Abstract
Thirty-one cats showing clinical signs of upper respiratory tract disease with a presumed bacterial component based on clinical signs were administered either amoxycillin or azithromycin to determine which drug protocol was optimal for empirical use. A clinical score was determined and nasal and pharyngeal swabs were collected for bacterial culture, virus isolation and polymerase chain reaction prior to the start of therapy. Cats failing to respond to the initial antibiotic were then administered the other drug. There were no differences in clinical scores between the two groups at the start of therapy. Eleven of 31 cats improved after administration of the first antibiotic, 16 cats were switched to the alternate antibiotic, and four cats were removed from the study for additional supportive treatments. Eight of 27 cats failed to respond to either antibiotic. The χ2 test for outcomes revealed no differences in response to therapy for either antimicrobial.
Upper respiratory tract disease (URTD) characterized by sneezing with or without nasal discharge is extremely common in both traditional shelters (Foley and Bannasch 2004) and no-kill shelters (Pedersen et al 2004). There is on-going debate in animal shelters about the most efficacious and cost effective methods for treating feline URTD. Limited resources rarely allow for determining the definitive causative agent(s); however, the most common organisms detected in recent studies of cats in shelter or cattery environments included feline herpesvirus-1 (FHV-1), feline calicivirus (FCV), Pasteurella species, Chlamydophila felis, Mycoplasma species, Bordetella bronchiseptica, and coagulase-negative Staphylococcus species (Cape 1992, Stein and Lappin 2001, Johnson et al 2005, Helps et al 2005, Bannasch and Foley 2005, Schultz et al 2006, Veir et al in press). While the majority of bacterial infections are thought to be secondary to other primary diseases, most veterinarians believe antimicrobial therapy is indicated for cats exhibiting mucopurulent discharge.
β-lactams, potentiated β-lactams, fluoroquinolones and tetracyclines are often selected as antimicrobial treatment for cats with suspected bacterial URTD. Results of antimicrobial susceptibility testing were recently reported for bacteria grown from the nasal discharges or airways of cats housed in Germany or north-central Colorado (Stein and Lappin 2001, Schultz et al 2006). All of the drug classes previously mentioned killed > 67% of the isolates in vitro. However, the efficacy of these drugs in treating URTD is variable in the field, likely in part because it is difficult to differentiate cats with primary viral cause of disease with secondary bacterial overgrowth from those with primary bacterial pathogens like B bronchiseptica, Mycoplasma species, or C felis.
Amoxycillin is commonly used for the treatment of cats with suspected bacterial URTD because it is inexpensive and has a good spectrum against bacterial flora like Pasteurella species that may overgrow secondary to primary viral infections. In addition, amoxycillin is effective for the treatment of many anaerobic bacterial species; this group of organisms has been suggested to be associated with disease in chronic rhinitis (Johnson et al 2005). However, many B bronchiseptica isolates have been resistant to amoxycillin (Hoskins et al 1998) and because the drug is cell-wall inhibitor, amoxycillin should not be effective for the treatment of Mycoplasma species. Amoxycillin–clavulanate has effect against C felis infections (Sturgess et al 2001) but it is unknown whether amoxycillin is also effective against this organism. Lastly, there is also Gram-negative flora in the respiratory passageways that may overgrow secondary to other primary diseases like FHV-1 and FCV that may also be resistant to amoxycillin (Stein and Lappin 2001).
Azithromycin is a macrolide antibiotic with a broad spectrum against bacteria associated with respiratory tract disease in people (Jordan 2001). In cats, it has bacteriostatic effects against many Gram-positive organisms, Gram-negative organisms, and Mycoplasma species. In one feline study, azithromycin was equivalent to doxycycline for eliminating clinical signs of C felis infection (Owen et al 2003). Because azithromycin has a long tissue half-life in cats, infrequent dosing is adequate to maintain plasma levels which has led to frequent use of the drug in feline practice (Hunter et al 1995, Jordan 2001). This could be of potential benefit in shelter situations where multiple cats may need to be treated at one time and it may be difficult to administer drugs because of the demeanor of the cat. Most of the other drugs used to treat respiratory tract disease in cats need to be administered at least daily. However, there is currently no published information on the efficacy of azithromycin for the empirical treatment of suspected bacterial causes of URTD in cats. Further information is needed to help shelter veterinarians determine the optimal empirical antibiotic choice for cats with URTD with a suspected bacterial component. The purpose of this study was to assess the comparative efficacy of amoxycillin and azithromycin in cats with clinical URTD from a humane society in north-central Colorado.
Materials and methods
Experimental design
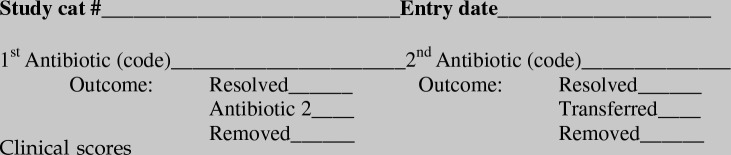
This study was conducted in combination with another larger study that was designed to determine the prevalence rates of infectious causes of URTD cats, to determine optimal sample collection sites (nasal or oropharyngeal), and to compare microbiological culture and nucleic acid amplification techniques for select infectious agents (Veir et al 2008). The studies were completed in a private humane society with an animal control contract that serves a combined rural and urban area in north- central Colorado. The shelter has an open admission policy and the full-time veterinary staff attempts to manage animals entering with treatable diseases or conditions. However, euthanasia is performed if the animals are non-rehabilitable or non-treatable. Cats admitted to the shelter usually receive a parenteral, modified live feline viral rhinotracheitis-calici-panleukopenia vaccine and one dose of pyrantel pamoate (5 mg/kgPO). Cats entered into this part of the study were sampled between 24 January and 4 December 2003 and had been in the shelter for variable lengths of time. Thirty-one cats with clinical signs of URTD with a suspected bacterial component (oculonasal purulent discharge, sneezing, and stertorous breathing) and no obvious facial deformity were identified by the shelter veterinarian (MS). Cats identified for the study had a temperament consistent with single handler management. Within 24 h of admission, each cat was clinically scored (Table 1) and three swabs from both the nasal cavity and oropharynx were collected by a single investigator (RR) prior to treatment. Nasal swabs were obtained by gently rolling a sterile transurethral culture swab (Ca alginate swabs, Ultrafine Al, product #14-959-78, Fischer Scientific) in the anterior aspect of the right nares after removing any excess mucous. Oropharyngeal swabs were obtained using a sterile cotton tipped applicator gently rotated in the oropharynx of each cat. One swab from each sampling site was placed into a commercial transport medium (BBL CultureSwab Plus Amies Medium with Charcoal, Becton, Dickinson and Company; Sparks, MD) and submitted for culture of Mycoplasma species and aerobic bacteria species within 4 h. A second swab was placed in viral transport medium (viral transport media: modified Eagle's medium with 1% HEPES, 4% bovine growth serum, 0.0025% amphotericin B+antibiotics) and submitted for virus isolation within 4 h. The final swab was placed in 1 ml sterile phosphate buffered saline (PBS) solution, allowed to equilibrate for 2–3 h at room temperature according to the DNA/RNA extraction kit (Qiagen, Valencia, CA) manufacturer's instructions and then stored at−70 °C until assayed for the presence of FHV-1 DNA, Chlamydophila species DNA, Mycoplasma species DNA, and calicivirus RNA. Culture, virus isolation, and nucleic acid amplification methods are described elsewhere (Veir et al 2008). Antimicrobial susceptibility testing was performed using the Kirby-Bauer method.
Table 1.
Clinical scoring sheet used to evaluate URTD in shelter cats
After samples were obtained, cats were randomly grouped into those administered amoxycillin (22 mg/kgPO q12 h) or azithromycin (15 mg/kgPO q 72 h) (Zithromax, Pfizer Labs, New York, NY) by the shelter veterinarian. The amoxycillin protocol was that currently used by the shelter and the azithromycin protocol was selected based on extrapolation from previous literature (Hunter et al 1995, Westfall et al 2001, Owen et al 2003). Cats were given a clinical score prior to treatment and then every 3 days by an investigator blinded to the treatment group (RR). Trained shelter personnel administered the medications. Amoxycillin tablets were prescribed for each cat and new dosing syringes were used for each azithromycin liquid dose. Following the primary treatment period of days 0–9; those cats with persistent clinical signs were administered the other antibiotic for an additional 9 days. The shelter veterinarian retained the right to remove cats from the study for any reason. Cats enrolled in the study remained housed individually in the isolation ward of the humane society. The study was completed with the approval of the Humane Society Board of Directors and a campus-wide Animal Care and Use Committee at Colorado State University.
Statistical analyses
Data was entered into Microsoft Excel. Difference between clinical scores for each group prior to treatment and at cross-over was determined by Student's t-test. Difference between clinical outcomes of antimicrobial therapy was determined by the χ2 test for outcome between groups. Significance was defined at P<0.05.
Results
Of 31 cats entered into the study, 30 had descriptive data (age, sex, reproductive status and breed) recorded. Six were intact male, five intact female, 15 altered male and four altered female. Ages ranged from 3.5 months to 6 years (mean 2.5 years, median 2 years). Twenty-three cats were classified as domestic shorthairs, three as domestic longhairs and four as purebred (three Siamese, one Manx). Over half the cats had positive virus isolation from either the nasal or oropharyngeal swab (67.7% or 51.6%, respectively). Each of the cats that were positive on virus isolation was also positive for FHV-1 DNA by polymerase chain reaction (PCR) assay but negative for calicivirus RNA by real-time PCR assay and so we assume that these cats were infected with FHV-1 only (Veir et al 2008). All cats were PCR negative for Chlamydophila felis. Eighteen bacterial species were cultured; Mycoplasma, Pasteurella and Moraxella species were the most common isolates (Table 2). Pasteurella, Moraxella, Streptococcus, Staphylococcus, Simonsiella and Flavobacterium species isolates were determined to be sensitive to ampicillin except for Staphylococcus aureus (resistant) and Streptococcus B (intermediate). Pasteurella and Moraxella species had intermediate sensitivities to erythromycin, the only macrolide antimicrobial tested.
Table 2.
Aerobic organisms isolated from nasal or pharyngeal swabs of cats with URTD with suspected bacterial involvement
| Bacterial isolate | Nasal (%) | Pharyngeal (%) |
|---|---|---|
| Mycoplasma species | 58.1 | 61.3 |
| Pasteurella multocida | 35.5 | 67.7 |
| Moraxella species | 12.9 | 29.0 |
| Staphylococcus species (coagulase-negative) | 12.9 | 16.1 |
| Streptococcus species (non-hemolytic) | 9.7 | 16.1 |
| Simonsiella species | 0.0 | 9.7 |
| Flavobacterium species | 0.0 | 22.6 |
| Pasteurella dogmatis | 0.0 | 9.7 |
| Staphylococcus aureus | 0.0 | 3.2 |
| Staphylococcus intermedius | 3.2 | 0.0 |
| Enterobacter species | 0.0 | 3.2 |
| Clostridium species | 3.2 | 0.0 |
| Escherichia coli | 0.0 | 3.2 |
| Streptococcus (group B) | 22.6 | 19.4 |
| Corynebacterium species | 3.2 | 3.2 |
| Haemophilus species | 0.0 | 3.2 |
| Bacillus species | 3.2 | 0.0 |
| Bordetella bronchiseptica | 3.2 | 0.0 |
Within 24 h of admission, samples were collected from admissions to a combined rural and urban humane society shelter with clinical signs of URTD. Routine aerobic culture was performed on samples within 4 h of collection.
Twenty-one cats were initially administered amoxycillin and 10 were administered azithromycin. Pre-treatment clinical scores (Table 3) ranged from 1 to 11 (mean 5.7, median 5) and did not differ between antibiotic groups (Student's t-test; P=0.33). There were no differences in age (Student's t-test; P=0.08) or sex (χ 2 test; P=0.21) between the two groups. Of the 21 cats initially administered amoxycillin, eight had resolution of clinical signs, 10 were switched to azithromycin, and three were removed from the study. Of the 10 cats initially administered azithromycin, three had resolution of clinical signs, six were switched to amoxycillin and one was removed from the study. The four cats removed from the study had persistent anorexia or severe dehydration requiring intravenous fluid administration. There were no differences in outcome between groups of cats after the primary antibiotic treatment (χ2 test of outcomes between groups; P=0.8). Clinical scores of the 16 cats administered the second antibiotic ranged from 0 to 9 (mean 4.0, median 4) at the time of cross-over and there were no differences in clinical scores between groups (Student's t-test; P=0.16). One of these cats had a resolution of clinical signs on day 9 (clinical score=0), but recrudescence of signs on day 10 (clinical score=3) and was maintained in the study. Clinical signs resolved in five of the 10 cats switched from amoxycillin to azithromycin and three of the six cats switched from azithromycin to amoxycillin. There were no differences in the cross-over outcome between groups (χ2 test of outcomes between groups; P=0.71).
Table 3.
Aerobic bacterial culture, antimicrobial susceptibility testing, FHV-1 PCR results and response to antibiotic administration in 31 shelter cats with suspected bacterial upper respiratory infections
| Cat | FHV-1 PCR | Culture | Amp sensitivity | Azithro sensitivity | Drug 1 | Response | Drug 2 | Response |
|---|---|---|---|---|---|---|---|---|
| 614 | Pos | Mycoplasma species | ND | ND | Amox | Yes | NA | NA |
| P multocida | ||||||||
| Moraxella species | ||||||||
| Staph (coag neg) | ||||||||
| Strep (non-hemolytic) | ||||||||
| 604 | Pos | Mycoplasma species | ND | ND | Amox | Yes | NA | NA |
| P multocida | S | I | ||||||
| Moraxella species | S | S | ||||||
| Staph intermedius | S | S | ||||||
| Enterobacter species | R | R | ||||||
| 514 | Pos | Staph (coag neg) | ND | ND | Amox | Yes | NA | NA |
| Clostridium species | ND | ND | ||||||
| E coli | ND | ND | ||||||
| 782 | Pos | Mycoplasma species | ND | ND | Amox | Yes | NA | NA |
| P multocida | ND | ND | ||||||
| Strep B | ND | ND | ||||||
| 135 | Pos | Mycoplasma species | ND | ND | Amox | Yes | NA | NA |
| P multocida | ND | ND | ||||||
| Flavobacterium species | ND | ND | ||||||
| Strep B | ND | ND | ||||||
| 789 | Pos | Mycoplasma species | ND | ND | Azithro | Yes | NA | NA |
| P multocida | S | I | ||||||
| Flavobacterium species | S | S | ||||||
| Strep B | S | S | ||||||
| 799 | Pos | P dogmatis | S | I | Amox | Yes | NA | NA |
| Strep B | I | S | ||||||
| 000 | Pos | Mycoplasma species | ND | ND | Azithro | Yes | NA | NA |
| P multocida | S | I | ||||||
| Haemophilus species | ND | ND | ||||||
| 036 | Pos | Mycoplasma species | ND | ND | Amox | Yes | NA | NA |
| Flavobacterium species | ND | ND | ||||||
| P dogmatis | S | S | ||||||
| Bacillus species | ND | ND | ||||||
| 638 | Pos | Mycoplasma species | ND | ND | Amox | Yes | NA | NA |
| P multocida | S | S | ||||||
| Moraxella species | ND | ND | ||||||
| Staph (coag neg) | ND | ND | ||||||
| Strep B | ND | ND | ||||||
| Corynebacterium species | ND | ND | ||||||
| B bronchiseptica | ND | ND | ||||||
| 099 | Pos | NG | Azithro | Yes | NA | NA | ||
| 165 | Pos | P multocida | S | I | Amox | No-crossed | Azithro | No |
| Moraxella species | S | I | ||||||
| 890 | Pos | Mycoplasma species | ND | ND | Amox | No-crossed | Azithro | Yes |
| P multocida | S | I | ||||||
| 747 | Pos | Mycoplasma species | ND | ND | Azithro | No-crossed | Amox | Yes |
| P multocida | S | I | ||||||
| 409 | Pos | P multocida | S | I | Azithro | No-crossed | Amox | Yes |
| Moraxella species | ND | ND | ||||||
| Flavobacterium species | ND | ND | ||||||
| 416 | Pos | P multocida | S | I | Amox | No-crossed | Azithro | No |
| Moraxella species | S | S | ||||||
| Strep (non-hemolytic) | ND | ND | ||||||
| Simonsiella species | S | S | ||||||
| P dogmatis | S | I | ||||||
| 722 | Pos | Mycoplasma species | ND | ND | Amox | No-crossed | Azithro | Yes |
| Staph aureus | R | S | ||||||
| 504 | Pos | Mycoplasma species | ND | ND | Amox | No-crossed | Azithro | No |
| P multocida | S | I | ||||||
| Staph (coag neg) | ND | ND | ||||||
| Strep B | S | S | ||||||
| 937 | Neg | Mycoplasma species | ND | ND | Amox | No-crossed | Azithro | Yes |
| P multocida | S | I | ||||||
| Moraxella species | S | S | ||||||
| 774 | Pos | Mycoplasma species | ND | ND | Amox | No-crossed | Azithro | Yes |
| P multocida | S | I | ||||||
| Staph (coag neg) | ND | ND | ||||||
| Corynebacterium species | ND | ND | ||||||
| 104 | Pos | Mycoplasma species | ND | ND | Azithro | No-crossed | Amox | No |
| P multocida | S | I | ||||||
| Strep B | S | S | ||||||
| 004 | Neg | Mycoplasma species | ND | ND | Azithro | No-crossed | Amox | Yes |
| P multocida | S | S | ||||||
| Strep (non-hemolytic) | ND | ND | ||||||
| Flavobacterium species | S | I | ||||||
| Haemophilus species | S | S | ||||||
| 467 | Pos | P multocida | S | S | Amox | No-crossed | Azithro | No |
| Strep (non-hemolytic) | ND | ND | ||||||
| Flavobacterium species | S | I | ||||||
| 041 | Pos | Mycoplasma species | ND | ND | Amox | No-crossed | Azithro | Yes |
| P multocida | S | I | ||||||
| 628 | Pos | Mycoplasma species | ND | ND | Amox | No-crossed | Azithro | No |
| P multocida | S | S | ||||||
| Strep B | S | S | ||||||
| 359 | Pos | NG | Azithro | No-crossed | Amox | No | ||
| 058 | Pos | NG | Azithro | No-crossed | Amox | No | ||
| 635 | Pos | Mycoplasma species | ND | ND | Amox | No-removed | NA | NA |
| P multocida | ||||||||
| Moraxella species | ||||||||
| Staph (coag neg) | ||||||||
| Strep (non-hemolytic) | ||||||||
| 166 | Pos | Mycoplasma species | ND | ND | Amox | No-removed | NA | NA |
| P multocida | S | I | ||||||
| Moraxella species | S | S | ||||||
| Simonsiella species | ND | ND | ||||||
| 860 | Pos | Mycoplasma species | ND | ND | Amox | No-removed | NA | NA |
| P multocida | S | I | ||||||
| Moraxella species | S | S | ||||||
| Simonsiella species | ND | ND | ||||||
| 071 | Pos | P multocida | ND | ND | Azithro | No-removed | NA | NA |
| Flavobacterium species | ND | ND |
Cats were randomly placed on amoxycillin 22 mg/kgPO bid or azithromycin 15 mg/kgPO q 72 h. Cats that failed to respond to treatment were then placed on the other antibiotic. Culture and sensitivity results are pre-treatment results. Pos=positive; Neg=negative; NA=not applicable; amp=ampicillin; amox=amoxycillin; azithro=azithromycin; ND=not determined; S=susceptible; I=intermediate; R=resistant.
Aerobic bacteria or Mycoplasma species were grown from 24 of the 31 cats that completed the drug trial (Table 3). All 11 cats that resolved during the first antibiotic treatment period were documented with FHV-1 infection. Based on pre-treatment susceptibility results and assuming azithromycin has anti-Mycoplasma species activity and amoxycillin does not, six of the eight amoxycillin-only treated cats and one of the three azithromycin-only treated cats would have been predicted to fail treatment because of the presence of bacteria resistant to the first antibiotic used. Of the 16 cats that required the cross-over, 14 were concurrently infected by FHV-1. After cross-over to the second antibiotic, clinical signs resolved in eight of 16 cats of which only two (cat 409 and cat 722) would have been predicted to resolve based on the bacteria isolated. Of the eight cats still clinically ill after both antibiotic treatment periods, two had no bacteria cultured and the other six would have been predicted to respond to the combination of the drugs. All of these cats had known FHV-1 infections and were transferred to an anti-viral treatment study (Veir et al 2006).
Discussion
With the exception of FCV and C felis, each of the known or suspected primary pathogens thought to be associated with URTD in cats were detected in this study; Pasteurella and Mycoplasma species were the most commonly isolated bacteria. The results of the study document the difficulty in using bacterial culture and susceptibility from nasal samples or the pharynx to predict antibiotic responses. This likely relates to the fact that these areas are home to a rich normal flora and so not all bacteria that are cultured are causing clinical disease. The results suggest that culture and sensitivity of nasal discharges or pharyngeal swabs is a low yield procedure when assessing cats with acute disease URTD.
One of the primary limitations of this study is that it is currently impossible to prove bacterial or viral causation of clinical signs. The URTD syndrome in cats is multi-factorial and most of the organisms isolated here can be detected in both healthy and clinically ill cats. The eight cats in this study that failed both antibiotics were likely to have primary FHV-1 infection or other undiagnosed nasal diseases, including undiagnosed, antimicrobial drug resistant bacteria. The data from these cats also suggest that the presence of mucopurulent discharge does not definitely prove that a bacterial component to the disease process exists. Overall, FHV-1 infection was documented in 17 of 19 cats that ultimately had their clinical signs resolve, eight of eight cats with persistent disease, and four of four cats removed from the study.
In the 31 shelter cats described here, there were no outcome differences detected between groups of cats treated with amoxycillin or azithromycin. Thus, there was no clear advantage to selecting one drug over the other as the initial empirical therapy. This finding may merely reflect the fact that the cats did not have a bacterial component to their URTD or the number of cats included in the study was too few to detect a difference. Clinical signs of bacterial or FHV-1 associated disease often wane over time. Thus, even the cats in this study with clinical resolution while on antibiotics may have been spontaneously resolving. Twenty-one of 31 cats cultured were positive for Mycoplasma species; 75% (6/8) of cats positive for Mycoplasma species had clinical resolution of disease when treated with amoxycillin alone. Two of three cats that were administered azithromycin alone were positive for Pasteurella and Mycoplasma species. One cat did culture positive for Bordetella bronchiseptica but clinical signs resolved with amoxycillin alone.
Although azithromycin is readily bio-available in cats and has a long tissue half-life (Hunter et al 1995), dose recommendations vary and are not well defined. Plumb's Veterinary Drug Handbook (5th edition, 2005) lists three dosages for cats including 5–10 mg/kgPO daily for 3–5 days for susceptible infections. Azithromycin was unsuccessful at eliminating Chlamydophila felis at 10–15 mg/kg daily for 3 days, then twice weekly (Owen et al 2003) and Haemobartonella felis at 15 mg/kg twice daily for 7 days (Westfall et al 2001). Cats in these studies reportedly tolerated the drug well. An increased dose interval is the primary benefit of using azithromycin in animal shelters and 15 mg/kg every 3 days was selected based on extrapolation from the previous studies. A greater response may have been detected if a daily loading dose had been used.
Carry-over effects can bias cross-over study data. Including a long wash out between cross- over can alleviate this bias. However, the fact that there were no differences between the treatment groups and 8/31 (25.8%) cats were clinically ill at the end of both antimicrobial trials suggests carry-over was not a factor. Cats were not randomly enrolled in the study but selected for convenience. Cats likely to be easily managed by a single person were preferentially selected by the shelter veterinarian. It is unlikely that these cats had different clinical signs or pathogens than other cats entering the shelter as total clinical scores ranged widely as did pathogens identified.
Shelters will continue to look for ways to decrease the morbidity and mortality related to URTD. This study showed in a limited number of cats, azithromycin and amoxycillin have a similar efficacy. Amoxycillin is relatively inexpensive (US$2.44 for the 9-day treatment for an average size cat) with rare side effects (none in this study). However, the twice daily protocol selected may be a hardship for shelter personnel, leading to treatment failure and increasing the risk of disease transmission through multiple handlings of sick cats. Azithromycin is comparatively expensive (US$6.60 for the 9-day treatment for an average size cat) but has the advantage of longer dosing intervals. No adverse reactions were recorded with azithromycin treatment in this study. Given the stress and crowding inherent in most sheltering situations, upper respiratory infections will continue to effect animals in that environment. Veterinarians will need to select antimicrobial treatments based on each shelter's need following the AVMA judicious antimicrobial use guidelines including implementation of biosecurity and sanitation protocols, as well as managed housing and vaccination. While empirical antimicrobial therapy may not always be warranted in a shelter environment, azithromycin may be a valid choice. Further investigation into the efficacy of azithromycin in shelter situations is warranted before recommending the drug for routine use.
References
- Bannasch M.J., Foley J.E. Epidemiologic evaluation of multiple respiratory pathogens in cats in animal shelters, Journal of Feline Medicine and Surgery 7, 2005, 109–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cape L. Feline idiopathic chronic rhinosinusitis: a retrospective study of 30 cases, Journal of the American Animal Hospital Association 28, 1992, 149–155. [Google Scholar]
- Foley J., Bannasch M.J. Infectious diseases of dogs and cats. Miller L.S., Zawitowski S. Shelter Medicine for Veterinarians and Staff, 2004, Blackwell Publishing: Ames, 235–284. [Google Scholar]
- Helps C.R., Lait P., Damhuis A., Bjornehammar U., Bolta D., Brovida C., Chabanne L., Egberink H., Ferrand G., Fontbonne A., Pennisi M.G., Gruffydd-Jones T., Gunn-Moore D., Hartmann K., Lutz H., Malandain E., Mostl K., Stengel C., Harbour D.A., Graat E.A. Factors associated with upper respiratory tract disease caused by feline herpesvirus, feline calicivirus, Chlamydophila felis and Bordetella bronchiseptica in cats: experience from 218 European catteries, Veterinary Record 156, 2005, 669–673. [DOI] [PubMed] [Google Scholar]
- Hoskins J.D., Williams J., Roy A.F., Peters J.C., McDonough P. Isolation and characterization of Bordetella bronchiseptica from cats in southern Louisiana, Veterinary Immunology and Immunopathology 65, 1998, 173–176. [DOI] [PubMed] [Google Scholar]
- Hunter R.P., Lynch M.J., Ericson J.F., Millas W.J., Fletcher A.M., Ryan N.I., Olson J.A. Pharmacokinetics, oral bioavailability and tissue distribution of azithromycin in cats, Journal of Veterinary Pharmacology and Therapeutics 18, 1995, 38–46. [DOI] [PubMed] [Google Scholar]
- Johnson L.R., Foley J.E., De Cock H.E.V., Clarke H.E., Maggs D.J. Assessment of infectious organisms associated with chronic rhinosinusitis in cats, Journal of the American Veterinary Medical Association 227 (4), 2005, 579–585. [DOI] [PubMed] [Google Scholar]
- Jordan D.G. Azithromycin, Compendium on Continuing Education for the Practicing Veterinarian 23, 2001, 242–269. [Google Scholar]
- Owen W.M.A., Sturgess C.P., Harbour D.A., Egan K., Gruffydd-Jones T.J. Efficacy of azithromycin for the treatment of feline chlamydophilosis, Journal of Feline Medicine and Surgery 5, 2003, 305–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen N.C., Sato R., Foley J.E., Poland A.M. Common virus infections in cats, before and after being placed in shelters, with emphasis on feline enteric coronavirus, Journal of Feline Medicine and Surgery 6, 2004, 83–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schultz B.S., Wolf G., Hartmann K. Bacteriological and antibiotic sensitivity test results in 271 cats with respiratory tract infections, Veterinary Record 158, 2006, 269–270. [DOI] [PubMed] [Google Scholar]
- Stein J.E., Lappin M.R. Bacterial culture results in cats with upper and lower airway disease: 255 cases (1995–1999), American College of Veterinary Internal Medicine Annual Forum, May 2001, (abstract), 885
- Sturgess C.P., Gruffydd-Jones T.J., Harbour D.A., Jones R.L. Controlled study of the efficacy of clavulanic acid-potentiated amoxycillin in the treatment of Chlamydia psittaci in cats, Veterinary Record 149, 2001, 73–76. [DOI] [PubMed] [Google Scholar]
- Veir J.K., Lappin M.R., Dow S.W. Evaluation of a novel immunotherapy for treatment of chronic rhinitis in cats, Journal of Feline Medicine and Surgery 8, 2006, 400–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veir J.K., Ruch-Gallie R., Spindel M.E., Lappin M.R. Prevalence of selected infectious organisms in shelter cats with upper respiratory tract disease, Journal of Feline Medicine and Surgery 10, 2008, 551–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westfall D.S., Jensen W.A., Reagan W.J., Radecki S.V., Lappin M.R. Inoculation of two genotypes of Haemobartonella felis (California and Ohio variants) to induce infection in cats and the response with azithromycin, American Journal of Veterinary Research 62, 2001, 687–691. [DOI] [PubMed] [Google Scholar]