Peroral pancreatoscopy (POPS) is useful for the direct visualization of intraductal lesions in the pancreatic duct 1 2 3 . However, POPS in patients with Roux-en-Y anastomosis via the papilla under balloon enteroscopy is difficult because pancreatoscopes are approximately 10 Fr in diameter and cannot pass through the forceps channel of the balloon enteroscope. We report a successful inspection of an intraductal papillary mucinous neoplasm (IPMN) using a novel slim pancreatoscope under balloon enteroscopy in a patient with Roux-en-Y gastrectomy.
A 74-year-old man had undergone total gastrectomy with Roux-en-Y for gastric cancer 4 years earlier. On referral to our facility, computed tomography and magnetic resonance imaging revealed pancreatic duct dilation and a pancreatic cyst in the tail region ( Fig. 1 ). Endoscopic ultrasonography revealed pancreatic duct dilation and a pancreatic cyst with a suspected mural nodule connected with the main pancreatic duct ( Fig. 2 ). Therefore, endoscopic retrograde cholangiopancreatography (ERCP) was performed using a short-type single-balloon enteroscope (SIF-H290; Olympus, Tokyo, Japan) with a working length of 152 cm and a working channel diameter of 3.2 mm 4 5 . Additionally, POPS was performed using a slim pancreatoscope (DRES Slim Scope; Japan Lifeline, Tokyo, Japan) with a length of 195 cm and a diameter of 2.6 mm ( Fig. 3 , Video 1 ). Endoscopic findings revealed mucus discharge from the papilla ( Fig. 4 a ). Pancreatography revealed defects in the pancreatic tail ( Fig. 4 b ). Subsequently, POPS was performed using a slim pancreatoscope. A villous, protruding lesion was observed in the tail of the pancreatic duct, whereas no lesions were observed in the head and body of the pancreatic duct ( Fig. 5 ). Finally, we diagnosed the patient with IPMN with mural nodules in the tail of the pancreatic duct.
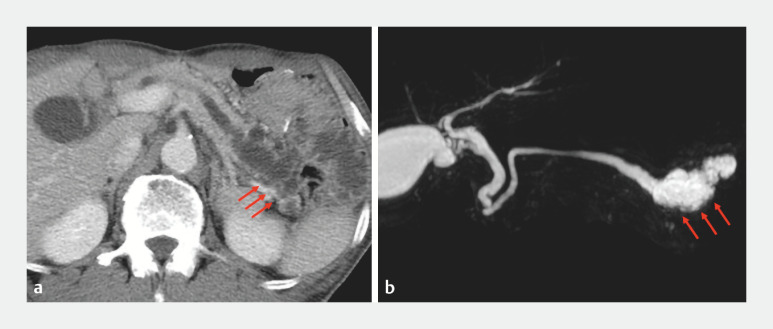
Fig. 1.
Findings revealing pancreatic duct dilation and pancreatic cyst in the tail region (red arrow). a Computed tomography. b Magnetic resonance imaging.
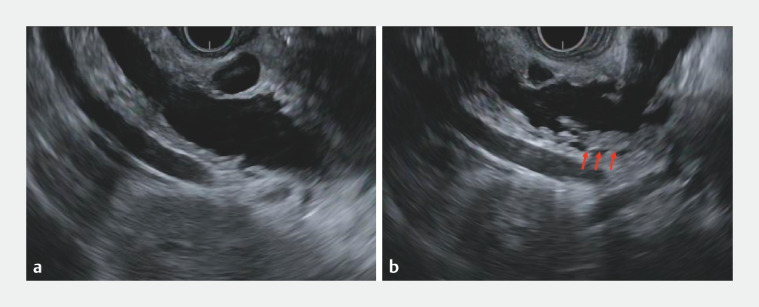
Fig. 2.
Endoscopic ultrasonography revealing pancreatic duct dilation and pancreatic cyst with a suspected mural nodule connected with the main pancreatic duct (red arrow).
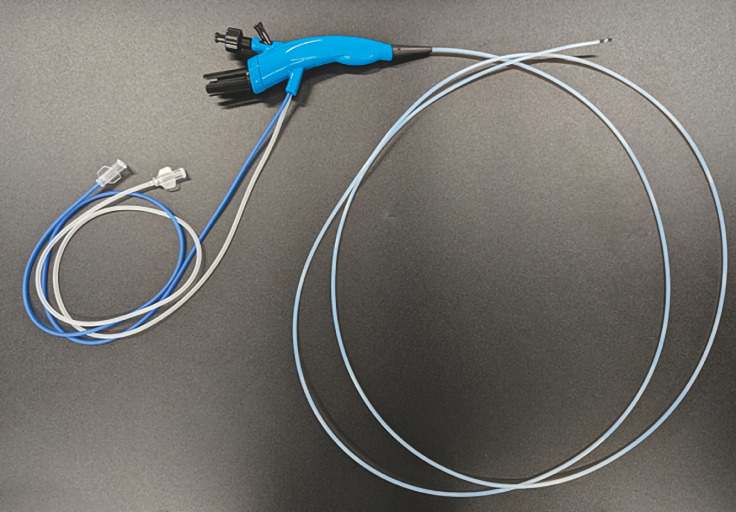
Fig. 3.
A slim pancreatoscope with a length of 195 cm and a diameter of 2.6 mm.
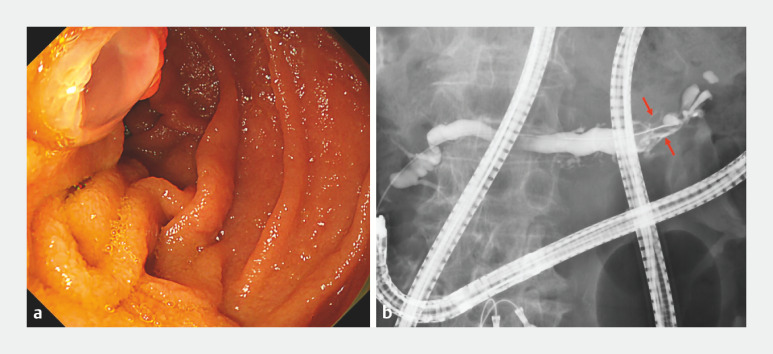
Fig. 4.
Endoscopic and pancreatography findings. a Endoscopic findings showing mucus discharge from the papilla. b Pancreatography revealing defects in the pancreatic tail (red arrow).
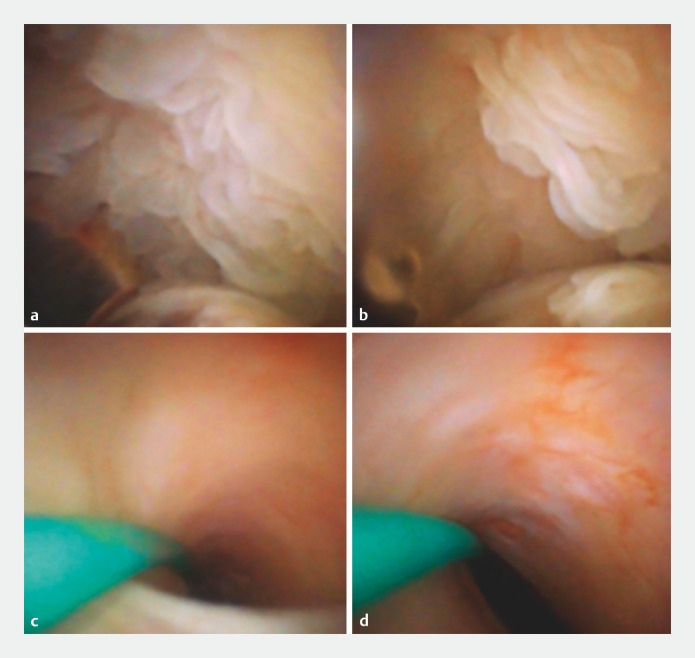
Fig. 5.
Peroral pancreatoscopy findings. a,b A villous, protruding lesion in the tail of the pancreatic duct. c No lesions were observed in the head of the pancreatic duct. d No lesions were observed in the body of the pancreatic duct.
Successful inspection of intraductal papillary mucinous neoplasm via the papilla using a novel slim pancreatoscope under balloon enteroscopy in a patient with Roux-en-Y gastrectomy.
Video 1
Although POPS via the papilla is considered difficult in patients with Roux-en-Y anastomosis under balloon enteroscopy, this novel slim pancreatoscope makes it possible, potentially improving the diagnostic yield in such patients.
Endoscopy_UCTN_Code_TTT_1AR_2AI
Acknowledgement
We would like to thank Editage (www.editage.com) for English language editing.
Footnotes
Conflict of Interest The authors declare that they have no conflict of interest.
Endoscopy E-Videos https://eref.thieme.de/e-videos .
E-Videos is an open access online section of the journal Endoscopy , reporting on interesting cases and new techniques in gastroenterological endoscopy. All papers include a high-quality video and are published with a Creative Commons CC-BY license. Endoscopy E-Videos qualify for HINARI discounts and waivers and eligibility is automatically checked during the submission process. We grant 100% waivers to articles whose corresponding authors are based in Group A countries and 50% waivers to those who are based in Group B countries as classified by Research4Life (see: https://www.research4life.org/access/eligibility/ ). This section has its own submission website at https://mc.manuscriptcentral.com/e-videos .
References
- 1.Tringali A, Lemmers A, Meves V et al. Intraductal biliopancreatic imaging: European Society of Gastrointestinal Endoscopy (ESGE) technology review. Endoscopy. 2015;47:739–753. doi: 10.1055/s-0034-1392584. [DOI] [PubMed] [Google Scholar]
- 2.Tanisaka Y, Mizuide M, Ryozawa S. Usefulness of texture and color enhancement imaging in peroral pancreatoscopy. J Hepatobiliary Pancreat Sci. 2023;30:1201–1203. doi: 10.1002/jhbp.1312. [DOI] [PubMed] [Google Scholar]
- 3.de Jong DM, Stassen PMC, Groot Koerkamp B et al. The role of pancreatoscopy in the diagnostic work-up of intraductal papillary mucinous neoplasms: a systematic review and meta-analysis. Endoscopy. 2023;55:25–35. doi: 10.1055/a-1869-0180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tanisaka Y, Ryozawa S, Mizuide M et al. Usefulness of the “newly designed” short-type single-balloon enteroscope for ERCP in patients with Roux-en-Y gastrectomy: a pilot study. Endosc Int Open. 2018;6:E1417–E1422. doi: 10.1055/a-0754-2290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tanisaka Y, Ryozawa S, Itoi T et al. Efficacy and factors affecting procedure results of short-type single-balloon enteroscopy-assisted ERCP for altered anatomy: a multicenter cohort in Japan. Gastrointest Endosc. 2022;95:310–3180. doi: 10.1016/j.gie.2021.09.008. [DOI] [PubMed] [Google Scholar]