Abstract
Background
The COVID-19 pandemic exacerbated access barriers for patients with opioid use disorder. Telehealth presents an opportunity to improve access, treatment quality, and patient outcomes.
Objective
To determine patient characteristics associated with initiating buprenorphine treatment via telehealth and to examine how telehealth initiation is associated with access, treatment quality, and health outcomes.
Design and Participants
This cross-sectional study used deidentified insurance claims to identify opioid use disorder adult patients initiating buprenorphine treatment between March 1, 2020, and November 30, 2021. Multivariable logistic regression assessed determinants of telehealth initiation. Propensity score matching addressed observed differences between in-person and telehealth initiators.
Main Measures
Treatment quality outcomes included initiation within 14 days of diagnosis, engagement (at least 2 opioid use disorder-related visits), and any buprenorphine refill during the study period. Health outcomes included opioid overdose and opioid use disorder-related emergency department and inpatient visits.
Key Results
We identified 23,565 adult buprenorphine initiators, including 3314 (14.1%) patients using telehealth. Younger patients (OR 0.91 to 0.77), females (OR 1.18), South (OR 1.63) and Midwest (OR 1.27) regions, rural area (OR 1.12), and higher-income (OR 1.16) neighborhood residents were more likely to use telehealth. Telehealth patients were more likely than in-person patients (54.5% vs. 48.4%; adjusted odds ratio (AOR), 1.29; 95% CI, 1.19–1.40) to stay engaged with opioid use disorder treatment, and more likely to refill buprenorphine during the study period (83.6% vs. 79.0%, AOR 1.37; 95% CI, 1.23–1.52). Telehealth initiation of buprenorphine was associated with 36% lower overdose rate than in-person initiation (adjusted incidence rate ratio 0.64; 95% CI, 0.45–0.94). The two groups evidenced no significant differences in opioid use disorder-related ED visit and hospitalization.
Conclusions
Our findings suggest that telehealth-initiated buprenorphine treatment is associated with reduced opioid overdose rate and improved patient engagement. Our findings strengthen the case for extending telehealth exemptions and prescribing flexibilities for treatment.
INTRODUCTION
Medication treatment, including methadone, buprenorphine, and naltrexone, is considered the gold standard care for opioid use disorder.1 Nevertheless, estimates show that only 20 to 40% of patients with an opioid use disorder receive these treatments.2, 3 Barriers to opioid use disorder treatment included stigma, provider availability, high out-of-pocket costs, reimbursement constraints, and transportation.4, 5 While telehealth can play a promising role in increasing availability and reach of opioid use disorder care, prior to the COVID-19 pandemic, relatively few patients with opioid use disorder had used telehealth,6 due to reimbursement and regulatory barriers, lack of patient access to technology, and limited provider acceptability.7 More importantly, the Ryan Haight Act of 2008 restricts the prescribing of controlled substances (including buprenorphine) via telemedicine. Among patients with commercial insurance, telehealth accounted for just 0.1% of all substance use disorder visits from 2010 to 2017.8
The COVID-19 pandemic exacerbated the unmet needs and access barriers for the highly regulated medications for opioid use disorder treatment (MOUD).9 With stay-at-home orders, limited in-person hours, and reduced capacity in providing care, patients with opioid use disorder dependent on in-person healthcare delivery struggled to maintain their opioid use disorder (OUD) treatment continuity. In March 2020, federal regulators temporarily relaxed policy restrictions and expanded the use of telehealth services.10 A key exemption to the Ryan Haight Act allowed providers to prescribe controlled substances like buprenorphine via telemedicine without an in-person visit.11 A study showed that after relaxation of the restriction, 13.9% of buprenorphine initiations occurred via telemedicine.12 While patients have continued and established opioid use disorder treatment virtually in the last 2 years, few studies have provided evidence on how telehealth use during the pandemic may affect MOUD delivery quality and patients’ health outcomes using large databases.13, 14 Given that telehealth is likely to remain available going forward as one of the delivery modes,15 it is important to examine treatment and patient outcomes by medication-assisted treatment (MAT) delivery modes.
Emerging research using retrospective chart review or data pilot showed that allowing telehealth-based opioid use disorder treatment during the pandemic helped patients initiate and remain on medication treatment and achieved similar rates of treatment retention compared to in-person care.16–18 However, few studies have examined the impact of telehealth policies on disparate treatment populations across medication type and initiation status, as well as those with limited access to telehealth. A study from the largest nonprofit health system in Massachusetts showed that during the COVID-19 surge, there was an increase in mental health and substance use disorder visits, driven by telehealth.15 To gain a comprehensive understanding of the telehealth transformation in opioid use disorder care, further research using large datasets is urgently needed. Our research objectives are threefold. First, we identified patient characteristics and baseline conditions associated with initiating buprenorphine (BUP) treatment via a telehealth visit. Second, we examined how telehealth may affect buprenorphine early initiation — defined as initiating buprenorphine within 14 days of first OUD diagnosis — and treatment engagement. Last, we explored how BUP telehealth initiation may affect patient outcomes, including opioid overdose and opioid use disorder-related emergency department (ED) and inpatient visits. The study offers insights into the potential impacts of telehealth on the delivery of MAT and patient outcomes through comparisons between telehealth and in-person visits.
METHODS
Study Design and Sample
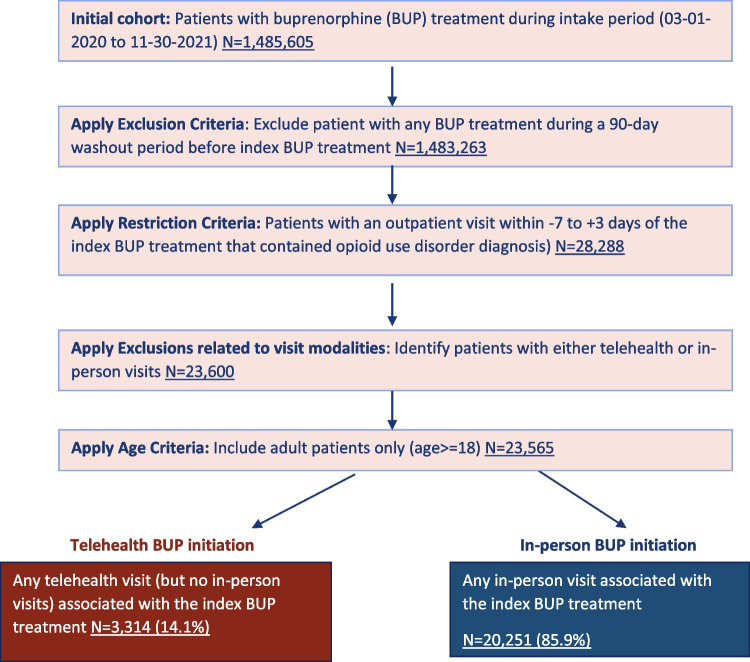
This cross-sectional study used deidentified commercial and Medicare Advantage claims from Elevance Health’s affiliated health plans across 14 US states. We identified opioid use disorder adult patients (age 18 or older) who initiated buprenorphine treatment during the study period March 1, 2020, to November 30, 2021 (Fig. 1). The first treatment episode (index buprenorphine treatment) was defined as the first buprenorphine treatment during the study period. We followed the methods of Barsky et al. in identifying study cohort, opioid use disorder diagnosis, and buprenorphine initiation.12 Buprenorphine initiation was defined as no previous buprenorphine treatment in the 90 days before the first treatment episode (washout period). We also required patients to be continuously enrolled in medical and pharmacy benefits during the baseline period (180 days before the index buprenorphine treatment) and during the study period. This study was exempt from institutional board review since it was an observational study utilizing deidentified secondary data in compliance with 45 CFR Part 164 Subpart E.
Fig. 1.
Cohort assembly flow chart. Note: BUP, buprenorphine.
To determine whether buprenorphine treatment was initiated via telemedicine vs. in-person, we first linked index buprenorphine treatments with outpatient visits occurring within the initiation window (defined as 7 days prior to or up to 3 days after the index buprenorphine treatment that contained opioid use disorder diagnosis). We then identified telehealth and in-person initiation visits based on a previously published algorithm.19 If the patient had multiple outpatient visits during the initiation time window, for telehealth buprenorphine initiation, we required all those visits to be via telehealth; for in-person buprenorphine initiation, we required only one of those visits to be in-person. We excluded patients with neither telehealth nor in-person buprenorphine initiation.
Variables
Demographic and socioeconomic covariates included age at diagnosis, sex, urbanicity (suburb, rural, urban under the US census designation), geographic region of residence, county-level broadband internet access quartiles (percentage of household with internet access from Federal Communication Commissions),20 and county-level median household income quartiles (from County Health Ranking data).21 Clinical covariates included baseline Elixhauser Comorbidity Index,22 baseline health conditions such as co-existing behavioral health problems, overdose diagnosis, musculoskeletal pain, baseline utilization history such as outpatient visit with opioid use disorder as primary diagnosis, opioid use disorder-related ED visits, and prior encounter with initiation provider.
Early opioid use disorder treatment initiation was defined as initiating the index buprenorphine treatment within 14 days of the first OUD diagnosis from medical claims. Treatment engagement was defined as having two or more opioid use disorder-related medical visits on separate days within 34 days of buprenorphine initiation. These two outcomes were adopted and modified from HEDIS measures to align with current performance and quality improvement tools.23 Any buprenorphine refill was defined as buprenorphine treatment after the index buprenorphine claim during the study period. We also examined the incidence of the first opioid overdose following buprenorphine initiation during the study period. Opioid use disorder-related visits were defined as visits with an associated opioid use disorder diagnosis code during the study period.
Statistical Analysis
We examined patient demographic, socioeconomic, and clinical characteristics associated with telehealth use for initiating buprenorphine treatment using multivariable logistic regression.
We used a propensity score (PS) matching technique to address the observed differences between the telehealth and in-person groups. We employed the 1 to 3 greedy nearest neighbor matching to achieve good covariate balance. We also conducted multiple sensitivity analyses using alternative matching methods such as optimal matching and 1 to 1 matching, but the overall between-group balance and key study results remained consistent.
After performing PS matching, we established the matched sample with balanced covariates, and we used this matched sample for all subsequent analyses. Specifically, we compared the early initiation and engagement rates between the telehealth and in-person groups, adjusting for PS matching covariates. We used regression to estimate adjusted incidence rates and incidence rate ratios (IRRs) for overdose, and opioid use disorder-related emergency department (ED) and inpatient visits after initiation of buprenorphine treatment. Additionally, we assessed how initiation method was associated with time to first overdose event, and time to buprenorphine refill using a multivariable Cox proportional hazards regression model to estimate a hazard ratio (HR) between the telehealth and in-person groups. We constructed Kaplan-Meier curves to compare time to hazard outcomes between the two groups. Patients were censored when they experienced the outcome, disenrolled from the study, or at study end. We estimated incidence rates and adjusted incidence rate ratios (IRRs) for opioid overdose, opioid use disorder-related emergency department (ED) visits, and opioid use disorder-related inpatient visits following treatment initiation. Statistical analysis was performed using Stata version 16.1 (StataCorp) and SAS version 8.3 (SAS Institute). All statistical tests were 2-sided and considered to be significant at p < 0.05.
RESULTS
We identified a total of 23,565 adult patients who initiated buprenorphine treatment during March 2020 to November 2021, including 3314 (14.1%) patients using telehealth. A majority of the sample lived in urban areas and the South, and had at least one co-existing behavioral health problem. Logistic regression results indicated that those living in the South and the Midwest regions and rural areas were more likely to use telehealth (Table 1). Older patients with opioid use disorder aged 36–50 and aged 51–65 were less likely to initiate opioid use disorder treatment via telehealth visit compared to younger patients aged 18–35. Female patients were more likely to have telehealth initiation compared to their male counterparts. Patients living in areas in the third and fourth highest income quartiles were more likely to have telehealth initiation compared to those living in the poorest quartile. Nevertheless, baseline health conditions, utilization history, and broadband internet access appeared to be not statistically associated with telehealth initiation.
Table 1.
Characteristics of Patients Using Telemedicine vs. In-person Services for Buprenorphine Treatment Initiation Among Commercial Plan Enrollees Before Matching
| In-person N=20,251 |
Telehealth N=3314 |
Adjusted odds ratio (95% CI) | p value | |
|---|---|---|---|---|
| Age, mean (SD) | 46.8 (14.1) | 45.3 (14.2) | ||
| 18 to 35, N (%) | 4399 (21.7) | 850 (25.7) | 1 [Reference] | – |
| 36 to 50, N (%) | 7394 (36.5) | 1201 (36.2) | 0.91 (0.83–1.01) | 0.06 |
| 51 to 65, N (%) | 6230 (30.8) | 945 (28.5) | 0.86 (0.77–0.96) | 0.009 |
| 65+, N (%) | 2228 (11.0) | 318 (9.6) | 0.77 (0.66–0.89) | 0.001 |
| Female, N (%) | 8916 (44.0) | 1548 (46.7) | 1.18 (1.1–1.28) | <0.001 |
| Urbanicity, N (%) | ||||
| Urban (reference group) | 9507 (46.9) | 1573 (47.5) | 1 [Reference] | – |
| Suburb | 4423 (21.8) | 758 (22.9) | 1.03 (0.92–1.14) | 0.63 |
| Rural | 5298 (26.2) | 808 (24.4) | 1.12 (1–1.25) | 0.06 |
| Missing | 1023 (5.1) | 175 (5.3) | 1.24 (1.01–1.53) | 0.04 |
| Geographic region of residence, N (%) | ||||
| Northeast | 2852 (14.1) | 588 (17.7) | 1 [Reference] | – |
| Midwest | 5945 (29.4) | 897 (27.1) | 1.27 (1.12–1.44) | <0.001 |
| South | 8868 (43.8) | 1173 (35.4) | 1.63 (1.45–1.84) | <0.001 |
| West | 2503 (12.4) | 642 (19.4) | 0.89 (0.81–0.98) | 0.02 |
| Median household income, N (%) | ||||
| Q1 (lowest) | 5384 (26.6) | 742 (22.4) | 1 [Reference] | – |
| Q2 | 6015 (29.7) | 894 (27.0) | 1.09 (0.96–1.23) | 0.19 |
| Q3 | 4972 (24.6) | 864 (26.1) | 1.16 (1.01–1.34) | 0.03 |
| Q4 (highest) | 3880 (19.2) | 814 (24.6) | 1.36 (1.16–1.59) | <0.001 |
| Baseline Elixhauser Comorbidity Index, mean (SD) | 2.1 (2.2) | 1.9 (2.2) | ||
| 0, N (%) | 4792 (23.7) | 1075 (32.4) | 1 [Reference] | – |
| 1, N (%) | 5252 (25.9) | 774 (23.4) | 0.73 (0.63–0.84) | <0.001 |
| 2, N (%) | 3686 (18.2) | 533 (16.1) | 0.72 (0.62–0.84) | <0.001 |
| 3+, N (%) | 6521 (32.2) | 932 (28.1) | 0.76 (0.66–0.88) | <0.001 |
| Baseline conditions, N (%) | ||||
| Co-existing behavioral health problems | 12,954 (64.0) | 1911 (57.7) | 1.02 (0.91–1.15) | 0.73 |
| Baseline overdose Dx | 174 (0.9) | 34 (1.0) | 1.31 (0.86–1.98) | 0.21 |
| Musculoskeletal pain | 9144 (45.2) | 1281 (38.7) | 0.83 (0.76–0.91) | <0.001 |
| Baseline utilization history, N (%) | ||||
| Outpatient visit (opioid use disorder as primary dx) | 12,824 (63.3) | 1940 (58.5) | 0.94 (0.85–1.04) | 0.22 |
| Opioid use disorder-related ED visits | 510 (2.5) | 74 (2.2) | 0.88 (0.66–1.16) | 0.35 |
| Prior encounter with initiation provider | 1998 (9.9) | 258 (7.8) | 0.93 (0.81–1.07) | 0.32 |
| Broadband Internet access, N (%) | ||||
| Fourth quartile (highest) | 10,928 (54.0) | 1876 (56.6) | 1.00 (0.91–1.09) | 0.92 |
| Eligibility months, mean (SD) | 15.7 (6.5) | 14.9 (6.0) | 0.99 (0.98–0.99) | <0.001 |
Table 2 shows the disposition of the study cohorts after propensity score matching, including 9934 in-person initiators and 3314 telehealth initiators. A higher percentage of telehealth initiators had an Elixhauser Comorbidity Index of 0 than in-person initiators. Additionally, utilization of outpatient visits with opioid use disorder as the primary diagnosis was present in a higher percentage of the telehealth initiators. Otherwise, there were no significant covariate differences between the cohorts at baseline.
Table 2.
Baseline Characteristics After Performing Propensity Score Matching
| After propensity score matching | |||
|---|---|---|---|
| In-person | Telehealth | p value | |
| Baseline characteristics | N (%)/mean (SD) | N (%)/mean (SD) | |
| Number of observations in sample | 9934 | 3314 | |
| Age in years, mean (SD) | 45.3 (14.3) | 45.3 (14.2) | 0.93 |
| Female, N (%) | 4660 (46.9) | 1548 (45.7) | 0.84 |
| Urbanicity, N (%) | |||
| Urban (reference group) | 4683 (47.1) | 1573 (47.5) | 0.75 |
| Suburb | 2313 (23.3) | 758 (22.9) | 0.63 |
| Rural | 2371 (23.9) | 808 (24.4) | 0.55 |
| Missing | 567 (5.7) | 175 (5.3) | 0.35 |
| Eligibility months, mean (SD) | 14.8 (6.7) | 14.9 (6.0) | 0.71 |
| Geographic region of residence, N (%) | |||
| Northeast | 1779 (17.9) | 588 (17.7) | 0.83 |
| Midwest | 2642 (26.6) | 897 (27.1) | 0.60 |
| South | 3604 (36.3) | 1173 (35.4) | 0.36 |
| West | 1868 (18.8) | 642 (19.4) | 0.47 |
| Median household income, N (%) | |||
| First quartile (lowest) | 2225 (22.4) | 742 (22.4) | 0.99 |
| Second quartile | 2645 (26.6) | 894 (27.0) | 0.69 |
| Third quartile | 2621 (26.4) | 864 (26.1) | 0.72 |
| Fourth quartile (highest) | 2443 (24.6) | 814 (24.6) | 0.97 |
| Elixhauser Comorbidity Index, mean (SD) | 1.9 (2.2) | 1.9 (2.2) | 0.79 |
| 0, N (%) | 2963 (29.8) | 1075 (32.4) | 0.005 |
| 1, N (%) | 2487 (25.0) | 774 (23.4) | 0.052 |
| 2, N (%) | 1661 (16.7) | 533 (16.1) | 0.39 |
| 3 to 5, N (%) | 2141 (21.6) | 695 (21.0) | 0.48 |
| 6+, N (%) | 682 (6.9) | 237 (7.2) | 0.57 |
| Baseline conditions, N (%) | |||
| Co-existing behavioral health problems | 5712 (57.5) | 1911 (57.7) | 0.87 |
| Baseline overdose diagnosis | 100 (1.0) | 34 (1.0) | 0.92 |
| Baseline alcohol use disorder | 540 (5.4) | 159 (4.8) | 0.15 |
| Baseline severe mental illness disorder diagnosis | 3452 (34.7) | 1184 (35.7) | 0.31 |
| Bipolar disorder | 611 (6.2) | 217 (6.5) | 0.41 |
| Anxiety | 2618 (26.4) | 899 (27.1) | 0.38 |
| Major depressive disorder | 1934 (19.5) | 676 (20.4) | 0.24 |
| Baseline opioid use disorder* utilization history, N (%) | |||
| Outpatient visit | 5547 (55.8) | 1940 (58.5) | 0.01 |
| Inpatient stay | 266 (2.7) | 78 (2.4) | 0.31 |
| Emergency department visits | 108 (1.1) | 46 (1.4) | 0.16 |
| Broadband Internet access percentage, N (%) | |||
| First quartile (lowest) | 489 (4.9) | 184 (5.6) | 0.15 |
| Second quartile | 1055 (10.6) | 353 (10.7) | 0.96 |
| Third quartile | 2199 (22.1) | 726 (21.9) | 0.78 |
| Fourth quartile (highest) | 5624 (56.6) | 1876 (56.6) | 1.00 |
*Utilization with opioid use disorder as the primary diagnosis
Table 3 shows the study results on outcome variables in the PS-matched sample. Nearly 40% of patients initiated buprenorphine treatment within 14 days of an opioid use disorder diagnosis, with no significant difference seen between the telehealth and in-person groups. However, patients who initiated buprenorphine via telehealth were more likely than the in-person group to stay engaged with treatment within 34 days of buprenorphine treatment initiation. Telehealth groups were more likely to have a second buprenorphine refill during the study period than the in-person group, although this difference was only significant during the period of 31 to 90 days after index treatment. Within the first 30 days of initiation, in both groups, about 60% of patients had the second buprenorphine refill, and beyond 180 days of initiation, only 3.6% of patients had the second refill.
Table 3.
Treatment Engagement and Adverse Outcomes by Delivery Mode of Buprenorphine Treatment Initiation (Telehealth vs. In-person) in a Propensity Score-Matched Sample
| Outcomes | In-person | Telehealth | Adjusted effect size (CI) | p value | ||
|---|---|---|---|---|---|---|
| N (%)/mean (SD) | Incidence rate per 100 person-years (CI) | N (%)/mean (SD) | Incidence rate per 100 person-years (CI) | |||
| Number of observations | 9934 | 3314 | ||||
| Initiation/engagement, N (%) | ||||||
| Early Initiation of treatment | 3916 (39.7) | - | 1267 (38.6) | - | OR 0.93 (0.85–1.02) | 0.12 |
| Treatment engagement | 4805 (48.4) | - | 1804 (54.4) | - | OR 1.29 (1.19–1.40) | <0.001 |
| Second buprenorphine refill | 7848 (79.0) | 2771 (83.6) | OR 1.37 (1.23–1.52) | <0.001 | ||
| ≤ 30 days of initiation | 5990 (60.3) | 2038 (61.5) | OR 1.05 (0.97–1.15) | 0.21 | ||
| 31 to 90 days of initiation | 1152 (11.6) | 490 (14.8) | OR 1.32 (1.18–1.48) | <0.001 | ||
| 91 to 180 days of initiation | 348 (3.5) | 119 (3.6) | OR 1.02 (0.83–1.27) | 0.83 | ||
| >180 days of initiation | 358 (3.6) | 126 (3.8) | OR 1.05 (0.85–1.29) | 0.67 | ||
| Adverse outcomes | ||||||
| Opioid overdose, N (%) | 172 (1.7) | 1.9 (1.7–2.3) | 36 (1.1) | 1.2 (0.9–1.7) | IRR 0.64 (0.45–0.94) | 0.02 |
| Opioid use disorder-related ED visits, mean (SD) | 0.1 (0.4) | 6.0 (5.5–6.5) | 0.1 (0.3) | 6.0 (5.1–6.9) | IRR 0.88 (0.67–1.17) | 0.40 |
| Opioid use disorder-related inpatient visits, mean (SD) | 0.1 (0.7) | 9.7 (9.0–10.3) | 0.1 (0.6) | 10.8 (9.7–12.1) | IRR 1.12 (0.88–1.44) | 0.35 |
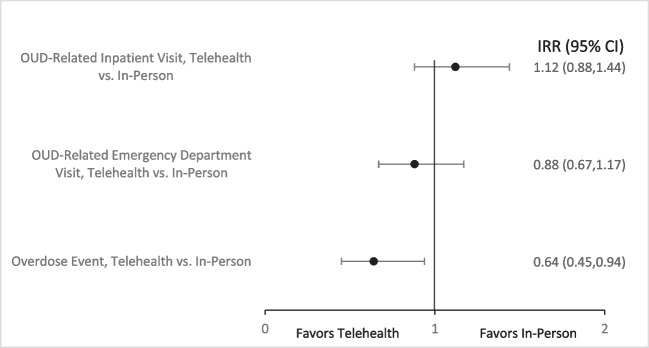
In the propensity score-matched sample, 1.1% of the telehealth group and 1.7% of the in-person group had an opioid overdose following buprenorphine treatment initiation within the study period. When accounting for the time to first overdose diagnosis, telehealth patients had 1.2 overdose events per 100 person-years, compared with 1.9 overdose events per 100 person-years among in-person patients. The adjusted incidence rate ratio indicated that telehealth initiation of buprenorphine was associated with a 36% lower overdose rate than in-person initiation (Fig. 2). Survival analysis results demonstrated the telehealth group appeared to have a consistently lower overdose hazard proportionally, compared to the in-person group (hazard ratio: 0.623, 95% CI: (0.436, 0.891), p value = 0.01). We found no statistically significant differences in opioid use disorder-related ED visits and hospitalizations between the two groups.
Fig. 2.
Adverse events for telehealth and in-person group comparison. Note: Incidence rate per 100 person-years, calculated over the duration of the study follow-up period.
DISCUSSION
In this cohort study within a commercially insured population, approximately 1 in 7 adult patients diagnosed with opioid use disorder initiated buprenorphine treatment during March 2020 to November 2021 via a telehealth visit (as opposed to in-person visit). Patients initiating buprenorphine via telehealth were more likely to continue receiving care for opioid use disorders and receive at least one refill for buprenorphine compared to the counterparts who initiated buprenorphine via in-person visits. We found supporting evidence that telehealth buprenorphine initiation mitigates overdose risk, possibly through better treatment engagement in the early months of treatment as telehealth makes access to follow-up visits easier, and without exacerbating other adverse patient outcomes such as ED or inpatient visits. To our knowledge, our study is the first to establish that telehealth-initiated buprenorphine treatment is associated with a lower risk of opioid overdose in a commercially insured population, adding to existing evidence from the Medicare beneficiaries.14 Since our study focused on the commercially insured population which represents a broader range of treatment needs, it adds to the generalizability of the body of published evidence.
While this is an improvement compared to before the pandemic,8 the opioid use disorder telehealth adoption rate is low compared to other behavioral health conditions.8, 12 Younger, females, and those living in the Midwest and the South regions, rural areas, and higher-income neighborhoods were more likely to initiate buprenorphine treatment via telehealth services. Older adults and individuals in lower-income counties had fewer telemedicine initiations, potentially because of their lacking necessary digital literacy or technology to use telehealth.12 A previous study showed that only 27.8% of people needing opioid use disorder treatment received MOUD with lower MOUD use among adolescents and females.24 Young and female populations may be most benefited from expanding treatment access via telehealth as we found that they were also more likely to engage in digital application-supported treatment, a useful approach to enhance MOUD adherence for these populations who have been reported to have low MOUD engagement rates.25 In addition, consistent with a recently published study finding no difference in telehealth use among patients with markers of greater clinical severity and complexity,12 our results suggested that baseline health conditions, including co-existing behavioral health problems and overdose, utilization history, and county-level broadband internet access had no statistically significant association with telehealth opioid use disorder treatment initiation.
Our results provide evidence that patients initiating buprenorphine via telehealth had higher odds of receiving at least 2 opioid use disorder-related medical visits within 34 days of buprenorphine initiation and higher odds of having a second buprenorphine refill compared to the in-person initiation group. Telehealth may increase access to buprenorphine treatment because it requires less time commitment to attend follow-up visits and to receive refill by eliminating traveling time and removing transportation barriers that patients face for attending in-person visits. While reducing substance use has traditionally been the primary end point, there is an increasing recognition in the literature that addiction, especially opioid use, is a chronic, relapsing condition, and individuals engaged and retained in care can receive harm-reduction services and appropriate treatment.26, 27 Subsequently, treatment retention and engagement are associated with reduced substance use and mortality.28 Research shows that sustainably increased medication initiation and decreased treatment relapse could reduce projected opioid-related deaths through 2029 by 37% and reduce opioid use disorder prevalence by 27.5%.5 Similarly, we also found continued effect of telehealth treatment initiation on mitigating overdose risk throughout the study period. Nevertheless, in our study, only 40% of individuals received early treatment initiation, and only about 50% had engaged in treatments. This highlights the ongoing challenges in engaging and retaining patients in opioid use disorder treatment and urges multi-pronged, evidence-based strategies to improve access to treatment and engagement in care.
Our study provided important evidence that telehealth can mitigate some of the barriers regarding treatment access, which in turn improves treatment engagement and retention and reduces risks for overdose events. Our findings also support the recent proposed amendments to DEA regulations, expanding authorization for individual practitioners to prescribe substance use disorder treatment via telemedicine. However, the amendment retains the 30-day supply constraint until an in-person medical evaluation.29 Based on our research, we propose a more flexible approach to in-person evaluation. Our study shows that telehealth-initiated buprenorphine treatment reduces opioid overdose rates and improves patient engagement, suggesting potential benefits of adjusting evaluation guidelines. In addition, other comprehensive strategies such as improved training to providers, social and housing support, and more comprehensive insurance coverage should be considered to expand access to treatment even more, given the opioid endemic.4, 5
Limitations
This study has limitations. The observational study design may limit our ability to establish a causal effect, although the propensity score matching method may control for observable differences between the two groups. The data are from a single managed care organization and a sample of patients with opioid use disorder initiating buprenorphine during the COVID-19 pandemic, so the results may not generalize to the whole commercial market, nor to other insured populations such as those with Medicaid coverage, or those using other MOUD such as methadone and naltrexone. In addition, while claims may offer a high degree of precision regarding the identification of telehealth services and buprenorphine treatment, they may not fully capture all visits or distinguish between modalities such as telephonic and video visits. There might be some potential misclassification in the group assignment if a patient used a combination of in-person visits and telehealth visits. However, less than 5% of the patients classified as in-person group had a telehealth visit. Classifying a patient into telehealth group only if all of their OUD visits were telehealth visits is also a conservative approach because it is likely biased toward null results if any. Finally, we were unable to examine telehealth use after the treatment initiation: whether patients continue to use that modality or switch to another one during the study period, although the first treatment modality is arguably the most important one.
Conclusions
Despite these limitations, our findings strengthen the case for the permanent adoption of expanded telehealth services and prescribing flexibilities for MOUD. While future research is needed to understand the long-term implications of telehealth use across opioid use disorder treatment modalities, continuous strategies to expand access to MOUD via telehealth may help maximize pathways of care for patients with opioid use disorder and address the ongoing opioid crisis.
Acknowledgements
The authors would like to acknowledge Elizabeth Marks, BS Pharm, RPh (Carelon Research), for her contributions in editing and formatting this manuscript.
Data Availability
The data that support the findings of this study are available from Carelon Research, an Elevance Health subsidary, but restrictions apply to the availability of these data to external sources, and therefore they are not publicly available. Data may be made available through the corresponding author upon reasonable request and with permission of Carelon Research.
Declarations
Conflict of Interest
Authors expressed no conflict of interest.
Footnotes
Nguyen, Zhao, Bailly were employee of Elevance health at the time this research was conducted but they are no longer employee of Elevance Health.
Preliminary findings from this study were presented at AcademyHealth annual research meeting in June 2023.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.National Academies of Sciences Engineering and Medicine . Medications for Opioid Use Disorder Save Lives. Washington, DC: The National Academies Press; 2019. [PubMed] [Google Scholar]
- 2.Lembke A, Chen JH. Use of Opioid Agonist Therapy for Medicare Patients in 2013. JAMA Psychiatry. 2016;73(9):990–992. doi: 10.1001/jamapsychiatry.2016.1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saloner B, Daubresse M, Caleb Alexander G. Patterns of Buprenorphine-Naloxone Treatment for Opioid Use Disorder in a Multistate Population. Med Care. 2017;55(7):669–676. doi: 10.1097/MLR.0000000000000727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Andrews CM, Abraham AJ, Grogan CM, Westlake MA, Pollack HA, Friedmann PD. Impact of Medicaid Restrictions on Availability of Buprenorphine in Addiction Treatment Programs. Am J Public Health. 2019;109(3):434–436. doi: 10.2105/AJPH.2018.304856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ballreich J, Mansour O, Hu E, et al. Modeling Mitigation Strategies to Reduce Opioid-Related Morbidity and Mortality in the US. JAMA Netw Open. 2020;3(11):e2023677. doi: 10.1001/jamanetworkopen.2020.23677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Creedon TB, Schrader KE, O'Brien PL, Lin JR, Carroll CD, Mulvaney-Day N. Rural-Nonrural Differences in Telemedicine Use for Mental and Substance Use Disorders Among Medicaid Beneficiaries. Psychiatr Serv. 2020;71(8):756–764. doi: 10.1176/appi.ps.201900444. [DOI] [PubMed] [Google Scholar]
- 7.Yang YT, Weintraub E, Haffajee RL. Telemedicine's Role in Addressing the Opioid Epidemic. Mayo Clin Proc. 2018;93(9):1177–1180. doi: 10.1016/j.mayocp.2018.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huskamp HA, Busch AB, Souza J, et al. How Is Telemedicine Being Used In Opioid And Other Substance Use Disorder Treatment? Health Aff (Millwood). 2018;37(12):1940–1947. doi: 10.1377/hlthaff.2018.05134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alexander GC, Stoller KB, Haffajee RL, Saloner B. An Epidemic in the Midst of a Pandemic: Opioid Use Disorder and COVID-19. Ann Intern Med. 2020;173(1):57–58. doi: 10.7326/M20-1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Andrilla CHA, Moore TE, Patterson DG, Larson EH. Geographic Distribution of Providers With a DEA Waiver to Prescribe Buprenorphine for the Treatment of Opioid Use Disorder: A 5-Year Update. J Rural Health. 2019;35(1):108–112. doi: 10.1111/jrh.12307. [DOI] [PubMed] [Google Scholar]
- 11.Prevoznik TW. Letter Regarding Use of Telephone Evaluations to Initiate Buprenorphine Prescribing. In: Drug Enforcement Administration, ed. DEA068. Springfield, Virginia: U.S. Department of Justice; 2020.
- 12.Barsky BA, Busch AB, Patel SY, Mehrotra A, Huskamp HA. Use of Telemedicine for Buprenorphine Inductions in Patients With Commercial Insurance or Medicare Advantage. JAMA Netw Open. 2022;5(1):e2142531. doi: 10.1001/jamanetworkopen.2021.42531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jones CM, Compton WM, Han B, Baldwin G, Volkow ND. Methadone-Involved Overdose Deaths in the US Before and After Federal Policy Changes Expanding Take-Home Methadone Doses From Opioid Treatment Programs. JAMA Psychiatry. 2022;79(9):932–934. doi: 10.1001/jamapsychiatry.2022.1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jones CM, Shoff C, Hodges K, et al. Receipt of Telehealth Services, Receipt and Retention of Medications for Opioid Use Disorder, and Medically Treated Overdose Among Medicare Beneficiaries Before and During the COVID-19 Pandemic. JAMA Psychiatry. 2022;79(10):981–992. doi: 10.1001/jamapsychiatry.2022.2284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang J, Landrum MB, Zhou L, Busch AB. Disparities in outpatient visits for mental health and/or substance use disorders during the COVID surge and partial reopening in Massachusetts. Gen Hosp Psychiatry. 2020;67:100–106. doi: 10.1016/j.genhosppsych.2020.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cole TO, Robinson D, Kelley-Freeman A, et al. Patient Satisfaction With Medications for Opioid Use Disorder Treatment via Telemedicine: Brief Literature Review and Development of a New Assessment. Front Public Health. 2020;8:557275. doi: 10.3389/fpubh.2020.557275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang L, Weiss J, Ryan EB, Waldman J, Rubin S, Griffin JL. Telemedicine increases access to buprenorphine initiation during the COVID-19 pandemic. J Subst Abuse Treat. 2021;124:108272. doi: 10.1016/j.jsat.2020.108272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weintraub E, Greenblatt AD, Chang J, et al. Outcomes for patients receiving telemedicine-delivered medication-based treatment for Opioid Use Disorder: A retrospective chart review. Heroin Addict Relat Clin Probl. 2021;23(2):5–12. [PMC free article] [PubMed] [Google Scholar]
- 19.Avula R, Grabner M, Eshete B, Stanek E, Willey V. RWD106 Characterizing Telehealth Utilization from Administrative Claims in the US Using a Standardized Definition. Value in Health. 2022;25(7,Supplement):S596. doi: 10.1016/j.jval.2022.04.1630. [DOI] [Google Scholar]
- 20.Federal Communications Commission. Mapping Broadband Health in America. 2020; https://www.fcc.gov/health/maps. Accessed 2020.
- 21.Robert Wood Johnson Foundation. County Health Ranking Data. 2022; https://www.countyhealthrankings.org/. Accessed 2022.
- 22.Sharma N, Schwendimann R, Endrich O, Ausserhofer D, Simon M. Comparing Charlson and Elixhauser comorbidity indices with different weightings to predict in-hospital mortality: an analysis of national inpatient data. BMC Health Serv Res. 2021;21(1):13. doi: 10.1186/s12913-020-05999-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.NCQA. Initiation and Engagement of Alcohol and Other Drug Abuse or Dependence Treatment (IET). 2022; https://www.ncqa.org/hedis/measures/initiation-and-engagement-of-alcohol-and-other-drug-abuse-or-dependence-treatment/. Accessed April 11, 2023.
- 24.Mauro PM, Gutkind S, Annunziato EM, Samples H. Use of Medication for Opioid Use Disorder Among US Adolescents and Adults With Need for Opioid Treatment, 2019. JAMA Netw Open. 2022;5(3):e223821. doi: 10.1001/jamanetworkopen.2022.3821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Voelker R. App Aids Treatment Retention for Opioid Use Disorder. Jama. 2019;321(5):444. doi: 10.1001/jama.2018.21932. [DOI] [PubMed] [Google Scholar]
- 26.Alford DP, LaBelle CT, Kretsch N, et al. Collaborative care of opioid-addicted patients in primary care using buprenorphine: five-year experience. Arch Intern Med. 2011;171(5):425–431. doi: 10.1001/archinternmed.2010.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hadland SE, Bagley SM, Rodean J, et al. Receipt of Timely Addiction Treatment and Association of Early Medication Treatment With Retention in Care Among Youths With Opioid Use Disorder. JAMA Pediatr. 2018;172(11):1029–1037. doi: 10.1001/jamapediatrics.2018.2143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Englander H, Dobbertin K, Lind BK, et al. Inpatient Addiction Medicine Consultation and Post-Hospital Substance Use Disorder Treatment Engagement: a Propensity-Matched Analysis. J Gen Intern Med. 2019;34(12):2796–2803. doi: 10.1007/s11606-019-05251-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Drug Enforcement Administration Expansion of Induction of Buprenorphine via Telemedicine Encounter A Proposed Rule by the Drug Enforcement Administration on 03/01/2023. Federal Register. 2023;88(40):12890–12906. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from Carelon Research, an Elevance Health subsidary, but restrictions apply to the availability of these data to external sources, and therefore they are not publicly available. Data may be made available through the corresponding author upon reasonable request and with permission of Carelon Research.