Abstract
This study compares the rate of selected types of mental illnesses (stress, anxiety, depression) and sleep disorders (insomnia, sleep apnea) according to the status of eight male genital problems. Analyses utilize medical claims data for male employees aged 18 to 64 years of a large corporation, 2017 to 2021. Approximately 1,076 (7.3%) men per year have one or more genital problems. The most common being benign prostatic hyperplasia (BPH; 3.8%) and then erectile dysfunction (ED; 1.7%). For BPH patients, the rate experiencing stress, anxiety, depression, or a combination of these is 0.96%, 6.2%, 5.3%, and 5.1%, respectively. Corresponding rates for ED are 1.5%, 7.2%, 5.9%, and 7.5%. For BPH patients, the rate experiencing insomnia, sleep apnea, or both is 3.1%, 22.7%, and 2.0%, respectively. Corresponding rates for ED are 1.2%, 20.6%, and 2.2%. Male genital problems positively associate with having one or more mental illnesses (stress, anxiety, depression), except for hydrocele, with ED and penis disorder having the strongest associations. Male genital problems also positively associate with having insomnia and/or sleep apnea, except for infertility and orchitis, with BPH and ED having the strongest associations. The positive associations involving BPH and ED with mental illnesses are each more pronounced in the younger age group (18–49 vs. 50–64). Similar results are seen in the models involving sleep disorders. Thus, comorbid male genital problems, mental illnesses, and sleep disorders exist, with the strength of associations unique to the male genital problem and sometimes modified by age.
Keywords: anxiety, depression, stress, insomnia, sleep apnea, male genital problems, medical claims
Introduction
Male genital problems, mental illnesses, and sleep disorders are important and interrelated challenges that can greatly affect an individual’s overall quality of life. Male genital problems, comprising a spectrum of conditions such as benign prostatic hyperplasia (BPH), erectile dysfunction (ED), and infertility, pose health concerns for men throughout the world. These conditions are associated with psychological health and mental illness (Tan et al., 2012). Studies have identified that these genital problems are linked to an increased risk of stress, anxiety, depression, bipolar disorder, and sleep problems (Harvard Health Publishing, 2009; Tzeng et al., 2019). Conversely, mental health disorders can also influence the progression of male genital problems (Waldinger, 2015). For example, a meta-analysis reported that depression increased the risk of ED, and that ED also increased the risk of depression (Q. Liu et al., 2018). While BPH can cause stress, it is possible that stress may cause levels of certain hormones to change and trigger the release of adrenaline, contributing to prostate enlargement (Ullrich et al., 2005, 2007).
Sleep disorders are also intricately linked to male genital problems. Sleep disorders, such as sleep apnea and insomnia, have been linked to an increased risk of BPH, ED, and infertility (Andersen & Tufik, 2022; Cho & Duffy, 2019; Ma & Dong, 2023). For example, sleep disorders can increase oxidative stress, which then contributes to DNA fragmentation and subsequent infertility (Alahmar, 2019; Pasqualotto et al., 2000). In addition, male genital problems such as BPH may lead to sleep disturbances and disorders, further putting an increased burden on individuals’ mental well-being (Chartier-Kastler et al., 2012; Ma & Dong, 2023).
Certain risk factors can contribute to the development of male genital problems, mental illness, and sleep disorders. Some common factors that may underlie their interconnections include obesity (Jorm et al., 2003; Y. Liu et al., 2023), sedentary lifestyle (Gerbild et al., 2018; Kredlow et al., 2015), stress (De Berardis et al., 2014; Kalmbach et al., 2018), age (Rosen et al., 2003), and genetics (Carr et al., 2013; Green et al., 2022).
The current study will examine associations between several common male genital problems and mental illnesses and sleep disorders. The focus will be on mental illnesses involving stress, anxiety, and/or depression and sleep disorders involving insomnia and/or sleep apnea. The strength of the associations will be compared between models involving mental illnesses and sleep disorders. Interaction effects with selected demographic variables (age, marital status, and dependent children) will also be considered in the models.
Materials and Methods
Study Population
The current study involves individuals receiving health insurance from the Deseret Mutual Benefit Administrator (DMBA). Since 1970 the DMBA has provided health insurance and retirement income to employees and their families of the Church of Jesus Christ of Latter-day Saints. The study utilizes electronic claims data for the years 2017 to 2021. A “claim” is a notification to DMBA requesting a medical benefit payment. We do not include pharmaceutical claims in this paper.
Each year the cohort consisted of approximately 23,175 (27%) employees, 18,334 (21%) spouses, 41,693 (49%) dependent children, and 2,583 (3%) other (e.g., married child, stepchild, disabled dependent). Among employees, 7,880 (34%) worked in the Church education system, seminaries, and institutes; 7,184 (31%) as manual laborers; 2,318 (10%) in other companies; 1,391 (6%) were retired; and the remaining 4,403 (19%) worked in other capacities. Geographic areas represented by the employees were 16,706 (72%) in Utah, 2,073 (9%) in Idaho, 2,174 (9%) in Pacific states, and 2,222 (10%) in other American states. Employee retention was about 92% from year to year.
When employees retired, DMBA is no longer subsidized, and many chose another insurance carrier. For this reason, we dropped individuals aged 65 years or older from the current study.
Data Collection
The study involved male DMBA employees: 14,781 in 2017, 15,029 in 2018, 14,849 in 2019, 14,379 in 2020, and 14,408 in 2021. These data represent eligibility data linked to automated medical claims records using a common identifying number. After the data linkage and prior to analysis, the database was de-identified in accordance with the Health Insurance Portability and Accountability Act guidelines.
Classification of mental illness, sleep disorders, and male genital problems was based on the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM). Diagnostic and Statistical Manual of Mental Disorders (DSM) helps psychiatrists, physicians, clinical psychologists, and other health professionals diagnose behavioral health issues (American Psychiatric Association, 2022). The DSM diagnostic criteria serve as a guide in determining billing codes according to the ICD-10-CM. Codes used to classify mental illnesses are F32–F33 for depression, F40–F41 for anxiety, and F43 for stress. Codes used to classify sleep disorders are G470 for insomnia and G473 for sleep apnea. Codes used for classifying male genital problems are N40 for BPH, N41 for inflammatory diseases of the prostate (IDP), N43 for hydrocele and spermatocele, N45 for orchitis and epididymitis, N46 for male infertility, N48 for other disorders of the penis, N49 for inflammatory disorders of the male genital organs, and N52 for ED. Other male genital problems combine N42 for other and unspecified disorders of the prostate, N44 for noninflammatory disorders of the testis, N47 for disorders of prepuce, N49 for inflammatory disorders of male genital organs, N51 for disorders of male genital organs in diseases classified elsewhere, and N53 for other male sexual dysfunction.
Rates consist of the number of employees filing one or more claims for each condition divided by the total number of employees. If multiple claims are filed by an employee in a year for a given condition, it is only counted once in the numerator of the rate calculation. However, an individual may contribute to more than one type of mental illness, sleep disorder, or genital problem each year.
Other variables considered in this study are age, marital status, dependent children status, and year. Classifications for these variables appear in Table 1.
Table 1.
Selected Mental Illnesses (Stress, Anxiety, Depression) and Sleep Disorders (Insomnia, Sleep Apnea) According to Demographic and Men’s Health Variables Among DMBA Employees, 2017–2021.
| Number | % | Stress, anxiety, depression | Insomnia, sleep apnea | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | c2 P value | Odds ratio a | 95% LCL a | 95% UCL a | % | c2P value | Odds ratio a | 95% LCL a | 95% UCL a | |||
| All employees | 73,446 | 12.47 | 13.23 | |||||||||
| Age | ||||||||||||
| 50–64 | 29,650 | 40.37 | 12.81 | .0007 | 1.00 | 19.86 | ||||||
| 18–49 | 43,796 | 59.63 | 11.97 | 1.04 | 0.99 | 1.09 | 8.75 | <.0001 | 0.40 | 0.38 | 0.42 | |
| Married | ||||||||||||
| No | 8,054 | 10.97 | 13.15 | .0508 | 1.00 | 7.45 | <.0001 | |||||
| Yes | 65,392 | 89.03 | 12.39 | 0.83 | 0.77 | 0.91 | 13.95 | 1.73 | 1.58 | 1.90 | ||
| Dependent children | ||||||||||||
| No | 18,222 | 24.81 | 11.50 | <.0001 | 1.00 | 13.81 | .0083 | |||||
| Yes | 55,224 | 75.19 | 12.79 | 1.20 | 1.12 | 1.27 | 13.04 | 0.99 | 0.94 | 1.05 | ||
| BPH | ||||||||||||
| No | 70,623 | 96.16 | 12.27 | <.0001 | 1.00 | 12.66 | <.0001 | |||||
| Yes | 2,823 | 3.84 | 17.53 | 1.65 | 1.49 | 1.83 | 27.67 | 1.75 | 1.61 | 1.91 | ||
| IDP | ||||||||||||
| No | 72,944 | 99.32 | 12.43 | .0002 | 1.00 | 13.17 | <.0001 | |||||
| Yes | 502 | 0.68 | 17.93 | 1.62 | 1.28 | 2.03 | 22.31 | 1.48 | 1.19 | 1.83 | ||
| Hydrocele | ||||||||||||
| No | 73,167 | 99.62 | 12.47 | .8265 | 1.00 | 13.21 | .0014 | |||||
| Yes | 279 | 0.38 | 12.90 | 1.05 | 0.74 | 1.49 | 19.71 | 1.43 | 1.06 | 1.94 | ||
| Infertile | ||||||||||||
| No | 73,194 | 99.66 | 12.45 | <.0001 | 1.00 | 13.23 | .802 | |||||
| Yes | 252 | 0.34 | 19.44 | 1.77 | 1.30 | 2.43 | 12.7 | 1.40 | 0.96 | 2.03 | ||
| Orchitis | ||||||||||||
| No | 73,155 | 99.6 | 12.45 | .0016 | 1.00 | 13.22 | .141 | |||||
| Yes | 291 | 0.4 | 18.56 | 1.63 | 1.21 | 2.19 | 16.15 | 1.30 | 0.95 | 1.79 | ||
| Erectile dysfunction | ||||||||||||
| No | 72,207 | 98.31 | 12.30 | <.0001 | 1.00 | 13.01 | <.0001 | |||||
| Yes | 1,239 | 1.69 | 22.11 | 2.09 | 1.82 | 2.40 | 26.15 | 1.79 | 1.57 | 2.04 | ||
| Penis | ||||||||||||
| No | 73,202 | 99.67 | 12.43 | <.0001 | 1.00 | 13.21 | .0016 | |||||
| Yes | 244 | 0.33 | 24.59 | 2.36 | 1.76 | 3.16 | 20.08 | 1.42 | 1.04 | 1.96 | ||
| Other | ||||||||||||
| No | 72,908 | 99.27 | 12.45 | .1188 | 1.00 | 13.21 | .0114 | |||||
| Yes | 538 | 0.73 | 14.68 | 1.20 | 0.95 | 1.53 | 16.91 | 1.33 | 1.06 | 1.68 | ||
| Any | ||||||||||||
| No | 68,066 | 92.7 | 11.12 | <.0001 | 1.00 | 12.4 | <.0001 | |||||
| Yes | 5380 | 7.3 | 18.49 | 1.77 | 1.64 | 1.91 | 23.81 | 1.68 | 1.57 | 1.80 | ||
| Year | ||||||||||||
| 2017 | 14,781 | 20.12 | 10.71 | <.0001 | 1.00 | 12.2 | .0011 | |||||
| 2018 | 15,029 | 20.46 | 11.72 | 1.11 | 1.03 | 1.19 | 13.25 | 1.10 | 1.03 | 1.18 | ||
| 2019 | 14,849 | 20.22 | 12.80 | 1.22 | 1.14 | 1.31 | 13.64 | 1.14 | 1.07 | 1.22 | ||
| 2020 | 14,379 | 19.58 | 13.11 | 1.26 | 1.17 | 1.35 | 13.55 | 1.13 | 1.05 | 1.21 | ||
| 2021 | 14,408 | 19.62 | 14.98 | 1.36 | 1.27 | 1.46 | 13.53 | 1.13 | 1.06 | 1.21 | ||
Note. DMBA = Deseret Mutual Benefit Administrator; LCL = lower confidence level; UCL = upper confidence limit; BPH = benign prostatic hyperplasia; IDP = inflammatory diseases of the prostate.
Adjusted for age, marital status, dependent children, and year.
Statistical Techniques
Numbers, percentages, means, and standard deviations (SD) were used to describe selected variables. The method of maximum likelihood estimated parameters in the logistic regression models. The models derived odds ratios measuring associations between male genital problems and mental illnesses (stress, anxiety, and/or depression) and sleep disorders (insomnia and/or sleep apnea), adjusted for age, marital status, dependent children, and year. Interaction terms were assessed in the models using the Wald Chi-square test. Statistical significance was based on two-sided tests and the 0.05 level. Significance of the adjusted odds ratios occurred when the 95% confidence intervals (CIs) did not contain 1. We conducted our statistical analyses using Statistical Analysis System (SAS) software, version 9.4 (SAS Institute Inc., Cary, NC, USA, 2012).
Results
The mean number of male employees each year is 14,689 (SD = 285). Mean age is 46.2 (SD = 11.3), ranging from 18 to 64. Male employees tend to be married and have dependent children (Table 1). Each year approximately 1,076 (7.3%) experience one or more genital problems. Of these problems, the most common is BPH (n = 565, 3.8%), of which 95 (16.8%) have comorbid conditions. The next most common problem is ED (n = 248, 1.7%), of which 59 (23.8%) have comorbid conditions. Experiencing stress, anxiety, and/or depression occurs in 1,832 (12.5%) men and experiencing insomnia and/or sleep apnea occurs in 1,943 (13.2%) men.
Having a male genital problem positively associates with having one or more of the selected mental illnesses (stress, anxiety, depression), except for hydrocele (Table 1). ED and penis disorder have the strongest significant associations with the mental illnesses. Having a male genital problem also positively associates with having insomnia and/or sleep apnea, except for infertility and orchitis. ED and BPH have the strongest significant associations with these sleep disorders.
Interaction terms were evaluated in the models. Age by BPH and age by ED were each statistically significant (Table 2). The significantly positive associations between BPH and mental illness and between ED and mental illness are each more pronounced in the younger age group (18–49 vs. 50–64). Similar results are seen in the models involving sleep disorders. In addition, BPH is more strongly associated with a sleep disorder among singles (odds ratio = 2.61, 95% CI = [1.74, 3.91]) than married (odds ratio 1.71, 95% CI = [1.57, 1.88]; Wald Chi-Square p = .0091).
Table 2.
Odds of Mental Illnesses or Sleep Disorders by Certain Male Genital Problems According to Age
| Mental illness (stress, anxiety, depression) | |||||||
|---|---|---|---|---|---|---|---|
| Male genital problem | Ages 18–49 | Ages 50–64 | Interaction P value |
||||
| Odds ratio a | 95% LCL a | 95% UCL a | Odds ratio a | 95% LCL a | 95% UCL a | ||
| BPH | 2.38 | 1.85 | 3.07 | 1.56 | 1.39 | 1.74 | .0028 |
| Erectile dysfunction | 2.77 | 2.19 | 3.51 | 1.84 | 1.55 | 2.18 | .0053 |
| Any | 1.96 | 1.74 | 2.22 | 1.67 | 1.52 | 1.84 | .0351 |
| Sleep disorder (insomnia, sleep apnea) | |||||||
| Male genital problem | Ages 18–49 | Ages 50–64 | Interaction P value |
||||
| Odds ratio a | 95% LCL a | 95% UCL a | Odds ratio a | 95% LCL a | 95% UCL a | ||
| BPH | 2.41 | 1.82 | 3.18 | 1.68 | 1.53 | 1.84 | .0028 |
| Erectile dysfunction | 2.87 | 2.21 | 3.71 | 1.56 | 1.35 | 1.81 | .0053 |
| Any | 1.85 | 1.60 | 2.13 | 1.63 | 1.51 | 1.77 | .2156 |
Note. IDP = inflammatory diseases of the prostate. Other (ICD-10-CM): other and unspecified disorder of the prostate (N42), noninflammatory disorders of the testis (N44), disorders of prepuce (N47), inflammatory disorders (N49), disorders of male genital organs (N51), and other male sexual dysfunction (N53). LCL = lower confidence level; UCL = upper confidence limit; BPH = benign prostatic hyperplasia.
Adjusted for marital status, dependent children, and year. Shaded cells are statistically significant at the 0.05 level.
The mental illness outcome variable consists of a combination of stress, anxiety, and depression (Figure 1). Anxiety is the most prevalent mental illness, except among men with a penis disorder, where depression is more common. Men with infertility are most likely to experience a combination of stress, anxiety, and depression, followed by men with ED and then penis disorders.
Figure 1.
Mental Illnesses (Stress, Anxiety, Depression) According to Male Genital Problems Among DMBA Employees, 2017–2021
Note. DMBA = Deseret Mutual Benefit Administrator.
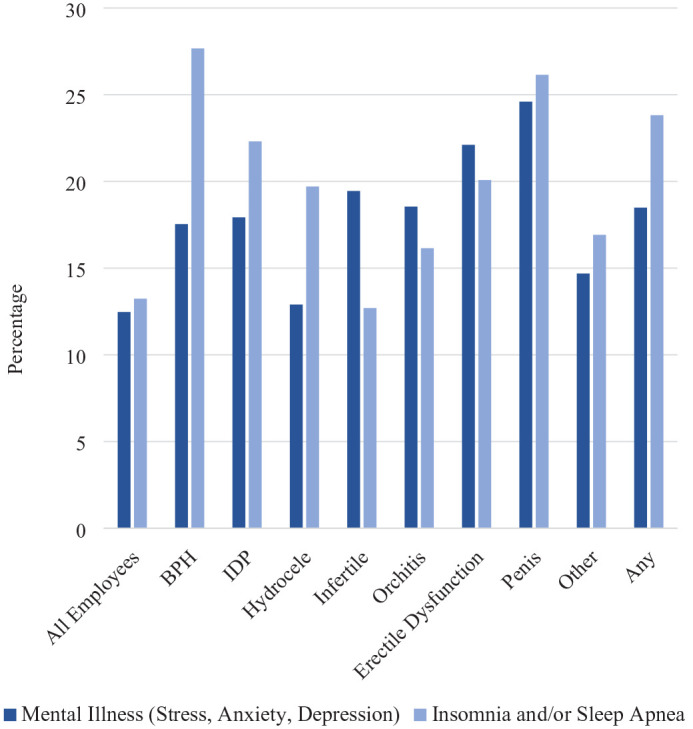
The sleep disorder outcome variable consists of a combination of insomnia and sleep apnea (Figure 2). Sleep disorders are more common in those with a male genital problem, except for male infertility. They are most common in men with BPH and then in men with penis disorders. Sleep apnea is much more common than insomnia for each of the male genital problems.
Figure 2.
Selected Sleep Disorders According to Male Genital Problems Among DMBA Employees, 2017–2021
Note. DMBA = Deseret Mutual Benefit Administrator.
For all males, the prevalence of insomnia and/or sleep apnea is 6.2% greater than the prevalence of mental illnesses (stress, anxiety, depression; Figure 3). Among those men with a genital problem, it is 28.8% greater, with the higher percentage primarily reflected by men with BPH, IDP, and hydrocele. The percentage is lower in men with infertility (−34.7%), orchitis (−12.9%), and ED (−9.2%).
Figure 3.
Mental Illnesses (Stress, Anxiety, Depression) and Sleep Disorders (Insomnia, Sleep Apnea) According to Male Genital Problems in DMBA Employees, 2017–2021
Note. DMBA = Deseret Mutual Benefit Administrator.
Discussion
This study explores the relationship between male genital problems, mental illnesses (stress, anxiety, depression), and sleep disorders (insomnia, sleep apnea) within an adult employee (DMBA) population. The results provide valuable insights into the associations among these health components and confirm the comorbid relationship between male genital problems, mental illness, and sleep disorders. The study compares associations between male genital problems and mental illnesses with associations between male genital problems and sleep disorders. Interaction terms involving selected demographic variables (age, marital status, and dependent children) and the men’s health variables are assessed in the models.
Age, marital status, and dependent children relate to mental illnesses and sleep disorders differently. Whereas mental illness decreases with age and is lower in married (vs. single) and in those without dependent children (vs. having dependent children), sleep disorders increase with age, among married (vs. single), and is not associated with dependent children.
The decrease in mental illness with age is consistent with results from the 2021 National Survey on Drug Use and Health by the Substance Abuse and Mental Health Services Administration (National Institute of Mental Health, 2023). The increase of sleep disorders with age is also identified in previous research (Charandabi et al., 2016; Miner & Kryger, 2017). Sleep disorders increase with age in part because older age is positively associated with factors that negatively affect sleep such as heart disease, diabetes, and arthritis.
Several studies have reported that married people have lower levels of mental illness, especially among men (Coyne et al., 2001; Grundström et al., 2021; Malzberg, 1936; Williams et al., 1992). This may be because married individuals tend to experience more social support, financial support, purpose in life, and are mentally healthier to begin with (Grundström et al., 2021). In contrast, higher levels of sleep apnea among married people may be because having a sleeping partner can help identify the problem. The higher level of stress, anxiety, and depression among men with dependent children may stem from their having extra responsibilities and the added stress this puts on their relationship with their partner (Davé et al., 2009).
Benign Prostatic Hyperplasia
BPH is the most prevalent male genital problem. Among men with BPH, having a sleep disorder is more common than a mental illness. The positive odds ratio comparing the strength of the association between BPH and mental illness is similar to the odds ratio comparing the strength of the association between BPH and sleep disorders, after adjusting for age, marital status, dependent children, and year (see Table 1).
Other research has identified a relationship between BPH and anxiety and depression (Koh et al., 2015). BPH had the strongest association with sleep apnea. In a cohort study of 202 sleep apnea patients and 1,010 controls in Taiwan’s National Health Insurance Research Database, sleep apnea was linked to increased longitudinal risk of BPH (Chou et al., 2014). Sleep disorders can increase oxidative stress, thereby contributing to BPH (Aryal et al., 2007; Pace et al., 2010).
Positive associations between BPH and mental illness and sleep disorders are significantly greater in younger men. Since BPH is more common in older men, a younger man with the problem may experience greater concern. Also, younger men tend to experience more mental illness, contributing to greater oxidative stress and BPH. There may further be a complex link between mental illness and BPH that is influencing the stronger association in younger men between BPH and sleep disorders.
Inflammatory Diseases of the Prostate
Among men with IDP, having a sleep disorder is more common than a mental illness. It is similarly positively associated with both mental illness and sleep disorders in the adjusted models (see Table 1).
Consistent with our results, a study involving rats reported that chronic stress-induced histological inflammation of the prostate (Gatenbeck et al., 1987). In a study of 703 African American men, high self-perceived stress was associated with an increased risk of prostatitis history (Wallner et al., 2009). A study of 1,236 males with obstructive sleep apnea (OSA) and 4,944 males without OSA in the Taiwan Longitudinal Health Insurance Database 2005 identified a positive association between OSA and chronic prostatitis, urinary incontinence, nocturia, ED, urinary calculi, and prostate cancer (Chung et al., 2016).
Hydrocele
A higher percentage of men with hydrocele have sleep disorders than mental illness. Hydrocele is significantly positively associated with sleep disorders but not mental illness in the adjusted models (see Table 1). It may be that inflammation is linked to hydrocele with inflammation resulting from OSA (Chung et al., 2016).
Infertility
A higher percentage of men with infertility experience mental illness than sleep disorders. Infertility is significantly positively associated with mental illness but not sleep disorders (see Table 1). A study of 113 patients reported that depressive symptoms were low at the start of infertility work-up and increased significantly with the duration of infertility. Of those with infertility longer than 2 years, 23.1% experienced mild depressive symptoms (Hegyi et al., 2019).
Orchitis
Men with orchitis (inflammation of one or both testicles) have a higher percentage of mental illness than sleep disorders. Orchitis is significantly positively associated with mental illness but not sleep disorders (see Table 1). Orchitis is usually caused by a bacterial infection or the mumps virus and may cause pain and infertility. Orchialgia is intermittent or constant unilateral or bilateral testicular pain. Research has associated urologic pain and mental health disorders. For example, one study reported that 56% of male patients with genital pain had somatization, 27% had major depression, and 27% had chemical dependency (Schover, 1990). Another study reported that 14% of orchialgia patients had psychiatric or behavioral issues (Ching et al., 2015). In a study of 444 men with orchialgia, the prevalence of mental illnesses (anxiety, depression, post-traumatic stress disorder) was significantly higher than in the general U.S. population based on National Institute of Mental Health Statistics (Mwamukonda et al., 2019).
Erectile Dysfunction
Men with ED have a higher percentage of mental illness than sleep disorders. However, ED is positively associated with both mental illness and sleep disorders (see Table 1).
Considerable research has investigated the psychological effect of ED, with the disorder associated with lower self-esteem and poorer satisfaction with sexual activity, thereby increasing the prevalence of anxiety and depression (Latini et al., 2002). The prevalence of anxiety among men with ED may be as high as 37% (Corretti, 2007). A review article identified a high prevalence and greater severity of anxiety disorder among men with ED (Velurajah et al., 2022). It may be that anxiety contributes to ED and that ED contributes to communication problems and communication problems impedes sexual function (Hedon, 2003). Another review and meta-analysis looked specifically at the association between depression and ED, finding a bidirectional relationship (Q. Liu et al., 2018). The current research found that while anxiety only (7.2%) was more common than depression only (5.9%), most men with ED had both anxiety and depression (7.5%).
Men with ED were much more likely to have sleep apnea than insomnia. Several previous studies have identified an association between sleep apnea and ED (Andersen & Tufik, 2022; Cho & Duffy, 2019; Chung et al., 2016; Pascual et al., 2018). In a study of 207 men with OSA, severe OSA patients had significantly lower testosterone concentration and higher prevalence of ED (Zhang et al., 2016).
The relationship between ED and mental illness is positive, significantly more so for men aged 18 to 49 (vs. 50–64). A similar result is seen for sleep disorders. It may be more psychologically challenging for a younger man to face having ED. Also, younger men are generally more likely to have mental illness, which may contribute to this difference. The stronger positive association between ED and sleep disorders in younger men is unclear and requires further study.
Penis Disorders
Men with penis disorders experience more sleep disorders than mental illness. Adjusted rate ratios measuring the strength of association between penis disorders and mental illness and penis disorders and sleep disorders are similar (see Table 1). Among the male genital problems, penis disorders had the strongest positive association with each of the mental illnesses (stress, anxiety, depression). It also had the second strongest positive association (after BPH) with sleep disorders.
There are several potential causes of penis disorders (congenital abnormalities, alcohol and drug abuse, medications, spinal cord problems, injury, blood diseases, vasculitis, connective tissue disorders, poor hygiene, dermatitis, inflammation, and scar tissue; Beaumont, 2023). Some risk factors for penile conditions (having sexually transmitted infections, abusing alcohol and drugs, smoking) are also associated with greater mental illness and sleep disorders (National Institute of Drug Abuse [NIDA], 2023; Nuñez et al., 2021; Roehrs & Roth, 2015; Singh & Singh, 2021; Smith & Book, 2008).
We did not report associations between the male genital problems and attention-deficit/hyperactivity disorder (ADHD), bipolar disorder, obsessive-compulsive disorder (OCD), and schizophrenia. Further research may consider performing this analysis. Preliminary study found significantly positive associations between any male genital problem and each of these mental illnesses, especially schizophrenia. However, the numbers are small when considering individual male genital types and the less common mental illness, so we chose not to report the results in this paper. In addition, mental illness and sleep disorders are often related, with common risk factors. The odds ratios measuring the associations between the male genital problems and mental illnesses were further adjusted for sleep disorders, but the significance of the relationships did not change (data not reported). A similar outcome occurred when we further adjusted the associations between male genital problems and sleep disorders for mental illnesses (data not reported).
Limitations
Although this study provides valuable insights into the relationships between male genital problems, mental illnesses, and sleep disorders, it is important to acknowledge certain study limitations. The results are based on the employee population, so generalization of the findings is limited to this type of group, who are generally healthier than the nonworking population. Furthermore, as employees retired and many chose another insurance provider than DMBA, we were limited in being able to study those men in this particularly high-risk group for genital problems (e.g., increasing ED; Gareri et al., 2014). The study sample size of men with specific combinations of types of genital problems and mental illnesses or sleep disorders limited finding statistical significance in some situations. For instance, we did not consider some of the rarer mental illnesses such as bipolar disorder, OCD, or schizophrenia. However, these mental illnesses are often comorbid with stress, anxiety, and depression, which we did consider. That is, of the small percentage of employees with bipolar disorder (0.62%), many also had stress (1.8%), anxiety (21.7%), depression (12.3%), or a combination of these (22.2%). The current study is limited to identifying associations and not causal relationships. The causal direction between male genital problems and mental illnesses and sleep disorders is sometimes two-way. The extent of this bi-directional relationship could not be determined in our data.
Conclusion
These results indicate that the impact of male genital problems extends beyond physical pain or discomfort and can significantly affect mental health and sleep quality. This may be due to feelings of inadequacy or social stigma arising from coping with these conditions.
It is important to note that demographic factors play a considerable role in shaping the associations observed in this study. Factors that affected the relationships between male genital problems, mental illness, and sleep disorders include age, marital status, and dependent children. Associations between BPH and ED with mental illnesses and sleep disorders are also greater in younger men. These findings indicate a need for interventions to consider the influence of age on the effect of BPH and ED on mental illness and sleep disorders.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: This study was performed in line with the principles of the Declaration of Helsinki. The Brigham Young University Institutional Review Board approved the study (IRB2021-157).
Informed Consent: Not applicable.
ORCID iDs: Ray M. Merrill  https://orcid.org/0000-0002-4201-0704
https://orcid.org/0000-0002-4201-0704
McKay K. Ashton  https://orcid.org/0000-0001-6532-4848
https://orcid.org/0000-0001-6532-4848
References
- Alahmar A. T. (2019). Role of oxidative stress in male infertility: An updated review. Journal of Human Reproductive Sciences, 12(1), 4–18. 10.4103/jhrs.JHRS_150_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (5th ed., Text Revision). [Google Scholar]
- Andersen M. L., Tufik S. (2022). The association between sleep disturbances and erectile dysfunction during the COVID-19 pandemic. Sexual Medicine Reviews, 10(2), 263–270. 10.1016/j.sxmr.2021.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aryal M., Pandeya A., Gautam N., Baral N., Lamsal M., Majhi S., Chandra L., Pandit R., Das B. K. L. (2007). Oxidative stress in benign prostate hyperplasia. Nepal Medical College Journal, 9(4), 222–244. [PubMed] [Google Scholar]
- Beaumont. (2023). Penile conditions and diseases. https://www.beaumont.org/conditions/penile-conditions-diseases
- Carr C. P., Martins C. M., Stingel A. M., Lemgruber V. B., Juruena M. F. (2013). The role of early life stress in adult psychiatric disorders: A systematic review according to childhood trauma subtypes. The Journal of Nervous and Mental Disease, 201(12), 1007–1020. 10.1097/NMD.0000000000000049 [DOI] [PubMed] [Google Scholar]
- Charandabi S. M., Rezaei N., Hakimi S., Khatami S., Valizadeh R., Azadi A. (2016). Sleep disturbances and sexual function among men aged 45-75 years in an urban area of Iran. Sleep Science, 9(1), 29–34. 10.1016/j.slsci.2016.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chartier-Kastler E., Leger D., Comet D., Haab F., Ohayon M. M. (2012). Prostatic hyperplasia is highly associated with nocturia and excessive sleepiness: A cross-sectional study. BMJ Open, 2(3), e000505. 10.1136/bmjopen-2011-000505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ching C. B., Hays S. R., Luckett T. R., Clayton D. B., Tanaka S. T., Thomas J. C., Adams M. C., Brock J. W., 3rd, Pope J. C., 4th. (2015). Interdisciplinary pain management is beneficial for refractory orchialgia in children. Journal of Pediatric Urology, 11, 123.e1–123.e6. 10.1016/j.jpurol.2014.12.005 [DOI] [PubMed] [Google Scholar]
- Cho J. W., Duffy J. F. (2019). Sleep, sleep disorders, and sexual dysfunction. The World Journal of Men’s Health, 37(3), 261–275. 10.5534/wjmh.180045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou P. S., Chang W. C., Chou W. P., Liu M. E., Lai C. L., Liu C. K., Ku Y. C., Tsai S. J., Chou Y. H., Chang W. P. (2014). Increased risk of benign prostate hyperplasia in sleep apnea patients: A nationwide population-based study. PLOS ONE, 9(3), e93081. 10.1371/journal.pone.0093081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung S. D., Hung S. H., Lin H. C., Tsai M. C., Kao L. T. (2016). Obstructive sleep apnea and urological comorbidities in males: A population-based study. Sleep and Breathing, 20(4), 1203–1208. 10.1007/s11325-016-1336-x [DOI] [PubMed] [Google Scholar]
- Corretti G. (2007). The relationship between anxiety disorders and sexual dysfunction. Psychiatric Times, 24, 58–59. [Google Scholar]
- Coyne J. C., Rohrbaugh M. J., Shoham V., Sonnega J. S., Nicklas J. M., Cranford J. A. (2001). Prognostic importance of marital quality for survival of congestive heart failure. American Journal of Cardiology, 88(5), 526–529. 10.1016/s0002-9149(01)01731-3 [DOI] [PubMed] [Google Scholar]
- Davé S., Sherr L., Senior R., Nazareth I. (2009). Major paternal depression and child consultation for developmental and behavioural problems. British Journal of General Practice, 59(560), 180–185. 10.3399/bjgp09X407063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Berardis D., Serroni N., Marini S., Rapini G., Carano A., Valchera A., Iasevoli F., Mazza M., Signorelli M., Aguglia E., Perna G., Martinotti G., Varasano P. A., Pressanti G. L., Di Giannantonio M. (2014). Alexithymia, suicidal ideation, and serum lipid levels among drug-naïve outpatients with obsessive-compulsive disorder. Revista Brasileira de Psiquiatria (Sao Paulo, Brazil: 1999), 36(2), 125–130. 10.1590/1516-4446-2013-1189 [DOI] [PubMed] [Google Scholar]
- Gareri P., Castagna A., Francomano D., Cerminara G., De Fazio P. (2014). Erectile dysfunction in the elderly: An old widespread issue with novel treatment perspectives. International Journal of Endocrinology, 2014, 878670. 10.1155/2014/878670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gatenbeck L., Aronsson A., Dahlgren S., Johansson B., Stromberg L. (1987). Stress stimuli-induced histopathological changes in the prostate: An experimental study in the rat. The Prostate, 11, 69–76. [DOI] [PubMed] [Google Scholar]
- Gerbild H., Larsen C. M., Graugaard C., Areskoug Josefsson K. (2018). Physical activity to improve erectile function: A systematic review of intervention studies. Sexual Medicine, 6(2), 75–89. 10.1016/j.esxm.2018.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green H. D., Merriel S. W. D., Oram R. A., Ruth K. S., Tyrrell J., Jones S. E., Thirlwell C., Weedon M. N., Bailey S. E. R. (2022). Applying a genetic risk score for prostate cancer to men with lower urinary tract symptoms in primary care to predict prostate cancer diagnosis: A cohort study in the UK Biobank. British Journal of Cancer, 127(8), 1534–1539. 10.1038/s41416-022-01918-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grundström J., Konttinen H., Berg N., Kiviruusu O. (2021). Associations between relationship status and mental well-being in different life phases from young to middle adulthood. SSM Population Health, 14, 100774. 10.1016/j.ssmph.2021.100774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvard Health Publishing. (2009). Stress and benign prostatic hyperplasia (BPH). https://www.health.harvard.edu/blog/stress-and-benign-prostatic-hyperplasia-bph-20090929192
- Hedon F. (2003). Anxiety and erectile dysfunction: A global approach to ED enhances results and quality of life. International Journal of Impotence Research, 15, S16–S69. 10.1038/sj.ijir.3900994 [DOI] [PubMed] [Google Scholar]
- Hegyi B. E., Kozinszky Z., Badó A., Dombi E., Németh G., Pásztor N. (2019). Anxiety and depression symptoms in infertile men during their first infertility evaluation visit. Journal of Psychosomatic Obstetrics & Gynecology, 40(4), 311–317. 10.1080/0167482X.2018.1515906 [DOI] [PubMed] [Google Scholar]
- International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM). https://www.icd10data.com/ICD10CM/Codes
- Jorm A. F., Korten A. E., Christensen H., Jacomb P. A., Rodgers B., Parslow R. A. (2003). Association of obesity with anxiety, depression and emotional well-being: A community survey. Australian and New Zealand Journal of Public Health, 27(4), 434–440. 10.1111/j.1467-842x.2003.tb00423.x [DOI] [PubMed] [Google Scholar]
- Kalmbach D. A., Anderson J. R., Drake C. L. (2018). The impact of stress on sleep: Pathogenic sleep reactivity as a vulnerability to insomnia and circadian disorders. Journal of Sleep Research, 27(6), e12710. 10.1111/jsr.12710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koh J. S., Ko H. J., Wang S. M., Cho K. J., Kim J. C., Lee S. J., Pae C. U. (2015). The relationship between depression, anxiety, somatization, personality and symptoms of lower urinary tract symptoms suggestive of benign prostatic hyperplasia. Psychiatry Investigation, 12(2), 268–273. 10.4306/pi.2015.12.2.268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kredlow M. A., Capozzoli M. C., Hearon B. A., Calkins A. W., Otto M. W. (2015). The effects of physical activity on sleep: A meta-analytic review. Journal of Behavioral Medicine, 38(3), 427–449. 10.1007/s10865-015-9617-6 [DOI] [PubMed] [Google Scholar]
- Latini D. M., Penson D. F., Colwell H. H., Lubeck D. P., Mehta S. S., Henning J. M., Lue T. F. (2002). Psychological impact of erectile dysfunction: Validation of a new health related quality of life measure for patients with erectile dysfunction. Journal of Urology, 168, 2086–2091. 10.1016/S0022-5347(05)64302-9 [DOI] [PubMed] [Google Scholar]
- Liu Q., Zhang Y., Wang J., Li S., Cheng Y., Guo J., Tang Y., Zeng H., Zhu Z. (2018). Erectile dysfunction and depression: A systematic review and meta-analysis. The Journal of Sexual Medicine, 15(8), 1073–1082. 10.1016/j.jsxm.2018.05.016 [DOI] [PubMed] [Google Scholar]
- Liu Y., Hu X., Xiong M., Li J., Jiang X., Wan Y., Bai S., Zhang X. (2023). Association of BMI with erectile dysfunction: A cross-sectional study of men from an andrology clinic. Frontiers in Endocrinology, 14, 1135024. 10.3389/fendo.2023.1135024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma K., Dong Q. (2023). Association between sleep quality and benign prostate hyperplasia among middle-aged and older men in India. BMC Public Health, 23(1), 1147. 10.1186/s12889-023-15972-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malzberg B. (1936). Marital status in relation to the prevalence of mental disease. Psychiatric Quarterly, 10, 245–261. [Google Scholar]
- Miner B., Kryger M. H. (2017). Sleep in the aging population. Sleep Medicine Clinics, 12(1), 31–38. 10.1016/j.jsmc.2016.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mwamukonda K. B., Kelley J. C., Cho D. S., Smitherman A. (2019). Relationship between chronic testicular pain and mental health diagnoses. Translational Andrology and Urology, 8(Suppl. 1), S38–S44. 10.21037/tau.2019.02.05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of Mental Health. (2023). Mental illness. https://www.nimh.nih.gov/health/statistics/mental-illness
- National Institute of Drug Abuse. (2023, February 24). Do people with mental illness and substance use disorders use tobacco more often? https://nida.nih.gov/publications/research-reports/tobacco-nicotine-e-cigarettes/do-people-mental-illness-substance-use-disorders-use-tobacco-more-often
- Nuñez A., Rhee J. U., Haynes P., Chakravorty S., Patterson F., Killgore W. D. S., Gallagher R. A., Hale L., Branas C., Carrazco N., Alfonso-Miller P., Grandner M. A. (2021). Smoke at night and sleep worse? The associations between cigarette smoking with insomnia severity and sleep duration. Sleep Health, 7(2), 177–182. 10.1016/j.sleh.2020.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pace G., Di Massimo C., De Amicis D., Corbacelli C., Di Renzo L., Vicentini C., Miano L., Tozzi Ciancarelli M. G. (2010). Oxidative stress in benign prostatic hyperplasia and prostate cancer. Urologia Internationalist, 85(3), 328–333. 10.1159/000315064 [DOI] [PubMed] [Google Scholar]
- Pascual M., de Batlle J., Barbé F., Castro-Grattoni A. L., Auguet J. M., Pascual L., Vilà M., Cortijo A., Sánchez-de-la-Torre M. (2018). Erectile dysfunction in obstructive sleep apnea patients: A randomized trial on the effects of Continuous Positive Airway Pressure (CPAP). PLOS ONE, 13(8), e0201930. 10.1371/journal.pone.0201930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasqualotto F. F., Sharma R. K., Nelson D. R., Thomas A. J., Jr., Agarwal A. (2000). Relationship between oxidative stress, semen characteristics, and clinical diagnosis in men undergoing infertility investigation. Fertility and Sterility, 73(3), 459–464. 10.1016/S0015-0282(99)00567-1 [DOI] [PubMed] [Google Scholar]
- Roehrs T. A., Roth T. (2015). Sleep disturbance in substance use disorders. Psychiatric Clinics of North America, 38(4), 793–803. 10.1016/j.psc.2015.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen R., Altwein J., Boyle P., Kirby R. S., Lukacs B., Meuleman E., O’Leary M. P., Puppo P., Robertson C., Giuliano F. (2003). Lower urinary tract symptoms and male sexual dysfunction: The multinational survey of the aging male (MSAM-7). European Urology, 44(6), 637–649. 10.1016/j.eururo.2003.08.015 [DOI] [PubMed] [Google Scholar]
- Schover L. R. (1990). Psychological factors in men with genital pain. Clevland Clinic Journal of Medicine, 57, 697–700. 10.3949/ccjm.57.8.697 [DOI] [PubMed] [Google Scholar]
- Singh S., Singh S. K. (2021). Psychological health and well-being in patients with sexually transmitted infections: A prospective cross-sectional study. Indian Journal of Sexually Transmitted Diseases and AIDS, 42(2), 125–131. 10.4103/ijstd.IJSTD_77_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith J. P., Book S. W. (2008). Anxiety and substance use disorders: A review. Psychiatric Times, 25(10), 19–23. [PMC free article] [PubMed] [Google Scholar]
- Tan H. M., Tong S. F., Ho C. C. (2012). Men’s health: Sexual dysfunction, physical, and psychological health—Is there a link? The Journal of Sexual Medicine, 9(3), 663–671. 10.1111/j.1743-6109.2011.02582.x [DOI] [PubMed] [Google Scholar]
- Tzeng N. S., Yeh H. W., Chung C. H., Chang H. A., Kao Y. C., Chiang W. S., Chien W. C. (2019). Risk of psychiatric morbidity in psychosexual disorders in male patients: A nationwide, cohort study in Taiwan. American Journal of Men’s Health, 13(2), 1557988319842985. 10.1177/1557988319842985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullrich P. M., Lutgendorf S. K., Kreder K. J. (2007). Physiologic reactivity to a laboratory stress task among men with benign prostatic hyperplasia. Urology, 70, 487–491. 10.1016/j.urology.2007.04.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullrich P. M., Lutgendorf S. K., Leserman J., Turesky D. G., Kreder K. J. (2005). Stress, hostility, and disease parameters of benign prostatic hyperplasia. Psychosomatic Medicine, 67, 476–482. 10.1097/01.psy.0000161208.82242.f8 [DOI] [PubMed] [Google Scholar]
- Velurajah R., Brunckhorst O., Waqar M., McMullen I., Ahmed K. (2022). Erectile dysfunction in patients with anxiety disorders: A systematic review. International Journal of Impotent Research, 34(2), 177–186. 10.1038/s41443-020-00405-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldinger M. D. (2015). Psychiatric disorders and sexual dysfunction. Handbook of Clinical Neurology, 130, 469–489. 10.1016/B978-0-444-63247-0.00027-4 [DOI] [PubMed] [Google Scholar]
- Wallner L. P., Clemens J. Q., Sarma A. V. (2009). Prevalence of and risk factors for prostatitis in African American men: The Flint Men’s Health Study. The Prostate, 69(1), 24–32. 10.1002/pros.20846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D. R., Takeuchi D. T., Adair R. K. (1992). Marital status and psychiatric disorders among blacks and whites. Journal of Health and Social Behavior, 33(2), 140–157. [PubMed] [Google Scholar]
- Zhang X. B., Lin Q. C., Zeng H. Q., Jiang X. T., Chen B., Chen X. (2016). Erectile dysfunction and sexual hormone levels in men with obstructive sleep apnea: Efficacy of continuous positive airway pressure. Archives of Sexual Behavior, 45(1), 235–240. 10.1007/s10508-015-0593-2 [DOI] [PubMed] [Google Scholar]




