Abstract
Background
Iron deficiency (ID) is often associated with other comorbidities in older patients and is a factor of morbimortality. However, the prevalence of ID remains poorly documented in this population.
Methods
The CARENFER PA study was a French multicenter cross-sectional study whose objective was to evaluate ID in patients (> 75 years) admitted to a geriatric unit. The primary endpoint was the ID prevalence defined as: serum ferritin < 100 µg/L and/or transferrin saturation coefficient (TSAT) < 20%. The Short Physical Performance Battery (SPPB) test was used to identify older patients at high risk of adverse events (e.g., disability, falls, hospitalization, death).
Results
A total of 888 patients (mean age, 85.2 years; women, 63.5%) from 16 French centers were included from October 2022 to December 2022. The prevalence of ID was 57.6% (95% CI, 54.3–60.9) in the cohort of older patients (62.6% in anemic and 53.3% in non-anemic patients; p = 0.0062). ID prevalence increased significantly with the presence of more than three comorbidities (65.6% vs. 55.9%; p = 0.0274), CRP ≥ 12 mg/L (73.0% vs. 49.3%; p < 0.001) and treatment that may influence ID/anemia (60.5% vs. 49.6%; p = 0.0042). In multivariate analysis, only CRP ≥ 12 mg/L was an independent predictive factor of ID (odds ratio, 2.78; 95% CI, 1.92–4.08; p < 0.001). SPPB scores were low (0–6) in 60.5% of patients with ID versus 48.6% of patients without ID (p = 0.0076).
Conclusion
More than half of older patients had ID, including non-anemic patients. ID was associated with the presence of inflammation and a low SPPB score.
Trial registration
Supplementary Information
The online version contains supplementary material available at 10.1186/s12877-024-04719-6.
Keywords: Iron deficiency, Older patient, Anemia, Serum ferritin, Intravenous iron, Transferrin saturation
Introduction
In addition to its key role in the synthesis of hemoglobin (Hb) and oxygen transport, iron is an essential element in many physiological processes such as energy metabolism, cardiac and peripheral muscle function [1]. Therefore, even though iron deficiency (ID) is a common cause of anemia, it can also be responsible for physiological and clinical disorders before the onset of anemia [2]. Anemia is the most common hematological disorder encountered in geriatric practice. Its prevalence, in the general ambulatory population, has been evaluated between 10 and 15% after 65 years of age and more than 20% beyond 85 years of age [3]. Approximately one third of cases of anemia in the older age group are attributable to iron, folic acid or B12 deficiency [3]. Anemia is associated with increased morbidity in terms of cardiac complications, cognitive decline, frailty, hospitalizations, impaired quality of life and increased mortality [4, 5].
ID is common in chronic diseases such as heart failure, chronic kidney disease (CKD) or cancer [6–9]. Independently of anemia, ID is also associated to more rapid clinical worsening in heart failure [10], non-dialysis CKD [11, 12] and cancer [13] and is a risk factor of mortality in patients with heart failure [10, 14] and CKD [11, 12]. Indeed, the treatment of ID allows restoring Hb levels, reduces the prescription of erythropoiesis-stimulating agents (ESA) and the need for transfusion in oncology [15], gastroenterology [16, 17] and nephrology [18–22]. The most useful biomarkers for assessing iron status are serum ferritin, which reflects iron stores, and transferrin saturation (TSAT), which is indicative of the iron transported in the circulation and available for cell metabolism [23]. ID is absolute when iron reserves are low; it is functional when iron mobilization is impaired despite normal reserves (and therefore not available for hematopoiesis), generally due to chronic inflammation which blocks intestinal iron absorption and inhibits iron export from macrophage and hepatocyte iron stores [2, 24].
The frailty of older patients, who often have several comorbidities, indicates the importance of better diagnosing ID in this population. However, there is no consensus definition of ID in the older population and no specific thresholds for biomarkers of iron metabolism. Nevertheless, taking into account recent publications on ID in different conditions (heart failure, chronic kidney disease, cancer) which are frequent in the older population, there is an emerging consensus to define ID in these chronic diseases by serum ferritin < 100 μg/L and/or TSAT < 20% [25–27]. Using this definition of ID, we evaluated the prevalence of ID in a national multicenter study in older patients admitted to a geriatric unit (hospitalized or outpatients); we also assessed the association between ID and a low SPPB score, which is a marker of a high risk of adverse events (e.g., disability, falls, hospitalization, death).
Methods
Type of study and patients
The CARENFER PA (“CARence EN FER Personnes Âgées”) study was a French multicenter cross-sectional study performed in geriatric centers. The study was interventional only because blood sampling and SPPB test were done at inclusion.
The main objective of this study was to evaluate the prevalence of ID in patients 75 years of age or older admitted to a geriatric unit. A secondary objective was to evaluate the association between ID and SPPB test score.
Patients were consecutively included if they met the following criteria: patient aged over 75; patient hospitalized in a geriatric ward or seen on an outpatient basis; patient with written consent; patient affiliated with or benefiting from a social security insurance. Protected patients were excluded (i.e. subject to a legal protection measure: guardianship, curatorship or safeguard of justice). Patients unable to understand what was asked of them were not included.
The consent was explained to the patient by the geriatrician. If the physician suspected cognitive decline, consent was explained to the patient's relative in the patient's presence. If the geriatrician thought the patient had not understood and/or the patient's relative objected to the consent, the patient was not included in the study.
The study conformed to the principles of the Declaration of Helsinki and Good Clinical Practice Guidelines. It was approved by a national independent Ethics Committee (“Comité de Protection des Personnes Ile de France III”) and written informed consent was obtained from all subjects participating in the trial. The trial was registered prior to patient enrollment at clinicaltrials.gov (NCT05514951, https://www.clinicaltrials.gov/ct2/show/NCT05514951; Date of registration: August 25, 2022).
Data collected
The main data collected during the inclusion visit were the followings: demographics (age, gender, height, weight), admission to geriatric unit (hospitalized, outpatient), comorbidities, treatment of anemia and/or iron deficiency (oral and intravenous iron, ESA, transfusion) and concomitant treatments possibly influencing ID or anemia (anticoagulant, proton pump inhibitor, platelet antiaggregant, other).
A blood test was performed within 48 h after inclusion for serum electrolytes, serum ferritin, TSAT, Hb, C-reactive protein (CRP), albumin and serum creatinine.
The Short Physical Performance Battery (SPPB) test was used to identify older patients at high risk of adverse events (e.g., disability, falls, hospitalization, death). It is composed of 3 parts: balance, repeated chair stands and gait speed [28]. Each of the three domains was scored from 0 (worst) to 4 (best) with a total score from 0 to 12 [29]. The global SPPB score interpretation was the following: 0–6, poor performance; 7–9, intermediate performance; 10–12, high performance.
Statistical analyses
The primary endpoint was the prevalence of ID defined as serum ferritin < 100 µg/L and/or TSAT < 20% [26]. Absolute ID was defined as serum ferritin < 100 µg/L and functional ID as serum ferritin ≥ 100 µg/L and TSAT < 20%.
ID prevalence was described with the Agresti-Coull confidence interval (CI). The analysis population included all patients who met the eligibility criteria and completed a blood test within 2 days of signing the written consent.
In the literature, ID prevalence in patients over 65 years of age is 10–15% [3]. With an assumption of 15% for the prevalence of ID in older patients, a precision of 2.4%, a first-order risk of 5% and 5% of patients not evaluable, 900 patients were to be included in this study.
Anemia was defined as Hb < 13 g/dL for men and Hb < 12 g/dL for women, according to World Health Organization (WHO) [30].
A multivariate logistic regression analysis was performed to define the factors associated to ID. Variables that were statistically significant in univariate analysis at a threshold ≤ 0.2 were entered into a multivariate analysis to be tested in a multivariate model with a risk alpha level set at p = 0.05.
The statistical analysis was performed with SAS software version 9.4 (SAS Institute, Inc., Cary, North Carolina, USA).
Results
Patient disposition and characteristics
A total of 902 patients were included in 16 centers from October 5, 2022 to December 9, 2022; 14 patients were excluded. Eligibility criteria not met for 5 patients (patient under 75 years of age, n = 1; protected patient, n = 4) and iron workup was not done or done 48 h after inclusion for 9 patients. The analysis population included 888 patients.
Patients had a mean (SD) age of 85.2 (5.6) years and 63.5% were women (Table 1). Admission to the geriatric unit led to hospitalization in 52.1% of cases, and 47.9% of patients were seen on an outpatient basis. At least one comorbidity was reported in almost all patients (93.2%); the main comorbidities were arterial hypertension (67.5%), diabetes (21.5%), heart failure (21.3%), ischemic heart disease (19.5%), CKD (18.7%) and cancer (10.0%).
Table 1.
Patient characteristics
| Characteristics | N | Analysis population (N = 888) |
|---|---|---|
| Age, years, mean (SD) | 888 | 85.2 (5.6) |
| Women, n (%) | 888 | 564 (63.5) |
| Admission to geriatric unit, n (%) | ||
| Hospitalized | 888 | 463 (52.1) |
| Outpatients | 888 | 425 (47.9) |
| Body mass index, kg/m2 | ||
| Mean (SD) | 860 | 25.8 (5.1) |
| Classes, n (%) | ||
| < 18.5 (underweight) | 860 | 42 (4.9) |
| 18.5–25 (normal) | 860 | 374 (43.5) |
| 25–30 (overweight) | 860 | 278 (32.3) |
| ≥ 30 (obesity) | 860 | 166 (19.3) |
| ≥ 1 comorbidity, n (%) | 888 | 828 (93.2) |
| Arterial hypertension | 888 | 599 (67.5) |
| Diabetes | 888 | 191 (21.5) |
| Heart failure | 888 | 189 (21.3) |
| Ischemic heart disease | 888 | 173 (19.5) |
| Chronic kidney disease | 888 | 166 (18.7) |
| Cancer | 888 | 89 (10.0) |
| At least one treatment of ID or anemia, n (%) | 888 | 142 (16.0) |
| Folic acid (ongoing at inclusion) | 888 | 69 (7.8) |
| Vitamin B12 (ongoing at inclusion) | 888 | 27 (3.0) |
| Oral iron (ongoing at inclusion) | 888 | 39 (4.4) |
| Transfusion (within 3 months) | 888 | 41 (4.6) |
| Intravenous iron (within 3 months) | 888 | 23 (2.6) |
| ESA (within 3 months) | 888 | 8 (0.9) |
| ≥ 1 treatment with an impact on ID or anemia, n (%) | 888 | 655 (73.8) |
| Anticoagulant | 888 | 374 (42.1) |
| Proton pump inhibitor | 888 | 303 (34.1) |
| Platelet antiaggregant | 888 | 234 (26.4) |
| Other | 888 | 28 (3.2) |
| Biological parameters, mean (SD) | ||
| Serum ferritin, µg/L | 872 | 262.5 (302.9) |
| Transferrin saturation (TSAT), % | 852 | 23.9 (14.0) |
| Hb, g/dL | 874 | 12.2 (1.9) |
| C-reactive protein, mg/L | 869 | 24.4 (44.9) |
| Serum creatinine, µmol/L | 879 | 92.6 (57.6) |
| Glomerular filtration rate,a mL/min/1.73 m2 | 878 | 62.7 (20.1) |
| Serum albumin, g/L | 853 | |
| Mean (SD) | 35.9 (6.1) | |
| > 54 | 0 | |
| [34–54]b | 560 (65.7) | |
| < 34 | 293 (34.3) | |
| Serum potassium, mmol/L | 874 | |
| Mean (SD) | 4.13 (0.47) | |
| > 5.5 | 5 (0.6) | |
| [3.5–5.5]b | 810 (92.7) | |
| < 3.5 | 59 (6.8) | |
ESA erythropoiesis stimulating-agent, Hb hemoglobin, ID iron deficiency
aCalculated with CKD-EPI formula
bNormal range
Biological parameters are described in Table 1. Mean (SD) values of CRP were elevated at 24.4 (44.9) mg/L with CRP > 5 mg/L in 52.1% of patients.
At least one specific treatment of iron deficiency and/or anemia was reported by 16.0% of patients, either ongoing treatment (folic acid, 7.8%; Vitamin B12, 3.0%; oral iron, 4.4%) or within last 3 months (transfusion, 4.6%; intravenous iron, 2.6%; ESA, 0.9%) (Table 1).
At least one treatment with an impact on ID or anemia was reported at inclusion for 655 (73.8%) patients (anticoagulant, 42.1%; proton pump inhibitor, 34.1%; platelet antiaggregant, 26.4%).
Prevalence of iron deficiency and/or anemia
The prevalence of ID was 57.6% (95% CI, 54.3–60.9) in the cohort of older patients admitted in geriatric unit (Table 2). Among ID patients, ID was absolute in 56.2% and functional in 43.8%.
Table 2.
Prevalence of iron deficiency in analysis population
| Parameters of iron deficiency | N | Analysis population (N = 888) |
|---|---|---|
| Iron deficiencya | ||
| n (%) | 859 | 495 (57.6) |
| 95% CI, % | 859 | 54.3–60.9 |
| Absolute iron deficiency (serum ferritin < 100 µg/L), n (%) | 495 | 278 (56.2) |
| Functional iron deficiency (serum ferritin ≥ 100 µg/L and TSAT < 20%), n (%) | 495 | 217 (43.8) |
CI confidence interval, TSAT transferrin saturation
aDefined as serum ferritin < 100 µg/L and/or TSAT < 20%
The prevalence of anemia was 48.5% (95% CI, 45.2–51.8). ID was significantly more frequent in anemic patients (62.6%; 95% CI 57.8–67.1) than in non-anemic patients (53.3%; 95% CI, 48.6–57.9; p = 0.0062).
ID was assessed in different subgroups presented in Fig. 1. ID was significantly more frequent in patients with > 3 comorbidities (65.6% vs. 55.9%; p = 0.0274), those receiving a treatment with a possible impact on ID or anemia (60.5% vs. 49.6%; p = 0.0042) or those with CRP ≥ 5 mg (64.8% vs. 49.6%; p < 0.001). The ROC curve method showed that a CRP threshold at 12 mg/mL was optimal for diagnosing ID. With this threshold, the difference of ID prevalence for inflammation vs. no inflammation was more marked (73.0% vs. 49.3%; p < 0.001). No specific pharmacological class for the treatment of ID/anemia or with a possible impact on ID could be evidenced with a significant effect on ID prevalence (Supplementary Table S1).
Fig. 1.
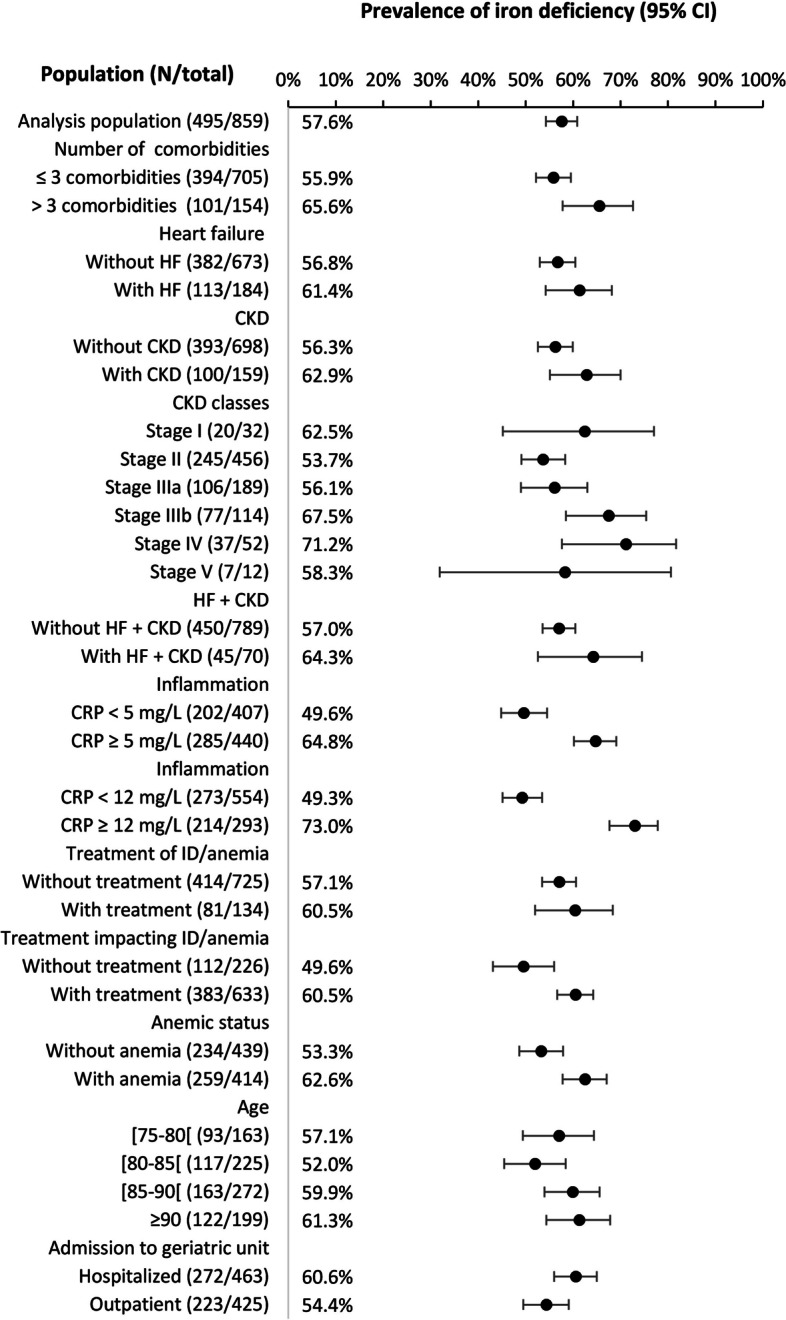
Prevalence of iron deficiency in different subgroups
ID prevalence was high whatever patient age (from 52.0% to 61.3%) or the type of admission to geriatric unit (60.6% for hospitalized patients and 54.4% for outpatients) (Fig. 1). ID prevalence was 61.4% in patients with heart failure, 62.9% in patients with CKD and 64.3% patients with both CKD and heart failure.
In univariate analysis, > 3 comorbidities, CRP ≥ 12 mg/L, anemia, low serum albumin, and stages III-IV-V vs. I-II of renal failure were significantly associated with ID (Supplementary Table S2). In multivariate analysis, CRP ≥ 12 mg was the only independent predictive factor of ID (odds ratio, 2.78; 95% CI, 1.92–4.08; p < 0.001) (Supplementary Table S3).
SPPB test scores in patients with iron deficiency
In the 661 patients with available data for both iron status and SPPB test, scores were significantly lower in patients with ID than in patients without ID for global score and each dimension of SPPB (Table 3). Scores were low (SPPB 0–6) in 60.5% of patients with ID and in 48.6% of patients without ID (p = 0.0076). Low scores were reported in 40.8% of patients without ID and without anemia and in 74.3% of patients with both ID and anemia (Fig. 2A). In CKD patients, scores were low in 61.0% of patients without ID and 69.7% with ID; in patients with heart failure, these rates were 68.8% and 77.3%, respectively (Fig. 2B).
Table 3.
SPPB test scores according to iron deficiency
| SPPB items | N | Without ID N = 364 |
N | With ID N = 495 |
N | Total N = 859 |
P-value |
|---|---|---|---|---|---|---|---|
| Dimensions, median (IQR) | |||||||
| Balance score | 284 | 3 (1; 4) | 377 | 2 (1; 4) | 661 | 2 (1; 4) | 0.0115 |
| Gait speed score | 284 | 3 (1; 4) | 377 | 2 (1; 4) | 661 | 2 (1; 4) | 0.0445 |
| Repeated chair stand score | 284 | 1 (0; 3) | 377 | 1 (0; 2) | 661 | 1 (0; 2) | 0.0101 |
| Global score, median (IQR) | 284 | 7 (4; 9) | 377 | 5 (3; 9) | 661 | 6 (3; 9) | 0.0058 |
| Global score interpretation, n (%) | |||||||
| Poor performance (SPPB 0–6) | 284 | 138 (48.6) | 377 | 228 (60.5) | 661 | 366 (55.4) | 0.0076 |
| Intermediate performance (SPPB 7–9) | 284 | 91 (32.0) | 377 | 87 (23.1) | 661 | 178 (26.9) | |
| High performance (SPPB 10–12) | 284 | 55 (19.4) | 377 | 62 (16.4) | 661 | 117 (17.7) | |
ID iron deficiency, IQR interquartile range, SPPB Short Physical Performance Battery
Fig. 2.
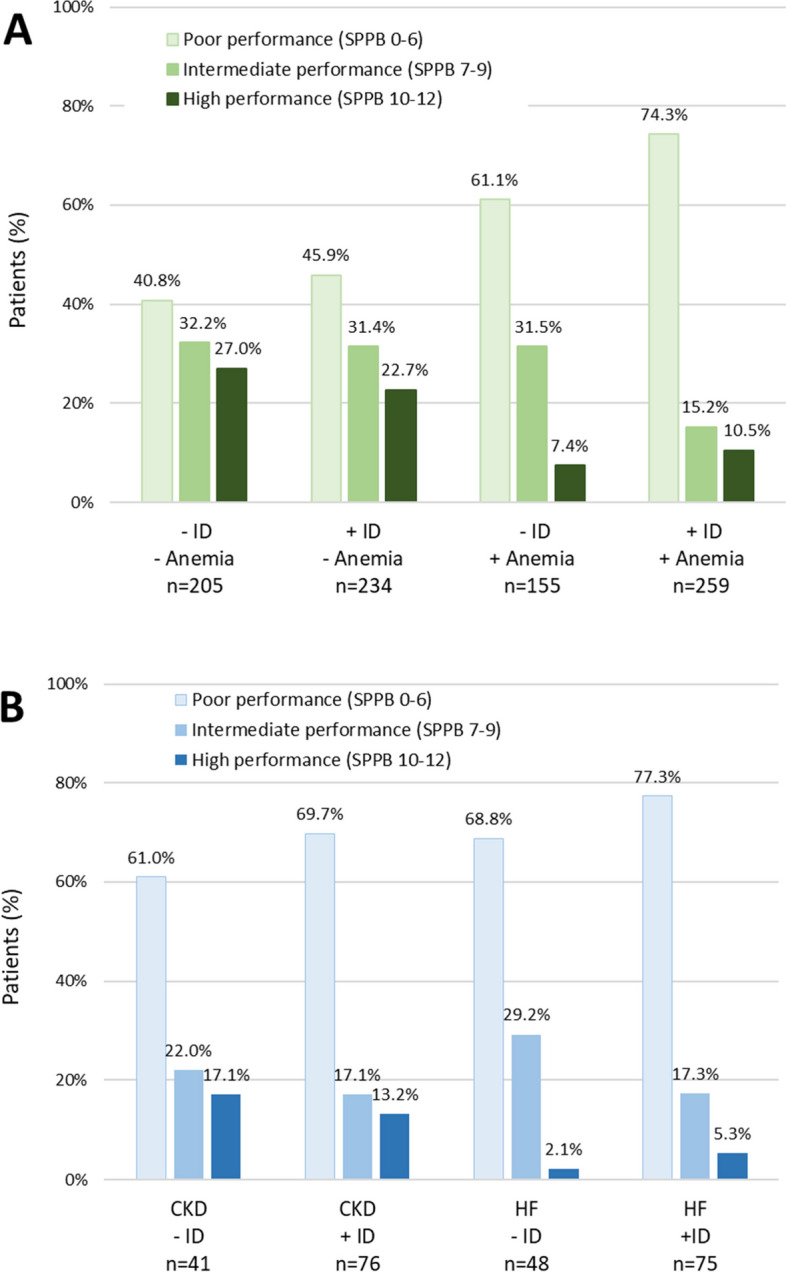
Physical performance (SPPB score) of older patients: A, according to iron deficiency (ID) and/or anemia; B, in patients with chronic kidney disease (CKD) or heart failure (HF)
Discussion
In this large multicenter cross-sectional study, we found that more than half of patients admitted to a geriatric unit had ID (with about half absolute ID and half functional ID). Of note, half of ID patients were non-anemic. ID was associated with low SPPB score, which is predictive of high risk of adverse events (e.g., disability, falls, hospitalization, death).
Only few studies have specifically assessed the prevalence of ID in geriatric population while this topic is more often addressed in relation with anemia. As a consequence, ID-related anemia is often erroneously considered as a synonymous of ID. Because ID often precedes the onset of anemia, evaluating ID through only ID-related anemia underestimates the prevalence of ID. Thus, in the NHANES III study, nutrient deficiency was reported in about one-third of patients aged 65 years and older with anemia; half of these cases were related to ID [3]. In a single-center observational study performed in Germany in 2,191 patients ≥ 65 years undergoing major surgery, 791 were anemic (36.1%) and 276 (12.6%) were diagnosed with ID-related anemia [31]. In the DO-HEALTH study in 2,157 relatively healthy European adults aged 70 and older, ID prevalence defined by soluble transferrin receptor (sTfR) > 28.1 nmol/L was 26.8% [32]. In the study of Neidlein et al. in patients aged 65 years and over admitted to a geriatric ward, 41% had ID (defined as serum ferritin < 30 ng/mL and TSAT < 16% for absolute ID and serum ferritin ≥ 30 µg/L and TSAT < 16% for functional ID) [33]. The prevalence of non-anemic ID defined as serum ferritin < 30 µg/L was 8.8% in an English cohort of 4,451 adults of 45 years and older by Philip et al.; however this criterion evaluated only absolute ID [34]. Among 149 community-dwelling patients aged 55 years and older with a general good health status, ID (defined as serum ferritin < 15 µg/L or two other ID biomarkers) was diagnosed in 29.5% [35].
Comparisons between clinical studies are difficult because there is no consensus for definition of ID and for the thresholds of the available tests which frequently vary according to authors and clinical setting. For the present study, we have chosen a definition for which a consensus is emerging in patients with chronic diseases, namely serum ferritin < 100 μg/L and/or TSAT < 20% [25–27]. Indeed, in older patients, the underlying cause of ID is often multifactorial because several chronic comorbidities are frequently present. In the other CARENFER studies, high ID prevalence was reported in patients with cancer (57.9%) [6], heart failure (49.6%) [7], inflammatory bowel diseases (23.7%) [9] CKD (47.1%) [8] or preoperatively in patients undergoing major elective surgery (47.0%) [36]. By using a common definition of ID (serum ferritin < 100 μg/L and/or TSAT < 20%), the prevalence rates for the different chronic conditions were 58.1% in cancer, 62.8% in heart failure, 61.2% in inflammatory bowel disease and 47.1% in CKD [26]. A study in 101 US anemic veterans classified patients as iron deficient or iron sufficient on the basis of bone marrow hemosiderin, which is considered the gold standard for assessing iron stores [37]. Of interest, serum ferritin ≤ 100 µg/L had high specificity for the diagnosis of ID in these older patients with a wide variety of concomitant diseases and low TSAT had an even better diagnostic performance for ID. Other studies have also reported that the serum ferritin threshold for ID diagnosis should be higher for older patients than for the younger population [38, 39].
The patients from our cohort had the demographic characteristics and comorbidities of the geriatric population seen routinely in the hospital or included in real-life clinical studies [40]. Although the number of comorbidities aggravated ID, each of them had only a limited impact and ID seemed to be primarily associated with old person status. Only inflammation appeared to have a significant impact on ID prevalence and was the only independent factor predictive of ID in the multivariate analysis. Thus, at the CRP threshold of 12 mg/L, ID prevalence varied significantly from 49.3% (CRP < 12 mg/L) to 73.0% (CRP ≥ 12 mg/L). The inflammatory status is an important point to consider for ID treatment. Inflammation is often present in chronic diseases and has a significant impact on iron mobilization. Indeed, inflammation induces the synthesis of hepcidin by the liver; hepcidin in turn blocks iron export from intestinal cells and macrophages recycling iron, thus leading to a functional ID [2]. As a consequence, intravenous iron, which bypasses the intestinal barrier, is more effective than oral iron in inflammatory setting [41]. In our cohort, only a limited percentage of patients were treated for ID and/or anemia. Less than 3% received intravenous iron which is the preferred treatment of ID in inflammatory chronic diseases.
Patients with ID had lower scores to the SPPB test compared to patients without ID. Although we cannot conclude to a causal relationship between ID and low performance, these results are of interest since lower scores with SPPB have been associated with falls, hospitalization, long-term care needs, frailty and all-cause mortality [28]. In addition to erythropoiesis, iron is also involved in the physiology of skeletal muscle, which is highly dependent on iron for the synthesis of myoglobin and for energy production to support mechanical contraction [42]. Thus, ID is associated with impaired exercise capacity, due to a decrease of oxygen storage in myoglobin, decrease of energetic efficiency and mitochondrial dysfunction [43]. Our results are in line with those of Neidlein et al. who evaluated functional status (handgrip strength, isometric knee extension strength, walking, climbing stairs) during hospitalization in a geriatric population [33]. ID was an independent risk factor for fatigue and functional status on admission and during hospital stay.
The strengths of our study are the multicenter design and the large number of patients included. Our study is one of the few to have addressed the subject of ID in older patients, and such data were lacking in France. Moreover, our study is the first to evaluate physical performance in older patients with ID. However, our study has some limitations. Data were obtained from 16 centers spread over the French territory, but we cannot exclude some biases in patient recruitment, in particular because of the different profiles of hospitalized patients and outpatients. However, ID prevalence was high in each of the centers and therefore does not call into question the main conclusion of the study. The study was designed to evaluate ID prevalence and we did not evaluate the impact of iron supplementation, particularly on SPPB scores.
In conclusion, ID was diagnosed in more than half of patients admitted to a geriatric unit – both in non-anemic and anemic patients – and was associated to inflammation. ID was also associated to a low SPPB score which is a factor of poor prognosis. These new data underline the importance of more systematic screening of ID in the older population. Future randomized controlled trials will have to assess the efficacy of iron supplementation on physical performance and outcome of older iron-deficient patients.
Supplementary Information
Additional file 1: Supplementary Table S1. Prevalence of iron deficiency according to treatment of iron deficiency/anemia or treatment with a possible impact on iron deficiency/anemia (analysis population, N=888). Supplementary Table S2. Univariate analysis of factors associated with iron deficiency (N=859). Supplementary Table S3. Multivariate analysis of factors associated with iron deficiency (N=859).
Acknowledgements
* We thank the investigators of the CARENFER PA study: Dr Anne-Sophie Billet (CH Chambery), Dr Florent Fiasson (Hôpital Saint-Jean-de-Luz), Dr Antoine Garnier-Crussard (HCL, Lyon), Dr Isabelle Goidin (CH Calais), Pr Marc Paccalin (CHU Poitiers), Dr Laure Parnet (CH Sud Francilien), Dr Mikel Sarasibar (CH Pau) and Dr Caroline Thomas (Hôpital Saint-Antoine, APHP).
Abbreviations
- CKD
Chronic kidney disease
- CRP
C-reactive protein
- ESA
Erythropoiesis stimulating-agent
- ID
Iron deficiency
- SPPB
Short Physical Performance Battery
- TSAT
Transferrin saturation coefficient
Authors’ contributions
BF, FP, PCh and PCa have made substantial contributions to conception and design. BF, FP, PCh, CA, EM, LJ, FB and AEA have participated to the data collection. BF, FP, PCh, VDF and PCa have participated to the statistical analyses. BF wrote the manuscript. BF, FP, PC, VDF and PC have made substantial contributions to the final manuscript. All authors read and approved the final manuscript.
Funding
The CARENFER PA study was funded by CSL VIFOR.
Availability of data and materials
The datasets used and analyzed during the current study will be made available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study conformed to the principles of the Declaration of Helsinki and Good Clinical Practice Guidelines. It was approved by a national independent Ethics Committee (“Comité de Protection des Personnes Ile de France III”) and written informed consent was obtained from all subjects participating in the trial.
Consent for publication
Not applicable.
Competing interests
B. Fougère: consultancies, honoraria, advisory board, speakers: AstraZeneca, Bayer, Biogen, Biophitys, BMS, Boehringer-Ingelheim, CSL Vifor, GSK, MSD, Nestlé, Novartis, Pfizer.
F. Puisieux: consultancies, honoraria, advisory board, speakers’ fees: Bayer, BMS, Boehringer-Ingelheim, CSL Vifor, GSK, MSD, Sanofi, Novartis, Pfizer.
P. Chevalet: speaker’s fees for Vifor.
C. Annweiler: no conflict of interest.
E. Michel: no conflict of interest.
L. Joly: no conflict of interest.
F. Blanc: no conflict of interest.
A. El Azouzi: no conflict of interest.
V. Desré-Follet: employee of CSL Vifor, France.
P. Cacoub: consultancies, honoraria, advisory board, speakers’ fees: Alnylam, Innotech, Mylan, Pfizer, Servier, and Vifor.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Bertrand Fougère, Email: bertrand.fougere@univ-tours.fr.
on behalf of the CARENFER PA study group*:
Anne-Sophie Billet, Florent Fiasson, Antoine Garnier-Crussard, Isabelle Goidin, Marc Paccalin, Laure Parnet, Mikel Sarasibar, and Caroline Thomas
References
- 1.Camaschella C. Iron deficiency. Blood. 2019;133:30–39. doi: 10.1182/blood-2018-05-815944. [DOI] [PubMed] [Google Scholar]
- 2.Pasricha SR, Tye-Din J, Muckenthaler MU, Swinkels DW. Iron deficiency. Lancet. 2021;397:233–248. doi: 10.1016/S0140-6736(20)32594-0. [DOI] [PubMed] [Google Scholar]
- 3.Guralnik JM, Eisenstaedt RS, Ferrucci L, Klein HG, Woodman RC. Prevalence of anemia in persons 65 years and older in the United States: evidence for a high rate of unexplained anemia. Blood. 2004;104:2263–2268. doi: 10.1182/blood-2004-05-1812. [DOI] [PubMed] [Google Scholar]
- 4.Culleton BF, Manns BJ, Zhang J, Tonelli M, Klarenbach S, Hemmelgarn BR. Impact of anemia on hospitalization and mortality in older adults. Blood. 2006;107:3841–3846. doi: 10.1182/blood-2005-10-4308. [DOI] [PubMed] [Google Scholar]
- 5.Pang WW, Schrier SL. Anemia in the elderly. Curr Opin Hematol. 2012;19:133–140. doi: 10.1097/MOH.0b013e3283522471. [DOI] [PubMed] [Google Scholar]
- 6.Luporsi E, Turpin A, Massard V, Morin S, Chauffert B, Carnot A, Cacoub P. Behalf of the CARENFER Study Group: Iron deficiency in patients with cancer: a prospective cross-sectional study. BMJ Support Palliat Care. 2021:bmjspcare-2021-002913. 10.1136/bmjspcare-2021-002913. [DOI] [PubMed]
- 7.Cohen-Solal A, Philip JL, Picard F, Delarche N, Taldir G, Gzara H, Korichi A, Trochu JN, Cacoub P, Group CS Iron deficiency in heart failure patients: the French CARENFER prospective study. ESC Heart Fail. 2022;9:874–884. doi: 10.1002/ehf2.13850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Choukroun G, Kazes I, Dantal J, Vabret E, Couzi L, Le Meur Y, Trochu JN, Cacoub P. investigateurs de l'etude CI: [Prevalence of iron deficiency in patients with non-dialysis chronic kidney disease: The CARENFER national, multicentre, observational study] Nephrol Ther. 2022;18:195–201. doi: 10.1016/j.nephro.2021.12.003. [DOI] [PubMed] [Google Scholar]
- 9.Peyrin-Biroulet L, Bouguen G, Laharie D, Pellet G, Savoye G, Gilletta C, Michiels C, Buisson A, Fumery M, Trochu JN, et al. Iron Deficiency in Patients with Inflammatory Bowel Diseases: A Prospective Multicenter Cross-Sectional Study. Dig Dis Sci. 2022;67:5637–5646. doi: 10.1007/s10620-022-07474-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Klip IT, Comin-Colet J, Voors AA, Ponikowski P, Enjuanes C, Banasiak W, Lok DJ, Rosentryt P, Torrens A, Polonski L, et al. Iron deficiency in chronic heart failure: an international pooled analysis. Am Heart J. 2013;165(575–582):e573. doi: 10.1016/j.ahj.2013.01.017. [DOI] [PubMed] [Google Scholar]
- 11.Cho ME, Hansen JL, Peters CB, Cheung AK, Greene T, Sauer BC. An increased mortality risk is associated with abnormal iron status in diabetic and non-diabetic Veterans with predialysis chronic kidney disease. Kidney Int. 2019;96:750–760. doi: 10.1016/j.kint.2019.04.029. [DOI] [PubMed] [Google Scholar]
- 12.Eisenga MF, Nolte IM, van der Meer P, Bakker SJL, Gaillard C. Association of different iron deficiency cutoffs with adverse outcomes in chronic kidney disease. BMC Nephrol. 2018;19:225. doi: 10.1186/s12882-018-1021-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ludwig H, Muldur E, Endler G, Hubl W. Prevalence of iron deficiency across different tumors and its association with poor performance status, disease status and anemia. Ann Oncol. 2013;24:1886–1892. doi: 10.1093/annonc/mdt118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jankowska EA, Kasztura M, Sokolski M, Bronisz M, Nawrocka S, Oleskowska-Florek W, Zymlinski R, Biegus J, Siwolowski P, Banasiak W, et al. Iron deficiency defined as depleted iron stores accompanied by unmet cellular iron requirements identifies patients at the highest risk of death after an episode of acute heart failure. Eur Heart J. 2014;35:2468–2476. doi: 10.1093/eurheartj/ehu235. [DOI] [PubMed] [Google Scholar]
- 15.Marinho J, Leao I, Custodio S, Dias E, Moreira Pinto A, Costa T, Capela A, Dias M, Coelho H, Cunha A, et al. Ferric Carboxymaltose in the treatment of chemotherapy-induced anaemia: an effective, safe and cost- sparing alternative to blood transfusion. Sci Rep. 2019;9:20410. doi: 10.1038/s41598-019-56999-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aksan A, Isik H, Radeke HH, Dignass A, Stein J. Systematic review with network meta-analysis: comparative efficacy and tolerability of different intravenous iron formulations for the treatment of iron deficiency anaemia in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2017;45:1303–1318. doi: 10.1111/apt.14043. [DOI] [PubMed] [Google Scholar]
- 17.Aksan A, Schoepfer A, Juillerat P, Vavricka S, Bettencourt M. Ramirez de Arellano A, Gavata S, Morin N, Valentine WJ, Hunt B: Iron Formulations for the Treatment of Iron Deficiency Anemia in Patients with Inflammatory Bowel Disease: A Cost-Effectiveness Analysis in Switzerland. Adv Ther. 2021;38:660–677. doi: 10.1007/s12325-020-01553-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Macdougall IC, Tucker B, Thompson J, Tomson CR, Baker LR, Raine AE. A randomized controlled study of iron supplementation in patients treated with erythropoietin. Kidney Int. 1996;50:1694–1699. doi: 10.1038/ki.1996.487. [DOI] [PubMed] [Google Scholar]
- 19.Rottembourg J, Sonigo Y, Dansaert A, Diaconita M, Guerin A. Intravenous iron during predialysis period improves anemia management and cardiovascular parameters in incident hemodialysis patients. Nephrol Ther. 2013;9:486–493. doi: 10.1016/j.nephro.2013.07.364. [DOI] [PubMed] [Google Scholar]
- 20.Rottembourg J, Rostoker G. Use of intravenous iron supplementation in chronic kidney disease: Interests, limits, and recommendations for a better practice. Nephrol Ther. 2015;11:531–542. doi: 10.1016/j.nephro.2015.04.009. [DOI] [PubMed] [Google Scholar]
- 21.Rottembourg J. Other Estimation of Blood Losses in Hemodialysis and Formula for Translating Liver Iron Concentration From Iron Balance Calculation Based on Iron Removal by Phlebotomy. Kidney Int Rep. 2018;3:220. doi: 10.1016/j.ekir.2017.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Toblli JE, Lombrana A, Duarte P, Di Gennaro F. Intravenous iron reduces NT-pro-brain natriuretic peptide in anemic patients with chronic heart failure and renal insufficiency. J Am Coll Cardiol. 2007;50:1657–1665. doi: 10.1016/j.jacc.2007.07.029. [DOI] [PubMed] [Google Scholar]
- 23.Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, Gonzalez-Juanatey JR, Harjola VP, Jankowska EA, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129–2200. doi: 10.1093/eurheartj/ehw128. [DOI] [PubMed] [Google Scholar]
- 24.Batchelor EK, Kapitsinou P, Pergola PE, Kovesdy CP, Jalal DI. Iron Deficiency in Chronic Kidney Disease: Updates on Pathophysiology, Diagnosis, and Treatment. J Am Soc Nephrol. 2020;31:456–468. doi: 10.1681/ASN.2019020213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cacoub P, Vandewalle C, Peoc'h K. Using transferrin saturation as a diagnostic criterion for iron deficiency: A systematic review. Crit Rev Clin Lab Sci. 2019;56:526–532. doi: 10.1080/10408363.2019.1653820. [DOI] [PubMed] [Google Scholar]
- 26.Cacoub P, Choukroun G, Cohen-Solal A, Luporsi E, Peyrin-Biroulet L, Peoc'h K, Andrieu V, Lasocki S, Puy H, Trochu JN. Towards a Common Definition for the Diagnosis of Iron Deficiency in Chronic Inflammatory Diseases. Nutrients. 2022;14(5):1039. doi: 10.3390/nu14051039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peyrin-Biroulet L, Williet N, Cacoub P. Guidelines on the diagnosis and treatment of iron deficiency across indications: a systematic review. Am J Clin Nutr. 2015;102:1585–1594. doi: 10.3945/ajcn.114.103366. [DOI] [PubMed] [Google Scholar]
- 28.Western MJ, Malkowski OS. Associations of the Short Physical Performance Battery (SPPB) with Adverse Health Outcomes in Older Adults: A 14-Year Follow-Up from the English Longitudinal Study of Ageing (ELSA) Int J Environ Res Public Health. 2022;19(23):16319. doi: 10.3390/ijerph192316319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, Scherr PA, Wallace RB. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–94. doi: 10.1093/geronj/49.2.M85. [DOI] [PubMed] [Google Scholar]
- 30.Nutritional anaemias. Report of a WHO scientific group. World Health Organ Tech Rep Ser. 1968;405:5–37. [PubMed]
- 31.Blum LV, Zierentz P, Hof L, Kloka JA, Messroghli L, Zacharowski K, Meybohm P, Choorapoikayil S. The impact of intravenous iron supplementation in elderly patients undergoing major surgery. BMC Geriatr. 2022;22:293. doi: 10.1186/s12877-022-02983-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stahl-Gugger A, de Godoi Rezende Costa Molino C, Wieczorek M, Chocano-Bedoya PO, Abderhalden LA, Schaer DJ, Spahn DR, Orav EJ, Vellas B, da Silva JAP, et al. Prevalence and incidence of iron deficiency in European community-dwelling older adults: an observational analysis of the DO-HEALTH trial. Aging Clin Exp Res. 2022;34:2205–2215. doi: 10.1007/s40520-022-02093-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Neidlein S, Wirth R, Pourhassan M. Iron deficiency, fatigue and muscle strength and function in older hospitalized patients. Eur J Clin Nutr. 2021;75:456–463. doi: 10.1038/s41430-020-00742-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Philip KEJ, Sadaka AS, Polkey MI, Hopkinson NS, Steptoe A, Fancourt D. The prevalence and associated mortality of non-anaemic iron deficiency in older adults: a 14 years observational cohort study. Br J Haematol. 2020;189:566–572. doi: 10.1111/bjh.16409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Portugal-Nunes C, Castanho TC, Amorim L, Moreira PS, Mariz J, Marques F, Sousa N, Santos NC, Palha JA. Iron Status is Associated with Mood, Cognition, and Functional Ability in Older Adults: A Cross-Sectional Study. Nutrients. 2020;12(11):3594. doi: 10.3390/nu12113594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Capdevila X, Lasocki S, Duchalais A, Rigal JC, Mertl P, Ghewy P, Farizon F, Lanz T, Buckert A, Belarbia S, et al. Perioperative Iron Deficiency in Patients Scheduled for Major Elective Surgeries: A French Prospective Multicenter Cross-Sectional Study. Anesth Analg. 2023;137(2):322–331. doi: 10.1213/ANE.0000000000006445. [DOI] [PubMed] [Google Scholar]
- 37.Kis AM, Carnes M. Detecting iron deficiency in anemic patients with concomitant medical problems. J Gen Intern Med. 1998;13:455–461. doi: 10.1046/j.1525-1497.1998.00134.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Babaei M, Shafiei S, Bijani A, Heidari B, Hosseyni SR, Vakili Sadeghi M. Ability of serum ferritin to diagnose iron deficiency anemia in an elderly cohort. Rev Bras Hematol Hemoter. 2017;39:223–228. doi: 10.1016/j.bjhh.2017.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Holyoake TL, Stott DJ, McKay PJ, Hendry A, MacDonald JB, Lucie NP. Use of plasma ferritin concentration to diagnose iron deficiency in elderly patients. J Clin Pathol. 1993;46:857–860. doi: 10.1136/jcp.46.9.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hanon O, Vidal JS, Pisica-Donose G, Orvoen G, David JP, Chaussade E, Caillard L, de Jong LW, Boulloche N, Vinsonneau U, et al. Bleeding risk with rivaroxaban compared with vitamin K antagonists in patients aged 80 years or older with atrial fibrillation. Heart. 2021;107:1376–1382. doi: 10.1136/heartjnl-2020-317923. [DOI] [PubMed] [Google Scholar]
- 41.Auerbach M, Coyne D, Ballard H. Intravenous iron: from anathema to standard of care. Am J Hematol. 2008;83:580–588. doi: 10.1002/ajh.21154. [DOI] [PubMed] [Google Scholar]
- 42.Cairo G, Bernuzzi F, Recalcati S. A precious metal: Iron, an essential nutrient for all cells. Genes Nutr. 2006;1:25–39. doi: 10.1007/BF02829934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Haas JD. Brownlie Tt: Iron deficiency and reduced work capacity: a critical review of the research to determine a causal relationship. J Nutr. 2001;131:676S–688S. doi: 10.1093/jn/131.2.676S. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Supplementary Table S1. Prevalence of iron deficiency according to treatment of iron deficiency/anemia or treatment with a possible impact on iron deficiency/anemia (analysis population, N=888). Supplementary Table S2. Univariate analysis of factors associated with iron deficiency (N=859). Supplementary Table S3. Multivariate analysis of factors associated with iron deficiency (N=859).
Data Availability Statement
The datasets used and analyzed during the current study will be made available from the corresponding author on reasonable request.


