Abstract
Surgical intervention is the treatment of choice for recurrent lateral patellar instability.
Surgery should be considered for first time lateral patella dislocations with osteochondral fractures or underlying anatomical risk factors.
Primary repair and nonanatomical imbrications/reconstructions have fallen out of favor due to abnormal biomechanics and high rates of recurrence. Anatomical reconstruction of the MPFL using a variety of auto and allograft tissues have yielded good outcomes and low redislocation rates.
Physeal sparing MPFL reconstruction techniques under radiological control are safe and do not cause growth disturbance. Allografts may be indicated for hyperlax patients.
Although no clear cutoff points exist, correction of valgus and excessive femoral anteversion should be considered when indicated.
Osteochondral and chondral injuries are common and should be addressed during surgery for instability.
Keywords: patellar instability, medial patellofemoral ligament reconstruction, patellar dislocation, femoral anteversion
Patellar instability is an important cause of knee disability in children and adolescents. A recent population-based study found an annual incidence rate of 2.58 per 100 000 individuals for lateral patella dislocations (LPD), with higher rates in females and patients aged <19. Two thirds of the injuries were related to sports (1). Higher annual rates up to 125 per 100 000 individuals have been found in smaller studies (2).
Risk factors for patellar instability including patella alta, generalized hyperlaxity (e.g. Ehlers–Danlos syndrome), trochlear dysplasia, dysplasia of vastus medialis obliquus (VMO), increased Q angle, genu valgum, increased femoral anteversion and tibial torsion have been adequately discussed in a previous review in this journal (3).
Initial evaulation
The workup of a patient with acute patellar instability starts with a physical exam focusing on patellar tracking, presence of J sign, joint hyperlaxity, coronal extremity alignment and rotational profile of the extremity. Anteroposterior, lateral knee x-rays and Laurin views of the patella are reviewed for the presence of patellar subluxation, osteochondral fracture, trochlear dysplasia and patellar height. A magnetic resonance imaging (MRI) scan is mandatory to assess the location and extent of MPFL injury, osteochondral damage to the patella and/or lateral femoral condyle and to measure tibial tuberosity–trochlear groove (TT-TG) distance. Long leg radiographs are used to analyze coronal extremity alignment if genu valgum is observed in the clinical exam. Assessment of the rotational profile of the extremity with a CT scan is performed only if warranted by the clinical exam. Increased internal rotation of the femoral condyles in MRIs where the knees are fixed with the patellae facing upward during the scans may be a sign of excessive femoral anteversion and is an indication for CT evaluation for the authors. The decision for conservative vs surgical treatment is made after a complete evaluation of morphology and injury. Several studies have analyzed the risk factors for recurrence after the first episode of patellar dislocation. Balcarek et al. have described a ‘Patellar Instability Severity Score’ where age, bilaterality, trochlear dysplasia, patellar tilt and height and TT-TG distance are assessed. A score greater than 4 out of a maximum score of 7 implies a higher risk for recurrence and surgery is advised (4). Jaquith & Parikh have identified trochlear dysplasia, history of contra-lateral dislocation, skeletal immaturity Caton-Deschamps index 1.45+ as the main risk factors in a population of 222 patients (5). The recurrence risk increases from 14% in a first-time dislocator with none of the above risk factors to 88% in a patient with all four factors. It seems that the combination of underlying risk factors is more important than a single anatomical abnormality and the decision to operate should be tailored for each patient. Table 1 outlines the authors’ thresholds for surgical vs conservative treatment.
Table 1.
The authors’ indications for conservative vs surgical treatment. The presence of two or more risk factors strongly favors surgery.
| Consider surgery | Consider conservative treatment |
|---|---|
| Large osteochondral fragment/loose body | Small flakes on the medial patellar border |
| Patella subluxed in transverse imaging, patellar tilt >20˚ | Patella centralized in transverse imaging, patellar tilt <20˚ |
| Dejour type B, C and D trochlear dysplasia | Dejour type A trochlea |
| Presence of J-sign and preexisting symptoms of instability | No previous symptom of instability |
| Genu valgum >10˚ | Neutral or constitutional varus alignment |
| Femoral anteversion >30˚ | Femoral anteversion <20˚ |
| Syndromic joint hyperlaxity (Ehlers–Danlos, etc.) Beighton score >6 | Beighton score <6 |
| Patella alta (Caton index 1.3+) | Caton index 0.8–1.2 |
| TT-TG distance >16 mm | TT-TG distance <16 mm |
| Contralateral patellar instability | Unilateral instability |
Conservative treatment
Traditionally conservative treatment was considered to be the standard of care in the treatment of first time LPD unless an osteochondral fracture or loose body was present. Surgery was advised for patients with recurrent instability. However, the outcomes of conservative treatment were not as good as expected. A 3-year follow-up of 111 patients treated conservatively found that although 73% did not have another episode of instability, many still reported limitations in their activities and only 26% were able to return to sport (6). The risk of recurrent instability is higher in skeletally immature patients compared to adults.
A meta-analysis of 11 randomized controlled trials and 5 cohort studies including 918 patients comparing conservative vs operative treatment found lower recurrence rates and better Kujala scores in the operative group (7). However, the difference in pain scores and episodes of subluxation was not significant.
It seems that conservative treatment may be indicated in a small subset of patients without underlying anatomical risk factors or osteochondral fractures. If nonoperative treatment is chosen, a brief period of rest and immobilization is followed by early knee range-of-motion exercises and quadriceps reeducation. A patellar brace may be helpful. Casting for extended periods of time should be avoided.
The risk of recurrent dislocation increases with length of follow-up in skeletally immature patients. Sanders et al. found that the cumulative incidence rate for recurrence was 11% at 1 year, 21.1% at 2 years, 37% at 5 years, 45.1% at 10 years, 54% at 15 years and 54% at 20 years (8). Therefore, it is not clear how long these patients should be followed up after the initial dislocation. As the majority of the recurrences occur in the first 5 years, this period of observation seems reasonable.
Operative treatment
There is an increasing trend toward surgical treatment of first-time LPD in patients with underlying risk factors (9). Patients with recurrent instability should be treated operatively to prevent progressive cartilage damage and improve quality of life.
Surgical treatment should be tailored to the patient, with reconstruction of the injured medial restraints and treatment of osteochondral fractures while avoiding injury to the growth plates. Lateral release or lengthening should be reserved for permanent dislocations with severe tightness of the retinaculum and should be avoided in hyperlax patients. Correction of excessive femoral anteversion and pathological genu valgum can be performed in the same setting if needed. Comparative studies have shown the superiority of medial patellofemoral ligament (MPFL) reconstruction to traditional lateral release and medial imbrication procedures (10). Nonanatomical techniques of plication or primary repair of medial structures do not restore normal biomechanics and may increase patellofemoral joint reaction forces (11); these have fallen out of favor and have generally been replaced by more anatomical MPFL reconstructions.
MPFL anatomy in skeletally immature patients
MPFL is the main static stabilizer of the patella and provides up to 60% of the restraint to lateral translation at 0–30˚ of knee flexion. Recent anatomical studies have identified other structures such as the medial quadriceps tendon femoral ligament (MQTFL) that contributes to the stability near extension. Although MPFL reconstruction remains the mainstay of treatment of children with patellar instability, combined techniques that also reconstruct the MQFL have also been described (12). The medial patellotibial ligament (MPTL) and medial patellomeniscal ligament (MPML) are the distal stabilizers of the patella and have a role in preventing lateral patellar translation in flexion (13).
MPFL injury has been identified in over 90% of the patients following acute patellar dislocation (12, 13). The location of MPFL injury is at the patellar insertion site in over 80% of the children and multifocal in the rest (14, 15).
The relationship of the femoral insertion of MPFL and the distal femoral physis has been extensively studied. A systematic review of seven studies has shown that the femoral insertion is 3.7 to 10 mm distal to the physis, with a mean distance of 6.9 mm in 93% of the cases (16). The relationship of age and insertion site is controversial, with some studies finding distal and others demonstrating proximal migration with age (16). If femoral sockets are to be used in MPFL reconstruction, the starting point should be on the center of MPFL insertion and angled distally and anteriorly to avoid physeal damage and violation of the intercondylar notch (Fig. 1). The tunnel length should be limited to 20 mm (17, 18). No growth disturbance has been reported with fluoroscopically placed femoral sockets avoiding the physis (19). The patellar insertion of the MPFL has been found to be slightly distal compared to adults in smaller children, extending and sometimes passing distally to the center of the patellar length (20).
Figure 1.
Femoral tunnel drilling under image intensifier control during physeal sparing MPFL reconstruction.
MPFL repair
The role of repair of MPFL in the treatment of first-time LPD is controversial. A randomized study involving 74 immature patients found a lower redislocation rate compared to brace treatment in patients undergoing acute repair (21). No difference between subjective and objective outcomes could be demonstrated between operative repair and brace treatment. However, the rate of redislocation was 22% in the repair group which is almost four times higher compared to most studies with MPFL reconstruction. Given that primary repair attempts to suture an already injured and attenuated ligament and does not correct underlying anatomical risk factors, the higher rates of failure are expected.
MPFL reconstruction
MPFL reconstruction in skeletally immature patients is a safe operation, with no reported growth disturbance unless a technical error occurs. A meta-analysis of seven studies including 132 children and adolescents found no growth disturbance but reported 3.8% redislocation and 11.4% subluxation events, which is higher than adults (22). Graft choice and femoral fixation method had no effect on outcome or complications in this systematic review (22). Immature patients also have a higher rate of subsequent injury to the knee after MPFL reconstruction (23).
The outcomes of MPFL reconstruction in children and adolescents are favorable. A systematic review of 15 studies comprising 517 procedures found improved Kujala scores and return to sport at 6.1 months. The redislocation rate was 5% and 4% of the patients required further surgery (24).
MPFL reconstruction with free tendon grafts
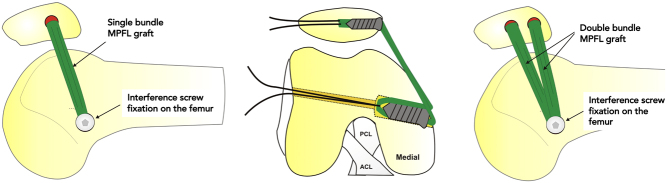
Hamstrings are the most commonly used grafts for MPFL reconstruction. The doubled gracilis tendon is adequate for most patients and the semitendinosus can be preserved. Femoral fixation is made in a single socket at the anatomical insertion distal to the physis. Technical details described in the previous section are important to avoid injury to the distal femoral physis, medial collateral and cruciate ligaments. A variety of patellar fixation methods using single or double sockets, and anchors in a groove on the medial patella have been described (Fig. 2). Nelitz et al. (25) have shown no recurrence and good Kujala scores after anatomic MPFL reconstruction using a gracilis tendon graft, regardless of the presence of patella alta or increased TT-TG distance. Double tunnels in the patella better mimic the anatomy of the MPFL and have slightly lower recurrence rates; however, they are associated with increased risk of patellar fracture (26).
Figure 2.
Schematic illustration of single- and double-bundle MPFL reconstructions.
MPFL reconstruction is a very powerful tool but over tensioning the graft may lead to increased patellofemoral contact pressure, loss of knee motion and in severe cases medial subluxation of the patella. The reduction of the patella in the trochlea should be verified arthroscopically and a lateral mobility of one-fourth patellar width in extension should be preserved when tensioning the graft.
MPFL reconstruction with pedicled quadriceps tendon grafts
A pedicled quadriceps tendon graft with the patellar insertion intact has also been used for MPFL reconstruction. This technique is advantageous in children with small patella and avoids the problems of patellar tunnels and consequent risk of articular penetration or fracture. The graft can either be fixed in a femoral socket anatomically, or may be sutured to the adductor magnus tendon in a quasi-anatomical fashion. Nelitz et al. (27) have reported on the 2.6-year follow-up of 25 children undergoing anatomical MPFL reconstruction with a pedicled quadriceps tendon graft. They found no recurrence, and 80% of the patients were satisfied with the procedure. Return to sports was possible for most of the patients at 5 months. A systematic review of nine studies in children and young adults undergoing MPFL reconstruction using pedicled quadriceps tendon grafts also found favorable outcomes with no redislocations/reoperations and 3% residual positive apprehension test (28).
Adductor sling fixation with free grafts
Adductor magnus based MPFL reconstructions aim to avoid drilling tunnels near the distal femoral physis. A free tendon graft is looped around the adductor magnus and fixed to the patella in tunnels or in a boney groove on the medial side. However, high rates of redislocation and revision (20% and 21%, respectively) have been reported with this technique, probably due to the nonanatomical placement of the graft and reliance on soft tissue fixation (29).
A modification of this technique with the distal end of the hamstring tendon left on intact on the tibia and looping the proximal end around the adductor magnus and securing it to the medial patella has also been reported to have slightly higher (13%) redislocation rates (30).
Adductor magnus tendon MPFL reconstruction
A distal pedicled adductor magnus tendon can also be used in skeletally immature patients to avoid a bony femoral fixation near the physis (31). A partial or total strip of adductor magnus tendon is harvested, leaving the distal insertion of the tendon intact. Care must be taken not to injure the superficial femoral artery during harvest. The pedicled tendon graft is passed under the vastus medialis and fixed to the medial margin of the patella using an osseous or a soft tissue technique.
Malecki et al. reported on 26 patients treated with this technique (32). The authors found favorable clinical outcomes that were maintained throughout the observation period over 10 years without inducing degenerative changes.
Allograft reconstructions
Allograft tissues have been proposed as an alternative to autografts for MPFL reconstruction, especially for patients with pathological hyperlaxity (Beighton score >6) and syndromic patellar instability (33). Hohn and Pandya reported similar outcomes (8% recurrence and 16% complications) with the use of allografts compared to autografts in their series of 25 children and adolescents undergoing MPFL reconstruction at 2-year follow-up (34). Another series of 24 knees undergoing MPFL reconstruction using gracilis allografts reported 12.5% recurrent instability without growth disturbance (35). In the largest study performed up to date, Reddy reported the outcomes of 76 allograft MPFL reconstructions in hyperlax children with a mean Beighton score of 7 (36). The mean Kujala score was 89 and the recurrence rate was found to be 9% at 3 years. The advantages of absence of donor site morbidity and loss of flexor strength of allografts should be balanced against the increased cost, poor incorporation and the risk of disease transmission and infection. The authors recommend the use of allografts in cases with generalized hyperlaxity due to pathologic collagen synthesis (e.g. Ehlers–Danlos syndrome).
Derotation osteotomies
Rotational abnormalities of the lower extremity such as excessive femoral anteversion and tibial external rotation have been implicated as risk factors for patellar instability and failure of operative treatment. CT scans provide the most objective measurements of these deformities. Different methods to measure femoral anteversion and tibial rotation produce variable results and the surgeon should familiarize himself or herself with the differences between the techniques and use a standard technique for measurement (37). Most of the studies on transverse plane correction have been performed in young adults with closed physes.
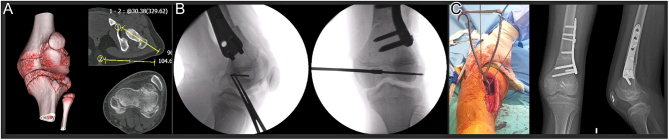
Derotation osteotomy combined with MPFL reconstruction has been shown to have better clinical outcomes and less residual J-sign compared to isolated MPFL reconstructions (Fig. 3). Twenty-five degrees has been proposed as a cutoff point in skeletally mature patients (38). Failed MPFL reconstructions in patients with increased anteversion also benefit from revision MPFL reconstruction combined with DFO (39). A recent systematic review of six studies reported DFO was indicated for 20˚–30˚ anteversion in skeletally mature patients with patellar instability; however, femoral anteversion >30˚ is generally considered to be a cutoff point for DFO (40). Mild anteversion around 20˚ does not seem to adversely affect the outcomes of MPFL reconstruction (41).
Figure 3.
Combined distal femoral derotation osteotomy and MPFL reconstruction in a patient with bilateral patellar instability. (A) Preoperative CT scan demonstrating subluxed patella and femoral anteversion of 30˚ in a 13-year-old girl. (B) Drilling of the MPFL femoral tunnel, MPFL graft was placed in a groove on the medial border of the patella and suture anchors were used for fixation. (C) K-wires depict the amount of correction achieved intraoperatively, x-rays show healing of the osteotomy at 6 weeks.
Correction of tibial external rotation has been reported less frequently. External tibial torsion >35˚ is considered to be an indication for tibial osteotomy, and can be performed in the proximal or distal tibia. A fibular osteotomy is usually needed and prophylactic peroneal nerve decompression has been advised for the correction of severe deformities (42).
Correction of valgus
Genu valgum is an important factor for patellar instability due to increased Q angle and the lateral vector of the quadriceps mechanism. Genu valgum >10°, mechanical axis in or outside the lateral knee compartment, and a mechanical lateral distal femoral angle (mLDFA) <84° in a skeletally immature patient have been recommended for correction of valgus deformity (43). Growth modulation techniques are minimally invasive and can be used in children with at least 1 year of remaining growth; however, the best outcomes are achieved in girls <12 and boys <14 years of age. Kearney et al. (44) have treated 26 valgus knees associated with patellar instability with hemiepiphysiodesis and reported resolution of symptoms of pain and instability in 69% of the patients with correction of aLDFA to normal. The authors did not perform any procedure to realign the extensor mechanism in this series, the cutoff point for surgery was <79˚ or smaller for aLDFA. Tan et al. (45) performed isolated medial hemiepiphysiodesis to treat patellar instability 20 patients with valgus knees. Sixteen patients had no further instability at the final follow-up, but the authors concluded that this procedure was effective in less deformed knees. Parikh et al. (46) reported the use of a transphyseal screw placed from the lateral cortex to achieve medial hemiepiphysiodesis combined with gracilis autograft reconstruction of MPFL using patellar and femoral tunnels in eight patients. All but one patient with Down syndrome achieved satisfactory outcomes. Guided growth correction of valgus also provides a significant correction of the TT-TG distance (47), which is beneficial in patients with open growth plates where tibial tuberosity osteotomies are contraindicated. The eight plates used for guided growth impede with MPFL reconstructions and require a certain amount of time to achieve the desired correction; therefore, they may not always be an option in patients with painful recurrent patellar instability. In this case, distal femoral osteotomy proximal to the physis may be indicated. Distal femoral osteotomies may also be utilized in teenagers after skeletal maturity (48) but should probably be combined with MPFL reconstructions.
In summary, the authors recommend correction of genu valgum in children with open physes with guided growth. A distal femoral osteotomy should be considered in skeletally mature adolescents for genu valgum exceeding 5°.
Osteochondral fractures and cartilage injuries
Osteochondral fractures may occur in the medial facet/central ridge of the patella and the lateral femoral condyle at the time of dislocation (49). The prevalence of these osteochondral lesions has been reported to be between 17 and 30% for the lateral femoral condyle (50) and up to 76% for the patella (51).
Isolated treatment of osteochondral fractures without addressing the instability results in high rates of recurrence and the need for secondary surgery (up to 61% in one series) and should be avoided (52). Current thinking is that both the fracture and instability should be treated in the same surgical episode with modern reconstruction techniques (53).
Osteochondral injury is associated with the development of arthritis, with rates up to 48% at 25 years (54) follow-up, and should be addressed at the time of MPFL surgery.
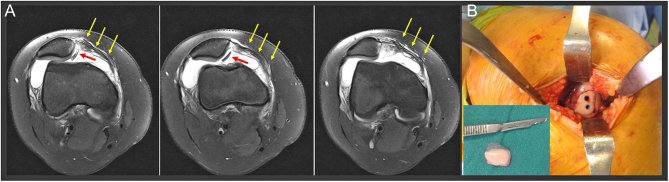
Small impression fractures on the lateral edge of the condyle can be debrided, while larger lesions extending to the weight-bearing area need to be fixed or managed with cartilage restoration techniques (Fig. 4). A variety of fixation methods including metal and bioabsorbable screws, arrows, pins, sutures and fibrin glue can be used. No superiority of one technique over the others has been demonstrated. Metal screws provide superior compression but carry the risk of chondral damage if the fragment subsides and may necessitate secondary removal. Biodegradable implants provide inferior compression and fixation strength and may cause cystic/allergic reactions during resorption. Although over 90% healing rates have been reported (55), secondary surgery for trimming of protuberant nails or chondral debridement may still be needed. The fixation of pure chondral fragments is controversial, but given the younger age and greater healing potential of these patients, it may be attempted in acute lesions. A recent multicenter study found 56% complete healing in MRI scans after fixation of these pure chondral fragments with bioabsorbable screws in adolescents (56).
Figure 4.
(A) Loose osteochondral fragment originating from the lateral femoral condyle (red arrows) following LPD. Injury to the MPFL can be seen (yellow arrows). (B) Fixation of the fragment with two headless screws.
Patellar lesions usually involve the median ridge and the medial facet. These lesions need to be fixed if adequate bone stock is present, and a conflict with the MPFL reconstruction sockets should be avoided. The same applies for patients undergoing mosaicplasty; fixation of the MPFL graft should be modified if a conflict with the mosaicplasty sockets emerges.
Conclusion
The paradigm of conservative treatment for first-time LPD has changed in recent years for patients with underlying anatomical risk factors. MPFL reconstruction using physeal sparing techniques is safe and results in low recurrence rates. Coronal and transverse plane deformities should be corrected. Cartilage repair/restoration should be an integral part of the surgical treatment.
ICMJE Conflict of Interest Statement
RT declares receiving honoraria from Menarini Pharma and consultancy fees from Stryker and Smith & Nephew. ML declares receiving honoraria from DepuySynthes, Medacta, Athrex and Stryker. AK declares receiving honoraria for lectures from Menarini Pharma and consultancy fees from Stryker. The other authors have nothing to disclose.
Funding Statement
This review did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
Author contribution statement
ES performed the literature search and contributed to the writing of the paper; RT designed the structure and flow of the article, wrote the manuscript, provided and edited the images and reviewed the final version; GD, ML and AK contributed to the writing of the paper and critically reviewed the manuscript. All authors read and approved the final version of the manuscript.
References
- 1.Lyons JG Hudson TL & Krishnamurthy AB. Epidemiology of patellar dislocations in the United States from 2001 to 2020: results of a national emergency department database. Physician and Sportsmedicine 20221–10. ( 10.1080/00913847.2022.2156765) [DOI] [PubMed] [Google Scholar]
- 2.Isacsson A Olsson O Englund M & Frobell RB. Incidence and concomitant chondral injuries in a consecutive cohort of primary traumatic patellar dislocations examined with sub-acute MRI. International Orthopaedics 202347973–981. ( 10.1007/s00264-023-05707-y) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hasler CC & Studer D. Patella instability in children and adolescents. EFORT Open Reviews 20161160–166. ( 10.1302/2058-5241.1.000018) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Balcarek P Oberthür S Hopfensitz S Frosch S Walde TA Wachowski MM Schüttrumpf JP & Stürmer KM. Which patellae are likely to redislocate? Knee Surgery, Sports Traumatology, Arthroscopy 2014222308–2314. ( 10.1007/s00167-013-2650-5) [DOI] [PubMed] [Google Scholar]
- 5.Jaquith BP & Parikh SN. Predictors of recurrent patellar instability in children and adolescents after first-time dislocation. Journal of Pediatric Orthopedics 201737484–490. ( 10.1097/BPO.0000000000000674) [DOI] [PubMed] [Google Scholar]
- 6.Magnussen RA Verlage M Stock E Zurek L Flanigan DC Tompkins M Agel J & Arendt EA. Primary patellar dislocations without surgical stabilization or recurrence: how well are these patients really doing? Knee Surgery, Sports Traumatology, Arthroscopy 2017252352–2356. ( 10.1007/s00167-015-3716-3) [DOI] [PubMed] [Google Scholar]
- 7.Yang F Guo W Wang Q Zhu Z Guan C Zhao S & Yuan B. Surgical versus nonsurgical treatment of primary acute patellar dislocation: a systematic review and meta-analysis. Medicine 201998e16338. ( 10.1097/MD.0000000000016338) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sanders TL Pareek A Hewett TE Stuart MJ Dahm DL & Krych AJ. High rate of recurrent patellar dislocation in skeletally immature patients: a long-term population-based study. Knee Surgery, Sports Traumatology, Arthroscopy 2018261037–1043. ( 10.1007/s00167-017-4505-y) [DOI] [PubMed] [Google Scholar]
- 9.McFarlane KH Coene RP Feldman L Miller PE Heyworth BE Kramer DE Kocher MS Yen YM & Milewski MD. Increased incidence of acute patellar dislocations and patellar instability surgical procedures across the United States in paediatric and adolescent patients. Journal of Children’s Orthopaedics 202115149–156. ( 10.1302/1863-2548.15.200225) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Herdea A Pencea V Lungu CN Charkaoui A & Ulici A. A prospective cohort study on quality of life among the pediatric population after surgery for recurrent patellar dislocation. Children 20218830. ( 10.3390/children8100830) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Edmonds EW & Glaser DA. Adolescent patella instability extensor mechanics: insall extensor realignment versus medial patellofemoral ligament reconstruction. Journal of Pediatric Orthopedics 201636262–267. ( 10.1097/BPO.0000000000000430) [DOI] [PubMed] [Google Scholar]
- 12.Spang RC Tepolt FA Paschos NK Redler LH Davis EA & Kocher MS. Combined reconstruction of the medial patellofemoral ligament (MPFL) and medial quadriceps tendon-femoral ligament (MQTFL) for patellar instability in children and adolescents: surgical technique and outcomes. Journal of Pediatric Orthopedics 201939e54–e61. ( 10.1097/BPO.0000000000001259) [DOI] [PubMed] [Google Scholar]
- 13.Chahla J Smigielski R LaPrade RF & Fulkerson JP. An updated overview of the anatomy and function of the proximal medial patellar restraints (medial patellofemoral ligament and the medial quadriceps tendon femoral ligament). Sports Medicine and Arthroscopy Review 201927136–142. ( 10.1097/JSA.0000000000000252) [DOI] [PubMed] [Google Scholar]
- 14.Anazor FC & Evangelou K. Patterns of associated knee ligament and chondral injuries in first-time traumatic patellar dislocation: a retrospective magnetic resonance imaging (MRI) -Based study. Cureus 202214e31850. ( 10.7759/cureus.31850) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Askenberger M Arendt EA Ekström W Voss U Finnbogason T & Janarv PM. Medi al patellofemoral ligament injuries in children with first-time lateral patellar dislocations: a magnetic resonance imaging and arthroscopic study. American Journal of Sports Medicine 201644152–158. ( 10.1177/0363546515611661) [DOI] [PubMed] [Google Scholar]
- 16.Sochacki KR Shea KG Varshneya K Safran MR Abrams GD Donahue J & Sherman SL. Relationship of the medial patellofemoral ligament origin on the distal femur to the distal femoral physis: a systematic review. American Journal of Sports Medicine 202149261–266. ( 10.1177/0363546520904685) [DOI] [PubMed] [Google Scholar]
- 17.Greenrod W Cox J Astori I Baulch J & Williams J. A magnetic resonance imaging study of the significance of the distal femoral physis during medial patellofemoral ligament reconstruction. Orthopaedic Journal of Sports Medicine 201312325967113502638. ( 10.1177/2325967113502638) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Irarrázaval S Besa P Fernández F Fernández T Tuca M Lira MJ & Orrego M. Anterior and distal tunnel orientation for anatomic reconstruction of the medial patellofemoral ligament is safer in patients with open growth plates. Knee Surgery, Sports Traumatology, Arthroscopy 2021291822–1829. ( 10.1007/s00167-020-06229-5) [DOI] [PubMed] [Google Scholar]
- 19.Uppstrom TJ Price M Black S Gausden E Haskel J & Green DW. Medial patellofemoral ligament (MPFL) reconstruction technique using an epiphyseal femoral socket with fluoroscopic guidance helps avoid physeal injury in skeletally immature patients. Knee Surgery, Sports Traumatology, Arthroscopy 2019273536–3542. ( 10.1007/s00167-019-05412-7) [DOI] [PubMed] [Google Scholar]
- 20.Shea KG Polousky JD Jacobs JC Ganley TJ Aoki SK Grimm NL & Parikh SN. The patellar insertion of the medial patellofemoral ligament in children: a cadaveric study. Journal of Pediatric Orthopedics 201535e31–e35. ( 10.1097/BPO.0000000000000399) [DOI] [PubMed] [Google Scholar]
- 21.Askenberger M Bengtsson Moström E Ekström W Arendt EA Hellsten A Mikkelsen C & Janarv PM. Operative repair of medial patellofemoral ligament injury versus knee brace in children with an acute first-time traumatic patellar dislocation: a randomized controlled trial. American Journal of Sports Medicine 2018462328–2340. ( 10.1177/0363546518770616) [DOI] [PubMed] [Google Scholar]
- 22.Shamrock AG Day MA Duchman KR Glass N & Westermann RW. Medial patellofemoral ligament reconstruction in skeletally immature patients: a systematic review and meta-analysis. Orthopaedic Journal of Sports Medicine 201972325967119855023. ( 10.1177/2325967119855023) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Quinlan NJ Tomasevich KM Mortensen AJ Hobson TE Adeyemi T Metz AK & Aoki SK. Medial patellofemoral ligament reconstruction in the pediatric population: skeletal immaturity does not affect functional outcomes but demonstrates increased rate of subsequent knee injury. Arthroscopy, Sports Medicine, and Rehabilitation 20224e1589–e1599. ( 10.1016/j.asmr.2022.05.007) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Migliorini F Maffulli N Bell A & Betsch M. Outcomes, return to sport, and failures of MPFL reconstruction using autografts in children and adolescents with recurrent patellofemoral instability: a systematic review. Children 202291892. ( 10.3390/children9121892) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nelitz M Dreyhaupt J Reichel H Woelfle J & Lippacher S. Anatomic reconstruction of the medial patellofemoral ligament in children and adolescents with open growth plates: surgical technique and clinical outcome. American Journal of Sports Medicine 20134158–63. ( 10.1177/0363546512463683) [DOI] [PubMed] [Google Scholar]
- 26.Parikh SN Nathan ST Wall EJ & Eismann EA. Complications of medial patellofemoral ligament reconstruction in young patients. American Journal of Sports Medicine 2013411030–1038. ( 10.1177/0363546513482085) [DOI] [PubMed] [Google Scholar]
- 27.Nelitz M Dreyhaupt J & Williams SRM. Anatomic reconstruction of the medial patellofemoral ligament in children and adolescents using a pedicled quadriceps tendon graft shows favourable results at a minimum of 2-year follow-up. Knee Surgery, Sports Traumatology, Arthroscopy 2018261210–1215. ( 10.1007/s00167-017-4597-4) [DOI] [PubMed] [Google Scholar]
- 28.Migliorini F Trivellas A Eschweiler J Betsch M Tingart M & Maffulli N. Pedicled strip of quadriceps tendon graft for primary medial patellofemoral ligament reconstruction in recurrent patellofemoral instability: a systematic review. Arthroscopy 2021371992–1999. ( 10.1016/j.arthro.2021.01.048) [DOI] [PubMed] [Google Scholar]
- 29.Lind M Enderlein D Nielsen T Christiansen SE & Faunø P. Clinical outcome after reconstruction of the medial patellofemoral ligament in paediatric patients with recurrent patella instability. Knee Surgery, Sports Traumatology, Arthroscopy 201624666–671. ( 10.1007/s00167-014-3439-x) [DOI] [PubMed] [Google Scholar]
- 30.Alm L Krause M Mull C Frosch KH & Akoto R. Modified adductor sling technique: a surgical therapy for patellar instability in skeletally immature patients. Knee 2017241282–1288. ( 10.1016/j.knee.2017.08.051) [DOI] [PubMed] [Google Scholar]
- 31.Sillanpää PJ Mäenpää HM Mattila VM Visuri T & Pihlajamäki H. A mini-invasive adductor magnus tendon transfer technique for medial patellofemoral ligament reconstruction: a technical note. Knee Surgery, Sports Traumatology, Arthroscopy 200917508–512. ( 10.1007/s00167-008-0713-9) [DOI] [PubMed] [Google Scholar]
- 32.Małecki K Niedzielski K Korczyc-Stępnicka A Stelmach W Beczkowski J Fabiś J & Fabiś-Strobin A. A clinical, radiological and isokinetic evaluation in patients with recurrent patellar dislocation undergoing MPFL reconstruction according to Avikainen: a prospective study evaluating early degenerative changes after a minimum 10-year follow-up period. BMC Musculoskeletal Disorders 202324147. ( 10.1186/s12891-023-06249-5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Popkin CA Bayomy AF Trupia EP Chan CM & Redler LH. Patellar instability in the skeletally immature. Current Reviews in Musculoskeletal Medicine 201811172–181. ( 10.1007/s12178-018-9472-5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hohn E & Pandya NK. Does the utilization of allograft tissue in medial patellofemoral ligament reconstruction in pediatric and adolescent patients restore patellar stability? Clinical Orthopaedics and Related Research 20174751563–1569. ( 10.1007/s11999-016-5060-4) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Allahabadi S & Pandya NK. Allograft medial patellofemoral ligament reconstruction in adolescent patients results in a low recurrence rate of patellar dislocation or subluxation at midterm follow-up. Arthroscopy 202238128–138. ( 10.1016/j.arthro.2021.05.005) [DOI] [PubMed] [Google Scholar]
- 36.Reddy G Hayer PS UlIslam S Mehta NJ Iqbal HJ Stables G & Barton-Hanson NG. Outcomes of allograft medial patellofemoral ligament reconstruction in children and adolescents with hypermobility. International Journal of Applied and Basic Medical Research 202212161–166. ( 10.4103/ijabmr.ijabmr_25_22) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Palmer RC Podeszwa DA Wilson PL & Ellis HB. Coronal and transverse malalignment in pediatric patellofemoral instability. Journal of Clinical Medicine 2021103035. ( 10.3390/jcm10143035) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hao K Niu Y Kong L & Wang F. Medial patellofemoral ligament reconstruction combined with derotational distal femoral osteotomy yields better outcomes than isolated procedures in patellar dislocation with increased femoral anteversion. Knee Surgery, Sports Traumatology, Arthroscopy 2023312888–2896. ( 10.1007/s00167-022-07264-0) [DOI] [PubMed] [Google Scholar]
- 39.Cao Y Zhang Z Shen J Song G Ni Q Li Y Zheng T & Zhang H. Derotational distal femoral osteotomy yields satisfactory clinical outcomes in pathological femoral rotation with failed medial patellofemoral ligament reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy 2022301809–1817. ( 10.1007/s00167-021-06739-w) [DOI] [PubMed] [Google Scholar]
- 40.Zhang Z Cao Y Song G Li Y Zheng T & Zhang H. Derotational femoral osteotomy for treating recurrent patellar dislocation in the presence of increased femoral anteversion: a systematic review. Orthopaedic Journal of Sports Medicine 2021923259671211057126. ( 10.1177/23259671211057126) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Blanke F Watermann K Haenle M Feitenhansl A Camathias C & Vogt S. Isolated medial patellofemoral ligament reconstruction can be an effective procedure in patellofemoral instability with risk factors. Journal of Knee Surgery 202033992–997. ( 10.1055/s-0039-1688917) [DOI] [PubMed] [Google Scholar]
- 42.Palmer RC Podeszwa DA Wilson PL & Ellis HB. Coronal and transverse malalignment in pediatric patellofemoral instability. Journal of Clinical Medicine 2021103035. ( 10.3390/jcm10143035) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shah A & Parikh SN. Medial patellofemoral ligament reconstruction with growth modulation in children with patellar instability and genu valgum. Arthroscopy Techniques 20209e565–e574. ( 10.1016/j.eats.2019.12.008) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kearney SP & Mosca VS. Selective hemiepiphyseodesis for patellar instability with associated genu valgum. Journal of Orthopaedics 20151217–22. ( 10.1016/j.jor.2015.01.005) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tan SHS Tan LYH Lim AKS & Hui JH. Hemiepiphysiodesis is a potentially effective surgical management for skeletally immature patients with patellofemoral instability associated with isolated genu valgum. Knee Surgery, Sports Traumatology, Arthroscopy 201927845–849. ( 10.1007/s00167-018-5127-8) [DOI] [PubMed] [Google Scholar]
- 46.Parikh SN Redman C & Gopinathan NR. Simultaneous treatment for patellar instability and genu valgum in skeletally immature patients: a preliminary study. Journal of Pediatric Orthopedics 201928132–138. ( 10.1097/BPB.0000000000000546) [DOI] [PubMed] [Google Scholar]
- 47.Ceroni D Dhouib A Merlini L & Kampouroglou G. Modification of the alignment between the tibial tubercle and the trochlear groove induced by temporary hemiepiphysiodesis for lower extremity angular deformities: a trigonometric analysis. Journal of Pediatric Orthopedics 201726204–210. ( 10.1097/BPB.0000000000000409) [DOI] [PubMed] [Google Scholar]
- 48.Wilson PL Black SR Ellis HB & Podeszwa DA. Distal femoral valgus and recurrent traumatic patellar instability: is an isolated Varus producing distal femoral osteotomy a treatment option? Journal of Pediatric Orthopedics 201838e162–e167. ( 10.1097/BPO.0000000000001128) [DOI] [PubMed] [Google Scholar]
- 49.Uimonen M Ponkilainen V Paloneva J Mattila VM Nurmi H & Repo JP. Characteristics of osteochondral fractures caused by patellar dislocation. Orthopaedic Journal of Sports Medicine 202192325967120974649. ( 10.1177/2325967120974649) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zheng L Shi H Feng Y Sun BS Ding HY & Zhang GY. Injury patterns of medial patellofemoral ligament and correlation analysis with articular cartilage lesions of the lateral femoral condyle after acute lateral patellar dislocation in children and adolescents: an MRI evaluation. Injury 2015461137–1144. ( 10.1016/j.injury.2015.02.001) [DOI] [PubMed] [Google Scholar]
- 51.Seeley MA Knesek M & Vanderhave KL. Osteochondral injury after acute patellar dislocation in children and adolescents. Journal of Pediatric Orthopedics 201333511–518. ( 10.1097/BPO.0b013e318288b7a0) [DOI] [PubMed] [Google Scholar]
- 52.Pedowitz JM Edmonds EW Chambers HG Dennis MM Bastrom T & Pennock AT. Recurrence of patellar instability in adolescents undergoing surgery for osteochondral defects without concomitant ligament reconstruction. American Journal of Sports Medicine 20194766–70. ( 10.1177/0363546518808486) [DOI] [PubMed] [Google Scholar]
- 53.Repo JP Uimonen MM Nevalainen MT Nurmi H Ponkilainen VT Tuominen A & Paloneva J. Outcomes following the operative treatment of intra-articular fracture combined with medial patellofemoral ligament reconstruction after patellar dislocation. Knee Surgery and Related Research 20223421. ( 10.1186/s43019-022-00150-6) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sanders TL Pareek A Johnson NR Stuart MJ Dahm DL & Krych AJ. Patellofemoral arthritis after lateral patellar dislocation: a matched population-based analysis. American Journal of Sports Medicine 2017451012–1017. ( 10.1177/0363546516680604) [DOI] [PubMed] [Google Scholar]
- 55.Aitchison AH Hidalgo Perea S Schlichte LM & Green DW. Medial patellofemoral ligament reconstruction with simultaneous osteochondral fracture fixation is an effective treatment for adolescent patellar dislocation with osteochondral fractures. Journal of Children’s Orthopaedics 202216393–400. ( 10.1177/18632521221119541) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fabricant PD Yen YM Kramer DE Kocher MS Micheli LJ Lawrence JTR Ganley TJ & Heyworth BE. Fixation of traumatic chondral-only fragments of the knee in pediatric and adolescent athletes: a retrospective multicenter report. Orthopaedic Journal of Sports Medicine 201862325967117753140. ( 10.1177/2325967117753140) [DOI] [PMC free article] [PubMed] [Google Scholar]



 This work is licensed under a
This work is licensed under a