Abstract
Background and Objectives
Atrial fibrillation is common in patients with cardiac amyloidosis. However, the optimal anticoagulation strategy to prevent thromboembolic events in patients with cardiac amyloidosis and atrial fibrillation is unknown. This systematic review and meta-analysis compares direct oral anticoagulants (DOACs) vs. vitamin K antagonists (VKAs) in patients with cardiac amyloidosis and atrial fibrillation.
Methods
We performed a systematic literature review to identify clinical studies of anticoagulation therapies for patients with cardiac amyloidosis and atrial fibrillation. The primary outcomes of major bleeding and thrombotic events were reported using random effects risk ratios (RRs) with 95% confidence interval (CI).
Results
Our search yielded 97 potential studies and evaluated 14 full-text articles based on title and abstract. We excluded 10 studies that were review articles or did not compare anticoagulation. We included 4 studies reporting on 1,579 patients. The pooled estimates are likely underpowered due to small sample sizes. There was no difference in bleeding events for patients with cardiac amyloidosis and atrial fibrillation treated with DOACs compared to VKAs with a RR of 0.64 (95% CI, 0.38–1.10; p=0.10). There were decreased thrombotic events for patients with cardiac amyloidosis and atrial fibrillation treated with DOACs compared to VKAs with a RR of 0.50 (95% CI, 0.32–0.79; p=0.003).
Conclusions
This systematic review and meta-analysis suggests that DOACs are as safe and effective as VKAs in patients with cardiac amyloidosis and atrial fibrillation. However, more data are needed to investigate clinical differences in anticoagulation therapy in this patient population.
Keywords: Anticoagulation, Cardiac amyloidosis
INTRODUCTION
Atrial fibrillation and thromboembolic events are significant complications of cardiac amyloidosis.1,2) The frequency of atrial arrhythmias is highest in wild-type transthyretin amyloidosis (ATTRwt), followed by variant transthyretin amyloidosis, and light chain amyloidosis (AL).2) There is a high incidence of intracardiac thrombus in patients with cardiac amyloidosis and these thrombi have even been identified in patients in normal sinus rhythm.1,3) Patients with AL have been shown to have a higher rate of intracardiac thrombus compared to transthyretin amyloidosis by transesophageal echocardiography and cardiac magnetic resonance imaging.4,5) Furthermore, the congestive heart failure, hypertension, age above 75, diabetes, stroke, vascular disease, age above 65, sex (CHA2DS2-VASc) score is not reliable in patients with cardiac amyloidosis, and likely underestimates the true risk of thromboembolism.6)
Direct oral anticoagulants (DOACs) have been established as alternatives to vitamin K antagonists (VKAs) for stroke prevention in patients with atrial fibrillation.7) However, the safety and efficacy of anticoagulation therapy for stroke prophylaxis is not well studied in the cardiac amyloidosis population.
In this systematic review and meta-analysis, we examine DOACs vs. VKAs in patients with cardiac amyloidosis and atrial fibrillation. The main objective of this review was to assess the safety and efficacy of anticoagulation in patients with cardiac amyloidosis and atrial fibrillation.
METHODS
This study did not require ethical approval because only public published data were used. The reporting of this systematic review and meta-analysis follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.8) This review was submitted to PROSPERO for registration.
Search strategy
We performed a systematic literature review to identify randomized and nonrandomized clinical studies that reported clinical outcomes from anticoagulation therapy in patients with cardiac amyloidosis and atrial fibrillation. Searches were limited to peer-reviewed articles published in English up to July 9th, 2023. This search was limited to studies with human subjects and those that described the clinical impact of anticoagulation therapy on patients with cardiac amyloidosis and atrial fibrillation. We developed the search strategy according to available guidance from the Cochrane Collaboration.9)
The search strategy in PubMed explored Medical Subject Heading (MesH) terms related to anticoagulation in patients with cardiac amyloidosis and atrial fibrillation. The exact search strategy was “("anticoagulants"[Pharmacological Action] OR "anticoagulants"[MeSH Terms] OR "anticoagulants"[All Fields] OR "anticoagulant"[All Fields] OR "anticoagulate"[All Fields] OR "anticoagulated"[All Fields] OR "anticoagulating"[All Fields] OR "anticoagulation"[All Fields] OR "anticoagulations"[All Fields] OR "anticoagulative"[All Fields]) AND ("cardiacs"[All Fields] OR "heart"[MeSH Terms] OR "heart"[All Fields] OR "cardiac"[All Fields]) AND ("amyloid"[MeSH Terms] OR "amyloid"[All Fields] OR "amyloids"[All Fields] OR "amyloidal"[All Fields] OR "amyloidic"[All Fields])”. The articles found to be relevant during the search were stored in EndNote (Clarivate Analytics, London, UK). References from full-text articles were also evaluated and considered for inclusion.
Study selection
Articles were selected for inclusion based on predefined criteria, including the comparison of DOACs and VKAs in patients with cardiac amyloidosis and atrial fibrillation. The primary outcomes were major bleeding and thrombotic events. We excluded case reports and studies that did not provide patient numbers for event data.
Three authors (Lacy SC, Kinno M, and Yu MD) independently completed literature searches and screened abstracts to choose potentially relevant articles. Selected articles underwent a full evaluation to assess their potential inclusion in the systematic review.
Risk for bias
The risk of bias for non-randomized trials was evaluated using the ROBINS-I tool.10) Two independent reviewers (Lacy SC, Yu MD) assessed the risk for bias.
Endpoints
Each included study defined the primary endpoints of bleeding and thrombotic events separately. In general, major bleeding required hospitalization or blood transfusion. Thrombotic events included stroke, transient ischemic attack, or peripheral embolism.
Statistical analysis
Review Manager software 5.4 (Cochrane, London, UK) was used for data analysis. The meta-analysis outcomes were pooled using Mantel-Hansel methods due to sparse event rates. The DerSimonian and Laird approach was used for random effects model estimation of the average effect across the studies.11) Pooled estimates were presented as risk ratios (RRs) with 95% confidence intervals (CIs). A χ2 test of heterogeneity was calculated for each pooled analysis. The I2 measure of statistical heterogeneity relative to sampling error between studies was also estimated, with higher I2 values representing greater heterogeneity. All statistical tests were 2-sided and p values <0.05 were considered significant.
RESULTS
Literature search
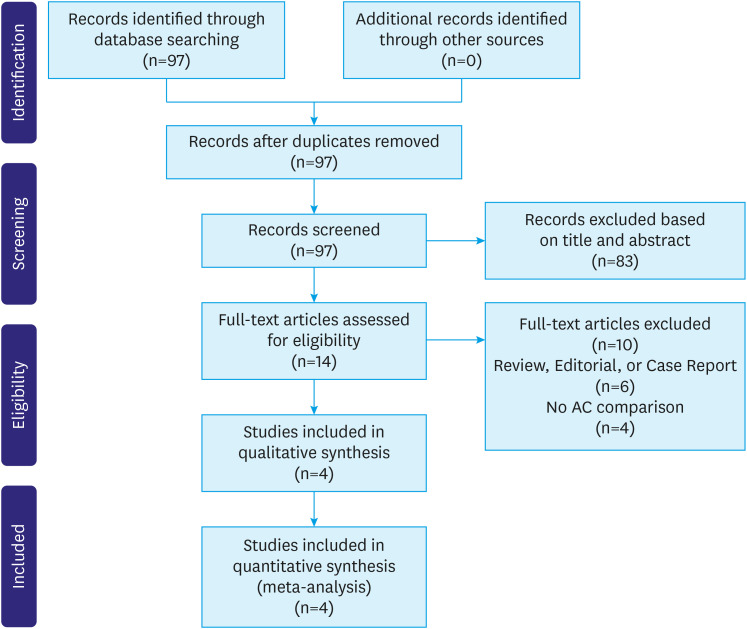
Our search yielded 97 abstracts. We excluded 83 studies at the abstract level and selected 14 full-text articles for detailed assessment. We excluded 6 studies based on case report, editorial, or review article status and 4 studies did not report anticoagulation comparison data. We ultimately included 4 studies in our systematic review and meta-analysis. Figure 1 describes the flow-chart of included studies.
Figure 1. Flow chart of the included studies.
Baseline characteristics of the studies
Table 1 shows the baseline characteristics of the included studies. All studies were published between 2020 and 2022. The 4 studies included 1,579 patients and the median age of the participants was 77.2 years interquartile range (IQR) (76.6–77.7). The median percentage of men was 85.8 IQR (70.7–88.9). The median percentage of ATTRwt was 80.0 IQR (75.3–89.4). The median percentage of hypertension was 47.0 IQR (46.2–48.3). The median percentage of diabetes mellitus was 15.6 IQR (14.3–20.1). The median percentage of prior embolism was 16.2 IQR (12.0–17.9).
Table 1. Baseline characteristics of the included studies.
| Characteristics | Study author, Year | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Mitrani et al., 202012) | Cariou et al., 202113) | Mentias et al., 202114) | Vilches et al., 202215) | ||||||
| Sample size | 194 | 273 | 551 | 561 | |||||
| Group | DOAC | VKA | DOAC | VKA | DOAC | VKA | DOAC | VKA | |
| Group size | 116 | 78 | 126 | 147 | 338 | 213 | 239 | 322 | |
| Mean/Median age (years) | 75.3±7.6 | 54.9±7.9 | 79±8 | 77±11 | 77.6±9.1 | 77.0±9.7 | 77.3 (73.1–81.7) | 77.8 (73.1–83.3) | |
| Men (%) | 88.8 | 88.5 | 83 | 73 | 63.6 | 60.6 | 90.4 | 89.1 | |
| BMI (kg/m2) | 27.1±4.2 | 26.1±3.4 | 25±4 | 25±4 | NR | NR | 26.2 (24.3–28.5) | 25.8 (23.9–28.1) | |
| ATTRwt (%) | 84 | 76 | 75 | 58 | NR | NR | 91.2 | 91.6 | |
| ATTRv (%) | 16 | 24 | 13 | 5 | NR | NR | 8.8 | 8.4 | |
| AL (%) | 0 | 0 | 12 | 37 | NR | NR | 0 | 0 | |
| Hypertension (%) | 52.6 | 48.7 | 46 | 47 | NR | NR | 43.9 | 46.9 | |
| Diabetes mellitus (%) | 15.5 | 9.0 | 13 | 16 | 32.5 | 33.8 | 15.6 | 14.7 | |
| Vascular disease (%) | NR | NR | 25 | 21 | NR | NR | 18.5 | 19.6 | |
| Prior embolism (%) | 12.1 | 20.5 | 17 | 21 | 9.1 | 11.7 | 15.9 | 16.5 | |
| CHA2DS2-VASc | 3.8±1.2 | 3.7±1.2 | 4±1 | 4±1 | 5 (4–6) | 5 (4–6) | NR | NR | |
| HAS-BLED | 2.5±0.7 | 3.1±0.9 | NR | NR | NR | NR | 2 (1–2) | 2 (1–2) | |
| eGFR (mL/min/1.73 m2) | NR | NR | 55±18 | 39±22 | NR | NR | 63.2 (51.7–75.8) | 56.8 (45.4–70.3) | |
| LVEF (%) | NR | NR | 51±12 | 46±12 | NR | NR | 47.7±12.3 | 48.7±13.6 | |
DOAC = direct oral anticoagulant; VKA = vitamin K antagonist; BMI = body mass index; ATTRwt = wild-type transthyretin amyloidosis; ATTRv = hereditary transthyretin amyloidosis; AL = light chain amyloidosis; CHA2DS2-VASc = congestive heart failure, hypertension, age above 75, diabetes, stroke, vascular disease, age above 65, sex; eGFR = estimated glomerular filtration rate; LVEF = left ventricular ejection fraction; NR = not reported.
Risk for bias
The risk for bias revealed appropriate study designs for pre-intervention, at-intervention, and post-intervention domains in the non-randomized clinical trials included in this study. Overall, the risk for bias for clinical outcomes was low.
Anticoagulation in cardiac amyloidosis
The included studies reported clinical outcomes in patients with cardiac amyloidosis and atrial fibrillation treated with anticoagulation as summarized in Table 2. Mitrani et al.12) completed a single-center retrospective analysis on anticoagulation therapy in patients with transthyretin cardiac amyloidosis (ATTR-CA) and atrial fibrillation. There was no difference in major bleeding and thrombotic events between patients treated with warfarin and DOACs. The thrombotic event rate was 3.9 per 100 person-years for patients treated with DOACs compared to 2.9 per 100 person-years for patients treated with VKAs (p=0.74) and the bleeding event rate was 5.21 per 100 person-years for patients treated with DOACs compared to 3.74 per 100 person-years for patients treated with VKAs (p=0.45) as shown in Table 3.12) Cariou et al.13) reported a single-center retrospective analysis on anticoagulation therapy in patients with cardiac amyloidosis and atrial arrhythmia. There were increased bleeding complications in patients treated with VKAs when compared to DOACs, but no difference for stroke events. This was the only included study that evaluated patients with AL and transthyretin amyloid. Subgroup analysis of patients with AL showed no difference in bleeding or stroke events between anticoagulation groups in this patient population.13) Mentias et al.14) completed a single-center retrospective analysis on anticoagulation therapy in patients with cardiac amyloidosis and atrial fibrillation. There was a decreased risk of all-cause mortality, major bleeding, and stroke in patients treated with DOACs when compared to VKAs.14) Vilches et al.15) reported a multicenter retrospective analysis on embolic events and anticoagulation therapy in patients with ATTR-CA. In ATTR-CA patients with atrial fibrillation, there was no difference in bleeding or embolic events between those treated with VKAs or DOACs. The thrombotic event rate was 1.6 per 100 patient-years for patients treated with DOACs compared to 2.0 per 100 patient-years for patients treated with VKAs and the bleeding event rate was 5.1 per 100 patient-years for patients treated with DOACs compared to 3.2 per 100 patient-years for patients treated with VKAs as shown in Table 3.15)
Table 2. Summary of study design for the included studies.
| Characteristics | Study author, Year | ||||
|---|---|---|---|---|---|
| Mitrani et al., 202012) | Cariou et al., 202113) | Mentias et al., 202114) | Vilches et al., 202215) | ||
| Location | Single-center (NY, USA) | Single-center (France) | Single-center (OH, USA) | Multicenter (4; Italy, USA, UK, Spain) | |
| Sample size | 194 | 273 | 551 | 561 | |
| Study design | Retrospective cohort | Retrospective cohort | Retrospective cohort | Retrospective cohort | |
| Study population | Transthyretin cardiac amyloidosis and atrial fibrillation | Cardiac amyloidosis and atrial arrhythmia | Cardiac amyloidosis | Transthyretin cardiac amyloidosis and atrial fibrillation | |
| Follow-up duration | 2.4 years (range 0.1–12) | 18 months (IQR 8–43) | 444 days (IQR 170–823) | 19.9 months (IQR 9.9–35.5) | |
| Primary outcome | Time to event analysis for combined outcome of stroke, TIA, major bleed, or death | All-cause and cardiovascular mortality | All-cause mortality | Incidence and prevalence of thromboembolic events | |
| Definition of major bleeding | Bleed requiring hospitalization, intracranial bleeding, or any drop in hemoglobin necessitating a transfusion | Symptomatic bleeding or bleeding causing a fall in hemoglobin level of 2 g/dL | Hospitalization associated with a code for bleeding and reported bleeding overall and by site, including gastrointestinal and intracranial | Bleeding requiring hospitalization and/or causing a decrease in hemoglobin level of 0.2 g/L and/or requiring blood transfusion | |
| Definition of thrombotic events | Stroke or TIA by combination of CT, MRI, chart review, and patient reporting | Stroke | Stroke | Stroke, TIA, or peripheral embolism | |
TIA = transient ischemic attack; CT = computed tomography; MRI = magnetic resonance imaging; IQR = interquartile range.
Table 3. Thrombotic and bleeding event rates for patients with cardiac amyloidosis and atrial fibrillation receiving anticoagulation with DOACs or VKA.
| Rates | Study | DOACs | VKA | p value |
|---|---|---|---|---|
| Thrombotic event rates | Mitrani et al., 202012) | 3.9 per 100 person years | 2.9 per 100 person years | 0.74 |
| Vilches et al., 202215) | 1.6 per 100 patient-years | 2 per 100 patient-years | NR | |
| Bleeding event rates | Mitrani et al., 202012) | 5.21 per 100 person years | 3.74 per 100 person years | 0.45 |
| Vilches et al., 202215) | 5.1 per 100 patient-years | 3.2 per 100 patient-years | NR |
DOAC = direct oral anticoagulant; VKA = vitamin K antagonist; NR = not reported.
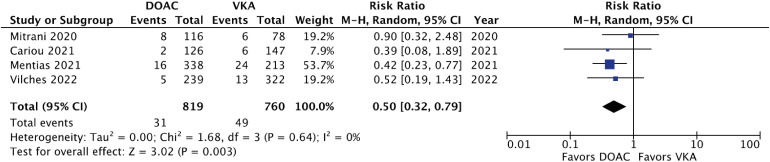
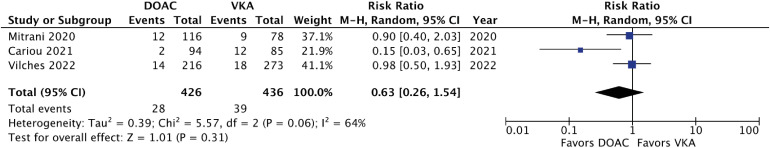
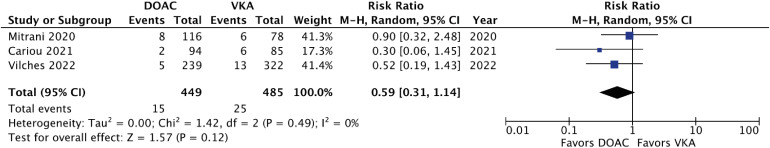
Meta-analysis of the included studies revealed a non-significant trend towards decreased bleeding events for patients with atrial fibrillation and cardiac amyloidosis treated with DOACs compared to VKAs with a RR of 0.64 (95% CI, 0.38–1.10; p=0.10). The forest plot for bleeding events is shown in Figure 2. The statistical heterogeneity was moderate for bleeding events with an I2 value of 61%. There were decreased thrombotic events for patients with atrial fibrillation and cardiac amyloidosis treated with DOACs compared to VKAs with a RR of 0.50 (95% CI, 0.32–0.79; p=0.003). The forest plot for thrombotic events is shown in Figure 3. The statistical heterogeneity was low for thrombotic events with an I2 value of 0%. Subgroup analysis for patients with ATTR-CA revealed no difference in major bleeding or thrombotic events with RRs of 0.63 (95% CI, 0.26–1.54; p=0.31) and 0.59 (95% CI, 0.31–1.14; p=0.12), respectively. The subgroup analysis forest plots for bleeding and thrombotic events are shown in Figures 4 and 5.
Figure 2. Forest plot of bleeding events for DOAC vs. VKA in cardiac amyloid patients.
DOAC = direct oral anticoagulant; VKA = vitamin K antagonist; CI = confidence interval.
Figure 3. Forest plot of thrombotic events for DOAC vs. VKA in cardiac amyloid patients.
DOAC = direct oral anticoagulant; VKA = vitamin K antagonist; CI = confidence interval.
Figure 4. Forest plot of bleeding events for DOAC vs. VKA in transthyretin cardiac amyloid patients.
DOAC = direct oral anticoagulant; VKA = vitamin K antagonist; CI = confidence interval.
Figure 5. Forest plot of thrombotic events for DOAC vs. VKA in transthyretin cardiac amyloid patients.
DOAC = direct oral anticoagulant; VKA = vitamin K antagonist; CI = confidence interval.
DISCUSSION
This is the first systematic review and meta-analysis on the safety and efficacy of anticoagulation therapy in patients with cardiac amyloidosis and atrial fibrillation. Our findings are derived from 4 studies reporting clinical outcomes in 1,579 patients with cardiac amyloidosis and atrial fibrillation. There were decreased thrombotic events and no difference in major bleeding in patients with cardiac amyloidosis treated with DOACs when compared to VKAs.
The initial landmark randomized clinical trials established the non-inferiority of DOACs compared to VKAs for anticoagulation in atrial fibrillation.16,17,18,19) Several recent meta-analyses have shown DOACs to have decreased systemic embolism, major bleeding, hemorrhagic stroke, and all-cause mortality when compared to VKAs.20,21,22) Patients with cardiac amyloidosis warrant particular consideration for DOAC anticoagulation therapy since they have an increased risk of both thromboembolism and bleeding.1,23) Our study demonstrates decreased thrombotic events and a non-significant trend towards decreased major bleeding events for DOACs when compared to VKAs in patients with cardiac amyloidosis and atrial fibrillation.
VKAs require frequent laboratory monitoring to maintain efficacy and patients treated with VKAs have been shown to only spend about 55–68% of time in therapeutic range.24) The included studies by Mitrani et al.12) and Vilches et al.15) reported 87% and 19% of patients treated with VKAs had labile international normalized ratio, respectively. Interestingly, the included study by Cariou et al.13) did show increased risk of bleeding for VKAs when compared to DOACs that was not demonstrated in our meta-analysis. The authors proposed the increased bleeding rate to be from impaired renal function, but this was not seen in the multivariate analysis. These findings suggest it may be reasonable to consider DOACs as an alternative to VKAs given the challenges of maintaining therapeutic INR in patients with cardiac amyloidosis and atrial fibrillation. Randomized clinical trials are needed to study anticoagulation therapy in patients with cardiac amyloidosis and atrial fibrillation before guideline recommendation changes can be made for this specific patient population.
The mechanism behind the increased risk of thromboembolism is related to amyloid deposition causing increased left ventricular filling pressures and resulting in left atrial enlargement and remodeling. This atrial remodeling leads to blood stasis and turbulence that predisposes to the development of intracardiac thrombi.25) Additionally, amyloid infiltration causes myocardial injury and endothelial dysfunction, which can trigger cytokines and the prothrombotic inflammatory cascade.26) AL has additional thromboembolic mechanisms compared to ATTR due to the systemic nature of the disease. In AL, nephrotic syndrome leads to urinary loss of anticoagulant factors and increased synthesis of procoagulant factors. Hyposplenism leads to thrombocytosis and there is increased blood viscosity and procoagulant activity due to circulating monoclonal proteins.25) There are multiple mechanisms for the increased risk of bleeding in cardiac amyloidosis. Perivascular amyloid deposition causes vascular fragility causing amyloid angiopathy. Advanced kidney dysfunction in amyloidosis can lead to uremia-induced platelet dysfunction. In AL, clotting abnormalities due to circulating monoclonal proteins and chemotherapy-induced bone marrow suppression contribute to bleeding risk. Dysautonomia from amyloidosis also increases fall risk in this patient population.25)
The limitations of this systematic review and meta-analysis are influenced by the limitations of the included studies. CIs for estimates were wide in spite of pooling due to low event rates in the included studies. The pooled estimates are likely underpowered and more data are needed to further investigate clinical differences between anticoagulation groups in this patient population. Variations in clinical settings, population characteristics, follow-up time, and endpoint definitions are potential sources of heterogeneity. We used a random effects model to account for these variations. All of the included studies are likely influenced by between-center variability and lack of centralized independent assessment of outcomes. The inclusion of patients with AL and ATTR-CA likely influences the generalizability of the aggregate data as outcomes vary by each subtype of cardiac amyloidosis. However, subgroup analysis of only ATTR-CA patients showed similar results to the aggregate data. The study by Vilches et al.15) is a multicenter study that included the same single-center patient population reported earlier by Mitrani et al.12) We did not have access to patient-specific data, so were unable to remove patients previously accounted for in the pooled estimates. This likely lead to double counting of some cases and introduced statistical error to our results. However, analysis with the Mitrani et al.’s study12) excluded revealed similar results.
In this systematic review and meta-analysis, there were decreased thrombotic events and no difference in major bleeding events in patients with cardiac amyloidosis and atrial fibrillation treated with DOACs when compared to VKAs. This suggests DOACs are as safe and effective as VKAs for anticoagulation therapy in this specific patient population.
ACKNOWLEDGEMENTS
The authors would like to acknowledge Dr. Amgad Mentias and Dr. Mazen Hanna from the Cleveland Clinic Foundation who shared data for inclusion in this meta-analysis.
Footnotes
Conflict of Interest: The authors have no financial conflicts of interest.
- Conceptualization: Lacy SC, Kinno M, Yu MD.
- Data curation: Lacy SC.
- Formal analysis: Lacy SC, Joyce C.
- Investigation: Lacy SC, Yu MD.
- Methodology: Lacy SC, Joyce C, Yu MD.
- Software: Lacy SC.
- Supervision: Kinno M, Joyce C, Yu MD.
- Writing - original draft: Lacy SC, Kinno M, Yu MD.
- Writing - review & editing: Lacy SC, Kinno M, Yu MD.
References
- 1.Feng D, Edwards WD, Oh JK, et al. Intracardiac thrombosis and embolism in patients with cardiac amyloidosis. Circulation. 2007;116:2420–2426. doi: 10.1161/CIRCULATIONAHA.107.697763. [DOI] [PubMed] [Google Scholar]
- 2.Giancaterino S, Urey MA, Darden D, Hsu JC. Management of arrhythmias in cardiac amyloidosis. JACC Clin Electrophysiol. 2020;6:351–361. doi: 10.1016/j.jacep.2020.01.004. [DOI] [PubMed] [Google Scholar]
- 3.Cappelli F, Tini G, Russo D, et al. Arterial thrombo-embolic events in cardiac amyloidosis: a look beyond atrial fibrillation. Amyloid. 2021;28:12–18. doi: 10.1080/13506129.2020.1798922. [DOI] [PubMed] [Google Scholar]
- 4.Feng D, Syed IS, Martinez M, et al. Intracardiac thrombosis and anticoagulation therapy in cardiac amyloidosis. Circulation. 2009;119:2490–2497. doi: 10.1161/CIRCULATIONAHA.108.785014. [DOI] [PubMed] [Google Scholar]
- 5.Martinez-Naharro A, Gonzalez-Lopez E, Corovic A, et al. High prevalence of intracardiac thrombi in cardiac amyloidosis. J Am Coll Cardiol. 2019;73:1733–1734. doi: 10.1016/j.jacc.2019.01.035. [DOI] [PubMed] [Google Scholar]
- 6.Donnellan E, Elshazly MB, Vakamudi S, et al. No association between CHADS-VASc score and left atrial appendage thrombus in patients with transthyretin amyloidosis. JACC Clin Electrophysiol. 2019;5:1473–1474. doi: 10.1016/j.jacep.2019.10.013. [DOI] [PubMed] [Google Scholar]
- 7.January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the Heart Rhythm Society in collaboration with the Society of Thoracic Surgeons. Circulation. 2019;140:e125–e151. doi: 10.1161/CIR.0000000000000665. [DOI] [PubMed] [Google Scholar]
- 8.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Higgins J, Thomas J, Chandler J, et al. Cochrane Handbook for Systematic Reviews of Interventions. Version 6.3. Chichester: John Wiley & Sons; 2022. [Google Scholar]
- 10.Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 12.Mitrani LR, De Los Santos J, Driggin E, et al. Anticoagulation with warfarin compared to novel oral anticoagulants for atrial fibrillation in adults with transthyretin cardiac amyloidosis: comparison of thromboembolic events and major bleeding. Amyloid. 2021;28:30–34. doi: 10.1080/13506129.2020.1810010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cariou E, Sanchis K, Rguez K, et al. New oral anticoagulants vs. vitamin K antagonists among patients with cardiac amyloidosis: prognostic impact. Front Cardiovasc Med. 2021;8:742428. doi: 10.3389/fcvm.2021.742428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mentias A, Alvarez P, Chaudhury P, et al. Direct oral anticoagulants in cardiac amyloidosis-associated heart failure and atrial fibrillation. Am J Cardiol. 2022;164:141–143. doi: 10.1016/j.amjcard.2021.10.018. [DOI] [PubMed] [Google Scholar]
- 15.Vilches S, Fontana M, Gonzalez-Lopez E, et al. Systemic embolism in amyloid transthyretin cardiomyopathy. Eur J Heart Fail. 2022;24:1387–1396. doi: 10.1002/ejhf.2566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365:981–992. doi: 10.1056/NEJMoa1107039. [DOI] [PubMed] [Google Scholar]
- 17.Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–1151. doi: 10.1056/NEJMoa0905561. [DOI] [PubMed] [Google Scholar]
- 18.Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365:883–891. doi: 10.1056/NEJMoa1009638. [DOI] [PubMed] [Google Scholar]
- 19.Giugliano RP, Ruff CT, Braunwald E, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369:2093–2104. doi: 10.1056/NEJMoa1310907. [DOI] [PubMed] [Google Scholar]
- 20.Dentali F, Riva N, Crowther M, Turpie AG, Lip GY, Ageno W. Efficacy and safety of the novel oral anticoagulants in atrial fibrillation: a systematic review and meta-analysis of the literature. Circulation. 2012;126:2381–2391. doi: 10.1161/CIRCULATIONAHA.112.115410. [DOI] [PubMed] [Google Scholar]
- 21.Adam SS, McDuffie JR, Ortel TL, Williams JW., Jr Comparative effectiveness of warfarin and new oral anticoagulants for the management of atrial fibrillation and venous thromboembolism: a systematic review. Ann Intern Med. 2012;157:796–807. doi: 10.7326/0003-4819-157-10-201211200-00532. [DOI] [PubMed] [Google Scholar]
- 22.Ntaios G, Papavasileiou V, Diener HC, Makaritsis K, Michel P. Nonvitamin-K-antagonist oral anticoagulants versus warfarin in patients with atrial fibrillation and previous stroke or transient ischemic attack: an updated systematic review and meta-analysis of randomized controlled trials. Int J Stroke. 2017;12:589–596. doi: 10.1177/1747493017700663. [DOI] [PubMed] [Google Scholar]
- 23.Cannistraro RJ, Meschia JF. The clinical dilemma of anticoagulation use in patients with cerebral amyloid angiopathy and atrial fibrillation. Curr Cardiol Rep. 2018;20:106. doi: 10.1007/s11886-018-1052-1. [DOI] [PubMed] [Google Scholar]
- 24.Agarwal S, Hachamovitch R, Menon V. Current trial-associated outcomes with warfarin in prevention of stroke in patients with nonvalvular atrial fibrillation: a meta-analysis. Arch Intern Med. 2012;172:623–631. doi: 10.1001/archinternmed.2012.121. [DOI] [PubMed] [Google Scholar]
- 25.Bukhari S, Khan SZ, Bashir Z. Atrial fibrillation, thromboembolic risk, and anticoagulation in cardiac amyloidosis: a review. J Card Fail. 2023;29:76–86. doi: 10.1016/j.cardfail.2022.08.008. [DOI] [PubMed] [Google Scholar]
- 26.Berghoff M, Kathpal M, Khan F, Skinner M, Falk R, Freeman R. Endothelial dysfunction precedes C-fiber abnormalities in primary (AL) amyloidosis. Ann Neurol. 2003;53:725–730. doi: 10.1002/ana.10552. [DOI] [PubMed] [Google Scholar]