Abstract
Background:
Pulmonary Embolism (PE) represents a life-threatening medical emergency that, given the serious complications, requires urgent application of anticoagulant therapy. In addition to other factors that are taken into account when choosing a therapy for treatment of PE, the anatomical distribution of thrombi is also considered–whether it is a central, lobar, segmental or subsegmental PE. D-dimer is an intermediate product of degradation of fibrin molecules and its values in the plasma are increased in the case of PE, but also in other diseases.
Objective:
To determine whether there is a difference in D-dimer values in subjects with different anatomical distribution of PE.
Methods:
The study included 100 subjects with diagnosed PE by using MSCT and/or V/P SPECT and with measured values of D-dimer.
Results:
Out of 100 subjects, PE was not diagnosed in 37 subjects, while 63 subjects PE was diagnosed. All subjects with diagnosed PE were divided into 3 groups regarding the anatomical localization of thrombus: lobar, segmental or subsegmental. Average D-dimer values were calculated for all 3 groups. Statistical analysis showed that there was no significant difference in D-dimer values between subjects with different anatomical distribution of PE.
Conclusion:
There is no significant difference in D-dimer values between subjects with different anatomical distribution od PE–lobar, segmental and subsegmental PE.
Keywords: anatomical distribution of pulmonary embolism, D-dimer, MSCT, V/P SPECT
1. BACKGROUND
Pulmonary embolism (PE) is a life-threatening medical emergency where the main pulmonary arteries and/or their lobar, segmental and subsegmental branches are obstructed by thrombotic masses, which leads to compromised blood flow. Considering the serious complications of this disease, it is necessary to prescribe therapy as soon as possible, and in most cases the therapy of choice is anticoagulant therapy (1, 2).
Choosing the appropriate therapy for the treatment of PE is very demanding and a significant number of factors must be taken into account in order to make the right decision that will be the most effective for the patient. In the process of choosing therapy, numerous factors are taken into account, such as the assessment of the risk of a fatal outcome, the state of liver and renal function, the risk of bleeding, comorbidities, the patient’s cooperation, the availability of therapeutic options, the existence of risk factors for the occurrence of PE and the anatomical distribution of PE (3, 4, 5).
Unfortunately, the clinical presentation together with anamnestic data and standard laboratory findings can arouse suspicion of the existence of PE, but they do not have sufficient sensitivity and specificity in diagnosing pulmonary embolism necessary for the application of anticoagulant therapy (2,6,7,8).
In subjects with clinical suspicion of PE, first step in the evaluation is measuring the level of D-dimer in the blood, as this value is used to select subjects who will be referred for further imaging methods.
D-dimer is an intermediate product of the degradation of fibrin molecules and its values in the plasma are increased in the case of acute thrombosis due to the simultaneous activation of the coagulation and fibrinolysis processes. The detection of D-dimer in serum is performed through the detection of D-dimer antigen by using tests that bind antibodies to epitopes present on D-dimer molecules and are not present on other intermediate products of fibrin degradation (9).
The two imaging methods with the highest sensitivity and specificity, most commonly used in diagnosing PE and monitoring the effects of prescribed anticoagulant therapy, are Multislice Computed Tomography (MSCT) and Ventilation/Perfusion Single-Photon Emission Computed Tomography (V/P SPECT) (1).
Based on MSCT and/or V/P SPECT findings, the anatomical distribution of the pulmonary artery can be classified as central (in the main trunk), lobar, segmental and subsegmental.
2. OBJECTIVE
The aim of this study was to determine whether there is a difference in D-dimer values in subjects with different anatomical distribution of PE.
3. METHODS
The prospective study conducted at the Clinical Center University of Sarajevo included 100 consecutive adult subjects with preserved renal function in whom the competent clinician suspected the presence of PE and who underwent to D-dimer, MSCT and/or V/P SPECT examination within 48 hours.
The study did not include minors, pregnant women and subjects with impaired renal function (creatinine clearance <60 ml/min).
The subjects with clinically suspected PE and elevated D-dimer values were referred for MSCT and/or V/P SPECT examination of the thoracic organs. MSCT and/or V/P SPECT examination were performed only in subjects with pathological D-dimer values, considering that the negative predictive value of D-dimer is high and normal D-dimer values in the blood indicate a low probability of PE, i.e. in the case of a normal D-dimer values it is practically possible to rule out PE.
All MSCT examinations were performed on a machine with 64 or more rows of detectors. After obtaining the topogram and determining the scanning field that covers the area of the thoracic organs from the tops to the bases of the lungs, a contrast series of scans commenced. Iodine-based contrast agent was applied with an automatic syringe in the amount of 80 to 100 ml, depending on the subject’s body weight, at a rate of 4 mL/S. The following parameters were used for scanning: SMART PREP technique, breath-hold scanning in layers of 0.5 mm (120 kV, 250 mA, gantry rotation time 0.75 s). If, during the analysis of the scans, the existence of a partial or complete defect in the contrast filling in the pulmonary arteries and their branches was determined, the examination was classified as positive for PE (11).
V/P SPECT examinations were performed according to a one-day standardized protocol recommended by the European Association of Nuclear Medicine (8). As the first part of the examination, ventilation tomography was performed with previous inhalation of Technegas. Immediately after the completed ventilation tomography, perfusion tomography was performed, after the application of Tc-99m-MAA. Acquisition–Ventilation: 30-50 MBq of Technegas; Acquisition–Perfusion: 100-120MBq 99mTc MAA. A wide-field gamma camera with a low-energy, high-resolution collimator with the following parameters was used for acquisition: matrix size 64 x 64, 128 projections/360°; duration: 10 sec/frame-V; 5sec/frame P. The analysis of V/P SPECT findings was performed according to the interpretation criteria of the European Association of Nuclear Medicine (5). The examination was classified as positive for PE if at least one segmental perfusion defect or two subsegmental perfusion defects were observed, while at the same time ventilation was preserved in the same region/regions–“mismatch”.
Subjects with PE confirmed by at least one of the imaging methods (MSCT and V/P SPECT) were classified as positive for the presence of PE.
Based on the location of thrombus in main pulmonary arteries and/or their lobar, segmental and subsegmental branches on MSCT examination and/or location of the mismatch, the anatomical distribution of pulmonary embolism was classified as PE involving the main pulmonary artery trunk (central) or lobar artery or segmental or subsegmental. In the case of mixed distribution of PE, we took into account the more central anatomical distribution.
D-dimer values were measured on a Siemens BCSXP device (Siemens Healthneers) using the Innovance D-dimer calibrator CA-600 System. D-dimer values higher than 0.55 (mg/L) were considered pathological (reference interval: 0.00 – 0.55 mg/L).
For statistical analysis of the results the Microsoft Excel 365 (Microsoft Corporation, Redmond, Washington, USA) and IBM SPSS ver. 26.0 (IBM, Armonk, New York, USA) software was used. The significance level α = 0.05 was chosen, and p values lower than this were considered statistically significant.
The results consisted partly of nominal variables and partly of ordinal variables. However, most of the collected data belong to the group of continuous variables. The median () was used as a measure of their central tendency, and the interquartile range (ΔQ) was used as a measure of dispersion, given that the distribution does not follow a normal distribution.
The Mann-Whitney U test was used to compare groups of independent data that do not follow a normal distribution.
4. RESULTS
A total of 100 clinically suspected PE subjects based on pathological values of D-dimer who undergone to MSCT and V/P SPECT imaging studies were included in the study.
Out of the total number of subjects, 45 were male and 55 were female. The number of male subjects did not differ significantly from the number of female subjects (binomial test, p = 0.368).
The median age of the subjects was 60 years (ΔQ = 26), with no significant differences between men and women (Mann-Whitney U test, p = 0.521).
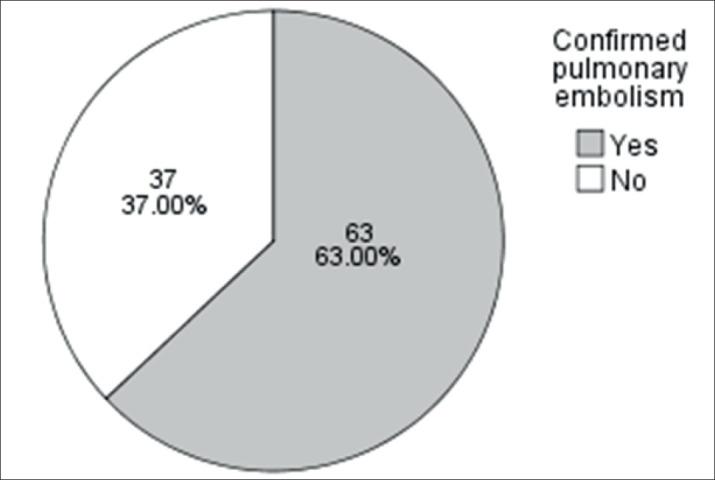
Of the total number of subjects included in the study (n = 100), 37 of them were not diagnosed with PE, while 63 subjects were diagnosed with PE and underwent anticoagulant treatment (Figure 1).
Figure 1. The percentage of subjects with excluded and confirmed pulmonary embolism.
All subjects with diagnosed PE were divided into 3 groups: a group of subjects with confirmed lobar PE, a group of subjects with confirmed segmental PE and a group of subjects with confirmed subsegmental PE, based on the finding of imaging methods. In our study we didn’t have patients with PE in main pulmonary artery. Average D-dimer values were calculated for all 3 groups (Table 1).
Table 1. Median () and interquartile range (ΔQ) of D-dimer values for patients with different distribution of pulmonary embolism, and p-values of Mann-Whitney U test.
| Anatomical distribution of pulmonary embolism | ||||||||
|---|---|---|---|---|---|---|---|---|
| Excluded PE | Segmental PE | Subsegmental PE | Lobar PE | |||||
|
|
ΔQ | ΔQ | ΔQ | ΔQ | ||||
| D-dimer | 9.2 | 20.2 | 7.7 | 21 | 11.3 | 24.6 | 40.7 | 1.1 |
| P | Ref. | 0.518 | 0.858 | 0.081 | ||||
Through subsequent analysis of D-dimer values in the subjects included in the study, we observed that there is no significant difference in D-dimer values among patients with lobar, segmental and subsegmental pulmonary embolism (Mann-Whitney U test).
5. DISCUSSION
All subjects included in our study had elevated D-dimer values. One of the basic clinical criteria for suspecting PE and inclusion in the study, in addition to symptomatology, was elevated D-dimer values. The sensitivity of D dimer for diagnosing PE is 96.4%, while the negative predictive value is 99.6% (12, 13, 14), i.e. normal D-dimer values practically exclude the possibility of PE.
Based on subsequent analysis of D-dimer values in subjects included in the study, we observed that there is no significant difference in D-dimer values between subjects with different anatomical distribution od PE (lobar, segmental and subsegmental PE). This result is in accordance with the results of small number of researchers who didn’t find the correlation between plasma levels of D-dimer and between the location of thrombus (15). On the other hand, the majority of researchers have found a strong correlation between plasma D-dimer concentration and embolus location; furthermore, their data indicate that the accuracy of D-dimer measurement to exclude PE depends strongly on embolus location (16, 17, 18).
The discrepancy between our results and data from the literature can be explained by the relatively small number of subjects included in the study, as well as by the fact that D-dimer values can be elevated in numerous other conditions (deep venous trombosis, disseminated intravascular coagulation (DIC), acute aortic dissection, aortic aneurysm, peripheral arterial disease, coronary artery disease, acute myocardial infarction, stroke, malignant diseases, inflammation, bleeding, trauma, surgical procedures and necrosis), not only in pulmonary embolism.
6. CONCLUSION
Based on analysis of D-dimer values in subjects with different anatomical location of thrombus, we observed that there is no significant difference in D-dimer values between subjects with different anatomical distribution od PE–lobar, segmental and subsegmental PE.
Declaration of subject consent:
the authors certify that they have obtained all appropriate subject consent forms. In the form, the subjects have given their consent for their images and other clinical information to be reported in the journal.
Authors’s Contributions:
SK, AB, SVZ and AB gave substantial contribution to the conception or design of the article an in the acquisition, analysis and interpretation of data for the article. Each author had role in article drafting and in process of revision. Each author gave final approval of the version to be published and they agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Conflict of interest:
There are no conflict of interest.
Financial support and sponsorship:
Nil.
REFERENCES
- 1.Konstantinides SV, Meyer G, Becattini C, Bueno H, Geersing GJ, Harjola VP, et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS) Eur Heart J. 2020 Jan 21;41(4):543–603. doi: 10.1093/eurheartj/ehz405. [DOI] [PubMed] [Google Scholar]
- 2.Vyas V, Goyal A. StatPearls (Internet) Treasure Island (FL): StatPearls Publishing; 2022. [2023 Feb 17]. Acute Pulmonary Embolism. Available from: http://www.ncbi.nlm.nih.gov/books/NBK560551/ [PubMed] [Google Scholar]
- 3.Roy PM, Douillet D, Penaloza A. Contemporary management of acute pulmonary embolism. Trends in cardiovascular medicine. 2022;32(5):259–268. doi: 10.1016/j.tcm.2021.06.002. [DOI] [PubMed] [Google Scholar]
- 4.Panahi L, Udeani G, Horseman M, Weston J, Samuel N, Joseph M, et al. Review of medical therapies for the management of pulmonary embolism. Medicina. 2021;57(2):110. doi: 10.3390/medicina57020110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nie Y, Sun L, Long W, et al. Clinical importance of the distribution of pulmonary artery embolism in acute pulmonary embolism. Journal of International Medical Research. 2021;49(4) doi: 10.1177/03000605211004769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thomson KL, Pool E, Kerray P. Risk assessment and thromboprophylaxis in adult patients with lower-limb immobilisation. Emergency Nurse. 2023;31(2) doi: 10.7748/en.2023.e2155. [DOI] [PubMed] [Google Scholar]
- 7.Piovella F, Iosub DI. Acute pulmonary embolism: risk assessment, risk stratification and treatment options. Clin Respir J. 2016 Sep;10(5):545–554. doi: 10.1111/crj.12264. [DOI] [PubMed] [Google Scholar]
- 8.Bajc M, Schümichen C, Grüning T, Lindqvist A, Le Roux PY, Alatri A, et al. EANM guideline for ventilation/perfusion single-photon emission computed tomography (SPECT) for diagnosis of pulmonary embolism and beyond. European journal of nuclear medicine and molecular imaging. 2019;46:2429–51. doi: 10.1007/s00259-019-04450-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Soomro AY, Guerchicoff A, Nichols DJ, Suleman J, Dangas GD. The current role and future prospects of D-dimer biomarker. European Heart Journal-Cardiovascular Pharmacotherapy. 2016;2(3):175–184. doi: 10.1093/ehjcvp/pvv039. [DOI] [PubMed] [Google Scholar]
- 10.Freund Y, Chauvin A, Jimenez S, Philippon AL, Curac S, Fémy F, et al. Effect of a diagnostic strategy using an elevated and age-adjusted D-dimer threshold on thromboembolic events in emergency department patients with suspected pulmonary embolism: a randomized clinical trial. Jama. 2021;326(21):2141–2149. doi: 10.1001/jama.2021.20750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wittram C, Maher MM, Yoo AJ, Kalra MK, Shepard JAO, McLoud TC. CT angiography of pulmonary embolism: diagnostic criteria and causes of misdiagnosis. Radiographics. 2004;24(5):1219–1238. doi: 10.1148/rg.245045008. [DOI] [PubMed] [Google Scholar]
- 12.Kearon C, de Wit K, Parpia S, Schulman S, Afilalo M, Hirsch A, et al. Diagnosis of pulmonary embolism with d-dimer adjusted to clinical probability. New England Journal of Medicine. 2019;381(22):2125–2134. doi: 10.1056/NEJMoa1909159. [DOI] [PubMed] [Google Scholar]
- 13.Dunn KL, Wolf JP, Dorfman DM, Fitzpatrick P, Baker JL, Goldhaber SZ. Normal D-dimer levels in emergency department patients suspected of acute pulmonary embolism. Journal of the American College of Cardiology. 2002;40(8):1475–1478. doi: 10.1016/s0735-1097(02)02172-1. [DOI] [PubMed] [Google Scholar]
- 14.Patel P, Patel P, Bhatt M, Braun C, Begum H, Wiercioch W, et al. Systematic review and meta-analysis of test accuracy for the diagnosis of suspected pulmonary embolism. Blood advances. 2020;4(18):4296–4311. doi: 10.1182/bloodadvances.2019001052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gao H, Liu H, Li Y. Value of Ddimer levels for the diagnosis of pulmonary embolism: An analysis of 32 cases with computed tomography pulmonary angiography. Experimental and therapeutic medicine. 2018 Aug 1;16(2):1554–1560. doi: 10.3892/etm.2018.6314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.De Monye W, Sanson BJ, Mac Gillavry MR, Pattynama PM, Buller HR, van den Berg-Huysmans AA, Huisman MV. Embolus location affects the sensitivity of a rapid quantitative D-dimer assay in the diagnosis of pulmonary embolism. American journal of respiratory and critical care medicine. 2002 Feb 1;165(3):345–348. doi: 10.1164/ajrccm.165.3.2104099. [DOI] [PubMed] [Google Scholar]
- 17.Kubak MP, Lauritzen PM, Borthne A, Ruud EA, Ashraf H. Elevated d-dimer cut-off values for computed tomography pulmonary angiography—d-dimer correlates with location of embolism. Annals of Translational Medicine. 2016 Jun;4(11) doi: 10.21037/atm.2016.05.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chrysikos S, Papaioannou O, Karampitsakos T, Tavernaraki K, Thanou I, Filippousis P, Anyfanti M, Hillas G, Tzouvelekis A, Thanos L, Dimakou K. Diagnostic Accuracy of Multiple D-Dimer Cutoff Thresholds and Other Clinically Applicable Biomarkers for the Detection and Radiographic Evaluation of Pulmonary Embolism. Advances in Respiratory Medicine. 2022 Aug 5;90(4):300–309. doi: 10.3390/arm90040039. [DOI] [PMC free article] [PubMed] [Google Scholar]


