Abstract
Background and study aims Chronically inflamed colonic mucosa is primed to develop dysplasia identified at surveillance colonoscopy by targeted or random biopsies. We aimed to explore the effect of mucosal inflammation on detection of visible and “invisible” dysplasia and the concordance between the degree of endoscopic and histologic inflammation.
Patients and methods This was a 6-year cross-sectional analysis of endoscopic and histologic data from IBD. A multinomial model was created to estimate the odds for a specific lesion type as well as the odds of random dysplasia relative to the degree of inflammation. Kappa statistics were used to measure concordance between endoscopic and histologic inflammation.
Results A total of 3437 IBD surveillance colonoscopies between 2016–2021 were reviewed with 970 procedures from 721 patients containing 1603 visible lesions. Kappa agreement between histologic and endoscopic degree of inflammation was low at 0.4. There was a positive association between increased endoscopic inflammation and presence of tubulovillous adenomas (TVAs) (odds ratio [OR] 2.18; 95% confidence interval [CI] 1.03–4.62; P =0.04). Among cases with visible lesions, the yield of concomitant random dysplasia was 2.7% and 1.9% for random indefinite dysplasia. The odds of random dysplasia significantly increased as the degree of endoscopic and histologic inflammation increased (OR 2.18, 95%CI 1.46–3.26; P <0.001 and OR 2.75; 95%CI 1.65–4.57, P <0.001, respectively. The odds of indefinite random dysplasia also significantly increased as endoscopic and histologic inflammation increased (OR 2.90; 95%CI 1.85, 4.55, P <0.001 and OR 1.98; 95%CI 1.08, 3.62, P <0.035, respectively.
Conclusions Endoscopic and histologic inflammation are associated with higher odds of finding TVAs and random low-grade, high-grade, and indefinite dysplasia. Concordance between histologic and endoscopic inflammation severity is low.
Keywords: Inflammatory bowel disease; Diagnosis and imaging (inc chromoendoscopy, NBI, iSCAN, FICE, CLE...)
Introduction
Longstanding inflammatory bowel disease (IBD) is associated with a higher risk of developing colorectal cancer (CRC) 1 with declining incidence in the past 30 years, likely secondary to better therapeutic control of inflammation, improved surveillance strategies, enhanced technologies for dysplasia detection, and effective endoscopic treatment of colorectal lesions 2 3 . Current guidelines recommend surveillance colonoscopy 8 to 10 years after diagnosis of ulcerative colitis (UC) or Crohn’s colitis, followed by surveillance at 1- to 3-year intervals, while for IBD-primary sclerosing cholangitis (PSC), the recommendation is for colonoscopy at diagnosis and then annually 4 5 6 7 8 .
During surveillance colonoscopy, patients with IBD can present a wide array of colorectal lesions, including non-dysplastic lesions (hyperplastic polyps, lymphoid aggregates and pseudopolyps); dysplastic lesions (tubular adenomas now referred as polypoid dysplasia containing low/high or indefinite dysplasia, tubulovillous adenomas (TVAs), sessile serrated adenomas/polyps, adenocarcinomas), and serrated epithelial changes (SECs), which are increasingly identified in patients with longstanding colitis 9 10 .
Some dysplastic lesions may be flat and difficult to visualize, especially when localized within inflamed mucosa. This has led to continued recommendations for random mucosal sampling for detection of “invisible” dysplasia 11 12 13 14 . Importantly, inflammation at the time of surveillance is also associated with increased findings of dysplasia in random biopsies 15 16 17 18 and development of CRC has been linked to persistent subclinical histologic inflammation 19 20 21 22 23 . Current guidelines endorse endoscopic healing (EH) as an objective therapeutic target, with histologic healing as an adjunctive one 24 and several endoscopic and histologic scoring systems for inflammation have been developed to document mucosal healing with poor correlation or agreement between these scores 25 26 .
The aims of this study were to assess the effect of mucosal inflammation on type of visible colorectal lesions identified at surveillance colonoscopy, assess the association between degree of mucosal inflammation and yield of dysplasia found in random biopsies, and analyze the concordance between endoscopic and histologic degree of inflammation.
This study was approved by the Institutional Review Board of Mayo Clinic. There was no potential harm to patients given the cross-sectional and deidentified nature of the study.
Patients and methods
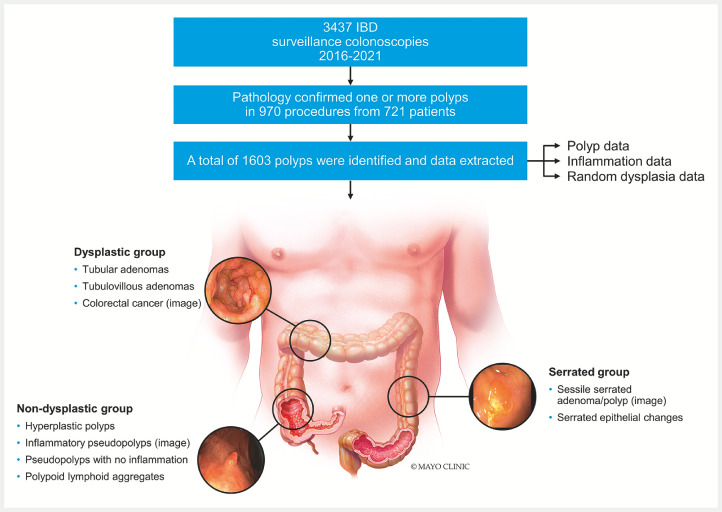
This was a 6-year (2016–2021) cross-sectional study at a tertiary care center with IBD expertise. We included 970 surveillance colonoscopies from 721 subjects with IBD who were found to have visible colorectal lesions during surveillance with available corresponding pathology for the lesion ( Fig. 1 ).
Fig. 1.
Study flowchart and types of visible colorectal lesions included in the study. Source: Used with permission of Mayo Foundation for Medical Education and Research, all rights reserved.[rerif]
Exclusion criteria included patients with no history of IBD, patients with IBD undergoing colonoscopy for an indication other than surveillance, patients with IBD who underwent surveillance colonoscopy but did not have visible lesions sampled or the pathology report of visible lesions was not available, patients who declined research participation.
Pertinent data were extracted from the endoscopy and pathology reports for each case. Chart review was performed to obtain patient, procedure, and lesion characteristics. ( Table 1 )
Table 1 Patient, lesion, and procedure characteristics .
| Patient characteristics (first procedure per patient) [N=721] | |
| SD, standard deviation; UC, ulcerative colitis; CD, Crohn’s disease; HGD, high-grade dysplasia; LGD, low-grade dysplasia; CRC, colorectal cancer; EMR, endoscopic mucosal resection; APC, Argon plasma coagulation; HDWL, high-definition white light; NBI, narrow-band imaging. | |
| Gender | |
|
285 (39.5%) |
|
436 (60.5%) |
| Age at procedure | |
|
57 (43, 66) |
|
54.2 (15.0) |
| Years since IBD diagnosis | |
|
12.8 (7.2, 21.4) |
|
15.5 (11.4) |
| Age at diagnosis | |
|
37 (26, 52) |
|
38.5 (16.2) |
| |
|
471 (66.0%) |
|
237 (33.2%) |
| History of smoking at index | |
|
89 (12.9%) |
|
599 (87.1%) |
| PSC at index | |
|
149 (21.7%) |
|
539 (78.3%) |
| History of random dysplasia at index colonoscopy | |
|
14 (2.0%) |
|
94 (13.7%) |
|
579 (84.3%) |
| Family history of CRC | |
|
172 (26.4%) |
|
480 (73.6%) |
| Lesion characteristics [N=1603] | |
| Size | |
|
1080 (68.6%) |
|
306 (19.4%) |
|
138 (8.8%) |
|
50 (3.2%) |
| Location | |
|
399 (25.1%) |
|
74 (4.7%) |
|
282 (17.7%) |
|
29 (1.8%) |
|
234 (14.7%) |
|
325 (20.5%) |
|
204 (12.8%) |
|
42 (2.6%) |
| Lesion dysplasia | |
|
1146 (72.4%) |
|
26 (1.6%) |
|
397 (25.1%) |
|
8 (0.5%) |
|
3 (0.2%) |
|
3 (0.2%) |
| Morphology | |
|
1093 (73.7%) |
|
34 (2.3%) |
|
42 (2.8%) |
|
166 (11.2%) |
|
1 (0.1%) |
|
18 (1.2%) |
|
0 (0.0%) |
|
80 (5.4%) |
|
50 (3.4%) |
| Resection technique | |
|
745 (47.8%) |
|
481 (30.9%) |
|
210 (13.5%) |
|
112 (7.2%) |
|
11 (0.7%) |
| Histopathology | |
|
356 (22.6%) |
|
345 (21.9%) |
|
283 (18.0%) |
|
182 (11.6%) |
|
153 (9.7%) |
|
67 (4.3%) |
|
12 (0.8%) |
|
55 (3.5%) |
|
19 (1.2%) |
|
11 (0.7%) |
|
83 (5.7%) |
|
6 (0.4%) |
| Endoscopic modality for lesion assessment | |
|
819 (59.0%) |
|
166 (12.0%) |
|
248 (17.9%) |
|
154 (11.1%) |
| Procedure characteristics [N=970] | |
| Bowel prep | |
|
655 (67.9%) |
|
259 (26.9%) |
|
50 (5.2%) |
| Chromoendoscopy performed | |
|
326 (33.6%) |
|
644 (66.4%) |
Procedure details
At our institution, random biopsies are routinely obtained segmentally during IBD surveillance colonoscopies. A standard protocol is followed by obtaining eight biopsies per colon segment – cecum and ascending, transverse, descending, and rectosigmoid. These are placed in four separate pathology bottles, labeled with the anatomic segment as such. This yields a total of 32 biopsies (8 bites in each of the 4 segments) per colonoscopy. All visible dysplasia that is removed or sampled is placed in separate bottles, labeled with the corresponding location. All colonoscopies were performed with high-definition white light (HDWL) and/or dye-based chromoendoscopy (CE), which is obtained when the patient has risk factors for development of dysplasia or CRC including prior dysplasia, concomitant PSC, or a personal history of prior CRC. However, if there is active inflammation or inadequate bowel preparation at the time of surveillance, we forego CE due to inefficacy in these settings.
Endoscopic inflammation
The degree of endoscopic inflammation was classified as inactive, mild, moderate, or severe based on the highest reported degree of inflammation in the colon. At our center, the Mayo Endoscopic Subscore (MES) is used for patients with UC. For Crohn's disease cases, the endoscopic degree of inflammation was extracted from endoscopy reports with the majority of endoscopists describing it as inactive, mild, moderate, or severe, similar to the MES. The Simple Endoscopic Score for Crohn Disease (SES-CD) was not applied for all procedures in patients with Crohn’s colitis, and hence was not utilized in this study. Endoscopists had a wide range of experience from<5 years to > 30 years of gastroenterology practice. All endoscopists in the practice (approximately 50) are trained to perform surveillance colonoscopy in patients with IBD.
Histologic inflammation
Pathologists who interpreted the samples were gastroenterology-focused (approximately 8 in any time period). Some have<5 years to > 30 years of experience. When there is uncertainty regarding a case, pathologists discuss among the group for consensus. For histologic scoring of inflammation, the system utilized in our center includes inactive – no inflammatory cells; mildly active when there is evidence of focal neutrophilic cryptitis; moderately active showing at least one crypt abscess, crypt loss, scattered ulcers; and severely active showing multiple crypt abscesses, numerous ulcers, and areas of denuded mucosa. The degree of histologic inflammation was reported per colonic segment. ( Fig. 1, Supplementary material )
Dysplasia assessment
Dysplasia in random biopsies was classified as low-grade dysplasia (LGD), high-grade dysplasia (HGD), or indefinite dysplasia (IND), accounting for the severest degree of dysplasia identified in any colon segment. LGD features included enlarged, crowded nuclei with pseudostratification, and dark nuclei no longer confined to the base of the cell but maintaining polarity and uniform size and shape. HGD was determined when both architectural and cytologic changes with some key features including complex architecture, glands within glands, variability in nuclear size and shape, loss of nuclear polarity, and prominent nucleoli were seen. IND included some features of dysplasia (enlarged, dark nuclei) but not enough features for dysplasia to be reported. Acute inflammation tends to produce dysplasia-like changes, with abundant neutrophils, which can lead the pathologist to label it IND.
All colonoscopies were performed with HDWL, and/or CE, including dye-based CE or HDWL plus virtual CE at the endoscopist’s discretion. A recent American Gastroenterological Association clinical practice update on IBD surveillance indicates that virtual CE is a suitable alternative to dye spray CE for dysplasia detection in individuals with colonic IBD when using HDWL 7
Statistical analysis
Logistic regression was used to measure associations between endoscopic and histologic degree of inflammation and odds of finding random dysplasia. A multinomial model was created to estimate the odds for a type of colorectal lesion relative to increased degree of endoscopic and histologic inflammation as well as the odds of a specific lesion type when synchronous “invisible” dysplasia was found. Agreement between endoscopic and histologic degree of inflammation was measured with Kappa statistics and marginal homogeneity was tested.
Results
Procedure characteristics
A total of 3437 of the surveillance colonoscopies performed between 2016 and 2021 had pathology available for analysis. A total of 970 procedures from 721 patients contained 1603 visible lesions. Bowel preparation per the Boston Bowel Prep Scale was good, fair, and poor in 68%, 27%, and 5% of procedures, respectively, and preparation quality was not affected by the degree of colon inflammation ( P =0.09). Random biopsies were taken in 95.4% of cases. Dye-based CE was performed in 326 procedures (34%) and was not associated with higher odds of finding polypoid dysplasia (odds ratio [OR]: 1.07; 95% confidence interval [CI]: 0.86–1.35; P =0.54), or higher odds of finding SECs (OR:1.34; 95%CI: 0.82–2.19; P =0.24) when compared with HDWLE.
Patient characteristics
Males comprised 61% of patients. The median age at the time of index procedure was 57 years (interquartile range [IQR] 43–66). The median disease duration from IBD diagnosis to index colonoscopy was 12.8 years (IQR 7.2–21.4) and the average age for initial IBD diagnosis was 37 years (IQR 26–52). Sixty-six percent of patients had UC, 33% had CD, and 0.8% had indeterminate colitis (IC).
Analysis for risk factors for colonic dysplasia revealed that 22% of patients had a concomitant diagnosis of PSC at index colonoscopy, 26% had a family history of first-degree relative with CRC, 13% were active cigarette smokers, 14% had a prior finding of LGD in random biopsies, and 2% had a prior finding of HGD in random biopsies. A concomitant diagnosis of PSC was associated with a higher degree of endoscopic inflammation ( P =0.036) and histologic inflammation ( P =0.025). PSC at index colonoscopy was also associated with concomitant random LGD or HGD (38.1% for PSC patients vs 20.5% for no PSC, P =0.05). PSC was significantly associated with random IND (62% for PSC vs 20% for no PSC, P =0.001). Patients who exhibited moderate and severe histologic and endoscopic inflammation were significantly younger than those with inactive or mild disease (42 vs 56 years old for severe vs inactive endoscopic disease, and 37 vs 59 years old for severe vs inactive histologic disease, P <0.001). Presence of dysplasia in random biopsies in a prior surveillance colonoscopy was significantly associated with a current/new finding of random, non-visible dysplasia ( P <0.001) ( Table 1 Supplementary ).
Characteristics of visible colorectal lesions
Visible lesions were evaluated with HDWL (59%), NBI (12%), dye-based CE (18%) or multiple methods (11%). Sixty-nine percent of identified visible lesions measured ≤ 5 mm and the most common locations were cecum, ascending, sigmoid, and rectosigmoid colon. Of the lesions, 59.4% were non-dysplastic, 24.4% were dysplastic, and 14.9% were serrated. The term sessile was used in the endoscopy report to describe the lesion morphology in 74% of cases followed by the term flat in 11% of cases. Lesions were fully resected in 83% of cases and biopsied in 17% of cases. Patients with CD were more likely to have a dysplastic visible lesion than patients with UC or IC (OR 1.34; 95% CI 1.06, 1.71; P =0.016), The most common type of lesion in patients with CD was polypoid LGD (27.3%) followed by inflammatory pseudopolyps (21.2%). The most common type of lesion in patients with UC was inflammatory pseudopolyps (22.3%) followed by polypoid LGD (20.5%). Hyperplastic polyps were the third most common type of visible lesion for both UC and CD. There were seven cases of CRC in UC (0.7%) and four cases of CRC in CD (0.8%).
Association between lesion histopathology and degree of inflammation
Endoscopic inflammation The severity of endoscopic disease activity was as follows: inactive 63%, mild 25%, moderate 9%, severe 3%. There was a positive association between higher degree of endoscopic inflammation and presence of inflammatory pseudopolyps (OR 1.79; 95%CI 1.25–2.55; P =0.001) and TVA with LGD (OR 2.18; 95%CI 1.03–4.62; P =0.04). All additional lesion types were not associated with higher presence of endoscopic inflammation.
Histologic inflammation The frequency of histologic disease activity was as follows: inactive 59%, mild 32%, moderate 9%, severe 0.3%. There was a negative association between higher degree of histologic inflammation and presence of hyperplastic polyps (OR 0.61; 95%CI 0.41–0.93; P =0.02) and a positive association between higher degree of histologic inflammation and presence of inflammatory pseudopolyps (OR 1.67; 95%CI 1.15–2.43; P =0.007) ( Table 2 )
Table 2 Association between endoscopic and histologic inflammation and polyp type.
| Inflammatory pseudopolyp | Hyperplastic polyp | Pseudopolyp with no inflammation | Sessile serrated adenoma | Serrated epithelial change | Polypoid low-grade dysplasia | Tubulo-villous adenoma | Adenocarcinoma | |
| CI, confidence interval. | ||||||||
| Endoscopic inflammation | ||||||||
| Inactive | 177 (17.2%) | 212 (20.6%) | 125 (12.2%) | 101 (9.8%) | 47 (4.6%) | 233 (22.7%) | 4 (0.4%) | 8 (0.8%) |
| Mild | 100 (27.9%) | 54 (15.0%) | 38 (10.6%) | 32 (8.9%) | 11 (3.1% | 83 (23.1%) | 5 (1.4%) | 3 (0.8%) |
| Moderate | 45 (34.9%) | 12 (9.3%) | 12 (9.3%) | 15 (11.6%) | 8 (6.2%) | 29 (22.5%) | 3 (2.3%) | 0 (0.0%) |
| Severe | 18 (47.4%) | 3 (7.9%) | 6 (15.8%) | 1 (2.6%) | 1 (2.6%) | 5 (13.2) | 0 (0.0%) | 0 (0.0%) |
| P value | 0.001 | 0.48 | 0.41 | 0.39 | 0.47 | 0.33 | 0.042 | 0.65 |
| OR 95% CI |
1.79
(1.25–2.55) |
0.87 (0.59 – 1.28) |
1.18 (0.80–1.74) |
1.19 (0.80–1.78) |
1.19 (0.74–1.90) |
1.20 (0.83–1.72) |
2.18
(1.03–4.63) |
0.78 (0.26–2.35) |
| Histologic inflammation | ||||||||
| Inactive | 145 (15.1%) | 205 (21.3%) | 127 (13.2%) | 109 (11.3%) | 45 (4.7%) | 216 (22.5%) | 2 (0.2%) | 6 (0.6%) |
| Mild | 155 (33.3%) | 58 (12.5%) | 43 (9.2%) | 35 (7.5%) | 14 (3.0%) | 106 (22.8%) | 8 (1.7%) | 5 (1.1%) |
| Moderate | 42 (37.8%) | 12 (10.8%) | 11 (9.9%) | 6 (5.4%) | 3 (2.7%) | 26 (23.4%) | 1 (0.9%) | 0 (0%) |
| Severe | 1 (33.3%) | 0 (0%) | 1 (33.3%) | 0 (0%) | 0 (0%) | 0 (0.0%) | 0 (0%) | 0 (0%) |
| P value | 0.007 | 0.020 | 0.23 | 0.07 | 0.15 | 0.84 | 0.10 | 0.94 |
| OR 95% CI |
1.67
(1.15–2.43) |
0.61
(0.41–0.93) |
0.77 (0.50–1.18) |
0.65 (0.41–1.03) |
0.66 (0.37–1.16) |
0.96 (0.66–1.41) |
2.23 (0.85–5.86) |
0.96 (0.35–2.63) |
Association between random dysplasia and degree of inflammation
Random biopsies were obtained in 924 cases, with 23 LGD, 2 HGD, and 18 IND cases with an overall yield of random dysplasia in 2.7% and random IND in 1.9% of cases. A logistic regression model was fit on procedure level data to assess the association between random LGD, HGD, and IND and degree of inflammation. The odds of detecting random LGD or HGD significantly increased as the degree of endoscopic inflammation increased (OR 2.18, 95%CI 1.46–3.26; P <0.001) and as the degree of histologic inflammation increased (OR 2.75; 95%CI 1.65–4.57, P <0.001). The odds of detecting IND also significantly increased as the degree of endoscopic increased (OR 2.90; 95%CI 1.85–4.55, P <0.001) and the degree of histologic inflammation increased (OR 1.98; 95%CI 1.08–3.62, P <0.035) ( Table 3 ).
Table 3 Association between dysplasia (both visible and random) with degree of inflammation (both endoscopic and histologic).
| Visible dysplasia | Random dysplasia | ||||
| Explanatory Variable and Effect |
Non-dysplastic
(N = 1172) |
Dysplastic
(N = 411) |
Non-dysplastic
(N = 911) |
Dysplastic LGD/HGD
(N = 25) |
Indefinite dysplasia
(N = 18) |
| LGD, low-grade dysplasia; HGD, high-grade dysplasia. | |||||
| Degree of endoscopic inflammation | |||||
| Inactive | 758 (65.6%) | 273 (67.4%) | 575 (64%) | 10 (41.7%) | 3 (16.7%) |
| Mild | 269 (23.3%) | 92 (22.7%) | 227 (25.3%) | 5 (20.8%) | 7 (38.9%) |
| Moderate | 97 (8.4%) | 32 (7.9%) | 76 (8.5%) | 5 (20.8%) | 5 (27.8%) |
| Severe | 32 (2.8%) | 8 (2.0%) | 20 (2.2%) | 4 (16.7%) | 3 (16.7%) |
| OR (95% CI) | 0.94 (0.80–1.09) | Reference | 2.18 (1.46–3.26) | 2.90 (1.85–4.55) | |
| P value | 0.39 | < 0.001 | < 0.001 | ||
| Degree of histologic inflammation | |||||
| Inactive | 712 (62.1%) | 252 (62.8%) | 551 (61.2%) | 5 (20.8%) | 3 (16.7%) |
| Mild | 347 (30.3%) | 120 (29.9%) | 271 (30.1%) | 13 (54.2%) | 15 (83.3%) |
| Moderate | 85 (7.4%) | 29 (7.2%) | 75 (8.30%) | 6 (25.0%) | 0 (0%) |
| Severe | 3 (0.3%) | 0 (0.0%) | 3 (0.3%) | 0 (0.0%) | 0 (0%) |
| OR (95% CI) | 0.96 (0.81–1.15) | Reference | 2.75 (1.65–4.57) | 1.98 (1.08–3.62) | |
| P value | 0.70 | < 0.001 | 0.035 | ||
Patients with IND in random biopsies were significantly younger than those with no dysplasia (44 versus 55 years old, P <0.001), and had a shorter disease duration (8 vs 13 years, P =0.04). These findings were not significant for random LGD or HGD. PSC was significantly associated with IND in random biopsies (62% for PSC versus 20% for no PSC, P =0.001).
Association between random dysplasia and lesion histology:
The odds of finding dysplasia in random biopsies increased when there was presence of a synchronous TVA (OR 1.56; 95%CI 1.80–1.35; P =0.013). In four cases of TVA and synchronous random dysplasia, all cases had random LGD, and one case had multifocal LGD. Random dysplasia was found in the same colon segment as TVA only in one case (ascending colon). Importantly, the odds of finding random dysplasia did not increase when other visible lesions—including SECs and inflammatory pseudopolyps – were present ( Table 4 ).
Table 4 Association between random dysplasia and polyp type.
| Polyp type | Random low- or high-grade dysplasia | |||
| Yes | No | P value | Odds ratio (95% CI) | |
| CI, confidence interval. | ||||
| Inflammatory pseudopolyp | 4 (15.4%) | 329 (21.8%) | 0.53 | 0.59 (0.11–3.09) |
| Hyperplastic polyp | 5 (19.2%) | 270 (17.9%) | 0.72 | 0.74 (0.14–3.87) |
| Sessile serrated adenomas | 3 (11.5%) | 150 (10.0%) | 0.53 | 0.53 (0.07–3.83) |
| Serrated changes | 1 (3.8%) | 65 (4.3%) | 0.85 | 1.22 (0.17–8.88) |
| Tubulovillous adenomas | 4 (15.4%) | 6 (0.4%) | 0.013 |
1.57
(1.80 – 1.34) |
| Adenocarcinoma | 1 (3.8%) | 10 (0.7%) | 0.28 | 3.89 (0.32–4.69) |
Concordance between endoscopic and histologic degree of inflammation
In 941 surveillance colonoscopies in 721 patients, endoscopic scoring overestimated the frequency of inactive disease (63%) when compared with histologic scoring (59%). Similarly, the frequency of severe inflammation was higher in endoscopy (3%) than in histology (0.3%) while the frequency of mild inflammation was higher in histology than in endoscopy (32% vs 25%, respectively), with a P <0.001 for marginal homogeneity between endoscopic and histologic inflammation scoring. Moderate inflammation was comparable for both endoscopy and histology scores. The overall Kappa agreement between histologic and endoscopic degree of inflammation was low at 0.4 ( Table 5 ).
Table 5 Crosstabulation of concordance between endoscopic and histologic inflammation scoring.
| Histo | Inactive | Mild | Moderate | Severe | Total endoscopic |
| Endo | |||||
| Inactive | 471 | 113 | 7 | 0 | 591 |
| Mild | 82 | 131 | 25 | 1 | 239 |
| Moderate | 5 | 47 | 32 | 0 | 84 |
| Severe | 0 | 8 | 17 | 2 | 27 |
| Total histologic | 558 | 299 | 81 | 3 | 941 |
Discussion
Chronic colonic inflammation plays a fundamental role in the pathogenesis of colitis-associated neoplasia with DNA damage via oxidative stress, activation of procarcinogenic molecules, and silencing of tumor suppressor genes 1 . The Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE) II endorses EH as a long-term treatment target whereas histologic remission is not a treatment target in either CD or UC but could be used as an adjunct to EH to represent a deeper level of healing 24 . Also, persistent histologic inflammation has been linked to the development of CRC in several studies. 19 21 23 27
Surveillance colonoscopy is best performed when patients have achieved disease remission to decrease the chances of labeling reactive changes as dysplasia 28 . Our study findings indicate a clear correlation between higher degree of colonic inflammation at the time of surveillance and increased odds of finding not only low- and high-grade random dysplasia but also random IND. In our study, approximately 37% of patients undergoing surveillance had some degree of endoscopic activity and 41% had some degree of histologic activity. Similarly, multiple studies have shown that up to 30% to 40% of patients in clinical remission undergoing surveillance colonoscopy have some degree of endoscopic and histologic inflammation 29 30 .
In STRIDE-II, histologic remission remains an “aspirational” target with many challenges to be addressed before it can become a formal treatment target, particularly the heterogeneity of histologic scoring systems among practices and the interobserver and intra-observer variability among pathologists when grading both inflammation and dysplasia. None of the currently available histologic scoring systems for inflammation have been developed or validated in conjunction with endoscopic assessment of disease activity. Our study confirms that the agreement between endoscopic and histologic inflammation is low (Kappa 0.4). This is important as we design clinical trials and measure efficacy of therapeutics to achieve long-term healing.
In the present study, among 591 cases where endoscopists declared inactive disease, pathologists still identified mild inflammation in 113 cases and moderate inflammation in seven cases, underscoring the difficulty of detecting persistent histologic inflammation with endoscopy. The variability is even more remarkable in the 27 cases in which the endoscopist reported severe activity, of which only three were reported as severe on histology, whereas 17 were reported as moderate and eight as mild, indicating that histology likely underestimates the degree of activity in severe cases or perhaps endoscopists tend to overestimate the degree of inflammation, compared with histology. In a recent study, Maeda and colleagues developed and evaluated an artificial intelligence system to predict persistent histologic inflammation using endocytoscopy with 91% accuracy 31 . Gui et al recently developed the Paddington International virtual ChromoendoScopy ScOre (PICaSSO) Histologic Remission Index (PHRI) in conjunction with a deep learning strategy that strongly correlates with endoscopic scores and clinical outcomes 32 . Several technologies are expected to be developed in the next decade to tackle endo-histologic remission as a therapeutic target.
To our knowledge, this is the first study investigating the association between degree of colonic inflammation and dysplastic potential of visible colorectal lesions as well as coexistent random dysplasia. As expected, inflammatory pseudopolyps were found to be associated with higher degrees of endoscopic and histologic inflammation but did not entail higher odds of concomitant dysplasia in random biopsies. Similarly, in a retrospective analysis from two large surveillance cohorts, pseudopolyps were associated with greater severity and extent of colon inflammation and higher rates of colectomy but were not associated with development of any degree of colorectal neoplasia 33 . In our study, TVAs with LGD were associated with a higher degree of endoscopic inflammation as well as with higher odds of finding concomitant dysplasia in random biopsies. It is important to note that presence of dysplasia in random biopsies was not increased when other visible colorectal lesions such as SECs, SSAs, or TVAs were found. This is particularly important for SECs given that their dysplastic potential and association with higher rates of CRC in patients with IBD is conflicting with some studies suggesting higher rates of dysplasia/neoplasia when SECs are identified but mostly underpowered to demonstrate a clear association 9 34 . Lastly, we found a negative association between degree of histologic inflammation and the odds of finding hyperplastic polyps (HPs). This is likely because HP visualization may be obscured in a background of inflamed mucosa – the higher the degree of inflammation, the lower the probability of visualizing and resecting HPs.
This study has some limitations. First, the cross-sectional nature allows us to investigate the relationships between inflammation, dysplasia, and colorectal lesions only at one given point in time; therefore, more studies looking at the longitudinal relationship and cumulative effect between these variables are warranted. Second, the assignment of endoscopic degree of inflammation did not follow rigorous scoring systems, with most endoscopists grading inflammation either by MES in UC cases or by simply assigning the words “inactive, mild, moderate or severe.” The SES-CD score was rarely used and mainly by those endoscopists with IBD expertise. Although this is a limitation, it also likely reflects routine clinical practice in most centers with SES-CD score mainly used for clinical trial purposes. Third, there are several histology scoring systems for inflammation used across institutions and the external reproducibility of these study results may vary depending on such scoring systems. Lastly, our tertiary care center serves a large population of CD and PSC patients; hence, the proportion of patients with Crohn’s colitis undergoing surveillance in this study is likely higher than in most centers. This study highlights the need for a simple endo-histologic score for disease activity that can be validated and implemented across centers and practices while reducing intra-observer and interobserver variability.
Conclusions
In this large cross-sectional analysis of IBD surveillance colonoscopies, TVAs appear to be more prevalent in patients with more severe endoscopic inflammation and presence of concomitant dysplasia in random biopsies. A higher degree of both endoscopic and histologic inflammation carries higher odds of detecting LGD IBD, HGD IBD, and IND in random biopsies. Agreement between histologic and endoscopic inflammation scoring is low, highlighting the need for a simple endo-histologic score for disease activity across practices.
Funding Statement
This support was made possible by the Mayo Clinic.
Footnotes
Conflict of Interest Nayantara Coelho-Prabhu: research funding from Cook Endoscopy, Fujifilm, Alexion Pharma. The remaining authors have no conflict of interest to declare.
Supplementary Material
References
- 1.Beaugerie L, Itzkowitz SH. Cancers complicating inflammatory bowel disease. N Engl J Med. 2015;372:1441–1452. doi: 10.1056/NEJMra1403718. [DOI] [PubMed] [Google Scholar]
- 2.Alkhayyat M, Abureesh M, Gill A et al. Lower rates of colorectal cancer in patients with inflammatory bowel disease using anti-TNF therapy. Inflamm Bowel Dis. 2021;27:1052–1060. doi: 10.1093/ibd/izaa252. [DOI] [PubMed] [Google Scholar]
- 3.Kappelman MD, Farkas DK, Long MD et al. Risk of cancer in patients with inflammatory bowel diseases: a nationwide population-based cohort study with 30 years of follow-up evaluation. Clin Gastroenterol Hepatol. 2014;12:265–2730. doi: 10.1016/j.cgh.2013.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Laine L, Kaltenbach T, Barkun A et al. SCENIC international consensus statement on surveillance and management of dysplasia in inflammatory bowel disease. Gastroenterology. 2015;148:639–6.51E30. doi: 10.1053/j.gastro.2015.01.031. [DOI] [PubMed] [Google Scholar]
- 5.Lamb CA, Kennedy NA, Raine T et al. British Society of Gastroenterology consensus guidelines on the management of inflammatory bowel disease in adults. Gut. 2019;68:s1–s106. doi: 10.1136/gutjnl-2019-318484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Magro F, Gionchetti P, Eliakim R et al. Third European Evidence-based Consensus on Diagnosis and Management of Ulcerative Colitis. Part 1: Definitions, Diagnosis, Extra-intestinal Manifestations, Pregnancy, Cancer Surveillance, Surgery, and Ileo-anal Pouch Disorders. J Crohns Colitis. 2017;11:649–670. doi: 10.1093/ecco-jcc/jjx008. [DOI] [PubMed] [Google Scholar]
- 7.Murthy SK, Feuerstein JD, Nguyen GC et al. AGA Clinical Practice Update on Endoscopic Surveillance and Management of Colorectal Dysplasia in Inflammatory Bowel Diseases: Expert Review. Gastroenterology. 2021;161:1043–1.051E7. doi: 10.1053/j.gastro.2021.05.063. [DOI] [PubMed] [Google Scholar]
- 8.Rubin DT, Ananthakrishnan AN, Siegel CA et al. ACG Clinical Guideline: Ulcerative Colitis in Adults. Am J Gastroenterol. 2019;114:384–413. doi: 10.14309/ajg.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 9.Johnson DH, Khanna S, Smyrk TC et al. Detection rate and outcome of colonic serrated epithelial changes in patients with ulcerative colitis or Crohn's colitis. Aliment Pharmacol Ther. 2014;39:1408–1417. doi: 10.1007/s00535-018-1449-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brcic I, Dawson H, Gröchenig HP et al. Serrated lesions in inflammatory bowel disease: genotype-phenotype correlation. Int J Surg Pathol. 2021;29:46–53. doi: 10.1177/1066896920963798. [DOI] [PubMed] [Google Scholar]
- 11.Moussata D, Allez M, Cazals-Hatem D et al. Are random biopsies still useful for the detection of neoplasia in patients with IBD undergoing surveillance colonoscopy with chromoendoscopy? Gut. 2018;67:616–624. doi: 10.1136/gutjnl-2016-311892. [DOI] [PubMed] [Google Scholar]
- 12.Saraiva S, Rosa I, Moleiro J et al. Dysplasia surveillance in inflammatory bowel disease: a cohort study. GE Port J Gastroenterol. 2021;28:97–105. doi: 10.1159/000510728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mooiweer E, van der Meulen-de Jong AE, Ponsioen CY et al. Chromoendoscopy for surveillance in inflammatory bowel disease does not increase neoplasia detection compared with conventional colonoscopy with random biopsies: results from a large retrospective study. Am J Gastroenterol. 2015;110:1014–1021. doi: 10.1038/ajg.2015.63. [DOI] [PubMed] [Google Scholar]
- 14.Azizi S, Al-Rubaye H, Turki MAA et al. Detecting dysplasia using white light endoscopy or chromoendoscopy in ulcerative colitis patients without primary sclerosing cholangitis: A systematic review and meta-analysis. Int J Surg. 2018;52:180–188. doi: 10.1016/j.ijsu.2018.02.028. [DOI] [PubMed] [Google Scholar]
- 15.Hu AB, Burke KE, Kochar B et al. Yield of random biopsies during colonoscopies in inflammatory bowel disease patients undergoing dysplasia surveillance. Inflamm Bowel Dis. 2021;27:779–786. doi: 10.1093/ibd/izaa205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Navaneethan U, Kochhar G, Venkatesh PG et al. Random biopsies during surveillance colonoscopy increase dysplasia detection in patients with primary sclerosing cholangitis and ulcerative colitis. J Crohns Colitis. 2013;7:974–981. doi: 10.1016/j.crohns.2013.02.009. [DOI] [PubMed] [Google Scholar]
- 17.Wan J, Wang X, Zhang Y et al. Systematic review with meta-analysis: incidence and factors for progression to advanced neoplasia in inflammatory bowel disease patients with indefinite and low-grade dysplasia. Aliment Pharmacol Ther. 2022;55:632–644. doi: 10.1111/apt.16789. [DOI] [PubMed] [Google Scholar]
- 18.Watanabe T, Ajioka Y, Mitsuyama K et al. Comparison of targeted vs random biopsies for surveillance of ulcerative colitis-associated colorectal cancer. Gastroenterology. 2016;151:1122–1130. doi: 10.1053/j.gastro.2016.08.002. [DOI] [PubMed] [Google Scholar]
- 19.Choi CR, Al Bakir, I, Ding NJ et al. Cumulative burden of inflammation predicts colorectal neoplasia risk in ulcerative colitis: a large single-centre study. Gut. 2019;68:414–422. doi: 10.1136/gutjnl-2017-314190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Flores BM, O'Connor A, Moss AC. Impact of mucosal inflammation on risk of colorectal neoplasia in patients with ulcerative colitis: a systematic review and meta-analysis. Gastrointest Endosc. 2017;86:1006–1.011E11. doi: 10.1016/j.gie.2017.07.028. [DOI] [PubMed] [Google Scholar]
- 21.Gupta RB, Harpaz N, Itzkowitz Set al. Histologic inflammation is a risk factor for progression to colorectal neoplasia in ulcerative colitis: a cohort study Gastroenterology 20071331099–1105.quiz 340–341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pai RK, Jairath V, Vande Casteele N et al. The emerging role of histologic disease activity assessment in ulcerative colitis. Gastrointest Endosc. 2018;88:887–898. doi: 10.1016/j.gie.2018.08.018. [DOI] [PubMed] [Google Scholar]
- 23.Rutter M, Saunders B, Wilkinson K et al. Severity of inflammation is a risk factor for colorectal neoplasia in ulcerative colitis. Gastroenterology. 2004;126:451–459. doi: 10.1053/j.gastro.2003.11.010. [DOI] [PubMed] [Google Scholar]
- 24.Turner D, Ricciuto A, Lewis A et al. STRIDE-II: An update on the Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE) initiative of the International Organization for the Study of IBD (IOIBD): Determining therapeutic goals for treat-to-target strategies in IBD. Gastroenterology. 2021;160:1570–1583. doi: 10.1053/j.gastro.2020.12.031. [DOI] [PubMed] [Google Scholar]
- 25.Kovach AE, Moulton DE, Plummer WD et al. Correlation of endoscopic and histologic severity scores in pediatric ulcerative colitis at first presentation. Pediatr Dev Pathol. 2019;22:106–111. doi: 10.1177/1093526618803736. [DOI] [PubMed] [Google Scholar]
- 26.Lemmens B, Arijs I, Van Assche G et al. Correlation between the endoscopic and histologic score in assessing the activity of ulcerative colitis. Inflamm Bowel Dis. 2013;19:1194–1201. doi: 10.1097/MIB.0b013e318280e75f. [DOI] [PubMed] [Google Scholar]
- 27.Korelitz BI, Sultan K, Kothari M et al. Histological healing favors lower risk of colon carcinoma in extensive ulcerative colitis. World J Gastroenterol. 2014;20:4980–4986. doi: 10.3748/wjg.v20.i17.4980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eaden JA, Mayberry JF. Guidelines for screening and surveillance of asymptomatic colorectal cancer in patients with inflammatory bowel disease. Gut. 2002;51:V10–V12. doi: 10.1136/gut.51.suppl_5.v10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baars JE, Nuij VJAA, Oldenburg B et al. Majority of patients with inflammatory bowel disease in clinical remission have mucosal inflammation. inflammatory bowel diseases. 2011;18:1634–1640. doi: 10.1002/ibd.21925. [DOI] [PubMed] [Google Scholar]
- 30.Rosenberg L, Nanda KS, Zenlea T et al. Histologic markers of inflammation in patients with ulcerative colitis in clinical remission. Clin Gastroenterol Hepatol. 2013;11:991–996. doi: 10.1016/j.cgh.2013.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Maeda Y, Kudo SE, Mori Y et al. Fully automated diagnostic system with artificial intelligence using endocytoscopy to identify the presence of histologic inflammation associated with ulcerative colitis (with video) Gastrointest Endosc. 2019;89:408–415. doi: 10.1016/j.gie.2018.09.024. [DOI] [PubMed] [Google Scholar]
- 32.Gui X, Bazarova A, Del Amor R et al. PICaSSO Histologic Remission Index (PHRI) in ulcerative colitis: development of a novel simplified histological score for monitoring mucosal healing and predicting clinical outcomes and its applicability in an artificial intelligence system. Gut. 2022;71:889–898. doi: 10.1136/gutjnl-2021-326376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mahmoud R, Shah SC, Ten Hove JR et al. No association between pseudopolyps and colorectal neoplasia in patients with inflammatory bowel diseases. Gastroenterology. 2019;156:1333–1.344E6. doi: 10.1053/j.gastro.2018.11.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Parian AM, Lazarev MG. Serrated colorectal lesions in patients with inflammatory bowel disease. Gastroenterol Hepatol (NY) 2018;14:19–25. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.