Google Scholar]
- 4.Booccvar K S, Maybodi M, Washington M K, Hibbs J B, Jr, Kurlander R L. Nitric oxide produced during murine listeriosis is protective. Infect Immun. 1994;62:1089–1100. doi: 10.1128/iai.62.3.1089-1100.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bras A, Rodriguez-Borlando L, Garcia A G, Martinez-A C. Nitric oxide regulates clonal expansion and activation-induced cell death triggered by staphylococcal enterotoxin B. Infect Immun. 1997;65:4030–4037. doi: 10.1128/iai.65.10.4030-4037.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Busse R, Fleming I, Schini V B. Nitric oxide formation in vascular wall: regulation and functional implications. Microbiol Immunol. 1995;196:7–8. doi: 10.1007/978-3-642-79130-7_3. [DOI] [PubMed] [Google Scholar]
- 7.Byrom B, Yunker C E, Donovan P L, Smith G E. In vitro isolation of Cowdria ruminantium from plasma of infected ruminants. Vet Microbiol. 1991;26:263–268. doi: 10.1016/0378-1135(91)90019-c. [DOI] [PubMed] [Google Scholar]
- 8.Clark R. The pathological physiology of heartwater (Cowdria ruminantium) Onderstepoort J Vet Res. 1962;29:25–33. [Google Scholar]
- 9.Cowdry E V. 11th–12th Report of the Director of Education and Veterinary Research, Union of South Africa. 1926. Cytological studies on heartwater. I. The observations of Rickettsia ruminantium in the tissues of infected animals; pp. 161–177. [Google Scholar]
- 10.Furchgott R F, Zawadski J V. The obligatory role of endothelial cells in the relaxation of arterial smooth muscle by acetylcholine. Nature (London) 1980;288:373–376. doi: 10.1038/288373a0. [DOI] [PubMed] [Google Scholar]
- 11.Gale K R, Leatch G, Dimmock C K, Wood P R. Anaplasma marginale: effect of the treatment of cattle with an interferon gamma neutralizing monoclonal antibody or the nitric oxide synthetase inhibitor aminoguanidine on the course of infection. Parasite Immunol. 1997;19:411–417. doi: 10.1046/j.1365-3024.1997.d01-237.x. [DOI] [PubMed] [Google Scholar]
- 12.Hanson B. Susceptibility of Rickettsia tsutsugamushi Gilliam to gamma interferon in cultured mouse cells. Infect Immun. 1991;59:4125–4133. doi: 10.1128/iai.59.11.4125-4133.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Inoue N, Venema R C, Sayegh H S, Ohara Y, Murphy T J, Harrison D G. Molecular recognition of the bovine endothelial cell nitric oxide synthase by transforming growth factor-beta. Arteriosclerosis Thromb Vasc Biol. 1995;15:1255–1261. doi: 10.1161/01.atv.15.8.1255. [DOI] [PubMed] [Google Scholar]
- 14.Jackson C, Neitz W O. 18th Report of the Director of Veterinary Services and Animal Industry, South Africa. 1932. On the aetiology of heartwater; pp. 49–66. [Google Scholar]
- 15.Jungi T W, Brcic M, Sager H, Dobbelaere D A E, Furger A, Roditi I. Antagonistic effects of IL-4 and interferon-gamma (IFN gamma) on inducible nitric oxide synthase expression in bovine macrophages exposed to Gram-positive bacteria. Clin Exp Immunol. 1997;109:431–438. doi: 10.1046/j.1365-2249.1997.4891384.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lane J E, Otero G C, Wuhsieh B A, Howard D H. Expression of inducible nitric oxide by stimulated macrophages correlates with their antihistoplasma activity. Infect Immun. 1994;62:1478–1479. doi: 10.1128/iai.62.4.1478-1479.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liew F Y, Li Y, Severa A, Millott S, Schimidt J, Salter M, Moncada S. Regulation of lymphocyte functions by nitric oxide. Curr Opin Immunol. 1991;7:396–399. doi: 10.1016/0952-7915(95)80116-2. [DOI] [PubMed] [Google Scholar]
- 18.Mahan S M, Sileghem M, Smith G E, Byrom B. Neutralization of bovine concanavalin-A T cell supernatant-mediated anti-Cowdria ruminantium activity with antibodies specific to interferon gamma but not to tumour necrosis factor. Parasite Immunol. 1996;18:317–324. doi: 10.1046/j.1365-3024.1996.d01-106.x. [DOI] [PubMed] [Google Scholar]
- 19.Migliorini P, Corradin G, Corradin B. Macrophage nitrite as a sensitive and rapid assay for the quantitation of murine BorIFN-γ. J Immunol Methods. 1991;139:4794–4797. doi: 10.1016/0022-1759(91)90357-l. [DOI] [PubMed] [Google Scholar]
- 20.Molloy A, Laichmroonvorapong P, Kaplan G. Apoptosis, but not necrosis, of infected monocytes is coupled with killing of intracellular Bacillus Calmette-Guerin. J Exp Med. 1994;180:1499–1509. doi: 10.1084/jem.180.4.1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moncada S, Palmer R M J. The l-arginine-nitric oxide pathway. N Engl J Med. 1993;329:2002–2012. doi: 10.1056/NEJM199312303292706. [DOI] [PubMed] [Google Scholar]
- 22.Moncada S, Palmer R M J, Higgs E A. The discovery of nitric oxide as the endogenous nitrovasodilator. Hypertension. 1988;12:365–372. doi: 10.1161/01.hyp.12.4.365. [DOI] [PubMed] [Google Scholar]
- 23.Moncada S, Palmer R M J, Higgs E A. Nitric oxide: the endogenous regulator of vascular tone. In: Warren J B, editor. The endothelium: an introduction to current research. New York, N.Y: Wiley-Liss; 1990. pp. 1–6. [Google Scholar]
- 24.Oswald P I, Eltoum I, Schwartz B, Casper P, Paulin D, Sher A, James S L. Endothelial cells are activated by cytokine treatment to kill an intravascular parasite Schistosoma mansoni, through the production of nitric oxide. Proc Natl Acad Sci USA. 1994;91:999–1003. doi: 10.1073/pnas.91.3.999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Polunovsky A, Wendt C H, Ingbar D H, Peterson M S, Bitterman P B. Induction of endothelial cell apoptosis by TNF-α: modulation by inhibitors of protein synthesis. Exp Cell Res. 1994;214:584–594. doi: 10.1006/excr.1994.1296. [DOI] [PubMed] [Google Scholar]
- 26.Prozesky L, Duplessis J L. The pathology of heartwater. II. A study of the lung lesions in sheep and goats infected with the Ball 3 strain of Cowdria ruminantium. Onderstepoort J Vet Res. 1985;52:81–85. [PubMed] [Google Scholar]
- 27.Radi R, Beckman J S, Bush K M, Freeman B A. Peroxynitrite oxidation of sulfhydryls: the cytotoxic potential of superoxide and nitric oxide. J Biol Chem. 1991;266:4244–4250. [PubMed] [Google Scholar]
- 28.Rotman B, Papermaster B W. The membrane properties of living mammalian cells as studied by enzymatic hydrolysis of fluorogenic esters. Proc Natl Acad Sci USA. 1966;55:134. doi: 10.1073/pnas.55.1.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sequin M C, Klotz F W, Schneider I, Weir J P, Goodbary M, Slayter M, Rayner J J, Aniagolu J U, Green S J. Induction of nitric oxide synthase protects against malaria in mice exposed to irradiated P. berghei infected mosquitoes: involvement of interferon-gamma and CD8+ T cells. J Exp Med. 1994;180:353. doi: 10.1084/jem.180.1.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Totte P H, De Gee A L W, Werene J. Role of interferons in infectious diseases in the bovine species; effect of viruses and rickettsias. Rev Elev Med Vet Pays Trop. 1993;46:83–86. [PubMed] [Google Scholar]
- 31.Uilenberg G. Heartwater (Cowdria ruminantium infection): current status. Adv Vet Sci Comp Med. 1983;27:427–480. [PubMed] [Google Scholar]
- 32.Umansky V, Becur M, Schirrmacher V, Rocha M. Activated endothelial cells induce apoptosis in lymphoma cells: role of nitric oxide. Int J Oncol. 1997;10:465–471. doi: 10.3892/ijo.10.3.465. [DOI] [PubMed] [Google Scholar]
- 33.Visser A E, Abraham A, Bell-Sakyi L J, Brown C G D, Preston P M. Nitric oxide inhibits establishment of macroschizont-infected cell lines and is produced by macrophages of calves undergoing bovine tropical theileriosis or East Coast Fever. Parasite Immunol. 1995;17:91–102. doi: 10.1111/j.1365-3024.1995.tb00971.x. [DOI] [PubMed] [Google Scholar]
- 34.Walker D H, Popov V L, Crocquet-Valdes P A, Welsh C J R, Feng H. Cytokine-induced, nitric oxide-dependent, intracellular antirickettsial activity of mouse endothelial cells. Lab Invest. 1997;76:129–138. [PubMed] [Google Scholar]
- 35.Woodman J P, Dimier I J, Bout D T. Human endothelial cells are activated by IFN-γ to inhibit Toxoplasma gondii replication—inhibition is due to a different mechanism from that existing in mouse macrophages and human fibroblasts. J Immunol. 1991;147:2019–2023. [PubMed] [Google Scholar]
- 36.Wynn T A, Oswald I P, Eltoum I A, Casper P, Lowenstain C J, Lewis F A, James S L, Sher A. Elevated expression of Th1 cytokines and nitric oxide synthase in the lungs of vaccinated mice after challenge infection with Schistosoma mansoni. J Immunol. 1994;153:5200–5209. [PubMed] [Google Scholar]