Abstract
PURPOSE
Therapeutic alliances (TAs) between oncologists and patients are bonds characterized by mutual caring, trust, and respect. We here relate oncologist characteristics and behaviors to TA among Latino and non-Latino patients with advanced cancer.
METHODS
Participants included non-Latino oncologists (n = 41) and their Latino (n = 67) and non-Latino White (n = 90) patients with advanced cancer who participated in Coping with Cancer III, a multisite, US-based prospective cohort study of Latino/non-Latino disparities in end-of-life cancer care, conducted 2015-2019. Oncologist characteristics included age, sex, race, institution type, Spanish language proficiency, familismo practice style (emphasis on family) and clinical etiquette behaviors. Patient-reported TA was assessed using the average score of six items from The Human Connection scale. Hierarchical linear modeling (HLM) estimated effects of oncologist characteristics on TA.
RESULTS
Of 157 patients, a majority were female (n = 92, 58.6%) and age younger than 65 years (n = 95, 60.5%). Most oncologists were male (n = 24, 58.5%), non-Latino White (n = 25, 61%), and age 40 years and older (n = 25, 61%). An adjusted HLM in the full sample showed that Latino patient ethnicity was associated with significantly lower TA (β = −.25; P < .001). In an adjusted stratified HLM for TA, among Latino patients, oncologist familismo practice style (β = .19; P = .012), preference using first names (β = .25; P = .023), and greater Spanish fluency (β = .11; P < .001) were positively associated with TA. In contrast, familismo practice style had no impact on TA for non-Latino White patients.
CONCLUSION
Latino patients with advanced cancer had worse TAs with their oncologists versus non-Latino patients. Modifiable oncologist behaviors may be targeted in an intervention designed to improve the patient-physician relationship between oncologists and their Latino patients with advanced cancer.
Changing non-Latino oncologist clinical etiquette may help patient-clinician relationships with Latino patients.
INTRODUCTION
The patient-clinician relationship is fundamental to the delivery of high-quality patient-centered medical care.1,2 A therapeutic alliance (TA) is a patient-clinician relationship that is characterized by mutual caring, trust, understanding, and respect; it is presumed to facilitate engagement in shared decision making regarding treatment goals.2-4 A strong TA between oncologists and adult patients with advanced cancer is associated with higher emotional acceptance of terminal illness, decreased invasive interventions, higher quality of life at the end of life,3,5 greater treatment adherence, and less suicidal ideation.6,7 A positive TA between patients with cancer and their oncologists has also been shown to benefit the bereaved caregivers–it has been associated with their enhanced social function, health-related quality of life, and emotional wellbeing after the patient's death.8
CONTEXT
Key Objective
Therapeutic alliances (TAs) are patient-clinician relationships characterized by mutual caring, trust, understanding, and respect. In this study, we examined how non-Latino oncologist characteristics and behaviors were associated with TAs among Latino and non-Latino patients with advanced cancer.
Knowledge Generated
Latino patients with advanced cancer had a worse TA with their oncologists compared with non-Latino White patients. Modifiable oncologist behaviors related to clinical etiquette and communication were found to be associated with the TA. Some oncologist behaviors were shown to relate differently to the TA for Latino patients compared with non-Latino White patients, such as promoting familism in practice, culturally appropriate communication, and physician self-disclosure.
Relevance
Modifiable clinical etiquette behaviors and culturally appropriate communication among non-Latino oncologists may improve patient-clinician TAs with Latino patients and promote the provision of culturally competent and sensitive care to Latino patients with advanced cancer.
The Latino population in the United States is one of the fastest-growing population groups, currently comprising 18.7% of the total US population and projected to increase to 25% by the year 2060.9,10 However, only 4.7% of practicing oncologists self-identify as Hispanic or Latino,11 and this has remained essentially unchanged since 2008 (4.1%).11,12 Furthermore, oncology fellowships are the least diverse of all internal medicine subspecialty fellowships, with the lowest percentage of Latino fellows.13 Although increasing the diversity of the physician workforce may reduce disparities by improving access, cultural effectiveness, and quality of care,14-19 it is important to identify more immediate approaches to improve the quality of cancer care for Latino patients.
Few empirical studies have examined the TA between Latinos and their oncologists in the United States. Our previous prospective study demonstrated a disparity in TA between Latino immigrants with advanced cancer compared with US-born non-Latinos; the latter population were 8-11 times more likely to report a better TA.20 The main drivers of the disparity in this study were patients' perceptions that their oncologists did not care about them, take the time to listen to them, or offer hope.20 Other reported disparities in end-of-life care among Latino patients with advanced cancer include less engagement in advance care planning and prognostic communication with their oncologists, oftentimes leading to an inaccurate understanding of disease course and prognosis,21 and a higher likelihood of receiving value-inconsistent, aggressive end-of-life care when compared with non-Latino patients.22-24
Given the demonstrated importance of the TA between patients with cancer and their oncologists and the current TA disparity in the Latino population, it is imperative to develop strategies that target the patient-clinician relationship in this patient population. The TA between Latino patients and their oncologists is potentially a modifiable factor that can mitigate end-of-life care disparities in this important patient population. In this study, we sought to explore how modifiable oncologist characteristics of interest were associated with the TA in Latino versus non-Latino White patients with advanced cancer, to inform the development of an intervention aimed at providing oncologists with training on how to develop a strong TA with their Latino patients.
METHODS
Sample
This study is based on a sample of non-Latino oncologists (n = 41) and their Latino (n = 67) and non-Latino White (hereafter non-Latino; n = 90) patients who participated in Coping with Cancer III (CwC III), an NIH-sponsored (R01 MD007652), multisite, longitudinal, observational cohort study of patients with advanced cancer, their informal (often family) caregivers, and their oncology providers designed to evaluate the influence of medical, religious, and sociocultural beliefs on Latino/non-Latino ethnic disparities in advance care planning and end-of-life cancer care. CwC III participants were recruited between November 2015 and May 2019 at the following institutions: Memorial Sloan-Kettering Cancer Center (New York, NY), Columbia University Medical Center (New York, NY), Northwestern University Robert H. Lurie Comprehensive Cancer Center (Chicago, IL), Rush University Medical Center (Chicago, IL), University of Texas-Southwestern (Dallas, TX), University of Texas at El Paso (El Paso, TX), and University of Miami Health System (Miami, FL). Institutional review board approval was obtained from all participating sites. Informed consent was provided by all study participants.
Patients were eligible to participate in CwC III if they were diagnosed with locally advanced or metastatic gastrointestinal, gynecologic, or lung cancers and had experienced disease progression on one or more lines of chemotherapy. Thus, patient participants generally had incurable cancers and, as we have shown,23,25 limited (ie, months, not years) life expectancies. Patients were excluded if they were age younger than 21 years, not fluent in either English or Spanish, severely cognitively impaired (ie, Short Portable Mental Status Questionnaire1 score <6),26 judged by research staff members to be too weak or ill to complete study interviews, or enrolled in hospice at the time of study recruitment. Oncology providers were eligible to participate in CwC III if they cared for patients who met the study's patient eligibility criteria.
Trained research staff gathered information directly from patient participants longitudinally in up to two structured interviews, that is, baseline interviews at study entry and follow-up interviews nominally 2 months after baseline. Patients' medical information was obtained by medical chart review. Patient participants received $25 in US dollars per interview. Oncology provider participants provided information about themselves in an online survey completed before the recruitment of any of their patients.
In the present analysis, we focus on effects of characteristics of non-Latino oncologists on TAs with their Latino and non-Latino White patients with advanced cancers. We chose to focus on non-Latino oncologists because they provided care for a majority of CwC III patient participants, and because we were interested in identifying potential mechanisms by which non-Latino oncologists might improve TAs with their Latino patients.
The present analytic sample includes 41 non-Latino oncologists and 157 Latino (n = 67) and non-Latino White (n = 90) patients who participated in CwC III. These 41 non-Latino oncologist participants provided care for 168 Latino and non-Latino patient participants, 157 (93.5%) of whom provided information about their TAs with their oncologists during their baseline interviews. Non-Latino, compared with Latino, patients were more likely to provide TA information (98.9% v 87.0%; P = .002).
Measures
Patient Sociodemographic Characteristics
During their study intake and baseline interviews, patients provided information regarding their age, sex, ethnicity, race, form of health insurance, level of education, and marital status. Site of patient recruitment was categorized by geographic location (north v south).
Oncologist Sociodemographic Characteristics
During their study intake surveys, oncologists provided information regarding their age, sex, and race. Site of oncologist practice was categorized by institution type (cancer center v hospital).
Oncologist Characteristics of Interest
As indicators of clinical etiquette behaviors, oncologists were also asked if they addressed their patients by their first name (“Would you prefer to: address patients by their first name, or, address patients by their last name”) and if they preferred to share personal information about themselves with their patients (“Would you prefer to: tell your patients about personal information, or, not tell your patients personal information”). These behaviors were selected based on evidence from a narrative review of the literature demonstrating a possible association with the patient-physician relationship.27-31 As a measure of cross-cultural engagement, oncologists were asked about their level of Spanish language proficiency, with response options including none (0), elementary (1), limited working proficiency (2), professional working proficiency (3), full professional proficiency (4), and native or bilingual proficiency (5). Familismo, or familism, is a central cultural value among Latinos that emphasizes a strong connection to the family unit, including commitment to support family members both emotionally and financially, reliance on family for help, and deferring to family for how one should think or behave.32 As a proxy for the tendency of an oncologist to practice with style that demonstrates a sensitivity to and awareness of familismo, oncologists' familismo was assessed using the average score from three items from Sabogal's Familism Scale, that is, (1) aging parents should live with relatives, (2) a person should share his/her home with uncles, aunts, or first cousins if they are in need, and (3) the family should consult close relatives (uncles and aunts) concerning its important decisions, each rated on a scale from 1 = strongly disagree to 5 = strongly agree.33,34 These items were internally consistent (Cronbach's α = .64) in the present oncologist study sample.
TA
Patients' TA with their oncologists was assessed using the average score from six items from The Human Connection scale,3 that is, (1) To what extent does your doctor pay close attention to what you are saying? (2) How much do you trust your doctor? (3) How thorough is your doctor? (4) How open-minded do you feel your doctor is? (5) How often does your doctor offer hope? (6) How often does your doctor ask how you are coping with cancer? Each item was rated on a scale from 1 = not at all/never to 4 = to a large extent/extremely/at every visit. These items were internally consistent (Cronbach's α = .73) in the present patient study sample. In the Latino patient subsample (n = 67), 42 (62.7%) were interviewed in Spanish and 25 (37.3%) were interviewed in English.
Statistical Analysis
We described patient and oncologist sample characteristics using frequencies and percentages for categorical variables and means and standard deviations for variables treated as continuous measures. We used two-sample t-tests to evaluate associations between TA and patient attributes. We used two-level hierarchical linear modeling (HLM) to evaluate associations between TA (level-1 outcome) and oncologist attributes (level-2 predictors). We used HLM initially in the full patient sample (n = 157 patients; n = 41 oncologists) to evaluate interactive effects of patient ethnicity and oncologist attributes of interest on TA to determine if effects of oncologist characteristics on TA differ between the Latino and the non-Latino patient groups. We then used HLM in the Latino (n = 67 patients; n = 26 oncologists) and non-Latino (n = 90 patients; n = 35 oncologists) patient samples to evaluate effects of oncologist attributes on TA stratified by patient ethnicity.
We conducted analyses using SAS statistical software, version 9.4 (SAS Institute, Cary, NC), and HLM, version 7 (Scientific Software International, Inc, Skokie, IL). We based statistical inferences on two-sided tests with P < .05 taken to be statistically significant.
RESULTS
Patient Characteristics and Association With TA
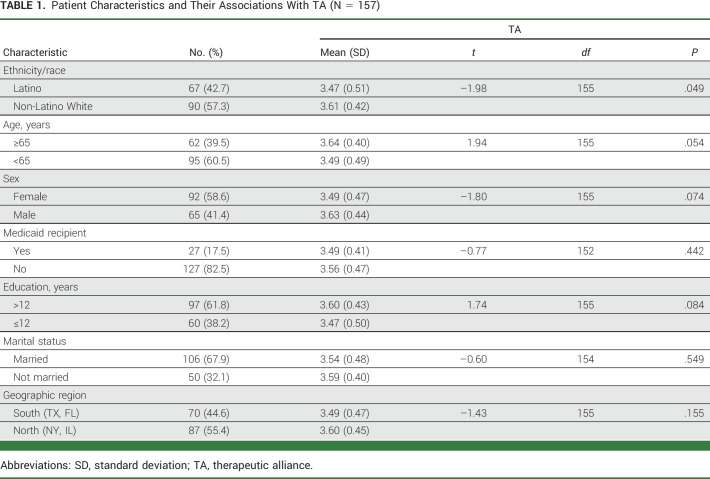
Patient characteristics and their associations with TA are shown in Table 1. Of the 157 patients, 67 (42.7%) patients were Latino; most were female (n = 92, 58.6%) and age younger than 65 years (n = 95, 60.5%). Latino patients had significantly lower mean TA scores compared with non-Latino White patients (3.47 v 3.61, respectively; P = .049). There were no significant associations between age, sex, Medicaid recipient, education level, marital status, and geographic region with TA scores.
TABLE 1.
Patient Characteristics and Their Associations With TA (N = 157)
Oncologist Characteristics and Association With TA in the Full Sample
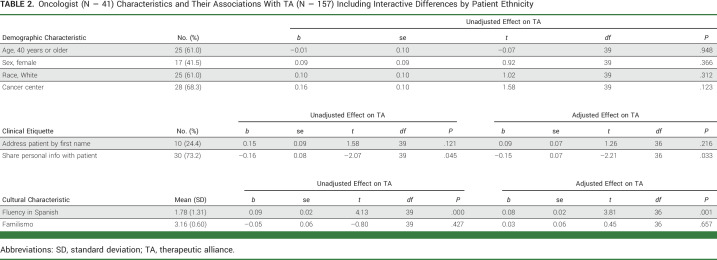
Oncologist characteristics (n = 41) and their associations with TA in the full patient sample are shown in Table 2. Most oncologists were male (n = 24, 58.5%), White (n = 25, 61.0%), and age 40 years or older (n = 25, 61%). Although only 24.4% (n = 10) oncologists stated that they prefer to address their patients by their first name, 73.2% (n = 30) stated that they prefer to share personal information with the patient. Stating a preference for sharing personal information with patients was negatively associated with TA (adjusted β = –.15; P = .033). Greater fluency in Spanish was positively associated with TA (adjusted β = .08; P = .001).
TABLE 2.
Oncologist (N = 41) Characteristics and Their Associations With TA (N = 157) Including Interactive Differences by Patient Ethnicity
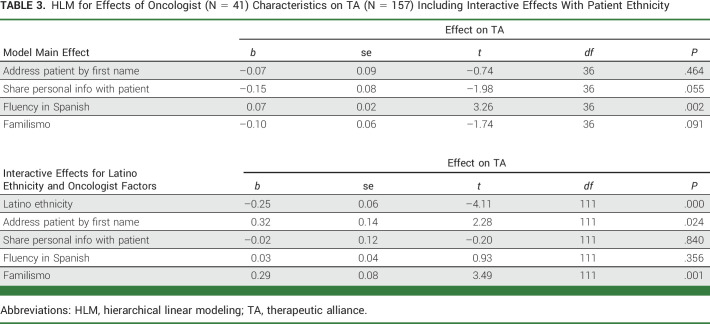
Main and interactive effects of oncologist characteristics of interest and patient Latino ethnicity in the full patient sample are shown in Table 3. Consistent with results presented in Table 2, oncologist preference to share personal information with their patients and greater fluency in Spanish were, respectively, negatively (effect on model intercept: β = –.15; P = .055) and positively (effect on model intercept: β = .07; P = .002) associated with TA irrespective of patient ethnicity (ie, no significant effects on model slope for patient Latino ethnicity). Although neither oncologist preference to address their patients by their first names nor their degree of familismo had effects on the model intercept, both oncologist preference to address patients by their first names (effect on model slope for patient Latino ethnicity: β = .32; P = .024) and degree of familismo (effect on model slope for patient Latino ethnicity: β = .29; P = .001) were significantly associated with greater TA for Latino relative to non-Latino patients. Independent of these effects, Latino ethnicity was associated with lower TA (model slope for patient Latino ethnicity, constant: β = –.25; P < .001).
TABLE 3.
HLM for Effects of Oncologist (N = 41) Characteristics on TA (N = 157) Including Interactive Effects With Patient Ethnicity
Oncologist Characteristics and Association With TA, Stratified by Ethnicity
Given evidence that effects of oncologist characteristics of interest on TA may differ by patient ethnicity, we conducted an analysis of oncologist characteristics and their associations with TA in two separate models, stratified by ethnicity: among Latino patients only (Table 4) and non-Latino patients only (Table 5).
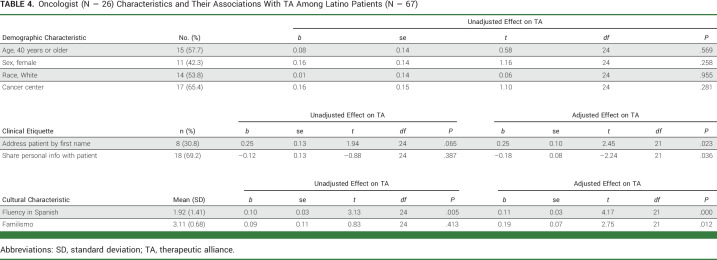
TABLE 4.
Oncologist (N = 26) Characteristics and Their Associations With TA Among Latino Patients (N = 67)
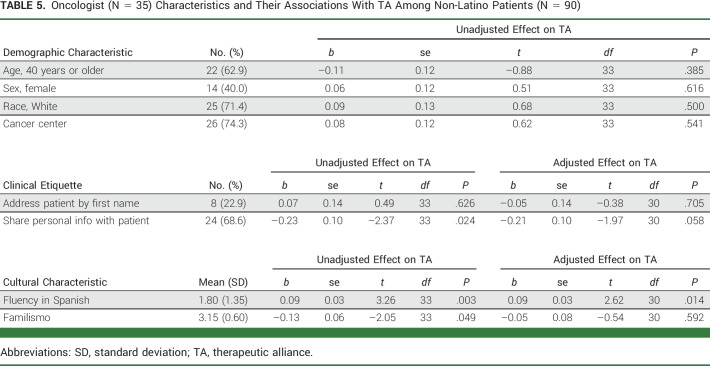
TABLE 5.
Oncologist (N = 35) Characteristics and Their Associations With TA Among Non-Latino Patients (N = 90)
The stratified analysis of oncologist (n = 26) characteristics and their associations with TA among Latino patients (n = 67) are shown in Table 4. In an adjusted model for TA that included four oncologist characteristics of interest as predictors and only Latino patients, oncologist preference to address patients by their first names (β = .25; P = .023), greater fluency in Spanish (β = .11; P < .001), and greater degree of familismo (β = .19; P = .012) were all positively associated with TA; oncologist preference to share personal information with their patients was negatively associated with TA (β = –.18; P = .036).
Oncologist (n = 35) characteristics and their associations with TA among non-Latino patients (n = 90) are found in Table 5. Among non-Latino patients, in an adjusted model for TA including four oncologist characteristics of interest as predictors, oncologist preference to share personal information was negatively (β = –.21; P = .058) and greater fluency in Spanish was positively (β = .09; P = .014) associated with TA.
DISCUSSION
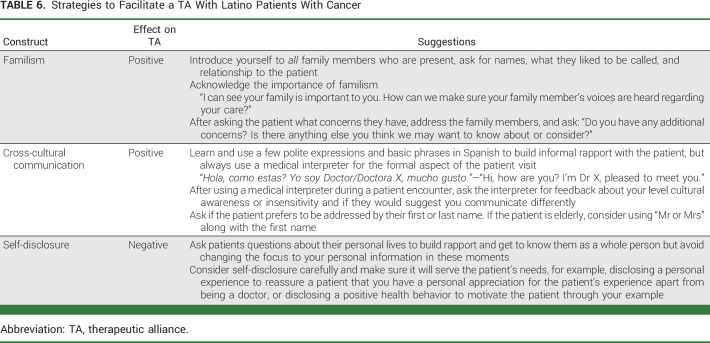
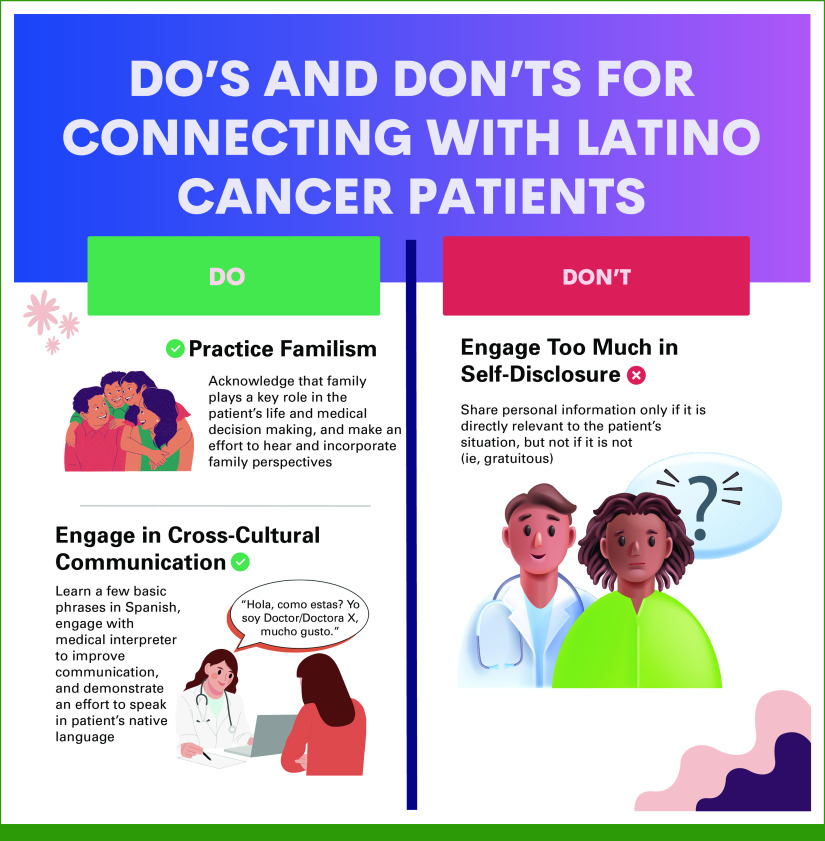
The results of this prospective, multisite cohort study show that Latino patients with advanced cancer had a worse TA with non-Latino oncologists compared with non-Latino White patients. Certain modifiable oncologist behaviors, such as aspects of clinical etiquette and culturally appropriate communication, were found to be associated with TA. Some behaviors were shown to relate differently to TA for Latino compared with non-Latino White patients. Among all patients, preference for sharing personal information with patients was negatively associated with TA, whereas being fluent in Spanish had a positive association with TA. In the stratified and adjusted analysis of Latino patients only, practicing with a familismo style, addressing patients by their first name, and greater Spanish fluency remained positively associated with TA. By contrast, among non-Latino White patients only, practicing with a familismo style was not associated with TA after adjusting for other oncologist characteristics. These clinical etiquette and cross-cultural engagement behaviors are potentially modifiable (Table 6; Fig 1), thereby representing a promising target for an intervention aimed at improving the TA between oncologists and their Latino (and non-Latino) patients with advanced cancer.
TABLE 6.
Strategies to Facilitate a TA With Latino Patients With Cancer
FIG 1.
Do's and don'ts for connecting with Latino patients with cancer.
We found that practicing in a way that is consistent with familism was positively associated with the TA between oncologists and their Latino patients with advanced cancer, but not among non-Latino White patients with advanced cancer. This finding is not surprising, given that familism is a core Latino cultural value that prioritizes the collectivist needs of the family over the needs of oneself, while in mainstream American or US culture, the focus is more individualistic.35 Familism can profoundly affect health care behaviors and use of health care services, particularly in the setting of palliative and end-of-life care.36-38 For example, end-of-life care decisions are often made through family consensus, and often, several family members attend clinic and treatment visits.38 Behaviors that support familism can be incorporated into oncologists' practice with minimal effort. Approaches such as asking their patients what role they would like their family to play in their care, how their family is coping with their illness, and actively engaging and providing emotional support for all family members may signal to patients that their oncologist understands and respects their cultural values, facilitating the development of a TA among Latino patients.
Addressing patients by their first name also was positively associated with TA between oncologists and their Latino patients, but not the non-Latino White patients. Preference for first name is consistent with the cultural value of “personalismo,” which is the valuing of warm, caring, informal, and personal relationships.38,39 Personalismo can lead to the prioritization of people and relationships over conflict, timeliness, efficiency, and other competing priorities.39 Professional relationships with personalismo may involve behaviors such as engaging in chatty conversations (small talk) and/or physical contact and proximity between patients and providers.39,40 Preference for being addressed by their first name is consistent with this cultural value, yet may contradict another core cultural value—respeto. Respeto is deference to societal hierarchal structures based primarily on age, but also positions of authority, sex, and socioeconomic status.40,41 Respeto dictates that one should use formal titles to indicate respect, rather than first names, particularly for older patients.40,41 Several studies have demonstrated that patients tend to prefer being called by their first name.27,28,42-46 However, as we found in this study, most physicians tend not to do so.28,45
With regards to sharing personal information, although this behavior could be construed as beneficial to building a TA, in our study, we found a negative effect when examined in the entire sample, and in the Latino sample when stratified by ethnicity. It may be that this is perceived by patients as the oncologist focusing attention on themselves rather than on them. Although not statistically significant, a similar trend was seen in the non-Latino sample. Our findings are consistent with a study that examined the value of physician self-disclosure in primary care visits by conducting a sequence analysis of transcripts of 113 unannounced, undetected, standardized patient visits to primary care physicians.29 There was no evidence that instances of physician self-disclosure had a positive effect on the encounters, and some were noted to be disruptive. Traditionally, physician self-disclosure is frowned upon47; medical students are taught to behave as a representative of a tradition, of an institution, and, ultimately, of the health care system.48 The patient-physician relationship is of a professional nature, and therefore, there is an expectation that physicians will not disclose personal information since doing so might blur the boundary of professionalism.47,48 However, self-disclosure does have some advantages and may be beneficial.30,31,48 In the right setting and context, self-disclosure can lead to a greater sense of closeness, greater sympathy, and a climate of trust.48 Physician disclosure of healthy personal behaviors has been shown to improve physician credibility and patient motivation.49 In another study, physician self-disclosure of personal illness was evaluated favorably by most patients and encouraged empathy, thereby strengthening the patient-physician relationship.50 Most of the oncologists included in our study reported that they do share personal information, yet this clinical etiquette behavior may have the opposite effect than intended.
As highlighted in the Institute of Medicine 's 2002 Unequal Treatment report, suboptimal communication contributes heavily to disparities in health care quality.51 Language concordance between patient and physician is beneficial to patient satisfaction, and adherence to physician recommendations has been shown to reduce overall patient and hospital costs.52,53 Bilingual doctors have been shown to have a positive impact on quality of care for patients who speak limited English and have higher ratings for interpersonal care.54,55 Our findings also demonstrate a positive effect of Spanish fluency on the TA between oncologists and the Latino patients with advanced cancer. Interestingly, Spanish fluency also had a positive effect on the TA between oncologists on non-Latino White patients. There are limited data on what motivates physicians to learn another language. Although many non-Latino students in the United States learn Spanish during their K–12 years of education as part of their obligatory second language in school, having at least a working proficiency in a second language typically requires advanced training. Perhaps physicians who seek advanced training in a second language have a stronger desire to prioritize communication with their patients than those who do not learn a second language. Learning a second language could also be related to personality traits that would also have a positive impact on relationship building. In a recently published meta-analysis of the Big Five personality traits and second-language learning, openness to experience, a person's willingness of being curious, imaginative, investigative, and exploring, or seeking new experience and intellectual pursuits, was the personality trait that had the strongest positive correlation with learning a second language.56 One who is highly open to experience is likely open and accepting of different cultures, which may facilitate relationship building with patients in general, regardless of racial or ethnic identity.
Spanish is the second most spoken language in the United States, with 13.2% of the total population speaking Spanish at home.57 According to a recent study using the profile data from the leading social network for physicians that includes 70% of all physicians in the United States, 36.2% of US-based physicians who are on this social network speak Spanish.58 Other estimates for Spanish-speaking physicians include 22% using data from the American Board of Family Medicine from 2013 through 2019 (35713629).59 In a cross-sectional analysis of California Medical Board Survey data of 61,138 practicing physicians, 23.5% and 15.5% of primary care and non–primary care physicians, respectively, self-reported fluency in Spanish.60 Most (52%) Spanish-speaking physicians were non-Latino White and 23% were Latinos. Seventeen percent of non-Latino White physicians reported fluency in Spanish compared with 92% of Latino physicians.60 In this study, only 12.2% of participating non-Latino oncologists reported at least professional working proficiency. Thus, there is considerable room for improvement.
The results of our study should be interpreted in the context of its limitations. We found in our small sample of study participants that the non-Latino White patients in the study sample were more likely to provide TA information versus the Latino patients (98.9% v 87.0%; P = .002). This may be due to social desirability bias, where underreporting of negative responses may lead to systematic differences in study results.61 Therefore, an even greater disparity in the TA between Latino patients and their oncologists may be present than observed in our data. Although we enrolled participants from cities in four different states from different regions of the country, we did not recruit from rural populations, which may limit the generalizability of our study findings. Other limitations in the assessment of the TA are that we did not examine if there were changes in TA over time, nor did we account for the duration of the patient-clinician relationship. However, to our knowledge, this is the first study that directly examines oncologist behaviors and cross-cultural engagement and their association with the TA with their Latino and non-Latino patients with advanced cancer. Despite our small sample size, we did find statistically significant and important findings.
In conclusion, cultural differences between Latino patients and the common cultural norms of the US health system may be leveraged via modifiable non-Latino oncologist clinical etiquette behaviors and cross-cultural engagement to improve end-of-life care for Latino patients with advanced cancer. It is important to emphasize that Latinos are a large and heterogeneous group and thus can vary greatly in their adherence to traditional beliefs and values; thus, future research needs to account for such heterogeneity while also identifying common ground to inform the development of effective interventions.62,63 Future studies are needed to confirm these results in larger, more diverse samples and then use this invaluable information to improve patient-clinician TAs to promote sensitive and thoughtful care of Latino patients with advanced cancer.
ACKNOWLEDGMENT
The authors thank Francesco Osso, research assistant at the Cornell Center for Research on End-of-Life Care, for graphic design services.
Ana I. Tergas
Consulting or Advisory Role: Helomics, Merck
Frank J. Penedo
Employment: Blue Note Therapeutics
Consulting or Advisory Role: Blue Note Therapeutics
No other potential conflicts of interest were reported.
SUPPORT
Data collection was supported by R01 grant to P.K.M. and H.G.P. on Latino/non-Latino cancer patient disparities in end-of-life care from the National Institute of Minority Health and Health Disparities (MD007652), a grant to examine health care chaplaincy in reduction of cancer disparities (MD017704), and a UL1 grant to the Weill Cornell Clinical and Translational Science Center from the National Center for Advancing Translational Sciences (TR002384). A.I.T. is a recipient of an NIH K08 Career Development Award (CA245193). H.G.P. was supported by the National Cancer Institute R35 Outstanding Investigator Award (CA197730) and grants from the National Institute of Minority Health and Health Disparities (MD017652 and MD017704).
AUTHOR CONTRIBUTIONS
Conception and design: All authors
Financial support: Ana I. Tergas, Holly G. Prigerson, Paul K. Maciejewski
Administrative support: Holly G. Prigerson
Collection and assembly of data: Ana I. Tergas, Holly G. Prigerson, Paul K. Maciejewski
Data analysis and interpretation: Ana I. Tergas, Frank J. Penedo, Paul K. Maciejewski
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Human Connection: Oncologist Characteristics and Behaviors Associated With Therapeutic Bonding With Latino Patients With Advanced Cancer
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/op/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Ana I. Tergas
Consulting or Advisory Role: Helomics, Merck
Frank J. Penedo
Employment: Blue Note Therapeutics
Consulting or Advisory Role: Blue Note Therapeutics
No other potential conflicts of interest were reported.
REFERENCES
- 1. Mead N, Bower P. Patient-centredness: A conceptual framework and review of the empirical literature. Soc Sci Med. 2000;51:1087–1110. doi: 10.1016/s0277-9536(00)00098-8. [DOI] [PubMed] [Google Scholar]
- 2. Mead N, Bower P. Patient-centred consultations and outcomes in primary care: A review of the literature. Patient Educ Couns. 2002;48:51–61. doi: 10.1016/s0738-3991(02)00099-x. [DOI] [PubMed] [Google Scholar]
- 3. Mack JW, Block SD, Nilsson M, et al. Measuring therapeutic alliance between oncologists and patients with advanced cancer: The Human Connection Scale. Cancer. 2009;115:3302–3311. doi: 10.1002/cncr.24360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mack JW, Jaung T, Uno H, et al. Parent and clinician perspectives on challenging parent-clinician relationships in pediatric oncology. JAMA Netw Open. 2021;4:e2132138. doi: 10.1001/jamanetworkopen.2021.32138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zhang B, Nilsson ME, Prigerson HG. Factors important to patients' quality of life at the end of life. Arch Intern Med. 2012;172:1133–1142. doi: 10.1001/archinternmed.2012.2364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Trevino KM, Fasciano K, Prigerson HG. Patient-oncologist alliance, psychosocial well-being, and treatment adherence among young adults with advanced cancer. J Clin Oncol. 2013;31:1683–1689. doi: 10.1200/JCO.2012.46.7993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Trevino KM, Abbott CH, Fisch MJ, et al. Patient-oncologist alliance as protection against suicidal ideation in young adults with advanced cancer. Cancer. 2014;120:2272–2281. doi: 10.1002/cncr.28740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Trevino KM, Maciejewski PK, Epstein AS, et al. The lasting impact of the therapeutic alliance: Patient-oncologist alliance as a predictor of caregiver bereavement adjustment. Cancer. 2015;121:3534–3542. doi: 10.1002/cncr.29505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jones N, Marks R, Ramirez R, et al. https://www.census.gov/library/stories/2021/08/improved-race-ethnicity-measures-reveal-united-states-population-much-more-multiracial.html 2020 census illuminates racial and ethnic composition of the country.
- 10.Vespa J, Medina L, Armstrong D.Demographic turning points for the United States: Population projections for 2020 to 2060. Current Population Report Number P25-1144, 2020. https://www.census.gov/library/publications/2020/demo/p25-1144.html
- 11.AAMC https://www.aamc.org/data-reports/workforce/report/diversity-medicine-facts-and-figures-2019 Diversity in medicine: Facts and figures 2019. Association of American Medical Colleges (AAMC), 2019.
- 12. Lett E, Murdock HM, Orji WU, et al. Trends in racial/ethnic representation among US medical students. JAMA Netw Open. 2019;2:e1910490. doi: 10.1001/jamanetworkopen.2019.10490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Santhosh L, Babik JM. Trends in racial and ethnic diversity in internal medicine subspecialty fellowships from 2006 to 2018. JAMA Netw Open. 2020;3:e1920482. doi: 10.1001/jamanetworkopen.2019.20482. [DOI] [PubMed] [Google Scholar]
- 14. Moy E, Bartman BA. Physician race and care of minority and medically indigent patients. JAMA. 1995;273:1515–1520. [PubMed] [Google Scholar]
- 15. Komaromy M, Grumbach K, Drake M, et al. The role of black and Hispanic physicians in providing health care for underserved populations. N Engl J Med. 1996;334:1305–1310. doi: 10.1056/NEJM199605163342006. [DOI] [PubMed] [Google Scholar]
- 16. Cohen JJ, Gabriel BA, Terrell C. The case for diversity in the health care workforce. Health Aff. 2002;21:90–102. doi: 10.1377/hlthaff.21.5.90. [DOI] [PubMed] [Google Scholar]
- 17. Walker KO, Moreno G, Grumbach K. The association among specialty, race, ethnicity, and practice location among California physicians in diverse specialties. J Natl Med Assoc. 2012;104:46–52. doi: 10.1016/s0027-9684(15)30126-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Duma N, Velazquez AI, Franco I, et al. Dónde Están? Latinx/Hispanic representation in the oncology workforce: Present and future. JCO Oncol Pract. 2022;18:388–395. doi: 10.1200/OP.22.00153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Penner LA, Dovidio JF, Gonzalez R, et al. The effects of oncologist implicit racial bias in racially discordant oncology interactions. J Clin Oncol. 2016;34:2874–2880. doi: 10.1200/JCO.2015.66.3658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tergas AI, Prigerson HG, Shen MJ, et al. Disparities in therapeutic alliance among Latino immigrants with advanced cancer. J Pain Symptom Manage. 2022;64:e173–e176. doi: 10.1016/j.jpainsymman.2022.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ingersoll LT, Alexander SC, Priest J, et al. Racial/ethnic differences in prognosis communication during initial inpatient palliative care consultations among people with advanced cancer. Patient Educ Couns. 2019;102:1098–1103. doi: 10.1016/j.pec.2019.01.002. [DOI] [PubMed] [Google Scholar]
- 22. Weeks JC, Catalano PJ, Cronin A, et al. Patients' expectations about effects of chemotherapy for advanced cancer. N Engl J Med. 2012;367:1616–1625. doi: 10.1056/NEJMoa1204410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Enzinger AC, Zhang B, Schrag D, et al. Outcomes of prognostic disclosure: Associations with prognostic understanding, distress, and relationship with physician among patients with advanced cancer. J Clin Oncol. 2015;33:3809–3816. doi: 10.1200/JCO.2015.61.9239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gramling R, Fiscella K, Xing G, et al. Determinants of patient-oncologist prognostic discordance in advanced cancer. JAMA Oncol. 2016;2:1421–1426. doi: 10.1001/jamaoncol.2016.1861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lambden J, Zhang B, Friedlander R, et al. Accuracy of oncologists' life-expectancy estimates recalled by their advanced cancer patients: Correlates and outcomes. J Palliat Med. 2016;19:1296–1303. doi: 10.1089/jpm.2016.0121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23:433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 27. Gillette RD, Filak A, Thorne C. First name or last name: Which do patients prefer? J Am Board Fam Pract. 1992;5:517–522. [PubMed] [Google Scholar]
- 28. Makoul G, Zick A, Green M. An evidence-based perspective on greetings in medical encounters. Arch Intern Med. 2007;167:1172–1176. doi: 10.1001/archinte.167.11.1172. [DOI] [PubMed] [Google Scholar]
- 29. McDaniel SH, Beckman HB, Morse DS, et al. Physician self-disclosure in primary care visits: Enough about you, what about me? Arch Intern Med. 2007;167:1321–1326. doi: 10.1001/archinte.167.12.1321. [DOI] [PubMed] [Google Scholar]
- 30. Beach MC, Roter D, Larson S, et al. What do physicians tell patients about themselves? A qualitative analysis of physician self-disclosure. J Gen Intern Med. 2004;19:911–916. doi: 10.1111/j.1525-1497.2004.30604.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Beach MC, Roter D, Rubin H, et al. Is physician self-disclosure related to patient evaluation of office visits? J Gen Intern Med. 2004;19:905–910. doi: 10.1111/j.1525-1497.2004.40040.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Llanque SM, Enriquez M. Interventions for Hispanic caregivers of patients with dementia: A review of the literature. Am J Alzheimers Dis Other Demen. 2012;27:23–32. doi: 10.1177/1533317512439794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Campos B, Roesch SC, Gonzalez P, et al. Measurement properties of Sabogal's Familism Scale: Findings from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL) Sociocultural Ancillary Study. J Lat Psychol. 2019;7:257–272. doi: 10.1037/lat0000126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Sabogal F, Marín G, Otero-Sabogal R, et al. Hispanic familism and acculturation: What changes and what doesn't? Hispanic J Behav Sci. 1987;9:397–412. [Google Scholar]
- 35. Balbim GM, Marques IG, Cortez C, et al. Coping strategies utilized by middle-aged and older Latino caregivers of loved ones with Alzheimer's disease and related dementia. J Cross Cult Gerontol. 2019;34:355–371. doi: 10.1007/s10823-019-09390-8. [DOI] [PubMed] [Google Scholar]
- 36. Savage B, Foli KJ, Edwards NE, et al. Familism and health care provision to Hispanic older adults. J Gerontol Nurs. 2016;42:21–29. doi: 10.3928/00989134-20151124-03. quiz 30-31. [DOI] [PubMed] [Google Scholar]
- 37. Garcini LM, Brown RL, Chen MA, et al. Bereavement among widowed Latinos in the United States: A systematic review of methodology and findings. Death Stud. 2021;45:342–353. doi: 10.1080/07481187.2019.1648328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Adames HY, Chavez-Dueñas NY, Fuentes MA, et al. Integration of Latino/a cultural values into palliative health care: A culture centered model. Palliat Support Care. 2014;12:149–157. doi: 10.1017/S147895151300028X. [DOI] [PubMed] [Google Scholar]
- 39. Davis RE, Lee S, Johnson TP, et al. Measuring the elusive construct of personalismo among Mexican American, Puerto Rican, and Cuban American adults. Hisp J Behav Sci. 2019;41:103–121. doi: 10.1177/0739986318822535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Juckett G. Caring for Latino patients. Am Fam Physician. 2013;87:48–54. [PubMed] [Google Scholar]
- 41. Floríndez LI, Floríndez DC, Como DH, et al. Differing interpretations of health care encounters: A qualitative study of non-Latinx health care providers' perceptions of Latinx patient behaviors. PLoS One. 2020;15:e0236706. doi: 10.1371/journal.pone.0236706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. McKinstry B. Should general practitioners call patients by their first names? BMJ. 1990;301:795–796. doi: 10.1136/bmj.301.6755.795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Wallace LS, Cassada DC, Ergen WF, et al. Setting the stage: Surgery patients' expectations for greetings during routine office visits. J Surg Res. 2009;157:91–95. doi: 10.1016/j.jss.2009.03.065. [DOI] [PubMed] [Google Scholar]
- 44. Parsons SR, Hughes AJ, Friedman ND. ‘Please don't call me Mister’: Patient preferences of how they are addressed and their knowledge of their treating medical team in an Australian hospital. BMJ Open. 2016;6:e008473. doi: 10.1136/bmjopen-2015-008473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Limon D, Perry S, Granot T, et al. ReCAP: Perspectives of patients, caregivers, and medical staff on greetings in oncology practice: A prospective survey. JCO Oncol Pract. 2016;12:170–171; e188-e196. doi: 10.1200/JOP.2015.006049. [DOI] [PubMed] [Google Scholar]
- 46. Davies-House A, Ball N, Balmer C. Meeting and greeting in the clinical setting—Are we doing what patients want? Br Dent J. 2017;222:457–461. doi: 10.1038/sj.bdj.2017.269. [DOI] [PubMed] [Google Scholar]
- 47. Candib LM. What should physicians tell about themselves to patients? Am Fam Physician. 2001;63:1440–1442. [PubMed] [Google Scholar]
- 48. Lussier MT, Richard C. Communication tips. Self-disclosure during medical encounters. Can Fam Physician. 2007;53:421–422. [PMC free article] [PubMed] [Google Scholar]
- 49. Frank E, Breyan J, Elon L. Physician disclosure of healthy personal behaviors improves credibility and ability to motivate. Arch Fam Med. 2000;9:287–290. doi: 10.1001/archfami.9.3.287. [DOI] [PubMed] [Google Scholar]
- 50. Knishkowy B, Guggenheim N. The ill physician who self-discloses: What do patients think? Eur J Gen Pract. 2022;28:244–251. doi: 10.1080/13814788.2022.2146091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care . In: Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Smedley BD, Stith AY, et al., editors. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 52. Stoneking LR, Waterbrook AL, Garst Orozco J, et al. Does Spanish instruction for emergency medicine resident physicians improve patient satisfaction in the emergency department and adherence to medical recommendations? Adv Med Educ Pract. 2016;7:467–473. doi: 10.2147/AMEP.S110177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Jacobs EA, Sadowski LS, Rathouz PJ. The impact of an enhanced interpreter service intervention on hospital costs and patient satisfaction. J Gen Intern Med. 2007;22:306–311. doi: 10.1007/s11606-007-0357-3. suppl 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Flores G. The impact of medical interpreter services on the quality of health care: A systematic review. Med Care Res Rev. 2005;62:255–299. doi: 10.1177/1077558705275416. [DOI] [PubMed] [Google Scholar]
- 55. Detz A, Mangione CM, Nunez de Jaimes F, et al. Language concordance, interpersonal care, and diabetes self-care in rural Latino patients. J Gen Intern Med. 2014;29:1650–1656. doi: 10.1007/s11606-014-3006-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Chen X, He J, Swanson E, et al. Big five personality traits and second language learning: A meta-analysis of 40 years’ research. Educ Psychol Rev. 2022;34:851–887. [Google Scholar]
- 57.UCB https://data.census.gov/table?tid=ACSDP5Y2021.DP02&hidePreview=true U.S. Census Bureau American Community Survey 5-year estimates data profiles, 2021.
- 58.Doximity https://press.doximity.com/articles/first-ever-national-study-to-examine-different-languages-spoken-by-us-doctors First-ever national study to examine different languages spoken by U.S. doctors, 2017.
- 59. Flores-Rodarte J, Topmiller M, Jabbarpour Y. Distribution of Spanish-speaking family physicians, 2013-2019. Am Fam Physician. 2022;105:654–655. [PubMed] [Google Scholar]
- 60. Moreno G, Walker KO, Grumbach K. Self-reported fluency in non-English languages among physicians practicing in California. Fam Med. 2010;42:414–420. [PMC free article] [PubMed] [Google Scholar]
- 61. Krumpal I. Determinants of social desirability bias in sensitive surveys: A literature review. Qual Quant. 2013;47:2025–2047. [Google Scholar]
- 62. Huerta EE, Macario E. Communicating health risk to ethnic groups: Reaching Hispanics as a case study. JNCI Monogr. 1999;1999:23–26. doi: 10.1093/oxfordjournals.jncimonographs.a024202. [DOI] [PubMed] [Google Scholar]
- 63. Zamudio CD, Sanchez G, Altschuler A, et al. Influence of language and culture in the primary care of Spanish-speaking Latino adults with poorly controlled diabetes: A qualitative study. Ethn Dis. 2017;27:379–386. doi: 10.18865/ed.27.4.379. [DOI] [PMC free article] [PubMed] [Google Scholar]