Abstract
In this study we analyzed whether infection with Helicobacter pylori gives rise to specific B-cell responses against a number of putative virulence factors of H. pylori, e.g., urease, flagellin, and different bacterial surface antigens, locally in the gastric mucosa. This was studied in antrum and corpus biopsies collected from 11 H. pylori-infected patients with duodenal ulcers, 11 asymptomatic H. pylori carriers, and 13 noninfected, healthy controls. Mononuclear cells were isolated from the biopsies and assayed for frequencies of total and H. pylori-specific antibody-secreting cells (ASCs) by means of the enzyme-linked immunospot technique. The H. pylori-infected subjects had remarkably higher frequencies of total immunoglobulin A (IgA)- and IgM-secreting cells than the noninfected subjects, while the frequencies of IgG-secreting cells were virtually the same in the different groups. In addition, most of the infected subjects had IgA ASCs reacting with H. pylori membrane proteins, flagellin, and urease, while none of the noninfected subjects had any detectable H. pylori-reactive ASCs. Furthermore, half of the infected subjects also had ASCs reacting with a Helicobacter-specific 26-kDa protein, while only a few of them had ASCs reacting with neutrophil-activating protein, the neuraminyllactose-binding hemagglutinin HpaA, or lipopolysaccharides purified from different H. pylori strains. The frequencies of H. pylori-specific ASCs in the antrum and corpus were almost identical, and no differences in either antigen specificity or magnitude of the B-cell response in the stomach could be detected between the ulcer patients and the asymptomatic H. pylori carriers. This study demonstrates that H. pylori infection induces strong antibody responses in the human gastric mucosa, both in asymptomatic carriers and in duodenal ulcer patients. However, the outcome of infection could not be explained by differences in the local B-cell response to any of the antigens used in this study.
Infection with Helicobacter pylori is strongly associated with the development of chronic active gastritis, peptic ulcers, and gastric cancer (6, 43, 52). Since H. pylori is a noninvasive bacterium and is restricted to the gastric mucosa it is likely that an effective immune response against H. pylori should be of mucosal rather than of systemic origin. In accordance with this, it is well known that the infection is characterized by a massive infiltration of the gastric mucosa with neutrophils and lymphocytes (61). In particular, the infection results in dramatically increased numbers of immunoglobulin A (IgA)-secreting cells in the human gastric mucosa (32). H. pylori-specific antibody-secreting cells (ASCs) have also been documented (54), but the antigenic specificity of these ASCs has not yet been determined. Furthermore, the infection usually induces high levels of H. pylori-specific antibodies in serum, and significant antibody levels have also been demonstrated in saliva, gastric juice, and feces (28, 61). In spite of the strong antibody responses, the bacteria are rarely eliminated from the stomach and the infection is usually lifelong. Although H. pylori infection can result in the development of peptic ulcers or gastric cancer, the majority of infected individuals remain asymptomatic (AS) throughout life. The reasons for the different outcomes of H. pylori infection are poorly understood, as are the mechanisms by which H. pylori causes disease (33). Some groups have suggested that peptic ulceration is the result of an imbalance in the complex interactions between the digestive effect of the gastric juice (39) and the mucosal defense system (19, 48), while others regard the immune responses to the infection as more important for the development of H. pylori-associated disease (2, 37).
One explanation for the different outcomes of infection may be variable expression of certain virulence factors by the infecting strains. Although several putative virulence factors have been described for H. pylori, e.g., surface antigens that may be adhesins, lipopolysaccharides (LPS) with endotoxin activity, flagella that promote motility, and urease that neutralizes the gastric acid, only some isoforms of the vacuolating cytotoxin (VacA) and the pathogenicity island containing the cytotoxin-associated protein (CagA) gene have been shown to be more prevalent in strains causing peptic ulcer disease (PUD) than in strains isolated from AS carriers (3, 59). Another possible explanation for the different outcomes of infection might be different abilities of hosts to control the inflammation caused by H. pylori. This possibility is supported by results from animal studies which have shown that a certain strain of H. pylori or Helicobacter felis can cause different clinical outcomes when given to different mouse strains (25, 38), and similar conclusions can be drawn from human studies (29). Host factors influencing the outcome of H. pylori infection have usually been attributed to differences in the specific T-cell responses mounted by the infected individual (13). However, effects of specific antibodies, particularly locally in the gastric mucosa, may also be considered to play a role in this process. It is possible, for example, that an increased local IgG response may induce a more severe inflammation (8), while IgA antibodies neutralizing inflammation-inducing antigens and toxins may be protective (22, 34).
In this study we have evaluated whether H. pylori infection may give rise to specific B-cell responses against a number of postulated virulence factors and prominent surface antigens in H. pylori, locally in the gastric mucosa, since mucosal antibodies probably are more efficient in protecting against infection or disease than systemic antibodies. We also studied whether there may be a difference in antibody responses between patients with duodenal ulcers (DU) and AS H. pylori carriers, to evaluate if there is a correlation between local production of antibodies with a certain specificity and the outcome of infection.
MATERIALS AND METHODS
Subjects and specimens.
The study was approved by the Human Research Ethical Committee of the Medical Faculty, Göteborg University, Göteborg, Sweden, and comprised 35 subjects, who gave informed consent to participate. Twenty-two of the subjects were infected with H. pylori; 11 of them were DU patients (mean age, 50.9 years; 5 males and 6 females), and 11 were AS (mean age, 49.6 years; 9 males and 2 females). In addition, 13 healthy, noninfected subjects (mean age, 42.0 years; 5 males and 8 females) were included in the study. The AS and noninfected subjects had no history of gastrointestinal disease or any other relevant illness. The DU patients had chronic relapsing DU disease, confirmed by endoscopy, but were in clinical remission at the time of the investigation. None of the subjects were on any medication at the time of the study, and no premedication was used except for local anesthesia.
From each subject 11 punch biopsies were collected from the antrum and 11 from the corpus region of the stomach. One biopsy from each location was fixed in formalin and sent for routine histology to the Department of Pathology, Göteborg University, where they were examined by the same, experienced histopathologist, who was unaware of the subjects’ clinical symptoms. The inflammatory cell infiltration (both polymorphonuclear cells and mononuclear cells [MNCs]) and H. pylori colonization were evaluated and rated on a scale of 0 to 3 (none, mild, moderate, and severe, respectively) according to the Sydney system (45). The remaining biopsies were used for isolation of lymphocytes. In addition, a blood sample was collected by venous puncture and used for determination of H. pylori-specific antibody titers and, for some subjects, the presence of circulating ASCs.
Diagnosis of H. pylori infection.
The biopsies from the antrum and corpus, respectively, were pooled, cut into 0.1- by 0.1-mm pieces with a semiautomated tissue chopper (McIlwan, Gilford, Great Britain), and dispersed in 10 ml of phosphate-buffered saline (PBS). Two hundred microliters of the mixture was inoculated on a Skirrow blood agar plate containing 10% horse blood, and after incubation under microaerophilic conditions (10% CO2, 5% O2, and 85% N2), at 37°C for 3 days, the plates were examined for H. pylori-like colonies. The bacteria were confirmed to be H. pylori by a rapid urease test and a dot blot assay with an H. pylori-specific monoclonal antibody (MAb) (Hp30-1:1:6) (8), and subjects with positive cultures were considered to be H. pylori infected. The isolated H. pylori strains were frozen at −70°C in freeze-drying medium containing 20% glycerol until use. The sera of all subjects were screened for the presence of H. pylori-specific antibodies (21), and these analyses showed that all subjects with positive cultures also had positive serologies. Only subjects who were negative by both culture and serology were included as noninfected controls.
Bacterial strains and preparation of antigens. (i) Strains.
The reference strains CCUG 17874, E32, and E50 (kindly provided by E. Falsen, Göteborg University, and J.-P. Butzler, St. Pieters University Hospital, Brussels, Belgium) and two strains from our own strain collection, Hel 73 (isolated from a patient with gastritis) and Hel 305 (isolated from a DU patient), were used for purification of antigens. The latter strains had been subcultured only twice before use in the study. All strains were grown on horse blood agar plates under microaerophilic conditions at 37°C for 3 days.
(ii) MP.
Whole membrane proteins (MP) were prepared from strains CCUG 17874, Hel 73, and Hel 305 by sonication followed by differential centrifugations as previously described (1).
(iii) Flagellins.
Flagellins (FlaA and FlaB) were purified from strain E32 as described by Kostrzynska et al. (24). The material was further purified by fast protein liquid chromatography fractionation on a Resource Q column (Pharmacia, Uppsala, Sweden), and the flagellin-containing fractions were identified by immunoblotting with a MAb against FlaA and FlaB (27).
(iv) Urease.
Urease was purified from strain E32 by a combination of the methods described by Dunn et al. (15) and Evans et al. (17). Briefly, H. pylori bacteria were harvested in PBS and centrifuged at 17,000 × g for 10 min. The pellet was then suspended in 1% N-octylglucose and left for 20 min at room temperature. After centrifugation at 26,000 × g for 15 min, the supernatant was dialyzed against PBS overnight at 4°C. Further purification was obtained by size exclusion chromatography on a Sepharose CL 6B column (Pharmacia). The urease-containing fractions were identified, pooled, and dialyzed against PBS. After filtration through a 0.45-μm-pore-size filter, the suspension was subjected to anion-exchange chromatography by fast protein liquid chromatography on a Resource Q column (Pharmacia).
(v) LPS.
LPS were obtained from three H. pylori strains, E50, CCUG 17874, and Hel 73, which have different LPS profiles as determined by silver staining and by assaying reactivity with MAbs raised against LPS from different H. pylori strains (56). The LPS were purified by the hot phenol-water extraction method of Westphal and Jann (60). The LPS preparations were then treated with DNase II (Boehringer Mannheim GmbH, Mannheim, Germany), RNase (Boehringer), and protease (type XIV; Sigma Chemical Co., St. Louis, Mo.), followed by ultracentrifugation as described previously (23). The LPS preparations, which contained less than 1% protein as determined by Peterson’s modification of the method of Lowry et al. with the Sigma Diagnostics protein assay kit (44), were characterized by using specific MAbs against homologous and heterologous H. pylori LPS as described previously (56).
(vi) Other antigens.
Neutrophil-activating protein (NAP) (18), the neuraminyllactose-binding protein HpaA (16, 41), and a 26-kDa protein (42) were recombinantly produced in Escherichia coli. NAP and HpaA were kindly provided by Susanne Nyström (Astra/Hässle, Umeå, Sweden), and the 26-kDa protein was provided by Genomic Therapeutic Company (Cambridge, Mass.). The purity of the antigen preparations was demonstrated by subjecting the proteins to electrophoresis in sodium dodecyl sulfate-polyacrylamide gels and staining with Coomassie blue or transblotting to nitrocellulose membranes and staining with rabbit polyclonal antisera against whole H. pylori bacteria and MAbs specific for the respective native protein (NAP [55], HpaA [7] and the 26-kDa protein [27]).
Isolation of lymphocytes.
Gastric lymphocytes were isolated from antrum and corpus biopsies as previously described (46). Briefly, the cut biopsies were treated with 0.5 mg of Bacillus thermoproteolyticus thermolysin (Boehringer) per ml and incubated at 4°C for 30 min. Single cells were collected, and the remaining tissue fragments were further treated with 1 mg of collagenase-dispase (Boehringer) per ml at 37°C for 45 min. Finally, the extracted cells were pooled and incubated at 37°C for 20 min in 2 mg of DNase (Sigma) per ml. Isolated cells were washed and resuspended in Iscove’s medium (Biochrom KG, Berlin, Germany) supplemented with 5% fetal calf serum and 100 μg of gentamicin (Essex Läkemedel AB, Stockholm, Sweden) per ml. On average, the enzymatic dispersion procedure yielded 2.2 × 105 (range, 0.7 × 105 to 9.8 × 105) MNCs per pool of 10 antrum or corpus biopsies.
Lymphocytes were also isolated from the peripheral blood of five H. pylori-infected subjects by standard isopycnic gradient centrifugation on Ficoll-Hypaque (Pharmacia).
Detection of total and H. pylori-specific ASCs.
Gastric and blood cell suspensions were analyzed for numbers of total and H. pylori-specific ASCs by a two-color micromodification (11) of the original enzyme-linked immunospot (ELISPOT) technique (12, 49). Individual wells were coated with 60 μg of MP per ml, 25 μg of LPS per ml, 25 μg of flagellin per ml, 10 μg of urease per ml, 25 μg of NAP per ml, 25 μg of HpaA per ml, or 25 μg of the 26-kDa protein per ml at 4°C overnight. These coating concentrations had been optimized in preliminary titration experiments on both human and mouse MNCs in such a way that there was a quantitative relation between the number of added cells and the number of counted spots, the spots were distinct, and the background was low. Furthermore, the possibility of detecting ASCs specific for the different antigens by using the ELISPOT method had been evaluated by analyzing cells from mice immunized with the respective antigen. In all of these assays, substantial numbers of ASCs were detected. For detection of the total frequencies of Ig-secreting cells, wells were coated with 5 μg of affinity-purified goat antibodies to the F(ab′)2 fragment of human IgG (Jackson ImmunoResearch Laboratories, West Grove, Pa.) per ml. The coated plates were washed with PBS and then blocked with Iscove’s medium supplemented with 10% fetal calf serum and 100 μg of gentamicin per ml at 37°C for 30 min. Gastric lymphocytes were then added to duplicate wells at concentrations ranging from 102 to 104 MNCs/well, while peripheral blood lymphocytes were added at concentrations of 105 to 106 MNCs/well, and incubated at 37°C overnight in air containing 7.5% CO2. MNCs from almost all of the subjects were analyzed for ASCs reacting with MP, flagellin, and urease, while ASCs specific for the other antigens, i.e., LPS, NAP, HpaA, and the 26-kDa protein, were assayed for only some of the subjects, due to limited numbers of cells. After thorough washes, goat anti-human Ig antibodies conjugated with either horseradish peroxidase (HRP) or alkaline phosphatase (AP) (Southern Biotechnology Associates, Birmingham, Ala.) were added to the plates and incubated at room temperature for 3 h. In each well two isotypes were detected, i.e., either IgA and IgG or IgM and IgA. For the detection of IgA-IgG, a mixture of HRP-conjugated anti-IgA antibodies and AP-conjugated anti-IgG antibodies was added to the wells, and for the detection of IgM-IgA, a mixture of HRP-conjugated anti-IgM antibodies and AP-conjugated anti-IgA antibodies was added. After addition of the respective chromogen substrate (45), the plates were examined for the presence of red (HRP) and blue (AP) spots under low magnification (×40) by two independent investigators. The frequencies of ASCs were expressed as the number of spot-forming cells per 105 MNCs for total Ig-secreting cells or as the number of specific ASCs per 104 total Ig-secreting cells of the corresponding isotype. The presence of more than two specific ASCs per well was considered a significant ASC response.
Determination of H. pylori-specific antibodies in serum.
H. pylori-specific antibody titers in sera were determined by enzyme-linked immunosorbent assay (47, 56). Briefly, 96-well microtiter plates were coated with 25 μg of MP per ml, 2.5 μg of urease per ml, 1.5 μg of HpaA per ml, or 1.5 μg of the 26-kDa protein per ml at room temperature overnight. After blocking of the plates, serum samples were added at an initial dilution of 1/10 and threefold diluted in PBS containing 0.1% bovine serum albumin and 0.05% Tween. After washings, HRP-labeled anti-human IgA or IgG antibodies (Jackson) were added, and the plates were subsequently developed by the addition of ortho-phenylenediamine and H2O2. The plates were read after 20 min in a photometer at 450 nm, and titers were determined as the reciprocal interpolated dilution giving an absorbance of 0.4 above the background level.
Statistical analyses.
Differences in frequencies of ASCs or serum antibody titers between the study groups were evaluated by the Mann-Whitney hypothesis test, while differences in ASC frequencies between the antrum and corpus within the same study group were evaluated by the Wilcoxon signed rank test for paired data; P values of <0.01 were considered to represent significant differences. The correlation between grade of inflammation and frequency of ASCs was expressed as Spearman’s rank correlation coefficient, rs.
RESULTS
Inflammation and bacterial load.
One biopsy from the antrum and one from the corpus of each subject were histologically examined for the presence of inflammatory cells and Helicobacter-like organisms (HLO) according to the Sydney system. The biopsies from the noninfected subjects were histologically normal without HLO, and mild chronic inflammation of antrum and corpus, respectively, could be detected in only two of the noninfected volunteers. In contrast, chronic inflammation was observed in the antra of all of the H. pylori-infected subjects (grade 2 for most of the subjects), and most of these subjects also had chronic inflammation in the corpus, although this inflammation seemed to be milder than that in the antrum (grade 1 for most of the subjects). HLO were found in all but two of the subjects who had been classified as H. pylori infected according to positive serology and culture, and there was no evident difference in bacterial density between the antrum and corpus. No difference in the number of inflammatory cells or HLO was seen between the AS subjects and the DU patients, in either the antrum or corpus biopsies.
Frequencies of total Ig-secreting cells.
MNCs were isolated from antrum and corpus biopsies and analyzed for frequencies of total and H. pylori-specific ASCs by the ELISPOT technique. In order to evaluate the methods used, three of the H. pylori-infected subjects were reexamined 3 weeks after the initial endoscopy. These analyses confirmed the reproducibility of the cell extraction as well as of the ELISPOT procedures, since very similar results were recorded at the first and the second examinations with regard to both the frequencies of ASCs with different antigen specificities and the isotype distribution; i.e., the results from the first and second examinations did not differ more than 1.5-fold with any of the antigens tested. In addition, the ELISPOT assays were evaluated by two independent investigators throughout the study, and their results were almost identical.
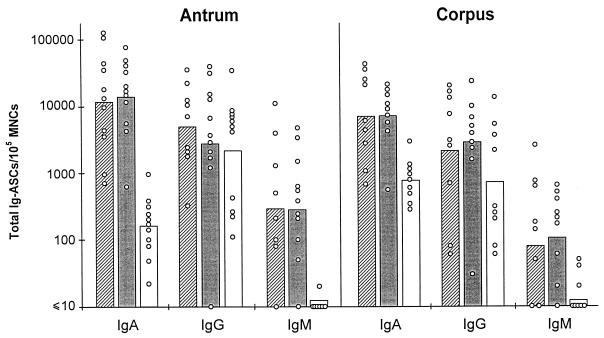
In the antra of the noninfected subjects, IgG-producing cells were more abundant than IgA ASCs, whereas almost no IgM-secreting cells were detected (Fig. 1). Both the DU patients and AS volunteers had significantly higher (about 80-fold) numbers of total IgA-secreting cells per 105 MNCs in the antrum than the noninfected subjects (P < 0.001). The frequencies of total IgM-secreting cells were also substantially higher (about 40-fold) in the infected subjects (P < 0.01), while the frequencies of total IgG-secreting cells were very similar in the H. pylori-infected and the noninfected subjects. Although there were great variations in the frequencies of total Ig-secreting cells between individuals, the mean numbers of ASCs of all isotypes per 105 MNCs were very similar in the AS and DU groups, and no significant differences in frequencies of total Ig-secreting cells of any of the isotypes were found between AS subjects and DU patients for the antrum mucosa.
FIG. 1.
Numbers of total IgA, IgG, and IgM ASCs per 105 MNCs in the gastric mucosa. MNCs were isolated from the antra and corpora of H. pylori-infected subjects with DU (hatched bars), AS H. pylori carriers (filled bars), and noninfected subjects (open bars), and the frequencies of ASCs were determined in ELISPOT assays. Each circle represents one subject, and the bars represent the geometric means within each group.
For the corpora of the noninfected subjects, similar frequencies of total IgA- and IgG-secreting cells were found, whereas almost no total IgM-secreting cells could be detected (Fig. 1). As in the antrum, the frequencies of total IgA- and IgM-secreting cells in the corpus were significantly higher (about 9-fold for IgA [P < 0.01] and >10-fold for IgM [P < 0.01]) in the H. pylori-infected subjects than in the noninfected subjects, with the mean frequencies of total Ig-secreting cells not differing between the AS subjects and DU patients. In the noninfected subjects the frequencies of total IgA-secreting cells were found to be significantly higher in the corpus than in the antrum when the paired data for each subject were compared (P < 0.01), while the frequencies of total IgG- and IgM-secreting cells did not differ between the two locations in these subjects. In the H. pylori-infected subjects, on the other hand, there were no significant differences between the frequencies of Ig-secreting cells in the antrum and corpus.
When all of the subjects were included in the analysis, a positive correlation between the inflammation score and the frequency of total IgA-secreting cells was found, both in the antrum (rs = 0.76; P < 0.01) and in the corpus (rs = 0.51; P < 0.01).
Frequencies of H. pylori-specific ASCs.
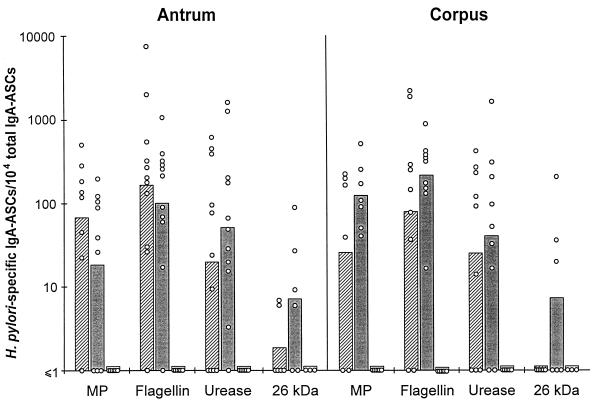
The gastric MNCs were also assayed for frequencies of ASCs specific for different H. pylori antigens, i.e., MP, flagellin, urease, NAP, HpaA, the 26-kDa protein, and LPS, by the ELISPOT technique. None of the noninfected subjects had detectable numbers of ASCs reacting with any of the antigens. In contrast, all of the H. pylori-infected volunteers had ASCs that reacted with at least one of the H. pylori antigens studied. Most of the infected subjects had high frequencies of ASCs specific for MP, flagellin, and urease, and half of them also had ASCs reacting with the 26-kDa protein (Fig. 2). In most instances, subjects who had high frequencies of ASCs reacting with urease also had high frequencies of ASCs reacting with MP or flagellin. However, some of the subjects had unexpectedly high frequencies of ASCs reacting with a single antigen. Only a few of the H. pylori-infected volunteers had ASCs that were specific for NAP, HpaA, or LPS (Table 1).
FIG. 2.
Prevalence of H. pylori-specific IgA ASCs in gastric mucosae of H. pylori-infected subjects with DU (hatched bars), AS H. pylori carriers (filled bars), and noninfected subjects (open bars). MNCs were isolated from the antrum and corpus of each subject, and the frequencies of total IgA ASCs as well as H. pylori-specific IgA ASCs were determined in ELISPOT assays. Each circle represents one subject; the bars represent the geometric means within each group. MP were prepared from strain CCUG 17874.
TABLE 1.
Frequencies of subjects with H. pylori-specific IgA and IgG ASCs in the antra
| Antigen and strain | No. positive/total for:
|
|||||
|---|---|---|---|---|---|---|
| IgA ASCs
|
IgG ASCs
|
|||||
| DU | AS | Noninfected | DU | AS | Noninfected | |
| MP | ||||||
| CCUG 17874 | 7/8 | 6/9 | 0/13 | 3/6 | 6/9 | 0/11 |
| Hel 73 | 6/6 | 4/4 | 0/3 | 5/6 | 3/4 | 0/3 |
| Hel 305 | 5/5 | 4/4 | 0/3 | 5/6 | 2/3 | 0/3 |
| LPS | ||||||
| CCUG 17874 | 0/3 | 0/2 | 0/3 | 0/3 | 0/2 | 0/3 |
| E50 | 1/8 | 0/9 | 0/11 | 0/6 | 0/9 | 0/9 |
| Hel 73 | 3/6 | 1/6 | 0/3 | 0/6 | 0/6 | 0/3 |
| NAP | 1/4 | 0/4 | 0/3 | 1/4 | 0/4 | 0/3 |
| HpaA | 1/6 | 2/9 | 0/8 | 0/6 | 1/9 | 0/7 |
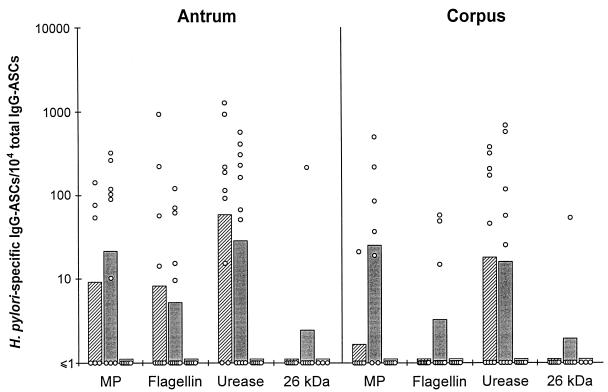
The predominant isotype of the antigen-specific ASCs was IgA (Fig. 2), whereas almost no H. pylori-specific IgM ASCs were detected. High frequencies of IgG ASCs were seen only against urease (Fig. 3). No differences in the frequencies of ASCs or in the specificities of the antibodies produced were found between the DU patients and AS subjects. Furthermore, no significant differences in H. pylori-specific ASCs were found between the antrum and corpus. In contrast to the case for the total Ig-secreting cells, no correlation between the frequencies of H. pylori-specific ASCs and the inflammation score or density of HLO was observed.
FIG. 3.
Prevalence of H. pylori-specific IgG ASCs in gastric mucosae of H. pylori-infected subjects with DU (hatched bars), AS H. pylori carriers (filled bars), and noninfected subjects (open bars). MNCs were isolated from the antrum and corpus, respectively, of each subject, and the frequencies of total IgG ASCs as well as H. pylori-specific IgG ASCs were determined in ELISPOT assays. Each circle represents one subject; the bars represent the geometric means within each group. MP were prepared from strain CCUG 17874.
To evaluate whether ASC responses against antigens prepared from various H. pylori strains differed, MNCs from some of the subjects were tested in parallel against MP prepared from strains CCUG 17874, Hel 73, and Hel 305. All of these subjects had IgA ASCs that reacted with all MP preparations, but the frequencies of specific ASCs were about four times higher against MP from the two clinical isolates, Hel 73 and Hel 305, than against those from the reference strain CCUG 17874 (Table 1). MNCs were also tested in parallel for ASCs against LPS prepared from strains E50, Hel 73, and CCUG 17874. Four of 12 H. pylori-infected volunteers had IgA ASCs that reacted with LPS from Hel 73, while none of the subjects had ASCs reacting with LPS from strain CCUG 17874 (Table 1).
MNCs were also isolated from the blood of five of the H. pylori-infected individuals and analyzed in parallel with the gastric MNCs. However, none of these subjects had any detectable circulating ASCs that reacted with any of the antigens studied, even though they had substantial numbers of specific ASCs in the gastric mucosa.
Serum antibody levels.
Serum samples from all of the subjects were also assayed for antibody titers against MP from strain CCUG 17874, urease, HpaA, and the 26-kDa protein. All of the infected subjects had significantly higher IgA and IgG titers against MP than the noninfected subjects, and most of the DU patients and AS subjects also had significantly elevated IgG titers against urease. In contrast, no significant differences in antibody titers against either HpaA or the 26-kDa protein between the infected and the noninfected subjects were seen (data not shown). In agreement with the ELISPOT data, no significant differences in antibody titers between the DU patients and the AS subjects could be detected.
DISCUSSION
In the present study we have for the first time demonstrated the presence of B cells that spontaneously secrete antibodies specific for a number of putative virulence factors and prominent antigens locally in the gastric mucosae of H. pylori-infected individuals. However, we did not find any differences in antigen specificity or magnitude of the ASC responses against the antigens used in this study between DU patients and AS H. pylori carriers.
When the frequencies of total Ig-secreting cells in the H. pylori-infected and noninfected subjects were compared, we found considerably higher frequencies of both total IgA- and IgM-secreting cells in the antra of the infected subjects than in those of the noninfected subjects. Indeed, the frequency of IgA-secreting cells was on average higher in the H. pylori-infected stomachs than what we have previously reported for the small intestines of both H. pylori-infected and noninfected subjects (32, 46). The frequencies of IgG-secreting cells, on the other hand, did not vary for infected and noninfected individuals. This is in sharp contrast to the findings for the colons of patients with inflammatory bowel disease, in whom considerably elevated numbers of IgG-producing cells have been observed (20). These differences suggest diverse mechanisms triggering the inflammation and could be the result of different endothelial expression of adhesion molecules directing trafficking of B cells to the inflamed colon or gastric mucosa.
The distributions of Ig-containing cells in inflamed and noninflamed gastric mucosae have previously been examined by immunofluorescence staining (57). In addition to significantly increased frequencies of IgA- and IgM-containing cells, increased frequencies of IgG-containing cells in the inflamed mucosa were also observed. Furthermore, IgA-containing cells predominated over IgG- and IgM-containing cells, independent of the degree of inflammation. In contrast, we observed more IgG- than IgA-secreting cells in the antra of the noninfected subjects and did not see any increase in the frequencies of IgG-secreting cells in the H. pylori-infected subjects. These discrepant results might be due to the fact that the immunofluorescence staining method detects all Ig-containing cells while the ELISPOT assay detects only actively Ig-secreting cells, which presumably results in considerable differences. In addition, the cause of gastric inflammation in the previous study was unknown. Furthermore, we have recently analyzed Ig contents in gastric aspirates and detected only low levels of IgG, while substantial amounts of IgA were detected, especially in the H. pylori-infected volunteers (30), supporting the dominance of IgA-secreting cells in H. pylori-associated gastritis.
Although the H. pylori-specific antibody response induced by natural infection is not capable of eliminating the infection, it is likely that an effective vaccine against H. pylori should induce strong secretory antibody responses locally in the stomach. In accordance with this notion, immunization of mice with H. pylori urease has been shown to induce mucosal IgA antibodies which correlate with protection against infection with H. felis (26). Blanchard et al. have also shown that mice given urease-specific MAbs together with H. felis bacteria are protected against infection (5). However, in the present study urease, together with flagellin and MP, was the most immunogenic among the antigens studied, but local production of urease-specific antibodies did not seem to protect against either infection or symptoms. Urease was also the only antigen that induced high frequencies of IgG ASCs, which could activate the complement system and thereby increase the inflammation of the gastric mucosa. However, we did not observe a correlation between numbers of antiurease IgG ASCs and inflammation.
On the other hand, only a small proportion of the infected subjects in this study had ASCs that were specific for HpaA and the 26-kDa protein, even though these proteins are found in relatively large amounts in all H. pylori strains studied hitherto (27). The LPS response was also very poor in most of the subjects, which might be due to the heterogeneity in LPS O chains between different H. pylori strains (36) or to the fact that H. pylori LPS often contains Lewis blood group antigens (2, 51) and thereby might evade the immune system.
As discussed above, an effective antibody response against H. pylori should preferentially consist of locally produced antibodies which are able to reach the gastric epithelium, where the bacteria are located. Although several studies have shown that H. pylori infection induces high levels of serum antibodies specific for many of the best-characterized H. pylori antigens, such as CagA, VacA, urease, LPS, and the heat shock proteins (14, 50, 56), few studies have evaluated the gastric antibody responses against that kind of purified antigen. Such analyses are of great importance, since it has been clearly shown that the systemic antibody responses do not necessarily reflect the mucosal immune responses (35, 58). This was also the case in our study, in which we found ASCs specific for the 26-kDa protein in the gastric mucosae of many of the H. pylori-infected subjects, while we could not detect increased levels of serum antibodies against this antigen in the infected compared with the noninfected subjects. However, there seems to be a correlation between specific ASCs in gastric biopsies and specific antibodies in gastric aspirates, since we have also been able to detect high levels of antibodies specific for MP, flagellin, and urease in gastric aspirates from H. pylori-infected subjects (31).
The H. pylori-specific ASCs detected in this study were shown to constitute approximately one-third of the enormous increase in the frequencies of total IgA-secreting cells in the H. pylori-infected subjects, but a substantial portion of the induced ASCs probably react with H. pylori antigens other than those analyzed. It is also possible that there is a certain influx of B cells with other specificities into the gastric mucosa. This is further demonstrated by a previous study in which we have shown that H. pylori-infected but not noninfected subjects respond with high frequencies of vaccine-specific ASCs after oral immunization with a cholera vaccine, demonstrating that ASCs against antigens other than those derived from H. pylori can indeed be induced in the H. pylori-infected stomach (32).
It has previously been suggested that H. pylori colonizes the antrum mucosa more heavily than the corpus mucosa (4, 53). In order to evaluate if the possible difference in bacterial load might result in higher frequencies of ASCs in the antrum than in the corpus, we analyzed biopsies from both locations. However, most of the subjects in our study had the same or even a higher density of bacteria in the corpus than in the antrum, according to the histological examination. On the other hand, a majority of the H. pylori-infected subjects had a higher degree of inflammation in the antrum than in the corpus. Despite these findings, no differences in either the magnitude or the specificity of the ASC response between the two locations could be demonstrated.
Only a relatively low proportion of H. pylori-infected individuals develop DU, while the majority remain AS. One aim of this study was to evaluate whether there were any differences between the AS and DU subjects in the magnitude of the ASC responses or in the specificity of the antibodies produced that could explain the different outcomes of infection. However, no such differences were observed for any of the antigens tested, and in spite of large individual differences, the mean frequencies of H. pylori-specific ASCs in the AS and DU groups were strikingly similar. The AS subjects tended to have somewhat higher frequencies of IgA ASCs reacting with the 26-kDa protein and urease than the DU patients, but these differences were not statistically significant. Furthermore, no significant differences between the AS subjects and DU patients in serum antibody titers against the tested antigens were observed. This is in accordance with previous work in which we studied serum antibody responses against a large number of antigens without being able to detect any differences in antigen specificity between DU patients and AS subjects (31). However, the fact that the DU patients were in clinical remission may to some extent have evened out a potential difference between the two study groups. Several previous studies have reported that H. pylori strains isolated from patients with PUD more often express VacA and CagA than strains isolated from individuals with other symptoms (3, 59) and also that patients with PUD more often have antibodies against CagA than other H. pylori-infected individuals (9, 10). Unfortunately, we did not have access to these proteins for use in ASC analyses and could not compare the frequencies of ASCs reacting with these antigens for the DU patients and AS subjects. However, even though we did not identify any differences in antibody responses in AS and symptomatic H. pylori carriers, there may be discriminating immune responses against antigens not included in this study, e.g., VacA, CagA, or hitherto-not-identified protective antigens, that may be relevant for inclusion in a vaccine against H. pylori (10, 40).
In conclusion, we have shown that H. pylori infection gives rise to significant increases particularly in IgA- but also in IgM-producing cells locally in the stomach and that a high proportion of these cells produce antibodies specific for different H. pylori antigens. Furthermore, very similar numbers of ASCs were observed in the antrum and corpus, and no differences either in antigen specificity or in numbers of ASCs could be detected between DU patients and AS H. pylori carriers for the antigens tested in this study. These findings might have important implications for elucidating pathogenic mechanisms in H. pylori.
ACKNOWLEDGMENTS
This study was financially supported by grants from Astra Hässle AB, Mölndal, Sweden, and Astra Research Center, Boston, Mass.
We thank all participants and the staff at the Department of Gastroenterology at Sahlgrenska Hospital. The skillful assistance of Maria Hjulström and Mikael Innocenti is gratefully acknowledged.
REFERENCES
- 1.Achtman M, Schwuchow S, Helmuth R, Morelli G, Manning P A. Cell-cell interactions in conjugating Escherichia coli: Con− mutants and stabilization of mating aggregates. Mol Gen Genet. 1978;164:171–183. [Google Scholar]
- 2.Appelmelk B J, Negrini R, Moran A P, Kuipers E J. Molecular mimicry between Helicobacter pylori and the host. Trends Microbiol. 1997;5:70–73. doi: 10.1016/S0966-842X(96)10084-6. [DOI] [PubMed] [Google Scholar]
- 3.Atherton J C, Cao P, Peek R M, Jr, Tummuru M K, Blaser M J, Cover T L. Mosaicism in vacuolating cytotoxin alleles of Helicobacter pylori. Association of specific vacA types with cytotoxin production and peptic ulceration. J Biol Chem. 1995;270:17771–17777. doi: 10.1074/jbc.270.30.17771. [DOI] [PubMed] [Google Scholar]
- 4.Bayerdorffer E, Lehn N, Hatz R, Mannes G A, Oertel H, Sauerbruch T, Stolte M. Difference in expression of Helicobacter pylori gastritis in antrum and body. Gastroenterology. 1992;102:1575–1582. doi: 10.1016/0016-5085(92)91716-h. [DOI] [PubMed] [Google Scholar]
- 5.Blanchard T G, Czinn S J, Maurer R, Thomas W D, Soman G, Nedrud J G. Urease-specific monoclonal antibodies prevent Helicobacter felis infection in mice. Infect Immun. 1995;63:1394–1399. doi: 10.1128/iai.63.4.1394-1399.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blaser M J. Hypotheses on the pathogenesis and natural history of Helicobacter pylori-induced inflammation. Gastroenterology. 1992;102:720–727. doi: 10.1016/0016-5085(92)90126-j. [DOI] [PubMed] [Google Scholar]
- 7.Bölin I, Lönroth H, Svennerholm A-M. Identification of Helicobacter pylori by immunological dot blot method based on reaction of a species-specific monoclonal antibody with a surface-exposed protein. J Clin Microbiol. 1995;33:381–384. doi: 10.1128/jcm.33.2.381-384.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brandtzaeg P, Halstensen T S, Kett K, Krajci P, Kvale D, Rognum T O, Scott H, Sollid L M. Immunobiology and immunopathology of human gut mucosa: humoral immunity and intraepithelial lymphocytes. Gastroenterology. 1989;97:1562–1584. doi: 10.1016/0016-5085(89)90406-x. [DOI] [PubMed] [Google Scholar]
- 9.Ching C K, Wong B C, Kwok E, Ong L, Covacci A, Lam S K. Prevalence of CagA-bearing Helicobacter pylori strains detected by the anti-CagA assay in patients with peptic ulcer disease and in controls. Am J Gastroenterol. 1996;91:949–953. [PubMed] [Google Scholar]
- 10.Crabtree J E, Taylor J D, Wyatt J I, Heatley R V, Shallcross T M, Tompkins D S, Rathbone B J. Mucosal IgA recognition of Helicobacter pylori 120 kDa protein, peptic ulceration, and gastric pathology. Lancet. 1991;338:332–335. doi: 10.1016/0140-6736(91)90477-7. [DOI] [PubMed] [Google Scholar]
- 11.Czerkinsky C, Moldoveanu Z, Mestecky J, Nilsson L Å, Ouchterlony Ö. A novel two colour ELISPOT assay. I. Simultaneous detection of distinct types of antibody-secreting cells. J Immunol Methods. 1988;115:31–37. doi: 10.1016/0022-1759(88)90306-7. [DOI] [PubMed] [Google Scholar]
- 12.Czerkinsky C C, Nilsson L Å, Nygren H, Ouchterlony Ö, Tarkowski A. A solid-phase enzyme-linked immunospot (ELISPOT) assay for enumeration of specific antibody-secreting cells. J Immunol Methods. 1983;65:109–121. doi: 10.1016/0022-1759(83)90308-3. [DOI] [PubMed] [Google Scholar]
- 13.D’Elios M M, Manghetti M, Almerigogna F, Amedei A, Costa F, Burroni D, Baldari C T, Romagnani S, Telford J L, Del Prete G. Different cytokine profile and antigen-specificity repertoire in Helicobacter pylori-specific T cell clones from the antrum of chronic gastritis patients with or without peptic ulcer. Eur J Immunol. 1997;27:1751–1755. doi: 10.1002/eji.1830270723. [DOI] [PubMed] [Google Scholar]
- 14.Donati M, Moreno S, Storni E, Tucci A, Poli L, Mazzoni C, Varoli O, Sambri V, Farencena A, Cevenini R. Detection of serum antibodies to CagA and VacA and of serum neutralizing activity for vacuolating cytotoxin in patients with Helicobacter pylori-induced gastritis. Clin Diagn Lab Immunol. 1997;4:478–482. doi: 10.1128/cdli.4.4.478-482.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dunn B E, Campbell G P, Perez Perez G I, Blaser M J. Purification and characterization of urease from Helicobacter pylori. J Biol Chem. 1990;265:9464–9469. [PubMed] [Google Scholar]
- 16.Evans D G, Karjalainen T K, Evans D J, Jr, Graham D Y, Lee C H. Cloning, nucleotide sequence, and expression of a gene encoding an adhesin subunit protein of Helicobacter pylori. J Bacteriol. 1993;175:674–683. doi: 10.1128/jb.175.3.674-683.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Evans D J, Jr, Evans D G, Kirkpatrick S S, Graham D Y. Characterization of the Helicobacter pylori urease and purification of its subunits. Microb Pathog. 1991;10:15–26. doi: 10.1016/0882-4010(91)90062-f. [DOI] [PubMed] [Google Scholar]
- 18.Evans D J, Jr, Evans D G, Takemura T, Nakano H, Lampert H C, Graham D Y, Granger D N, Kvietys P R. Characterization of a Helicobacter pylori neutrophil-activating protein. Infect Immun. 1995;63:2213–2220. doi: 10.1128/iai.63.6.2213-2220.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goggin P M, Marrero J M, Spychal R T, Jackson P A, Corbishley C M, Northfield T C. Surface hydrophobicity of gastric mucosa in Helicobacter pylori infection: effect of clearance and eradication. Gastroenterology. 1992;103:1486–1490. doi: 10.1016/0016-5085(92)91168-4. [DOI] [PubMed] [Google Scholar]
- 20.Halstensen T S, Mollnes T E, Garred P, Fausa O, Brandtzaeg P. Epithelial deposition of immunoglobulin G1 and activated complement (C3b and terminal complement complex) in ulcerative colitis. Gastroenterology. 1990;98:1264–1271. doi: 10.1016/0016-5085(90)90343-y. [DOI] [PubMed] [Google Scholar]
- 21.Hamlet A K, Erlandsson K I, Olbe L, Svennerholm A M, Backman V E, Pettersson A B. A simple, rapid, and highly reliable capsule-based 14C urea breath test for diagnosis of Helicobacter pylori infection. Scand J Gastroenterol. 1995;30:1058–1063. doi: 10.3109/00365529509101607. [DOI] [PubMed] [Google Scholar]
- 22.Holmgren J, Svennerholm A-M. Bacterial enteric infections and vaccine development. Gastroenterol Clin N Am. 1992;21:283–302. [PubMed] [Google Scholar]
- 23.Jonson G, Svennerholm A-M, Holmgren J. Vibrio cholerae expresses cell surface antigens during intestinal infection which are not expressed during in vitro culture. Infect Immun. 1989;57:1809–1815. doi: 10.1128/iai.57.6.1809-1815.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kostrzynska M, Betts J D, Austin J W, Trust T J. Identification, characterization, and spatial localization of two flagellin species in Helicobacter pylori flagella. J Bacteriol. 1991;173:937–946. doi: 10.1128/jb.173.3.937-946.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee A, O’Rourke J, Corazon de Ungria M, Robertson B, Daskalopoulos G, Dixon M F. A standardized mouse model of Helicobacter pylori infection: introducing the Sydney strain. Gastroenterology. 1997;112:1386–1397. doi: 10.1016/s0016-5085(97)70155-0. [DOI] [PubMed] [Google Scholar]
- 26.Lee C K, Weltzin R, Thomas W D, Jr, Kleanthous H, Ermak T H, Soman G, Hill J E, Ackerman S K, Monath T P. Oral immunization with recombinant Helicobacter pylori urease induces secretory IgA antibodies and protects mice from challenge with Helicobacter felis. J Infect Dis. 1995;172:161–172. doi: 10.1093/infdis/172.1.161. [DOI] [PubMed] [Google Scholar]
- 27.Lindholm C, Osek J, Svennerholm A-M. Quantification of conserved antigens in Helicobacter pylori during different culture conditions. Infect Immun. 1997;65:5376–5380. doi: 10.1128/iai.65.12.5376-5380.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Luzza F, Imeneo M, Maletta M, Monteleone G, Doldo P, Biancone L, Pallone F. Isotypic analysis of specific antibody response in serum, saliva, gastric and rectal homogenates of Helicobacter pylori-infected patients. FEMS Immunol Med Microbiol. 1995;10:285–288. doi: 10.1111/j.1574-695X.1995.tb00045.x. [DOI] [PubMed] [Google Scholar]
- 29.Malaty H M, Engstrand L, Pedersen N L, Graham D Y. Helicobacter pylori infection: genetic and environmental influences. A study of twins. Ann Intern Med. 1994;120:982–986. doi: 10.7326/0003-4819-120-12-199406150-00002. [DOI] [PubMed] [Google Scholar]
- 30.Mattsson, A., et al. Unpublished data.
- 31.Mattsson A, Tinnert A, Hamlet A, Lönroth H, Bölin I, Svennerholm A-M. Specific antibodies in sera and gastric aspirates of symptomatic and asymptomatic Helicobacter pylori infected subjects. Clin Diagn Lab Immunol. 1998;5:288–293. doi: 10.1128/cdli.5.3.288-293.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mattsson, A., H. Lönroth, M. Quiding-Järbrink, and A.-M. Svennerholm. Induction of B-cell responses in the stomach of Helicobacter pylori infected subjects after oral cholera vaccination. J. Clin. Invest., in press. [DOI] [PMC free article] [PubMed]
- 33.McColl K E L. Helicobacter pylori infection and its role in human disease—an overview. Pharm World Sci. 1996;18:49–55. doi: 10.1007/BF00579705. [DOI] [PubMed] [Google Scholar]
- 34.McGhee J R. Molecular mechanisms of immunoglobulin A defense. Annu Rev Microbiol. 1989;43:503–536. doi: 10.1146/annurev.mi.43.100189.002443. [DOI] [PubMed] [Google Scholar]
- 35.Mestecky J. The common mucosal system and current strategies for induction of immune responses in external secretions. J Clin Immunol. 1987;7:265–276. doi: 10.1007/BF00915547. [DOI] [PubMed] [Google Scholar]
- 36.Mills S D, Kurjanczyk L A, Penner J L. Antigenicity of Helicobacter pylori lipopolysaccharides. J Clin Microbiol. 1992;30:3175–3180. doi: 10.1128/jcm.30.12.3175-3180.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mohammadi M, Czinn S, Redline R, Nedrud J. Helicobacter-specific cell-mediated immune responses display a predominant TH1 phenotype and promote a DTH response in the stomachs of mice. J Immunol. 1996;156:4729–4738. [PubMed] [Google Scholar]
- 38.Mohammadi M, Redline R, Nedrud J, Czinn S. Role of the host in pathogenesis of Helicobacter-associated gastritis: H. felis infection of inbred and congenic mouse strains. Infect Immun. 1996;64:238–245. doi: 10.1128/iai.64.1.238-245.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Moss S F, Calam J. Acid secretion and sensitivity to gastrin in duodenal ulcer patients: effect of eradicating the organism. Gut. 1993;34:888–892. doi: 10.1136/gut.34.7.888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Negrini R, Savio A, Poiesi C, Appelmelk B J, Buffoli F, Paterlini A, Cesari P, Graffeo M, Vaira D, Franzin G. Antigenic mimicry between Helicobacter pylori and gastric mucosa in the pathogenesis of body atrophic gastritis. Gastroenterology. 1996;111:655–665. doi: 10.1053/gast.1996.v111.pm8780570. [DOI] [PubMed] [Google Scholar]
- 41.O’Toole P W, Janzon L, Doig P, Huang J, Kostrzynska M, Trust T J. The putative neuraminyllactose-binding hemagglutinin HpaA of Helicobacter pylori CCUG 17874 is a lipoprotein. J Bacteriol. 1995;177:6049–6057. doi: 10.1128/jb.177.21.6049-6057.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.O’Toole P W, Logan S M, Kostrzynska M, Wadstrom T, Trust T J. Isolation and biochemical and molecular analyses of a species-specific protein antigen from the gastric pathogen Helicobacter pylori. J Bacteriol. 1991;173:505–513. doi: 10.1128/jb.173.2.505-513.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Parsonnet J, Friedman G D, Vandersteen D P, Chang Y, Vogelman J H, Orentreich N, Sibley R K. Helicobacter pylori infection and the risk of gastric carcinoma. N Engl J Med. 1991;325:1127–1131. doi: 10.1056/NEJM199110173251603. [DOI] [PubMed] [Google Scholar]
- 44.Peterson G L. A simplification of the protein assay method of Lowry et al. which is more generally applicable. Anal Biochem. 1977;83:346–356. doi: 10.1016/0003-2697(77)90043-4. [DOI] [PubMed] [Google Scholar]
- 45.Price A B. The Sydney system: histological division. J Gastroenterol Hepatol. 1991;6:209–222. doi: 10.1111/j.1440-1746.1991.tb01468.x. [DOI] [PubMed] [Google Scholar]
- 46.Quiding M, Nordström I, Kilander A, Andersson G, Hansson L-Å, Holmgren J, Czerkinsky C. Intestinal immune responses in humans. Oral cholera vaccination induces strong intestinal antibody responses and interferon-γ production and evokes local immunological memory. J Clin Invest. 1991;88:143–148. doi: 10.1172/JCI115270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rudin A, McConnell M M, Svennerholm A-M. Monoclonal antibodies against enterotoxigenic Escherichia coli colonization factor antigen I (CFA/I) that cross-react immunologically with heterologous CFAs. Infect Immun. 1994;62:4339–4346. doi: 10.1128/iai.62.10.4339-4346.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sarosiek J, Marshall B J, Peura D A, Hoffman S, Feng T, McCallum R W. Gastroduodenal mucus gel thickness in patients with Helicobacter pylori: a method for assessment of biopsy specimens. Am J Gastroentrol. 1992;86:729–734. [PubMed] [Google Scholar]
- 49.Sedgwick J D, Holt P G. A solid-phase immunoenzymatic technique for the enumeration of specific antibody-secreting cells. J Immunol Methods. 1983;57:301–309. doi: 10.1016/0022-1759(83)90091-1. [DOI] [PubMed] [Google Scholar]
- 50.Sharma S A, Miller G G, Perez-Perez G I, Grupta R S, Blaser M J. Humoral and cellular immune recognition of Helicobacter pylori proteins are not concordant. Clin Exp Immunol. 1994;97:126–132. doi: 10.1111/j.1365-2249.1994.tb06590.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sherburne R, Taylor D E. Helicobacter pylori expresses a complex surface carbohydrate, Lewis X. Infect Immun. 1995;63:4564–4568. doi: 10.1128/iai.63.12.4564-4568.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sipponen P, Hyvärinen H. Role of Helicobacter pylori in the pathogenesis of gastritis, peptic ulcer and gastric cancer. Scand J Gastroenterol Suppl. 1993;196:3–6. doi: 10.3109/00365529309098333. [DOI] [PubMed] [Google Scholar]
- 53.Stolte M, Eidt S, Ohnsmann A. Differences in H. pylori-associated gastritis in the antrum and body of the stomach. Z Gastroenterol. 1990;28:229–233. [PubMed] [Google Scholar]
- 54.Sugiyama, T., S. Furuyama, T. Awakawa, T. Kobayashi, T. Yabana, and A. Yachi. 1993. Local immune response in gastric mucosa to Helicobacter pylori infection with and without intestinal metaplasia. Eur. J. Gastroenterol. Hepatol. 5(Suppl. 1):119–122.
- 55.Svennerholm, A.-M., and D. G. Evans. Unpublished data.
- 56.Tinnert A, Mattsson A, Bölin I, Dalenbäck J, Hamlet A, Svennerholm A-M. Local and systemic immune responses in humans against Helicobacter pylori antigens from homologous and heterologous strains. Microb Pathog. 1997;23:285–296. doi: 10.1006/mpat.1997.0158. [DOI] [PubMed] [Google Scholar]
- 57.Valnes K, Brandtzaeg P, Elgjo K, Stave R. Quantitative distribution of immunoglobulin-producing cells in gastric mucosa: relation to chronic gastritis and glandular atrophy. Gut. 1986;27:505–514. doi: 10.1136/gut.27.5.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Walker R I. New strategies for using mucosal vaccination to achieve more effective immunization. Vaccine. 1994;12:387–400. doi: 10.1016/0264-410x(94)90112-0. [DOI] [PubMed] [Google Scholar]
- 59.Weel J F, van der Hulst R W, Gerrits Y, Roorda P, Feller M, Dankert J, Tytgat G N, van der Ende A. The interrelationship between cytotoxin-associated gene A, vacuolating cytotoxin, and Helicobacter pylori-related diseases. J Infect Dis. 1996;173:1171–1175. doi: 10.1093/infdis/173.5.1171. [DOI] [PubMed] [Google Scholar]
- 60.Westphal O, Jann K. Bacterial lipopolysaccharide: extraction with phenol-water and further applications of the procedure. In: Whitler R, editor. Methods in carbohydrate chemistry. New York, N.Y: Academic Press; 1965. pp. 83–92. [Google Scholar]
- 61.Wyatt J I, Rathbone B J. Immune response of the gastric mucosa to Campylobacter pylori. Scand J Gastroenterol Suppl. 1988;142:44–49. [PubMed] [Google Scholar]