Abstract
This case report describes the skin condition ceruminous gland hyperplasia of the ears of a cat. The diagnosis was made through histopathology. Treatment consisted of carbon dioxide laser ablation of the cystic structures and postoperative care associated with the surgery, as well as a hydrolyzed protein diet, weekly ear cleaning and intermittent topical corticosteroid drops in the ears to minimize the reoccurrence of the cysts.
Case Report
An approximately 5-year-old neutered male 4.5 kg domestic shorthair cat presented for evaluation of large multiple masses in both ears (Figures 1 and 2). The cat was acquired from the humane society (as an owner surrender) 1 week prior to presentation. Other than the masses in the ears, the cat was healthy and tested negative for feline leukemia virus and feline immunodeficiency virus. On physical examination, multiple sized, dark, purple, cystic-appearing masses were present on the external pinnae and opening of the vertical ear canal of both ears (Figure 1). The masses obscured the visual inspection of the remainder of the vertical and horizontal ear canals. An otic cytology showed 4+ bacteria, both rod- and cocci-shaped bacteria and 3+ yeast, consistent with malazzesia. Blood work, including a complete blood count (CBC) and chemistry panel, was performed by an outside laboratory. The blood work was unremarkable except for mild dehydration as indicated by the elevated total plasma protein of 8.3 g/dl (6.0–8.0 g/dl). The globulins were slightly increased 4.7 g/dl (2.3– 3.8 g/dl) most likely owing to antigenic stimulation from the chronic otitis externa.
Figure 1.

Pinna of feline patient upon presentation. Note the multiple dark, blue-purple, cystic masses obstructing the ear canal
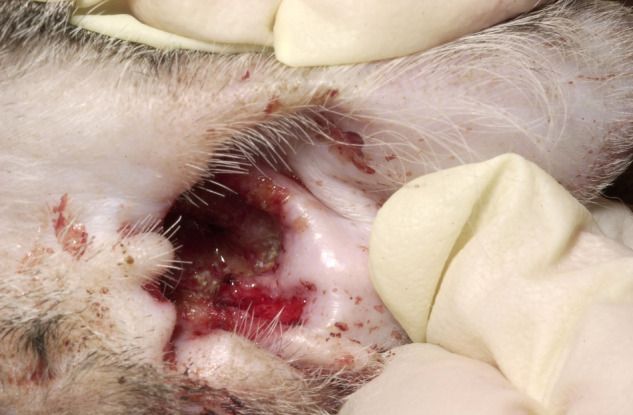
Figure 2.

Pinna immediately following CO2 laser surgery ablation of the ceruminous gland hyperplasia
The cat was premedicated with 0.05 mg/kg (0.11 mg/lb) of acepromazine and 0.1 mg/kg (0.22 mg/lb) of hydromorphone intramuscularly (IM). An intravenous (IV) catheter was placed and Lactated Ringer’s solution at 10 ml/kg/h (22 ml/lb/h) was administered. Anesthesia was induced by giving 5 mg/kg (11 mg/lb) of propofol IV slowly to effect. Anesthesia was maintained with isoflurane via an endotrachael tube. The carbon dioxide (CO2) laser (laser setting of 6 watts of continuous wave super-pulse with a 0.3 mm straight metal tip) was used to surgically remove one of the large masses from both ears for submission for histopathology. The CO2 laser was then used to ablate the remaining masses in the external ear canal using 6–8 watts of continuous wave power with a 0.8 mm ceramic tip. Once the opening to the vertical ear canal was cleared, visual inspection of the remaining vertical and horizontal canal was permitted using a video otoscope. Otoscopic examination revealed the proximal aspect of the ear canals to be clear of any mass structures or debris. The surgical area was wiped clean of any char created by the CO2 laser using saline soaked 4 × 4 gauze pads (Figure 2). Upon completion of the procedure, the cat was given 0.2 mg/kg (0.44 mg/lb) of meloxicam subcutaneously (SC) and 2 drops of flucinolone acetonide 0.01% and dimethyl sulfoxide 60% (Synotic; Fort Dodge Animal Health) were placed in each ear to help with inflammation. The cat was discharged with amoxicillin with clavulonic acid (Clavamox; Pfizer) liquid at 15 mg/kg (33 mg/lb) orally q12h for 10 days. The cat also received meloxicam (Metacam; Boehinger Ingelheim) at 0.1 mg/kg (0.2 mg/lb ) orally q24h for the next 5 days. Topically, the ears were to be cleansed with Squalane 25% in an isopropyl myristate-liquid-petroleum base (Cerumene; Vétoquinol USA) ear cleanser twice-weekly. Mupirocin 2% ointment (Perrigo) 22 g compounded with 30 ml of propylene glycol was to be applied to the lasered region twice daily after administration of 1 drop of flucinolone acetonide 0.01% and dimethyl sulfoxide 60% in each ear. The cat was sent home with an e-collar to minimize/prevent self-trauma to the ears. The diet of this patient was also changed to a hydrolyzed protein diet of Hill’s Prescription diet z/d.
The histopathology of the masses in both ears was consistent with ceruminous gland cystic hyperplasia. The biopsy sample contained stratified squamous epithelium lined with multiple cysts lined by single cuboidal-to-squamous epithelium, filled with variable amounts of eosinophilic inspissated material or with clear liquid, sometimes containing cholesterol clefts and mineralized material.
The cat was re-evaluated 1 week post surgery. Upon re-evaluation, the ears were very pruritic and contained a large amount of dried blood and crusting with ulcerations present under the crusting (Figure 3). The evaluation at 1 week is consistent with the healing by second intention. The flucinolone acetonide 0.01% and dimethyl sulfoxide 60% was discontinued at this time as the potent steroid in it may have hindered the healing process. All other medications were continued as previously prescribed. The cat was then re-evaluated 17 days post surgery and the pinnae were erythematous, both at the surgery site and the surrounding skin around both ears. The surgical site appeared to be healing well by second intention; however, the pruritus was still present and addressed by administration of 0.5 mg (0.11 mg/kg; 0.24 mg/lb) of triamcinalone SC. The patient was re-evaluated 24 days after the surgery. The ears were less erythematous, the cat was less pruritic and the procedure site was almost 100% healed. A second injection of triamcinalone 1 mg (0.22 mg/kg) SC was given. Ear cytology showed occasional yeast. The squalane 25% in an isopropyl myristate-liquid-petroleum base ear cleanser and mupirocin ointment 2% were discontinued and natural enzymes (lysozyme, lactoferrin and lactoperoxidase) with 1% hydrocortisone (Zymox Otic HC; PKB Animal Health) was used instead of these medications at 5 drops in both ears every other day. Re-evaluation of the patient 36 days post surgery showed the CO2 laser sites to be healed and waxy debris was present within the ear (Figure 4). According to the owner, the cat still had mild auricular pruritus. Ear cytology showed only waxy material and no yeast or bacteria present. The natural enzymes lysozyme, lactoferrin and lactoperoxidase with 1% hydrocortisone was decreased to 2 drops in each ear every other day and the flucinolone acetonide 0.01% and dimethyl sulfoxide 60% was started again at 1 drop once-weekly to help with the auricular pruritus. Any debris in the ears was to be cleaned weekly with squalane 25% in an isopropyl myristate-liquid-petroleum base ear cleanser. The patient was then re-evaluated about 2 months after being on the hydrolyzed food trial (Hill’s z/d) for 8 weeks. The auricular pruritis had improved but was not 100% resolved and the ears had only a mild amount of waxy debris with normal ear cytology. The recommendation was to remain on the hydrolyzed diet to prevent reoccurrence of the lesions and weekly ear-cleaning with squalane 25% in an isopropyl myristate-liquid-petroleum base ear cleanser to minimize the reoccurrence of the cysts. A topical corticosteroid [flucinolone acetonide 0.01% and dimethyl sulfoxide 60% or natural enzymes (lysozyme, lactoferrin and lactoperoxidase) with 1% hydrocortisone] was to be used as required for the auricular pruritus. In the 2.5 years of follow-up available, the cat’s auricular pruritus never completely resolved and it had a few more episodes of otitis that were treated and followed up until resolution. One of these episodes occurred when the owner ran out of the hydrolyzed protein diet and fed the cat a diet bought at the grocery store. The masses that were lasered in the external ear canal never returned.
Figure 3.
Pinna 7 days following CO2 laser surgery ablation of the ceruminous gland hyperplasia
Figure 4.

Pinna 36 days following CO2 laser surgery ablation of the ceruminous gland hyperplasia
Ceruminous gland hyperplasia/adenoma also known as ceruminous cystomatosis or apocrine cystadenomatosis is a benign neoplastic disorder of uncertain etiology.1–3 It may be a sequela to otitis externa, a senile degenerative change or, in some cases, a congenital condition.1,4 The most common neoplasm of the ear canal is ceruminal gland in origin.2,3,5,6 These neoplasms are more common in the cat than in the dog.5–7 One report noted that tumors of the ceruminous glands accounted for 40.7% of the histopathology of external ear masses evaluated in cats and are most often benign. 6 The category ‘ceruminous cyst/hyperplasia’ accounted for 1.7% of all feline skin tumors in another large survey.2,8
The ear masses in this case were classic of ceruminous hyperplasia in appearance: multiple, often numerous, punctuated nodules or vesicles, usually less than 2 mm in diameter, in the external ear canal and inner pinna. 1 They are dark blue, brown or black, 1 and are usually confined to the external ear canal and rarely extend beyond the vertical canal. 9 Benign ceruminous gland neoplasia tends to present with signs of obstructive otitis externa as in this case: pruritus, head shaking, malodor, otorrhea and occasionally hemorrhage. 10 Malignant ceruminous gland tumors tend to be ulcerative and infiltrating rather than obstructive/occlusive. 10
Ceruminous glands are located in the deeper dermis of the external ear canal.7,10 They are believed to be modified apocrine sweat glands that secrete waxy cerumen instead of watery sweat. In the normal dog and cat, the ducts of the ceruminous glands are virtually non-visable. 10
Ceruminous otitis is either the initiating cause for the ceruminous gland hyperplasia or is a sequelae caused by the obstructive nature of these masses in the external ear canal. Squalane 25% in an isopropyl myristate-liquid-petroleum base ear cleanser was chosen because if the ear can be treated topically with an oil, it is hopeful that this would decrease production by the ceruminous glands, thus minimizing the start of the hyperplasia process from constant production of material. There are several other products that could have been used instead of the natural enzymes lysozyme, lactoferrin and lactoperoxidase with 1% hydrocortisone for the mild yeast otitis and auricular pruritus. As hydrocortisone is a less potent steroid to help control pruritus, this product did not help the auricular pruritus as much as the flucinolone acetonide 0.01% and dimethyl sulfoxide 60%. However, there was no return of bacteria and the yeast was absent on the following ear cytology indicating that the natural enzymes may have helped with this.
Surgery is indicated to remove the multiple occlusive nodules. More aggressive surgical options include a lateral ear canal resection, total ablation of the ear canal or surgical removal of the affected pinnae. Tumors of the pinnae are often difficult to remove with conventional scalpel surgical excision without causing some disfiguration of the pinnae and sutures are usually required to control bleeding.4,9 CO2 laser vaporization is an effective therapy that is the least traumatic but most effective therapy. 9 Lasers have been used in veterinary medicine for many years. 9 The CO2 laser has little-to-no collateral tissue damage when the laser is used properly, making it an excellent choice for laser surgery. Laser ablation is the best mode of therapy because of the ability to fine tune the laser ablation by variation of the spot size, the power setting and the duration of exposure. 9 The laser surgeon is also able to limit removal to just the lesion, thereby avoiding damage to adjacent normal structures. Laser ablation results in much less scar formation and thus little-to-no deformity of the pinnae. 9 The CO2 laser is also well known for its excellent hemostasis and can effectively seal blood vessels less than 0.5 mm in size. 9 With the CO2 laser, hemostasis allows tumor removal without the need for sutures. Overall, the surgical procedure and healing process in this case progressed as expected. Perhaps if the flucinolone acetonide 0.01% and dimethyl sulfoxide 60% had only been used immediately post-operatively in the hospital to minimize post-surgical inflammation of the ear and not dispensed with the owner to use, healing may have been faster. The addition of buprenorphine at a dose of 0.01 mg/kg sublingually may have been a good addition to the meloxicam to provide better analgesia to the cat postoperatively. The use of the CO2 laser minimized any deformities to the pinnae allowing the ears to look normal. In my experience, the CO2 laser is definitely the treatment of choice for ceruminous gland hyperplasia masses of the ear pinnae.Food allergy most likely played a role in this cat’s pruritic ceruminous otitis and, thus, ceruminous gland hyperplasia as the owner accidently performed a food challenge and the auricular pruritus and otitis worsened/returned. As the pruritus still persisted somewhat after resolution of the otitis while on an appropriate hydrolyzed protein diet, it is possible that this cat might also have an underlying inhalant allergy/atopy issue. One could have pursued this with blood sampling for allergen testing. The addition of an antihistamine or essential omega 3 and 6 fatty acids might also have helped this cat’s auricular pruritus.Treatment for ceruminous otitis consists of identifying and correcting the underlying cause if possible, resolving any secondary bacterial and yeast otitis, and instituting weekly ear cleanings. 11 Mupirocin 2% is a well-established antibacterial agent to help treat the bacterial otitis. However, it has also been shown to have antifungal activity and so was used to treat the initial bacterial and yeast otitis.12,13 As the entire underlying cause could not be corrected, the judicious use of topical otic preparations containing a steroid and/or an astringent every 1–7 days is often helpful in controlling cerumen accumulation. 11 This clinical report illustrates that CO2 laser vaporization is the least traumatic, but very effective, therapy for ceruminous gland hyperplasia and with the treatment of underlying causes reoccurrence can be minimized.
Funding
The author received no specific grant from any funding agency in the public, commercial or not-for-profit sectors for the preparation of this case report.
Conflict of interest
The author does not have any potential conflicts of interest to declare.
References
- 1. Gross TL, Ihrke P, Walder E, Affolter V. Skin diseases of the dog and cat – clinical and histopathologic diagnosis. 2nd ed. Oxford: Blackwell Science, 2005, pp 667–668. [Google Scholar]
- 2. London C, Dubilzeig R, Vail D, et al. Evaluation of dogs and cats with tumors of the ear canal: 145 cases (1978–1992). J Am Vet Med Assoc 1996; 208: 1413–1418. [PubMed] [Google Scholar]
- 3. Legendre AM, Krahwinkel DJ, Jr. Feline ear tumors. J Am Anim Hosp Assoc 1981; 17: 1035–1037. [Google Scholar]
- 4. Cox C. Surgical management of inflammatory and neoplastic conditions affecting the cat’s ear. Vet Annu 1990; 30: 309–314. [Google Scholar]
- 5. Scott DW, Miller WH, Griffin CE. Small animal dermatology. 6th ed. Oxford: WB Saunders, 2001. [Google Scholar]
- 6. De Lorenzi D, Bonfanti U, Masserdotti C, Tranquillo M. Fine-needle biopsy of external ear canal masses in the cat: cytological results and histologic correlations in 27 cases. Vet Clin Pathol 2005; 34: 100–105. [DOI] [PubMed] [Google Scholar]
- 7. Moisan P, Watson G. Ceruminous gland tumors in dogs and cats: A review of 124 cases. J Am Anim Hosp Assoc 1996; 32: 448–452. [DOI] [PubMed] [Google Scholar]
- 8. Goldschmidt MH, Shofer FS. Skin tumors of the dog and cat. Oxford: Pergamon Press, 1992, pp 2, 85–89. [Google Scholar]
- 9. Duclos D. Lasers in veterinary dermatology. Vet Clin North Am Small Anim Pract 2006; 36: 15–17, 27–29. [DOI] [PubMed] [Google Scholar]
- 10. Harvey R, Harari R, Delauche A. Ear diseases of the dog and cat. Ames, Iowa State University Press, 2001, pp 23, 84,, 106. [Google Scholar]
- 11. Medleau L, Hnilica KA. Small animal dermatology: a color atlas and therapeutic guide. Oxford: WB Saunders, 2001, pp 280. [Google Scholar]
- 12. Nicholas RO, Berry V, Hunter P, Kelly J. The antifungal activity of mupirocin. J Antimicrob Chemother 1999; 43: 579–582. [DOI] [PubMed] [Google Scholar]
- 13. de Wet P, Rode H, van Dyke A, Millar A. Perianal candidosis – a comparative study with mupirocin and nystatin. Int J Dermatol 1999; 38: 618–622. [DOI] [PubMed] [Google Scholar]


