Abstract
Introduction
Amplifying lay-rescuer response is a key priority to increase survival from out-of-hospital cardiac arrest (OHCA). We describe the current state of lay-rescuer response, how we envision the future, and the gaps, barriers, and research priorities that will amplify response to OHCA.
Methods
‘Amplifying Lay-Rescuer Response’ was one of six focus topics for the Wolf Creek XVII Conference held on June 14–17, 2023, in Ann Arbor, Michigan, USA. Conference invitees included international thought leaders and scientists in the field of cardiac arrest resuscitation from academia and industry. Participants submitted via online survey knowledge gaps, barriers to translation and research priorities for each focus topic. Expert panels used the survey results and their own perspectives and insights to create and present a preliminary unranked list for each category that was debated, revised and ranked by all attendees to identify the top 5 for each category.
Results
The top five knowledge gaps as ranked by the panel, reflected a recognition of the need to better understand the psycho-social aspects of lay response. The top five barriers to translation reflected issues at the individual, community, societal, structural, and governmental levels. The top five research priorities were focused on understanding the social/psychological and emotional barriers to action, finding the most effective/cost-effective strategies to educate lay persons and implement community life-saving interventions, evaluation of new technological solutions and how to enhance the role of dispatch working with lay-rescuers.
Conclusion
Future research in lay rescuer response should incorporate technology innovations, understand the “humanity” of the situation, leverage implementation science and systems thinking to save lives. This will require the field of resuscitation to engage with scholars outside our traditional ranks and to be open to new ways of thinking about old problems.
Keywords: sudden cardiac arrest, lay rescuer, lay response
Introduction
As we look to the future of saving more lives from out-of-hospital cardiac arrest (OHCA), the ‘chain of survival’ remains a foundational conceptual framework to guide our thinking.1 However in this future state, will all the rings in the chain of survival be equally important?2 The full spectrum of community and lay-rescuer response have in the past often been undervalued, both in terms of scientific research and research funding. Amplifying the timely response by lay persons is one area that has great potential to pay high return on investment for improving outcomes for out of hospital cardiac arrest victims.3, 4, 5, 6, 7, 8, 9, 10 The lay people available at the scene have a key role in starting cardiopulmonary resuscitation (CPR) and delivering defibrillation saving crucial time and beginning the resuscitation process before the professional response arrives.11, 12, 13, 14, 15
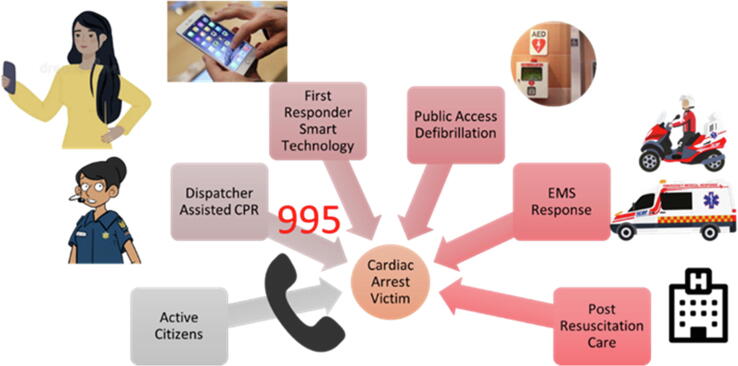
Such a timely response requires co-ordination and collaboration between active citizens, dispatcher systems, smart technology, public access defibrillation programs and integrated emergency medical systems (EMS) (Fig. 1). It also requires us to think differently about the lay-rescuer as a person and the impact of psychology and sociology of human response in an emergency. In this paper, we aim to describe the current state of lay-rescuer response, how we envision the future, and the gaps, barriers, and research priorities that will amplify this crucial level of response to OHCA.
Fig. 1.
The Key role of the Lay-Rescuer Response (illustrated using the Singapore emergency medical services system).
Methods
Since its inception in 1975, the Wolf Creek Conference has a well-established tradition of providing a unique forum for robust intellectual exchange between thought leaders and scientist from academia and industry that focuses on advancing the science and practice of cardiac arrest resuscitation.16 The Wolf Creek XVII Conference was hosted by the Max Harry Weil Institute for Critical Care Research and Innovation in Ann Arbor, Michigan, USA on June 15–17, 2023.17
Amplifying lay-rescuer response was one of 6 focus topics for the conference. Meeting invitees included international academic and industry scientists as well as thought leaders in the field of cardiac arrest resuscitation. All participants were required to complete conflict of interest disclosures. Prior to the meeting, all participants were asked via online survey to list up to three knowledge gaps, barriers to translation and research priorities for each topic. Participants were instructed that the topic of amplifying lay-rescuer response would focus on optimizing the frequency and quality of lay-rescuer response to out-of-hospital cardiac arrest. Lay-rescuers are defined as those who are not obligated to respond at the time of the arrest as part of their employment.
Knowledge gaps were defined as areas where our understanding or knowledge is incomplete or limited. These gaps can arise due to various factors, such as lack of research, inadequate information, limited access to data or resources, or simply because the topic is new or complex. Barriers to translation were defined as obstacles that can prevent the successful transfer of knowledge or innovations from research or development settings to practical applications in the real world. Research priorities were defined as the areas of study that are considered most important or urgent by the scientific community or society as a whole. These priorities are often determined by a range of factors such as knowledge gaps, scientific breakthroughs, new challenges, societal needs, or funding opportunities.
Panels made up of experts in each topic used the survey results and their own perspectives and insights to create an initial unranked list of up to ten items for each category. During the conference, expert panelists provided an overview of the current state and potential future state of the field lay the groundwork for an informed debate. This was followed by presentation and initial ranking of the knowledge gaps, barriers to translation, and research priorities by all attendees using electronic voting, discussion and revision by the panel and attendees, and then re-ranking. The complete results and rankings from all three categories are listed in Supplemental Materials. The top 5 items in each category underwent final review and discussion on the last day of the conference. An overview of the current and potential future state of the field and prioritized results for lay-rescuer response was presented by experts in this area and summarized in this manuscript.
Current state of lay-rescuer response
Basic life support (BLS) and early defibrillation by lay-rescuers have been recognized for many years as very important components of the chain of survival.18, 19 However, the majority of OHCAs occur in residential settings, i.e. private homes where lay rescuers are family members and AEDs were rarely available.20, 21 The absolute number of patients collapsing with ventricular fibrillation in residential areas is double of those in public settings. Hence, the need to develop faster response systems in residential areas has come to the forefront as a key priority area.
A review of 29 original papers22 found wide variation in the prevalence of CPR training of the public, ranging between 19% and 65% among continents. A significant correlation with Gross National Income (GNI) per capita per country and resuscitation training was also shown. Given the time, effort and cost it takes to conduct CPR training, training the entire population every 2 years remains an expensive and time- consuming undertaking.
Basic Life Support delivery in OHCA was analyzed in an analysis of 16 national and regional registries.23 Bystander CPR ranged from 19% to 79%, with a minority of registries reporting a comparison of chest compression-only (CCO) CPR vs. chest compressions combined with ventilation. CCO CPR ranged from 15% to 50% of CPR. 11 registries reported on AED use and found that AEDs were connected in 2% to 37% of OHCA, with shocks delivered in a median 1.4% of cases (range 0.5% to 7%).23 A second paper reported a standardized survey in 2017 of 28 European countries with a mean 58% of OHCA cases receiving bystander CPR (range 13% to 82%).24 Of those in which it was reported, 72% received CCO CPR.
The introduction of the smartphone has provided new opportunities for dispatch centers to activate nearby lay-rescuers to initiate BLS and in some cases find public AEDs. Valeriano et al. described the design and organization of 25 alert systems worldwide.25 This review showed that several design features have been generally adopted such as: activation by the dispatch center, Global Positioning Satellite (GPS) location of the rescuer allowing selection of rescuers in the proximity of a victim, an AED locator, instructions to go directly to the victim for BLS or collect an AED first. Interestingly, the diameter of the circle around the victim varies between 300 m. and 1800 m within the systems. All systems except one, alerted rescuers for cases in the public and at home. The majority of systems allowed registration of lay-rescuers, some requiring proof of training, and certification for (semi)-professionals. Rarely, systems offered videoconferencing with the dispatch center as an option.
Scquizzato et al. identified 12 alert systems specifically designed for citizen responders and focused on design and outcomes of the systems.26 Only four studies reported on outcomes with a reference group, either historic controls or concurrent (randomized) controls (Table 1). From the four studies, citizen responders activated by an alert system increased BLS by 10% to 15%. Most apps include the location of (and often optimal directions to) one or more AEDs in the vicinity. Three studies with a comparative group reported on the contribution of defibrillation by the citizen responder who brought an AED directed by location information from the mobile phone app (Table 2). Stieglis et al reported median time interval from call to dispatch center to the first defibrillation by EMS prior to introduction of the alert system was 12.5 minutes and by citizen responders median 9.3 minutes after introduction - a time gain of 3.2 minutes for 16% of cases where the citizen responder defibrillated first.27 Three studies reported on survival in a controlled way, allowing some insight to the contribution of alert systems (that included trained citizen responders, adding public AEDs and after introducing an alert app) to survival (Table 3). The results must be interpreted with caution, not only because of the possibility of bias, but also because all systems differed in their organization (see above). Nevertheless, the studies demonstrated that an alert system with citizen responders is feasible, and a contribution to survival can be expected.
Table 1.
Alert system studies with effect estimate of rate of bystander CPR before EMS arrival.
| Author | Study type | Year | Country | Pre-app | During app | Comment |
|---|---|---|---|---|---|---|
| Ringh36 | RCT | 2015 | Sweden | 47.8% | 61.6% | Public + residential |
| Lee37 | Before-after | 2019 | S. Korea | 54.9% | 59.8% | Public + residential |
| Andelius38 | Cohort | 2020 | Denmark | - | 76.8%# 85.3%$ |
Public + residential |
| Stieglis25 | Before-after | 2021 | Netherlands | 78% | 91% | Residential |
RCT: Randomized Clinical Trial; #EMS arrived first; $Citizen responder arrived first.
Table 2.
Studies with control observations estimating the contribution of citizen-responder to defibrillation.
| Author | Study type | Year | Country | Pre-app | During app | Comment |
|---|---|---|---|---|---|---|
| Lee37 | Before-after | 2019 | S. Korea | 0.9% | 0.6% | Public + residential |
| Andelius38 | Cohort | 2020 | Denmark | - | 0%# | Public + residential |
| 10%$ | ||||||
| Stieglis25 | Before-after | 2021 | Netherlands | 0% | 16% | Residential |
EMS arrived first;
Citizen responder arrived first.
Table 3.
Controlled studies estimating survival benefit contribution by citizen responders.
| Author | Study type | Year | Country | Pre-app | During app | Comment |
|---|---|---|---|---|---|---|
| Lee37 | Before-after | 2019 | S. Korea | 9.0% | 12.7% | Public + residential |
| Andelius38 | Cohort | 2020 | Denmark | 12.6%# | Public + residential | |
| 15.8%$ | ||||||
| Stieglis25 | Before-after | 2021 | Netherlands | 26% | 39% | Residential, VF only |
| Stieglis25 | Before-after | 2021 | Netherlands | 12% | 16% | Residential, all rhythms |
VF: Ventricular Fibrillation.
EMS arrived first;
Citizen responder arrived first.
The future of lay-rescuer response
In the near future, artificial intelligence (AI) will make coordination and integration of data sources and systems into platforms for sense-making of information and action the norm.28 The strategic use of data and technology will have an enormous multiplying effect upon the first three rings of the chain of survival - improving early access, early CPR, as well as early defibrillation. Data, when properly applied, can not only be used to initiate the chain of survival but to automate the detection of potential cardiac arrests as well.
Although technology will be a key enabler to amplify lay person response, there is a need for local advocates to develop a cardiac arrest strategy and roadmap to drive the coordinator of advancements in this area. This could include:
-
(1)
Community based efforts, supported by government, corporations, philanthropy, and socio-civic organizations, sustaining these efforts legislatively in protecting responders, providing leadership, funding for programs, and activating the community.
-
(2)
Embedding the training of laypersons in CPR/AED skills as part of a citizenship and community journey. Government, educational institutions, healthcare organizations and communities play a key role in advocating for providing training in school, community, and workplace programs.
-
(3)
Support (including mental health support)29 for first responders especially for non-healthcare professionals who may be encountering such a medical emergency for the first time in their lives.
-
(4)
A technology roadmap that can take advantage of emerging technologies which are relevant to the EMS system. Although countries have different levels of mobile technologies penetration, it continues to increase in the foreseeable future and as technological thrusts become mature, the costs and readiness for adoption will increase.
New methodologies in AI to analyze non-structured data like voice, images and videos will become increasingly affordable to support the automated detection of OHCA situations via internet of things (iOT) devices such as connected closed circuit security cameras, consumer smart speakers and smartphones.30 Increasing use of wearable devices31 will provide additional opportunities for early access to detect the onset of OHCA. More people will have access to skills training through publicly available self-service, gamified programs and mobile gaming kiosks.32 Call centers will use AI to rapidly detect OHCA, mobile apps will bring trained responders to the scene and identify AED locations within seconds, and responders will also have wearables that guide them to do high quality CPR. Smart AEDs will help responders navigate to the device, navigate responders to the victim and help guide EMS professionals towards the incident. It will also leverage AI/cloud technologies to rapidly share the data to the EMS, the receiving ED/ICU.
Further along the lines of advanced technology, using historical OHCA data will allow us to visualize heatmaps of areas with low bystander CPR rates to use for targeting community-based CPR/AED training interventions as well as public access defibrillators (PAD) installation. Speech-to-Text and Deep Learning machine learning methodologies and AI with Large Language Models (LLMs) such as may increase the accuracy of OHCA diagnosis and initiation of bystander CPR. High speed 5G mobile technology with video calls will enable dispatchers to provide more effective CPR coaching in real time. LLMs may offer promise of modeling persuasive behavioral nudges to better help the caller to initiate CPR.
On the personal side, wearables such as smart watches with accelerometers have enabled the building of CPR quality apps that can provide responders with CPR quality. The miniaturization of such technologies has also made it possible to develop credit card size accelerometers that can be used by lay responders to obtain real time guidance for better CPR quality. AEDs will continue to decrease in price and size to become ‘pocketable’ such that lay responders can potentially carry such devices as lay public safety devices. Activated citizens who download first responder apps can carry pocket AEDs to respond to life-saving alerts in their neighborhood. AED drone systems can cover rural areas to bring in AEDs within 4 mins of a 911 call. Connectivity and cloud technologies may allow dispatch centre, responder apps, PADs, EMS technologies and Health IT systems to share much more information about the single episode of care and improve the handoff between multiple persons involved in the entire chain of survival.
The future must also see us turning to the fields of psychology, sociology, and anthropology to help us understand the “humanity” of bystander CPR.33 The human brain works through two systems34 – System 1 works on intuition and instinct and is engaged 95% of the time. System 2 is rational thinking and is only engaged 5% of the time. Our current approach to bystander CPR assumes rational thinking. For real impact we need to leverage the intuition and instinct system of the brain and design training and messaging accordingly.
‘Socialization’ is the process of internalizing the norms and ideologies of a society.35 Finding ways to more consistently socialize the concept of cardiac arrest and bystander CPR could increase lay-rescuer response more than any other intervention. In fact, we may not have a CPR training problem, but rather a cardiac arrest marketing problem and the future of lay responder CPR must involve sociologic and behavioral psychology principles just the way social media and online retail marketing (Amazon, Alibaba, etc.) do very successfully right now.
Lastly, an area we have woefully undervalued in resuscitation science is the impact of cultural differences in understanding of bystander CPR and response to OHCA.36 A successful future state will see us understand how the behaviors and practices we expect of lay responders are heavily influenced by their perceptions, attitudes, beliefs, and values which in turn are built from their location, demographics, socioeconomic status, education, ideology, religion, etc.37 Understanding system level ‘best practices’, along with the psychologic and sociologic frameworks discussed above will improve lay response rates more than anything else we study in the future.
Knowledge gaps
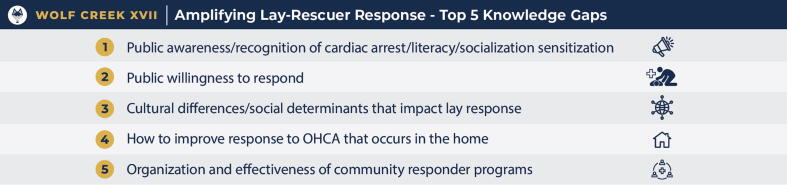
The following top 5 knowledge gaps were identified and discussed by conference participants during the Amplifying Lay-Rescuer Response Panel (Fig. 2).
-
1.
Public awareness/recognition of cardiac arrest/literacy/socialization/sensitization
Fig. 2.
Amplifying Lay-Rescuer Response: Top 5 knowledge gaps as ranked by attendees at Wolf Creek XVII, June 15–17, 2023, Ann Arbor, MI, USA.
The panel discussion highlighted that ‘health literacy’ is a key issue in all our communities, with an urgent need to understand better how to communicate and ‘market’ our messages in a positive way that will convey hope and engagement. Also, the need to make these messages personal, given that often the bystander of a cardiac arrest is not a stranger but rather someone with a relationship to the victim. Finally, the role of telephone/dispatcher-assisted CPR was also discussed and the need to optimize this critical element.
-
2.
Improving public willingness to respond
There were not many participants in the room with a deep understanding of the connection of the psychology of human motivation to public willingness in OHCA and yet, several ranked a focus on understanding how to improve public willingness as a key knowledge gap. Despite all of the science we have on the impact of early CPR on survival, bystander CPR requires a human being to make a choice under very stressful and uncertain circumstances. As noted in our future state discussion, to date we have placed almost all of our emphasis on skills training however filling this knowledge gap will require us to partner with our colleagues in the fields of psychology, sociology, and anthropology to help us understand the human ecology of willingness to respond to OHCA.
-
3.
Understanding cultural differences/social determinants that impact lay response
Many nation-states in Africa, Asia, and the Americas are increasingly culturally diverse and are 'multicultural' in a descriptive sense. An area we have woefully undervalued in resuscitation science is the impact of cultural differences in understanding of bystander CPR and response to OHCA. The high ranking of this particular knowledge gap reflects the need to understand how the behaviours and practices we expect of lay responders are heavily influenced by their cultural norms, perceptions, attitudes, beliefs and values which in turn are built from their location, demographics, socioeconomic status, education, ideology, religion, etc. A lack of understanding of cultural influences and social determinants on lay rescuer response directly impacts our ability to improve bystander CPR rates globally, improve the design and uptake of CPR training and truly understand differences in survivor and lay rescuer experience.
-
4.
Improving response to OHCA that occurs in the home
We know that approximately 70% of OHCA occurs in the home and many go unwitnessed. Speech-to-Text and Deep Learning machine learning methodologies have accelerated the application of AI in unstructured data domains such as speech related diagnostics. AI has already been shown to be consistently faster than human dispatchers and more sensitive in detecting OHCA in phone calls. With the proliferation and improvement of AI with large learning models such as ChatGPT, the ability to recognize conversation patterns may increase the accuracy of OHCA diagnosis and initiation of bystander CPR in the home setting. This kind of innovative thinking will be the basis for significant research in this area in the future.
-
5.
Organization and effectiveness of community responder programs
There was significant discussion of the opportunity for community responder programs to bolster lay-rescuer response at a systems level. However, our understanding of how best to organize such programs and assess effectiveness remains a gap. Successful models of how such community responder program will be helpful, as well as more research into how these systems can be successfully implemented.
These topics reflect many of the areas we discussed in the section on the future of lay-rescuer response including an important recognition of the need to better understand the psycho-social aspects of lay response. Interestingly, historical areas of focus such as ways to improve CPR training and optimizing telecommunicator/dispatch-assisted CPR did not rank highly as knowledge gaps, which likely reflects the participants view that we need to move to implementation research approaches in these areas rather than developing more primary evidence.
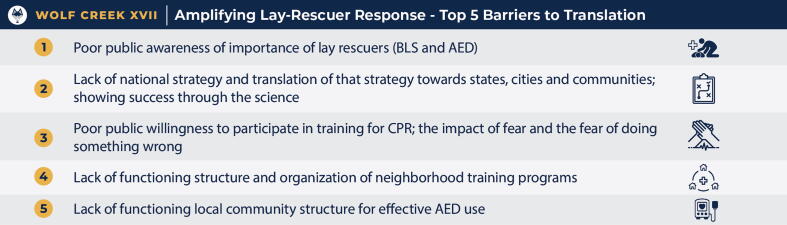
Barriers to translation
The following top 5 barriers to translation were identified and discussed by conference participants during the Amplifying Lay-Rescuer Response Panel (Fig. 3).
-
1.
Poor public awareness of importance of lay-rescuers (BLS and AED)
Fig. 3.
Amplifying Lay-Rescuer Response: Top 5 barriers to translation as ranked by attendees at Wolf Creek XVII, June 15–17, 2023, Ann Arbor, MI, USA.
Linked closely to the top-ranked knowledge gap noted above is the number one barrier to translation: poor public awareness of the importance of lay rescuers. The panel discussed that besides lack of awareness, misperception of what cardiac arrest is, that it is a medical emergency, and what can be done to address are long-standing barriers. Fear is a huge factor that affects the lay-rescuer, whether it is a fear of doing something wrong, or acting ‘unnecessarily’. It was suggested that besides messaging the science, highlighting success was important, to have something for people to rally around. Also, it was highlighted that compared to awareness about CPR, there is still a lack of understanding of the role of lay-person defibrillation.
-
2.
Lack of an evidence based national strategy and translation of that strategy towards states, cities, and communities
The group supported the principle that ‘It takes a system to save a life’. However, a major barrier remains to be a lack of understanding of the essential elements of a successful system, and how these elements can be melded into a coherent strategy at a local, regional or even national level. Sharing of best practices and successful benchmark models will be helpful. Real world studies of successful intervention bundles, as well as implementation focused research is needed in order to help systems adopt best practices.9, 38, 39, 40
-
3.
Low willingness of the public to participate in CPR training
As noted by the group, participation in CPR training by those not required by law or by job requirements, remains low. This is unfortunate, as it will help to remove the first barrier. Barriers are often local, social, cultural, financial and personal. More research into the local barriers to CPR training is needed, as well as strategies to overcome those barriers and to increase participation of the public in CPR training.
-
4.
Lack of functioning structure and organization of neighborhood training programs
Community CPR and AED training programs are often not coordinated, under-funded and lack a thorough strategy for implementation. Disparities have been highlighted, where communities that have the highest risk for OHCA have the lowest access to CPR training.41, 42, 43 Stronger leadership and coordination is needed to remove barriers at the local community, municipal, regional and national levels, as well as evidence informed strategy, policy and funding.
-
5.
Lack of local community structure for effective AED use
AEDs are often deployed in the community with good intentions but haphazardly and in an uncoordinated fashion. Deployment of AEDs may not match the actual ‘demand’ or ‘risk’, with underserved areas and communities.44, 45 Access to AEDs is also problematic, including restricted hours of access (e.g. in locked buildings or cabinets), lack of maintenance and registration. Linkage between dispatch and AED location mapping, activation of community first responders and linking them to AEDs, lack of mobile AEDs and lack of an overall AED strategy are commonly observed barriers.46
The highlighted barriers to translation reflect issues at the individual, community, societal, structural and governmental levels. Majority of the barriers to translation that ranked outside the top five were related to AED availability, cost and maintenance and lay-rescuer crowd-sourcing design and usability. These topics could use attention from the AED developers/manufacturers to inform more publicly accessible and user-friendly versions.
While we are beginning to see the evidence base for addressing many of these barriers, a focus on implementation science methods to increase uptake would be beneficial. These barriers are not only challenging in terms of moving evidence to action but are also highly variable across different communities and countries, which makes spread and scale of best practices challenging.
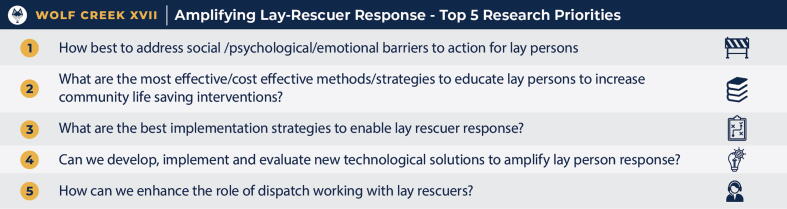
Research priorities
The following top 5 research priorities were identified and discussed by conference participants during the Amplifying Lay-Rescuer Response Panel (Fig. 4).
-
1.
How best to address social/psychological/emotional barriers to action for lay person?
Fig. 4.
Amplifying Lay-Rescuer Response: Top 5 research priorities as ranked by attendees at Wolf Creek XVII, June 15–17, 2023, Ann Arbor, MI, USA.
The top ranked research priority was: How best to address social/psychological/emotional barriers to action for lay person? The conference recognized that while the science behind CPR is well developed, there are still significant barriers for lay persons to perform bystanders. These barriers have large social and cultural components and will require contextual and local research that is both qualitative and quantitative. A better understanding of these social, psychological and emotional barriers to action will help inform creative and well-designed interventions and strategies to increase the likelihood of lay person activation during a cardiac arrest.
-
2.
Most effective/cost effective methods/strategies to educate lay persons to increase community life saving interventions
The second ranked research priority highlighted the need for evidence of the most effective/cost effective strategies to educate lay persons about life saving interventions. While the importance of lay person training is undisputed, the challenge is how to scale up high quality training to encompass large proportions of the population such that they are able to respond effectively in an emergency. To give a global perspective to this problem, we need to consider not just high-income, westernized settings, but also low-middle income countries with different value systems, where the majority of the world’s population lives. The use of technology and virtual training has an urgent need to be validated through robust research regarding its effectiveness.
-
3.
Identify the best implementation strategies to enable lay-rescuer response
Thirdly, the importance of implementation science and its role to identify the best implementation strategies to enable lay-rescuer response was ranked highly. While many creative and innovative strategies are being piloted in various EMS systems and communities, there is an urgent need to apply rigorous science to design and evaluate the full view of their implementation, to ensure that they are scalable and can be successfully replicated beyond the local settings.
-
4.
Develop, implement, and evaluate new technological solutions to amplify lay person response
The potential role of technology as an enabler has been elaborated in our ‘Future’ section above. The success of ridesharing mobile apps such as Uber have paved the way for crowdsourcing applications such as GoodSam, PulsePoint, myResponder app in Singapore, the HeartbeatNow system in the Netherlands or the Heartrunner app in Denmark have started to pave the way for citizens who are geographically nearby to an OHCA case to receive a notification from the emergency calls centre when OHCA is identified by the call taker. This has led to increased applications of CPR, earlier arrival of responders, additional manpower and increased usage of public access defibrillators (PAD) by bystanders. However robust research will be needed on the implementation and evaluation of such technologies, with an emphasis on scalability and sustainability. Developing lighter, smaller, smarter and more affordable AEDs is also much needed.47
-
5.
How to enhance the role of dispatch working with lay-rescuers
The fifth research priority focuses on the role of dispatch working with lay-rescuers. It was noted that currently few researchers have access to dispatch center data and the collaboration between dispatch/control room staff and researchers will be a key enabler for future improvements. In particular, video-CPR was noted to be an area of huge potential, as well as implementing training for dispatchers in vocal skills and effective coaching methods for dispatch-assisted CPR. Research on AI technology and large learning models may offer increasing promise of modeling persuasive behavioral nudges through the analysis and modeling of successful dispatcher conversations to learn how to psychologically influence the caller to initiate the performance of hands-only CPR.
Other priorities that were ranked outside the top five included addressing global and local inequities in resuscitation outcomes, improving lay person CPR quality, developing legal frameworks to empower lay persons, smaller/lighter/smarter AEDs and addressing the psychological impact on lay-rescuers who attend to (often unsuccessful) resuscitations.
Conclusion
Amplifying lay-person response is a key priority for the future of increased survival from out-of-hospital cardiac arrest. Important knowledge gaps exist and there are many barriers to translation of what we currently know. Bystander CPR requires a human being to recognize an emergency and to make a choice to respond. To date we have placed almost all of our emphasis on skills training and AED placement. However, the future should see us turning to technology, systems thinking and understand the “humanity” of the lay-rescuer response in order to make significant gains. Research with specific focus on closing the knowledge gaps and barriers to individual action, implementation and how to build systems that save lives should be prioritized. This will require the field of resuscitation science to engage with scholars outside our traditional ranks and to be open to new ways of thinking about old problems.
CRediT authorship contribution statement
Katie N. Dainty: Writing – review & editing, Writing – original draft, Supervision, Resources, Formal analysis, Data curation, Conceptualization.Yih Yng Ng: Conceptualization, Methodology, Data curation, Writing – original draft. Pin Pin Pek: Writing – original draft. Rudolph W. Koster: Writing – review & editing, Writing – original draft, Supervision, Resources, Formal analysis, Data curation, Conceptualization. Marcus Eng Hock Ong: Writing – review & editing, Writing – original draft, Supervision, Resources, Formal analysis, Data curation, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
Thank you to Lisa Coon, Megan Van Stratt, Linda Beasley and the Wolf Creek support staff at University of Michigan for their support during the Wolf Creek meeting.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.resplu.2023.100547.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Panchal A.R., et al. Part 3: Adult basic and advanced life support: 2020 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020;142:S366–S468. doi: 10.1161/CIR.0000000000000916. [DOI] [PubMed] [Google Scholar]
- 2.Deakin C.D. The chain of survival: Not all links are equal. Resuscitation. 2018;126:80–82. doi: 10.1016/j.resuscitation.2018.02.012. [DOI] [PubMed] [Google Scholar]
- 3.Song J., et al. The effect of bystander cardiopulmonary resuscitation on the survival of out-of-hospital cardiac arrests: a systematic review and meta-analysis. Scand. J. Trauma Resusc. Emerg. Med. 2018;26:86. doi: 10.1186/s13049-018-0552-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tanaka H., et al. Modifiable Factors Associated With Survival After Out-of-Hospital Cardiac Arrest in the Pan-Asian Resuscitation Outcomes Study. Ann. Emerg. Med. 2018;71:608–617.e15. doi: 10.1016/j.annemergmed.2017.07.484. [DOI] [PubMed] [Google Scholar]
- 5.Pek P.P., et al. Improved Out-of-Hospital Cardiac Arrest Survival with a Comprehensive Dispatcher-Assisted CPR Program in a Developing Emergency Care System. Prehosp. Emerg. Care. 2021;25:802–811. doi: 10.1080/10903127.2020.1846824. [DOI] [PubMed] [Google Scholar]
- 6.Sasson C., Rogers M.A.M., Dahl J., Kellermann A.L. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ. Cardiovasc. Qual. Outcomes. 2010;3:63–81. doi: 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- 7.Stiell I., et al. Health-related quality of life is better for cardiac arrest survivors who received citizen cardiopulmonary resuscitation. Circulation. 2003;108:1939–1944. doi: 10.1161/01.CIR.0000095028.95929.B0. [DOI] [PubMed] [Google Scholar]
- 8.Malta Hansen C., et al. Association of Bystander and First-Responder Efforts and Outcomes According to Sex: Results From the North Carolina HeartRescue Statewide Quality Improvement Initiative. J. Am. Heart Assoc. 2018;7 doi: 10.1161/JAHA.118.009873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Simmons K.M., McIsaac S.M., Ohle R. Impact of community-based interventions on out-of-hospital cardiac arrest outcomes: a systematic review and meta-analysis. Sci. Rep. 2023;13:10231. doi: 10.1038/s41598-023-35735-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brooks S.C., et al. Optimizing Outcomes After Out-of-Hospital Cardiac Arrest With Innovative Approaches to Public-Access Defibrillation: A Scientific Statement From the International Liaison Committee on Resuscitation. Circulation. 2022;145:e776–e801. doi: 10.1161/CIR.0000000000001013. [DOI] [PubMed] [Google Scholar]
- 11.Gregers M.C.T., et al. Association Between Number of Volunteer Responders and Interventions Before Ambulance Arrival for Cardiac Arrest. J. Am. Coll. Cardiol. 2023;81:668–680. doi: 10.1016/j.jacc.2022.11.047. [DOI] [PubMed] [Google Scholar]
- 12.Jonsson M., et al. Dispatch of Volunteer Responders to Out-of-Hospital Cardiac Arrests. J. Am. Coll. Cardiol. 2023;82:200–210. doi: 10.1016/j.jacc.2023.05.017. [DOI] [PubMed] [Google Scholar]
- 13.Scquizzato T., et al. Dispatching citizens as first responders to out-of-hospital cardiac arrests: a systematic review and meta-analysis. Eur. J. Emerg. Med. 2022;29:163–172. doi: 10.1097/MEJ.0000000000000915. [DOI] [PubMed] [Google Scholar]
- 14.Andelius L., et al. Smartphone-activated volunteer responders and bystander defibrillation for out-of-hospital cardiac arrest in private homes and public locations. Eur. Heart J. Acute Cardiovasc. Care. 2023;12:87–95. doi: 10.1093/ehjacc/zuac165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Riva G., et al. Survival in Out-of-Hospital Cardiac Arrest After Standard Cardiopulmonary Resuscitation or Chest Compressions Only Before Arrival of Emergency Medical Services. Circulation. 2019;139:2600–2609. doi: 10.1161/CIRCULATIONAHA.118.038179. [DOI] [PubMed] [Google Scholar]
- 16.Neumar R.W., Tang W. Wolf Creek XVII Part 2: The Origin, Evolution, and Impact of the Wolf Creek Conference. Resuscitation Plus. 2023 doi: 10.1016/j.resplu.2023.100505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Neumar R.W. Wolf Creek XVII Part 1: The Future of Cardiac Arrest Resuscitation. Resuscitation Plus. 2023 doi: 10.1016/j.resplu.2023.100504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Valenzuela T.D., et al. Outcomes of rapid defibrillation by security officers after cardiac arrest in casinos. N. Engl. J. Med. 2000;343:1206–1209. doi: 10.1056/NEJM200010263431701. [DOI] [PubMed] [Google Scholar]
- 19.Caffrey S.L., Willoughby P.J., Pepe P.E., Becker L.B. Public use of automated external defibrillators. N. Engl. J. Med. 2002;347:1242–1247. doi: 10.1056/NEJMoa020932. [DOI] [PubMed] [Google Scholar]
- 20.Berdowski J., et al. Impact of onsite or dispatched automated external defibrillator use on survival after out-of-hospital cardiac arrest. Circulation. 2011;124:2225–2232. doi: 10.1161/CIRCULATIONAHA.110.015545. [DOI] [PubMed] [Google Scholar]
- 21.Hansen S.M., et al. Bystander Defibrillation for Out-of-Hospital Cardiac Arrest in Public vs Residential Locations. JAMA Cardiol. 2017;2:507–514. doi: 10.1001/jamacardio.2017.0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ng T.P., et al. Global prevalence of basic life support training: A systematic review and meta-analysis. Resuscitation. 2023;186 doi: 10.1016/j.resuscitation.2023.109771. [DOI] [PubMed] [Google Scholar]
- 23.Kiguchi T., et al. Out-of-hospital cardiac arrest across the World: First report from the International Liaison Committee on Resuscitation (ILCOR) Resuscitation. 2020;152:39–49. doi: 10.1016/j.resuscitation.2020.02.044. [DOI] [PubMed] [Google Scholar]
- 24.Gräsner J.-T., et al. Survival after out-of-hospital cardiac arrest in Europe - Results of the EuReCa TWO study. Resuscitation. 2020;148:218–226. doi: 10.1016/j.resuscitation.2019.12.042. [DOI] [PubMed] [Google Scholar]
- 25.Valeriano A., Van Heer S., de Champlain F., C Brooks S. Crowdsourcing to save lives: A scoping review of bystander alert technologies for out-of-hospital cardiac arrest. Resuscitation. 2021;158:94–121. doi: 10.1016/j.resuscitation.2020.10.035. [DOI] [PubMed] [Google Scholar]
- 26.Scquizzato T., et al. Enhancing citizens response to out-of-hospital cardiac arrest: A systematic review of mobile-phone systems to alert citizens as first responders. Resuscitation. 2020;152:16–25. doi: 10.1016/j.resuscitation.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stieglis R., et al. Alert system-supported lay defibrillation and basic life-support for cardiac arrest at home. Eur. Heart J. 2022;43:1465–1474. doi: 10.1093/eurheartj/ehab802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dash S., Shakyawar S.K., Sharma M., Kaushik S. Big data in healthcare: management, analysis and future prospects. J. Big Data. 2019;6:54. [Google Scholar]
- 29.Zijlstra J.A., Beesems S.G., De Haan R.J., Koster R.W. Psychological impact on dispatched local lay rescuers performing bystander cardiopulmonary resuscitation. Resuscitation. 2015;92:115–121. doi: 10.1016/j.resuscitation.2015.04.028. [DOI] [PubMed] [Google Scholar]
- 30.Chan J., Rea T., Gollakota S., Sunshine J.E. Contactless cardiac arrest detection using smart devices. Npj Digit. Med. 2019;2:1–8. doi: 10.1038/s41746-019-0128-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chandrasekaran R., Katthula V., Moustakas E. Patterns of Use and Key Predictors for the Use of Wearable Health Care Devices by US Adults: Insights from a National Survey. J. Med. Internet Res. 2020;22 doi: 10.2196/22443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chang M.P., et al. A novel educational outreach approach to teach Hands-Only Cardiopulmonary Resuscitation to the public. Resuscitation. 2017;116:22–26. doi: 10.1016/j.resuscitation.2017.04.028. [DOI] [PubMed] [Google Scholar]
- 33.Fernald L.D. Sage Publications; 2008. Psychology: six perspectives. [Google Scholar]
- 34.Gawronski B., Creighton L.A. Oxford University Press; 2013. Dual process theories. in The Oxford handbook of social cognition 282–312. [Google Scholar]
- 35.Giddens A., Duneier M., Applebaum R. (W.W. Norton & Co.; 2007. Introduction to sociology. [Google Scholar]
- 36.The Routledge Encyclopedia of Social and Cultural Anthropology. (Routledge, 2010). doi:10.4324/9780203866474.
- 37.Hall E.T. Anchor Press; 1976. Beyond culture. [Google Scholar]
- 38.Blewer A.L., et al. Impact of bystander-focused public health interventions on cardiopulmonary resuscitation and survival: a cohort study. Lancet Public Health. 2020;5:e428–e436. doi: 10.1016/S2468-2667(20)30140-7. [DOI] [PubMed] [Google Scholar]
- 39.Tay P.J.M., et al. Effectiveness of a community based out-of-hospital cardiac arrest (OHCA) interventional bundle: Results of a pilot study. Resuscitation. 2020;146:220–228. doi: 10.1016/j.resuscitation.2019.10.015. [DOI] [PubMed] [Google Scholar]
- 40.Boland L.L., et al. Minnesota Heart Safe Communities: Are community-based initiatives increasing pre-ambulance CPR and AED use? Resuscitation. 2017;119:33–36. doi: 10.1016/j.resuscitation.2017.07.031. [DOI] [PubMed] [Google Scholar]
- 41.Blewer A.L., et al. Cardiopulmonary Resuscitation Training Disparities in the United States. J. Am. Heart Assoc. 2017;6 doi: 10.1161/JAHA.117.006124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Garcia R.A., et al. Racial and Ethnic Differences in Bystander CPR for Witnessed Cardiac Arrest. N. Engl. J. Med. 2022;387:1569–1578. doi: 10.1056/NEJMoa2200798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Anderson M.L., et al. Rates of cardiopulmonary resuscitation training in the United States. JAMA Intern. Med. 2014;174:194–201. doi: 10.1001/jamainternmed.2013.11320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dicker B., et al. Relationship between socioeconomic factors, distribution of public access defibrillators and incidence of out-of-hospital cardiac arrest. Resuscitation. 2019;138:53–58. doi: 10.1016/j.resuscitation.2019.02.022. [DOI] [PubMed] [Google Scholar]
- 45.Brown T.P., Perkins G.D., Smith C.M., Deakin C.D., Fothergill R. Are there disparities in the location of automated external defibrillators in England? Resuscitation. 2022;170:28–35. doi: 10.1016/j.resuscitation.2021.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Folke F., Shahriari P., Hansen C.M., Gregers M.C.T. Public access defibrillation: challenges and new solutions. Curr. Opin. Crit. Care. 2023;29:168–174. doi: 10.1097/MCC.0000000000001051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Todd V., et al. The First Responder Shock Trial (FIRST): Can We Improve Cardiac Arrest Survival by Providing Community Responders With Ultraportable Automated External Defibrillators? Heart Lung Circ. 2023;32:S88. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.