Abstract
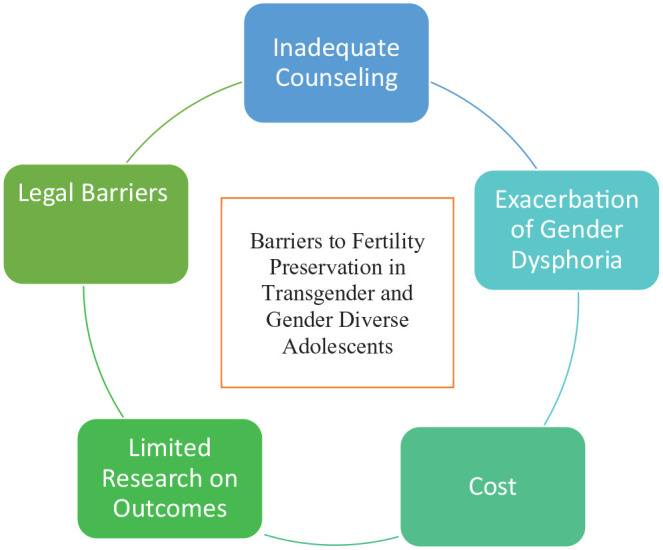
Fertility preservation (FP) involves the cryopreservation of gametes, embryos, and/or gonadal tissue oocytes, for future use in family building. FP as part of a comprehensive approach to care of transgender and gender diverse (TGD) individuals is an understudied topic. Current evidence indicates that gender affirming therapies may increase the risk for infertility. As a result, TGD individuals, including adolescents, should receive counseling regarding FP prior to beginning gender affirming treatment. Many barriers exist to TGD adolescents receiving FP counseling and undergoing FP if desired. The objective of this narrative review is to summarize the literature regarding the desire for FP in TGD adolescents, the barriers to TGD adolescents in accessing of FP, and to discuss potential interventions for alleviation of such barriers. A literature search using the following Medical Subject Headings search terms: ‘transgender persons’ and ‘fertility preservation’ and ‘adolescents’ was conducted via searching PubMed. Additional articles were located via reference review. Included articles consist of qualitative and quantitative research and society guidelines. Articles from inception to 1st July 2023 were included. The results of the literature search have been summarized into the format of a narrative review. Key barriers to FP for TGD adolescents include inconsistencies in form and timing of counseling, potential worsening of gender dysphoria with FP treatment, high cost of treatment, limited research on FP outcomes, and legal barriers. Intersectionality between gender identity and other forms of minority status can compound these barriers to FP and healthcare in general. Barriers to TGD adolescents accessing FP are significant. Increased research is needed upon methods to mitigate these barriers. Solutions include increasing uniformity and timing of FP counseling by varying health care providers, advocacy efforts to mitigate legal and financial barriers, increased research efforts in FP outcomes, and increased cultural competency in clinics offering FP care to TGD adolescents.
Keywords: adolescent, cryopreservation, fertility preservation, health care disparities, social determinants of health, transgender persons
Plain language summary
Barriers to fertility preservation access in transgender and gender diverse adolescents: a narrative review
Multiple barriers exist for adolescents identifying as transgender or gender diverse (TGD) in the pursuit of fertility preservation (FP). In this narrative review, we aim to summarize the literature regarding such barriers. Key barriers to FP for TGD adolescents include inconsistencies in the form and timing of counseling on this topic, the treatment process of fertility preservation can worsen gender dysphoria, there is a very high cost of treatment but limited research on FP results, and various legal barriers to surmount. Intersectionality between gender identity and other forms of minority status can also interact, making FP and healthcare in general difficult to access.
Introduction
Fertility preservation (FP) is an important aspect of care for transgender and gender diverse (TGD) adolescents undergoing gender affirming treatments.
TGD is a broad term defining individuals whose gender identity differs from the gender associated with the sex assigned at birth. 1 Transfeminine is a term referring to individuals assigned male at birth who identify with the female gender. 1 Transmasculine is a term referring to individuals assigned female at birth who identify with male gender. 1 Gender identity is a person’s sense of self in regard to their gender whether male, female, or alternate gender. 1 Sex assigned at birth refers to a person’s gender status as male, female, or intersex based on physical characteristics typically based on appearance of external genitalia at birth. 1 Gender dysphoria is a term to describe the negative emotional and psychological distress caused by incongruence between sex assigned at birth and gender identity. 1 Gender affirming treatment is targeted at the treatment of gender dysphoria; gender affirming treatments can have varying negative effects on fertility. 1
In individuals who have not yet undergone puberty, Gonadotropin-releasing hormone (GnRH) agonists or ‘hormone blockers’ used for gender affirming treatments pause germ cell maturation. 2 Estrogen therapy in transfeminine TGD persons can impair spermatogenesis and in transmasculine TGD persons, testosterone therapy can suppress ovulation and adversely affect ovarian tissue and cell architecture. 2 Surgical treatments for gender dysphoria include hysterectomy, oophorectomy, and orchiectomy, with resultant loss of fertility secondary to removal of reproductive organs; however, these treatments are reserved for adult patients, not adolescents.2,3 These gender affirming treatments may impair fertility to varying extents, emphasizing the importance of counseling on these effects and offering FP in concordance with gender affirming treatments.
There are a variety of established FP options for TGD adolescents (Table 1). In transmasculine TGD adolescents, FP can be achieved via oocyte cryopreservation and oocyte tissue cryopreservation, and in transfeminine TGD adolescents, FP methods include sperm cryopreservation via masturbation or testicular sperm extraction and percutaneous epididymal sperm aspiration (Figure 1). 4
Table 1.
Summary of FP procedures.
| FP options in TGD patients | |
| Transmasculine persons | Oocyte cryopreservation: Stimulation of ovarian tissue to produce multiple ovarian follicles and oocytes, surgical extraction of oocytes, and subsequent vitrification of oocytes |
| Ovarian tissue cryopreservation: Surgical removal of ovarian tissue and subsequent vitrification of tissue | |
| Transfeminine persons | Sperm cryopreservation: Retrieval of sperm via masturbation or surgical techniques involving extraction (TESE) or aspiration (TESA) of testicular tissue or aspiration of epididymis (PESA) with subsequent vitrification of sperm |
FP, fertility preservation; PESA, percutaneous epididymal sperm aspiration; TESE, testicular sperm extraction; TESA, testicular sperm aspiration; TGD, transgender and gender diverse.
Figure 1.
Multiple barriers exist in regards to the transgender and gender diverse adolescent population and access to fertility preservation. These barriers can compound upon pre-existing cultural and social barriers to healthcare, highlighting the importance of intersectionality in health care delivery and fertility preservation access.
Only a small minority of TGD adolescents undergo FP. A report published by members of a multidisciplinary gender affirming clinic at Stanford University sheds light on the limited uptake of FP in TGD adolescents: when an external referral to a fertility clinic is not required, 24% of patients accepted a FP consult. However, only 6.8% of TGD adolescents chose to subsequently undergo FP. 5 Multiple barriers may contribute to the lack of FP in TGD adolescents including inconsistency in access to FP counseling, decreased access to fertility care, the short- and long-term costs associated with FP, the delay in initiating gender affirming treatments in order to achieve FP, and worsening of gender dysphoria. 6 This literature review aims to highlight the barriers facing TGD adolescents in accessing FP while navigating gender identity and gender transitions. This review will discuss desire of FP in TGD adolescents, barriers to FP including lack of uniform counseling, exacerbation of associated gender dysphoria, high cost of treatment, limited research on outcomes, prohibitive legal landscape, impact of intersectionality, and finally recommendations for improvements in care.
Methods
A literature search was conducted via PubMed to inform this narrative review. The following Medical Subject Headings search terms were used: ‘transgender persons’ and ‘fertility preservation’ and ‘adolescents’. Additional articles were then selected upon reference review of initially identified articles when relevant to the discussion of barriers regarding FP in transgender adolescents. Included articles consist of peer-reviewed qualitative and quantitative research and society guidelines published in the English language. Primary and secondary research was included. Non-peer reviewed publications were excluded. Articles from inception to 1st July 2023 were included.
Desire regarding FP
A meta-analysis cited that 49–67% of transgender adolescents desire to have children, with a large proportion considering adoption as means of parenting. 7 Adolescents undergoing treatment for gender dysphoria place less emphasis on FP compared to other groups of similar age who have FP needs. 8 Multiple studies have shown that only a minority of TGD youth choose to pursue FP prior to gender affirming treatments, ranging from 5 to 10%.4,6 A survey assessing attitudes of TGD youth and the parents of TGD youth demonstrated that childbearing was important to only 20% of youth and 13% of their parents, in stark contrast to adolescents undergoing treatment for cancer, 80% of whom consider FP important. 8 In another study of life priorities of TGD adolescents, maintaining good health was ranked first and having children was ranked last. 4
By contrast, a higher proportion of TGD adults, when compared to TGD adolescents, report that FP is important and something they would choose to undergo, with 51% of transfeminine adults and 37.5% of transmasculine adults endorsing they would have chosen to preserve fertility prior to gender affirming treatments if they had been properly counseled regarding FP options. 5 This discrepancy in attitudes regarding FP between TGD adolescents and adults may be a reflection of evolving priorities with age and the rising average age of parenthood in the United States. 9 Given that FP becomes more important to TGD persons with the transition from adolescence to adulthood, continued discussion of FP over time is prudent to offer TGD individuals. Furthermore, TGD adolescents should be counseled on the possibility that fertility may become more important to them over time and encouraged to consider their potential future wishes for family building.
Counseling regarding FP
Multiple medical societies including World Professional Association for TGD Health, the Endocrine Society, American Society of Reproductive Medicine, and European Society of Human Reproduction and Embryology have recommended TGD youth be counseled on the option of pursuing FP prior to pursuing gender affirming treatments.10–12 However, in a study assessing perceived adequacy of fertility counseling in TGD individuals planning to pursue gender affirming treatments, only 58% of respondents reported the counseling received as adequate; 23% reported counseling as inadequate; and 19% reported no counseling at all. 13 Those who had strong or uncertain fertility desires were more likely to report perceived inadequate counseling than those who do not desire FP. Reasons for perceived inadequate counseling may include a physician’s personal bias and lack of a gender-inclusive environment in the healthcare system contributing to patient discomfort. In addition, knowledge gaps regarding FP either due to research limitations or physician inexperience with TGD FP may hinder adequate counseling.
Studies have demonstrated that the majority of FP counseling occurs via primary care physicians such as pediatricians. 6 This is in lieu of consultation with an reproductive endocrinology and infertility (REI) physician, though survey research has demonstrated that 33% of TGD and gender diverse individuals report they would be interested in counseling with an REI specialist. 6 A thematic analysis based on interviews of physicians specializing in pediatrics, mental health, and gynecology concluded that a multidisciplinary approach to FP counseling is most effective as it facilitates nuanced discussions of FP from the perspective of multiple physicians with different expertise, allows for numerous discussions over time, and helps create different avenues of patient-physician relationships. 14
A key barrier to counseling via REI specialists stems from TGD adolescents’ fears of encountering bias and improper pronoun use in the environment of REI practices. 15 By creating an inclusive clinic environment, providing gender neutral bathrooms, and ensuring proper pronoun use in documentation and during the process of FP counseling, this barrier can be mitigated. 16 Implementation of routine and high-quality counseling regarding FP is an area for improvement in gender affirming care.
Barrier: Gender dysphoria
Gender dysphoria in TGD youth can be severely debilitating and life threatening. 17 Consequently, gender affirming treatments can lead to a significant improvement in quality of life for TGD youth. 1 However, FP in most cases requires a delay or pause of gender affirming treatments. Though the exact amount of time required to stop or pause gender affirming treatments prior to FP to maximize FP outcomes is not well understood, a commonly cited time frame to delay or pause use of hormones such as testosterone prior to starting the FP process is 3 months. 8 However, choosing between treatment of gender dysphoria and optimization of FP can be a reality, as in transfeminine individuals, initiation of estrogen and androgen deprivation therapy in Tanner Stage 2 can lead to permanent, irreversible detrimental effects on spermatogenesis. 7 Survey research has demonstrated that many TGD youth demonstrate an unwillingness to delay gender affirming hormones (GAH) treatment by 3 months to preserve fertility. 8 Nonetheless, if GAH could be continued, one-third of TGD youth reported they would choose to preserve fertility. 8
For those who are amenable to delaying or pausing GAH for a brief period of time in order to facilitate FP, the FP process itself can exacerbate gender dysphoria. For example, TGD youth may feel that childbearing conflicts with their affirmed gender, while surgical procedures, transvaginal ultrasounds, and pelvic exams performed during the process of oocyte cryopreservation or masturbation to achieve sperm retrieval can be psychologically distressing. 8 The vast majority of TGD youth would not elect for dysphoria-exacerbating surgical procedures or masturbation for the purpose of preserving fertility. 8 Even when TGD individuals do elect for FP, due to the significant risk for worsened gender dysphoria during the process, American Society for Reproductive Medicine (ASRM) guidelines recommend offering these patient comprehensive counseling services. 8
Barrier: Cost
In a qualitative analysis of TGD adolescents, cost was the most commonly mentioned barrier to FP. 18
Cost of oocyte cryopreservation includes the cost of oocyte retrieval, ranging between $6000 and $10,000, cost of medications, ranging between $3000 and $6000 depending on dosage needed, and cost of tissue storage, ranging from $300 to $1,000 annually. 17 Sperm cryopreservation via masturbation costs $388 on average, and $555 on average annually for storage. 16 According to ReproTech, a cryogenic storage company, the average cumulative cost of sperm storage or oocyte storage alone surpasses $2500 over 10 years. 19
Fertility services are cost prohibitive in the general US population and insurance coverage for FP services is limited. 20 TGD individuals are a vulnerable population and are more likely to be uninsured and report cost-related barriers to general care compared to cisgender adults, leading to a greater difficulty in accessing FP services. 21 Many TGD adolescents face economic barriers to accessing healthcare as they are not financially independent and may lack financial support from parents to pursue FP.
Limited insurance coverage further compounds this issue, leading to disparities in access to FP services. Although state mandates for infertility insurance coverage date back to 1977, fertility coverage for iatrogenic infertility, such as infertility caused by gonadotoxic chemotherapy, is a relatively new advancement in the United States. 22 In 2017, Connecticut and Rhode Island were the first states to pass legislation allowing for insurance coverage of iatrogenic infertility. 24 3Since then, 15 states in the United States have some form of legislation regarding FP protection for iatrogenic infertility, and 2 more states have pending legislation. Unfortunately, those pursing GAH therapy are largely excluded from qualifying for this iatrogenic infertility coverage. 24 Thus, the financial burden associated with FP remains a significant barrier for TGD adolescents.
Barrier: Limited research on FP
There remains a paucity of research on FP in TGD adolescents and existing research is limited by small sample size and different exposures of hormones in reference to GAH treatment. This section will focus on oocyte cryopreservation, oocyte tissue cryopreservation, and sperm cryopreservation. Experimental methods of FP will not be discussed.
In a retrospective study comparing oocyte cryopreservation outcomes between TGD males prior to gender affirming treatments and cisgender females prior to cancer treatment, there was no significant difference between the number of oocytes retrieved. 25 Small studies have demonstrated oocyte cryopreservation is also possible in patients with prior testosterone exposure and ongoing testosterone exposure respectively. However, limited animal studies have demonstrated that long-term testosterone exposure impairs in vitro fertilitization (IVF) outcomes by yielding fewer mature oocytes, suggesting testosterone involvement in embryogenesis.10,26 At present, there is no consensus on the timing of testosterone therapy cessation in transmasculine TGD patients who have already started GAH therapy prior to oocyte cryopreservation. 10
Ovarian tissue cryopreservation, a treatment that is no longer considered experimental since 2019 in the United States, is another option for FP for TGD persons assigned female at birth. Ovarian tissue cryopreservation may be facilitated at the time of gender affirming surgery with removal of ovarian tissue. 27 A benefit of this method is that testosterone therapy does not need to be paused. A study published in 2022 comparing the effectiveness of vitrification versus slow freezing of ovarian tissue cryopreservation among TGD persons assigned female at birth found improved follicle preservation with vitrification of ovarian tissue. 28 This study was the only research study assessing ovarian tissue cryopreservation specifically in regard to TGD persons.
In a study of outcomes of sperm cryopreservation in transfeminine TGD patients, semen parameters were decreased compared to the general population. 29 Behavioral factors like tight undergarments and tucking were associated with a total motile sperm count under 5 million. 29 In contrast, other studies have shown there were no significant differences between semen parameters of TGD youth and adolescents with cancer undergoing FP. 30 Small studies comparing semen parameters in TGD women with history of GAH use who stopped 3–6.5 months prior to sperm collection, versus those who had not used hormones, showed comparable semen parameters with no significant differences. TGD Women who were using 1 mg estradiol daily while undergoing semen cryopreservation did show significant decreased semen parameters compared to those who had stopped GAH or those who had not yet started GAH. 31 Similar to the lack of evidence on cessation of hormonal therapy prior to oocyte cryopreservation, there is limited evidence and no evidence-based guidelines on cessation of hormonal therapy prior to sperm cryopreservation. 32
Barrier: Legal landscape in access to TGD care
The legal landscape regarding TGD healthcare is rapidly changing. According to the Williams Institute of UCLA, as of March 2023, 32 states in the United States have enacted laws that either restrict access or ban access to gender-affirming care, leading to 146,300 TGD youth not having access to care or at high risk for losing access to healthcare. 33 As of June 2023, 10 states currently have full bans on gender-affirming care; these states include TX, GA, IO, TN, MS, SD, UT, AL, AZ, and AK.33,34 Access to care for TGD individuals remains highly contested and 93% of TGD youth report worries about access to medical care. 35
In addition to legal barriers, individual REI physicians or clinics may not accept referrals from TGD individuals or provide treatment for TGD persons, despite ASRM’s clear stance that regardless of sexual orientation or gender identity, infertility clinics should treat all persons equally. 36 Though 21 states have anti-discrimination laws providing general protections for TGD persons, there are few specific policies regarding the use of assisted reproductive technology (ART) in particular by TGD individuals. In fact, the legal barriers facing TGD persons are so significant that ASRM guidelines recommend physicians encourage TGD persons to consult legal experts regarding parenting via ART. 11
Intersectionality of gender identity and racial/ethnic minority status
TGD persons who are racial/ethnic minorities have increased barriers to accessing care. Multiple studies have shown that TGD persons with racial or ethnic minority status suffer worse healthcare outcomes than TGD persons without minority status. 15 For example, TGD persons of color report less access to pubertal blocker medications used to provide gender-affirming care than white TGD persons. Furthermore, black TGD adolescents without access to gender-affirming care are also more likely to report no use of the general healthcare system compared to similar white TGD counterparts. 37 TGD youth of color are at higher risk of suicide, mental illness, and HIV diagnosis than white TGD youth. 38 In a survey of 39 TGD persons of color, 100% of responders felt they would receive better care if they were white and TGD; 33% of respondents attributed this to transphobia and 20% attributed this to racism. 39 Exploring the role of intersectionality in the care of TGD persons is a focus of improving care and has been pioneered in TGD family therapy with positive outcomes. 40 Further research is needed to understand the impact of racial/ethnic minority status on the ability of TGD adolescents to receive FP as well as interventions that can reduce barriers to care in this regard.
Sexual minority status is another area in which layering minority status can compound with increasing barriers to healthcare and FP specifically in TGD adolescents. A systematic literature review among sexual minorities and TGD individuals concluded that in the existing literature, those of sexual minority status and TGD status are grouped together under the umbrella term sexual and gender minority; there is minimal evidence on the extent of barriers of TGD individuals who also simultaneously identify as a sexual minority due to the grouping of TGD and sexual minority cohorts together. 41
Discussion
Despite the many barriers to TGD adolescents receiving FP, counseling patients regarding FP options is pivotal, especially since desire for parenthood among TGD persons increases with the transition from adolescence to adulthood. 8 While a TGD individual may not wish to pursue FP due to fear of an associated delay in gender-affirming care, this desire can change. Thus, repetitive FP counseling should be provided not only at the onset of Gender affirming therapy (GAT) but also after initiation, thereby responding to evolving patient needs.
Once a TGD patient elects for FP, there can still be significant barriers to care. Legal barriers and financial barriers are considerable systemic challenges, but advocacy efforts can help to lift these obstacles. Furthermore, individual clinics can equip their patients with resources regarding local funding sources and support networks ranging from therapists trained in TGD care to attorneys experienced in navigating legal issues.
However, some barriers faced by TGD patients are small-scale, such as the inclusivity of FP clinics. Individual REI practices can work to decrease any anxiety and fear of bias for transgender persons seeking FP. Interventions like staff trainings on inclusive pronouns and addition of gender neutral bathrooms may be tools to decrease bias and increase culturally competent care. 42 Word-of-mouth is important to the transgender community when seeking healthcare services and creating an inclusive REI clinic environment can result in a patients recommending FP to their local TGD communities. 43
Further research is needed to not only better characterize outcomes of FP in TGD adolescents but also to assess which interventions decrease barriers to care.
Conclusion
FP is an important and underutilized aspect of care for TGD adolescents undergoing gender-affirming treatments. Despite support from multiple medical societies for FP counseling, the number of TGD individuals pursuing and completing FP is low. TGD adolescents face challenges unique to their developmental stage, such as increased mental health challenges, varying stages of puberty, and decreased access to healthcare, which can create distinctive barriers to FP. TGD adolescents face challenges in their ability to access adequate healthcare in general, and this impacts uptake of gender-affirming treatments and FP if desired. Additional research to better understand the impact of gender-affirming treatments on FP outcomes, and the systems associated with enhanced access to FP is needed.
Though there are multiple barriers to FP in TGD adolescents, counseling and education regarding the effects of gender-affirming treatments on fertility should be broadly provided TGD adolescents and their parents/legal guardians as a part of a comprehensive approach to care.
Acknowledgments
None.
Footnotes
ORCID iD: Ashni S. Nadgauda  https://orcid.org/0000-0001-5538-3107
https://orcid.org/0000-0001-5538-3107
Contributor Information
Ashni S. Nadgauda, Department of Obstetrics and Gynecology, Reading Hospital – Tower Health, 420 South 5th Avenue, Reading, PA 19611, USA.
Samantha Butts, Division of Reproductive Endocrinology and Infertility, Department of Obstetrics and Gynecology, Penn State – Main Campus, Hershey, PA, USA.
Declarations
Ethics approval and consent to participate: Not applicable; no human subjects involved in this study as this study is a literature review.
Consent for publication: Not applicable; no human subjects involved in this study as this study is a literature review.
Author contributions: Ashni S. Nadgauda: Conceptualization; Investigation; Methodology; Writing – original draft; Writing – review & editing.
Samantha Butts: Conceptualization; Project administration; Resources; Writing – original draft; Writing – review & editing.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
The authors declare that there is no conflict of interest.
Availability of data and materials: Not applicable.
References
- 1. Coleman E, Radix AE, Bouman WP, et al. Standards of care for the health of transgender and gender diverse people, version 8. Int J Transgend Health 2022; 23: S1–S259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mattawanon N, Spencer JB, Schirmer DA, 3rd, et al. Fertility preservation options in transgender people: a review. Rev Endocr Metab Disord. 2018; 19: 231–242. [DOI] [PubMed] [Google Scholar]
- 3. Call DC, Challa M, Telingator CJ. Providing affirmative care to transgender and gender diverse youth: disparities, interventions, and outcomes. Curr Psychiatry Rep. 2021; 23: 33. [DOI] [PubMed] [Google Scholar]
- 4. Chiniara LN, Viner C, Palmert M, et al. Perspectives on fertility preservation and parenthood among transgender youth and their parents. Arch Dis Child 2019; 104: 739–744. [DOI] [PubMed] [Google Scholar]
- 5. Cooper HC, Long J, Aye T. Fertility preservation in transgender and non-binary adolescents and young adults. PLoS One 2022; 17: e0265043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vyas N, Douglas CR, Mann C, et al. Access, barriers, and decisional regret in pursuit of fertility preservation among transgender and gender-diverse individuals. Fertil Steril 2021; 115: 1029–1034. [DOI] [PubMed] [Google Scholar]
- 7. Stolk THR, Asseler JD, Huirne JAF, et al. Desire for children and fertility preservation in transgender and gender-diverse people: a systematic review. Best Pract Res Clin Obstet Gynaecol 2023; 87: 102312. [DOI] [PubMed] [Google Scholar]
- 8. Persky RW, Gruschow SM, Sinaii N, et al. Attitudes toward fertility preservation among transgender youth and their parents. J Adolesc Health 2020; 67: 583–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mathews TJ, Hamilton BE. Mean age of mothers is on the rise: United States, 2000–2014. National Center for Health Statistics, 2016. https://www.cdc.gov/nchs/data/databriefs/db232.pdf [PubMed] [Google Scholar]
- 10. Douglas CR, Phillips D, Sokalska A, et al. Fertility preservation for transgender males: counseling and timing of treatment. Obstet Gynecol 2022; 139: 1012–1017. [DOI] [PubMed] [Google Scholar]
- 11. Ethics Committee of the American Society for Reproductive Medicine. Access to fertility services by transgender and nonbinary persons: an Ethics Committee opinion. Fertil Steril 2021; 115: 874–878. [DOI] [PubMed] [Google Scholar]
- 12. Hembree WC, Cohen-Kettenis PT, Gooren L, et al. Endocrine treatment of gender-dysphoric/gender-incongruent persons: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 2017; 102: 3869–3903. [DOI] [PubMed] [Google Scholar]
- 13. Walton E, Abhari S, Tangpricha V, et al. Family planning and fertility counseling perspectives of gender diverse adults and youth pursuing or receiving gender affirming hormone therapy. Urology 2023; 171: 244–250. [DOI] [PubMed] [Google Scholar]
- 14. Lai TC, Davies C, Robinson K, et al. Effective fertility counselling for transgender adolescents: a qualitative study of clinician attitudes and practices. BMJ Open 2021; 11: e043237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kirubarajan A, Patel P, Leung S, et al. Cultural competence in fertility care for lesbian, gay, bisexual, transgender, and queer people: a systematic review of patient and provider perspectives. Fertil Steril 2021; 115: 1294–1301. [DOI] [PubMed] [Google Scholar]
- 16. Park SU, Sachdev D, Dolitsky S, et al. Fertility preservation in transgender men and the need for uniform, comprehensive counseling. F S Rep 2022; 3: 253–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Day DS, Saunders JJ, Matorin A. Gender dysphoria and suicidal ideation: clinical observations from a psychiatric emergency service. Cureus 2019; 11: e6132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Boguszewski KE, Woods S, Ducar DM, et al. Transgender and gender diverse fertility choices: supporting the decision-making process for adolescents and young adults. J Pediatr 2022; 240: 256–264.e1. [DOI] [PubMed] [Google Scholar]
- 19. ReproTech LLC. Oocyte storage costs, https://www.reprotech.com/oocyte-storage-costs/ (2023, accessed 29 October 2023).
- 20. Ethics Committee of the American Society for Reproductive Medicine. Disparities in access to effective treatment for infertility in the United States: an Ethics Committee opinion. Fertil Steril 2015; 104: 1104–1110. [DOI] [PubMed] [Google Scholar]
- 21. Gonzales G, Henning-Smith C. Barriers to care among transgender and gender nonconforming adults. Milbank Q 2017; 95: 726–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Peipert BJ, Montoya MN, Bedrick BS, et al. Impact of in vitro fertilization state mandates for third party insurance coverage in the United States: a review and critical assessment. Reprod Biol Endocrinol 2022; 20: 111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Preservation AfF. State laws and legislature, https://www.allianceforfertilitypreservation.org/state-legislation/ (2023, accessed 21 October 2023).
- 24. Peipert BJ, Tsai S, Montoya MN, et al. Analysis of state mandated insurance coverage for infertility treatment and fertility preservation in the United States. Fertil Steril 2020; 114: e4–e5. [Google Scholar]
- 25. Amir H, Oren A, Klochendler Frishman E, et al. Oocyte retrieval outcomes among adolescent transgender males. J Assist Reprod Genet 2020; 37: 1737–1744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Schwartz AR, Xu M, Henderson NC, et al. Impaired IVF outcomes following testosterone treatment improve with washout in a mouse model of gender-affirming hormone treatment. Am J Obstet Gynecol 2023; 229: 419.e1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lierman S, Tilleman K, Braeckmans K, et al. Fertility preservation for trans men: frozen-thawed in vitro matured oocytes collected at the time of ovarian tissue processing exhibit normal meiotic spindles. J Assist Reprod Genet 2017; 34: 1449–1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Borrás A, Manau D, Fabregues F, et al. Comparison between slow freezing and vitrification of ovarian tissue cryopreservation in assigned female at birth transgender people receiving testosterone therapy: data on histological and viability parameters. J Assist Reprod Genet 2022; 39: 527–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. de Nie I, Asseler J, Meißner A, et al. A cohort study on factors impairing semen quality in transgender women. Am J Obstet Gynecol 2022; 226: 390.e1–10. [DOI] [PubMed] [Google Scholar]
- 30. Dilday EA, Bukulmez O, Saner K, et al. Sperm cryopreservation outcomes in transgender adolescents compared with adolescents receiving gonadotoxic therapy. Transgend Health 2022; 7: 528–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Adeleye AJ, Reid G, Kao C-N, et al. Semen parameters among transgender women with a history of hormonal treatment. Urology 2019; 124: 136–141. [DOI] [PubMed] [Google Scholar]
- 32. Barnard EP, Dhar CP, Rothenberg SS, et al. Fertility preservation outcomes in adolescent and young adult feminizing transgender patients. Pediatrics 2019; 144: e20183943. [DOI] [PubMed] [Google Scholar]
- 33. Barbee H, Deal C, Gonzales G. Anti-transgender legislation – a public health concern for transgender youth. JAMA Pediatr 2022; 176: 125–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Tanne JH. Texas is biggest US state to ban transgender care for children, joining 18 other states. BMJ 2023; 381: 1311. [DOI] [PubMed] [Google Scholar]
- 35. Project T. National survey on LGBTQ youth mental health. The Trevor Project, 2019. https://www.thetrevorproject.org/survey-2019/ [Google Scholar]
- 36. Ethics Committee of the American Society for Reproductive Medicine. Access to fertility treatment irrespective of marital status, sexual orientation, or gender identity: an Ethics Committee opinion. Fertil Steril 2021; 116: 326–330. [DOI] [PubMed] [Google Scholar]
- 37. Lopez CM, Solomon D, Boulware SD, et al. Trends in the use of puberty blockers among transgender children in the United States. J Pediatr Endocrinol Metab 2018; 31: 665–670. [DOI] [PubMed] [Google Scholar]
- 38. Raynor PA, Nation A, Outlaw F. Exploring substance use and mental health for minority transgender youth: implications for advanced practice nurses. J Am Assoc Nurse Pract 2020; 32: 229–243. [DOI] [PubMed] [Google Scholar]
- 39. Howard SD, Lee KL, Nathan AG, et al. Healthcare experiences of transgender people of color. J Gen Intern Med 2019; 34: 2068–2074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Golden RL, Oransky M. An intersectional approach to therapy with transgender adolescents and their families. Arch Sex Behav 2019; 48: 2011–2025. [DOI] [PubMed] [Google Scholar]
- 41. Ayhan CHB, Bilgin H, Uluman OT, et al. A systematic review of the discrimination against sexual and gender minority in health care settings. Int J Health Serv 2020; 50: 44–61. [DOI] [PubMed] [Google Scholar]
- 42. Pampati S, Andrzejewski J, Steiner RJ, et al. ‘We deserve care and we deserve competent care’: qualitative perspectives on health care from transgender youth in the southeast United States. J Pediatr Nurs 2021; 56: 54–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Chiang T, Bachmann GA. TranZap: a transgender resource for identifying gender-affirming providers. Sex Med Rev 2022; 10: 632–635. [DOI] [PubMed] [Google Scholar]


