Abstract
Oral mucositis is a common distressing complication of cancer therapy, characterised by painful sores within the oral cavity. Current management options offer limited symptomatic relief. Curcumin, a natural polyphenolic compound with recognised anti-inflammatory and antioxidant properties, has emerged as a potential protective agent against oral mucositis. This study explores the therapeutic potential of curcumin in mitigating the impact of oral mucositis by investigating a commercially available curcumin-based oral gel, PerioGold®. Liquid chromatography–tandem mass spectrometry was used to characterise the main constituents of PerioGold®. The cytotoxicity of curcumin constituent was investigated in four cell lines: primary oral keratinocytes (HOKs), immortalised oral keratinocytes (OKF6), dysplastic oral keratinocytes (DOKs), and oral squamous cell carcinoma cells (PE/CA-PJ15). Concentrations of hydrogen peroxide were optimised to develop in vitro models that mimic oral mucositis. The inhibitory effects of PerioGold® against the production of reactive oxygen species were assessed using a designated kit. OKF6 cells were the most sensitive to oxidative stress, while PE/CA-PJ15 cells showed the highest resistance. Pretreatment of the investigated cells for 24 h with PerioGold® demonstrated a significant antioxidative effect in all cells based on a dose–response pattern. PerioGold® exhibits clinical potential for protecting against oxidative stress, warranting further individualised clinical investigations.
Keywords: oral mucositis, oxidative stress, reactive oxygen species, curcumin oral gel, antioxidant properties, mass spectrometry
1. Introduction
Head and neck squamous cell carcinoma (HNSCC) makes up over 90% of cancers in the head and neck area, and it is among the ten most common malignancies in humans worldwide [1]. The majority of HNSCCs originate from the mucosal epithelium found in the oral cavity, pharynx, and larynx. Tobacco use, excessive alcohol consumption, or a combination of both are commonly linked to oral cavity and larynx cancers. In contrast, pharynx cancers are increasingly associated with human papillomavirus (HPV) infection, predominantly HPV-16 [1]. In Australia, over 5000 new cases of HNSCCs were documented in 2022, with an average five-year survival rate of 72% [2]. Typically, treatment strategies for HNSCCs combine radiotherapy, chemotherapy, immunotherapy, and surgery, where surgical procedures primarily focus on removing the visible tumour. In contrast, postoperative radiotherapy is employed to prevent potential tumour spread beyond the surgical margins [3].
However, most patients undergoing oncotherapy in the oral cavity regions experience varying degrees of radiotherapy/chemotherapy-induced damage to the oral mucosa [3,4]. These damages are characterised as acute or delayed reactions, where oral mucositis is the most prevalent acute side effect [3]. Approximately 20% to 40% of individuals with solid tumours undergoing chemotherapy experience the onset of mucositis, typically occurring within five to fourteen days after initiating the treatment [3]. Oral mucositis is a highly incapacitating condition, often associated with a range of distressing symptoms, including redness, swelling, severe oral pain, difficulty swallowing (dysphagia), painful swallowing (odynophagia), and discomfort when speaking [3,5]. Additionally, patients with high-grade oral mucositis may experience disruptions in their radiotherapy and chemotherapy treatments, resulting in the resurgence of resistant cell populations and a subsequent compromise in disease control [6]. Whilst the exact pathogenesis of oral mucositis is still to be determined, it is believed to be linked with clonogenic radiation-induced mitotic death of basal keratinocytes and the subsequent release of reactive oxygen species (ROS) by injured cells [5].
Despite its debilitating nature, there is a limited selection of evidence-based therapeutic agents to manage oral mucositis [7,8]. Several natural-product-based therapies, such as calendula, zinc supplementation, and L-glutamine, have been proposed for controlling and limiting signs and symptoms of oral mucositis [8]. Calendula (Calendula Officinalis), derived from marigold flowers, has been reported in laboratory studies for its preventive radiation-induced skin toxicity [8,9]. However, clinical studies revealed limited evidence based on conflictive outcomes due to standardisation difficulties [9]. Likewise, zinc supplementation, which supports wound healing, has been proposed as a potential remedy for reducing the severity and duration of oral mucositis [10]. However, excessive zinc intake can lead to adverse effects, and optimal dosing requires careful monitoring [11]. Moreover, a previous meta-analysis showed that zinc supplements did not significantly decrease incidence, severity, or pain intensity among patients with oral mucositis [12]. L-glutamine, an amino acid crucial for mucosal cell growth, has shown contradicting outcomes in terms of mitigating oral mucositis [13]. Moreover, its effectiveness can vary among individuals, and high doses should be avoided due to potential neurological side effects [14].
On the other hand, curcumin, a polyphenol derived from the rhizome of the Curcuma longa plant, has gained substantial attention due to its well-known anti-inflammatory, antioxidant, and anticancer properties [15,16,17]. These characteristics position it as a promising remedy for oral mucositis [18]. Curcumin’s therapeutic potential is based on its ability to modulate various cellular and molecular pathways that are fundamental in addressing the pathogenesis of oral mucositis, such as pathways associated with inflammation, oxidative stress, and tissue repair [17,18]. One of these critical mechanisms involves the inhibition of nuclear factor-kappa B (NF-κB), a transcription factor central to inflammation, apoptosis, and cell proliferation [19]. Through the suppression of NF-κB activation, curcumin effectively reduces the expression of pro-inflammatory mediators and helps to alleviate tissue damage [19]. Additionally, curcumin is a scavenger for ROS, countering oxidative stress-induced damage to the oral mucosa. This is achieved through various pathways, including the chelation of metal ions, enhancement of endogenous antioxidants such as superoxide dismutase and catalase, and modulation of cellular signalling by activating the Nrf2/ARE pathway [16,20].
The primary objective of this study was to characterise the main chemical constituents of curcumin within a commercially available product, PerioGold® (Bharma Pty Ltd., Perth, WA, Australia), by carrying out liquid chromatography–tandem mass spectrometry (LC-MS-MS). The second primary objective was to explore the potential antioxidant effects of PerioGold® on oral cells within a controlled in vitro model simulating oral mucositis.
2. Material and Methods
2.1. Liquid Chromatography–Tandem Mass Spectrometry (LC-MS/MS)
Liquid chromatography–tandem mass spectrometry (LC-MS/MS) was the primary analytical technique for the quantification and identification of target curcumin compounds in samples of a commercially available curcumin-based oral gel (PerioGold®, Bharma Pty Ltd., Perth, WA, Australia). The LC-MS/MS system combines the separation abilities of liquid chromatography with the highly sensitive and selective detection capabilities of tandem mass spectrometry, allowing for the precise and simultaneous measurement of multiple analytes. The applied method has been optimised and validated in previous studies using a standard of curcumin (curcumin ≥98.0%, Cat. 08511, Sigma-Aldrich) [21].
In brief, sample preparation involved extraction and sonication for 40 min steps of the investigated samples using DMSO, followed by chromatographic separation on a high-performance liquid chromatography (HPLC) column. The LC system facilitated the elution of analytes, directing them into the mass spectrometer. Compounds were subjected to ionisation, fragmentation, and subsequent detection within the mass spectrometer. Quantification was achieved by comparing analyte peak intensities with those of standard reference compounds. Multiple reaction monitoring (MRM) transitions were utilised for enhanced specificity and sensitivity.
2.2. Cell Lines and Culture
In vitro models of four commercially available cell lines were employed in this study to assess the potential antioxidative effects of curcumin-based oral gel in managing cases with oral mucositis. The investigated cell lines were (i) human oral keratinocyte primary cells (HOKs, Cat. 2610, ScienCell, CA, USA) cultured in oral keratinocyte medium (Cat. 2611, ScienCell) and enhanced with 1% penicillin/streptomycin solution (Cat. 0503, ScienCell) and 2% oral keratinocyte growth supplement (Cat. 2652, ScienCell); (ii) immortalised human oral keratinocyte cell line (OKF6, Cat. CRL3397, ATCC, VI, USA) grown in Modified Eagle Medium/Nutrient Mixture F-12 (DMEM/F-12, Cat. 11320033, ThermoFisher, MA, USA) enriched with 10% foetal bovine serum (FBS, Cat. SFBS-F, Bovogen, VIC, Australia), 400 ng/mL hydrocortisone, and 1% antibiotic-antimycotic (ABAM, Cat. 15240062, ThermoFisher); and (iii) dysplastic oral keratinocyte cell line (DOKs, Cat. 94122104, Sigma-Aldrich, MO, USA) and (iv) oral squamous cell carcinoma cell line (PE/CA-PJ15, Cat. 96121230, Sigma-Aldrich), both grown in Advanced Modified Eagle Medium (Advanced DMEM, Cat. 12491015, ThermoFisher), with the addition of 2% Gibco GlutaMAX Supplement (Cat. 35050061, ThermoFisher), 10.3 µM hydrocortisone, and 1% antibiotic-antimycotic (ABAM, Cat. 15240062, ThermoFisher).
2.3. Acid-Phosphatase Cytotoxicity Assay (APH) to Identify Suitable Concentrations of the Curcumin-Based Oral Gel
The acid-phosphatase cytotoxicity assay (APH) aimed to assess the cytotoxicity of the curcumin-based oral gel and identify the most suitable concentrations for subsequent analysis. HOKs, OKF6, DOKs, and PE/CA-PJ15 were cultured overnight in 96-well plates with 10,000 cells/well and then exposed to eight different concentrations of curcumin-based oral gel (1 µM, 5 µM, 10 µM, 25 µM, 50 µM, 100 µM, 250 µM, and 500 µM). Each concentration was examined in triplicate for each cell line over five days.
In brief, a complete APH buffer was prepared using 100 mM of sodium acetate, 1.1% Triton X-100, and 2 mg/mL of 4-nitrophenyl phosphate disodium salt hexahydrate (Cat. 71768, Sigma-Aldrich). After removing the culture media from the designated wells, each well was washed twice with 150 µL of phosphate-buffered saline (PBS, Cat. 20012043, ThermoFisher). Subsequently, 150 µL of complete APH buffer was added to each well and incubated for 2 h at 37 °C. The reactions were then terminated by adding 15 µL of 1 N sodium hydroxide (NaOH) to each well. Absorbance at 405 nm was promptly recorded within 10 min using a Sunrise® absorbance reader (Cat. 16039400, Tecan, Grödig, Austria).
2.4. In Vitro Model of Oral Mucositis
In this study, we employed an established in vitro model that uses H2O2, a well-known inducer of oxidative stress, to evaluate curcumin-based oral gel’s potential effectiveness in alleviating oxidative stress’s impact in the context of oral mucositis. This model had been previously developed and validated in other studies [22]. Accordingly, preliminary APH assays were conducted, as explained previously, to determine the investigated cells’ IC50, which is the concentration of H2O2 at which 50% of cell viability is inhibited, over a 24 h timeframe. For this purpose, the following concentrations of H2O2 were assessed: 0 µM (control), 50 µM, 100 µM, 250 µM, 500 µM, 1 mM, and 5 mM. All experiments were conducted in triplicate.
2.5. Treatment of the H2O2-Induced Cells with the Curcumin-Based Oral Gel
The cells were seeded in triplicate in 96-well plates under optimal culture conditions until they reached 70% confluency before being treated with different concentrations of the curcumin-based oral gel for 24 h. The oxidative stress was then induced among the incubated cells using appropriate concentrations of H2O2 based on individual IC50 values of each cell line. ROS production was measured using a general oxidative stress indicator assay kit (CM-H2DCFDA, Cat. C6827, ThermoFisher) per the manufacturer’s instructions. Indicators of ROS production through 2′,7′-dichlorodihydrofluorescein diacetate (H2DCFDA) were measured using a CLARIOstar fluorescence microplate reader at EM/EX = 492/517 nm. Readings were recorded immediately after the H2O2 stimulation and every 30 min after that for 5 h.
2.6. Statistical Analyses
The statistical analyses, as well as relevant graphical representations, were conducted using GraphPad Prism® (Version 10.0.2, CA, USA). One-way ANOVA and Tukey’s multiple comparison tests evaluated group differences in the APH cytotoxicity assay. The effectiveness of the curcumin-based oral gel against ROS was evaluated using two-way ANOVA and Dunnett’s multiple comparison tests. Dose–response curves using curve-fit nonlinear regression models were individually generated for each cell line to determine the IC50 concentration of H2O2. Statistical significance was established at p < 0.05.
3. Results
3.1. Liquid Chromatography–Tandem Mass Spectrometry (LC-MS/MS) Analysis Shows Constituents of the Curcumin-Based Oral Gel and Curcumin Quantity
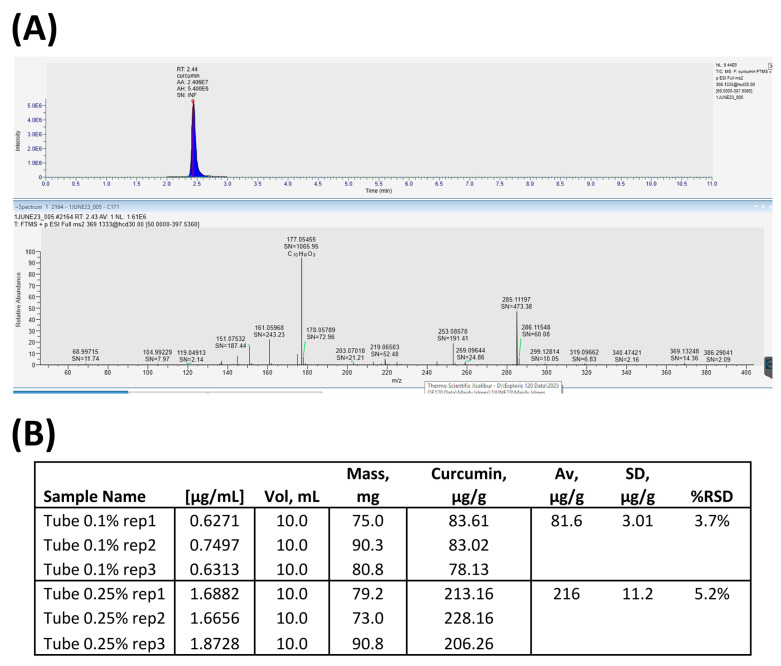
LC-MS/MS successfully identified 18 chemical constituents within the curcumin-based oral gel, as detailed in Table 1. Apart from curcumin, three components known for their antioxidant properties—diethanolamine, cinnamyl carbonate, and calcium monoselenide—were detected in the investigated samples. Moreover, three constituents were identified with known antimicrobial properties: 1,2,4-triazole, norfloxacin, and dextromethorphan (Table 1). The analysis also provided precise curcumin quantities in the samples, a crucial factor for subsequent experiments, as shown in Figure 1. Accordingly, it has been demonstrated that each gram of PerioGold® includes an average of 216 µg of pure curcumin (Figure 1B). Three separate investigations involving randomly selected samples were performed in triplicate to ensure result consistency and reproducibility.
Table 1.
Constituents of the curcumin-based oral gel (PerioGold® Bharma Pty Ltd., Perth, WA, Australia) based on the conducted liquid chromatography–tandem mass spectrometry (LC-MS/MS) analysis.
| No. | Molecular Weight | Name | Chemical Formula | Signal Intensity |
|---|---|---|---|---|
| 1 | 68.99715 | 1,2,4-Triazole | C2H3N3 | 11.74 |
| 2 | 104.99229 | Diethanolamine | C4H11NO2 | 7.97 |
| 3 | 119.04913 | Calcium monoselenide | CaSe | 2.14 |
| 4 | 151.07532 | Trifluoromethanesulfonic acid | CF3SO3H | 187.44 |
| 5 | 161.05968 | Alpha-aminoadipic acid | C6H11NO4 | 243023 |
| 6 | 177.05455 | Cinnamyl carbonate | C10H9O3 | 1065.95 |
| 7 | 178.05789 | 4-Chlorobenzylamine hydrochloride | C7H9Cl2N | 72.96 |
| 8 | 203.07018 | 2,7-Dichloro-1,2,3,8a-tetrahydroquinazoline | C8H8Cl2N2 | 21.21 |
| 9 | 219.06503 | 2-(2,6-Dichlorophenyl)acetohydrazide | C8H8Cl2N2O | 52.48 |
| 10 | 253.08578 | Diethyl 2-bromobutanedioate | C8H13BrO4 | 191.41 |
| 11 | 259.09644 | Methyl 4-(bromomethyl)-2-methoxybenzoate | C10H11BrO3 | 24.86 |
| 12 | 285.11197 | 1-(Bromomethyl)-4-[(difluoromethyl)sulfonyl]benzene | C8H7BrF2O2S | 473.38 |
| 13 | 286.11548 | 4-Bromo-5,7-difluoro-2-propylquinoline | C12H10BrF2N | 60.08 |
| 14 | 299.12814 | 5-Amino-3-chloro-2-octoxybenzoic acid | C15H22ClNO3 | 10.05 |
| 15 | 319.09662 | Norfloxacin | C16H18FN3O3 | 6.83 |
| 16 | 340.47421 | Behenic acid | C22H44O2 | 2.16 |
| 17 | 369.13248 | Dextromethorphan | C18H25NO | 14.36 |
| 18 | 386.29041 | 1-O-Sinapoyl-beta-D-glucose | C17H22O10 | 2.09 |
Figure 1.
(A) Chromatograms showing the intensity and the relative abundance of the constituents of the curcumin-based oral gel; (B) quantifications of curcumin in the investigated samples.
3.2. Acid-Phosphatase Cytotoxicity Assay (APH)
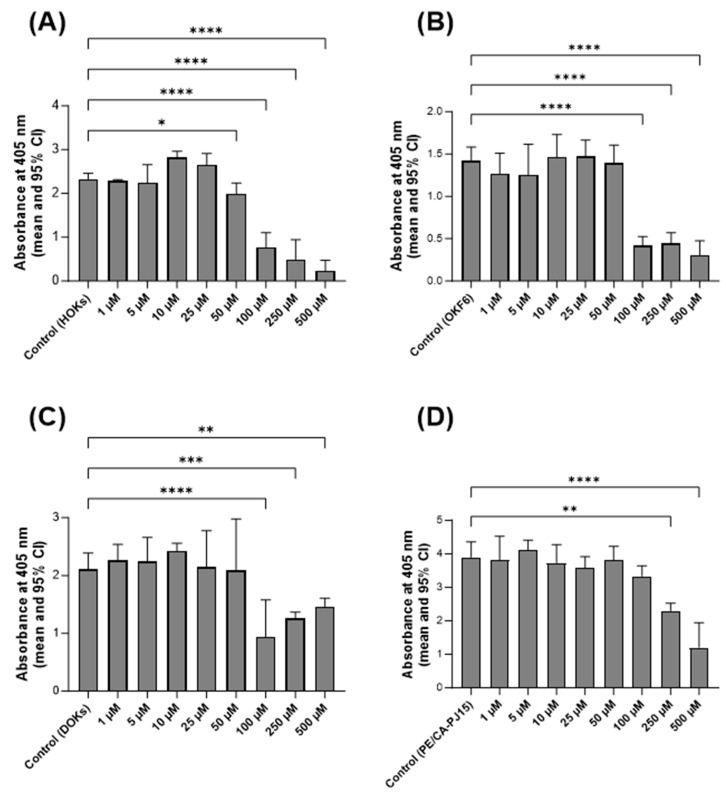
The cytotoxic impact of the curcumin-based oral gel on the viability of the included cell lines over 5 days was evaluated using APH assay. The findings indicate that, when present at concentrations of up to 25 µM, curcumin did not induce cytotoxic effects on HOKs. Consequently, 10 µM and 25 µM concentrations were chosen for further investigations involving this cell line (Figure 2A). In the case of OKF6 and DOKs, the highest curcumin concentration that did not result in cytotoxicity was determined to be 50 µM. Thus, 25 µM and 50 µM concentrations were selected for subsequent experiments, as illustrated in Figure 2B,C. Finally, the APH assay showed that curcumin statistically significantly inhibits the viability of PE/CA-PJ15 at concentrations of 250 µM and more. Therefore, curcumin concentrations of 50 µM and 100 µM were selected for upcoming experiments (Figure 2D).
Figure 2.
APH to evaluate the cytotoxicity of the curcumin-based oral gel at various concentrations on (A) HOKs, (B) OKF6, (C) DOKs, and (D) PE/CA-PJ15. Data are presented as means and 95% confidence intervals (95% CI). Statistical significance is represented as follows: * p < 0.05, ** p < 0.002, *** p < 0.0005, **** p < 0.0001.
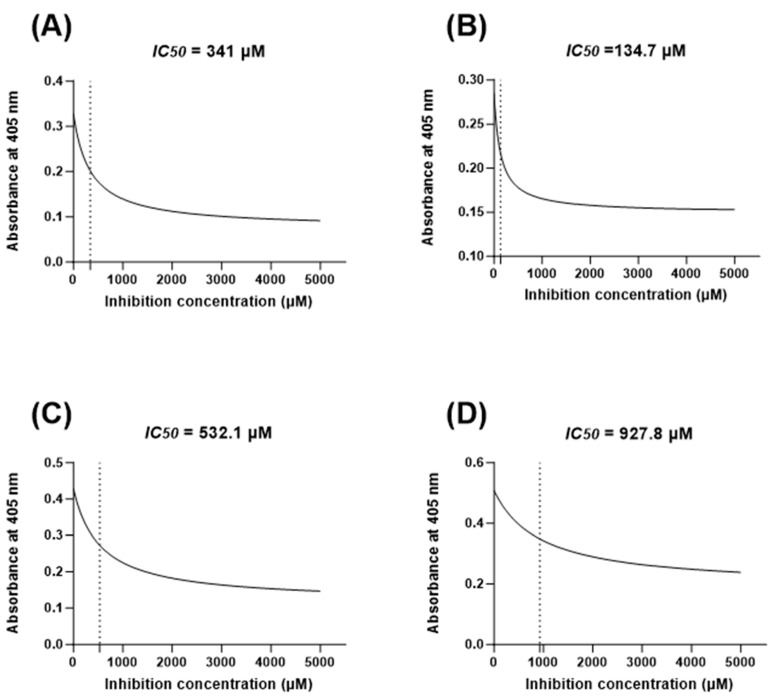
3.3. Identifying the IC50 of H2O2 Concentrations for the In Vitro Oral Mucositis Model
Appropriate IC50 values based on the concentrations of H2O2 that inhibit the viability of 50% of the investigated cells were identified in this study to develop the in vitro oral mucositis model. A curve-fit nonlinear regression model was created for each cell line based on seven concentrations of H2O2. Accordingly, IC50 values were defined as HOKs (341 µM), OKF6 (134.7 µM), DOKs (532.1 µM), and PE/CA-PJ15 (927.8 µM), as shown in Figure 3.
Figure 3.
Curve-fit nonlinear regression models (dose-response curves) to determine the concentration of H2O2 that inhibits 50% of cell viability (IC50) in 24 h for (A) HOKs, (B) OKF6, (C) DOKs, and (D) PE/CA-PJ15.
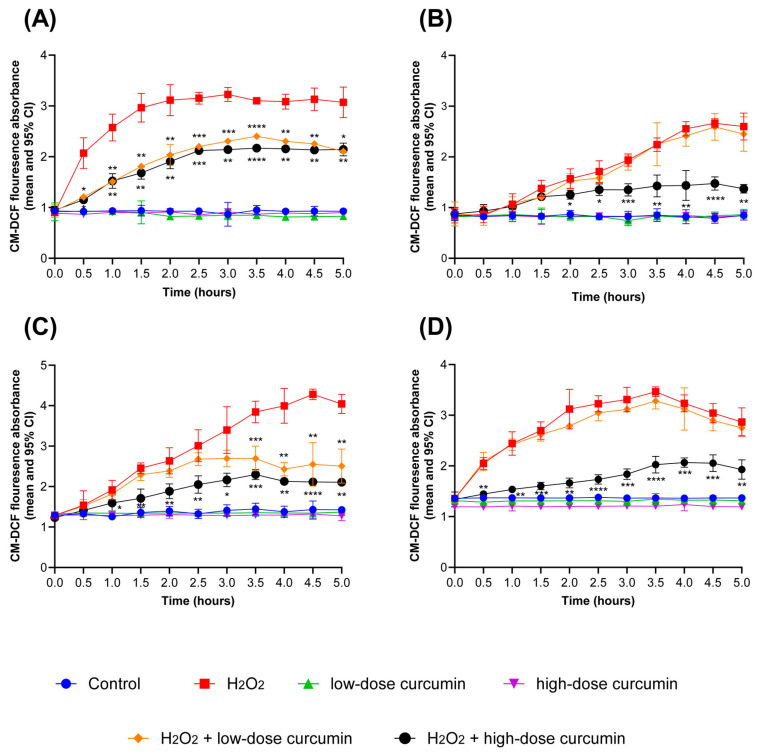
3.4. Efficacy of the Curcumin-Based Oral Gel against Reactive Oxygen Species
In this study, we aimed to assess the effectiveness of curcumin-based oral gel (PerioGold®, Bharma, Perth, WA, Australia) in mitigating ROS production in the in vitro oral mucositis models for the investigated cell lines. The results of this investigation showed a statistically significant decrease in ROS production when HOK cells were pretreated for 24 h with curcumin-based oral gel before stimulating them with H2O2, regardless of the curcumin concentration, as compared with cells exposed to H2O2 alone, p < 0.05 (Figure 4A). This reduction in ROS levels was consistently observed across all investigated time intervals, starting from 0.5 h to 5 h. Furthermore, a dose-dependent effect of curcumin on ROS production was also reported among HOKs; specifically, cell groups pretreated with higher curcumin concentrations (25 µM) exhibited a more pronounced reduction in ROS levels compared with those exposed to lower curcumin doses (10 µM). However, this significant difference in ROS reduction was primarily observed between the 3 h and 4.5 h timepoints, p < 0.05 (Figure 4A).
Figure 4.
The protective effect of the curcumin-based oral gel (PerioGold®, Bharma, Perth, WA, Australia) on ROS production in the model of oxidative stress for (A) HOKs, (B) OKF6, (C) DOKs, and (D) PE/CA-PJ15. H2O2 levels; HOKs (341 µM), OKF6 (134.7 µM), DOKs (532.1 µM), and PE/CA-PJ15 (927.8 µM). Low-dose curcumin; HOKs (10 µM), OKF6 (25 µM), DOKs (25 µM), and PE/CA-PJ15 (50 µM). High-dose curcumin; HOKs (25 µM), OKF6 (50 µM), DOKs (50 µM), and PE/CA-PJ15 (100 µM). Statistical significance values represent the difference in comparison with H2O2-induced groups. Statistical significance is defined as follows: * p < 0.05, ** p < 0.002, *** p < 0.0005, **** p < 0.0001.
In the case of OKF6 cells, pretreatment with low-dose curcumin (25 µM) for 24 h before stimulation with H2O2 did not result in a statistically significant reduction in ROS production when compared with groups exposed to H2O2 alone (p > 0.05). Conversely, when OKF6 cells were subjected to high-dose curcumin (50 µM), a statistically significant reduction in ROS production was observed (p < 0.05). This reduction commenced from the second hour of exposure and persisted in subsequent time intervals (Figure 4B).
In DOK cells, pretreatment with low curcumin levels (25 µM) failed to yield a statistically significant reduction in ROS production when compared with the groups exposed to H2O2 alone (p > 0.05); this lack of significance persisted until the third hour. Conversely, the application of high-dose curcumin (50 µM) before the H2O2 stimulation led to a statistically significant reduction in ROS production across all assessed time intervals, p < 0.05 (Figure 4C).
The PE/CA-PJ15 cell line displayed a distinctive response to curcumin treatment. Groups pretreated with low doses of curcumin-based oral gel (50 µM) failed to reduce ROS production compared with groups stimulated with H2O2 alone (Figure 4D). However, high-dose curcumin pretreatment (100 µM) 24 h before stimulation with H2O2 resulted in a statistically significant reduction in ROS production, and this pattern remained consistent throughout the experiment, p < 0.05 (Figure 4D).
4. Discussion
Oral mucositis remains a common and distressing side effect of cancer therapy, particularly in patients undergoing chemotherapy and radiation treatments. Curcumin is renowned for its antioxidant and anti-inflammatory properties, making it an attractive candidate for managing oral mucositis [15]. The present study aimed to characterise and evaluate the efficacy of a curcumin-based oral gel, PerioGold® (Bharma Pty Ltd., Perth, WA, Australia), in managing oral mucositis. To achieve this, a comprehensive investigation was conducted using various cell lines and experimental techniques. To the best of our knowledge, this is the first study that assesses the oxidant protective role of curcumin in a commercially available product among a panel of oral cell lines, including dysplastic and carcinogenic cells.
In our investigation, mass spectrometry played a pivotal role in characterising the composition of PerioGold®, specifically the presence and quantity of curcumin. The quantification of curcumin content ensures the reliability and consistency of this product for potential therapeutic use. Moreover, LC-MS/MS is often preferred for its superior selectivity and sensitivity, especially in complex matrices or when dealing with low concentrations of specific components [23]. Interestingly, the LC-MS/MS assay identified other parts with antioxidant roles, such as diethanolamine and cinnamyl carbonate [24,25]. Although cinnamyl carbonate is primarily used in industries to contribute to the aroma and scent of products, it is derived from cinnamic acid, an organic compound with various plant sources and established antioxidant activities [25]. The experiments of this study were conducted based on the concentration of curcumin in samples of PerioGold®; comprehensively quantifying other components and assessing their role in the developed in vitro model may provide an opportunity to understand the protective mechanism of PerioGold® better and help propose personalised treatment based on individual variables.
As in vitro cytotoxicity tests of therapeutic agents are more sensitive than in vivo tests, they serve as a screening tool to determine the likelihood of any material producing toxicological reactions in patients. Moreover, they play a vital aspect in planning in vitro studies, as they ensure that the observed effects are in a controlled environment and specific to the treatment being investigated, not due to cellular damage or other biological interactions [26,27]. In this study, the sensitivity to curcumin varied from 25µM to 100µM, as highlighted by the differences observed among the investigated cell lines. More importantly, the potential cytotoxicity of the curcumin-based oral gel was assessed in this study over five days rather than 24 or 48 h. This offered several advantages to evaluating cumulative cytotoxic effects that mimic prolonged exposure scenarios, especially when considering that the investigated product was not purely based on curcumin and included other manufacturing components that may exert cytotoxicity.
An integral aspect of this study was the development of an in vitro model that mimics oral mucositis by inducing cells with H2O2. Such a model is not novel and has been adopted and validated in several previous studies [22,28]. The literature includes several in vitro models that employed various approaches to simulate oxidative stress damage, such as ultraviolet (UV) radiation and ionising radiation [29,30]. However, inducing oxidative stress through H2O2 offers several advantages over other models. These advantages primarily result from the controlled and targeted nature of H2O2 exposure compared with UV and ionising radiation, which can be broader and less specific. Moreover, H2O2 predominantly generates hydroxyl radicals (OH•), a particular type of ROS relevant to oral mucositis pathogenesis [31,32]. UV and ionising radiation, on the other hand, produce a more comprehensive array of ROS, making it challenging to attribute effects solely to a specific ROS type [33].
The distinct responses of different cell lines to H2O2, as evidenced by the variability in their IC50 values, reveal the complex and cell-type-specific nature of the oral mucositis model. This is seen in the literature, where the range of H2O2 concentrations to induce oxidative stress spans from 10 µM for cells such as B lymphocytes to over 1000 µM in cancerous cell lines such as uterus squamous cell carcinoma [34,35,36]. This can be attributed to genetic variability, enzymatic defence systems, and cellular redox status [37]. This may also explain the high resistance of DOK PE/CA-PJ15 cell lines to oxidative stress in this study, as they may exhibit alterations in various cellular processes and have developed increased antioxidant systems compared with normal cells due to oncogenic changes [38,39]. More importantly, it reflects heterogeneities among patients undergoing cancer therapy, which necessitate treatment strategies personalised to the individuals’ risk.
The differential protective responses of curcumin against ROS production in the investigated cell lines highlight the cell-specific nature of curcumin’s impact on ROS regulation. Nonetheless, the curcumin-based oral gel significantly reduced ROS production at certain stages and concentrations. Thus, it is worth noting that, due to individual heterogeneities, applying curcumin for therapeutic uses should be based on agents that can stay long in the oral cavity, emphasising the significance of using hydrophobic gel rather than oral rinse. Our results are also consistent with previous studies where curcumin played a significant protective role against ROS in periodontal ligament stem cells [40] and epidermal immortal keratinocyte cells (HaCat) [41].
While this study offers promising insights, there are several limitations to consider. First, this study was conducted in vitro, and in vivo studies are necessary to evaluate the efficacy and safety of curcumin-based treatments in a more complex biological context. Second, the dose-dependent responses observed among different cell lines emphasise the need for precise dosing strategies. Dosing considerations may need further refinement to maximise the therapeutic benefits and minimise potential adverse effects. Finally, translating in vitro findings to clinical applications requires a comprehensive understanding of the pharmacokinetics, pharmacodynamics, and formulation of curcumin-based therapies. Further research is needed to bridge this gap and bring curcumin-based treatments closer to clinical use.
In conclusion, the present study is the first to identify the protective efficacy of a commercially available product based on curcumin against oral mucositis by utilising heterogeneous cell lines where curcumin significantly reduced ROS production. This reported dose–response pattern emphasised the need to utilise mucoadhesive and long-acting formulations. Clinical studies are essential to validate the in vitro findings by comparing them with other current therapies and establishing practical guidelines for managing patients with oral mucositis.
Author Contributions
Conceptualisation, M.I. and O.K.; methodology, M.I. and O.K.; validation, M.I. and O.K.; investigation, M.I. and O.K.; data curation, M.I. and O.K.; writing—original draft preparation, M.I. and O.K.; project administration, O.K.; funding acquisition, O.K.. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data supporting this study’s findings are available on request from the corresponding author. The data are not publicly available due to privacy.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
The authors declare that this study received funding from Curliniam Pty Ltd., awarded through an industry agreement signed with the University of Western Australia, Office of Research. The funder was not involved in the study design, collection, analysis, interpretation of data, writing of this article, or decision to submit it for publication.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Kok R., van Schaijik B., Johnson N.W., Malki M.I., Frydrych A., Kujan O. Breath biopsy, a novel technology to identify head and neck squamous cell carcinoma: A systematic review. Oral Dis. 2023;29:3034–3048. doi: 10.1111/odi.14305. [DOI] [PubMed] [Google Scholar]
- 2.Cancer-Australia Cancer Australia: Head and Neck Cancer in Australia Statistics. [(accessed on 24 September 2023)]; Available online: https://www.canceraustralia.gov.au/cancer-types/head-and-neck-cancer/statistics.
- 3.Pulito C., Cristaudo A., Porta C., Zapperi S., Blandino G., Morrone A., Strano S. Oral mucositis: The hidden side of cancer therapy. J. Exp. Clin. Cancer Res. 2020;39:210. doi: 10.1186/s13046-020-01715-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ahadian H., Yassaei S., Bouzarjomehri F., Ghaffari Targhi M., Kheirollahi K. Oral Complications of The Oromaxillofacial Area Radiotherapy. Asian Pac. J. Cancer Prev. 2017;18:721–725. doi: 10.22034/APJCP.2017.18.3.721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sciubba J.J., Goldenberg D. Oral complications of radiotherapy. Lancet Oncol. 2006;7:175–183. doi: 10.1016/S1470-2045(06)70580-0. [DOI] [PubMed] [Google Scholar]
- 6.Mallick S., Benson R., Rath G.K. Radiation induced oral mucositis: A review of current literature on prevention and management. Eur. Arch. Oto-Rhino-Laryngol. 2016;273:2285–2293. doi: 10.1007/s00405-015-3694-6. [DOI] [PubMed] [Google Scholar]
- 7.Rosenthal D.I., Trotti A. Strategies for managing radiation-induced mucositis in head and neck cancer. Semin. Radiat. Oncol. 2009;19:29–34. doi: 10.1016/j.semradonc.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 8.Aghamohamamdi A., Hosseinimehr S.J. Natural Products for Management of Oral Mucositis Induced by Radiotherapy and Chemotherapy. Integr. Cancer Ther. 2016;15:60–68. doi: 10.1177/1534735415596570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kodiyan J., Amber K.T. A Review of the Use of Topical Calendula in the Prevention and Treatment of Radiotherapy-Induced Skin Reactions. Antioxidants. 2015;4:293–303. doi: 10.3390/antiox4020293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oshvandi K., Vafaei S.Y., Kamallan S.R., Khazaei S., Ranjbar H., Mohammadi F. Effectiveness of zinc chloride mouthwashes on oral mucositis and weight of patients with cancer undergoing chemotherapy. BMC Oral. Health. 2021;21:364. doi: 10.1186/s12903-021-01706-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fosmire G.J. Zinc toxicity. Am. J. Clin. Nutr. 1990;51:225–227. doi: 10.1093/ajcn/51.2.225. [DOI] [PubMed] [Google Scholar]
- 12.Tian X., Liu X.L., Pi Y.P., Chen H., Chen W.Q. Oral Zinc Sulfate for Prevention and Treatment of Chemotherapy-Induced Oral Mucositis: A Meta-Analysis of Five Randomized Controlled Trials. Front. Oncol. 2018;8:484. doi: 10.3389/fonc.2018.00484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shuai T., Tian X., Xu L.L., Chen W.Q., Pi Y.P., Zhang L., Wan Q.Q., Li X.E. Oral Glutamine May Have No Clinical Benefits to Prevent Radiation-Induced Oral Mucositis in Adult Patients with Head and Neck Cancer: A Meta-Analysis of Randomized Controlled Trials. Front. Nutr. 2020;7:49. doi: 10.3389/fnut.2020.00049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Holecek M. Side effects of amino acid supplements. Physiol. Res. 2022;71:29–45. doi: 10.33549/physiolres.934790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wilken R., Veena M.S., Wang M.B., Srivatsan E.S. Curcumin: A review of anti-cancer properties and therapeutic activity in head and neck squamous cell carcinoma. Mol. Cancer. 2011;10:12. doi: 10.1186/1476-4598-10-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sahin T.K., Bilir B., Kucuk O. Modulation of inflammation by phytochemicals to enhance efficacy and reduce toxicity of cancer chemotherapy. Crit. Rev. Food Sci. Nutr. 2023;63:2494–2508. doi: 10.1080/10408398.2021.1976721. [DOI] [PubMed] [Google Scholar]
- 17.Barzegar A., Moosavi-Movahedi A.A. Intracellular ROS protection efficiency and free radical-scavenging activity of curcumin. PLoS ONE. 2011;6:e26012. doi: 10.1371/journal.pone.0026012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Normando A.G.C., de Meneses A.G., de Toledo I.P., Borges G.A., de Lima C.L., Dos Reis P.E.D., Guerra E.N.S. Effects of turmeric and curcumin on oral mucositis: A systematic review. Phytother. Res. 2019;33:1318–1329. doi: 10.1002/ptr.6326. [DOI] [PubMed] [Google Scholar]
- 19.Sivani B.M., Azzeh M., Patnaik R., Pantea Stoian A., Rizzo M., Banerjee Y. Reconnoitering the Therapeutic Role of Curcumin in Disease Prevention and Treatment: Lessons Learnt and Future Directions. Metabolites. 2022;12:639. doi: 10.3390/metabo12070639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Buhrmann C., Mobasheri A., Busch F., Aldinger C., Stahlmann R., Montaseri A., Shakibaei M. Curcumin modulates nuclear factor kappaB (NF-kappaB)-mediated inflammation in human tenocytes in vitro: Role of the phosphatidylinositol 3-kinase/Akt pathway. J. Biol. Chem. 2011;286:28556–28566. doi: 10.1074/jbc.M111.256180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ashrafizadeh M., Ahmadi Z., Mohammadinejad R., Farkhondeh T., Samarghandian S. Curcumin Activates the Nrf2 Pathway and Induces Cellular Protection Against Oxidative Injury. Curr. Mol. Med. 2020;20:116–133. doi: 10.2174/1566524019666191016150757. [DOI] [PubMed] [Google Scholar]
- 22.Cao Y., Xu R.X., Liu Z. A high-throughput quantification method of curcuminoids and curcumin metabolites in human plasma via high-performance liquid chromatography/tandem mass spectrometry. J. Chromatogr. B Analyt Technol. Biomed. Life Sci. 2014;949–950:70–78. doi: 10.1016/j.jchromb.2013.12.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yiannis C., Huang K., Tran A.N., Zeng C., Dao E., Baselyous O., Mithwani M.A., Paolini R., Cirillo N., Yap T., et al. Protective effect of kava constituents in an in vitro model of oral mucositis. J. Cancer Res. Clin. Oncol. 2020;146:1801–1811. doi: 10.1007/s00432-020-03253-3. [DOI] [PubMed] [Google Scholar]
- 24.Pitt J.J. Principles and applications of liquid chromatography-mass spectrometry in clinical biochemistry. Clin. Biochem. Rev. 2009;30:19–34. [PMC free article] [PubMed] [Google Scholar]
- 25.Fiume M.M., Heldreth B., Bergfeld W.F., Belsito D.V., Hill R.A., Klaassen C.D., Liebler D.C., Marks J.G., Jr., Shank R.C., Slaga T.J., et al. Safety Assessment of Diethanolamine and Its Salts as Used in Cosmetics. Int. J. Toxicol. 2017;36:89S–110S. doi: 10.1177/1091581817707179. [DOI] [PubMed] [Google Scholar]
- 26.Pontiki E., Hadjipavlou-Litina D., Litinas K., Geromichalos G. Novel cinnamic acid derivatives as antioxidant and anticancer agents: Design, synthesis and modeling studies. Molecules. 2014;19:9655–9674. doi: 10.3390/molecules19079655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Di Nunzio M., Valli V., Tomas-Cobos L., Tomas-Chisbert T., Murgui-Bosch L., Danesi F., Bordoni A. Is cytotoxicity a determinant of the different in vitro and in vivo effects of bioactives? BMC Complement. Altern. Med. 2017;17:453. doi: 10.1186/s12906-017-1962-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Castelmur I., DiPaolo C., Bachmann M.F., Hengartner H., Zinkernagel R.M., Kundig T.M. Comparison of the sensitivity of in vivo and in vitro assays for detection of antiviral cytotoxic T cell activity. Cell. Immunol. 1993;151:460–466. doi: 10.1006/cimm.1993.1254. [DOI] [PubMed] [Google Scholar]
- 29.Mohammed A.I., Sangha S., Nguyen H., Shin D.H., Pan M., Park H., McCullough M.J., Celentano A., Cirillo N. Assessment of Oxidative Stress-Induced Oral Epithelial Toxicity. Biomolecules. 2023;13:1239. doi: 10.3390/biom13081239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Straface E., Giacomoni P.U., Malorni W. Cultured cells as a model system for the study of UV-induced cytotoxicity. J. Photochem. Photobiol. B. 2001;63:52–60. doi: 10.1016/S1011-1344(01)00215-9. [DOI] [PubMed] [Google Scholar]
- 31.Khan A., Bai H., Liu E., Chen M., Yu C., Wang R., Khan A., Bai Z. Protective effect of neferine against UV-B-mediated oxidative damage in human epidermal keratinocytes. J. Dermatol. Treat. 2018;29:733–741. doi: 10.1080/09546634.2018.1441490. [DOI] [PubMed] [Google Scholar]
- 32.Puppo A., Halliwell B. Formation of hydroxyl radicals from hydrogen peroxide in the presence of iron. Is haemoglobin a biological Fenton reagent? Biochem. J. 1988;249:185–190. doi: 10.1042/bj2490185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sonis S.T. A hypothesis for the pathogenesis of radiation-induced oral mucositis: When biological challenges exceed physiologic protective mechanisms. Implications for pharmacological prevention and treatment. Support. Care Cancer. 2021;29:4939–4947. doi: 10.1007/s00520-021-06108-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.de Jager T.L., Cockrell A.E., Du Plessis S.S. Ultraviolet Light Induced Generation of Reactive Oxygen Species. Adv. Exp. Med. Biol. 2017;996:15–23. doi: 10.1007/978-3-319-56017-5_2. [DOI] [PubMed] [Google Scholar]
- 35.Ransy C., Vaz C., Lombes A., Bouillaud F. Use of H2O2 to Cause Oxidative Stress, the Catalase Issue. Int. J. Mol. Sci. 2020;21:9149. doi: 10.3390/ijms21239149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li X., Wu Z., Wang Y., Mei Q., Fu X., Han W. Characterization of adult alpha- and beta-globin elevated by hydrogen peroxide in cervical cancer cells that play a cytoprotective role against oxidative insults. PLoS ONE. 2013;8:e54342. doi: 10.1371/journal.pone.0054342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Saito A., Sugisawa A., Umegaki K., Sunagawa H. Protective effects of quercetin and its metabolites on H2O2-induced chromosomal damage to WIL2-NS cells. Biosci. Biotechnol. Biochem. 2004;68:271–276. doi: 10.1271/bbb.68.271. [DOI] [PubMed] [Google Scholar]
- 38.Aw T.Y. Molecular and cellular responses to oxidative stress and changes in oxidation-reduction imbalance in the intestine. Am. J. Clin. Nutr. 1999;70:557–565. doi: 10.1093/ajcn/70.4.557. [DOI] [PubMed] [Google Scholar]
- 39.Perillo B., Di Donato M., Pezone A., Di Zazzo E., Giovannelli P., Galasso G., Castoria G., Migliaccio A. ROS in cancer therapy: The bright side of the moon. Exp. Mol. Med. 2020;52:192–203. doi: 10.1038/s12276-020-0384-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tan L., Cao Z., Chen H., Xie Y., Yu L., Fu C., Zhao W., Wang Y. Curcumin reduces apoptosis and promotes osteogenesis of human periodontal ligament stem cells under oxidative stress in vitro and in vivo. Life Sci. 2021;270:119125. doi: 10.1016/j.lfs.2021.119125. [DOI] [PubMed] [Google Scholar]
- 41.Liu Y.H., Lin Y.S., Huang Y.W., Fang S.U., Lin S.Y., Hou W.C. Protective Effects of Minor Components of Curcuminoids on Hydrogen Peroxide-Treated Human HaCaT Keratinocytes. J. Agric. Food Chem. 2016;64:3598–3608. doi: 10.1021/acs.jafc.6b01196. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data supporting this study’s findings are available on request from the corresponding author. The data are not publicly available due to privacy.