Abstract
The present study aimed to replicate the finding that younger age predicts higher pre quit-day attrition. Our second aim was to explain this relation by examining empirically and theoretically informed age-related risk factors for low smoking cessation treatment engagement. 136 participants (Mage = 44.2 years, SD = 11.3 years; age = 22–64 years) were randomized to 15-weeks of either 1) an exercise intervention (n = 72) or 2) a wellness education control condition (n = 64). First, a logistic regression analysis was employed to test whether younger adults were more likely than older adults to drop prior to quit date. Next, we assessed whether smoking related health concerns, social expectancies, and/or perceived severity of craving affected the strength of the relation between age and attrition, by adding these three variables to the logistic regression along with age. The logistic regression model indicated that younger age and treatment condition were significantly related to the odds of dropping from treatment prior to the scheduled quit date. Further, health concerns, social expectancies, and/or perceived severity of cravings did not account for the effect of age on pre quit-day attrition. These findings highlight the importance of identifying empirically and theoretically informed variables associated with the pre quit-day attrition problem of young smokers.
Keywords: Smoking cessation, age, attrition, youth
Introducthion
Despite the large effort to develop effective smoking cessation interventions, approximately 20% of adults between the ages of 25–44 in the United States remain cigarette smokers (Jamal et al., 2016). Importantly, smokers aged 25–44 express the most interest in quitting smoking with 73% expressing interest, compared to 54% of smokers over the age of 65 and 62% of those between the ages of 18 and 24 expressing interest in quitting (Jamal et al., 2016). Although more than half of all current smokers attempt to quit annually, young adults approach quitting differently than older adults (Suls et al., 2012). Specifically, younger adults are less inclined to seek help from mental health professionals and less likely to complete standard smoking cessation interventions (cognitive behavioral therapy [CBT] and nicotine replacement therapy [NRT]) than older adults (Solberg et al., 2007). Likewise, research suggests that college students rely primarily on quitting cold turkey and see little need to seek help from health care professionals (DeBernardo et al., 1999; Hines, 1996; Morrison et al., 2003).
Furthermore, there is evidence to suggest that even when younger adults choose to participate in cessation services they are significantly more likely than older adults to discontinue treatment (Audrain-McGovern et al., 2007; Brorson et al., 2013; Cosci et al., 2011; Ferguson et al., 2005; Leeman et al., 2006). Among clinical trial participants, older age was a significant predictor of increased treatment adherence (Audrain-McGovern et al., 2007; Brorson et al., 2013; Cosci et al., 2011; Ferguson et al., 2005; Leeman et al., 2006). Health (i.e. the severity of health concerns related to smoking), social (i.e., number of friends who smoke, bar attendance), and craving (i.e., perceived severity of cravings) related motivations have been frequently cited as contributing to the inverse relationship existing between age and attrition (Dietz et al., 2013; Doolan & Froelicher, 2008; Villanti et al., 2016; Walker & Loprinzi, 2014).
Social Cognitive Theory (SCT) (Bandura, 1977), a cornerstone theory in clinical and health psychology (Luczczynska & Schwarzer, 2005), posits that behavior change occurs as a result of dynamic, reciprocal, and transactional processes between individuals and their environments. Within this theoretical framework, behavior change, including beliefs/thoughts about change, motivation to change, and expectancies related to change, are thought to be products of an individual’s environment and social context (Bandura, 1986). SCT has been frequently cited as a theoretical basis for understanding the underlying reasons related to variable success when quitting smoking (Bandura, 1997; Luczczynska & Schwarzer, 2005). Moreover, SCT posits that outcome expectancies related to the potential consequences of quitting smoking greatly influence one’s decision to make an attempt. Specifically, smokers who expect more positive health and social outcomes are more likely to take actions in line with quitting goals (Bandura, 1997; Dijkstra et al., 1997; Luczczynska & Schwarzer, 2005). For example, smokers placing more emphasis on the positive health expectancies of quitting smoking (i.e., increased energy, blood circulation, and immune system functioning) vs. the negative health expectancies associated with withdrawal experiences (i.e., cravings, fatigue, anxiety, headaches/dizziness) are more likely to adhere to a quit attempt. Research demonstrates that younger adults are more likely to fear cravings, dread quit day, and be less concerned with the severity of smoking related health concerns, as compared to older adults (Dierker & Mermelstein, 2010; O’ Loughlin et al., 2003; Villanti et al., 2016; Walker & Loprinzi, 2014). In other words, younger adults are more likely than older adults to experience negative health expectancies (i.e., cravings) associated with quitting smoking. Conversely, as older adults are likely more concerned with severe smoking related conditions (i.e., heart disease, cancer), it is also likely that older adults place more emphasis on the long-term positive health expectancies (i.e., decreased risk for lung cancer) vs. the relatively short-term negative health expectancies (i.e., cravings). In light of research suggesting that positive health expectancies are more significant than negative health expectancies in behavior change associated with quitting smoking, it can be hypothesized that younger adults are less likely to take action quitting smoking partly as a result of comparatively heightened negative physical health outcome expectancies.
Additionally, SCT purports that positive social expectancies are related to an increase in action-oriented behaviors (Bandura, 1997). For example, smokers who expect support from social groups are more likely to make an attempt than those who expect disapproval from smoking friends or negative social consequences (Luczczynska & Schwarzer, 2005). Younger adults are more likely to have a greater number of friends who smoke and attend bars more frequently (Dietz et al., 2013). Similarly, younger adults appear to be less likely to quit smoking when peers continue to smoke (Chen et al., 2001; Tucker et al., 2002b, 2002a). Therefore, in line with SCT and related empirical findings, it can be hypothesized that younger adults are more likely to have negative social expectations associated with quitting smoking, and thus may be less likely to perform actions in line with quitting goals (i.e., adhere to cessation treatment). However, these relationships are currently poorly understood and it is clear that further work is needed in order to replicate these findings and identify additional theoretically salient variables associated with attrition among this population.
Of treatment phases involved in smoking cessation interventions—the pre-cessation phase, cessation phase, and maintenance phase—the pre-cessation phase is the period in which most smokers discontinue treatment (Baker et al., 2011; Collins et al., 2011; Shiffman et al., 2006). The pre-cessation phase is comprised of the several weeks prior to the target quit date in which participants spend time preparing for their quit attempt. The target quit date immediately precedes the cessation phase, or the several weeks following the quit attempt. The maintenance phase is defined as the period of time which typically involves cessation monitoring and support via study staff, intervention procedures, and collection of outcome assessments (Baker et al., 2011; Collins et al., 2011; Powers et al., 2016; Smits et al., 2012). Of these phases, the pre-cessation, or pre-quit phase, is particularly relevant due to the alarming rate at which smokers discontinue treatment during this phase (Ahluwalia et al., 2002; Borrelli et al., 2002; Evins et al., 2008; Jacquart et al., 2017; Woods et al., 2002). The few studies that speak to younger smoker attrition rates suggest that younger adults are even more likely than older adults to suspend treatment prior to the prescribed quit date, and even before randomization (Ahluwalia et al., 2002; Woods et al., 2002). Given the treatment resistant nature of young smokers in combination with their empirically demonstrated vulnerability to the pre-quit period, there is a need to understand the factors involved in this complex relationship. Extant literature fails to provide clinical researchers with suitable information regarding reasons behind younger smoker pre-quit attrition. As a result, researchers are uninformed as to how to correct the problem and ensure that young smokers successfully achieve their cessation goals and ultimately reach their scheduled quit day.
Using data from a randomized controlled trial examining smokers with elevated anxiety sensitivity (Smits et al., 2016), the current study is a secondary analysis examining the relation between age and attrition during the pre-quit phase. Our first aim was to replicate the common finding that younger age predicts pre quit-day attrition. Our second aim was to explain the relationship between younger age and pre quit-day attrition by examining empirically and theoretically informed age-related risk factors for low smoking cessation treatment engagement: smoking related health motivation (i.e., heart disease, lung cancer), social expectancies (i.e., smoking facilitates relaxed conversation and social engagement), and expected severity of cravings (Dietz et al., 2013; Doolan & Froelicher, 2008; Villanti et al., 2016; Walker & Loprinzi, 2014).
Method
Participants
Eligible participants were 136 (Mage = 44.2 years, SD = 11.3 years; age range = 22–64 years) adult smokers with elevated levels of anxiety sensitivity (MASI-3 = 18.37, SD = 11.58), who consented to a treatment study comparing the effects of an exercise augmented smoking cessation treatment and a wellness education augmented treatment on smoking cessation outcomes (see Table 1 for participant baseline and demographic characteristics). A full overview of eligibility criteria is presented in Smits et al. (2012).
Table 1.
Baseline and demographics characteristics.
| Non-Droppers (n = 94) |
Droppers (n = 42) |
|||
|---|---|---|---|---|
| n | M (SD) | n | M (SD) | |
| Age (years) | 94 | 43.83 (11.01) | 42 | 38.71 (11.05) |
| TND | 86 | 5.36 (1.91) | 39 | 5.43 (2.00) |
| ASI-3 | 94 | 18.11 (11.80) | 42 | 18.95 (11.20) |
| Health Concerns (RFQ) | 83 | 14.71 (3.88) | 38 | 14.95 (3.85) |
| Social Facilitation (BSCQ-A) | 86 | 3.58 (2.54) | 38 | 3.63 (2.29) |
| Craving & Addiction (BSCQ-A) | 86 | 6.33 (2.14) | 38 | 6.64 (2.41) |
|
| ||||
| n (%) | n (%) | |||
|
| ||||
| Treatment Condition (Vigorous- Intensity Exercise Intervention) | 43 (45.7) | 29 (69.0) | ||
| Sex (Females) | 47 (50.0) | 24 (57.1) | ||
| Education (Graduate School) | 68 (72.3) | 35 (83.3) | ||
| Marital Status (Single) | 50 (53.2) | 28 (66.7) | ||
| Ethnicity (Hispanic or Latino) | 8 (8.5) | 3 (7.1) | ||
| Race | ||||
| White | 64 (68.1) | 28 (66.7) | ||
| Black or African American | 17 (18.1) | 11 (26.2) | ||
| Asian | 3 (3.2) | 0 (0.0) | ||
| Other or Not reported | 4 (4.3) | 1 (2.4) | ||
M = mean; SD = standard deviation; TND = Test for Nicotine Dependence; ASI-3 = Anxiety Sensitivity Index-3; RFQ = Reasons for Quitting (Curry et al., 1990); BSCQ-A = Brief Smoking Consequences Questionnaire- A (Rash & Copeland, 2008).
Interventions
All participants were prescribed a standard smoking cessation treatment consisting of seven weekly 60-minute sessions of cognitive behavioral therapy and nicotine replacement therapy (NRT). In addition, participants were randomized to either a vigorous-intensity exercise intervention or a wellness education intervention, each involving three weekly 45-minute sessions for 15 weeks. Each session consisted of treatment (exercise or wellness education), study staff support, and NRT in the form of transdermal patches. The exercise condition involved a program in which participants were asked to attend three exercise sessions a week. Study clinicians educated participants on the implications of anxiety sensitivity in smoking maintenance and presented exercise as a means for interoceptive exposure to these bodily sensations. Over the first couple of weeks, participants worked to increase the intensity of their exercise to reach 77% to 85% of their maximum heart rate. The wellness education condition incorporated a program in which participants engage with lectures, videos, handouts, and discussions regarding healthy lifestyle changes (i.e., healthy eating, time management). Participants were informed these education sessions were included to encourage smoking cessation by fostering a generally healthier lifestyle. For an in-depth description of study procedures see (Smits et al., 2012).
Defining attrition
Participants were asked to make a quit attempt on week 6 of the intervention (Smits et al., 2012). Therefore, participants who discontinued treatment during or prior to week 6 were considered pre-quit drops, and participants were correspondingly coded as either Droppers (n = 42, 30.9%) or Non-Droppers (n = 94, 69.1%) before the quit date in this 15-week program.
Measures
Anxiety sensitivity index- 3
(ASI; Taylor et al., 2007). The ASI is an 18- item measure in which individuals indicate the severity of concern related to perceived negative consequences of anxiety-related physical sensations. The ASI-3 has been validated among smokers (Farris et al., 2015).
Test for nicotine dependence
(TND; Fagerström, 2012). The TND is a 6-item measure utilized to demonstrate the severity of an individual’s daily dependence on nicotine.
Brief smoking consequences questionnaire-A
(BSCQ-A; Rash & Copeland, 2008). The BSQ-A is a 25-item questionnaire assessing negative and positive smoking outcome expectancies. For the purpose of this study, we employed the Social Facilitation subscale to assess social expectancies related to smoking and the Craving/Addiction subscale to assess expectancies related to craving satisfaction.
Reasons for quitting smoking
(RFQ; Curry et al., 1990). The RFQ is a 20-item self-report measure utilized to assess motivation for quitting smoking. In the present sample, we examined the Health Concerns subscale to measure cessation motivations related to current or potential health problems. In line with our theoretical basis for selecting relevant variables, we selectively included the Health Concerns subscale to assess physical health expectancies.
Data analytic plan
First, we tested the hypothesis that younger adults were more likely than older adults to drop before their quit date during a smoking cessation trial, using logistic regression (Droppers = 0, Non-Droppers = 1) in SPSS 25. Next, we assessed whether smoking related health motivations, social expectancies, and perceived severity of cravings affected the strength of relation between age and attrition, by adding these three variables to the logistic regression along with age. We tested whether the relation between age and dropout was significantly reduced by accounting for these psychological variables, and whether these variables were significantly related to dropout. The significance of the decrease in the regression coefficient for age when accounting for the additional variables was tested using the McGuigan & Langholtz method (MacKinnon et al., 2002). Finally, since the reasons of dropout might be different in the two very different treatment conditions (vigorous exercise vs. wellness education), we explored whether treatment condition moderated the relations between the four variables (age and the psychological variables) and dropout.
As there was a significant difference in the proportion of participants who were Droppers in the two treatment groups (vigorous-intensity exercise intervention: n = 29 droppers out of 72 participants [40.3% of “exercise” participants] vs. wellness education intervention: n = 13 droppers out of 64 participants [20%]), treatment condition was included as a covariate in all analyses (see Jacquart et al., 2017). Additionally, baseline anxiety sensitivity (ASI; Taylor et al., 2007) and baseline nicotine dependence (TND; Fagerström, 2012) were also included as covariates in all analyses. The ASI-3 and TND were included because they have been previously related to smoking cessation (Breslau et al., 2001). Finally, sensitivity analyses were also performed.
Results
Correlations between age, health concerns, social expectancies, and expected severity of cravings were calculated using Pearson’s r (Figure 1). Results indicated that age and health motivation were not significantly related, r(135) = 0.11, p =.23. However, higher age was significantly related to lower social expectancies, r(135) = −0.30, p = <.001, and to lower expected severity of cravings, r(135) = −0.18, p = .045.
Figure 1.
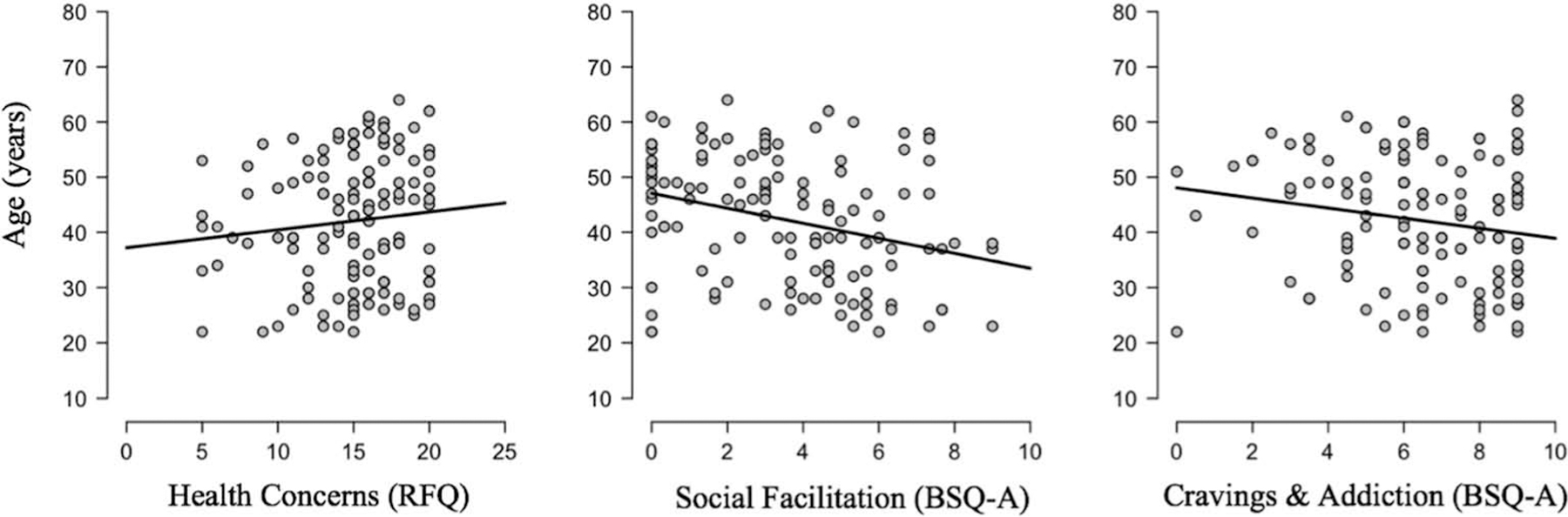
Correlations between age and a) health motivation (Pearson’s r = 0.11, p =.23), b) social expectancies (Pearson’sr= −0.30, p <.001*), and c) expected severity of cravings (Pearson’sr= −0.18, p =.045*).
Relation of age to dropout
Controlling for baseline ASI, baseline TND, and treatment condition, higher age was significantly related to lower log odds (and hence lower probability) of dropping out, b = .046, Wald χ2(1) = 5.71, p = .017, OR = 1.05, 95%CI: [1.01, 1.09] (see Figure 2). In this analysis, treatment condition was also significantly related to dropout, with participants assigned to vigorous-intensity exercise having higher log odds of dropping out than those assigned to wellness education, b = .97, Wald χ2(1) = 5.38, p = .020, OR = 2.65, 95%CI: [1.16, 6.03]. Neither ASI nor TND were significantly related to dropout (ps > .44).
Figure 2.

Age and Pre-quit dropout rates. The probability of a participant dropping out of treatment before quite date decreases with age. The grey shaded area around the line represents the 95% confidence interval.
Effects of health concerns, social facilitation, and cravings on dropout
To determine whether health concerns, social facilitation, and/or cravings accounted for the effect of age on dropout, these three variables were added to the logistic regression predicting dropout. None of these variables was significantly related to dropout (all ps>.44), and the Nagelkerke R2 of this model (.145) was only modestly higher than that for the model without these three predictors (.133). Further, age remained significantly related to dropout when controlling for these additional variables, b = .047, Wald χ2(1) = 5.10, p = .024, OR = 1.05, 95%CI: [1.01, 1.09], and the regression coefficient for age actually increased (if very slightly) in this model. Since the regression coefficient for age actually increased when accounting for health concerns, social facilitation, and cravings, it made no sense to test whether it significantly decreased when accounting for these variables in this model. As in the previous model, treatment condition remained significantly related to dropout, b = 1.03, Wald χ2(1) = 5.36, p = .021, OR = 2.80, 95%CI: [1.17, 6.71], but ASI and TND were not related to dropout (ps > .61).
Exploratory analysis: treatment condition moderating the effects of health concerns, social facilitation, and cravings on dropout
To investigate treatment condition as a moderator of the effects of the psychological variables on outcome, we added the interaction of treatment condition and each of the three psychological variables to the model. None of the interactions was significant (ps > .08).
Sensitivity analyses
Because the effect of age on dropout might be different for the two different treatment conditions, the interaction of age and treatment condition was added to all the above analyses and the models were recomputed. The age x treatment condition interaction was not significant in any of the analyses (ps>.73), and the other results from those analyses were not changed by adding this interaction to those analyses. Other sensitivity analyses examined whether the relation between age and dropout was quadratic by adding a quadratic term to the analyses. The quadratic terms were not significant in any analysis.
In further sensitivity analyses, all analyses were repeated using survival analyses which examined whether our variables were related to time to dropout (rather than to dropout yes/no). Results of these sensitivity analyses, using Cox Regression, were identical (in terms of which variables were significant) to those of our logistic regressions.
Discussion
The current study aimed to examine the relationship between age and pre quit-day attrition in a smoking cessation intervention. We found older smokers had a significantly greater likelihood of continuing with treatment past quit day than younger smokers. These results are consistent with evidence that found younger age was also related to greater odds of dropping early from smoking cessation treatment while older age was related to increased odds of attending smoking cessation treatment (Audrain-McGovern et al., 2007; Brorson et al., 2013; Cosci et al., 2011; Ferguson et al., 2005; Leeman et al., 2006). This relationship may exist for a number of logistical, treatment related, and/or other reasons. Younger smokers may be less likely to commit to treatment, have less time and energy to devote toward a scheduled quit day, and be more likely to lose motivation to quit as the scheduled quit-day approaches.
Research and theory suggest there are several reasons older adults may be more likely to adhere to cessation programs past quit day than younger adults (Dietz et al., 2013; Doolan & Froelicher, 2008; Luczczynska & Schwarzer, 2005; Villanti et al., 2016; Walker & Loprinzi, 2014). First, persistent smoking behavior among young adults has been strongly associated with self-identified status as a smoker and social lifestyle variables which may make approaching quit day more difficult (Dietz et al., 2013). Specifically, young people with a high frequency of visiting bars and clubs, consuming alcohol, and socializing with other smokers are four times less likely to quit smoking (Dietz et al., 2013). Further, social factors appear to negatively predict levels of treatment engagement and subsequent treatment success among young adults as opposed to older adults (Dietz et al., 2013). The lack of predictive relation between social facilitation expectancies and treatment attrition in our study suggests that social facilitation may relate to smoking cessation but apparently plays a small role in pre quit-day attrition rates, at least in this sample. Even though younger adults are more likely than older adults to fear negative social consequences when quitting smoking (i.e., social awkwardness, feeling as if one does not belong, nervousness in social situations), these social factors were not significantly involved in pre quit-day attrition in the current study. It is possible that social facilitation expectancies are better suited to describe which young smokers are motivated to seek cessation treatment. Younger smokers who feel their identity is largely tied to their status as a smoker may be less likely to seek cessation treatment in the first place. Therefore, while younger smokers may be more likely than older smokers to fear negative social evaluation, this particular construct appears unrelated to an individual’s likelihood of adhering to prescribed treatment beyond quit day.
Secondly, previous research suggests that older adults are more likely to endure uncomfortable smoking related cravings than younger smokers because younger adults perceive cravings to be acutely uncomfortable, and are thus more fearful of quit day (Dierker & Mermelstein, 2010; O’ Loughlin et al., 2003; Villanti et al., 2016; Walker & Loprinzi, 2014). Although it is true that younger smokers in the current sample were more likely to perceive greater challenges for the designated quit date due to expected unmanageable cravings, craving aversion did not contribute to pre quit-day attrition rates. Similarly, although younger smokers in the current sample did report less concern about the health consequences of smoking than the older smokers, these concerns were not related to dropout in the current sample. These results may be related to the fact that the current sample was selected based on elevated anxiety sensitivity. Future research should investigate whether our findings replicate in a sample of smokers who do not have elevated anxiety
It is important to consider the present findings in light of several limitations. The original study was not designed to test for age specific differences and did not target specific age-cohorts (Smits et al., 2012); therefore, we do not have extensive information regarding age relevant social and environmental variables potentially involved in quit day preparation. Additionally, the nature of our sample presents its own set of limitations. Although our sample included a large range of ages (Non-Dropper: age range = 22–64; Dropper: age range = 22–60), there is room for future studies to examine an even broader range of ages. Including individuals younger than 22 and older than 64 may help to better refine and augment smoking cessation treatments. Further, this study examines the effects of a rather unique intervention, involving 6-weeks of lifestyle modification (i.e., exercise and wellness education) preceding the quit date and includes individuals belonging to a subgroup of smokers of whom express relatively high levels of anxiety sensitivity. Given these specifics, it is important to consider that the present findings may not be generalizable to wider clinical populations. In order to sufficiently describe trends existing between age and pre quit-day attrition, future research should include larger samples, investigate the effects of an array of smoking cessation interventions, and measure variables that may be explicitly implicated in the relationship between age and pre-quit attrition.
The current findings support existing research that highlights younger age as it relates to elevated pre quit-day attrition rates in smoking cessation trials. However, this study fails to adequately explain the relationship between younger age and increased pre quit-day attrition. Importantly, future research should seek to understand the pre-quit attrition problem existing amongst younger smokers. Extant research does not provide a plausible explanation for the root of this problem and clinical researchers are accordingly uninformed on how to develop evidence-based pre-treatment interventions to effectively address it. Future research should examine the extent to which other theoretically informed variables related to positive behavior change, such as perceived self-efficacy, goal setting, and social encouragement, predict adherence to smoking cessation interventions. Given this knowledge and considering the current and impending negative public health implications, it is critical that future research identifies the variables related to pre quit-day attrition during smoking cessation trials amongst the young adult population.
Funding
This study was funded by a grant from the National Institute on Drug Abuse [NIDA; R01DA027533, 2009]. NIDA plays no role in approving this publication.
Footnotes
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Ahluwalia JS, Richter K, Mayo MS, Ahluwalia HK, Choi WS, Schmelzle KH, & Resnicow K (2002). African American smokers interested and eligible for a smoking cessation clinical trial: Predictors of not returning for randomization. Annals of Epidemiology, 12(3), 206–212. 10.1016/S1047-2797(01)00305-2 [DOI] [PubMed] [Google Scholar]
- Audrain-McGovern J, Halbert CH, Rodriguez D, Epstein LH, & Tercyak KP (2007). Predictors of participation in a smoking cessation program among young adult smokers. Cancer Epidemiology: Biomarkers & Prevention, 16(3), 617–619. 10.1158/1055-9965.EPI-06-0791 [DOI] [PubMed] [Google Scholar]
- Baker TB, Mermelstein RJ, Collins LM, Piper ME, Jorenby DE, Smith SS, Christiansen BA, Schlam TR, Cook JW, & Fiore MC (2011). New methods for tobacco dependence treatment research. Annals of Behavioral Medicine, 41(2), 192–207. 10.1007/s12160-010-9252-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A (1977). Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review, 84(2), 191–215. 10.1037/0033-295X.84.2.191 [DOI] [PubMed] [Google Scholar]
- Bandura A (1986). Social foundations of thought and action: A social cognitive theory Prentice-Hall. [Google Scholar]
- Bandura A (1997). Self-efficacy: The exercise of control Freeman. [Google Scholar]
- Borrelli B, Hogan JW, Bock B, Pinto B, Roberts M, & Marcus B (2002). Predictors of quitting and dropout among women in a clinic-based smoking cessation program. Psychology of Addictive Behaviors, 16(1), 22–27. 10.1037/0893-164X.16.1.22 [DOI] [PubMed] [Google Scholar]
- Breslau N, Johnson EO, Hiripi E, & Kessler R (2001). Nicotine dependence in the United States: Prevalence, trends, and smoking persistence. Archives of General Psychiatry, 58(9), 810–816. 10.1001/archpsyc.58.9.810 [DOI] [PubMed] [Google Scholar]
- Brorson HH, Arnevik EA, Rand-Hendriksen K, & Duckert F (2013). Drop-out from addiction treatment: A systematic review of risk factors. Clinical Psychology Review, 33(8), 1010–1024. 10.1016/j.cpr.2013.07.007 [DOI] [PubMed] [Google Scholar]
- Chen P-H, White RH, & Pandina RJ (2001). Predictors of smoking cessation from adolescence into young adulthood. Addictive Behaviors, 26(4), 517–529. 10.1016/S0306-4603(00)00142-8 [DOI] [PubMed] [Google Scholar]
- Collins LM, Baker TB, Mermelstein RJ, Piper ME, Jorenby DE, Smith SS, Christiansen BA, Schlam TR, Cook JW, & Fiore MC (2011). The multiphase optimization strategy for engineering effective tobacco use interventions. Annals of Behavioral Medicine, 41(2), 208–226. 10.1007/s12160-010-9253-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cosci F, Pistelli F, Lazzarini N, & Carrozzi L (2011). Nicotine dependence and psychological distress: Outcomes and clinical implications in smoking cessation. Psychology Research and Behavior Management, 4, 119–128. 10.2147/PRBM.S14243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curry S, Wagner EH, & Grothaus LC (1990). Intrinsic and extrinsic motivation for smoking cessation. Journal of Consulting and Clinical Psychology, 58(3), 310–316. 10.1037/0022-006X.58.3.310 [DOI] [PubMed] [Google Scholar]
- DeBernardo R, Aldinger C, Dawood O, Hanson R, Lee S, & Rinaldi S (1999). An E-mail assessment of undergraduates’ attitudes toward smoking. Journal of American College Health, 48(2), 61–66. 10.1080/07448489909595675 [DOI] [PubMed] [Google Scholar]
- Dierker L, & Mermelstein R (2010). Early emerging nicotine-dependence symptoms: A signal of propensity for chronic smoking behavior in adolescents. The Journal of Pediatrics, 156(5), 818–822. 10.1016/j.jpeds.2009.11.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietz NA, Sly DF, Lee DJ, Arheart KL, & McClure LA (2013). Correlates of smoking among young adults: The role of lifestyle, attitudes/beliefs,demographics, and exposure to anti-tobacco media messaging. Drug and Alcohol Dependence, 130(1–3), 115–121. 10.1016/j.drugalcdep.2012.10.019 [DOI] [PubMed] [Google Scholar]
- Dijkstra A, Bakker M, & DeVries H (1997). Subtypes within a precontemplating sample of smokers: A preliminary extension of the stages of change. Addictive Behaviors, 22(3), 227–237. 10.1016/S0306-4603(96)00054-8 [DOI] [PubMed] [Google Scholar]
- Doolan DM, & Froelicher ES (2008). Smoking cessation interventions and older adults. Progress in Cardiovascular Nursing, 23(3), 119–127. 10.1111/j.1751-7117.2008.00001.x [DOI] [PubMed] [Google Scholar]
- Evins AE, Culhane MA, Alpert JE, Pava J, Liese BS, Farabaugh A, & Fava M (2008). A controlled trial of bupropion added to nicotine patch and behavioral therapy for smoking cessation in adults with unipolar depressive disorders. Journal of Clinical Psychopharmacology, 28(6), 660–666. 10.1097/JCP.0b013e31818ad7d6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagerström K (2012). Determinants of tobacco use and renaming the FTND to the Fagerstrom test for cigarette dependence. Nicotine & Tobacco Research, 14(1), 75–80. 10.1093/ntr/ntr137 [DOI] [PubMed] [Google Scholar]
- Farris SG, DiBello AM, Allan NP, Hogan J, Schmidt NB, & Zvolensky MJ (2015). Evaluation of the anxiety sensitivity index-3 among treatment-seeking smokers. Psychological Assessment, 27(3), 1123–1128. 10.1037/pas0000112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson J, Bauld L, Chesterman J, & Judge K (2005). The English smoking treatment services: One-year outcomes. Society for the Study of Addiction, 100(2), 59–69. 10.1111/j.1360-0443.2005.01028.x [DOI] [PubMed] [Google Scholar]
- Hines D (1996). Young smokers’ attitudes about methods for quitting smoking: Barriers and benefits to using assisted methods. Addictive Behaviors, 21(4), 531–535. 10.1016/0306-4603(95)00076-3 [DOI] [PubMed] [Google Scholar]
- Jacquart J, Papini S, Davis ML, Rosenfield D, Powers MB, Frierson GM, Hopkins LB, Baird SO, Marcus BH, Church TS, Otto MW, Zvolensky MJ, & Smits JAJ (2017). Identifying attendance patterns in a smoking cessation treatment and their relationships with quit success. Drug and Alcohol Dependence, 174, 65–69. 10.1016/j.drugalcdep.2017.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamal A, King BA, Neff LJ, Whitmill J, Babb SD, & Graffunder CM (2016). Current cigarette smoking among adults—United States, 2005–2015. Centers for Disease and Control Prevention, 65(44), 1205–1211. Retrieved from https://www.jstor.org/stable/24859133 [DOI] [PubMed] [Google Scholar]
- Leeman RF, Quiles ZN, Molinelli LA, Terwal DM, Nordstrom BL, Garvey AJ, & Kinnunen T (2006). Attrition in a Multi-Component Smoking Cessation Study for Females. Tobacco Induced Diseases, 3(2), 59. 10.1186/1617-9625-3-2-59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luczczynska A, & Schwarzer R (2005). Social cognitive theory. In Predicting health behaviour: Research and practice with social cognition models (2nd ed., pp. 127–169). Open University Press. [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, & Sheets V (2002). A comparison of methods to test mediation and other intervening variable effects. Psychological Methods, 7(1), 83. 10.1037/1082-989X.7.1.83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison K, Banas J, & Burke M (2003). Understanding college students’ salient attitudes and beliefs about smoking: Distinctions between smokers, nonsmokers, and ex-smokers. Public Health Review, 31(2), 95–109. Retrieved from https://europepmc.org/article/med/15255159 [PubMed] [Google Scholar]
- O’ Loughlin J, DiFranza J, Tyndale RF, Meshefedjian G, McMillan-Davey E, Clarke PBS, Hanley J, & Paradis G (2003). Nicotine-dependence symptoms are associated with smoking frequency in adolescents. American Journal of Preventive Medicine, 25(3), 219–225. 10.1016/S0749-3797(03)00198-3 [DOI] [PubMed] [Google Scholar]
- Powers MB, Kauffman BY, Kleinsasser AL, Lee-Furman E, Smits JAJ, Zvolensky MJ, & Rosenfield D (2016). Efficacy of smoking cessation therapy alone or integrated with prolonged exposure therapy for smokers with PTSD: Study protocol for a randomized controlled trial. Contemporary Clinical Trials, 50, 213–221. 10.1016/j.cct.2016.08.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rash CA, & Copeland AL (2008). The brief smoking consequences questionnaire–Adult (BSCQ-A): Development of a short form of the SCQ-A. Nicotine & Tobacco Research, 10(11), 1633–1643. 10.1080/14622200802409990 [DOI] [PubMed] [Google Scholar]
- Shiffman S, Scharf DM, Schadel WG, Gwaltney CJ, Dang Q, Paton SM, & Clark DB (2006). Analyzing milestones in smoking cessation: Illustration in a nicotine patch trial in adult smokers. Journal of Consulting and Clinical Psychology, 74(2), 276–285. 10.1037/0022-006X.74.2.276 [DOI] [PubMed] [Google Scholar]
- Smits JAJ, Zvolenksy MJ, Davis ML, Rosenfield D, Marcus BH, Church TS, Powers MB, Frierson GM, Otto MW, Hopkins LB, & Baird SO (2016). The efficacy of vigorous-intensity exercise as an aid to smoking cessation in adults with high anxiety sensitivity: A randomized controlled trial. Psychosomatic Medicine, 78(3), 354–364. 10.1097/PSY.0000000000000264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smits JAJ, Zvolensky MJ, Rosenfield D, Marcus BH, Church TS, Frierson GM, Powers MB, Otto MW, Davis ML, DeBoer LB, & Briceno NF (2012). The efficacy of vigorous-intensity exercise as an aid to smoking cessation in adults with elevated anxiety sensitivity: Study protocol for a randomized controlled trial. Trials, 13(1), 207–221. 10.1186/1745-6215-13-207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solberg LI, Boyle RG, McCarty M, Asche SE, & Thoele MJ (2007). Young adult smokers: Are they different? The American Journal of Managed Care, 13(11), 626–632. Retrieved from https://www.researchgate.net/profile/Raymond_Boyle/publication/5859032_Young_adult_smokers_Are_they_different/links/545ce6360cf2c1a63bfa58ec.pdf [PubMed] [Google Scholar]
- Suls JM, Luger TM, Curry SJ, Mermelstein RJ, Sporer AK, & An LC (2012). Efficacy of smoking-cessation interventions for young adults: A Meta-analysis. American Journal of Preventive Medicine, 42(6), 655–662. 10.1016/j.amepre.2012.02.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, Abramowitz JS, Holaway RM, Sandin B, Stewart SH, Coles M, Eng W, Daly ES, Arrindell WA, Bouvard M, & Cardenas SJ (2007). Robust dimensions of anxiety sensitivity: Development and initial validation of the anxiety sensitivity index-3. Psychological Assessment, 19(2), 176–188. 10.1037/1040-3590.19.2.176 [DOI] [PubMed] [Google Scholar]
- Tucker JS, Ellickson PL, & Klein DJ (2002a). Five-year prospective study of risk factors for daily smoking in adolescence among early nonsmokers and experimenters 1. Journal of Applied Social Psychology, 32(8), 1588–1603. 10.1111/j.1559-1816.2002.tb02764.x [DOI] [Google Scholar]
- Tucker JS, Ellickson PL, & Klein DJ (2002b). Smoking cessation during the transition from adolescence to young adulthood. Nicotine & Tobacco Research, 4(3), 321–332. 10.1080/14622200210142698 [DOI] [PubMed] [Google Scholar]
- Villanti AC, Bover Manderski MT, Gundersen DA, Steinberg MB, & Delnevo CD (2016). Reasons to quit and barriers to quitting smoking in US young adults. Family Practice, 33 (2), 133–139. 10.1093/fampra/cmv103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker JF, & Loprinzi PD (2014). Longitudinal examination of predictors of smoking cessation in a national sample of U.S. Adolescent and young adult smokers. Nicotine & Tobacco Research, 16(1), 820–827. 10.1093/ntr/ntu005 [DOI] [PubMed] [Google Scholar]
- Woods MN, Harris KJ, Mayo MS, Catley D, Scheibmeir M, & Ahluwalia JS (2002). Participation of African Americans in a smoking cessation trial: A quantitative and qualitative study. Journal of the National Medical Association, 94(7), 609–618. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2594312/ [PMC free article] [PubMed] [Google Scholar]


