Abstract
Introduction:
Even though breast cancer incidence is lower in Sub-Saharan Africa, its mortality is higher in these countries. However, the impact does not end with diagnosis and treatment; rather many patients struggle with depression which is very common among these patients. This systematic review and meta-analysis helps to provide valuable insights into the overall prevalence of depression and associated factors among breast cancer patients in Sub-Saharan Africa.
Method:
We searched several databases, including MEDLINE, Embase, Scopus, Hinary, CINHAL and Google Scholar to retrieve relevant literatures from inception up to 15 June 2023. All observational studies, published in English at any time were included, while, letters to editor, review articles, commentaries, interventional and qualitative studies, and, abstracts presented in conferences or seminars were excluded. The results of this systematic review and meta-analysis have been written based on the PRISMA 2020 checklist and the protocol have been registered in PROSPERO database (CRD42023428910).
Result:
We have included nine articles with 2226 study participants. The result showed that, the pooled prevalence of depression among breast cancer patients in Sub-Saharan Africa was 45.6% (95% CI: 30%–61%) with significant heterogeneity I2 = 98.9%, (Cochrane) Q < 0.0001. There was no single study effect and publication bias but substantial heterogeneity was observed. In addition, there has been a publication bias with eggers test (p < 0.0033). However, there were no studies imputed after trim and fill analysis. From the factors, breast cancer patients who had poor financial support were 1.47 (95% CI: 1.02–2.13) times more at risk of developing depression than their counterparts.
Conclusion:
The prevalence of depression among breast cancer patients in Sub-Saharan Africa countries were higher than other regions. Thus, Emphasis should be given on developing financial assistance programs designed to cover the medical costs and improving the health care infrastructure.
Keywords: Depression, breast cancer, Sub-Saharan Africa, meta-analysis, systematic review
Introduction
Worldwide, in the year 2020, global observatory cancer (GLOBOCAN) reported about 19.3 million new cases and 10 million deaths of cancer cases having occurred. Among all cancer cases, the most commonly diagnosed (most prevalent) cancer is female breast cancer, which accounts for 2.3 million cases (11.7%) and the leading cause of cancer death among female cancers. 1 Africa reported 531,086 (74.3/100,00) new breast cancer cases with mortality of 85,787 (19.4/100,000) in 2020. Though the disease incidence seems to be lower in Sub-Saharan Africa (SSA), the disease is the leading cause of death among all cancer cases. It has also been projected that the prevalence and mortality of breast cancer will be doubled by 2050. 2 Breast cancer is also the leading prevalent cause of mortality among all cancer cases accounting for 16,133 (20.9%) new cases and 9061 (17.5%) deaths in Ethiopia. 3
The diagnosis and treatment of breast cancer has an impact on the emotional, life expectation, long time planning, and psychological signs of mental illness including depression.4,5 In addition, women may lose the symbols of feminity resulting in loss of self-esteem and resulting in social isolation, which may lead them to be exposed to psychological adverse symptoms. 6
Depression is a significant contributor to the global burden of disease and affects people in all communities across the world and it is estimated to affect 350 million people in 2004. 7 Depression is a comorbid disabling disease that affects approximately 30%–40% of cancer patients. 8 Studies have shown that the risk of depression in patients with breast cancer is higher than with other types of cancer9,10 and the general population. 11 Due to its complex aetiology and pathogenesis, early screening of depression among breast cancer patients is difficult resulting in many patients left undiagnosed and untreated.8,12
There has been a 25% and 39% higher mortality among breast cancer patients with depressive symptoms and major depressions respectively. The diagnosis of breast cancer may be devastating, resulting in adverse reactions causing depression, psychological distress, fatigue, sexual concerns and self-blame. 13 According to a systematic review and meta-analysis, the global prevalence of depression among breast cancer patients was reported to be 32.2%. 14 Similarly, the prevalence of depression in breast cancer patients in SSA ranges from 9% 15 to 84.2%. 16 A meta-analysis revealed that depression is very common among breast cancer patients associated with substantial functional impairment, physical deterioration and diminished survival. 17 It also impacts patient’s ability to cope with the burden of the disease and results in lower adherence to treatment, extended hospitalization and reduced quality of life.18,19
A number of factors have been identified from different literatures which affects the development of depression among breast cancer patients. These factors include: age,10,20 educational status,10,21,22 marital status,10,22 social-support,20,23 emotional support, advanced stage of cancer,10,23,24 poor patient–provider communication21,25,26 and poor financial support.15,25,26 In addition, the results were not consistent on the effect of type of treatment on depression among breast cancer patients. A study revealed that chemotherapy reduces the risk of Depression 27 while others show that, depression may not be affected by type of treatment like radiotherapy and type of surgery. On the other hand, it has been reported that chemotherapy increased the risk of depression.28–30
Even though there has been a systematic review and meta-analysis that have been conducted on the global prevalence of depression among breast cancer patients, 14 it did not incorporate most of the studies that have been conducted in SSA and did not incorporate studies published after 2019. Besides, individual studies conducted in SSA revealed a high degree of depression among breast cancer patients.16,25,26,31 Hence, this systematic review and meta-analysis aimed to identify the pooled prevalence of depression and associated factors among breast cancer patients in SSA. Assessing the pooled prevalence and associated factors would enable the public health practitioners to develop effective intervention and support strategies. Likewise, it will help policy makers to understand the promotion, prevention, and treatment mechanisms in this area and to understand the quality and effectiveness of care and treatments introduced. More importantly, since SSA has unique socio-cultural nuances, healthcare systems and limited resources compared to other regions, understanding the prevalence and associated factors in these countries is vital for tailoring care and support programs appropriately.
Methods and analysis
Study protocol registration
The reports of this systematic review and meta-analysis have been written based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 checklist (see Supplemental File 1), 32 and registered in PROSPERO-International Prospective Register of Systematic Reviews and Meta-analysis (PRISMA) reporting checklist under the reference number of CRD42023428910.
Information source, search strategy
An overarching systematic searching was cascade for all relevant studies on online databases, mainly PubMed/MEDLINE, Embase, Scopus, Google Scholar and Google. Besides, a search of online university repositories (University of Gondar and Addis Ababa University) and registries were conducted. To retrieve additional articles, we have also reviewed reference lists of already identified studies. The search was performed from 10 to 15 June 2023 by all authors and all articles which were published prior to the searching date were included. A search strategy was developed using a combination of keywords based on medical subject heading (MeSH) terms related to the outcome status ‘depression’, the disease status ‘breast cancer’, and the list of countries in SSA. During the literature search, the succeeding search terms were used: prevalence OR proportion OR incidence OR magnitude OR epidemiology AND depression* OR ‘depressive symptom*’ OR ‘symptom, depressive*’ OR ‘depression disorder*’ AND ‘Breast cancer’ OR ‘Breast carcinoma’ OR ‘breast tumor’ OR ‘mammary cancer’ OR ‘mammary adenocarcinoma’ AND Ethiopia OR Angola OR Benin OR Botswana OR ‘Burkina Faso’ OR Burundi OR Cameroon OR ‘Central African Republic’ OR Chad OR Congo OR ‘Cote d’Ivoire’ OR Eritrea OR Gabon OR Gambia OR Ghana OR Guinea OR ‘Guinea-Bissau’ OR Kenya OR Lesotho OR Liberia OR Madagascar OR Malawi OR Mali OR Mauritania OR Mauritius OR Mozambique OR Namibia OR Niger OR Nigeria OR Rwanda OR Senegal OR ‘Sierra Leone’ OR Somalia OR ‘South Africa’ OR Tanzania OR Togo OR Uganda OR Zaire OR Zambia OR Zimbabwe. (The full search strategy for all data bases is available in the Supplement File 2).
Study selection and eligibility criteria
To easily declare the eligibility criteria, we have followed COCOPOP (condition: Depression; Context: SSA; and population: breast cancer) for prevalence studies and PEO (population: Breast cancer; exposure: associated factors; and outcome: Depression) questions. All authors participated in the searching process in all databases and all articles retrieved through search strategy were merged and exported to Endnote version 8 and duplicates were removed. Titles and abstracts were independently reviewed for inclusion in full text assessment by three sets of review authors ((ZA, HY, TB), (HY, EA, MY) and (YT, AM, HE). Furthermore, two sets of reviewers (HE, AA) and (AE, FD) performed extra screening on articles included in the full-text for final inclusion. The disagreement between reviewers were handled by discussion and a consensus was reached. The PRISMA flow diagram showed reasons for exclusion of reports in all stages.
Eligibility criteria
All observational studies, (cross-sectional, case-controls, and cohort) both published and grey literatures, published in English language and conducted in SSA reporting the prevalence and/or associated factors of depression among breast cancer patients, and at any time were included. Moreover, letters to editor, review articles, commentaries, interventional studies, qualitative studies, and, abstracts presented in conference or seminar which did not present sufficient data to calculate the outcome of interest were excluded.
Quality assessment and critical appraisal
The qualities of the articles were assessed by using the Joanna Briggs Institute (JBI) quality appraisal checklist adapted for cross-sectional studies (Since all papers included are cross-sectional). 33 The tool consists of eight questions related to the methodological quality in the design, measurement eligibility and analysis. Two sets of reviewers (AE, AM) and (EA, HY) independently determined the possibility of bias in the design, conduct, and analysis of each article. Any disagreement by the two sets of reviewers were resolved by the third reviewer (FY), and a consensus was reached. Thus, studies which scored 1–3 out of 8 were low quality papers, 4–6 were medium, and 7–8 were high quality papers. (See Supplemental File 3).
Data extraction
Two reviewers (AM, FD) independently extracted the required information based on the prepared structured extraction checklist in Microsoft Excel. It included names of author, year of publication, the target population, country, study design, sample size, response rate, prevalence/proportion, number of success and failure in exposed and unexposed groups, and COR with CI of associated factors. Disagreement between the two reviews were solved by consensus between the two.
Data synthesis and analysis
After extracting the data, it was imported to STATA V-17 for analysis. Heterogeneity was assessed using I2 and Q statistics test and the values of I2 = 0 is considered no heterogeneity, I2 ⩽ 25% is low heterogeneity, 26%–50% moderate heterogeneity, 51%–75% was considered substantial heterogeneity and ⩾75% was considered as high heterogeneity. 34 Random effect meta-analysis was used for the presence of heterogeneity to calculate pooled proportion of depression, odds ratio, and corresponding 95% confidence interval.35,36 Wherever possible, sub-group analysis was conducted based on the quality of the study, type of study participants (based on the treatment), and outcome measurement. To evaluate the influence of one paper on overall proportion, we performed a leave one out sensitivity analysis. Publication bias was detected across studies objectively through Eggers tests. Thus, trim and fill analysis using fixed effect model restricted maximum likelihood (REML) method was conducted. The effect of selected independent variables was analysed using separate categories of meta-analysis and the findings were presented using forest plot and Odds Ratio (OR) with its 95% CI.
Result
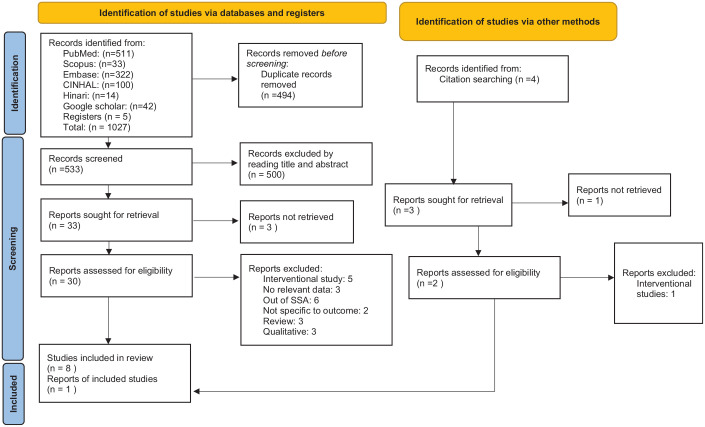
A total of 1027 records were retrieved through online databases and five were retrieved from registries. Of these, 494 were duplicates and 533 were left for title/abstract screening. Subsequently, 33 reports remained for full text screening. Additionally, four reports were identified from citation searching, of which three were assessed for eligibility. After reading the full text, eight articles from database and one from citation searching were included for the analysis. The PRISMA flow chart diagram is presented in Figure 1.
Figure 1.
Prisma flow diagram showing screening steps of articles.
Study characteristics
The characteristics of nine included studies in the meta-analysis with 2226 study participants were presented in Table 1. Out of nine articles, three were conducted in Ethiopia20,25,26 and three from Ghana,15,16,21 two from Nigeria,23,31 and one from South Africa. 37 All the articles have used cross-sectional study design and the sample size ranged from 120–428,16,20 with majority being 200–300 study participants. Five of the articles15,16,21,25,26 have used HADS tool for measuring the outcome status and one of them 20 used PHQ-9, and the rest used MINI23,31 and CESD. 37 Regarding the study participants, two of them included only breast cancer patients who were on chemotherapy,16,21 while others included all types of breast cancer patients20,23,25,26,37 and surgically treated patients.15,31 Based on the JBI quality assessment checklist, three studies had high quality and six had moderate quality (See Supplemental File 3).
Table 1.
Characteristics of included studies on depression among breast cancer patients in SSA.
| Author | Publication year | Country | Total population analysed | Age (years) | Outcome measurement | Developed outcome | Prevalence (%) | Study design | Type of study participants | Level of quality |
|---|---|---|---|---|---|---|---|---|---|---|
| Belay et al. 25 | 2022 | Ethiopia | 333 | 18+ | HADS | 195 | 58.56 | Cross-sectional | All breast cancer patients | High |
| Kagee et al. 37 | 2017 | South Africa | 201 | 27–83 | CESD | 73 | 36.31 | Cross-sectional | All breast cancer patients | Moderate |
| Kugbey et al. 21 | 2022 | Ghana | 205 | 18+ | HADS | 76 | 37.30 | Cross-sectional | Breast cancer on chemotherapy | High |
| Lueboonthavatchai al. 15 | 2007 | Ghana | 300 | 18+ | HADS | 27 | 9.0 | Cross-sectional | Surgical outpatient breast cancer patients | Moderate |
| Opadola et al. 31 | 2020 | Nigeria | 222 | 18+ | MINI | 161 | 72.52 | Comparative cross-sectional | Surgical outpatient breast cancer patients | Moderate |
| PaPoola et al. 23 | 2011 | Nigeria | 129 | 18+ | MINI | 50 | 38.75 | Cross-sectional | All breast cancer patients | Moderate |
| Wondimagegnehu et al. 20 | 2019 | Ethiopia | 428 | 18+ | PHQ-9 | 107 | 25.0 | Cross sectional | All breast cancer patients | High |
| Dereje 26 | 2019 | Ethiopia | 288 | 18+ | HADS | 135 | 46.87 | Cross-sectional | All breast cancer patients | Moderate |
| Calys-Tago et al. 16 | 2017 | Ghana | 120 | 30–84 | HADS | 101 | 84.16 | Cross-sectional | Breast cancer on chemotherapy | Moderate |
Prevalence of depression among breast cancer patients in SSA
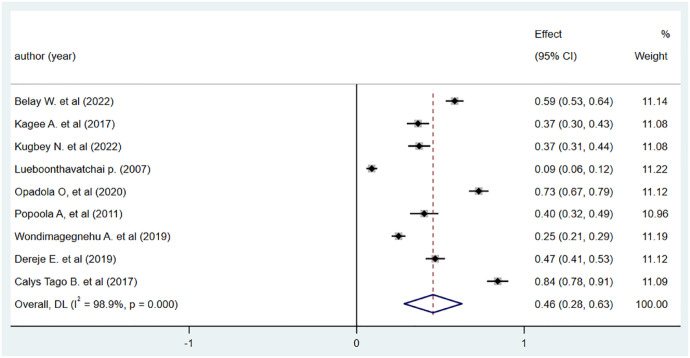
The overall prevalence of depression among breast cancer patients with fixed effect model from nine studies showed a significant heterogeneity across studies with I2 value of 98.8% and Q value of <0.0001 which is significant. As a result, we used random effect model. Consequently, the pooled prevalence of depression among breast cancer patients in SSA was 45.6% (95% CI: 0.283–0.63) with significant heterogeneity I2 = 98.9%, (Cochrane) Q < 0.0001 (See Figure 2).
Figure 2.
Pooled prevalence of depression among breast cancer patients in SSA.
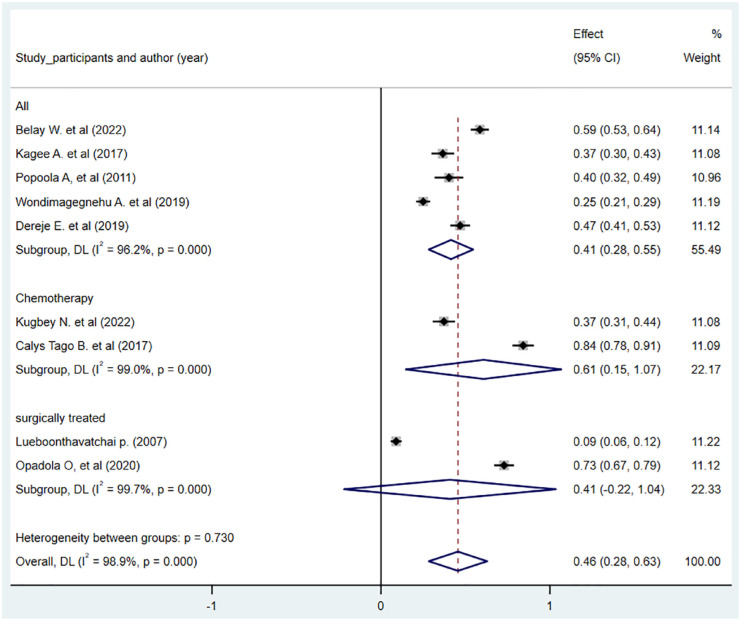
Sub-group analysis
A significant heterogeneity has been detected across studies in the sub-group analysis by type of study participants, type of outcome measurement, and quality of study (each having I2 value of 98.8% and p < 0.0001). The pooled prevalence of depression was 40% (95% CI: 19%–61%) among high study quality articles and 48% (95% CI: 22%–75%) among medium quality articles (Figure 1 in Supplemental File 3). Additionally, the pooled prevalence of depression among breast cancer patients was higher 61% (95% CI: 15%–105%) among breast cancer patients who were on chemotherapy than surgically treated patients 41% (95% CI: 28%–55%) (Figure 3). Lastly, the pooled prevalence of depression was varied among the types of outcome measurement each study had used. Consequently, the prevalence was higher among those studies which used HADS as a measurement tool for depression which was 47.1% (95% CI: 19.4–74.8) (Figure 2 in Supplemental File 3).
Figure 3.
Sub-group analysis of pooled prevalence of depression among breast cancer patients by type of study participants.
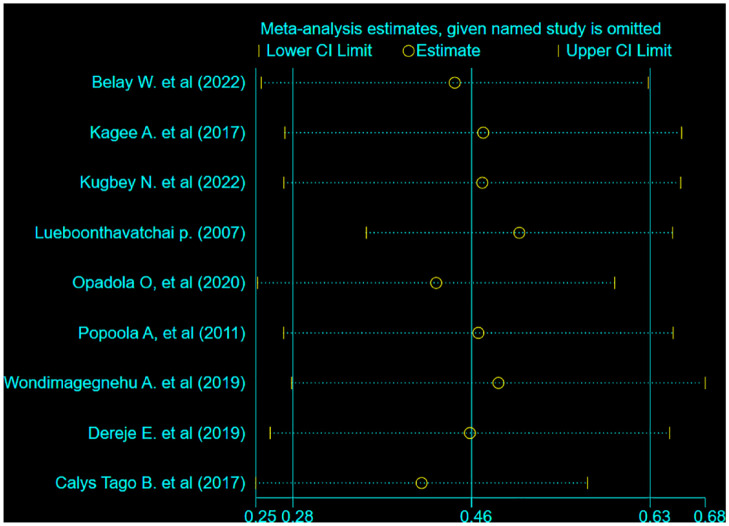
Sensitivity analysis and publication bias
Sensitivity analysis was conducted to check the source of heterogeneity across studies. Consequently, there has not been a single study effect. After deletion of one study, the pooled prevalence of depression varied between 41% (95% CI: 24%–56%) and 50% (95% CI: 35%–65%). (See Figure 4). In addition, publication bias was assessed using eggers test. The estimated bias coefficient was 22.9 (95% CI: 2.42–43.41) with standard error of 8.67 and p < 0.0033, which indicates the presence of publication bias. As a result, we have done trim and fill analysis. However, there was no study that was imputed, hence, the pooled prevalence of depression among breast cancer patients was 45.6% (95% CI: 30%–61%).
Figure 4.
Sensitivity analysis of prevalence of depression among breast cancer patients in SSA.
Factors associated with depression among breast cancer patients in SSA
We have included eight studies and incorporated nine variables in this meta-analysis for determining the significant factors associated with depression among breast cancer patients. The variables incorporated are educational status,21,23,31 marital status,21,23,26,31 social-support,23,26 employment status,20,21,23,31 stage of cancer,20,23 financial support,15,25,26 patient–provider communication,21,25,26 patient–family relationship15,25,26 and comorbidity.21,26 From the incorporated variables, only financial support becomes significantly associated with depression with p value < 0.05 (AOR: 1.47; 95%CI: 1.02–2.13). Hence breast cancer patients who have poor financial support were 1.47 times more at risk of developing depression than their counterparts (Table 2).
Table 2.
Factors associated with depression among breast cancer patients in SSA.
| Factors | No. of studies | Effect size | 95% CI | Heterogeneity Chi-square I2/p-value |
|---|---|---|---|---|
| Educational status (formal education) | 3 | 0.80 | 0.24–1.53 | 0.0%/0.512 |
| Marital status (single) | 4 | 1.10 | 0.75–1.61 | 0.0%/0.672 |
| Social-support (poor) | 2 | 0.89 | 0.50–1.58 | 0.0%/0.580 |
| Employment status (unemployed) | 4 | 0.73 | 0.48–1.10 | 0.0%/0.984 |
| Stage of cancer (late) | 2 | 1.40 | 0.66–2.96 | 0.01%/0.399 |
| Financial support (poor) | 3 | 1.47 | 1.02–2.13* | 0.01%/0.717 |
| Patient–provider communication (poor) | 3 | 1.23 | 0.59–2.57 | 70.1%/0.035 |
| Patient–family communication | 3 | 1.15 | 0.69–1.91 | 0.00%/0.749 |
| Comorbidity | 3 | 1.01 | 0.59–1.75 | 0.00%/0.676 |
Discussion
Based on the present finding, the pooled prevalence of depression in SSA was 45.6%. Sub-group analysis showed that the pooled prevalence was varied across countries with their income per capita. Hence, the pooled prevalence of depression among breast cancer patients was higher among patients who took chemotherapy. It is also varied based on outcome measurement tools, in which, the prevalence was higher among studies which used hospital anxiety and depression scale (HADS) as a measurement tool. In addition, though not statistically significant, there is also variation of the prevalence among high quality articles.
The pooled prevalence of depression among breast cancer patients was higher than a systematic review and meta-analysis of the global prevalence 14 , which is 32.2%, and Iranian women38,39, which is 11% and 44%. It was also higher than primary studies conducted in India, 18 Malaysia, 40 Jordan, 41 and Syria. 42 The discrepancy might mainly be due to the difference in the countries’ income level. The present review was mainly on the SSA countries where there is low healthcare expenditure, poor health care infrastructure, high cost of medication, transportation and accommodation. Hence, the majority of patients have poor access to crucial resources, which delays diagnosis, restricts treatment options, and provides insufficient psychosocial support.43–45 Additionally, compared to countries with higher incomes, there was a lack of awareness and knowledge, which led to delayed symptom recognition, denial, and a limited grasp of the significance of psychological assistance. Besides, cultural and social support systems in developed countries often provide a counseling service foundations and patient advocacy organisations, which plays a vital role in addressing emotional support.
Those breast cancer patients who had poor financial support were at 1.47 times more risk of developing depression than their counterparts. This is in line with studies conducted in India 46 and Malaysia. 40 Due to the high expense of follow-up care and inadequate financial support, patients with breast cancer frequently face significant financial strain. Feelings of powerlessness and melancholy are brought on by the inability to pay for these expenses. Likewise, poor financial support results in social isolation and strain social relationships and connections, exacerbating the patient’s sense of isolation and despair. Patients who do not receive financial support could not have access to social support groups which results in poor coping mechanisms with the disease and inability to navigate the emotional challenges of the disease effectively. The development of financial assistance programmes through partnership with medical experts, governmental and non-governmental organisations meant to cover the expenses of medical care and improving patient outcomes and improving healthcare infrastructures should receive more attention from organisations working on breast cancer prevention and control. Our finding strongly supports the role of financial restraint on the high prevalence of depression among breast cancer patients. Therefore, it has great public health implication that attention should be given to expanding financial assistance programmes for breast cancer patients.
Even though it is the first study conducted in SSA reporting the prevalence of depression and associated factors among breast cancer patients using comprehensive searching methods, this review has its own limitations and should be evaluated cautiously. First, due to a small number of studies in SSA, all countries could not be included in the review. And we recommend for researchers in SSA to conduct primary research showing the burden of the disease and its predictors on the depression level. Second, due to limited number of studies, low number of study participants, and cross-sectional in nature, measuring the prevalence of depression among breast cancer patients should be interpreted with caution. Third, the study may have missed eligible studies, since we did not include qualitative studies and studies published other than the English language. Another important limitation was the high level of heterogeneity among the studies.
Conclusion
The pooled prevalence of depression among breast cancer patients in SSA were higher than other regions. Besides, those patients who had poor financial support were more likely to develop depression than their counterparts. We recommend policy makers in SSA to promote and expand early screening programs for depression in collaboration with public media for creating awareness about the disease and its consequences.
Supplemental Material
Supplemental material, sj-doc-1-smo-10.1177_20503121241226897 for Prevalence and associated factors of depression among breast cancer patients in Sub-Saharan Africa: A systematic review and meta-analysis by Anissa Mohammed, Dagnachew Melak, Fekade Demeke Bayou, Husniya Yasin, Aregash Abebayehu Zerga, Birhanu Wagaye, Fanos Yeshanew Ayele, Ahmed Hussien Asfaw, Natnael Kebede, Asnakew Molla Mekonen, Mengistu Mera Mihiretu, Yawkal Tsega, Elsabeth Addisu, Niguss Cherie, Tesfaye Birhane, Hussien Endris, Zinet Abegaz and Abel Endawkie in SAGE Open Medicine
Supplemental material, sj-docx-2-smo-10.1177_20503121241226897 for Prevalence and associated factors of depression among breast cancer patients in Sub-Saharan Africa: A systematic review and meta-analysis by Anissa Mohammed, Dagnachew Melak, Fekade Demeke Bayou, Husniya Yasin, Aregash Abebayehu Zerga, Birhanu Wagaye, Fanos Yeshanew Ayele, Ahmed Hussien Asfaw, Natnael Kebede, Asnakew Molla Mekonen, Mengistu Mera Mihiretu, Yawkal Tsega, Elsabeth Addisu, Niguss Cherie, Tesfaye Birhane, Hussien Endris, Zinet Abegaz and Abel Endawkie in SAGE Open Medicine
Supplemental material, sj-docx-3-smo-10.1177_20503121241226897 for Prevalence and associated factors of depression among breast cancer patients in Sub-Saharan Africa: A systematic review and meta-analysis by Anissa Mohammed, Dagnachew Melak, Fekade Demeke Bayou, Husniya Yasin, Aregash Abebayehu Zerga, Birhanu Wagaye, Fanos Yeshanew Ayele, Ahmed Hussien Asfaw, Natnael Kebede, Asnakew Molla Mekonen, Mengistu Mera Mihiretu, Yawkal Tsega, Elsabeth Addisu, Niguss Cherie, Tesfaye Birhane, Hussien Endris, Zinet Abegaz and Abel Endawkie in SAGE Open Medicine
Acknowledgments
Not applicable.
Footnotes
Author contributions: DMB, FDB, AA, BW, FYA, AHA, NK, AMM, MMM, YT, AM, NC, TB, ZA, AE, HE and HY were responsible for searching, and screening literatures and made final decisions. AM conducted the analysis and wrote the original draft of the manuscript. All authors read, reviewed and edited the manuscript for intellectual content and read and approved the final manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics approval: Not applicable.
Informed consent: Not applicable.
Consent for publication: Not applicable.
ORCID iDs: Anissa Mohammed  https://orcid.org/0000-0002-1580-4269
https://orcid.org/0000-0002-1580-4269
Fekade Demeke Bayou  https://orcid.org/0000-0002-3437-9392
https://orcid.org/0000-0002-3437-9392
Aregash Abebayehu Zerga  https://orcid.org/0000-0002-2184-6457
https://orcid.org/0000-0002-2184-6457
Natnael Kebede  https://orcid.org/0000-0001-5734-6289
https://orcid.org/0000-0001-5734-6289
Mengistu Mera Mihiretu  https://orcid.org/0009-0005-8996-0589
https://orcid.org/0009-0005-8996-0589
Niguss Cherie  https://orcid.org/0000-0002-3497-2663
https://orcid.org/0000-0002-3497-2663
Zinet Abegaz  https://orcid.org/0000-0002-2542-7671
https://orcid.org/0000-0002-2542-7671
Availability of data: The data will be available upon request with the corresponding author.
Supplemental material: Supplemental material for this article is available online.
References
- 1. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021; 71(3): 209–249. [DOI] [PubMed] [Google Scholar]
- 2. Anyigba CA, Awandare GA, Paemka L. Breast cancer in sub-Saharan Africa: the current state and uncertain future. Exp Biol Med 2021; 246(12): 1377–1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ethiopia – Global Cancer Observatory. International agency for research on cancer, The Global cancer observatory, https://gco.iarc.fr/today/data/factsheets/populations/231-ethiopia-fact-sheets.pdf (2021, accessed 06 July 2023).
- 4. Di Giacomo D, Cannita K, Ranieri J, et al. Breast cancer and psychological resilience among young women. J Psychopathol 2016; 22: 191–195. [Google Scholar]
- 5. Martino ML, Lemmo D, Gargiulo A. A review of psychological impact of breast cancer in women below 50 years old. Health Care Women Int 2021; 42(7–9): 1066–1085. [DOI] [PubMed] [Google Scholar]
- 6. Chen W, Lv X, Xu X, et al. Meta-analysis for psychological impact of breast reconstruction in patients with breast cancer. Breast Cancer 2018; 25: 464–469. [DOI] [PubMed] [Google Scholar]
- 7. Chisholm D, Sanderson K, Ayuso-Mateos JL, et al. Reducing the global burden of depression: population-level analysis of intervention cost-effectiveness in 14 world regions. Br J Psychiatry Res 2004; 184: 393–403. [DOI] [PubMed] [Google Scholar]
- 8. Cardoso G, Graca J, Klut C, et al. Depression and anxiety symptoms following cancer diagnosis: a cross-sectional study. Psychol health Med 2016; 21(5): 562–570. [DOI] [PubMed] [Google Scholar]
- 9. Ng CG, Mohamed S, Kaur K, et al. Perceived distress and its association with depression and anxiety in breast cancer patients. PLoS One 2017; 12(3): e0172975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tsaras K, Papathanasiou IV, Mitsi D, et al. Assessment of depression and anxiety in breast cancer patients: prevalence and associated factors. Asian Pac J Cancer Prev 2018; 19(6): 1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Katon W. Epidemiology and treatment of depression in patients with chronic medical illness. Dialogues Clin Neurosci 2011; 13(1): 7–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cvetković J, Nenadović M. Depression in breast cancer patients. Psychiatry Res 2016; 240: 343–347. [DOI] [PubMed] [Google Scholar]
- 13. Cooper C, Faragher E. Psychosocial stress and breast cancer: the interrelationship between stress events, coping strategies and personality. Psychol Med 1991; 1: 143–57. [DOI] [PubMed] [Google Scholar]
- 14. Pilevarzadeh M, Amirshahi M, Afsargharehbagh R, et al. Global prevalence of depression among breast cancer patients: a systematic review and meta-analysis. Breast Cancer Res Treat 2019; 176: 519–533. [DOI] [PubMed] [Google Scholar]
- 15. Lueboonthavatchai P. Prevalence and psychosocial factors of anxiety and depression in breast cancer patients. J Med Assoc Thai 2007; 90(10): 2164. [PubMed] [Google Scholar]
- 16. Calys-Tagoe SN, Senaedza NAH, Arthur CA, et al. Anxiety and depression among breast cancer patients in a tertiary hospital in Ghana. Postgrad Med J Ghana 2017; 6(1): 54–58. [Google Scholar]
- 17. Wang X, Wang N, Zhong L, et al. Prognostic value of depression and anxiety on breast cancer recurrence and mortality: a systematic review and meta-analysis of 282,203 patients. Mol Psychiatry 2020; 25(12): 3186–3197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Purkayastha D, Venkateswaran C, Nayar K, et al. Prevalence of depression in breast cancer patients and its association with their quality of life: a cross-sectional observational study. Indian J Palliat Care 2017; 23(3): 268–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lei F, Vanderpool RC, McLouth LE, et al. Influence of depression on breast cancer treatment and survival: a Kentucky population-based study. Cancer 2023; 129(12): 1821–1835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wondimagegnehu A, Abebe W, Abraha A, et al. Depression and social support among breast cancer patients in Addis Ababa, Ethiopia. BMC Cancer 2019; 19(1): 836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kugbey N. Comorbid anxiety and depression among women receiving care for breast cancer: analysis of prevalence and associated factors. African Health Sci 2022; 22(3): 166–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Alagizy HA, Soltan MR, Soliman SS, et al. Anxiety, depression and perceived stress among breast cancer patients: single institute experience. Middle East Curr Psychiatry 2020; 27(1): 1–10. [Google Scholar]
- 23. Popoola AO, Adewuya AO. Prevalence and correlates of depressive disorders in outpatients with breast cancer in Lagos, Nigeria. Psychooncol 2012; 21(6): 675–679. [DOI] [PubMed] [Google Scholar]
- 24. Sadaqa D, Farraj A, Naseef H, et al. Risk of developing depression among breast cancer patients in Palestine. BMC Cancer 2022; 22(1): 295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Belay W, Labisso WL, Tigeneh W, et al. Magnitude and factors associated with anxiety and depression among patients with breast cancer in central Ethiopia: a cross-sectional study. Front Psychiatry 2022; 13: 957592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dereje E. Assessing the prevalence of depression and anxiety and associated factors among women with breast cancer in Tikur Anbesa Specialized Hospital: Addis Ababa University online repositeries, Masters thesis, 2019. [Google Scholar]
- 27. Cvetković J, an Nenadović M. Depression in breast cancer patients. Psychiatry Res 2016; 240: 343–347. [DOI] [PubMed] [Google Scholar]
- 28. Burgess C, Ramirez A, Richards M, et al. Does the method of detection of breast cancer affect subsequent psychiatric morbidity? Eur J Cancer 2002; 38(12): 1622–1625. [DOI] [PubMed] [Google Scholar]
- 29. Kiebert G, De Haes J, Van de Velde C. The impact of breast-conserving treatment and mastectomy on the quality of life of early-stage breast cancer patients: a review. J Clin Oncol 1991; 9(6): 1059–1070. [DOI] [PubMed] [Google Scholar]
- 30. Dean C. Psychiatric morbidity following mastectomy: preoperative predictors and types of illness. J Psychosom Res 1987; 31(3): 385–392. [DOI] [PubMed] [Google Scholar]
- 31. Opadola O, Alatishe T, Suleiman B, et al. Prevalence of major depressive disorder in patients diagnosed with breast cancer in Southwest Nigeria. Int Res J Oncol 2022; 6(4): 18–25. [Google Scholar]
- 32. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021; 372: n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Critical appraisal tools, https://jbi.global/critical-appraisal-tools (accessed 12 July 2023).
- 34. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002; 21(11): 1539–1558. [DOI] [PubMed] [Google Scholar]
- 35. George BJ, Aban IB. An application of meta-analysis based on DerSimonian and Laird method. J Nucl Cardiol 2016; 23; 690–692. [DOI] [PubMed] [Google Scholar]
- 36. IntHout J, Ioannidis J, Borm GF. The Hartung-Knapp-Sidik-Jonkman method for random effects meta-analysis is straightforward and considerably outperforms the standard DerSimonian-Laird method. BMC Med Res Methodol 2014; 14(1): 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kagee A, Roomaney R, Knoll N. Psychosocial predictors of distress and depression among South African breast cancer patients. Psychooncology 2018; 27(3): 908–914. [DOI] [PubMed] [Google Scholar]
- 38. Isfahani P, Arefy M, Shamsaii M. Prevalence of severe depression in Iranian women with breast cancer: a meta-analysis. Depress Res Treat 2020; 2020: 5871402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Rezaianzadeh A, Mousave M, Hassanipour S, et al. Prevalence of depression among Iranian women with breast cancer: a systematic review and meta-analysis. Health Scope 2019; 8(2): e62781. [Google Scholar]
- 40. Hassan MR, Shah SA, Ghazi HF, et al. Anxiety and depression among breast cancer patients in an urban setting in Malaysia. Asian Pac J Cancer Prev 2015; 16(9): 4031–4035. [DOI] [PubMed] [Google Scholar]
- 41. Su J-A, Yeh D-C, Chang C-C, et al. Depression and family support in breast cancer patients. Neuropsychiatr Dis Treat 2017; 13: 2389–2396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Soqia J, Al-Shafie M, Agha LY, et al. Depression, anxiety and related factors among Syrian breast cancer patients: a cross-sectional study. BMC Psychiatry 2022; 22(1): 796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Dechambenoit G. Access to health care in sub-Saharan Africa. Surg Neurol Int 2016; 7: 108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kingham TP, Alatise OI, Vanderpuye V, et al. Treatment of cancer in sub-Saharan Africa. Lancet Oncol 2013; 14(4): e158–e167. [DOI] [PubMed] [Google Scholar]
- 45. Stierle F, Kaddar M, Tchicaya A, et al. Indigence and access to health care in sub-Saharan Africa. Int J Health Plann Manag 1999; 14(2): 81–105. [DOI] [PubMed] [Google Scholar]
- 46. Srivastava V, Ansari MA, Kumar A, et al. Study of anxiety and depression among breast cancer patients from North India. Clin Psychiatry 2016; 2(1): 4. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-doc-1-smo-10.1177_20503121241226897 for Prevalence and associated factors of depression among breast cancer patients in Sub-Saharan Africa: A systematic review and meta-analysis by Anissa Mohammed, Dagnachew Melak, Fekade Demeke Bayou, Husniya Yasin, Aregash Abebayehu Zerga, Birhanu Wagaye, Fanos Yeshanew Ayele, Ahmed Hussien Asfaw, Natnael Kebede, Asnakew Molla Mekonen, Mengistu Mera Mihiretu, Yawkal Tsega, Elsabeth Addisu, Niguss Cherie, Tesfaye Birhane, Hussien Endris, Zinet Abegaz and Abel Endawkie in SAGE Open Medicine
Supplemental material, sj-docx-2-smo-10.1177_20503121241226897 for Prevalence and associated factors of depression among breast cancer patients in Sub-Saharan Africa: A systematic review and meta-analysis by Anissa Mohammed, Dagnachew Melak, Fekade Demeke Bayou, Husniya Yasin, Aregash Abebayehu Zerga, Birhanu Wagaye, Fanos Yeshanew Ayele, Ahmed Hussien Asfaw, Natnael Kebede, Asnakew Molla Mekonen, Mengistu Mera Mihiretu, Yawkal Tsega, Elsabeth Addisu, Niguss Cherie, Tesfaye Birhane, Hussien Endris, Zinet Abegaz and Abel Endawkie in SAGE Open Medicine
Supplemental material, sj-docx-3-smo-10.1177_20503121241226897 for Prevalence and associated factors of depression among breast cancer patients in Sub-Saharan Africa: A systematic review and meta-analysis by Anissa Mohammed, Dagnachew Melak, Fekade Demeke Bayou, Husniya Yasin, Aregash Abebayehu Zerga, Birhanu Wagaye, Fanos Yeshanew Ayele, Ahmed Hussien Asfaw, Natnael Kebede, Asnakew Molla Mekonen, Mengistu Mera Mihiretu, Yawkal Tsega, Elsabeth Addisu, Niguss Cherie, Tesfaye Birhane, Hussien Endris, Zinet Abegaz and Abel Endawkie in SAGE Open Medicine