Abstract
In the context of body image and mental health, transgender individuals face distinctive challenges stemming from the complexities of their gender identity journey, societal expectations, and body norms. However, the existing line of research on this topic remains limited. This study explores the complex relationship in transgender individuals between body objectification, body weight dissatisfaction, and eating concerns. A sample of 154 individuals (77 transgenders paired with 77 cisgenders) was recruited via LGBTQ+ groups’ mailing lists. Participants completed various questionnaires assessing body image, eating psychopathology, depression, and body objectification. Propensity score matching was performed with different variables: age, current BMI, years of education, current self-identified gender, and sexual orientation. The results revealed that transgender individuals experienced higher levels of body objectification, body weight dissatisfaction, and eating concerns compared to their cisgender counterparts. Additionally, age emerged as a protective factor, as older transgender individuals demonstrated improved body acceptance and self-esteem. Logistic regression analyzes indicated that bulimic behaviors, depressive symptoms, and appearance control beliefs were specific factors significantly associated with being transgender. Our findings highlight the unique challenges faced by transgender individuals in navigating their gender identity and body image, underscoring the importance of targeted interventions and support systems.
Keywords: Transgender, Body objectification, Eating concerns, Body weight dissatisfaction, Body perception, Physical comparison, Well-being
Introduction
Body image entails the intricate psychological encounter of being in one's own body, involving perceptions and attitudes towards oneself, encompassing thoughts, beliefs, feelings, and actions related to the body (Cash, 2004). It is commonly described as how individuals perceive their physical selves and the subsequent emotions and thoughts that arise from that perception. When any of these aspects are affected negatively, it is termed as body image concerns or negative body image. In recent years, increasing attention has been given to the intersectionality of body image concerns and mental health in various populations (Shagar et al., 2017; Yarborough et al., 2016). For transgender individuals, the journey toward self-acceptance and the achievement of positive body image is further complicated by unique challenges related to gender identity, transitioning, and societal expectations (Tabaac et al., 2018). In the realm of body image, the pressure to conform to societal beauty standards has long been a pervasive concern, impacting individuals in different ways across various gender identities and sexual orientations (McClain & Peebles, 2016; Meneguzzo et al., 2020; Owen-Smith et al., 2018). However, for transgender individuals, the passage towards self-acceptance and positive body image is further complicated by stereotypical gender expectations, which can exacerbate peoples’ concerns with their own appearance and may contribute to body dissatisfaction (Gillen & Markey, 2016; McGuire et al., 2016). Possible factors that can be part of self-evaluation and body concerns are weight dissatisfaction (Richard et al., 2016) and body objectification (Tiggemann & Lynch, 2001), so far both poorly evaluated in the transgender population (Jones et al., 2018).
Body weight dissatisfaction (BWD) refers to the negative thoughts and feelings individuals experience concerning their own body weight or shape (Austin et al., 2009). In a society that often equates worth with adherence to conventional beauty norms and expectations, many people, including transgender individuals, are struggling with feelings of inadequacy, self-consciousness, and frustration about their bodies. These emotions can be particularly pronounced during gender transition, as individuals strive to align their physical appearance with their true personal gender identity, navigating societal expectations and personal validation pressures (Jones et al., 2018; Peterson et al., 2017).
Body objectification (BO), on the other hand, revolves around the tendency to view and treat oneself or others as mere objects, judged primarily on physical appearance rather than their inherent qualities and achievements (Kahalon et al., 2018). In particular, the literature has found a consensus around the objectification theory (Fredrickson et al., 1997), a framework that allowed the tendency to perceive, consider and treat one's body as an object. This theory recognizes three main components: body surveillance, body shame, and appearance control beliefs (Mckinley & Hyde, 1996). The core principle of bodily surveillance involves continuous self-awareness and ongoing self-observation, adopting an external observer's viewpoint to adhere to societal body norms and prevent unfavorable evaluations. Body shame emerges from measuring oneself against cultural ideals and feeling inadequate in meeting them. Lastly, appearance control beliefs pertain to the idea that individuals bear the responsibility for their bodily appearance and can exert sufficient effort to manage their physical look. Transgender individuals may experience heightened levels of body objectification, as their bodies are frequently scrutinized and judged by others, often leading to feelings of vulnerability, inappropriateness, and detachment from their own sense of self (Anzani et al., 2021; Comiskey et al., 2020). This objectification may manifest in various contexts, from everyday interactions to media representation, exacerbating the challenges they face in cultivating a positive body image and increasing the shame perceived (Cascalheira & Choi, 2023).
The convergence of weight body dissatisfaction and body objectification might present a unique and complex experience for transgender individuals. For some, this might lead to engaging in unhealthy weight management practices, such as extreme dieting or exercising, as a means to conform to societal norms, and combat body dissatisfaction, and a sense of inadequacy (Brewster et al., 2019; Parker & Harriger, 2020; Strübel et al., 2020). In turn, such practices can further contribute to negative body image and a sense of disconnection from their bodies. By addressing weight body dissatisfaction, body objectification, and their intersection with transgender identity, a more inclusive and compassionate dialogue around body image issues may be practiced. Indeed, acknowledging and validating the diverse experiences of transgender individuals can pave the way for effective support systems, inclusive mental health care, and body-positive environments, improving transgenders’ mental health and allowing health stakeholders to identify people most at risk of developing psychopathology (Duffy et al., 2016; Hartman-Munick et al., 2021).
Therefore, this study aimed to evaluate BWD and body objectivation in transgender people. Our initial hypothesis posits that transgender individuals may experience higher levels of BWD and BO compared to their cisgender counterparts, based on the existing literature highlighting elevated levels of body dissatisfaction within the transgender community. This proposition stems from a recognition that body image plays a significant role in overall mental health. As a secondary exploration, our study aims to examine the intricate relationship between specific psychological factors, namely depression, and eating disorders, and the potential impact on mental health in transgender individuals. We hypothesize that there exists a meaningful connection between these psychological factors and mental health. By addressing these hypotheses, we strive to contribute valuable insights that may inform targeted interventions to enhance the psychological well-being of transgender individuals.
Methods
Participants and procedure
The participants were recruited via LGBTQ+ groups’ mailing lists from the Region of Veneto, in the northeastern area of Italy, through an official email from the legal representatives of those associations. People were invited to manifest their will to participate in an online evaluation of the psychological health and well-being of the transgender population. Then, a specific link to an online questionnaire was sent to those who agreed to participate via an online secure platform (surveymonkey.com). Eligible participants identified under a broad definition of transgender, without any requirements for social or medical gender transition.
The data were collected between August 2019 and January 2020. Each participant provided informed consent before receiving the online survey. The research was in accordance with the Declaration of Helsinki, and the local ethics committee approved the study. The anonymous nature of the data acquired does not require the application of European and national legislation about privacy.
Measures
The first part of the survey concerns the collection of demographic data: age, height, current weight, minimum and maximum life weight – data used to calculate body mass index (BMI) as weight (kg) divided by height squared (m2), and years of education. Participants were asked to identify themselves as cisgender, transgender, or queer, with specific items about the sex assigned at birth and their current gender. Sexual orientation was assessed, asking to choose from four possibilities: heterosexual, bisexual, gay/lesbian, and asexual. The second part of the survey was composed of four questionnaires and a figure rating scale.
The Patient Health Questionnaire (PHQ-9) is a 9-item Likert scale self-report measure of depression, and it is rated on a 4-point scale from 0 (not at all) to 3 (almost every day) (Kroenke et al., 2001; Mazzotti et al., 2003). Higher scores indicate greater depression symptomatology with a clinical cut-off of 10 for moderate depressive symptoms. Cronbach's alpha in the current study was 0.80.
The revised Physical Appearance Comparison Scale (PACS) is a five-item self-report measure of general appearance-comparison frequency (Meneguzzo et al., 2021; Schaefer & Thompson, 2014). Items are rated on a 5-point Likert scale ranging from 1 (never) to 5 (always). Higher scores indicate higher levels of general appearance comparison. Cronbach's alpha in the current study was 0.75.
The Eating Attitudes Test (EAT-26) is a self-rated measure of eating attitudes, including a 26-item scale that measures symptoms and concerns of eating disorders, rated on a six-point Likert scale (Dotti & Lazzari, 1998; Garner et al., 1982). It is composed of three factors (dieting, bulimia, and oral control) and a global score. Cronbach's alpha in the current study was 0.90.
The Objectified Body Consciousness (OBC) contains 24 items grouped into three subscales: Body Surveillance (BSV), Body Shame (BSH), and Appearance Control Beliefs (ACB) (Dakanalis et al., 2017; Mckinley & Hyde, 1996). Each subscale contains eight items, rated on a 7-point Likert scale (1 = strongly disagree, 7 = strongly agree). Higher scores indicate a greater manifestation of the variable measured. Cronbach's alpha in the current study was 0.86.
A biometric Figure Rating Scale (FRS) was used to assess body image disturbances (Meneguzzo et al., 2020; Mölbert et al., 2017). The FRS comprises a sequence of figures, typically drawings, depicting various weights from underweight to obese, prompting individuals to identify a particular weight, such as their current weight. This specific biometric FRS was developed using 3D body scans of real people, enhancing the precision of comparisons with participants' actual bodies (Mölbert et al., 2017). Two different 12-point FRSs were presented simultaneously, one with masculine and one with female attributes, allowing participants to choose the specific figure in a BMI spectrum from 14 to 36 kg/m2 with an increase of 2 kg/m2 and a center of 25 kg/m2. The participants were asked to choose firstly which figure best represented their body size, and then their ideal body; these questions were asked to identify possible biased representations and body weight dissatisfaction.
We thus extrapolated two different scores, one of Body Weight Dissatisfaction (BWD), and of Perceptual Distortion (PD). In particular, for the BWD score, we subtracted the selected ideal figure score from the estimated current figure score, while for the PD score, we subtracted the current figure score (i.e., the individual's body's score, which was closest to self-reported BMI) from the estimated current figure score.
Statistical analyzes
To estimate the sample size needed, an a priori power analysis was performed with G*Power 3.1.9.7, based on data from the literature regarding body dissatisfaction in transgender individuals (Witcomb et al., 2015). Utilizing results from a study on body dissatisfaction in 200 transgender individuals (10.72 ± 7.44) and 200 controls (7.17 ± 6.72), it was determined that 70 individuals per group would be necessary to achieve a medium effect size (Cohen's d = 0.49) with a significance level (α) of 0.05, a power (β) of 0.95, an allocation ratio of 1, and an actual power of 0.96. Considering an attrition of 10 %, 77 individuals were recruited.
All the responses were checked for quality. No participant responded in less than 15 min. Moreover, three open-ended items requiring the spelling of specific numbers were used to evaluate the active participation of the responders through the survey. All participants passed the evaluation.
The comparison subjects were selected from a sample of 1033 cisgender individuals who participated in a previous study (Meneguzzo et al., 2020). The propensity score matching procedure (Vanderweele, 2006) was performed as closely as possible and in the following order: age, current BMI, years of education, current self-identified gender, and sexual orientation. Comparison subjects were chosen without replacement. The total sample included in the study was composed of 77 transgender people (TP) and 77 cisgender peers (CP), see Results for details.
First, the distribution of categorical variables was evaluated with Chi-square analysis, while differences between trans- and cis-gender groups were evaluated with Mann-Whitney tests for independent samples due to the non-parametric nature of the data. Eta squared (η2 = Z2/N-1) was calculated to evaluate the magnitude of the differences found between the two samples. Second, Spearman's correlation analyzes were performed in both groups, exploring relationships between variables. Fisher's r-to-Z transformation was applied to allow comparison between different samples (Silver & Dunlap, 1987). Third, logistic regression was applied to evaluate the multivariate association between the two-level dependent variable (cisgender and transgender) and all the variables that were significant in the univariate analysis to evaluate the predictive value of psychological factors to discriminate between cisgender and queer cohorts, using the cisgender population as the reference category.
SPSS Statistics 25.0 (2022) was used for all statistical analyzes and for the matching procedure using the specific tool. The α was set to 0.05 for all the analyzes due to the exploratory nature of the study.
Results
Matching procedure
The TP group was composed of 65 (84.4%) individuals who self-identified as transgender and 12 (15.6%) individuals who self-identified as queer.
The CP group was paired with the experimental group (TP) for age, BMI, biological sex assigned at birth, sexual orientation, and years of education. Due to the matching procedure, the ages (TP = 24.34 ± 5.95, CP = 23.19 ± 5.60; Z = 1.449, p = 0.147), biological sex assigned at birth (TP n = 66(86 %) female, CP n = 61 (79 %), χ2 = 1.123, p = 0.289), BMI (TP = 21.08 ± 3.86, CP = 21.20 ± 3.61; Z = 0.681, p = 0.496), years of education (TP = 12.92 ± 2.90, CP = 13.89 ± 2.71; Z = 1.950, p = 0.051), and sexual orientations (TP: heterosexual n = 50 (65.3 %), bisexual n = 24 (31.2 %), gay/lesbian n = 3 (3.5 %), CP: heterosexual n = 56 (72.7 %), bisexual n = 14 (18.2 %), gay/lesbian n = 7 (9.1 %); χ2 = 4.571, p = 0.102) were all similar between groups.
Comparison analyzes between two group
Given the same current weight and previous weight fluctuations between groups, we found in the TP group significantly greater depressive and eating symptoms (both total score and EAT subscales are highest in TP), the highest tendency towards objectification of one's own body (differences in body shame and appearance control beliefs subscales of OBC), and the highest BWD and PD, even though it does not appear that more physically comparisons are in effect (PACS difference was not significant, as well as body surveillance). See Table 1 for a description of the sample.
Table 1.
Comparison between groups for sociodemographic and clinical profiles.
| TP (n = 77) | CP (n = 77) | Z | p (η2) | |
|---|---|---|---|---|
| BMI maximum | 24.58 (4.66) | 23.13 (4.41) | 1.887 | 0.059 |
| BMI minimum | 18.93 (3.65) | 18.70 (3.35) | 0.445 | 0.657 |
| PACS | 15.18 (5.07) | 14.82 (4.52) | 0.567 | 0.570 |
| PHQ-9 | 13.30 (5.51) | 8.75 (4.50) | 5.056 | < 0.001 (0.17) |
| OBC-BSV | 34.92 (8.12) | 31.73 (9.82) | 1.812 | 0.070 |
| OBC-BSH | 32.25 (10.42) | 27.68 (12.55) | 2.534 | 0.011(0.04) |
| OBC-ACB | 36.45 (8.29) | 33.26 (7.29) | 3.693 | <0.001(0.09) |
| EAT26 Dieting | 12.22 (9.41) | 6.80 (6.67) | 3.979 | < 0.001 (0.10) |
| EAT26 Bulimia | 4.70 (4.77) | 1.49 (2.83) | 4.416 | < 0.001 (13) |
| EAT26 Oral control | 4.62 (5.23) | 2.08 (3.51) | 3.336 | 0.001 (0.07) |
| EAT26 Total | 21.54 (17.52) | 10.38 (11.32) | 4.338 | < 0.001 (0.12) |
| FRS-BWD | 2.35 (1.74) | 1.49 (2.15) | 2.755 | 0.006 (0.05) |
| FRS-PD | −0.69 (3.62) | 0.83 (3.85) | 2.725 | 0.006 (0.05) |
Means and standard deviations (SD) are reported in the table. TP: transgender people; CP: cisgender people; BMI: body mass index; PACS: physical appearance comparison scale; PHQ-9: patient health questionnaire; OBC: objectified body consciousness; BSV: body surveillance; BSH: body shame; ACB: appearance control beliefs; EAT: eating attitudes test; FRS: figure rating scale; BWD: body weight dissatisfaction; PD: perception distortion.
Correlational analyzes
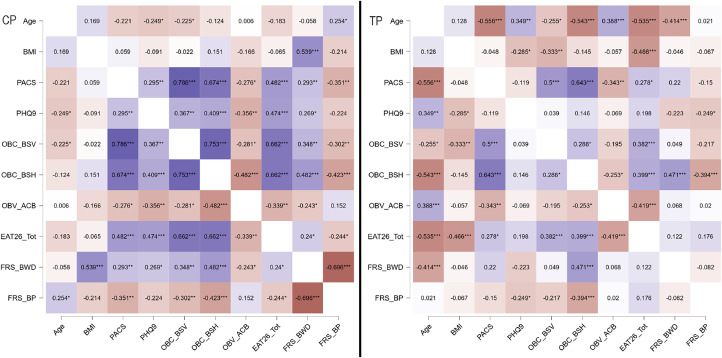
Correlation analyzes were performed to explore the interplay between factors. In the TP group, age has significant negative correlations with physical comparison, objectification, dissatisfaction, and eating concerns. Otherwise, strong positive correlations were found between physical comparisons, objectification, and eating concerns. See Table 2 for correlation comparisons analyzed with Fisher's Z transformation and Fig. 1 for a graphical representation of the correlations.
Table 2.
Comparison between Pearson's correlations with Fisher's Z transformation.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Age | – | |||||||||
| 2 | BMI | 0.146 | – | ||||||||
| 0.074 | |||||||||||
| 3 | PACS | −0.416 | 0.002 | – | |||||||
| <0.001 | 0.982 | ||||||||||
| 4 | PHQ-9 | 0.051 | −0.162 | 0.108 | – | ||||||
| 0.532 | 0.047 | 0.185 | |||||||||
| 5 | OBC-BSV | −0.216 | −0.170 | 0.750 | 0.241 | – | |||||
| 0.008 | 0.038 | <0.001 | 0.003 | ||||||||
| 6 | OBC-BSH | −0.355 | 0.001 | 0.824 | 0.328 | 0.628 | – | ||||
| <0.001 | 0.994 | <0.001 | <0.001 | <0.001 | |||||||
| 7 | OBC-ACB | 0.215 | −0.080 | −0.327 | −0.245 | −0.233 | −0.411 | – | |||
| 0.009 | 0.326 | <0.001 | 0.003 | 0.004 | <0.001 | ||||||
| 8 | EAT26 Total | −0.400 | −0.295 | 0.442 | 0.383 | 0.578 | 0.686 | −0.419 | – | ||
| <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| 9 | FRS-BWD | −0.225 | 0.243 | 0.289 | 0.025 | 0.235 | 0.538 | −0.125 | 0.231 | – | |
| 0.009 | 0.003 | <0.001 | 0.763 | 0.004 | <0.001 | 0.125 | 0.005 | ||||
| 10 | FRS-PD | 0.126 | −0.155 | −0.266 | −0.266 | −0.249 | −0.431 | 0.101 | −0.097 | −0.483 | – |
| 0.132 | 0.064 | 0.002 | 0.002 | 0.003 | <0.001 | 0.226 | 0.246 | <0.001 |
Each box reported r-to-Z transformation, with Z reported in the top row and the p-value reported in the bottom row. If r of the TP group is greater than r of the CP group, the resulting Z is reported with a positive sign, otherwise, Z is reported with a negative sign. In bold are reported the comparison statistically significant. BMI: body mass index; PACS: physical appearance comparison scale; PHQ-9: patient health questionnaire; OBC: objectified body consciousness; BSV: body surveillance; BSH: body shame; ACB: appearance control beliefs; EAT: eating attitudes test; FRS: figure rating scale; BWD: body weight dissatisfaction; PD: perception distortion.
Fig. 1.
Spearman's correlation analyzes were reported as heat maps for TP and CP and each box reported the rho value. Positive correlations are colored in purple, while negative correlations are colored in orange. * p < 0.05, ** p < 0.01, *** p < 0.001. BMI: body mass index; PACS: physical appearance comparison scale; PHQ-9: patient health questionnaire; OBC: objectified body consciousness; BSV: body surveillance; BSH: body shame; ACB: appearance control beliefs; EAT: eating attitudes test; FRS: figure rating scale; BWD: body weight dissatisfaction; PD: perception distortion.
Table 3 shows the multiple binary logistic regression results of being transgender. Significant factors were found: PHQ-9 (OR = 1.299, 95 % CI = 1.14–1.47), OBC-ACB (OR = 1.219, 95 % CI = 1.12–1.33), and EAT26-Bulimia (OR = 1.653, 95 % CI = 1.30–2.11).
Table 3.
Multivariate logistic regression model.
| Variable | OR | p | 95 % CI |
|---|---|---|---|
| PHQ-9 | 1.299 | <0.001 | 1.14–1.47 |
| OBC-BSH | 0.981 | 0.515 | 0.92–1.04 |
| OBC-ACB | 1.219 | <0.001 | 1.12–1.33 |
| EAT26 Dieting | 0.928 | 0.256 | 0.82–1.06 |
| EAT26 Bulimia | 1.653 | <0.001 | 1.30–2.11 |
| EAT26 Oral control | 0.954 | 0.564 | 0.81–1.12 |
| FRS-BWD | 1.183 | 0.233 | 0.90–1.56 |
| FRS-PD | 1.071 | 0.445 | 0.90–1.28 |
PHQ-9: patient health questionnaire; OBC: objectified body consciousness; BSH: body shame; ACB: appearance control beliefs; EAT: eating attitudes test; FRS: figure rating scale; BWD: body weight dissatisfaction; PD: perception distortion.
Discussion
The present study sought to explore specific aspects of the intricate relationship between body image and psychological well-being in transgender individuals. Our data confirmed the presence of higher levels of body weight dissatisfaction and body objectification in transgender people, shedding light on the unique challenges faced as they navigate their gender identity and body image. Even with similar body weight history, transgender participants reported higher levels of body dissatisfaction, body distortion, eating concerns, and eating negative behaviors than cisgender peers (Coelho et al., 2019).
Transgender individuals frequently experience body objectification, manifested through body shame, body surveillance, and appearance control. Body shame, resulting from societal stigmatization and internalized transphobia, leads to negative self-perception and dissatisfaction with one's physical appearance (Brewster et al., 2019). Body surveillance, driven by the need to conform to gender norms, intensifies self-monitoring of body image, often resulting in heightened anxiety and stress (Brewster et al., 2019; Hong et al., 2023). These factors contribute to body weight dissatisfaction, leading to negative psychological outcomes and eating concerns in transgender individuals. The internalization of high levels of body surveillance may contribute to body shame and dissatisfaction when individuals perceive their bodies as not meeting societal ideals (Fitzsimmons-Craft et al., 2015). These findings align with previous research on body image concerns in transgender populations, emphasizing the need for body neutrality (rather than solely relying on body positivity) and psychoeducational interventions to mitigate the effects of internalized appearance norms and social pressure (Heiden-Rootes et al., 2023; Strübel et al., 2020). However, our data only partially confirmed this aspect in our population, perhaps due to the presence of various stages in the gender affirmation process or different aspects that may be evaluated in future studies. Indeed, our transgender individuals show a limited physical comparison and only a tendency toward a significant difference in terms of body surveillance. These findings could align with the literature evidence for participants further along in consolidating their gender identity, as described by gaining a sense of social awareness, self-acceptance, and body satisfaction, reflecting a sense of resilience (McGuire et al., 2016).
Transgender individuals, similar to cisgender gay individuals, have demonstrated a tendency to underestimate their weight (Meneguzzo et al., 2020). Our data revealed elevated rates of heterosexual transgender people, taking into account their affirmed gender, consistent with prior literature (Defreyne et al., 2021). This observation highlights potential connections between gender and sexual orientation in transgender people. Indeed, this phenomenon has been attributed by previous studies to the internalization of LGBTQ+ body ideals, perpetuated through media and community norms and recorded as weight bias (Carper et al., 2010; Paine, 2021). Weight underestimation presents challenges in assessing the true extent of body image concerns among transgender populations, warranting further research to better understand its impact on their mental well-being.
Interestingly, age appears to be a protective factor for transgender individuals in the context of body image and psychological well-being. Older transgender individuals may exhibit improved self-acceptance, self-esteem, and body satisfaction, possibly due to increased resilience and reduced concerns about societal validation (Birkett et al., 2015; Kuper et al., 2018). Age-related coping mechanisms and the passage of time might contribute to a more positive body image experience for older transgender individuals, underlining the need to consider age as a salient factor in intervention strategies, as already reported in the cisgender population (Lacroix et al., 2022; Tiggemann & Lynch, 2001).
Our study corroborates existing evidence showing a higher prevalence of depressive symptoms among transgender populations (Pellicane & Ciesla, 2022). The chronic stress, stigma, and discrimination faced by transgender individuals may contribute to the emergence of depressive symptoms. Additionally, the unique challenges related to gender identity, body image, and societal expectations can lead to the development of eating psychopathology (Duffy et al., 2019; Ferrucci et al., 2022; Jones et al., 2018).
Finally, our findings underscore the relevance of specific elements, such as bulimia, depression, and appearance control beliefs, in the experiences of transgender individuals. Coping with the pressures of transitioning and societal expectations can intensify feelings of inadequacy and trigger maladaptive behaviors, such as binge eating or purging, to manage distress and anxiety (Parker & Harriger, 2020). Moreover, the pursuit of passing as their identified gender can fuel appearance control beliefs in transgender individuals. This obsessive focus on modifying physical attributes to conform to societal norms may exacerbate body dissatisfaction and contribute to the development of mental health issues (Grannis et al., 2023).
Limitations
This study's limitations are the reliance on self-report questionnaires and the absence of psychometric norms or specific questionnaires for the transgender population. Our sample and data did not allow us to evaluate the effects of hormonal treatment or affirmative therapies, and these elements might be taken into consideration in future studies. Moreover, being a cross-sectional study, causality between psychological elements cannot be established with our data. To address these limitations and improve the understanding of transgender individuals' psychological experiences, future research could consider using more diverse and comprehensive methods of data collection, including qualitative approaches and longitudinal study designs. Furthermore, future studies should assess the relationships between various aspects of mental health and elements of body image, aiming to enhance the specificity of interventions for improving the well-being of transgender individuals.
Conclusion
Transgender individuals face elevated levels of body objectification, body weight dissatisfaction, and eating concerns, with age acting as a potential protective factor in mitigating some of these challenges. Weight underestimation further complicates the assessment of body image issues in this population, underscoring the need for continued research. Specific constructs, namely bulimia, depression, and appearance control beliefs, are intricately linked to the transgender experience, necessitating targeted interventions to promote mental well-being and body positivity within this community. By addressing these nuanced factors, healthcare professionals and support networks can create a more affirming and inclusive environment for transgender individuals, fostering improved mental health outcomes and overall well-being.
Ethical approval
The study was conducted according to the Declaration of Helsinki, the National legislation and the local ethics committee approved the protocol. Informed consent was obtained from all participants involved in the study, both to participate and to publish.
Funding
No funding was received for conducting this study.
Availability of data and materials
The data sets used and analyzed during the current study are available from the corresponding author on a reasonable request.
CRediT authorship contribution statement
Paolo Meneguzzo: Conceptualization, Methodology, Investigation, Formal analysis, Writing – review & editing, Project administration. Daniele Zuccaretti: Investigation, Data curation, Writing – review & editing. Elena Tenconi: Conceptualization, Methodology, Resources, Writing – original draft, Project administration. Angela Favaro: Conceptualization, Methodology, Resources, Writing – original draft, Project administration.
Declaration of competing interest
The authors declare no conflict of interest.
Contributor Information
Paolo Meneguzzo, Email: paolo.meneguzzo@unipd.it.
Elena Tenconi, Email: elena.tenconi@unipd.it.
Angela Favaro, Email: angela.favaro@unipd.it.
References
- Anzani A., Lindley L., Tognasso G., Galupo M.P., Prunas A. Being talked to like i was a sex toy, like being transgender was simply for the enjoyment of someone else”: fetishization and sexualization of transgender and nonbinary individuals. Archives of Sexual Behavior. 2021;50(3):897–911. doi: 10.1007/s10508-021-01935-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin B., Ziyadeh N.J., Corliss H.L., Rosario M., Wypij D., Haines J., et al. Sexual orientation disparities in purging and binge eating from early to late adolescence. Journal of Adolescent Health. 2009;45(3):238–245. doi: 10.1016/j.jadohealth.2009.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birkett M., Newcomb M.E., Mustanski B. Does it get better? A longitudinal analysis of psychological distress and victimization in lesbian, gay, bisexual, transgender, and questioning youth. Journal of Adolescent Health. 2015;56(3):280–285. doi: 10.1016/j.jadohealth.2014.10.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewster M.E., Velez B.L., Breslow A.S., Geiger E.F. Unpacking body image concerns and disordered eating for transgender women: The roles of sexual objectification and minority stress. Journal of Counseling Psychology. 2019;66(2):131–142. doi: 10.1037/cou0000333. [DOI] [PubMed] [Google Scholar]
- Carper T.L.M., Negy C., Tantleff-Dunn S. Relations among media influence, body image, eating concerns, and sexual orientation in men: A preliminary investigation. Body Image. 2010;7(4):301–309. doi: 10.1016/j.bodyim.2010.07.002. [DOI] [PubMed] [Google Scholar]
- Cascalheira C.J., Choi N.Y. Transgender dehumanization and mental health: microaggressions, sexual objectification, and shame. Counseling Psychologist. 2023;51(4):532–559. doi: 10.1177/00110000231156161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cash T.F. Body image: Past, present, and future. Body image. 2004;1(1):1–5. doi: 10.1016/S1740-1445(03)00011-1. [DOI] [PubMed] [Google Scholar]
- Coelho J.S., Suen J., Clark B.A., Marshall S.K., Geller J., Lam P.Y. Vol. 21. Current Medicine Group LLC; 2019. Eating disorder diagnoses and symptom presentation in transgender youth: A scoping review; p. 1. (Current psychiatry reports). [DOI] [PubMed] [Google Scholar]
- Comiskey A., Parent M.C., Tebbe E.A. An inhospitable world: Exploring a model of objectification theory with trans women. Psychology of Women Quarterly. 2020;44(1):105–116. doi: 10.1177/0361684319889595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dakanalis A., Timko A.C., Clerici M., Riva G., Carrà G. Objectified body consciousness (OBC) in eating psychopathology: Construct validity, reliability, and measurement invariance of the 24-item OBC scale in clinical and nonclinical adolescent samples. Assessment. 2017;24(2):252–274. doi: 10.1177/1073191115602553. [DOI] [PubMed] [Google Scholar]
- Defreyne J., Elaut E., Den Heijer M., Kreukels B., Fisher A.D., T'Sjoen G. Sexual orientation in transgender individuals: Results from the longitudinal ENIGI study. International Journal of Impotence Research. 2021;33(7):694–702. doi: 10.1038/s41443-020-00402-7. [DOI] [PubMed] [Google Scholar]
- Dotti A., Lazzari R. Validation and reliability of the Italian EAT-26. Eating and Weight Disorders : EWD. 1998;3(4):188–194. doi: 10.1007/BF03340009. [DOI] [PubMed] [Google Scholar]
- Duffy M.E., Henkel K.E., Earnshaw V.A. Transgender clients’ experiences of eating disorder treatment. Journal of LGBT Issues in Counseling. 2016;10(3):136–149. doi: 10.1080/15538605.2016.1177806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffy M.E., Henkel K.E., Joiner T.E. Prevalence of self-injurious thoughts and behaviors in transgender individuals with eating disorders: A national study. Journal of Adolescent Health. 2019;64(4):461–466. doi: 10.1016/j.jadohealth.2018.07.016. [DOI] [PubMed] [Google Scholar]
- Ferrucci K.A., Lapane K.L., Jesdale B.M. Prevalence of diagnosed eating disorders in US transgender adults and youth in insurance claims. International Journal of Eating Disorders. 2022;55(6):801–809. doi: 10.1002/eat.23729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzsimmons-Craft, E.E., Bardone-Cone, A.M., Wonderlich, S.A., Crosby, R.D., Engel, S.G., & Bulik, C.M. (2015). The relationships among social comparisons, body surveillance, and body dissatisfaction in the natural environment. In Behavior therapy (Vol. 46). www.sciencedirect.comwww.elsevier.com/locate/bt. [DOI] [PMC free article] [PubMed]
- Fredrickson B.L., Roberts T.A., barr A., Stewart P., Costanzo K., Fischer L. Objectification theory. Psychology of Women Quarterly. 1997;21 [Google Scholar]
- Garner D.M., Olmsted M.P., Bohr Y., Garfinkel P.E. The eating attitudes test: Psychometric features and clinical correlates. Psychological Medicine. 1982;12(4):871–878. doi: 10.1017/s0033291700049163. [DOI] [PubMed] [Google Scholar]
- Gillen M.M., Markey C.N. Encyclopedia of mental health. 2nd ed. Elsevier Inc; 2016. Body Image and Mental Health; pp. 187–192. [DOI] [Google Scholar]
- Grannis C., Mattson W.I., Leibowitz S.F., Nahata L., Chen D., Strang J.F., et al. Expanding upon the relationship between gender-affirming hormone therapy, neural connectivity, mental health, and body image dissatisfaction. Psychoneuroendocrinology. 2023;156 doi: 10.1016/j.psyneuen.2023.106319. [DOI] [PubMed] [Google Scholar]
- Hartman-Munick S.M., Silverstein S., Guss C.E., Lopez E., Calzo J.P., Gordon A.R. Eating disorder screening and treatment experiences in transgender and gender diverse young adults. Eating Behaviors. 2021;41 doi: 10.1016/j.eatbeh.2021.101517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heiden-Rootes K., Linsenmeyer W., Levine S., Oliveras M., Joseph M. A scoping review of the research literature on eating and body image for transgender and nonbinary adults. Journal of Eating Disorders. 2023;11(1) doi: 10.1186/s40337-023-00828-6. BioMed Central Ltd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong D., Tang C., Barnhart W.R., Cui S., He J. Testing the associations between internalized cisgenderism, self-objectification, body shame, and mental health correlates in the framework of the pantheoretical model of dehumanization: A study in Chinese transgender adults. Body image. 2023;46:62–72. doi: 10.1016/j.bodyim.2023.05.003. [DOI] [PubMed] [Google Scholar]
- Jones B.A., Haycraft E., Bouman W.P., Brewin N., Claes L., Arcelus J. Risk Factors for eating disorder psychopathology within the treatment seeking transgender population: The role of cross-sex hormone treatment. European Eating Disorders Review. 2018;26(2):120–128. doi: 10.1002/erv.2576. [DOI] [PubMed] [Google Scholar]
- Kahalon R., Shnabel N., Becker J.C. Vol. 9. Frontiers Media S.A.; 2018. Experimental studies on state self-objectification: A review and an integrative process model. (Frontiers in psychology). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W.W. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuper L.E., Wright L., Mustanski B. Gender identity development among transgender and gender nonconforming emerging adults: An intersectional approach. International Journal of Transgenderism. 2018;19(4):436–455. doi: 10.1080/15532739.2018.1443869. [DOI] [Google Scholar]
- Lacroix E., Atkinson M.J., Garbett K.M., Diedrichs P.C. One size does not fit all: Trajectories of body image development and their predictors in early adolescence. Development and Psychopathology. 2022;34(1):285–294. doi: 10.1017/S0954579420000917. [DOI] [PubMed] [Google Scholar]
- Mazzotti E., Fassone G., Picardi A., Sagoni E., Ramieri L., Lega I., et al. The patient health questionnaire (PHQ) for the screening of psychiatric disorders: A validation study versus the structured clinical interview for DSM-IV axis I (SCID-I) Italian Journal of Psychopathology. 2003;9(3):235–242. [Google Scholar]
- McClain Z., Peebles R. Body image and eating disorders among lesbian, gay, bisexual, and transgender youth. Pediatric Clinics of North America. 2016;63(6):1079–1090. doi: 10.1016/j.pcl.2016.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire J.K., Doty J.L., Catalpa J.M., Ola C. Body image in transgender young people: Findings from a qualitative, community based study. Body image. 2016;18:96–107. doi: 10.1016/j.bodyim.2016.06.004. [DOI] [PubMed] [Google Scholar]
- Mckinley N.M., Hyde J.S. The objectified body consciousness scale development and validation. Psychology of Women Quarterly. 1996;20 [Google Scholar]
- Meneguzzo P., Collantoni E., Bonello E., Vergine M., Behrens S.C., Tenconi E., et al. The role of sexual orientation in the relationships between body perception, body weight dissatisfaction, physical comparison, and eating psychopathology in the cisgender population. Eating and Weight Disorders. 2020:1–6. doi: 10.1007/s40519-020-01047-7. 0123456789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meneguzzo P., Tenconi E., Collantoni E., Longobardi G., Zappalà A., Vindigni V., et al. The Cyberball task in people after obesity surgery: Preliminary evaluation of cognitive effects of social inclusion and exclusion with a laboratory task. Eating and Weight Disorders. 2021 doi: 10.1007/s40519-021-01297-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mölbert S.C., Thaler A., Streuber S., Black M.J., Karnath H.O., Zipfel S., et al. Investigating body image disturbance in anorexia nervosa using novel biometric figure rating scales: A pilot study. European Eating Disorders Review. 2017;25(6):607–612. doi: 10.1002/erv.2559. [DOI] [PubMed] [Google Scholar]
- Owen-Smith A.A., Gerth J., Sineath R.C., Barzilay J., Becerra-Culqui T.A., Getahun D., et al. Association between gender confirmation treatments and perceived gender congruence, body image satisfaction, and mental health in a cohort of transgender individuals. Journal of Sexual Medicine. 2018;15(4):591–600. doi: 10.1016/j.jsxm.2018.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paine E.A. Fat broken arm syndrome”: Negotiating risk, stigma, and weight bias in LGBTQ healthcare. Social Science and Medicine. 2021;270 doi: 10.1016/j.socscimed.2020.113609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker L.L., Harriger J.A. Eating disorders and disordered eating behaviors in the LGBT population: A review of the literature. Journal of Eating Disorders. 2020;8(1) doi: 10.1186/s40337-020-00327-y. BioMed Central Ltd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pellicane M.J., Ciesla J.A. Vol. 91. Elsevier Inc; 2022. Associations between minority stress, depression, and suicidal ideation and attempts in transgender and gender diverse (TGD) individuals: Systematic review and meta-analysis. (Clinical psychology review). [DOI] [PubMed] [Google Scholar]
- Peterson C.M., Matthews A., Copps-Smith E., Conard L.A. Suicidality, self-harm, and body dissatisfaction in transgender adolescents and emerging adults with gender dysphoria. Suicide and Life-Threatening Behavior. 2017;47(4):475–482. doi: 10.1111/sltb.12289. [DOI] [PubMed] [Google Scholar]
- Richard A., Rohrmann S., Lohse T., Eichholzer M. Is body weight dissatisfaction a predictor of depression independent of body mass index, sex and age? Results of a cross-sectional study. BMC Public Health. 2016;16(1):1–8. doi: 10.1186/s12889-016-3497-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaefer L.M., Thompson J.K. The development and validation of the physical appearance comparison scale-revised (PACS-R) Eating Behaviors. 2014;15(2):209–217. doi: 10.1016/j.eatbeh.2014.01.001. [DOI] [PubMed] [Google Scholar]
- Shagar P.S., Harris N., Boddy J., Donovan C.L. Vol. 34. Cambridge University Press; 2017. The relationship between body image concerns and weight-related behaviours of adolescents and emerging adults: A systematic review; pp. 208–252. (Behaviour change). [DOI] [Google Scholar]
- Silver N.C., Dunlap W.P. Averaging correlation coefficients: Should Fisher's z transformation be used? Journal of Applied Psychology. 1987;72(1):146. [Google Scholar]
- Strübel J., Sabik N., Tylka T. Body image and depressive symptoms among transgender and cisgender adults: Examining a model integrating the tripartite influence model and objectification theory. Body Image. 2020;35:53–62. doi: 10.1016/j.bodyim.2020.08.004. [DOI] [PubMed] [Google Scholar]
- Tabaac A., Perrin P.B., Benotsch E.G. Discrimination, mental health, and body image among transgender and gender-non-binary individuals: Constructing a multiple mediational path model. Journal of Gay and Lesbian Social Services. 2018;30(1):1–16. doi: 10.1080/10538720.2017.1408514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiggemann M., Lynch J.E. Body image across the life span in adult women: The role of self-objectification. Developmental Psychology. 2001;37(2):243–253. doi: 10.1037/0012-1649.37.2.243. [DOI] [PubMed] [Google Scholar]
- Vanderweele T. The use of propensity score methods in psychiatric research. International Journal of Methods in Psychiatric Research. 2006;15(2):95–103. doi: 10.1002/mpr.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witcomb G.L., Bouman W.P., Brewin N., Richards C., Fernandez-Aranda F., Arcelus J. Body image dissatisfaction and eating-related psychopathology in trans individuals: A matched control study. European Eating Disorders Review. 2015;23(4):287–293. doi: 10.1002/erv.2362. [DOI] [PubMed] [Google Scholar]
- Yarborough B.J.H., Leo M.C., Yarborough M.T., Stumbo S., Janoff S.L., Perrin N.A., et al. Improvement in body image, perceived health, and health-related self-efficacy among people with serious mental illness: The stride study. Psychiatric Services. 2016;67(3):296–301. doi: 10.1176/appi.ps.201400535. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data sets used and analyzed during the current study are available from the corresponding author on a reasonable request.