Abstract
Timely initiation of and adherence to antiretroviral therapy (ART) is critical for improving HIV outcomes and reducing HIV transmissibility. Social networks, or the social relationships individuals have with each other, have been linked with positive health outcomes, but less is known about the extent to which social network composition and structure are associated with improved ART adherence among people living with HIV (PLWH). We conducted an ego-centric network study among 828 previously ART-naïve PLWH presenting for ART initiation at 11 clinics in Mbarara, Uganda (rural population) and Gugulethu, South Africa (peri-urban population). We collected social network data using name generator and name interpreter questions. ART adherence was monitored over 12 months using wireless monitors (Wisepill). Our primary outcome of interest was ART adherence during the 12-month follow-up period. We used generalized linear models to estimate the associations between network measures and ART adherence. PLWH at the Uganda site (compared with the South Africa site) were less isolated, had larger social networks, and had more social ties providing sufficient social support; they were also more likely to bridge different social groups whereby not all social ties were connected to each other. In Uganda, social isolation was associated with a 5.5 percentage point reduction in ART adherence (95% confidence interval [CI] −9.95 to −1.13; p = 0.014), while having more same gender social ties was associated with higher ART adherence (b = 0.13, 95% CI 0.02–0.25, p = 0.025). In South Africa, there was no association between social isolation and ART adherence, and having more friendship ties (vs. family ties) was associated with lower ART adherence (b = −2.20, 95% CI −3.56 to −0.84; p = 0.002). Identifying and supporting PLWH who are isolated may facilitate optimal adherence, but understanding how networks differentially affect ART adherence by country context is important.
Keywords: Social networks, HIV/AIDS, Uganda, South Africa, Antiretroviral therapy, Adherence
Highlights
-
•
Social network structure and composition among PLWH are associated with ART adherence.
-
•
Network structure and composition differed among PLWH in Uganda versus South Africa.
-
•
Social isolation was the most important predictor of ART adherence in Uganda.
-
•
Same gender ties were associated with higher ART adherence in Uganda.
-
•
Friendship ties were linked with lower ART adherence in South Africa.
Abbreviations
- ART
antiretroviral therapy
- PLWH
people living with HIV
1. Introduction
Timely initiation of, and adherence to, antiretroviral therapy (ART) is critical for slowing disease progression (Bangsberg et al., 2001); improving health outcomes and survival (Mills et al., 2011; Wood et al., 2003); and, by achieving viral suppression, reducing transmissibility, and helping to achieve the goal of ending the HIV epidemic (Boender et al., 2015; Eisinger et al., 2019; Nachega et al., 2007; Prevention Access Campaign, 2022; United Nations, 2016). Yet people living with HIV (PLWH) face significant barriers to adherence, including poverty, food insecurity, geographic isolation, stigma, and misconceptions about ART (Hlongwa et al., 2022; Katz et al., 2013; Lankowski et al., 2014; Mills et al., 2006; Mukherjee et al., 2006; Siedner et al., 2013; Tsai et al., 2013; Weiser et al., 2014).
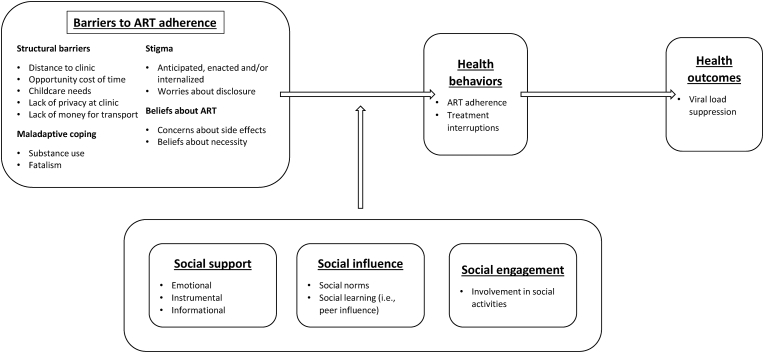
Social networks are generally understood as the complex structure of relationships linking individuals to each other (Marsden, 2000). They can potentially affect ART adherence in several different ways (Brown et al., 2020; Chen et al., 2021). To guide our analytic approach, we adapted the Berkman et al. (2000) framework on social networks and health, to demonstrate the potential relationships between network mechanisms, barriers to ART adherence, and the health outcomes of interest (Fig. 1). First, there is substantial evidence that social support is an important determinant of ART adherence (Campbell et al., 2020; Heestermans et al., 2016; Kagee et al., 2011; Tsai & Bangsberg, 2011). Social networks can serve as conduits for the transmission of different types of social support, including informational support, instrumental support (e.g. financial support, transportation assistance), or emotional support (Berkman et al., 2000; Cohen & Wills, 1985; Pearlin & Aneschensel, 1986; Weiss, 1974). These forms of support can help PLWH overcome barriers to adherence (Ajuna et al., 2021; Anonymous, 2020; Mukherjee et al., 2006; Ware et al., 2009). However, PLWH can only activate these sources of social support (Perry & Pescosolido, 2015) once they have disclosed their serostatus to people in their social networks (Klitzman et al., 2004; Maman et al., 2014; Nam et al., 2008; Smith et al., 2008). Social networks can also affect ART adherence through other channels, including changing behaviors via social influence resulting from having social ties with others living with HIV and who are taking ART (Enriquez et al., 2014; Gusdal et al., 2011; Sasaki et al., 2012); conveying perceptions of normative behaviors around ART adherence (Perkins, Kakuhikire, Baguma, Rasmussen, et al., 2022); and providing opportunities for social engagement which can affect self-efficacy (Mi et al., 2020).
Fig. 1.
Conceptual framework relating social network mechanisms and the barriers to ART adherence.
Social network theory suggests that the effect of social networks on ART adherence will depend on the social network characteristics of PLWH and will operate through social support, influence, social norms and/or social engagement. The social network characteristics of PLWH will depend on whether they disclose their serostatus to their social networks, their sociability, including tendencies to self-isolate and decisions about tie formation or dissolution. Certain network characteristics capture social support provided by social networks, whereas other characteristics proxy for social influence operating through networks. Network measures for social support include: isolation (having no social network), out-degree (network size), density, transitivity (friends being friends with each other), and the number of network ties by characteristic (e.g., number of family ties, friend ties, same-gender ties, ties to other PLWH, ties to PLWH on ART). For example, larger networks may offer more opportunities for informational, emotional and financial support to overcome adherence barriers, such as transportation costs to the health facility. In constraint, network measures capturing social influence including social norms can be represented by: percentage of ties by different characteristics (e.g. percentage of same gender ties, percentage of ties to PLWH), constraint in the network (having redundant ties all associated with each other implying less access to diverse influence), and betweenness (bridging different social groups). The effect of social influence on ART adherence will depend on the attitudes, beliefs and behaviors of the more prominent group within the network (captured by the percentage of ties with various characteristics). Social influence is likely to affect beliefs about ART, as well as stigma. There is little research about the extent to which social network characteristics relate to ART adherence. Understanding how network structure and composition are associated with ART adherence would provide a foundation for designing interventions that target certain network characteristics (e.g., social isolation) to facilitate the maintenance of high ART adherence.
To address these gaps in the literature, we conducted an ego-centric network study among PLWH in rural Uganda and peri-urban South Africa who were ART-naïve at study initiation and followed over 12 months with electronic adherence pill containers. Egocentric networks were used to represent social relationships from the perspective of each individual study participant (ego) and their perceptions of their ties to other individuals (alters) with whom they identified having relationships (Burgette et al., 2021). We expected to observe greater adherence among PLWH whose networks were characterized by less isolation, higher out-degree, higher density, lower constraint and higher betweenness (meaning greater access to different social groups), and more PLWH within those networks.
2. Materials and methods
2.1. Study setting and participants
Study participants were recruited from 11 clinics serving different catchment areas in Uganda and South Africa, two countries with generalized and mature HIV epidemics. We briefly described the study procedures here; a more detailed description has already been published (Haberer et al., 2019). In Uganda, the clinic settings were in Mbarara, a largely rural area approximately 275 km from Kampala where HIV prevalence is approximately 8%. In South Africa, the clinic settings were in the peri-urban settlement of Gugulethu, near Cape Town, where HIV prevalence is approximately 17%. Food and water insecurity are prevalent in both settings (Mushavi et al., 2020; Perkins et al., 2018; Tsai et al., 2016). Recruitment focused on both people initiating ART with asymptomatic early-stage HIV infection (CD4 > 350 cells/μL) as well as people initiating ART at later stages of HIV infection (CD4 < 200 cells/μL). Enrollment occurred from March 2015–September 2016, with follow-up through October 2017. The inclusion criteria for the study were: ART-naïve and initiating ART within 28 days of enrolment, 18 years of age or older, living within 60 km of clinic, and intention to stay in the study catchment area for at least one year. Pregnant participants were less than 35 weeks gestation at enrollment.
2.2. Study procedures and data collection
Study participants were surveyed at baseline (at ART initiation), 6 months, and 12 months, during study visits that took place where participants received routine HIV care. The study provided participants with standard first-line ART (once-daily tenofovir/emtricitabine/efavirenz in a single pill). ART regimen changes were rare but were guided by clinician judgment. At each study visit, participants answered survey questions administered by research assistants on handheld tablets. Surveys were conducted in the participants’ preferred language (English, Runyankole, or Xhosa).
Adherence to ART was monitored in real time using a wireless pill container (Wisepill Technologies, South Africa) (Haberer et al., 2019, Haberer et al., 2017). Each time the device was opened, a date- and time-stamp was recorded and transmitted over the cellular network; each day, the pill container also emitted a signal to confirm to the server its continued functionality (i.e., to confirm that a lack of opening signals represented lack of use rather than a dead battery or other problems with function). Participants were instructed to keep only their ART in the device and to remove pills one at a time.
Surveys included a broad set of questions eliciting socio-demographic characteristics, structural barriers to care (where scale values ranged from 0 to 52, with higher scores representing more barriers [Coetzee & Kagee, 2013]), food insecurity (Household Food Insecurity Access Scale (Tsai et al., 2012)), HIV stigma (where scale values ranged from 1 to 4, with higher scores representing more stigma; adapted from the Berger et al. (2001) HIV Stigma Scale [Jeyaseelan et al., 2013]), HIV disclosure, concerns about ART (measured as high, moderate or low [Horne & Weinman, 1999]), medical mistrust (where scale values ranged from 1 to 4, with higher scores representing more mistrust [LaVeist et al., 2009]), exchange of money for sex, mental and physical health (Medical Outcomes Study-HIV [Stangl et al., 2012]), hazardous alcohol use (3-item consumption subset of the Alcohol Use Disorders Identification Test [AUDIT-C] [Bush et al., 1998]), and cigarette use.
At the baseline study visit, social network data were collected using an egocentric approach: study participants (i.e., egos) were asked to identify social ties (i.e., alters) using name generator questions (Marsden, 1990), and then they were asked to provide data about each of the alters so enumerated. For the name generator, each study participant was asked to list all adults they had personally communicated with in person, by phone, by email, or by short message service (SMS) over the last 6 months. They were prompted to start with the most important person and list all different types of social relations (e.g., family, relatives, friends, acquaintances, neighbors, etc.). For each alter so enumerated, participants were asked: the alter's gender, their relationship with the alter, their level of trust in the alter (measured using a single item scale with values ranging from 1 to 10, with 1 denoting “No trust in this person” and 10 denoting “Complete trust in this person”), frequency of emotional and instrumental support received from the alter (each measured using a 4-point Likert-type scale, with values ranging from “as much as I would like” to “never”), whether the ego thought that the alter knew the ego's HIV status, their perception of the alter's HIV status, and (for alters thought to be living with HIV) the ego's perception of whether the alter was taking ART. To capture alter-alter ties, participants were also asked about the frequency of contacts between each alter-alter pair (with responses included: rarely, sometimes, often, or don't know).
2.3. Statistical analysis
2.3.1. Data cleaning
There were 904 individuals enrolled in the study. Our primary outcome of interest was ART adherence across the 12-month follow-up period. There were 869 study participants with adherence data. By the 12-month follow-up, 64 PLWH had disenrolled, and 3 had missing adherence data. The final analytic sample for this study (used for presenting summary statistics and regression analyses) consisted of 828 study participants (Uganda, N = 449; South Africa, N = 379).
Among the egos, 249 were isolates (i.e., had no named alters); 114 from the Uganda sites and 135 from the South Africa sites. Network science researchers are commonly faced with the task of determining whether egos who named no alters in response to a name generator question are true isolates or whether these observations have resulted from interviewer and/or participant learning that they will answer fewer survey questions if they report no ties (Harling et al., 2018; Paik & Sanchagrin, 2013). We examined the proportion of isolates enumerated by specific research assistants: in Uganda, one research assistant interviewed a significantly higher proportion of isolates compared to the other research assistants; in South Africa, two research assistants had a significantly lower proportion of isolates than the others. In our models, we included research assistant fixed effects to adjust for potential confounding due to differences in interviewer behavior (Harling et al., 2018).
2.3.2. Data analysis
Our primary outcome of interest was ART adherence over the 12-month period, measured as a continuous variable capturing percentage adherence across the 12 months of follow-up data. Adherence was calculated as the number of Wisepill opening events received divided by the number of Wisepill opening events expected for the 12-month follow-up (capped at 100% per day and censored at death). For participants lost to follow-up (defined as no contact despite multiple attempts through 13 months after enrolment), adherence was calculated either until the device stopped transmitting data or until the last scheduled study visit – whichever came first.
Our primary explanatory variables included a broad set of social network structure and composition measures computed from the baseline network data. Among the full set of egos, we generated a binary variable for isolation, taking a value of 1 if the ego nominated no alters and 0 if the ego nominated 1 or more alters. Among the sub-sample of egos who were not isolates, we generated a suite of network variables following Perry et al. (2018). The measures were grouped according to their potential mechanism of action (Table 1). We selected social network variables to identify those that proxy for social support (informational, emotional, or financial) versus social influence. Most of the social support measures would alleviate structural barriers, stigma and maladaptive coping. For example, being socially isolated will remove opportunities to access financial support for transportation to clinic or instrumental support for childcare needs. Social isolation may also aggravate anticipated, enacted or internalized stigma. In contrast, social networks composed of a greater proportion of same gender ties will give more influence to the prevailing norms, attitudes and beliefs of same gender ties and the association is ambiguous. A greater proportion of ties to PLWH or to PLWH on ART will give more influence to those ties’ beliefs about the necessity of ART.
Table 1.
Social network measures, definitions, and expected effect on ART adherence.
| Social network mechanisms | Social network measures | Network measure calculation | Hypothesized mechanisms | Expected association with ART adherence |
|---|---|---|---|---|
| Social support | Isolation (0/1) | Binary measure equal to 0 if ego nominated no alters in name generator and equal to 1 if ego nominated 1 or more alters | Lack of social support (financial support to get to clinic; instrumental support with childcare); Greater stigma (anticipated, enacted and/or internalized); More maladaptive coping | Negative |
| Out-degree (network size) | Total number of alters nominated in name generator question |
Greater social support (financial, emotional, informational); Less stigma |
Positive | |
| Density (%) | Total number of network ties in the ego network/Total number of possible network ties in the ego network | |||
| Transitivity | Ratio of the number of triangles in a network (A- > B; B- > C, and A- > C) divided by the number of triples in a network (A- > B and B- > C) | |||
| Family ties (n) | Total number of alters who are family | |||
| Friend ties (n) | Total number of alters who are friends | |||
| Same gender ties (n) | Total number of alters who are of same gender to ego | |||
| Ties providing sufficient instrumental support (n) | Total number of alters providing “as much as I would like” instrumental support | |||
| Ties providing sufficient emotional support (n) | Total number of alters providing “as much as I would like” emotional support | |||
| Ties disclosed to (n) | Total number of alters to whom ego disclosed serostatus | |||
| Partnered (0/1) | Binary measure for whether ego is partnered | [If partner is supportive]Greater social support (financial, emotional, informational); Less stigma | Ambiguous | |
| Ties to PLWH (n) | Total number of alters whom ego perceives as living with HIV |
Greater social support (financial, emotional, informational); Less stigma; Beliefs about ART (beliefs about necessity, dispelling myths, importance of adherence) |
Positive | |
| Ties to PLWH on ART (n) | Total number of alters who are taking ART (among alters whom ego perceives as living with HIV) | |||
| Social influence | Ties to PLWH (%) | Percentage of alters whom ego perceives as living with HIV = number of alters perceived to be living with HIV/total number of alters | Beliefs about ART: More influence from social norms, beliefs and attitudes among this group (e.g. (beliefs about necessity, dispelling myths, importance of adherence); Less stigma | Positive |
| Ties to PLWH on ART (%) | Percentage of alters who are taking ART (among alters whom ego perceives as living with HIV) = number of alters perceived to be taking ART/total number of alters perceived to be living with HIV | |||
| Family ties (%) | Number of alters who are family/Total number of alters | [Depends on norms within group]Beliefs about ART: More influence from social norms, beliefs and attitudes among this group (e.g. importance of care-seeking); Stigma | Ambiguous | |
| Friend ties (%) | Number of alters who are friends/Total number of alters | |||
| Same gender ties (%) | Number of alters who are same-gender as ego/Total number of alters | |||
| Ties disclosed to (%) | Number of alters to whom ego disclosed serostatus/Total number of alters | |||
| Constraint (more redundant ties) | Given binary network data, the reduced formula for constraint is calculated as the sum across all alters of the squared term for the reciprocal of ego network size (1/N) plus network density | Beliefs about ART: Less access to diverse information, beliefs and attitudes; Stigma[depends on norms within group] | Negative | |
| Betweenness (bridging more nodes) | For each pair of alters nominated by ego, calculate a proportion representing all shortest paths between both alters that go through ego divided by total number of shortest paths between alters; sum these values for all pairs of alters. | Beliefs about ART: Greater flow of information through node; potentially more diversity in information, beliefs and attitudes; Stigma[depends on norms within group] | Positive |
2.3.2.1. Social support
Measures of potential or received social support: out-degree (i.e., number of alters nominated by ego), number/percentage of alters nominated by ego who are family, who are friends, to whom the ego disclosed their HIV status (respectively), whether partnered (yes/no), density (i.e. percentage of all possible social ties of an ego which exist), transitivity (i.e., ego's social ties are also ties with each other), number/percentage of alters nominated by ego providing emotional support “as much as needed”, number/percentage of alters nominated by ego providing instrumental support “as much as needed”, and average level of trust in ties (ranging from 0 for “no trust” to 10 for “complete trust”); number of same gender ties, number of alters nominated by ego thought to be living with HIV, and number of alters nominated by ego thought to be on ART.
2.3.2.2. Social influence
Measures of potential social influence: number of alters thought to be living with HIV as a percentage of total out-degree (i.e. total alters named by ego), number of alters thought to be on ART as a percentage of total out-degree, number of same gender alters nominated by ego as a percentage of total out-degree, constraint (the extent to which a person's network is concentrated with redundant contacts and less evenly distributed (Burt [1992], i.e., “all my friends know each other”), and betweenness (number of times a node is needed for the shortest path between two nodes, i.e., they bridge different social groups [Freeman, 1977]).
We first presented summary statistics for social network measures by country. We conducted bivariate comparisons to assess differences by country using a Wilcoxon rank sum test. We then used generalized linear models with a Gaussian distribution, given that the ART adherence outcome was specified as a continuous variable, to estimate the relationship between ART adherence and social network measures. Since the outcome variable was right-skewed, we used bootstrapping with 1000 replications to obtain bootstrapped standard errors and reported normal-based 95% confidence intervals. We conducted the analyses separately by country. First, we estimated the association between ART adherence and social isolation using the full sample. Then, we restricted the sample to non-isolated individuals. For each analysis, we fitted separate regression models for each network measure, adjusting for covariates following Haberer et al. (2019) including research assistant fixed effects.
2.4. Ethics
All study participants provided written informed consent. The study was approved by the institutional review boards at Mass General Brigham, Mbarara University of Science and Technology, the University of Cape Town, and Western Cape province in South Africa. In Uganda, clearance to conduct the study was obtained from the Uganda National Council of Science and Technology. The University of California at San Francisco relied on Mass General Brigham for IRB approval of the secondary analysis reported in this manuscript.
3. Results
3.1. Characteristics of the sample
Summary characteristics of the sample are shown in Table 2. Median adherence was higher in Uganda compared to South Africa (89% vs. 65%, p < 0.001 based on a Wilcoxon rank sum test). One of the main differences between network structure and composition in Uganda versus South Africa was related to social isolation and network size. Individuals were less likely to be isolated in Uganda compared to South Africa (25% vs. 36%, p = 0.001). They also had larger networks (median out-degree = 12 vs. 7, p < 0.001). Among non-isolates, people in Uganda still reported larger network size compared to those in South Africa (median out-degree = 15 vs. 10, p < 0.001). Networks were less dense in Uganda compared to South Africa (0.71 vs. 0.82, p = 0.001).
Table 2.
Social network characteristics of people living with HIV initiating HIV antiretroviral therapy in Mbarara, Uganda and Gugulethu, South Africa (N = 828).
| Uganda |
South Africa |
P-value | |||
|---|---|---|---|---|---|
| n (%) or Median (IQR) | n (%) or Median (IQR) | ||||
| Full sample | N = 449 | N = 379 | |||
| ART adherence (%) | 89 | (76–97) | 65 | (28-87) | <0.001 |
| Network structure | |||||
| Out-degree (n) | 12 | (0–20) | 7 | (0–10) | <0.001 |
| Isolate | 113 | 25% | 137 | 36% | 0.001 |
| Sample excluding isolates | N = 335 | N = 244 | |||
| Network structure | |||||
| Out-degree | 15 | (11–20) | 10 | (7–12) | <0.001 |
| Density | 0.71 | (0.50–0.93) | 0.82 | (0.57–1.00) | 0.001 |
| Transitivity | 0.83 | (0.66–0.95) | 0.89 | (0.68–1.00) | 0.003 |
| Constraint | 0.23 | (0.19–0.31) | 0.34 | (0.25–0.44) | <0.001 |
| Betweenness | 0.04 | (0.00–0.14) | 0.02 | (0.00–0.08) | <0.001 |
| Network tie characteristics | |||||
| Partnered | 187 | 68% | 72 | 32% | <0.001 |
| Family ties (n) | 8 | (5–12) | 5 | (3–7) | <0.001 |
| Percentage of family ties (%) | 56% | 55% | 0.428 | ||
| Friendship ties (n) | 5 | (3–8) | 3 | (1–5) | <0.001 |
| Percentage of friendship ties (%) | 38% | 37% | 0.408 | ||
| Ties to whom HIV serostatus has been disclosed (n) | 3 | (1–8) | 2 | (1–5) | <0.001 |
| Percentage of ties to whom HIV serostatus has been disclosed (%) | 37% | 36% | 0.271 | ||
| Ties to PLWH (n) | 8 | (3–16) | 8 | (5–10) | 0.141 |
| Percentage of ties with HIV (%) | 58% | 78% | <0.001 | ||
| Ties to PLWH on ART (n) | 1 | (0–3) | 1 | (0–1) | <0.001 |
| Percentage of ties with HIV on ART (%) | 32% | 18% | <0.001 | ||
| Same-gender ties (n) | 7 | (0–11) | 4 | (0–8) | <0.001 |
| Percentage of same-gender ties (%) | 61% | 72% | <0.001 | ||
| Ties giving sufficient emotional supporta (n) | 2 | (0–5) | 0 | (0–2) | <0.001 |
| Percentage giving sufficient emotional support (%) | 18% | 15% | <0.001 | ||
| Ties giving sufficient instrumental supportb (n) | 4 | (0–7) | 0 | (0–2) | <0.001 |
| Percentage giving sufficient instrumental support (%) | 29% | 14% | <0.001 | ||
| Trust in ties | 7 | (6–8) | 7 | (6–9) | 0.005 |
Notes: p-values are associated with comparisons of medians using a Wilcoxon rank sum test. ART, antiretroviral therapy; E-I, external-internal; PLWH, people living with HIV.
For each alter enumerated, this variable takes on a value of 1 if the ego replied “as much as I would like” to questions about how much emotional support they received from the alter, and 0 otherwise. Response options included: “as much as I would like”, “less than I would like”, “much less than I would like”, and “never.”
For each alter enumerated, this variable takes on a value of 1 if the ego replied "as much as I would like" to questions about how much instrumental support they received from the alter, and 0 otherwise. Response options included: "as much as I would like", "less than I would like", "much less than I would like", and "never.
In Uganda, social networks were generally characterized by high levels of trust, with a median trust score of 7 (interquartile range [IQR], 6–8). However, only 18% of social ties were described as providing sufficient emotional support (“as much as needed”) and 29% were described as providing sufficient instrumental support. Similarly, in South Africa, social networks were also characterized by high levels of trust (median 7, IQR 6–9). Yet only 15% of social ties were characterized as providing sufficient emotional support and 14% were characterized as providing sufficient instrumental support.
Among non-isolated individuals, those in Uganda were more likely to be partnered (68% vs. 32%, p < 0.001). Their networks had fewer redundant social ties / lower constraint (i.e., their friends did not all know each other). Given that low constraint typically implies high betweenness, non-isolated individuals in Uganda also had a higher tendency to bridge different social groups. While those in Uganda had more ties of the same gender in their networks (median 7 vs. 4, p < 0.001), the proportion of same gender ties in their network was slightly smaller (61% vs. 72%, p < 0.001).
3.2. Associations between social isolation and ART adherence
In a multivariable regression model fitted to the data from the Uganda sample, social isolation was associated with a 5.5 percentage point reduction in ART adherence (95% confidence interval [CI] −9.95 to −1.13) (Table 3). Compared with the median adherence of 89% in Uganda over the 12-month period, this associational estimate represented a 6.1% relative reduction in adherence; and relative to the standard deviation of 20.3 in this sample, this associational estimate represented an effect size of approximately 0.27 standard deviation units. Positive physical well-being had a positive association with ART adherence (b = 0.54 per point on the MOS-HIV; 95% CI, 0.11–0.97). Severe food insecurity had a negative association with ART adherence (b = −4.63; 95% CI, −9.25 to −0.02) as did exchanging sex for money (b = −10.71; 95% CI, −17.47 to −3.95) and facing a greater number of structural barriers to care (b = −1.77 per point on the structural barriers scale, 95% CI, −3.02 to −0.51). Age was positively associated with ART adherence (b = 0.38 per year, 95% CI, 0.13–0.64) as was being female (b = 4.26, 95% CI, 0.53–7.99). Unexpectedly, ART adherence was also positively associated with medical mistrust (b = 3.10; 95% CI, 0.07–6.13).
Table 3.
Correlates of ART adherence, stratified by study site (Mbarara, Uganda vs. Gugulethu, South Africa).
| Uganda | South Africa | |
|---|---|---|
| Isolate | −5.54* | −1.35 |
| (2.25) | (3.89) | |
| Female | 4.26* | −0.73 |
| (1.91) | (4.41) | |
| Age | 0.38** | 0.60** |
| (0.13) | (0.22) | |
| Number of children | −0.28 | 0.15 |
| (0.44) | (1.36) | |
| No formal education | 2.00 | 29.50** |
| (3.59) | (9.92) | |
| Literate | 1.2 | 14.38 |
| (3.13) | (12.15) | |
| Regular income | 0.67 | 3.98 |
| (2.03) | (4.05) | |
| Employed | 5.54 | 5.52 |
| (3.39) | (3.97) | |
| Exchange money for sex | −10.71** | −42.52*** |
| (3.45) | (8.73) | |
| Structural barrier score | −1.77** | −0.69 |
| (0.64) | (0.38) | |
| Severe food insecurity | −4.63* | −4.56 |
| (2.35) | (4.04) | |
| Stigma – perceived negative attitudes towards HIV | −0.02 | 1.59 |
| (0.56) | (1.07) | |
| Stigma – disclosure concerns | 0.27 | 0.00 |
| (0.49) | (0.81) | |
| Disclosed aside from provider | 6.79 | 15.94* |
| (4.9) | (6.36) | |
| Disclosed outside of household | 0.04 | −2.53 |
| (2.29) | (4.71) | |
| Necessity of ART | −5.08 | 2.82 |
| (2.91) | (5.22) | |
| Medical mistrust | 3.10* | −5.03 |
| (1.54) | (6.00) | |
| Conspiracy | 2.74 | −5.77 |
| (1.71) | (5.66) | |
| Clinic satisfaction | 8.43 | −5.36 |
| (5.15) | (4.75) | |
| Use of medications other than ART | 4.05 | 0.52 |
| (5.57) | (4.83) | |
| Physical well-being | 0.54* | 0.71 |
| (0.22) | (0.41) | |
| Mental well-being | 0.19 | 0.13 |
| (0.12) | (0.24) | |
| Probable depression | 6.00 | −0.23 |
| (3.6) | (5.09) | |
| Cigarette use | −3.23 | −7.87 |
| (3.24) | (4.28) | |
| Constant | 4.82 | 23.26 |
| (23.41) | (45.78) | |
| Observations | 430 | 340 |
Note: Table displays estimated regression coefficients (with bootstrapped standard errors in parentheses) from two multivariable generalized linear models with ART adherence specified as a continuous outcome variable, with research assistant fixed effects. The estimated coefficient can be interpreted in terms of percentage point differences in adherence associated with the covariate. ART, antiretroviral therapy. *p < 0.05; **p < 0.01; ***p < 0.001.
In a multivariable regression model fitted to the data from South Africa, social isolation did not have a statistically significant association with ART adherence (b = −1.35; 95% CI, −8.99 to 6.28). Age was positively associated with ART adherence (b = 0.60 per year; 95% CI, 0.16–1.04), as was HIV serostatus disclosure to anyone (b = 15.94; 95% CI, 3.47–28.42). Exchanging sex for money was negatively associated with ART adherence (b = −42.52; 95% CI, −59.63 to −25.42). Having no formal education was positively associated with ART adherence (b = 29.50, 95% CI, 10.07–48.94).
3.3. Associations between social network structure/composition and ART adherence, among non-isolates
Among non-isolates in Uganda, the only social network measure associated with ART adherence was the percentage of same gender ties in the social network: a 1 percentage point increase in the percentage of same gender ties in the network was associated with a 0.13 percentage point increase in ART adherence (95% CI 0.02–0.25) (Table 4). Other measures of social network structure and composition were not associated with ART adherence in Uganda (among non-isolates).
Table 4.
Social network correlates of ART adherence, among non-isolates, stratified by study site (Mbarara, Uganda vs. Gugulethu, South Africa).
| Uganda | South Africa | |
|---|---|---|
| Measures of social support | ||
| Network size and tie characteristics | ||
| Out-degree | 0.27 | 0.19 |
| (0.31) | (0.53) | |
| Family ties | 0.18 | 1.21 |
| (0.26) | (0.72) | |
| Friendship ties | 0.05 | −2.20** |
| (0.27) | (0.66) | |
| Ties to whom HIV serostatus has been disclosed | −0.03 | 0.21 |
| (0.19) | (0.64) | |
| Same-gender ties | 0.50 | −0.54 |
| (0.33) | (0.62) | |
| Ties to PLWH | 0.15 | 0.54 |
| (0.16) | (0.53) | |
| Ties to HIV on ART | −0.13 | −1.16 |
| (0.68) | (1.62) | |
| Partnered | 1.27 | 2.47 |
| (2.60) | (4.83) | |
| Tie strength | ||
| Trust in ties | 0.03 | 0.40 |
| (0.73) | (1.10) | |
| Emotional support | ||
| Ties providing sufficient emotional support | 0.22 | 0.71 |
| (0.30) | (0.88) | |
| Instrumental support | ||
| Ties providing sufficient instrumental support | 0.17 | 0.33 |
| (0.21) | (0.91) | |
| Network structure | ||
| Density | −0.07 | 0.09 |
| (0.06) | (0.08) | |
| Transitivity | −0.07 | 0.09 |
| (0.06) | (0.08) | |
| Measures of social influence | ||
| Percentage of family ties | −0.004 | 0.11 |
| (0.05) | (0.09) | |
| Percentage of friendship ties | −0.01 | −0.24** |
| (0.05) | (0.08) | |
| Percentage of ties to whom HIV serostatus has been disclosed | −0.02 | 0.03 |
| (0.04) | (0.06) | |
| Percentage of same-gender ties | 0.13* | −0.20 |
| (0.06) | (0.11) | |
| Percentage of ties to PLWH | 0.01 | 0.08 |
| (0.03) | (0.07) | |
| Percentage of ties to PLWH on ART | −0.01 | −0.08 |
| (0.04) | (0.10) | |
| Constraint | −0.19 | −0.10 |
| (0.16) | (0.13) | |
| Betweenness | 5.42 | −6.78 |
| (5.64) | (17.80) | |
Note: Table displays estimated regression coefficients (with bootstrapped standard errors in parentheses) from 42 separate generalized linear regression models fitted to the subsample of non-isolates, stratified by study site, specifying ART adherence as a continuous outcome variable. Each row represents the estimated regression coefficient for the specified network measure, adjusted for the following covariates: sex, age, number of biological children, education, literacy, regular income, employment, exchange of money for sex, structural barrier score, severe food insecurity, perceived negative attitudes towards HIV, disclosure concerns, disclosure of serostatus to anyone aside from healthcare provider, disclosure of serostatus to anyone outside of household, necessity of ART, medical mistrust, conspiracy score, clinic satisfaction, use of medications other than ART, physical well-being, mental well-being, probable depression, cigarette use, and research assistant fixed effects. The estimated coefficient can be interpreted in terms of the percentage point difference in adherence associated with the covariate. ART, antiretroviral therapy; E-I, external-internal; PLWH, people living with HIV. *p < 0.05; **p < 0.01; ***p < 0.001.
Among non-isolates in South Africa, each additional friend tie was associated with a 2.20 percentage point lower ART adherence (95% CI −3.56 to −0.84). A 1 percentage point increase in the percentage of friend ties was associated with a 0.24 percentage point lower ART adherence (95% CI −0.40 to −0.08). Two other social network variables were weakly associated (p < 0.10) with ART adherence: having a higher percentage of same-gender ties (b = −0.20; 95% CI −0.40 to 0.01; p = 0.07) and betweenness (b = −3.05; 95% CI −6.25 to 0.15; p = 0.062).
4. Discussion
In this multi-site cohort study of PLWH in rural Uganda and peri-urban South Africa, we collected ego-centric network data to understand how social network characteristics were related to ART adherence and to understand whether differences in network structure and composition existed by country. One of the main differences that we identified was that PLWH in Uganda were less likely to be socially isolated compared to those in South Africa. Social isolation was the largest network-related predictor of ART adherence in Uganda. However, it had no association with adherence in South Africa. We also identified other network differences by country: PLWH in Uganda had larger social networks, were more likely to be partnered, and had a greater number of social ties providing self-perceived sufficient emotional and instrumental support. They were also more likely to bridge different groups in their networks, which also meant they had more evenly distributed networks (i.e., lower constraint from having fewer redundant ties all associated with each other) compared to PLWH in South Africa. Only certain network characteristics among non-isolated individuals were associated with ART adherence. In Uganda, having a greater percentage of social ties of the same gender was associated with higher ART adherence. In South Africa, having more social ties who were friends was negatively associated with ART adherence. Unexpectedly, there was no association between ART adherence and having social ties to PLWH or those taking ART.
Our primary finding on the importance of social isolation being associated with lower ART adherence in Uganda is consistent with the evidence on the role of social support in helping PLWH achieve high ART adherence (Campbell et al., 2020; Heestermans et al., 2016; Kagee et al., 2011; Katz et al., 2013). While there were fewer isolates in Uganda than in South Africa, the contribution of social isolation for ART adherence was much more significant. The SEARCH study, conducted in Uganda and Kenya, found similar results: PLWH in Uganda with low social connectedness were less likely to be on ART and less likely to be virally suppressed, but the same pattern was not observed among PLWH in Kenya (Chen et al., 2021). Having no social network meant individuals could lose access to critical forms of social support, including emotional, financial, informational and appraisal support, which are important in overcoming barriers to adherence (Ajuna et al., 2021; Mukherjee et al., 2006; Ware et al., 2009; Ware et al., 2020). Research in this same geographic location in Uganda confirmed that PLWH in this setting relied heavily on bonding networks (family and friends) to overcome patient-, medication-, and structural-related barriers to ART adherence (Ajuna et al., 2021). High rates of isolation among PLWH have been tied to several factors, including anticipated and enacted stigma, lower physical and mental health, and lower sociability (Ashaba et al., 2017; Takada et al., 2014; Takada et al., 2019). The absence of a relationship between social isolation and ART adherence in South Africa could be due to social networks in South Africa offering relatively less social support. This interpretation would be consistent with our findings related to smaller network size and less social support provided by network ties in South Africa. It could also be due to other adherence barriers being more prominent in South Africa and social support being insufficient to overcome them.
Among non-isolates, the network measures associated with ART adherence were different by country. In Uganda, having a social network composed of a greater percentage of same-gender ties was linked to higher ART adherence, even if those ties did not have HIV. The findings suggest that individuals might be most influenced by the prevailing attitudes, beliefs and behaviors of individuals of the same gender in their networks. For women living with HIV in our study, this positive association may partly be explained by the higher adherence rate among women compared to men. This finding contrasts with recent findings in Tanzania for related HIV behaviors (i.e. HIV testing), where having more women in one's network contributed to higher testing among men (Yamanis et al., 2017). It may be that having a network mainly composed of same-gender ties encourages care-seeking and adherence because individuals are more likely to access social support from others with similar experiences and circumstances by gender.
At the same time, we found no association between ART adherence and having ties to PLWH or PLWH on ART. This null finding is not inconsistent with what is known about the relative importance of perceived behavioral and attitudinal norms as compared to actual behaviors in affecting individuals’ own behavior and attitudes (Perkins, Kakuhikire, Baguma, Rasmussen, et al., 2022; Perkins, Kakuhikire, Baguma, Rasmussen, et al., 2022; Tsai et al., 2021). These studies have found evidence that perceptions of normative behaviors may be different from actual behaviors; these differences could explain the relatively low perception of ART use among social ties with HIV and, in turn, the absence of an association with ART adherence. In the SEARCH study, younger PLWH had higher adherence if they had a tie to a younger same-age PLWH initiating ART at the same time, but adherence was not associated with having a tie to an older youth who had initiated ART at the same time (Brown et al., 2020).
Overall, these findings suggest it is important to have social ties who are similar in characteristics (such as gender) to either exert social influence and/or provide social support for ART adherence. In South Africa, the negative association between ART adherence and the number or percentage of friendship ties suggested that social influence and/or social support from friends was different from that provided by family. There may be a greater reluctance to disclose serostatus to friends versus family, and the perceptions of normative behaviors among friends may be more influential. Overall, these differences in findings across both settings highlighted that network composition could have very different implications for behaviors such as ART adherence, depending on the underlying context of how individuals relate to and draw on resources from their networks.
The between-country differences that we identified—in terms of isolation, network size, and number of ties providing self-perceived sufficient social support—may have been partly due to differences in urbanicity, in addition to the lasting consequences of apartheid and colonization. Study participants in Uganda came from a more rural area while those in South Africa were from a peri-urban location. Evidence from South Africa has shown that PLWH face significant anticipated stigma, and disclosure of their serostatus within their social circles results in greater social support for some PLWH but greater isolation for others (Gilbert & Walker, 2010). Yet, even in Uganda, PLWH in our study reported that only a small portion of their social ties were providing sufficient emotional or instrumental support. Social support has been a crucial determinant of high ART adherence (Campbell et al., 2020; Heestermans et al., 2016; Kagee et al., 2011; Katz et al., 2013). Our findings suggest that, across both contexts, PLWH could benefit from receiving more social support from their networks, including support to achieve greater engagement in care and high ART adherence.
Our study's findings imply not only that we should focus directly on alleviating the barriers to ART adherence but also that we can address them through interventions via individuals' social networks. Given the importance of social isolation in contributing to sub-optimal ART adherence in Uganda, one policy recommendation drawing from network interventions is to focus on adding nodes to isolated individuals' networks (Valente, 2012). This approach could be done by linking PLWH to peer support groups, as has been shown to be effective in several contexts (Cataldo et al., 2017; Foster et al., 2017; Phiri et al., 2017; Sam-Agudu et al., 2014), or by assisting PLWH to activate existing network ties (Perry & Pescosolido, 2015). Policy recommendations could also include administering screeners when initiating individuals on ART to identify those who are socially isolated and targeting them for additional peer support. Given our findings related to network composition, policy recommendations would also include counseling PLWH initiating ART to specifically engage with certain social ties (same-gender ties in Uganda and non-friendship ties in South Africa) given these ties' potential beneficial influence on adherence.
Interpretation of our findings is subject to several limitations. First, the study was based on ego-centric network data, so our measures are based on ego perceptions of alter characteristics (e.g., HIV status and ART use) rather than confirmed conditions or behaviors. This aspect of the egocentric design could have biased many of our estimates toward the null. A sociocentric design (Takada et al., 2019) could have mitigated this limitation but was infeasible given the large catchment area of the HIV clinics and our inability to characterize whole-population networks across such a large expanse of geography. Furthermore, there may be concern that social network measures are not independent of each other (i.e. an ego with a more dense network may also have more constraint in their network or may have disclosed their serostatus to more alters). We included different measures to distinguish between potential mechanisms of action. Second, with network data there are typically concerns that measures of social isolation may instead be capturing interviewer or study participant learning (i.e., to avoid having to administer or answer additional survey questions). We conducted additional quality assurance checks with research assistants to confirm that they felt study participants were reporting their social networks correctly. We included research assistant fixed effects to remove potential biases from the interviewer side. We also used social network data from the baseline survey where study participants had no opportunities to adjust responses based on learning from prior surveys. Third, the use of the Wisepill technology provided objective adherence monitoring data. However, we may have misclassified non-adherence with non-use of the device (e.g., due to technical malfunction and problems with cellular transmission). Nonetheless, adherence data were available for 97% of participant-days, and no technical challenges occurred for 90% of participants (Haberer et al., 2019).
5. Conclusion
In conclusion, we found that social isolation was the most significant correlate of ART adherence among PLWH in Uganda though there was no such association among PLWH in South Africa. These findings suggest that it is critical to identify and support PLWH who are isolated in Uganda to facilitate optimal adherence. Our findings also highlight how different the social context is for PLWH in Uganda compared to South Africa and that there were significant differences for which network characteristics were associated with ART adherence by context. If we are to engage social networks to support optimal ART adherence, it is critical to understand how these networks affect ART adherence by context and social networks’ relative importance for ART adherence.
Funding
This study was supported by the Bill and Melinda Gates Foundation (OPP1056051) and the U.S. National Institutes of Health (K01HD105521, K24MH114732, R01MH113494). The funding sources had no involvement in the study design, collection and analysis of the data, or decision to submit for publication.
Declaration of interests
ACT reports receiving a financial honorarium from Elsevier, Inc. for his work as Co-Editor in Chief of the Elsevier-owned journal SSM-Mental Health. The other authors have no conflicts of interest to declare.
Ethics statement
All study participants provided written informed consent. The study was approved by the institutional review boards at Mass General Brigham, Mbarara University of Science and Technology, the University of Cape Town, and Western Cape province in South Africa. In Uganda, clearance to conduct the study was obtained from the Uganda National Council of Science and Technology. The University of California at San Francisco relied on Mass General Brigham for IRB approval of the secondary analysis reported in this manuscript.
CRediT authorship contribution statement
Alison B. Comfort: Formal analysis, Methodology, Writing – original draft. Stephen Asiimwe: Conceptualization, Funding acquisition, Project administration, Writing – review & editing. Gideon Amaniyre: Conceptualization, Funding acquisition, Project administration, Writing – review & editing. Catherine Orrell: Conceptualization, Funding acquisition, Project administration, Writing – review & editing. James Moody: Methodology, Writing – review & editing. Nicholas Musinguzi: Data curation, Writing – review & editing. Mwebesa Bosco Bwana: Conceptualization, Funding acquisition, Project administration, Writing – review & editing. David R. Bangsberg: Conceptualization, Funding acquisition, Writing – review & editing. Jessica E. Haberer: Funding acquisition, Project administration, Supervision, Writing – review & editing. Alexander C. Tsai: Conceptualization, Funding acquisition, Methodology, Writing – review & editing.
Acknowledgements
We would like to thank the study participants for their valuable time and commitment to participating in this study. We are also grateful to the research team for study management and data collection: research assistants, Nomakhaya April, Alienah Mpahleni, Vivie Situlo, Speech Mzamo, Nomsa Ngwenya, Khosi Tshangela, Regina Panda, Teboho Linda, Christine Atwiine, Sheila Moonight, Edna Tindimwebwa, Nicholas Mugisha, Peace Atwogeire, Vian Namana, Catherine Kyampaire, and Gabriel Nuwagaba; program managers, Annet Kembabazi, Stephen Mugisha, Victoria Nanfuka, Anna Cross, Nicky Kelly, Daphne Moralie, and Kate Bell; data managers, Dolphina Cogill, Justus Ashaba, Zoleka Xapa, Mathias Orimwesiga, Elly Tuhanamagyezi, and Catherine Kyampaire; laboratory managers, Don Bosco Mpanga, Leonia Kyarisima, and Simone Kigozi; and drivers, Edgar October, Silver Mugisha, and Ibrahim Kiviiri. We would like to thank participants of the Bixby Early Career Investigators Works in Progress seminar and the Sunbelt Conference 2022 for helpful comments and suggestions.
Contributor Information
Alison B. Comfort, Email: alison.comfort@ucsf.edu.
Stephen Asiimwe, Email: sasiimwe@must.ac.ug.
Gideon Amaniyre, Email: gideon.amanyire@gmail.com.
Catherine Orrell, Email: catherine.orrell@hiv-research.org.za.
James Moody, Email: jmoody77@soc.duke.edu.
Nicholas Musinguzi, Email: nmusinguzi@gmail.com.
David R. Bangsberg, Email: david.b@vinuni.edu.vn.
Jessica E. Haberer, Email: jhaberer@mgh.harvard.edu.
Alexander C. Tsai, Email: actsai@mgh.harvard.edu.
for the META Study Investigators:
Jessica E. Haberer, Catherine Orrell, Norma Ware, Mwebesa Bosco Bwana, Stephen Asiimwe, Gideon Amaniyre, Elioda Tumwesigye, and David R. Bangsberg
Data availability
Data will be made available on request.
References
- Ajuna N., Tumusiime B., Amanya J., Awori S., Rukundo G.Z., Asiimwe J.B. Social networks and barriers to ART adherence among young adults (18-24 years) living with HIV at selected primary health facilities of south-western Uganda: A qualitative study. HIV AIDS (Auckl) 2021;13:939–958. doi: 10.2147/hiv.S328643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anonymous . 2020. Details omitted for double-blind reviewing. [Google Scholar]
- Ashaba S., Kaida A., Coleman J.N., Burns B.F., Dunkley E., O'Neil K., Kastner J., Sanyu N., Akatukwasa C., Bangsberg D.R., Matthews L.T., Psaros C. Psychosocial challenges facing women living with HIV during the perinatal period in rural Uganda. PLoS One. 2017;12(5) doi: 10.1371/journal.pone.0176256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bangsberg D.R., Perry S., Charlebois E.D., Clark R.A., Roberston M., Zolopa A.R., Moss A. Non-adherence to highly active antiretroviral therapy predicts progression to AIDS. AIDS. 2001;15(9):1181–1183. doi: 10.1097/00002030-200106150-00015. [DOI] [PubMed] [Google Scholar]
- Berger B.E., Ferrans C.E., Lashley F.R. Measuring stigma in people with HIV: Psychometric assessment of the HIV stigma scale. Research in Nursing & Health. 2001;24(6):518–529. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- Berkman L.F., Glass T., Brissette I., Seeman T.E. From social integration to health: Durkheim in the new millennium. Social Science & Medicine. 2000;51(6):843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Boender T.S., Sigaloff K.C.E., McMahon J.H., Kiertiburanakul S., Jordan M.R., Barcarolo J., Ford N., Rinke de Wit T.F., Bertagnolio S. Long-term virological outcomes of first-line antiretroviral therapy for HIV-1 in low- and middle-income countries: A systematic review and meta-analysis. Clinical Infectious Diseases. 2015;61(9):1453–1461. doi: 10.1093/cid/civ556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown L.B., Balzer L.B., Kabami J., Kwarisiima D., Sang N., Ayieko J., Chen Y., Chamie G., Charlebois E.D., Camlin C.S., Cohen C.R., Bukusi E., Kamya M.R., Moody J., Havlir D.V., Petersen M.L. The influence of social networks on antiretroviral therapy initiation among HIV-infected antiretroviral therapy-I youth in rural Kenya and Uganda. Journal of Acquired Immune Deficiency Syndromes. 2020;83(1):9–15. doi: 10.1097/qai.0000000000002199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgette J.M., Rankine J., Culyba A.J., Chu K.H., Carley K.M. Best practices for modeling egocentric social network data and health outcomes. Herd. 2021;14(4):18–34. doi: 10.1177/19375867211013772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt R.S. Harvard University Press; 1992. Structural holes: The social structure of competition. [Google Scholar]
- Bush K., Kivlahan D.R., McDonell M.B., Fihn S.D., Bradley K.A. The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Ambulatory care quality improvement Project (ACQUIP). Alcohol use Disorders identification test. Archives of Internal Medicine. 1998;158(16):1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- Campbell L., Masquillier C., Thunnissen E., Ariyo E., Tabana H., Sematlane N., Delport A., Dube L.T., Knight L., Flechner T.K., Wouters E. Social and structural determinants of household support for ART adherence in low- and middle-income countries: A systematic review. International Journal of Environmental Research and Public Health. 2020;17(11) doi: 10.3390/ijerph17113808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cataldo F., Sam-Agudu N.A., Phiri S., Shumba B., Cornelius L.J., Foster G. The roles of expert mothers engaged in prevention of mother-to-child transmission (PMTCT) programs: A commentary on the INSPIRE studies in Malawi, Nigeria, and Zimbabwe. Journal of Acquired Immune Deficiency Syndromes. 2017;75(Suppl 2):S224–s232. doi: 10.1097/qai.0000000000001375. [DOI] [PubMed] [Google Scholar]
- Chen Y.T., Brown L., Chamie G., Kwarisiima D., Ayieko J., Kabami J., Charlebois E., Clark T., Kamya M., Havlir D.V., Petersen M.L., Balzer L.B. Social networks and HIV care outcomes in rural Kenya and Uganda. Epidemiology. 2021;32(4):551–559. doi: 10.1097/ede.0000000000001352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coetzee B., Kagee A. The development of an inventory to assess the structural barriers to clinic attendance and pill-taking amongst users of antiretroviral therapy. AIDS and Behavior. 2013;17(1):319–328. doi: 10.1007/s10461-012-0374-z. [DOI] [PubMed] [Google Scholar]
- Cohen S., Wills T.A. Stress, social support, and the buffering hypothesis. Psychological Bulletin. 1985;98(2):310–357. doi: 10.1037/0033-2909.98.2.310. [DOI] [PubMed] [Google Scholar]
- Eisinger R.W., Dieffenbach C.W., Fauci A.S. HIV viral load and transmissibility of HIV infection: Undetectable equals untransmittable. JAMA. 2019;321(5):451–452. doi: 10.1001/jama.2018.21167. [DOI] [PubMed] [Google Scholar]
- Enriquez M., Cheng A.-L., Banderas J., Farnan R., Chertoff K., Hayes D., Ortego G., Moreno J., Peterson J., McKinsey D. A peer-led HIV medication adherence intervention targeting adults linked to medical care but without a suppressed viral load. Journal of the International Association of Physicians in AIDS Care. 2014;14(5):441–448. doi: 10.1177/2325957414558301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster G., Orne-Gliemann J., Font H., Kangwende A., Magezi V., Sengai T., Rusakaniko S., Shumba B., Zambezi P., Maphosa T. Impact of facility-based mother support groups on retention in care and PMTCT outcomes in rural Zimbabwe: The EPAZ cluster-randomized controlled trial. Journal of Acquired Immune Deficiency Syndromes. 2017;75(Suppl 2):S207–s215. doi: 10.1097/qai.0000000000001360. [DOI] [PubMed] [Google Scholar]
- Freeman L.C. A set of measures of centrality based on betweenness. Sociometry. 1977;40(1):35–41. doi: 10.2307/3033543. [DOI] [Google Scholar]
- Gilbert L., Walker L. ‘My biggest fear was that people would reject me once they knew my status…’: Stigma as experienced by patients in an HIV/AIDS clinic in johannesburg, South Africa. Health and Social Care in the Community. 2010;18(2):139–146. doi: 10.1111/j.1365-2524.2009.00881.x. [DOI] [PubMed] [Google Scholar]
- Gusdal A.K., Obua C., Andualem T., Wahlström R., Chalker J., Fochsen G., on behalf of the, I.-I. A. A. p Peer counselors' role in supporting patients' adherence to ART in Ethiopia and Uganda. AIDS Care. 2011;23(6):657–662. doi: 10.1080/09540121.2010.532531. [DOI] [PubMed] [Google Scholar]
- Haberer J.E., Musinguzi N., Tsai A.C., Boum 2nd Y., Bwana B.M., Muzoora C., Hunt P.W., Martin J.N., Bangsberg D.R. Real-time electronic adherence monitoring plus follow-up improves adherence compared with standard electronic adherence monitoring. AIDS. 2017;31(1):169–171. doi: 10.1097/QAD.0000000000001310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haberer J.E., Bwana B.M., Orrell C., Asiimwe S., Amanyire G., Musinguzi N.…Bangsberg D.R. ART adherence and viral suppression are high among most non-pregnant individuals with early-stage, asymptomatic HIV infection: an observational study from Uganda and South Africa. Journal of the International AIDS Society. 2019;22 doi: 10.1002/jia2.25232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harling G., Perkins J.M., Gómez-Olivé F.X., Morris K., Wagner R.G., Montana L., Kabudula C.W., Bärnighausen T., Kahn K., Berkman L. Interviewer-driven variability in social network reporting: Results from health and aging in Africa: A longitudinal study of an INDEPTH community (HAALSI) in South Africa. Field Methods. 2018;30(2):140–154. doi: 10.1177/1525822x18769498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heestermans T., Browne J.L., Aitken S.C., Vervoort S.C., Klipstein-Grobusch K. Determinants of adherence to antiretroviral therapy among HIV-positive adults in sub-saharan Africa: A systematic review. BMJ Global Health. 2016;1(4) doi: 10.1136/bmjgh-2016-000125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hlongwa M., Jama N.A., Mehlomakulu V., Pass D., Basera W., Nicol E. Barriers and facilitating factors to HIV treatment among men in a high-HIV-burdened district in KwaZulu-natal, South Africa: A qualitative study. American Journal of Men's Health. 2022;16(5) doi: 10.1177/15579883221120987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horne R., Weinman J. Patients' beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. Journal of Psychosomatic Research. 1999;47(6):555–567. doi: 10.1016/s0022-3999(99)00057-4. [DOI] [PubMed] [Google Scholar]
- Jeyaseelan L., Kumar S., Mohanraj R., Rebekah G., Rao D., Manhart L.E. Assessing HIV/AIDS stigma in south India: Validation and abridgement of the berger HIV stigma scale. AIDS and Behavior. 2013;17(1):434–443. doi: 10.1007/s10461-011-0128-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kagee A., Remien R.H., Berkman A., Hoffman S., Campos L., Swartz L. Structural barriers to ART adherence in Southern Africa: Challenges and potential ways forward. Global Public Health. 2011;6(1):83–97. doi: 10.1080/17441691003796387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz I.T., Ryu A.E., Onuegbu A.G., Psaros C., Weiser S.D., Bangsberg D.R., Tsai A.C. Impact of HIV-related stigma on treatment adherence: Systematic review and meta-synthesis. Journal of the International AIDS Society. 2013;16(3 Suppl 2):18640. doi: 10.7448/ias.16.3.18640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klitzman R.L., Kirshenbaum S.B., Dodge B., Remien R.H., Ehrhardt A.A., Johnson M.O., Kittel L.E., Daya S., Morin S.F., Kelly J., Lightfoot M., Rotheram-Borus M.J. Intricacies and inter-relationships between HIV disclosure and HAART: A qualitative study. AIDS Care. 2004;16(5):628–640. doi: 10.1080/09540120410001716423. [DOI] [PubMed] [Google Scholar]
- Lankowski A.J., Siedner M.J., Bangsberg D.R., Tsai A.C. Impact of geographic and transportation-related barriers on HIV outcomes in sub-saharan Africa: A systematic review. AIDS and Behavior. 2014;18(7):1199–1223. doi: 10.1007/s10461-014-0729-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaVeist T.A., Isaac L.A., Williams K.P. Mistrust of health care organizations is associated with underutilization of health services. Health Services Research. 2009;44(6):2093–2105. doi: 10.1111/j.1475-6773.2009.01017.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maman S., van Rooyen H., Groves A.K. HIV status disclosure to families for social support in South Africa (NIMH Project Accept/HPTN 043) AIDS Care. 2014;26(2):226–232. doi: 10.1080/09540121.2013.819400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsden P.V. Network data and measurement. Annual Review of Sociology. 1990;16(1):435–463. doi: 10.1146/annurev.so.16.080190.002251. [DOI] [Google Scholar]
- Marsden P. In: Encyclopedia of sociology. Macmillan reference USA. Borgatta E.F., Montgomery R.J., editors. 2000. Social networks. [Google Scholar]
- Mi T., Li X., Zhou G., Qiao S., Shen Z., Zhou Y. HIV disclosure to family members and medication adherence: Role of social support and self-efficacy. AIDS and Behavior. 2020;24(1):45–54. doi: 10.1007/s10461-019-02456-1. [DOI] [PubMed] [Google Scholar]
- Mills E.J., Bakanda C., Birungi J., Chan K., Ford N., Cooper C.L., Nachega J.B., Dybul M., Hogg R.S. Life expectancy of persons receiving combination antiretroviral therapy in low-income countries: A cohort analysis from Uganda. Annals of Internal Medicine. 2011;155(4):209–216. doi: 10.7326/0003-4819-155-4-201108160-00358. [DOI] [PubMed] [Google Scholar]
- Mills E.J., Nachega J.B., Bangsberg D.R., Singh S., Rachlis B., Wu P., Wilson K., Buchan I., Gill C.J., Cooper C. Adherence to HAART: A systematic review of developed and developing nation patient-reported barriers and facilitators. PLoS Medicine. 2006;3(11):e438. doi: 10.1371/journal.pmed.0030438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukherjee J.S., Ivers L., Leandre F., Farmer P., Behforouz H. Antiretroviral therapy in resource-poor settings: Decreasing barriers to access and promoting adherence. Journal of Acquired Immune Deficiency Syndromes. 2006;43:S123–S126. doi: 10.1097/01.qai.0000248348.25630.74. [DOI] [PubMed] [Google Scholar]
- Mushavi R.C., Burns B.F.O., Kakuhikire B., Owembabazi M., Vořechovská D., McDonough A.Q., Cooper-Vince C.E., Baguma C., Rasmussen J.D., Bangsberg D.R., Tsai A.C. “When you have no water, it means you have no peace”: A mixed-methods, whole-population study of water insecurity and depression in rural Uganda. Social Science & Medicine. 2020;245:112561. doi: 10.1016/j.socscimed.2019.112561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nachega J.B., Hislop M., Dowdy D.W., Chaisson R.E., Regensberg L., Maartens G. Adherence to nonnucleoside reverse transcriptase inhibitor-based HIV therapy and virologic outcomes. Annals of Internal Medicine. 2007;146(8):564–573. doi: 10.7326/0003-4819-146-8-200704170-00007. [DOI] [PubMed] [Google Scholar]
- Nam S.L., Fielding K., Avalos A., Dickinson D., Gaolathe T., Geissler P.W. The relationship of acceptance or denial of HIV-status to antiretroviral adherence among adult HIV patients in urban Botswana. Social Science & Medicine. 2008;67(2):301–310. doi: 10.1016/j.socscimed.2008.03.042. [DOI] [PubMed] [Google Scholar]
- Paik A., Sanchagrin K. Social isolation in America: an artifact. American Sociological Review. 2013;78:339–360. doi: 10.1177/0003122413482919. [DOI] [Google Scholar]
- Pearlin L., Aneschensel C. In: Applications of social science to clinical medicine and health policy. Mechanic D., Aiken L.H., editors. Rutgers University Press; 1986. Coping and social supports: Their functions and applications. [Google Scholar]
- Perkins J.M., Kakuhikire B., Baguma C., Jurinsky J., Rasmussen J.D., Satinsky E.N., Namara E., Ahereza P., Kyokunda V., Perkins H.W., Hahn J.A., Bangsberg D.R., Tsai A.C. Overestimation of alcohol consumption norms as a driver of alcohol consumption: A whole-population network study of men across eight villages in rural, southwestern Uganda. Addiction. 2022;117(1):68–81. doi: 10.1111/add.15615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins J.M., Kakuhikire B., Baguma C., Rasmussen J.D., Satinsky E.N., Kiconco A., Kananura J., Audet C.M., Siedner M.J., Haberer J.E., Bangsberg D.R., Tsai A.C. Perceptions about local ART adherence norms and personal adherence behavior among adults living with HIV in rural Uganda. AIDS and Behavior. 2022;26(6):1892–1904. doi: 10.1007/s10461-021-03540-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins J.M., Nyakato V.N., Kakuhikire B., Tsai A.C., Subramanian S.V., Bangsberg D.R., Christakis N.A. Food insecurity, social networks and symptoms of depression among men and women in rural Uganda: A cross-sectional, population-based study. Public Health Nutrition. 2018;21(5):838–848. doi: 10.1017/S1368980017002154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry B.L., Pescosolido B.A. Social network activation: The role of health discussion partners in recovery from mental illness. Social Science & Medicine. 2015;125:116–128. doi: 10.1016/j.socscimed.2013.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry B., Pescosolido B.A., Borgatti S.P. Cambridge University Press; 2018. Egocentric network analysis: Foundations, methods, and models. [Google Scholar]
- Phiri S., Tweya H., van Lettow M., Rosenberg N.E., Trapence C., Kapito-Tembo A., Kaunda-Khangamwa B., Kasende F., Kayoyo V., Cataldo F., Stanley C., Gugsa S., Sampathkumar V., Schouten E., Chiwaula L., Eliya M., Chimbwandira F., Hosseinipour M.C. Impact of facility- and community-based peer support models on maternal uptake and retention in Malawi's option B+ HIV prevention of mother-to-child transmission program: A 3-arm cluster randomized controlled trial (PURE Malawi) Journal of Acquired Immune Deficiency Syndromes. 2017;75(Suppl 2):S140–s148. doi: 10.1097/qai.0000000000001357. [DOI] [PubMed] [Google Scholar]
- Prevention Access Campaign Undetectable = untransmittable. 2022. https://preventionaccess.org/faq/ Retrieved November 15, 2022 from.
- Sam-Agudu N.A., Cornelius L.J., Okundaye J.N., Adeyemi O.A., Isah H.O., Wiwa O.M., Adejuyigbe E., Galadanci H., Afe A.J., Jolaoso I., Bassey E., Charurat M.E. The impact of mentor mother programs on PMTCT service uptake and retention-in-care at primary health care facilities in Nigeria: A prospective cohort study (MoMent Nigeria) Journal of Acquired Immune Deficiency Syndromes. 2014;67(Suppl 2):S132–S138. doi: 10.1097/qai.0000000000000331. [DOI] [PubMed] [Google Scholar]
- Sasaki Y., Kakimoto K., Dube C., Sikazwe I., Moyo C., Syakantu G., Komada K., Miyano S., Ishikawa N., Kita K., Kai I. Adherence to antiretroviral therapy (ART) during the early months of treatment in rural Zambia: Influence of demographic characteristics and social surroundings of patients. Annals of Clinical Microbiology and Antimicrobials. 2012;11(1):34. doi: 10.1186/1476-0711-11-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siedner M.J., Lankowski A., Tsai A.C., Muzoora C., Martin J.N., Hunt P.W., Haberer J.E., Bangsberg D.R. GPS-measured distance to clinic, but not self-reported transportation factors, are associated with missed HIV clinic visits in rural Uganda. AIDS. 2013;27(9):1503–1508. doi: 10.1097/QAD.0b013e32835fd873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith R., Rossetto K., Peterson B.L. A meta-analysis of disclosure of one's HIV-positive status, stigma and social support. AIDS Care. 2008;20(10):1266–1275. doi: 10.1080/09540120801926977. [DOI] [PubMed] [Google Scholar]
- Stangl A.L., Bunnell R., Wamai N., Masaba H., Mermin J. Measuring quality of life in rural Uganda: Reliability and validity of summary scores from the medical outcomes study HIV health survey (MOS-HIV) Quality of Life Research. 2012;21(9):1655–1663. doi: 10.1007/s11136-011-0075-5. [DOI] [PubMed] [Google Scholar]
- Takada S., Nyakato V., Nishi A., O'Malley A.J., Kakuhikire B., Perkins J.M., Bangsberg D.R., Christakis N.A., Tsai A.C. The social network context of HIV stigma: Population-based, sociocentric network study in rural Uganda. Social Science & Medicine. 2019;233:229–236. doi: 10.1016/j.socscimed.2019.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takada S., Weiser S.D., Kumbakumba E., Muzoora C., Martin J.N., Hunt P.W., Haberer J.E., Kawuma A., Bangsberg D.R., Tsai A.C. The dynamic relationship between social support and HIV-related stigma in rural Uganda. Annals of Behavioral Medicine. 2014;48(1):26–37. doi: 10.1007/s12160-013-9576-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai A.C., Bangsberg D.R. The importance of social ties in sustaining medication adherence in resource-limited settings. Journal of General Internal Medicine. 2011;26(12):1391–1393. doi: 10.1007/s11606-011-1841-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai A.C., Bangsberg D.R., Frongillo E.A., Hunt P.W., Muzoora C., Martin J.N., Weiser S.D. Social Science & Medicine. 2012;74(12):2012–2019. doi: 10.1016/j.socscimed.2012.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai A.C., Bangsberg D.R., Weiser S.D. Harnessing poverty alleviation to reduce the stigma of HIV in Sub-Saharan Africa. PLoS Medicine. 2013;10(11) doi: 10.1371/journal.pmed.1001557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai A.C., Kakuhikire B., Perkins J.M., Downey J.M., Baguma C., Satinsky E.N.…Bangsberg D.R. Normative vs personal attitudes toward persons with HIV, and the mediating role of perceived HIV stigma in rural Uganda. Journal of Global Health. 2021;11(4956) doi: 10.7189/jogh.11.04056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai A.C., Tomlinson M., Comulada W.S., Rotheram-Borus M.J. Food insufficiency, depression, and the modifying role of social support: Evidence from a population-based, prospective cohort of pregnant women in peri-urban South Africa. Social Science & Medicine. 2016;151:69–77. doi: 10.1016/j.socscimed.2015.12.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS Political declaration on HIV and AIDS: On the fast track to accelerating the fight against HIV and to ending the AIDS epidemic by 2030. 2016. https://www.unaids.org/en/resources/presscentre/pressreleaseandstatementarchive/2016/june/20160608_PS_HLM_PoliticalDeclaration Retrieved November 10, 2022 from.
- Valente T.W. Network interventions. Science. 2012;337(6090):49–53. doi: 10.1126/science.1217330. [DOI] [PubMed] [Google Scholar]
- Ware N.C., Idoko J., Kaaya S., Biraro I.A., Wyatt M.A., Agbaji O., Chalamilla G., Bangsberg D.R. Explaining adherence success in sub-saharan Africa: An ethnographic study. PLoS Medicine. 2009;6(1) doi: 10.1371/journal.pmed.1000011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware N.C., Wyatt M.A., Pisarski E.E., Bwana B.M., Orrell C., Asiimwe S.…Haberer J.E., META Study Team. Influences on adherence to antiretroviral therapy (ART) in early-stage HIV disease: qualitative study from Uganda and South Africa. AIDS & Behavior. 2020;24(9):2624–2636. doi: 10.1007/s10461-020-02819-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiser S.D., Palar K., Frongillo E.A., Tsai A.C., Kumbakumba E., Depee S., Hunt P.W., Ragland K., Martin J., Bangsberg D.R. Longitudinal assessment of associations between food insecurity, antiretroviral adherence and HIV treatment outcomes in rural Uganda. AIDS. 2014;28(1):115–120. doi: 10.1097/01.aids.0000433238.93986.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss R.S. In: Doing unto others. Rubin Z., editor. Prentice Hall; 1974. The provisions of social relationships. [Google Scholar]
- Wood E., Hogg R.S., Yip B., Harrigan P.R., O'Shaughnessy M.V., Montaner J.S. Effect of medication adherence on survival of HIV-infected adults who start highly active antiretroviral therapy when the CD4+ cell count is 0.200 to 0.350 x 10(9) cells/L. Annals of Internal Medicine. 2003;139(10):810–816. doi: 10.7326/0003-4819-139-10-200311180-00008. [DOI] [PubMed] [Google Scholar]
- Yamanis T.J., Dervisevic E., Mulawa M., et al. Social network influence on HIV testing among urban men in Tanzania. AIDS and Behavior. 2017;21(4):1171–1182. doi: 10.1007/s10461-016-1513-8. 2017/04/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.