Abstract
Bordetella respiratory infections are common in people (B. pertussis) and in animals (B. bronchiseptica). During the last two decades, much has been learned about the virulence determinants, pathogenesis, and immunity of Bordetella. Clinically, the full spectrum of disease due to B. pertussis infection is now understood, and infections in adolescents and adults are recognized as the reservoir for cyclic outbreaks of disease. DTaP vaccines, which are less reactogenic than DTP vaccines, are now in general use in many developed countries, and it is expected that the expansion of their use to adolescents and adults will have a significant impact on reducing pertussis and perhaps decrease the circulation of B. pertussis. Future studies should seek to determine the cause of the unique cough which is associated with Bordetella respiratory infections. It is also hoped that data gathered from molecular Bordetella research will lead to a new generation of DTaP vaccines which provide greater efficacy than is provided by today's vaccines.
INTRODUCTION
Whooping cough (pertussis) is a highly contagious, acute respiratory illness of humans that is caused by the gram-negative bacterial pathogen Bordetella pertussis (149). B. pertussis is a strict human pathogen with no known animal or environmental reservoir (174). As such, transmission of disease is postulated to occur via respiratory droplets. While nine species of Bordetella have been identified to date, only three additional members, B. bronchiseptica, B. parapertussis, and B. holmesii, have been associated with respiratory infections in humans and other mammals (174, 504). B. bronchiseptica infects a wide range of hosts and occasionally causes cough illnesses in humans; in particular, severe infections have been noted in persons who are immunocompromised such as patients with AIDS (149, 831). Human-adapted B. parapertussis (B. parapertussishu) causes a milder pertussis-like disease and, like B. pertussis, lacks an environmental reservoir (149). B. holmesii, the most recent of the Bordetella species associated with human respiratory tract infection, has been found in the blood of young adults and occasionally in the sputum (752, 814, 839). Little is known about the biology, virulence mechanisms, and pathogenic significance of B. holmesii; in contrast, B. pertussis, B. bronchiseptica, and B. parapertussis have been extensively studied.
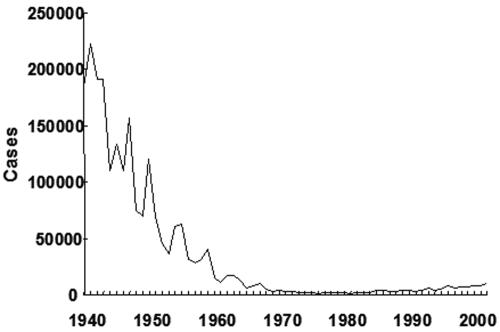
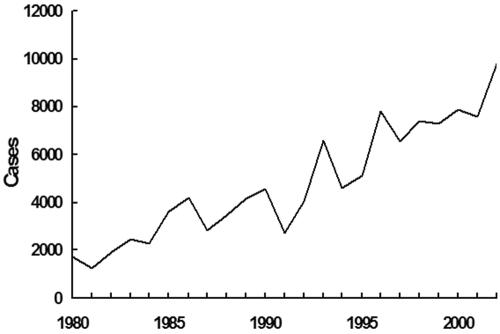
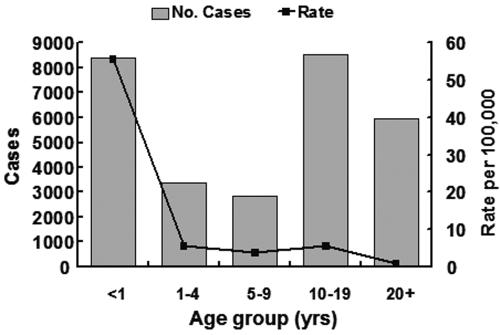
Although pertussis is relatively well controlled at present by extensive vaccination programs, it is evident that the circulation of B. pertussis throughout the world continues largely unabated (149). Whooping cough is still common in areas of the world where vaccine use is low. Recent studies suggest that there are presently ∼48.5 million yearly cases of pertussis worldwide, with as many as 295,000 deaths (187). One effect of vaccination has been a shift in the incidence of reported pertussis from children aged 1-9 years in unvaccinated populations to infants, adolescents, and adults in vaccinated populations (149). Reasons for this shift include incomplete immunity in infants who have received fewer than three doses of vaccine, the relatively short-lived immunity that results from vaccination, and the recent greater awareness of pertussis in adolescents and adults. Although adolescent and adult pertussis is significant in terms of medical costs and lost work, the most worrisome consequence is epidemiological (149, 645). Numerous studies have shown that adults and adolescents provide a reservoir of B. pertussis and are the major source of transmission to partially immunized infants and children (35, 56, 135, 149, 186, 583).
During the last 20 years, many good reviews have been written relating to the microbiology of Bordetella species and the clinical and epidemiologic aspects of pertussis (136, 147, 149, 174, 418, 504, 802). The purpose of the present review is to consolidate data from the previous literature and new information, as well as to correlate clinical events with the latest molecular evidence.
HISTORY
In contrast to other severe epidemic infectious diseases of humans (i.e., smallpox, polio, and measles), pertussis lacks an ancient history (356). Lapin stated that the first mentioning of the disease was found in Moulton's The Mirror of Health, in 1540 but he also refers to a paper by Nils Rosen von Rosenstein which suggested that the illness began in France in 1414 (442). The first epidemic was noted in Paris, France, in 1578 (162). In 1679, Sydenham named the illness pertussis (meaning violent cough).
Bordet and Gengou reported the isolation of B. pertussis in 1906, although they had observed the organism microscopically in the sputum of a patient with pertussis in 1900 (63, 356). Since pertussis was such a severe disease in infants, vaccine development began soon after the growth of the organism in the laboratory (136, 141, 147). Initially, experimental vaccines were used to treat and prevent pertussis. Epidemic pertussis was brought under control in the United States with the widespread use of whole-cell pertussis vaccines in the 1940s and 1950s. Control of the disease has continued in the United States over the last decade with the use of acellular pertussis component DTP vaccines (diphtheria-tetanus toxoids, acellular pertussis vaccine, adsorbed vaccines) (referred to as DTaP vaccines) (149).
B. bronchiseptica was first isolated during the first decade of the 20th century by Ferry, McGowan and perhaps others in studies of dogs suffering from distemper (240, 242, 243, 283, 511, 658, 761, 831). Further studies in the early 20th century demonstrated B. bronchiseptica infections in many animals and also humans (79, 241, 283, 511, 658, 689, 761, 831).
B. parapertussis was first isolated from children with pertussis in the 1930s by Eldering and Kendrick (220, 221) and Bradford and Slavin (73). Pertussis associated with B. parapertussis infections was in general somewhat less severe than that due to B. pertussis and was not associated with lymphocytosis, a hallmark of B. pertussis infection in children.
B. holmesii was presented as a new gram-negative species associated with septicemia in 1995 (814). This organism was first isolated in 1983 but was not associated with respiratory illness until 1998. During the period from 1995 through 1998, B. holmesii was recovered from nasopharyngeal specimens of 33 patients in Massachusetts with pertussis-like symptoms (508, 839).
PHYLOGENETIC RELATIONSHIPS BETWEEN BORDETELLA SUBSPECIES
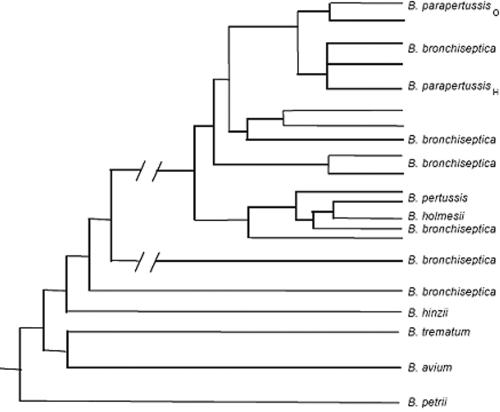
Figure 1 depicts the phylogeny of all nine known Bordetella species, namely, B. pertussis, B. bronchiseptica, B. parapertussishu, B. parapertussisov (ovine-adapted B. parapertussis), B. avium, B. hinzii, B. holmesii, B. trematum, and B. petrii. B. avium is a bird pathogen causing coryza and rhinotracheitis in poultry (263, 718). B. hinzii is found mainly as a commensal of the respiratory tracts of fowls but has pathogenic potential in immunocompromised humans (171, 404). B. trematum has been isolated from ear infections and skin wounds in humans but has never been associated with respiratory tract infections (777). B. parapertussisov causes a chronic infection of the sheep respiratory tract (631). B. petrii, the most recently identified Bordetella strain, was isolated from the environment and is capable of anaerobic growth (791, 792). It was assigned to the Bordetella genus based on comparative 16S rDNA sequence analysis, DNA base composition, isoprenoid quinone content, DNA-DNA hybridization experiments, and several metabolic properties and may represent the only Bordetella strain not known to occur in a close pathogenic, opportunistic, or commensal relationship with an animal or human host.
FIG. 1.
Phylogenetic relationships among the nine known Bordetella species based on a combination of multilocus enzyme electrophoresis, IS element, and sequence analysis. These species appear to have descended from a common B. petrii ancestor. Further, B. bronchiseptica appears to be the evolutionary progenitor of B. pertussis, B. parapertussishu, and B. parapertussisov; as such, these species have been reclassified as subspecies of the “B. bronchiseptica cluster.”
The dendrogram in Fig. 1 is based on a combination of multilocus enzyme electrophoresis, insertion sequence (IS) polymorphisms, and sequence data (including comparative 16S rDNA sequence analysis and microarray based comparative genome hybridization) analyses (189, 264, 608, 783). It confirms the close genetic relationship of all known bordetellae, with the B. pertii facultative anaerobe as the proposed environmental progenitor of pathogenic bordetellae. It further demonstrates remarkably limited genetic diversity among B. pertussis, B. parapertussis, and B. bronchiseptica strains; as such, these strains have been reclassified as “subspecies” of a single species with different host adaptations. For these subspecies, B. bronchiseptica is the likely evolutionary progenitor and B. pertussis and B. parapertussishu are considered two separate human-adapted lineages of B. bronchiseptica. B. pertussis, B. parapertussis (human and ovine), and B. bronchiseptica strains are collectively referred to as the “B. bronchiseptica cluster” (264). It must be noted that although 16S rDNA analysis and IS element polymorphisms place B. holmesii as part of the B. bronchiseptica cluster, B. holmesii does not share any characteristics of virulence protein expression with the members of the B. bronchiseptica cluster based on immunological detection with specific antisera and DNA hybridization experiments (264).
B. parapertussishu strains are particularly interesting. They comprise a single electrophoretic type and, based on PCR-based RAPD fingerprinting and IS element analyses, are nearly identical regardless of their geographic origin or year of isolation (783, 842). A plausible hypothesis is that B. parapertussishu evolved relatively recently from a closely related B. bronchiseptica strain (Fig. 1). Given its long-standing position as a host-restricted human pathogen, the isolation of strains identified as B. parapertussis from asymptomatic and pneumonic sheep came as a considerable surprise and prompted speculation that cross-species transmission may occur. Subsequent studies, however, clearly demonstrated that human and ovine strains of B. parapertussis represent distinct clonal lineages that diverged independently from B. bronchiseptica (782). B. parapertussisov isolates are genetically diverse, and there appears to be little or no transmission between the sheep and human reservoirs.
Investigators at the Sanger Center recently sequenced the genomes of three Bordetella subspecies (B. pertussis strain Tohama 1, B. parapertussishu strain 12822, and B. bronchiseptica strain RB50) (608). The genome of RB50 is 5.34 Mb, while those of Tohama 1 and 12822 are 4.09 and 4.77 Mb, respectively. The differences in genome sizes and sequence comparison of the three genomes support the hypothesis that B. pertussis and B. parapertussis recently and independently evolved from B. bronchiseptica-like ancestors. Interestingly, this restriction to the human host included significant loss of DNA, perhaps corresponding to a more “streamlined” genome. In comparison with Tohama 1 and 12822, a large portion of the extra DNA in RB50 is attributed to prophage and prophage remnants (608). Other genes lost by B. pertussis and B. parapertussis include loci involved in small-molecule metabolism, membrane transport, and biosynthesis of surface structures. In addition to this substantial gene deletion, B. pertussis and B. parapertussis contain 358 and 200 pseudogenes, respectively, many of which have been inactivated by insertion of IS elements, in-frame stop codons, or frameshift mutations. Interestingly, very few genes known or suspected to be involved in pathogenicity are missing in the genomes of human-adapted bordetellae. It is interesting that while Bordetella subspecies have been studied extensively for years, full functional data are available for only a small portion of the Bordetella genomes. For instance, genome sequence analysis predicts that at least 30 genes are involved in biosynthesis of lipopolysaccharides (LPS) for B. bronchiseptica, but functional data are available for only 13 of these genes. A detailed list of the functional annotation for predicted proteins from the sequenced Bordetella strains is presented in Table 1.
TABLE 1.
Functional annotation of predicted proteins based on genome sequence analysis of B. pertussis strain Tohama I, B. parapertussishu strain 12822 and B. bronchiseptica strain RB50
| Functional annotationa | No. of proteins with assigned COGs inb:
|
||
|---|---|---|---|
| B. pertussis (3,436) | B. parapertussishu (4,185) | B. bronchiseptica (4,994) | |
| Information storage and processing | |||
| Translation, ribosomal structure, and biogenesis | 162 | 191 | 201 |
| Transcription | 269 | 362 | 442 |
| DNA replication, recombination, and repair | 337 | 143 | 133 |
| RNA processing | 1 | 1 | |
| Chromatin structure and dynamics | 4 | 4 | 5 |
| Cellular processes | |||
| Cell division and chromosome partitioning | 30 | 30 | 35 |
| Posttranslational modification, protein turnover, chaperones | 100 | 132 | 140 |
| Cell envelope biogenesis, outer membrane | 175 | 208 | 226 |
| Cell motility and secretion | 57 | 64 | 82 |
| Inorganic ion transport and metabolism | 176 | 203 | 249 |
| Signal transduction mechanisms | 73 | 102 | 116 |
| Intracellular trafficking and secretion | 52 | 59 | 64 |
| Defense mechanisms | 25 | 31 | 41 |
| Metabolism | |||
| Energy production and conversion | 212 | 284 | 352 |
| Carbohydrate transport and metabolism | 139 | 197 | 237 |
| Amino acid transport and metabolism | 352 | 475 | 556 |
| Nucleotide transport and metabolism | 50 | 59 | 60 |
| Coenzyme metabolism | 107 | 114 | 121 |
| Lipid metabolism | 141 | 200 | 253 |
| Secondary metabolites biosynthesis, transport and catabolism | 98 | 143 | 172 |
| Poorly characterized | |||
| General function prediction only | 275 | 350 | 402 |
| Unknown function | 286 | 432 | 516 |
| Undetermined COGs | 315 | 401 | 591 |
| Total no. of proteins with assigned COGs | 3,121 | 3,784 | 4,403 |
Functional classifications are based on COG (Clusters of Orthologous Groups) categories. Additional annotated sequence information can be obtained from the Sanger Institute (http://www.sanger.ac.uk/Projects/Microbes/) and from the National Center for Biotechnology Information (http://www.ncbi.nlm.nih.gov/genomes/MICROBES/Complete.html).
Numbers of predicted proteins are given in parentheses.
VIRULENCE DETERMINANTS AND MOLECULAR PATHOGENESIS
Animal Models
B. pertussis pathogenesis has been studied mainly by using the mouse model of respiratory tract infection (90, 91, 265, 514, 778, 805). Intranasal and aerosol challenge experiments using B. pertussis and B. parapertussishu in mice have yielded important insights into the roles of specific virulence factors in determining colonization. Mouse respiratory as well as intracerebral challenge experiments have been used to determine immunity generated in response to B. pertussis infection (548, 549, 687). However, since B. pertussis and B. parapertussishu are restricted to humans, often large infectious doses are required to colonize the animals. This suggests that the above animal model systems are limited in their degree of sensitivity to accurately reflect events occurring during infection of the human host. In contrast, animal models have been developed for B. bronchiseptica that reflect both the natural course of infection and infections that are skewed towards disease (175-177, 324, 325, 506, 841). Specific-pathogen-free rabbits, rats, and mice inoculated intranasally by delivery of a 5-μl droplet of a B. bronchiseptica culture to the nares become persistently colonized in the nasal cavity, larynx, trachea, and lungs without showing any signs of clinical disease. Larynx, trachea, and lung specimens show no gross pathology, and histological examinations of tissue sections rarely show inflammation or abnormal tissue structure. A B. bronchiseptica strain, RB50, was isolated from the nose of a naturally infected New Zealand White rabbit and has been used extensively to understand mechanisms of Bordetella pathogenesis in animal models (175). Its intranasal 50% infective dose for rabbits, rats, and mice is less than 200, 25, and 5 CFU, respectively, indicating the ability of these model systems to accurately reflect the characteristics of naturally occurring infection. The availability of mice with knockout mutations in genes required for immune effector functions has allowed an investigation of interactions between Bordetella virulence factors and host defense (324, 424, 491, 621). These models are appropriate for probing mechanisms of colonization and signal transduction, since the balance is tipped towards disease in immunocompromised animals (324). Such model systems also provide an excellent opportunity to understand how bacteria establish persistent infections without causing damage to their hosts. As a result of the extremely high degree of genetic relatedness of members for the B. bronchiseptica cluster, a comparative analysis of the similarities and differences in the infectious cycles of Bordetella subspecies serves as a guide to understanding fundamental features of bacterium-host interactions.
Bordetella Virulence Regulon
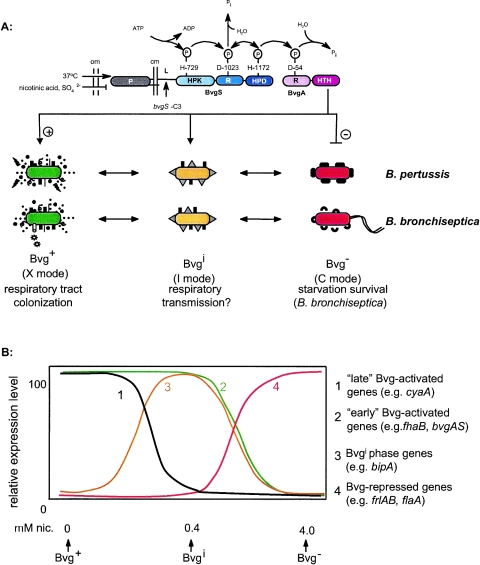
B. pertussis, B. parapertussis (human and ovine), and B. bronchiseptica share a nearly identical virulence control system encoded by the bvgAS locus. BvgA and BvgS are members of a two-component signal transduction system that uses a four-step His-Asp-His-Asp phosphotransfer signaling mechanism (Fig. 2A) (773-775). BvgA is a 23-kDa DNA-binding response regulator (70). BvgS is a 135-kDa transmembrane sensor kinase containing a periplasmic domain, a linker region (L), a transmitter (T), a receiver (R), and a histidine phosphotransfer domain (HPD) (730). BvgA and BvgS from B. pertussis and B. bronchiseptica have 100 and 96% amino acid sequence identity, respectively, and the loci are functionally interchangeable (496).
FIG. 2.
(A) The BvgAS phosphorelay. BvgS is a transmembrane sensor protein consisting of a periplasmic domain (P), a linker region (L), and histidine kinase (HPK), receiver (R), and histidine phosphotransfer domains (HPD). BvgA is a response regulator that contains receiver (R) and helix-turn-helix (HTH) domains. Under inducing signals, BvgS autophosphorylates and initiates a phosphorelay that eventually leads to the phosphorylation and activation of BvgA. The sequential steps in the phosphorelay and the amino acid residues involved are shown. The bvgS-C3 allele confers constitutive activity. BvgAS controls as least three distinct phenotypic phases in response to environmental conditions. The Bvg+ phase or X mode is necessary and sufficient for respiratory tract colonization and is associated with the expression of virulence factors. The Bvgi phase is hypothesized to be important for respiratory transmission and is characterized by the expression of a subset of Bvg+ phase-specific factors as well as factors expressed maximally in the Bvgi phase. B. pertussis and B. bronchiseptica express a significantly different array of proteins in their Bvg− phase. The Bvg− phase of B. bronchiseptica is necessary and sufficient for growth under nutrient-limiting conditions and is predicted to play a role in survival in the environment. Other abbreviations: om, outer membrane; cm, cell membrane. (B) Expression curves for the four classes of genes regulated by BvgAS. Genes expressed maximally in the Bvg+ phase (such as cyaA) are referred to as “late” Bvg-activated genes and are represented by the black curve (curve 1). Genes that are expressed maximally under both Bvg+ and Bvgi phase conditions (such as fhaB) are referred to as “early” Bvg-activated genes and are represented by the green curve (curve 2). Genes expressed maximally only under Bvgi phase conditions (such as bipA) are represented by the gold curve (curve 3). Finally, genes that are repressed by BvgAS and expressed maximally only under Bvg− phase conditions are represented by the red curve (curve 4). Abbreviation: nic, nicotinic acid.
BvgAS is environmentally responsive, although the relevant signals for regulating the bvgAS locus in vivo are yet to be determined. Over 70 years ago, Leslie and Gardner studied agglutinogenic properties of B. pertussis and described four phases (phases I, II, III, and IV) of the organism in response to varied environmental conditions (442, 454). Phases I and II were highly toxic for guinea pigs and mice, whereas phases III and IV were relatively harmless. Based on further extensive analyses, Lacey pioneered a hypothesis that Bordetella could exist in three distinct phenotypic modes, designated X, I, and C, in response to environmental signals (437). Several subsequent studies have demonstrated that in the laboratory, bvgAS expression can be activated by growth at 37°C in the relative absence of MgSO4 or nicotinic acid (527, 528). Bordetellae grown under such “nonmodulating” conditions are referred to as Bvg+-phase-specific bacteria and correspond to Lacey's X mode (Fig. 2A). Signal inputs detected by the periplasmic domain of BvgS are relayed through the membrane to the transmitter domain, which autophosphorylates at His-729 by a reaction that is reversible in vitro (544, 773-775). His-729 then donates the phosphoryl group to Asp-1023 of the receiver domain. Asp-1023 can donate the phosphoryl group to His-1172 of the HPD or to water to form inorganic phosphate. The HPD can then transfer the phosphate back to BvgS or, alternatively, can phosphorylate (and thus activate) BvgA at Asp-54. On phosphorylation by BvgS, BvgA promotes the transcription of Bvg+-phase-specific genes called vag genes (for “vir-activated genes” [bvgAS was originally termed vir]) by binding to cis-acting sequences in their promoter regions. An additional class of genes, termed vrg (for “vir-repressed genes), is repressed by the products of the bvgAS locus (7, 8, 425). The repression of these genes is mediated via a 32-kDa cytoplasmic repressor protein called BvgR (533). The gene encoding BvgR is located immediately downstream of the bvgAS locus and is also activated by BvgA (531, 532). The BvgAS phosphorelay can be inactivated by growing bordetellae under “modulating” conditions, such as at 25 or 37°C in the presence of ≥10 mM nicotinic acid or ≥40 mM MgSO4 (527). Under these Bvg− phase conditions, BvgAS is unable to activate the transcription of vag genes and repression of vrg genes. The Bvg− phase corresponds to Lacey's C mode (Fig. 2A).
The BvgS receiver is a pivotal component of the phosphorelay, acting as a biochemical checkpoint by mediating phosphorylation and dephosphorylation of the HPD and BvgA, as well as dephosphorylation of the transmitter. Mutational analyses of bvgAS have provided a number of tools for deciphering the structure of the virulence regulon and for investigating the role of Bvg-mediated signal transduction in vivo. Mutations that alter as well as those that completely abrogate signal transduction have been identified. The bvgS-C3 allele locks BvgS into an active form, rendering it insensitive to modulating signal (175, 544). Strains containing this mutation constitutively express all known Bvg-activated virulence factors. A deletion in bvgS, on the other hand, locks the bacteria in the Bvg− phase and renders them avirulent (544). The Bvg− phase of B. bronchiseptica is characterized by expression of motility and several metabolic processes involved in redox reactions and amino acid transport (8, 230, 268, 517). In contrast, B. pertussis and B. parapertussishu are nonmotile due to multiple frameshifted and transposon-disrupted genes in their flagellar loci (608). The Bvg− phase of B. pertussis is characterized by the expression of several outer membrane proteins of unknown function (287). Experiments with phase-locked and ectopic expression mutants have demonstrated that the Bvg+ phase is necessary and sufficient for respiratory tract colonization by B. pertussis and B. bronchiseptica (175, 496). These experiments also demonstrated that the Bvg− phase of B. bronchiseptica was necessary and sufficient for survival under nutrient-limiting conditions, suggesting the existence of an environmental reservoir (175). An environmental reservoir for B. pertussis and B. parapertussishu seems less plausible, as these strains are more fastidious and appear to be confined to transmission by the respiratory droplet route. A role for the Bvg− phase of these human-adapted bordetellae remains to be identified.
So, why is this BvgAS phosphorelay so complex? One possibility is that multiple steps allow multiple levels of control. The complexity of the system may also reflect the ability to respond to signal intensity in a graded manner. Indeed, it was recently demonstrated that instead of controlling a biphasic transition between the Bvg+ and Bvg− states, BvgAS controls expression of a spectrum of phenotypic phases in response to quantitative differences in environmental cues (176, 203, 204, 732). Wild-type bordetellae grown in the presence of submodulating conditions, such as concentrations of 0.4 to 2 mM nicotinic acid for B. bronchiseptica, express a phenotypic phase distinct from those described above. This phase is characterized by the absence of Bvg-repressed phenotypes, the presence of a subset of Bvg-activated virulence factors and the expression of several polypeptides that are expressed maximally or exclusively in this phase. Bordetellae growing in this phase display phenotypes intermediate between the Bvg+ and Bvg− phases; as such, this phase has been designated the Bvg-intermediate (Bvgi) phase and corresponds to Lacey's I mode (Fig. 2A) (176). A single nucleotide change in bvgS at position 733 resulting in a Thr-to-Met substitution mimics a Bvgi-phase phenotype. Bvgi phase bordetellae containing this mutation (designated bvgS-II) display increased resistance to nutrient limitation and a decreased ability to colonize the respiratory tract compared to wild-type Bvg+-phase bacteria (176). The Bvgi phase appears to be conserved between B. pertussis and B. bronchiseptica, and is predicted to play a role in the respiratory transmission of these strains (257). Recently, the Bvgi phase of B. bronchiseptica was shown to be associated with biofilm formation (383). Biofilms are bacterial communities that are attached to a solid surface and have characteristics different from free-living planktonic bacteria (173). Bacteria growing within biofilms appear to be more resistant to antibiotics and host immune defenses than are their planktonic counterparts (457). While the physiological relevance of Bvg-dependent biofilm formation in B. bronchiseptica remains to be determined, studying biofilm formation has potential implications in understanding the life-style of B. bronchiseptica (versus B. pertussis) as a chronically colonizing pathogen. Systematic analysis of gene expression in the Bvg+, Bvgi, and Bvg− phases of Bordetella reveals the existence of at least four classes of Bvg-regulated genes: (i) those that are expressed maximally only in the Bvg+ phase, (ii) those that are expressed maximally in both the Bvg+ and Bvgi phases, (iii) those that are expressed exclusively in the Bvgi phase, and (iv) those that are expressed only in the Bvg− phase (Fig. 2B). From a phylogenetic perspective, however, Bvg-regulated genes fall into two categories. Some loci are commonly expressed by B. pertussis, B. parapertussis (human and ovine), and B. bronchiseptica. Their products are highly similar and in some cases interchangeable between different subspecies. In contrast, other loci which are present in the genomes of all four subspecies appear to be differentially expressed. These genes provide important clues for understanding fundamental differences between Bordetella-host interactions.
Commonly Expressed Loci
Based on in vitro attachment assays and in vivo colonization experiments, several surface-exposed and secreted factors have been proposed to play a role in Bordetella pathogenesis (Table 2). Putative adhesins commonly expressed in the Bvg+ phase of all four subpecies of the B. bronchiseptica cluster include filamentous hemagglutinin (FHA), fimbriae (FIM), and pertactin (PRN), 1 of the 13 autotransporter proteins encoded in the Bordetella genomes: Additional autotransporters expressed by members of the B. bronchiseptica cluster include BrkA, SphB1, and Vag8. Commonly expressed Bvg+ phase toxins include a bifunctional adenylate cyclase/hemolysin (CyaA) and dermonecrotic toxin (DNT). The first identified Bvgi-phase-specific factor, BipA, also seems to be commonly expressed in B. pertussis and B. bronchiseptica and at significantly reduced levels in B. parapertussisov. Bvg−-phase-specific loci expressed in both B. pertussis and B. bronchiseptica include wlb, which is involved in LPS synthesis. In addition, commonly expressed Bvg-independent factors such as tracheal cytotoxin (TCT) play an important role in pathogenesis. Orthologous gene products display high levels of amino acid sequence identity when compared between Bordetella subspecies. For instance, the B. pertussis and B. bronchiseptica FHA, PRN, CyaA, and BipA proteins have 92, 91, 97, and 95% amino acid sequence identity, respectively (608). These factors are likely to perform similar, if not identical, functions during respiratory tract infection and polymorphisms may in some cases reflect specific host adaptations.
TABLE 2.
Expression and function information for various virulence determinants for B. pertussis and B. bronchiseptica
| Virulence determinant | Description | Gene expression
|
Protein expressiona
|
||
|---|---|---|---|---|---|
| B. pertussis | B. bronchiseptica | B. pertussis | B. bronchiseptica | ||
| Adhesins | |||||
| Filamentous hemagglutinin (FHA) | 220-kDa surface-associated and secreted protein; dominant adhesin; required for tracheal colonization; highly immunogenic; primary component of acellular pertussis vaccines | + | + | + | + |
| Fimbriae (FIM) | Filamentous cell surface structures; required for persistent tracheal colonization; component of some acellular pertussis vaccines: required for protective immunity to infection | + | + | + | + |
| Autotransporters | |||||
| Pertactin (PRN) | 68-70-kDa surface protein; mediates eukaryotic cell binding in vitro; enhances protective immunity | + | + | + | + |
| Vag8 | 95-kDa outer membrane protein | + | + | + | + |
| BrkA | 73-kDa surface-associated N-terminal passenger domain with 30-kDa outer membrane C-terminal protein; putative adhesin; confers serum resistance and protection against antimicrobial peptides in B. pertussis | + | + | + | + |
| SphB1 | Subtilisin-like Ser protease/lipoprotein required for FHA maturation in B. pertussis | + | + | + | + |
| Tracheal colonization factor (TcfA) | 60-kDa secreted protein; role in tracheal colonization in murine model | + | − | + | − |
| Toxins | |||||
| Pertussis toxin (PT) | A-B-toxin; ADP-ribosylates G proteins; responsible for pertussis-associated lymphocytosis; strong adjuvant and primary component of pertussis vaccines | + | − | + | − |
| Adenylate cyclase (CyaA) | Calmodulin-activated RTX family toxin with dual adenylate cyclase/hemolysin activity; acts as anti-inflammatory and antiphagocytic factor during infection | + | + | + | + |
| Type III secretion | Allows Bordetella to translocate effector proteins directly into host cells; required for persistent tracheal colonization; inhibits host immune response; activates ERK1/2; mislocalizes NF-κB; causes caspase-independent cell death | + | + | − | + |
| Dermonectrotic toxin (DNT) | 160-kDa heat-labile secreted toxin; activates Rho; induces necrosis in vitro | + | + | + | + |
| Tracheal cytotoxin (TCT) | Disaccharide-tetrapeptide monomeric by-product of peptidoglycan synthesis; causes mitochondrial bloating, disruption of tight junctions, damage to cilia, IL-1α and NȮ production | + | + | + | + |
| LPS | |||||
| wlb locus | Consists of 12 genes required for LPS (band A) biosynthesis | + | + | + | + |
| wbm locus | Encodes O antigen; may be important for confering serum resistance | − | + | − | + |
| PagP | Mediates palmitoylation modification of lipid A; may be important for persistence and resistance to serum killing | − | + | − | + |
| Additional loci | |||||
| Flagella | Peritrichous cell surface appendages required for motility; highly antigenic; ectopic expression of flagella in the Bvg+ phase is detrimental to the infection cycle | − | + | − | + |
| Type IV pili | Polar pili usually with an N-methylated phenylalanine as the N-terminal residue; possible functions include adherence, twitching motility, and DNA uptake | Δ | ND | NA | ND |
| Capsule | A type II polysaccharide coat predicted to be comprised of an N-acetylgalactosaminuronic acid Vi antigen-like polymer; possible role in protection against host defense mechanisms or survival in the environment | Δ | ND | ND | ND |
| Alcaligin | A siderophore for complexing iron, which is internalized through outer membrane receptors (B. bronchiseptica encodes 16 such receptors while B. pertussis encodes 12); iron uptake may be important for survival within mammalian hosts | + | + | + | + |
| Vrg loci | Several loci of uncharacterized function | + | − | + | − |
+, positive for expression; −, no expression; Δ, genome contains deletion mutations in these genes; ND, not determined; NA, not applicable.
Differentially Expressed and Differentially Regulated Loci
From an evolutionary viewpoint, differentially expressed loci are an informative class of Bvg-regulated genes. The ptx-ptl operon, which encodes the structural subunits of pertussis toxin (PT) and its export apparatus, falls into this category. The ptx-ptl locus is present in all four subspecies of the B. bronchiseptica cluster, but expression and toxin production are observed only in the Bvg+ phase of B. pertussis. Differences also exist in the LPS structures of all four subspecies (discussed in detail later in this review). A type III secretion system (TTSS), which allows gram-negative pathogens to deliver bacterial effector proteins directly into eukaryotic cells and alter host cell signaling functions, has been identified and characterized in Bordetella subspecies. Type III genes are intact and highly conserved in members of the B. bronchiseptica cluster; however, only B. bronchiseptica and B. parapertussisov readily display TTSS-associated phenotypes in vitro. Comparative sequence analysis of B. pertussis, B. parapertussishu, and B. bronchiseptica has also revealed the existence of a type IV pilin biogenesis cluster present only in B. bronchiseptica; further analysis of this recently discovered locus is pending (638). Likewise, a locus comprising three regions predicted to be involved in export/modification, biosynthesis, and transport of a type II capsule has been identified in the B. bronchiseptica genome (608). Capsules are often key contributors for enabling pathogens to survive host defense mechanisms or harsh ex vivo environments. While the central part of the capsular locus is mostly intact in B. pertussis, its 5′ end appears to have undergone massive IS element-mediated rearrangements and deletions (608). In B. parapertussishu, two genes have undergone nonsense and frameshift mutations (608). The above listed differences may contribute to determining host specificity or the nature of infection.
Although differences in Bvg+-phase phenotypes expressed by Bordetella subspecies are apparent, they exist in a background of overall similarity. In contrast, the Bvg− phases of these organisms are remarkably different. To date, there are few loci that are coexpressed in the Bvg− phases of all four subspecies (174). An interesting example involves the motility phenotype of B. bronchiseptica. Although B. pertussis and B. parapertussis contain the entire complement of motility genes, they are not expressed and these subspecies are therefore nonmotile (7, 8). In a similar vein, the B. pertussis vrg loci encode several outer membrane proteins that are specifically expressed in the Bvg− phase. The vrg genes in the B. bronchiseptica genome appear to be transcriptionally silent.
Understanding the role of Bvg-mediated signal transduction in the Bordetella life cycle is crucial in determining the pathogenic mechanisms and evolutionary trends involved in Bordetella-host interactions. It provides insightful details into the dynamics of virulence gene regulation and its implications for host adaptations.
Virulence Determinants
The virulence determinants of B. pertussis and B. bronchiseptica are discussed in Table 2.
Filamentous hemagglutinin.
The virulence determinants of B. pertussis and B. bronchiseptica are discussed in Table 2. FHA is a highly immunogenic, hairpin-shaped molecule which serves as the dominant attachment factor for Bordetella in animal model systems (174, 655). It has been included as a component in most acellular pertussis vaccines (149). Protein structure and immunological analyses suggest that the FHA proteins from B. pertussis and B. bronchiseptica are similar in their molecular mass, structure dimensions, and hemagglutination properties and have a common set of immunogenic epitopes (529, 594, 683).
FHA is encoded by fhaB, one of the strongest BvgAS-activated genes. It is maximally expressed under both Bvg+- and Bvgi-phase conditions. The fhaB promoter contains a primary high-affinity BvgA-binding site consisting of two nearly perfect inverted heptanucleotide repeats [TTTC(C/G)TA] that are centered at position −88.5 relative to the start of transcription (677). Binding of a phosphorylated BvgA dimer to this site, followed by cooperative binding of two additional Bvg∼P dimers 3′ to the high-affinity site, leads to the activation of fhaB transcription. Binding of the first BvgA∼P dimer to the primary high-affinity binding site seems to be the critical first step for fhaB transcription, since binding of the second and third dimers was found to be entirely cooperative and independent of nucleotide sequence (69, 71).
FHA is synthesized as a 367-kDa precursor, FhaB, which undergoes extensive N- and C-terminal modifications to form the mature 220-kDa FHA protein. It is exported across the cytoplasmic membrane by a Sec signal peptide-dependent pathway. Its translocation and secretion across the outer membrane requires a specific accessory protein, FhaC. FhaC folds into a transmembrane β-barrel that facilitates secretion by serving as an FHA-specific pore in the outer membrane (304, 392). FHA most probably crosses the outer membrane in an extended conformation and acquires its tertiary structure at the cell surface, following extensive N- and C-terminal proteolytic modifications which have recently been characterized in a series of elegant experiments (180, 181, 303, 304, 391-393). On translocation across the cytoplasmic membrane, the N terminus of FhaB undergoes cleavage of an additional 8 to 9 kDa at a site that corresponds to a Lep signal peptidase recognition sequence. This portion of the N terminus is predicted to be important for interacting with FhaC. Once at the cell surface, approximately 130 kDa of the C terminus of FhaB is proteolytically removed by a newly identified subtilisin-like autotransporter/protease, SphB1 (180, 181). FHA release depends on SphB1-mediated maturation. The C terminus of the FhaB precursor is predicted to serve as an intramolecular chaperone, preventing premature folding of the protein. Together, FHA and FhaC serve as prototypes for members of the two-partner secretion (TPS) system, which typically include secreted proteins with their cognate accessory proteins from several gram-negative bacteria. Although efficiently secreted via this process, a significant amount of FHA remains associated with the cell surface by an unknown mechanism.
In vitro studies using a variety of mammalian cell types suggest that FHA contains at least four separate binding domains that are involved in attachment. The Arg-Gly-Asp (RGD) triplet, situated in the middle of FHA and localized to one end of the proposed hairpin structure, stimulates adherence to monocytes/macrophages and possibly other leukocytes via the leukocyte response integrin/integrin-associated protein (LRI/IAP) complex and complement receptor type 3 (CR3) (384, 654, 690). Specifically, the RGD motif of FHA has been implicated in binding to very late antigen 5 (VLA-5; an α5β1-integrin) of bronchial epithelial cells (387). Ligation of VLA-5 by the FHA RGD domain induces activation of NF-κB, which then causes the up-regulation of epithelial intercellular adhesion molecule 1 (ICAM-1) (385, 386). ICAM-1 up-regulation is involved in leukocyte accumulation and activation at the site of bacterial infection (59, 593, 762). Interestingly, purified PT can abrogate NF-κB activation by this mechanism, suggesting the involvement of a PT-sensitive G protein in the signaling process (the role of PT is discussed in detail later in this review) (386). The CR3 recognition domain in FHA has yet to be identified. FHA also possesses a carbohydrate recognition domain (CRD), which mediates attachment to ciliated respiratory epithelial cells as well as to macrophages in vitro (636). In addition, FHA displays a lectin-like activity for heparin and other sulfated carbohydrates, which can mediate adherence to nonciliated epithelial cell lines. This heparin-binding site is distinct from the CRD and RGD sites and is required for FHA-mediated hemagglutination (530). FHA is also required for biofilm formation in B. bronchiseptica (383).
A role for FHA in vivo has been more difficult to discern mainly due to the lack of a natural animal host (other than humans) for B. pertussis, as well as the complexity of this molecule and its associated biological activities. In a rabbit model of respiratory tract infection, fewer FHA mutants compared to wild-type B. pertussis were recovered from the lungs at 24 hs after intratracheal inoculation (690). A comparison of in vivo results with in vitro binding characteristics of the various mutant strains used in the above study suggested that wild-type B. bronchiseptica was capable of adhering to both ciliated epithelial cells and macrophages. Further, competition experiments with lactose and anti-CR3 antibody suggested that both CRD- and RGD-dependent binding was involved (690). Using mouse models, however, others have found FHA mutants to be indistinguishable from wild-type B. pertussis in their ability to persist in the lungs but defective for tracheal colonization (421, 557). Still others, also using mouse models, have observed no difference between FHA mutants and wild-type B. pertussis (284, 419, 663, 810).
Construction and analysis of two types of FHA mutant derivatives of B. bronchiseptica, one containing an in-frame deletion in the structural gene fhaB and one in which FHA is expressed ectopically in the Bvg− phase, in the absence of the array of Bvg+-phase virulence factors with which it is normally expressed, proved invaluable in determining a role for FHA (7, 177). Comparison of these mutants with wild-type B. bronchiseptica showed that FHA is both necessary and sufficient to mediate adherence to rat lung epithelial cells in vitro. Using a rat model of respiratory infection, FHA was shown to be absolutely required, but not sufficient, for tracheal colonization in healthy, unanesthetized animals (177). FHA was not required for initial tracheal colonization in anesthetized animals, however, suggesting that its role in establishment may be dedicated to overcoming the clearance activity of the mucociliary escalator (177). While all the in vitro and in vivo studies so far demonstrate a predominant role for FHA as an adhesin, the release of copious amounts of FHA from the cell surface seems counterintuitive since adhesins typically remain associated with the bacterial surface to promote maximum attachment. The significance of FHA release during bacterial infection was investigated using a B. pertussis SphB1-deficient mutant in a mouse model of respiratory tract infection (179). SphB1 mutants are incapable of secreting FHA, and mature FHA remains surface associated in these strains. These mutants were found to be defective in their ability to multiply and persist in the lungs of mice, despite their increased adhesiveness in vitro. Since surface-associated FHA also causes autoagglutination of bordetellae, a secondary role for FHA may be to facilitate the dispersal of bacteria from microcolonies and their detachment from epithelial surfaces to promote bacterial spread.
B. pertussis inhibits T-cell proliferation to exogenous antigens in vitro in an FHA-dependent manner (67). Further, McGuirk and Mills have demonstrated that interaction of FHA with receptors on macrophages results in suppression of the proinflammatory cytokine, interleukin-12 (IL-12), via an IL-10 dependent mechanism (513, 515). These data reveal a role for FHA in facilitating persistence by curbing protective Th1 immune responses. In contrast, a subsequent study suggests that FHA can elicit proinflammatory and proapoptotic responses in human monocyte-like cells and bronchial epithelial cells (2). As mentioned earlier, binding of FHA to the VLA-5 integrin induces the expression of proinflammatory genes, such as ICAM-1, in an NF-κB-dependent manner in human bronchial epithelial cells (386). FHA-specific antibodies are also necessary to protect against reinfection by B. bronchiseptica in the rat model (503). Specifically, animals were challenged with marked B. bronchiseptica strains 30 days after receiving a primary inoculation of wild-type or mutant B. bronchiseptica. The animals developed a robust anti-Bordetella serum antibody response by the 30-day time point, which was monitored both qualitatively and quantitatively by enzyme-linked immunosorbent assay (ELISA). The presence of anti-FHA serum titers was correlated with the ability of the animal to resist further infection with the marked B. bronchiseptica challenge strains. However, antibodies to FHA also inhibit the phagocytosis of B. pertussis by neutrophils (554). Taken together, these data suggest FHA performs several immunomodulatory functions in vivo.
Data regarding the role played by FHA in the pathogenesis of B. pertussis infections in humans can be gleaned from recent pertussis vaccine studies. Vaccinees who received FHA containing pertussis vaccines mounted a substantial antibody response to this protein (217, 218, 332). In general, acellular vaccines which contain FHA as well as PT toxoid have slightly greater efficacy than monocomponent PT toxoids (3, 131, 149, 734, 735, 737). However, one whole-cell component DTP vaccine in which vaccinees did not mount an antibody response to FHA was nevertheless highly efficacious (218, 332, 334, 719). Most importantly, in two studies in which serologic correlates of immunity were determined, it was found that FHA made no contribution to protection (148, 736).
Analysis of the B. pertussis, B. bronchispetica, and B. parapertussishu genomes revealed the existence of two additional genes, fhaS and fhaL, which encode FHA-like proteins (608). While orthologs of these genes are conserved among the Bordetella subspecies, differences exist in their internal sequences. Bordetella subspecies display differential binding to ciliated cells derived from different hosts, suggesting that host specificity may in part be dependent on the interaction of bacterial adhesins to their host receptors (770). Analysis of fhaS and fhaL gene products may be of interest in this regard. It may also explain the exact contribution of FHA in modulating the host immune response.
Agglutinogens.
Agglutinogens (AGGs) are surface proteins that, with infection, elicit the production of antibodies that cause the agglutination of Bordetella organisms in vitro (10, 219, 489, 666, 667, 803). Early studies determined 14 antigenic types of AGGs, 6 of which were specific for B. pertussis (666). A serotyping scheme was developed from the results of the agglutination studies using antisera raised against Bordetella in rabbits following multiple injections of killed organisms. The antisera were made “monospecific” by adsorption with heterologous strains.
Of the six AGGs specific for B. pertussis, AGG1 was common to all strains while AGG2 to AGG6 were found in various combinations in different isolated strains (666). Three AGGs (AGG1, AGG2, and AGG3) have subsequently been determined to be the main agglutinating antigens, while AGG4, AGG5, and AGG6 have been classified as minor antigens that apparently associate with either AGG2 or AGG3. AGG2 and AGG3 have since been determined to be fimbrial in nature (fimbriae are discussed in detail later in this review).
The nature of AGG1 is not known (666). Since both PRN and LPS can function as AGGs, either could be AGG1 (75, 462, 551). It must be noted, however, that the original serotyping scheme was based on heat labile antigens, thereby discounting LPS as AGG1.
Studies done over 50 years ago found that protection from pertussis in exposed children correlated with high titers of serum agglutinating antibody (agglutinins) (546, 682). In the early 1960s it was noted that the apparent efficacy of British pertussis vaccines had decreased. Preston suggested that this decline in vaccine efficacy was because the vaccine used in England at the time did not contain AGG3 and the most prevalent circulating B. pertussis strains were serotype 1.3 (640, 643). Efficacy in England apparently increased following the addition of serotype 3-containing strains to the vaccine. This seemed to support Preston's opinion (641, 642, 644). However, the protective unitage of the British vaccine was also increased at the time, so that the increased efficacy may not have been due to the inclusion of serotype 3 strains in the vaccine (667).
Since pertussis seems to have been well controlled in Japan since 1981 and since none of the DTaP vaccines used in Japan contain AGG3, it seems that antibody to this antigen is of minor importance in protection against disease (422). However, in a small study of B. pertussis isolates in Japan it was found that six of seven collected between 1992 and 1996 were serotype AGG 3 (306).
Fimbriae.
Like many gram-negative pathogenic bacteria, bordetellae express filamentous, polymeric protein cell surface structures called fimbriae (FIM). The major fimbrial subunits that form the two predominant Bordetella fimbrial serotypes, Fim2 and Fim3 (AGG2 and AGG3), are encoded by unlinked chromosomal loci fim2 and fim3, respectively (470, 558). A third unlinked locus, fimX, is expressed only at very low levels if at all (660), and recently a fourth fimbrial locus, fimN, was identified in B. bronchiseptica (401). B. bronchiseptica and B. parapertussis contain a fifth gene, fimA, located immediately upstream of the fimbrial biogenesis operon fimBCD and 3′ of fhaB, which is expressed and capable of encoding a fimbrial subunit type, FimA (68). Genome sequence analysis of B. pertussis, B. parapertussishu and B. bronchiseptica reveals that all three subspecies contain fim2 and fim3, although the predicted C terminus of Fim2 is variable in B. pertussis (638). FimX is intact in B. pertussis and B. bronchiseptica but frameshifted in B. parapertussishu. While fimA is truncated, fimN is deleted in B. pertussis. Further, variations are seen in the FimN C termini of B. bronchiseptica and B. parapertussishu. There is also a novel putative fimbrial subunit upstream of fimN in B. bronchiseptica and B. parapertussishu that is missing in B. pertussis (638).
In addition to positive regulation by BvgAS, the fim genes are subject to fimbrial phase variation by slip-strand mispairing within a stretch of cytosine residues located between the −10 and −35 elements of the fim2, fim3, fimX, and fimN promoters (401, 817). The putative promoter region of fimA does not contain a “C stretch” and therefore is predicted not to undergo phase variation where expressed. Since slip-strand mispairing affects transcription of the individual fimbrial genes independently of each other, bacteria may express Fim2, Fim3, FimX, FimN, FimA, or any combination at any given time. However, all fimbrial serotypes have a common minor fimbrial subunit, FimD, which forms the tip adhesin (265). The fimD gene is located within the fimbrial biogenesis operon downstream of fimB and fimC (472, 819). Interestingly, this operon is positioned between fhaB and fhaC, genes required for synthesis and processing of FHA. Based on the predicted amino acid sequence similarity to the E. coli PapD and PapC proteins, FimB and FimC have been proposed to function as a chaperone and usher, respectively (471, 819). Mutation of any one of the genes in the fimBCD locus results in a complete lack of fimbriae on the bacterial cell surface, suggesting that fimBCD is the only functional fimbrial biogenesis locus on the Bordetella chromosome (818).
Attachment to host epithelia is often a crtical, early step in bacterial pathogenesis. Although fimbriae are implicated in this process, it has been difficult to establish a definitive role for Bordetella fimbriae as adhesins for several reasons. First, the multiple, unlinked major fimbrial subunit genes, as well as the transcriptional and translational coupling of the fimbrial biogenesis operon with the fha operon, have impeded the ability to construct strains completely devoid of fimbriae. Second, the presence of several other putative adhesins with potentially redundant functions has obscured the detection of clear phenotypes for Fim− mutants. Finally, since the interactions between bacterial adhesins and host receptor molecules are expected to be highly specific, the use of heterologous hosts for studies with B. pertussis has severely limited the ability to detect in vivo roles for putative adhesins. Nonetheless, several studies suggest that fimbriae may mediate the binding of Bordetella to the respiratory epithelium via the major fimbrial subunits and to monocytes via FimD (328, 329, 557). Geuijen et al. have shown that purified B. pertussis fimbriae, with or without FimD, were able to bind to heparan sulfate, chondroitin sulfate, and dextran sulfate, sugars that are ubiquitously present in the mammalian respiratory tract (266). Heparin-binding domains within the Fim2 subunit were identified and found to be similar to those of the eukaryotic extracellular matrix protein, fibronectin. Studies by Hazenbos et al. suggest that FimD mediates the binding of nonopsonized B. pertussis to VLA-5 on the surface of monocytes, which then causes activation of CR3, thereby enhancing its ability to bind FHA (328, 329). Fimbriae have also been suggested to play a minor role in biofilm formation (383).
In vivo studies have shown that Fim− B. pertussis strains are defective in their ability to multiply in the nasopharynx and trachea of mice (265, 557). By using a B. bronchiseptica strain devoid of fimbriae but unaltered in its expression of FHA and other putative adhesins, fimbriae have been shown to contribute to the efficiency of establishment of tracheal colonization and are absolutely required for persistence in the trachea using both rat and mouse models (506). Moreover, the serum antibody profiles of animals infected with Fim− bacteria differ qualitatively and quantitatively from those of animals infected with wild-type B. bronchiseptica (506). Specifically, fimbriae play an immunomodulatory role by (i) acting as T-independent antigens for an early immunoglobulin M IgM response and (ii) inducing a Th2-mediated component of the host immune response to Bordetella infection (503). Challenge experiments suggest that the presence of fimbriae is important for eliciting an immune response that is protective against superinfection (S. Mattoo et al., unpublished data). Fimbriae are also important for exerting an anti-inflammatory function and inhibiting killing by lung macrophages in mice (784).
Data from the two trials in which serologic correlates of immunity in children were determined also suggest that antibody to FIM contributes to protection (148, 736). In addition, when a vaccine containing PT, FHA, and PRN was compared to one which contained FIM 2/3 as well as PT, FHA, and PRN, the latter vaccine displayed significantly greater efficacy (597) (see the section on DTaP vaccine efficacy, below).
Taken together, all the above results suggest FIM-mediated interactions with epithelial cells and/or monocytes/macrophages may play important roles not only in adherence but also in the nature and magnitude of the host immune response to Bordetella infection.
Pertactin and other autotransporters.
Bordetella strains express a number of related surface-associated proteins belonging to the autotransporter secretion system, that are positively regulated by BvgAS. The autotransporter family includes functionally diverse proteins, such as proteases, adhesins, toxins, invasins, and lipases, that appear to direct their own export to the outer membrane (344). Autotransporters typically consist of an N-terminal region called the passenger domain, which confers the effector functions, and a conserved C-terminal region called the β-barrel, which is required for the secretion of the passenger proteins across the membrane. The N-terminal signal sequence facilitates translocation of the preproprotein across the inner membrane via the Sec pathway. On cleavage of the N-terminal signal in the periplasm, the C terminus folds into a β-barrel in the outer membrane, forming an aqueous channel. The linker region between the N and C termini directs the translocation of the passenger through the β-barrel channel. On the surface, passenger domains may be cleaved from the translocation unit and remain noncovalently associated with the bacterial surface or may be released into the extracellular milieu following an autoproteolytic event (for example, when the passenger domain is a protease) or cleavage by an endogenous outer membrane protease.
The first member of autotransporter family to be identified and characterized in Bordetella is PRN. Mature PRN is a 68-kDa protein in B. bronchiseptica (556), a 69-kDa protein in B. pertussis (128), and a 70-kDa protein in B. parapertussis (human) (461). It has been proposed to play a role in attachment since all three PRN proteins contain an Arg-Gly-Asp (RGD) tripeptide motif as well as several proline-rich regions and leucine-rich repeats, motifs commonly present in molecules that form protein-protein interactions involved in eukaryotic cell binding (226). The B. pertussis, B. bronchiseptica, and B. parapertussis PRNs differ primarily in the number of proline-rich regions they contain (460). The X-ray crystal structure of B. pertussis PRN suggests that it consists of a 16-strand parallel β-helix with a V-shaped cross section and is the largest β-helix known to date (225, 226). In support of the autotransporter secretion model, Charles et al. have shown that deletion of the 3′ region of prnBp prevents surface exposure of the molecule (127).
Other Bordetella proteins with predicted autotransport ability include TcfA (originally classified as a tracheal colonizations factor) (248), BrkA (238), SphB1 (180), and Vag8 (247). All of these proteins show significant amino acid sequence similarity in their C termini and contain one or more RGD tripeptide motifs. Unlike PRN, BrkA, SphB1, and Vag8, TcfA is expressed exclusively in B. pertussis. Based on predicted amino acid sequence similarity to all of these proteins, the B. pertussis genome appears to encode at least three additional members of this autotransporter family. A lot has been learned about Bordetella autotransporters in recent years. As mentioned earlier, SphB1 has been characterized as a subtilisin-like Ser protease/lipoprotein that is essential for cleavage and C-terminal maturation of FHA (180). SphB1 is the first reported autotransporter whose passenger protein serves as a maturation factor for another protein secreted by the same organism. BrkA is expressed as a 103-kDa preproprotein that is processed to yield a 73-kDa α (passenger)-domain and a 30-kDa β-domain that facilitates transport by functioning dually as a secretion pore and an intramolecular chaperone that effects folding of the passenger concurrent with or following translocation across the outer membrane (598, 599). Like PRN and SphB1, BrkA remains tightly associated with the bacterial surface. Vag8 is a 95-kDa outer membrane protein that is expressed in B. pertussis, B. bronchiseptica, and B. parapertussishu (247). The B. pertussis and B. bronchiseptica Vag8 homologs are highly similar, and their C termini show significant homology to the C termini of PRN, BrkA, and TcfA, suggesting that Vag8, too, may function as an autotransporter. However, cleavage of the α-domain from the C terminus may not occur in Vag8, since the predicted size of the entire protein encoded by vag8 corresponds to the size seen by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (247). In contrast, TcfA is produced as a 90-kDa cell-associated precursor form that is processed to release a mature 60-kDa protein (248). It is interesting that TcfA, the only known B. pertussis-specific autotransporter, is also the only Bordetella autotransporter that is not surface associated.
The ability of PRN and the other autotransporters to function as adhesins has been tested both in vitro and in vivo. In vitro studies demonstrated that purified PRN could promote the binding of CHO cells to tissue culture wells and that expression of prn in Salmonella or E. coli could increase the adherence and/or invasiveness of these bacteria to various mammalian cell lines (228). In contrast, a PRN− strain of B. pertussis did not differ from its wild-type parent in its ability to adhere to or invade HEp2 cells in vitro or to colonize the respiratory tracts of mice in vivo (664). Similarly, a B. bronchiseptica strain with an in-frame deletion mutation in prn was indistinguishable from wild-type B. bronchiseptica in its ability to establish a persistent respiratory tract infection in rats (P. A. Cotter and J. F. Miller, unpublished data). In contrast to the animal model studies discussed above, several pieces of data derived from vaccine trials and household contact study suggest that PRN may be the most important adhesin of B. pertussis (148, 203, 736). Of the seven vaccine efficacy trials conducted in the early 1990s, two were performed in a manner in which antibody values at the time of exposure were known (148, 736). In both of these trials it was noted that antibody to PRN was most important in protection. In addition to these observations, it is clear that DTaP vaccines which contain PRN in addition to PT and FHA are significantly more effective in preventing B. pertussis illness (131, 149, 310) (this is discussed in detail in the section on DTaP vaccine efficacy studies below).
With regard to the above studies, we predict that protection may be afforded by blocking PRN-mediated attachment of B. pertussis to host cells. More recently, Hellwig et al. have presented evidence that anti-pertactin antibodies are required for efficient phagocytosis of B. pertussis by the host immune cells (343).
Potential adhesive functions for TcfA, BrkA, and Vag8 have not been investigated directly, although TcfA− B. pertussis strains show a decreased ability to colonize the murine trachea compared to wild-type B. pertussis (248). BrkA has been proposed to play a role in serum resistance and contribute to the adherence of B. pertussis to host cells in vitro and in vivo. It also protects against lysis by certain classes of antimicrobial peptides (239). Interestingly, BrkA does not appear to be required for serum resistance of B. bronchiseptica (647). Most recently, Vag8 has been proposed to facilitate the secretion of type III proteins in B. bronchiseptica (507). This is the first reported example of an autotransporter involved in regulating type III secretion.
Adenylate cyclase.
All of the Bordetella species that infect mammals secrete CyaA, a bifunctional calmodulin-sensitive adenylate cyclase/hemolysin. CyaA is expressed maximally in the Bvg+ phase. Unlike the promoter for fhaB, cyaA does not contain any high-affinity BvgA-binding sites in its promoter region. Instead, it contains several heptameric variants of the BvgA-binding consensus 5′-TTTCCTA-3′ which extend between nucleotides −137 and −51 from the transcriptional start site. Phosphorylation of BvgA is absolutely required for binding at these sites. The main target sequence for the BvgA∼P and DNA interaction is located between positions −100 and −80; binding to this centrally located site is predicted to trigger cooperative interactions of BvgA∼P with the neighboring low-affinity sites.
CyaA is synthesized as a protoxin monomer of 1,706 amino acids. Its adenylate cyclase catalytic activity is located within the N-terminal 400 amino acids (277, 349). The 1,300-amino-acid C-terminal domain mediates delivery of the catalytic domain into the cytoplasm of eukaryotic cells and possesses low but detectable hemolytic activity for sheep red blood cells (46, 349, 668). Amino acid sequence similarity between the C-terminal domain of CyaA, the hemolysins of E. coli (HlyA) and Actinobacillus pleuropneumoniae (HppA), and the leukotoxins of Pasteurella hemolytica (LktA) and Actinobacillus actinomycetemcomitans (AaLtA) places CyaA within a family of calcium-dependent, pore-forming cytotoxins known as RTX (repeats-in-toxin) toxins (659, 672, 676, 813). Each of these toxins contains a tandem array of a nine amino acid repeat [LXGGXG(N/D)DX] that is thought to be involved in calcium binding (813). Before the CyaA protoxin can intoxicate host cells, it must be activated by the product of the cyaC gene, which is located adjacent to, and transcribed divergently from, the cyaABDE operon (36). CyaC activates the CyaA protoxin by catalyzing the palmitoylation of an internal lysine residue (Lys-983) (37, 311). The E. coli HlyA protoxin is also activated by fatty acyl group modification (322, 375, 388). Whereas E. coli hemloysin is released in the extracellular medium, the majority of the Bordetella CyaA remains surface associated, with only a small portion being released in the supernatant. It was recently suggested that FHA may play a role in retaining CyaA toxin on the bacterial cell surface; B. pertussis mutants lacking FHA released significantly more CyaA into the medium, and CyaA toxin association with the bacterial surface could be restored by expressing FHA from a plasmid in trans (844). CyaA also inhibits biofilm formation in B. bronchiseptica, possibly via its interaction with FHA and subsequent interference with FHA function (383).
The eukaryotic surface glycoprotein CD11b serves as the receptor for mature CyaA toxin. Interestingly, surface-bound CyaA does not appear to be responsible for host cell intoxication; a recent report demonstrates that intoxication requires close contact of live bacteria with target cells and active secretion of CyaA (292). CyaA can enter a variety of eukaryotic cell types (350). Once inside, CyaA is activated by calmodulin (830) and catalyzes the production of supraphysiologic amounts of cyclic AMP (cAMP) from ATP (89, 163, 164, 321). Purified CyaA inhibits chemiluminescence, chemotaxis and superoxide anion generation by peripheral blood monocytes and polymorphonuclear neutrophils in vitro (611). CyaA also induces apoptosis in cultured murine macrophages (419) and inhibits the phagocytosis of B. pertussis by human neutrophils (808, 809). Recently, CyaA was shown to inhibit the surface expression of costimulatory molecule CD40 and IL-12 production in bone marrow-derived dendritic cells from C57BL/6 mice infected with B. bronchiseptica (709). It was further shown to be required for p38 phosphorylation, suggesting that it plays a role in inhibiting the p38 mitogen-activated protein kinase pathway (709). In vivo studies have shown that, compared to wild-type B. pertussis, CyaA-deficient mutants are defective in their ability to cause lethal infections in infant mice (305, 810) and to grow in the lungs of older mice (284, 305). Taken together, these results suggest that CyaA functions primarily as an anti-inflammatory and antiphagocytic factor during infection.
The importance of CyaA in resisting constitutive host defense mechanisms was further demonstrated by using mice that lack the ability to mount an adaptive immune response. SCID, SCID-beige, and Rag-1−/− mice, which are deficient in T and B cells and NK cell activities, are dependent on constitutive, innate defense mechanisms for protection against microbial pathogens. When these mice were inoculated with wild-type B. bronchiseptica, they died within 50 days, while those inoculated with the CyaA-deficient strain remained healthy (324). Conversely, neutropenic mice, made so by treatment with cyclophosphamide or by a homozygous null mutation in the granulocyte colony-stimulating factor gene, were killed by both wild-type and CyaA-deficient strains of B. bronchiseptica, indicating that in the absence of neutrophils, CyaA is not required to cause a lethal infection (324). These data indicate that T and B cells are required to prevent killing by wild-type B. bronchiseptica but innate defenses alone are adequate to control infection by a CyaA-deficient mutant. It also suggests that phagocytic cells, particularly polymorphonuclear neutrophils, are a primary in vivo target of the adenylate cyclase toxin.
Primary infections of children with either B. pertussis or B. parapertussishu stimulate a vigorous serum antibody response to CyaA (153). In contrast, children immunized with DTP or DTaP vaccines who later became vaccine failures and developed pertussis had only minimal serum antibody responses to CyaA. This apparent induced tolerance is of interest, and it may be evidence of the phenomenon called “original antigenic sin” (395). With this phenomenon, a child's serum immunologic response at initial exposure is to all presenting epitopes of the infecting agent or vaccine. On subsequent exposure to the pathogen, the child responds preferentially to the epitopes shared with the original infecting agent or vaccine and the response to new epitopes of the infecting agent are blunted. In the present scenario, both vaccines contained multiple antigens and the vaccinated children responded to the antigens with which they had been primed but had only a minimal response to the new antigen (CyaA) following infection. CyaA is not present in DTaP vaccines, but very small amounts might be present in DTP vaccines.
Dermonecrotic toxin.
Although initially misidentified as an endotoxin, DNT was one of the first B. pertussis virulence factors to be described (62). This heat-labile toxin induces localized necrotic lesions in mice and other laboratory animals when injected intradermally and is lethal for mice at low doses when administered intravenously (62, 377, 470, 609). The DNTs of B. pertussis, B. bronchiseptica, and B. parapertussishu are nearly identical (∼99% amino acid identity) cytoplasmic, single polypeptide chains of about 160 kDa (183, 370, 580, 846). Bordetella DNT is a typical A-B toxin, composed of a 54-amino-acid N-terminal receptor-binding domain and a 300-amino-acid C-terminal enzymatic domain. While the receptor for DNT has not yet been identified, in vitro assays using fibroblast and osteoblast-like cell lines determined that on receptor binding, DNT is internalized via a dynamin-dependent endocytosis. Translocation is independent of acidification of endosomes and retrograde vesicular transport and requires the N-terminal region of the DNT enzymatic domain, which includes a putative transmembrane domain. On endocytosis, DNT undergoes proteolytic nicking by mammalian proteases such as furin, which is necessary for the cellular activity of DNT (502).
In vitro studies have shown that purified DNT from B. bronchiseptica induces dramatic morphological changes, stimulates DNA replication, and impairs differentiation and proliferation in osteoblastic clone MC 3T3 cells (369, 372). Recent evidence indicates that these effects are due to DNT-mediated activation of the small GTP-binding protein Rho (371), which results in tyrosine phosphorylation of focal adhesion kinase (p125fak) and paxillin (436). p125fak and paxillin are involved in embryonic development and cell locomotion (378), and their activation leads to profound alterations in the actin cytoskeleton and the assembly of focal adhesions (648, 703-705). Lacerda et al. also showed that DNT stimulates DNA synthesis without activation of p42mapk and p44mapk, providing evidence for a novel p21rho-dependent signaling pathway that leads to entry into the S phase of the cell cycle in Swiss 3T3 cells (436). If and how these effects of DNT contribute to Bordetella pathogenesis is not known. Although B. bronchiseptica strains with decreased dermonecrotic toxin activity have been associated with decreased turbinate atrophy in infected pigs (483, 671), transposon mutants of B. pertussis lacking dermonecrotic toxin are no less virulent than wild-type bacteria in mice (810).
Lipopolysaccharides.
Like endotoxins from other gram-negative bacteria, the LPS of Bordetella species are pyrogenic, mitogenic, and toxic and can activate and induce tumor necrosis factor production in macrophages (19, 582, 806). Bordetella LPS molecules differ in chemical structure from the well-known smooth-type LPS expressed by members of the family Enterobacteriaceae. Specifically, B. pertussis LPS lacks a repetitive O-antigenic structure and is therefore more similar to rough-type LPS. It resolves as two distinct bands (A and B) on silver-stained sodium dodecyl sulfate-polyacrylamide gels (612). The faster-migrating moiety, band B, consists of a lipid A molecule linked via a single ketodeoxyoctulosonic acid residue to a branched oligosaccharide core structure containing heptose, glucose, glucuronic acid, glucosamine, and galactosaminuronic acid (GalNAcA) (92, 443, 447). The charged sugars, GalNAcA, glucuronic acid, and glucosamine, are not commonly found as core constituents in other LPS molecules. The slower-migrating moiety (band A) consists of band B plus a trisaccharide consisting of N-acetyl-N-methylfucosamine (FucNAcMe), 2,3-deoxy-di-N-acetylmannosaminuronic acid (2,3-diNAcManA), and N-acetylglucosamine (GlcNAc) (92, 443, 447). B. bronchiseptica LPS is composed of band A and band B plus an O-antigen structure consisting of a single sugar polymer of 2,3-dideoxy-di-N-acetylgalactosaminuronic acid (208). B. parapertussishu isolates contain LPS that lacks band A, has a truncated band B, and contains an O antigen that, like B. bronchiseptica, consists of 2,3-dideoxy-di-N-acetylgalactosaminuronic acid. B. parapertussisov isolates lack O antigen and contain band A- and B-like moieties that appear to be distinct from those of the other Bordetella species (780).
The wlb locus, which is well conserved among the Bordetella subspecies, is required for the biosynthesis and assembly of the band A LPS trisaccharide (639). It is composed of 12 genes, wlbA to wlbL. Based on mutational analyses, certain putative functions have been assigned for these genes (639). WlbA to WlbD are involved in the biosynthesis of 2,3-diNAcManA, the second sugar of the band A trisaccharide. WlbE encodes a transferase that adds 2,3-diNAcManA to the growing trisaccharide chain. WlbF is a putative enzyme involved in FucNAcMe biosynthesis, and WlbG is a transferase that adds this sugar to an acyl carrier lipid on which the trisaccharide unit is synthesized prior to transfer en bloc to band B. WlbH is a GlcNAc transferase that adds the third and final sugar of the trisaccharide. WlbI is a predicted integral membrane protein which is likely to be involved in the transfer of band A and/or assembly of the final full-length LPS molecule rather than its biosynthesis. Interestingly, while wlbJ and wlbK are two apparently separate genes in B. pertussis, they are fused into a single open reading frame in B. bronchiseptica and B. parapertussishu. Mutations in wlbJK do not affect LPS biosynthesis or alter any phenotypes compared to the wild-type strains, and their function(s) remains unclear. WlbL is a putative dehydratase involved in the biosynthesis of the band A sugar FucNAcMc. Finally, the wbm locus, which lies adjacent to the wlb locus in B. bronchiseptica and B. parapertussishu, is required for the assembly of O antigen (85). Deletion of wbm in B. bronchiseptica and B. parapertussishu leads to loss of O-antigen expression, thus removing the major structural differences between the LPS molecules of these bacteria and B. pertussis (85).
Although a distinct role(s) for LPS in Bordetella pathogenesis has not yet been demonstrated, its importance is suggested by the observation that changes in LPS structure in B. bronchiseptica are controlled by the BvgAS virulence regulatory system (780). Recently, pagP was shown to encode a BvgAS-regulated lipid A palmitoyl transferase that mediates a palmitoylation modification of B. bronchiseptica lipid A. Identical pagP open reading frames have been identified in the B. pertussis and B. parapertussishu genomes. Preliminary evidence suggests that the B. parapertussishu lipid A also undergoes BvgAS-regulated, PagP-mediated palmitoylation. However, pagP is not expressed in B. pertussis due to a disruption of the putative promoter region by an IS element. These differences may contribute to determining host specificity or the nature of infection. Analysis of B. bronchiseptica pagP mutants showed that pagP is not required for the initial colonization of the mouse respiratory tract but may be important for persistence. Likewise, compared with their wild-type parental strains, B. pertussis, B. parapertussishu, and B. bronchiseptica strains which synthesize only band B LPS show decreased colonization in a mouse model of respiratory infection (325). For B. bronchiseptica and B. parapertussishu, this difference may be attributed to differences in sensitivity to antibody-dependent serum killing, for which palmitoylation by PagP may also be important (325). Analysis of B. bronchiseptica and B. parapertussishu wbm mutants, which lack the O antigen, showed that these strains activated complement and were highly susceptible to complement-mediated killing in vitro. Interestingly, while the B. parapertussishu Δwbm mutant was severely defective in colonization of the tracheas and lungs of mice, the B. bronchiseptica wbm mutant showed no defect. Perhaps the most interesting observation, however, is that B. pertussis strains which did not display significant resistance to killing by serum containing excess complement in vitro rapidly acquired resistance to complement-mediated killing in vivo in a BrkA-independent manner (620). Since B. pertussis does not express O antigen, this observation came as a considerable surprise, leading to the speculation that B. pertussis may have developed another means of resisting antibody-independent complement-mediated killing in vivo. A possible solution to this mystery seems to have been provided by the recent observation that LPS protects B. pertussis from surfactant protein A (SP-A)-mediated clearance, presumably by sterically limiting access of SP-A to the lipid A region, the target for SP-A binding (691). Thus, B. pertussis and B. bronchiseptica seem to have utilized their individual resources to acquire resistance to complement-mediated killing in vivo—B. bronchiseptica deploys serum resistance via its O-antigen-containing LPS and therefore does not requires BrkA for this purpose; B. pertussis lacks O antigen and therefore uses a combination of its O-antigen-deficient LPS and BrkA to acquire serum resistance. Further in vivo characterization of mutants with defined mutations affecting LPS structure will greatly facilitate deciphering the precise role(s) of LPS in Bordetella pathogenesis.
Type III secretion system.
A TTSS has been identified in Bordetella subspecies (841). TTSSs allow gram-negative bacteria to translocate effector proteins directly into the plasma membrane or cytoplasm of eukaryotic cells through a needle-like injection apparatus (433). These bacterial effector proteins then alter normal host cell-signaling cascades and other processes to promote the pathogenic strategies of the bacteria (450). Type III secretion has been identified in a variety of pathogens including those infecting humans, such as Yersinia, Shigella, Salmonella, and enteropathogenic E. coli, as well as the plant pathogens Pseudomonas syringae and Erwinia (for reviews, see references 172 and 374). Most recently, TTSSs have also been identified in endosymbionts and invertebrate pathogens, such as Rhizobium spp., Sodalis glossinidius, and Photorhabdus luminescens (192, 254, 789). Type III secretion represents one of the most complex mechanisms of protein translocation in biology. The complete TTSS often requires over 20 genes, which encode a secretion apparatus that spans the bacterial cytoplasmic and outer membranes, as well as translocator proteins that form pores in the eukaryotic cell membrane and a type III secretion-specific ATPase required for apparatus assembly and secretion (420). While the genes encoding the secretion apparatus and translocators are relatively highly conserved among different genera, the effector proteins secreted by these systems are quite diverse.
The Bordetella TTSS was first identified in B. bronchiseptica as a BvgAS-activated virulence factor. The Bordetella type III secretion locus, termed the bsc locus, includes 22 genes that encode components of the type III secretion apparatus, secreted proteins, and putative chaperones. Interestingly, while type III genes are intact and highly conserved in members of the B. bronchiseptica cluster, only B. bronchiseptica and B. parapertussisov readily display type III secretion-associated phenotypes in vitro. These include induction of cytotoxicity in several cultured cell lines (779, 841), dephosphorylation of specific host cell proteins (841), and activation of the mitogen-activated protein kinases, ERK1 and ERK2 (840). Bone marrow-derived dendritic cells derived from mice infected with B. bronchiseptica display a TTSS-mediated increase in surface expression of major histocompatibility complex class II and of CD86 and CD80 costimulatory molecules (709). In B. bronchiseptica, the TTSS also prevents translocation of the transcription factor NF-κB to the nucleus even on stimulation of the cells with tumor necrosis factor alpha; instead it causes aberrant aggregation of NF-κB within the host cell cytoplasm (840). B. bronchiseptica also causes very rapid cell death in macrophage and epithelial cell lines in a type III secretion-dependent manner (840). Cell death does not require caspase-1, is not blocked by the pancaspase inhibitor zVAD, and does not involve cleavage of procaspase-3, procaspase-7, and poly(ADP-ribose) polymerase, suggesting that the cell death pathway induced by the B. bronchiseptica TTSS is distinct from the death pathways induced by the Yersinia, Shigella, and Salmonella TTSSs (731). The Bordetella TTSS most probably induces a necrotic form of cell death, since dying cells morphologically resemble necrotic rather than apoptotic cells and since death is efficiently blocked by the addition of nonspecific cytoprotectants such as glycine. Despite extensive efforts, the Bordetella type III effector proteins and their cellular targets for the above phenotypes are presently unknown.
In vivo, the B. bronchiseptica TTSS contributes to persistent colonization of the trachea in both rat and mouse models of respiratory infection (840, 841). The inflammatory cells that infiltrate the lungs during infection undergo apoptosis in mice infected with a wild-type strain but not in those infected with a mutant strain deficient in type III secretion (840). Additionally, mice infected with the type III secretion-deficient strain elicit higher titers of anti-Bordetella antibodies (specifically serum IgA) than do animals infected with wild-type Bordetella (840). Consistent with this, rats infected with the type III secretion-deficient strain are completely protected against superinfection with wild-type B. bronchiseptica (Mattoo et al., unpublished data) and adoptive transfer of anti-Bordetella antibodies protects SCID-beige mice from tracheal and lung colonization by B. bronchiseptica (324). Interestingly, infection of immunocompromised SCID and SCID-beige mice with type III secretion mutants resulted in a hypervirulent phenotype (840). Taken together, these data suggest the B. bronchiseptica. TTSS may be involved in modulating the host immune response and could contribute to the typically chronic rather than pathological nature of B. bronchiseptica infections.
Recently, an additional locus consisting of four genes, btrS, btrU, btrW, and btrV, situated 3′ to the bsc locus was identified and shown to encode regulatory proteins for the Bordetella TTSS (507). Like the bsc genes, this locus, called btr (for “Bordetella type III regulation”), is also transcriptionally activated by BvgAS. btrS encodes an extracytoplasmic function sigma factor, homologous to the HrpL protein which activates type III secretion in P. syringae (507). btrU, btrW, and btrV encode proteins predicted to contain an array of domains that define “partner-switching” complexes that were traditionally thought to function only in gram-positive bacteria (507). Analysis of the btr locus in B. bronchiseptica revealed an intricate level of regulation of type III secretion, which falls downstream of the role of BvgA. BtrS was found to be necessary and sufficient for transcription of all bsc type III genes. Deletions in btrU and btrW revealed an uncoupling of protein expression from secretion, since these mutants expressed type III proteins at normal levels but failed to secrete them. Finally, while transcription of type III loci was unaffected, type III secretion-specific proteins could not be detected in a btrV deletion mutant. Thus, the btr locus encodes a novel regulatory cascade where BtrS is required for the expression of type III loci, BtrU and BtrW are required for secretion, BtrV is essential for translation and/or protein stability, and BvgAS exerts control over the entire TTSS by regulating btrS (507).
Like the bsc genes, the btr genes are highly conserved (97 to 100% amino acid sequence identity) between B. bronchiseptica and B. pertussis (507, 608). The bsc and btr genes of B. pertussis are predicted to be transcribed and translated to yield full-length polypeptides. However, unlike B. bronchiseptica and B. parapertussov, B. pertussis and B. parapertussishu failed to confer cytotoxicity to mammalian cell lines in vitro, consistent with the lack of expression of type III proteins, as determined by immunoblot analysis (507). Surprisingly, reverse transcription-PCR analysis of B. pertussis and B. parapertussishu showed that all bsc and btr loci were actively transcribed and BvgAS activated. Further, the BtrS regulon appears to be intact and functional in B. pertussis and B. parapertussishu. Thus, the block in type III secretion observed in human-adapted Bordetella strains under standard in vitro laboratory conditions appears to be post-transcriptional, similar to the phenotype observed in a B. bronchiseptica btrV deletion mutant. There appears to be an evolutionary pressure to maintain the TTSS in B. pertussis: in comparing B. pertussis and B. bronchiseptica, BtrS, BtrW, and BtrV are identical, BtrU differs at six amino acid residues, and of the nucleotide differences observed in the genes encoding TTSS proteins, substitutions are dramatically skewed toward those that are silent or conservative (507). It is therefore conceivable that B. pertussis does express a functional TTSS but in a manner where signal inputs are recognized, integrated, and regulated differently from in B. bronchiseptica. If so, then taken together with the immunomodulatory role suggested for the TTSS, this hypothesis provides new insight into how we view and vaccinate against B. pertussis infection. It further raises the possibility that TTSS-deficient Bordetella strains could serve as live vaccine delivery vehicles. Additional phylogenetic analyses of type III-related loci will help clarify the relationship between expression of the bsc and btr loci, host range, and course of disease.
Tracheal cytotoxin.
TCT corresponds to a disaccharide-tetrapeptide monomer of peptidoglycan that is produced by all gram-negative bacteria as they break down and rebuild their cell wall during growth. Its structure is N-acetylglucosaminyl-1,6-anhydro-N-acetylmuramyl-(l)-alanyl-γ-(d)-glutamyl-mesodiaminopimelyl-(d)-alanine (170). While other bacteria, such as E. coli, recycle this peptidoglycan fragment by transporting it back into the cytoplasm via an integral cytoplasmic membrane protein called AmpG, Bordetella spp. release it into the environment due to the lack of a functional AmpG (170, 394, 608, 674). As such, TCT is constitutively expressed and is independent of BvgAS control.
The activities of TCT have been studied in vitro using hamster tracheal organ culture and cultured hamster tracheal epithelial (HTE) cells (169, 280). TCT causes mitochondrial bloating, disruption of tight junctions, and extrusion of ciliated cells, with little or no damage to nonciliated cells, in hamster tracheal ring cultures and a dose-dependent inhibition of DNA synthesis in HTE cells. TCT also causes loss of ciliated cells, cell blebbing, and mitochondrial damage, as is evident in human nasal epithelial biopsy specimens (820). TCT alone is necessary and sufficient to reproduce the specific ciliated- cell cytopathology characteristic of B. pertussis infection in explanted tracheal tissue (280). TCT-dependent increase in nitric oxide (NȮ) is proposed to mediate this severe destruction of ciliated cells. TCT triggers IL-1α production in HTE cells, and both TCT and IL-1α result in increased NO• production when added to HTE cells (341, 342). It is hypothesized that, in vivo, TCT stimulates IL-1α production in nonciliated mucus-secreting cells, which positively controls the expression of inducible nitric oxide synthase, leading to high levels of NO• production. NO• then diffuses to neighboring ciliated cells, which are much more susceptible to its damaging effects (250). TCT also functions synergistically with Bordetella LPS to induce the production of NO• within the airway epithelium (251). The ability to construct TCT-deficient mutants by expressing a heterologous ampG gene in Bordetella will allow this hypothesis to be tested by using in vivo models.
Pertussis toxin.
PT is an ADP-ribosylating toxin synthesized and secreted exclusively by B. pertussis. It is an A-B toxin composed of six polypeptides, designated S1 to S5, which are encoded by the ptxA to ptxE genes, respectively. The S1 polypeptide comprises the A subunit of the toxin, while the pentameric B subunit consists of polypeptides S2, S3, S4, and S5 assembled in a 1:1:2:1 ratio (472, 590, 750). Each subunit is synthesized with an N-terminal signal sequence, suggesting that transport into the periplasmic space occurs via a general export pathway analogous to the sec system of E. coli. Secretion across the outer membrane requires a specialized transport apparatus composed of nine Ptl (for “pertussis toxin liberation”) proteins (231, 812). The ptl locus bears extensive similarity to the prototype type IV secretion system involved in exporting single-stranded “T-DNA” encoded by the Agrobacterium tumefaciens virB operon, suggesting that both these systems function by a common mechanism to transport large protein complexes (182, 434, 799). Furthermore, there is evidence that only the fully assembled PT holotoxin is efficiently secreted (585, 626).
The ptl genes are located directly 3′ to, and within the same transcriptional unit as, the ptxA to ptxE genes (430, 812). While the chromosomes of B. parapertussis and B. bronchiseptica also contain ptx-ptl loci that encode functional polypeptides, these genes are transcriptionally silent due to mutations in the promoter regions (13, 302, 494, 589). In both B. parapertussis and B. bronchiseptica, replacement of native ptx-ptl promoter sequences with those from B. pertussis results in the secretion of biologically active Ptx (327). The biological relevance of differential PT expression among bordetellae is not known.
The A component of PT, consisting of the enzymatically active S1 subunit, sits atop the B oligomer, a ringlike structure formed by the remaining S2 to S5 subunits (403, 700, 749). The subunits are held together by noncovalent interactions. The B oligomer binds to eukaryotic cell membranes and dramatically increases the efficiency with which the S1 subunit gains entry into host cells (749). It has been proposed that PT traverses the membrane directly without the need for endocytosis, since it does not require an acidic environment for entry into eukaryotic cells (396). Subsequent reports, however, have proposed that PT binds to cell surface receptors and undergoes endocytosis via a cytochalasin D-independent pathway. Early and late endosmes, as well as the Golgi apparatus, have been implicated in the PT trafficking process (507, 836, 837). Once within the host cell cytosol, the B oligomer intercalates into the cytoplasmic membrane and binds ATP, causing the release of the S1 subunit, which then becomes active on reduction of its disulfide bond (402). While the exact mechanism of how and when PT assembles and interacts with the Ptl transporter in vivo is currently unknown, a recent report suggests that subassemblies of PT consisting of the S1 subunit and a partial B oligomer can interact with the Ptl system (84).
Based on extensive in vitro characterization of PT, the S1 subunit in its reduced form has been shown to catalyze the transfer of ADP-ribose from NAD to the α subunit of guanine nucleotide-binding proteins (G proteins) in eukaryotic cells (61, 403, 749). PT can ADP-ribosylate and thus inactivate G proteins such as Gi, Gt (transducin), and Go. When active, Gi inhibits adenylyl cyclase and activates K+ channels, Gt activates cyclic GMP phosphodiesterase in specific photoreceptors, and Go activates K+ channels, inactivates Ca2+ channels, and activates phospholipase C-β (776). Biological effects attributed to the disruption of these signaling pathways include histamine sensitization, enhancement of insulin secretion in response to regulatory signals, and both suppressive and stimulatory immunologic effects (577, 623). The various effects of PT in pertussis vaccines, in purified form and released during infection, have been studied in various model systems and in humans and have been reviewed in depth previously (147). To summarize, histamine sensitization in mice in response to B. pertussis infection was first described over 50 years ago (606). Subsequently, histamine sensitization was studied by many investigators, but only five studies involving humans were carried out (269, 486, 501, 561, 574, 576, 618, 622, 625, 686, 701, 801). In a 1948 study, Parfentjev and Goodline found that mice injected intraperitoneally with a pertussis vaccine subsequently became hypersensitive to histamine challenge; 2 mg of histamine had similar lethality in sensitized (previously vaccinated) mice as did 50 mg in unvaccinated mice (606). In these animals, histamine sensitivity following intraperitoneal injection of pertussis vaccine increased over 4 to 5 days, plateaued, and then diminished over 3 to 4 weeks (801). Following intravenous pertussis vaccine administration, however, sensitization occurred within 90 min and peaked in 1 day. Histamine sensitization also occurs in mice following B. pertussis respiratory infection (625).
In three controlled studies in children, histamine sensitization could not be demonstrated in association with B. pertussis infection or following vaccination (269, 501, 618). In the most recent study, Gifford et al. compared skin test sensitivity to histamine in DT- and DTP-immunized children and found no significant difference in wheal size between the two groups (269).
In 1949 it was reported that mice that received pertussis vaccine intraperitoneally had a marked decrease in their blood glucose concentrations and that this hypoglycemia persisted for at least a week (607). This hypoglycemia was due to hyperinsulinemia. Peak levels of insulin following ip injection occurred 7 days after exposure in the mouse, and elevated levels persisted for 17 days (307). It was also noted that mice immunized with pertussis vaccine did not experience the usual hyperglycemic effect following histamine administration (743).
There is considerable evidence indicating that PT causes an increase in serum insulin levels in humans (21, 147). In the most definitive study, Toyota et al. administered PT intravenously to six volunteers and observed increased plasma insulin levels at the time when glucose tolerance tests were performed (763). Specifically, the ratio of the increment of the plasma insulin level to that of blood glucose at 30 min after the glucose challenge remained significantly greater 4, 30, and 60 days after the initial intravenous PT injection compared with the baseline glucose tolerance test response. Infants vaccinated with DTP vaccines have also been noted to have an increase in serum insulin levels (319, 552). Neonates with severe pertussis are occasionally found to be markedly hypoglycemic, suggesting hyperinsulinemia (156, 165, 360).
Almost 100 years ago, it was observed that children with pertussis often had marked leukocytosis in association with significant lymphocytosis (256). Early studies of mice found a similar leukocytosis (562-565, 575, 600). This occurred following the injection of either living B. pertussis organisms, killed B. pertussis cells, or B. pertussis culture supernatants. PT was later found to cause absolute lymphocytosis in many diverse species such as lampreys, swine, guinea pigs, rabbits, monkeys, calves, sheep, and mice (600). In the mouse model, PT administered intravenously elicits a leukocytosis which peaks in about 4 days and then decreases to normal values over a 2- to 3-week period (565). Both neutrophil and lymphocyte numbers increase, but the lymphocytic response is generally more pronounced. The leukocytosis is not due to increased cell production (562). Instead, there is an increase in the release of cells into the blood from extravascular sites and these cells continue to recirculate rather than emigrate from the blood, as would occur normally. Of the lymphocytes, both B and T cells are increased in the peripheral blood (53, 565). In most primary infections in children, there is a distinct leukocytosis with an absolute lymphocytosis (149). In contrast, infections in adults (which are always reinfections) are not associated with an absolute lymphocytosis (149, 550). Occasional primary infections in young infants also do not elicit a lymphocytosis. This is probably due to the presence of transplacentally acquired antibody to PT.
PT is a strong adjuvant in several immunologic systems in several animals and humans (14, 15, 190, 235, 246, 452, 453, 456, 553, 561, 573, 575, 578, 600, 610, 649, 699, 745, 746, 801, 804). This adjuvancy in the experimental-animal model is associated with enhancement of serum antibody responses to other antigens, increased cellular immune responses to various protein antigens, contribution to hyperacute experimental autoallergic encephalomyelitis, and increased anaphylactic sensitivity. Of these adjuvant activities demonstrated in animal model systems, only the enhancement of serum antibody responses to other vaccine antigens has been demonstrated to occur in vaccinated children.
Although, on the one hand, PT displays adjuvant properties, it has also been shown to inhibit chemotaxis, oxidative responses, and lysosomal enzyme release in neutrophils and macrophages (61, 72, 74, 438, 521, 555, 595, 717, 785). This phenotype has been confirmed using mouse and rat models, where PT was shown to inhibit chemotaxis and migration of neutrophils, monocytes/macrophages, and lymphocytes (76, 479, 522). Most recently, PT was shown to display an immunosuppressive activity, since mice infected with a PT− mutant elicited much higher anti-Bordetella serum antibody titers than did mice infected with wild-type B. pertussis (90). PT has also been suggested to function as an adhesin involved in the adherence of B. pertussis to human macrophages and ciliated respiratory epithelial cells (654, 771).
PT is commonly cited as the major virulence factor expressed by B. pertussis, responsible for many, if not all, of the symptoms typically associated with pertussis (623). However, despite a plethora of experimental evidence demonstrating PT function in vitro, in animal models, and in human studies, clear evidence for a substantial in vivo role for PT in human disease is lacking. Since B. pertussis and B. parapertussishu differ primarily in the absence of PT expression by B. parapertussishu, a comparative analysis of the symptoms in children infected with either of these organisms has been adopted as a means of isolating the effects of PT. Such studies have indicated that the most notable difference between the two is leukocytosis with lymphocytosis in B. pertussis- but not B. parapertussis-infected children (340, 825). However, PT does appear to contribute to morbidity in B. pertussis infections because the duration and severity of illness tend to be greater in B. pertussis infections than in B. parapertussis infections. In this regard, the frequent finding of extreme leukocytosis in neonates and young infants with fatal B. pertussis infections is noteworthy. However, it seems clear that PT does not play a role in causing the paroxysmal coughing, whooping, and vomiting characteristic of pertussis. The exact role of PT in the establishment of infection, disease, and/or transmission of pertussis remains to be determined.
PATHOLOGY
B. pertussis Infection
In 1943 Lapin wrote a 14-page chapter on the pathology of pertussis, and there has been little new information added during the ensuing 60 years (442). In his review Lapin cited 35 papers relating to postmortem data on children dying of pertussis. In spite of such a complete data set, there are no data available on the pathology of mild or typical pertussis in patients that survived.
In 1912 Mallory and Horner reported the findings of three children with illnesses of relatively short durations prior to death (487). However, all three of these children had high fevers prior to death, suggesting a secondary problem. Microscopic study in these cases showed large numbers of bacteria between the cilia of the cells lining the trachea. The microorganisms usually extended to the base of the cilia, and the long axis of the organisms tended to coincide with the direction of the cilia. Frequently there was a lateral spreading of the cilia (mushrooming) of individual cells, and in many places the cilia were reduced to stubs or were entirely gone. In two of the cases, no bacteria were found between the cilia of the cells lining the bronchi or bronchioles. In the third case, masses of bacteria were found between the cilia of the cells lining the bronchi and bronchioles. There was an unevenness in the distribution with some bronchi free of bacteria.
In experiments using rhesus and ringtail monkeys, Sauer and Hambrecht found pure cultures of B. pertussis between the cilia of the smaller bronchi and bronchioli during uncomplicated pertussis (442, 689). They also noticed endobronchitis and peribronchitis with an abundance of B. pertussis on and between the cilia of the finer bronchi and bronchioli at 11 days postinoculation in one monkey. The upper respiratory tract was normal macroscopically. The bronchi were found to contain leukocytes, mucus, and debris.
Most patients with fatal cases of pertussis have bronchopneumonia; this may be due to B. pertussis or to secondary infection with other respiratory bacteria (149). The initial stages of infection entail congestion and infiltration of the mucosa by lymphocytes and polymorphonuclear leukocytes. The lumens of the bronchi contain inflammatory debris. Lapin, in reviewing the data of several reports, suggests that the initial pulmonary lesion in pertussis is a lymphoid hyperplasia of peribronchial and tracheobronchial lymph nodes (442). A necrotizing process that affects the midzonal and basilar layers of the bronchial epithelim follows (149, 469). Necrosis and desquamation of the superficial epithelial layers of the small bronchi may subsequently occur. Numerous small areas of atelectasis occur, and there is an increase in fibrous tissue around the bronchi.
Of the more recent cases, postmortem data are available in the deaths of five infants (156, 712). A 27-day-old infant was found to have extensive hemorrhage in the apex of the left lung (156). Bilateral pulmonary edema and focal hemorrhages were noted microscopically. There was also a diffused infiltration by macrophages and moderate focal infiltrations with inflammatory cells, accompanied by extensive necrotizing bronchopneumonia and thromboemboli. Smith and Vyas noted similar postmortem findings in four infants (712). Widespread mucus plugging and extensive mucosal damage were reported. They also noted a severe depletion of lymphocytes from the thymus, lymph nodes, and spleen.
In fatal cases there are often pathologic changes in the brain. There may be microscopic or gross cerebral hemorrhage and cortical atrophy. Although it has been suggested that these findings may be the direct effect of bacterial toxins (624), it is most likely that they are the result of hypoxia and anoxic brain damage.
B. bronchiseptica Infection
Dogs.
B. bronchiseptica infection is a major cause of kennel cough in dogs (49, 509). This disease is a tracheobronchitis characterized by congestion of the mucosal lining of the trachea and bronchi and a mucoid or mucopurulent exulate. In addition, patchy areas of exudative pneumonia as well as petechiae and hemorrhages over the pleural surface may be noted. Often, no macroscopic abnormalities are seen in the respiratory tract. However, in most dogs, histologic examination reveals tracheobronchitis.
There are two patterns of microscopic findings. One pattern consists of focal, occasionally coalescing, areas of epithelial degeneration and necrosis. The cells are disorganized, with vacuolation and pyknosis. The lamina propria is congested and infiltrated with only a few macrophages and lymphocytes. In the other pattern, a mucopurulent exudate is present in the lumen of the airway and there is edema of the lamina propria with a marked infiltration of polymorphonuclear leukocytes. Clumps of gram-negative bacteria are seen among the cilia of the tracheobronchial epithelium. Infection complicated by pneumonia is accompanied by alveolar capillary congestion and exudation of fluid with polymorphonuclear leukocytes and macrophages into the air spaces. The lymph nodes and palatine tonsils frequently appear immunologically reactive, and lymphadenitis and tonsillitis are occasionally present.
Swine.
B. bronchiseptica causes upper respiratory illness in young piglets, which leads to atrophic rhinitis (201, 274, 483). Very young piglets (3 to 4 days old) may experience bronchopneumonia. Hypoplasia occurs within the snout, with the ventral scroll of the ventral turbinate most often affected. It may be a slightly shrunken and distorted scroll, or, at the extreme, there may be a complete absence of the scroll. The dorsal scrolls of the ventral turbinate may also be involved in more severe cases.
Histologically there is hyperplasia of the epithelium with some metaplasia. The epithelium is more stratified with polyhedral cells which are devoid of cilia. There is some infiltration with neutrophils and mononuclear cells and fibroblastic proliferation in the lamina propria. The osseous core may be reduced in size and replaced with fibrous tissue. There is an increase in the osteoblasts number of around the trabeculae, and osteoclasts are rare.
Laboratory animals. (i) Guinea pigs.
Lesions include mucopurulent or catarrhal exudates in the upper respiratory tract and the tympanic bullae (23). Microscopically there is a suppurative bronchopneumonia with the loss of the pulmonary histologic architecture. Variable amounts of fibrinous exudate fill the terminal air passages.
(ii) Rabbits.
Suppurative bronchopneumonia with interstitial pneumonitis occurs. Histologically there may be peribronchial lymphocytic cuffing (23).
PATHOGENESIS AND IMMUNITY
There are four important steps relating to infection and disease due to bacterial pathogens in general and specifically to B. pertussis: (i) attachment, (ii) evasion of host defenses, (iii) local damage, and (iv) systemic manifestations (147, 174, 279, 346, 571, 577, 581, 641, 811). The Bordetella virulence determinants were discussed earlier in this review, and a summary of these factors is presented in Table 2.
Infection is initiated by the attachment of B. pertussis organisms to the cilia of epithelial cells of the upper respiratory tract (811). Various factors (FHA, FIM, PT, LPS, TcfA, BrkA, Vag8, and PRN) have been implicated in facilitating attachment (174, 418, 577, 641, 769, 811). Of note is the redundancy of protein adhesins that may contribute to the attachment process. As a consequence of this redundancy, individual adhesive functions are often masked, and it has been difficult to designate one protein as the primary adhesin. Various animal model systems and tissue culture systems give different results in regard to the importance of the various proteins in the attachment process. In vitro attachment assays with a variety of cell lines, however, establish FHA as a potent adhesin, at least under laboratory conditions.
Information from vaccine efficacy studies can also provide some indirect evidence for the role of a particular protein as an adhesin. For instance, a vaccine containing FIM2/3, PT, FHA, and PRN, which elicited a strong antibody response to FIM2/3 antigens, had significantly greater efficacy than a vaccine containing just PT, FHA, and PRN (597) (see the sections on DTP and DTaP vaccine efficacy, below). This observation suggests that FIM (either FIM2, FIM3, or both) may serve as adhesins and that antibodies directed against these antigens may block attachment of Bordetella to host cells via FIM. However, as presented in the section on fimbriae (see above), the beneficial effect of antibody to FIM2/3 could be due to the inhibition of another antigenic function.
While it has been suggested in several in vitro and in vivo studies that FHA is the major Bordetella adhesin, data relating to two recent vaccine efficacy trials suggest that in the presence of other adhesins FHA may not be necessary for attachment. For example, the former Lederle DTP vaccine (Tri-Immunol) contained a minimal amount of FHA and generated a minimal anti-FHA response, but it was more efficacious than the Lederle-Takeda DTaP vaccine (ACEL-IMMUNE), which contained a large amount of FHA and generated a vigorous antibody response to FHA (332, 334, 719). The most definitive data relating to the importance of PT, FHA, PRN, and FIM are presented in two studies of serologic correlates of immunity (148, 736). These two investigations were nested household contact studies within cohort vaccine efficacy trials in which vaccinees had received two-component (PT and FHA), four-component (PT, FHA, PRN, and FIM2), or five-component (PT, FHA, PRN, and FIM2/3) DTaP vaccines and two different DTP vaccines with markedly different immunogenic profiles. Both of these studies indicated that PRN was the most important vaccine antigen, and in one of the studies (148) the data suggested a synergistic relationship between PRN and PT. Interestingly, in both studies antibody to FHA did not contribute to protection. Supporting these observations is the fact that vaccines that contain PRN as well as PT and FHA have significantly greater efficacy than do vaccines containing PT alone or PT plus FHA (131, 149). However, in a study in which a PT toxoid vaccine was compared with a vaccine containing both PT and FHA, it was found that the two-component vaccine had significantly greater efficacy (3, 734, 735, 737). These findings suggest that in the absence of antibody to PRN (and perhaps FIM), antibody to FHA contributes to protection.
Collectively, the above data suggest that pertactin may serve as an important adhesin but that, in its absence, other proteins can carry out this function. In addition, there may be a synergistic relationship between PRN and high concentrations of PT (148).
Evasion of host defenses is facilitated by adenylate cyclase toxin (CyaA) and PT (147, 348, 577). Specifically, CyaA enters neutrophils and catalyzes the excessive production of cAMP, which intoxicates the cells such that phagocytosis is compromised. Like CyaA, PT also adversely affects phagocytosis and killing of organisms by inhibiting migration of lymphocytes and macrophages to areas of infection.
Local tissue damage of the ciliated epithelial cells may be due to TCT, DNT, and perhaps CyaA (147, 280, 581). Of these toxins, it is likely that TCT is most potent in this regard. The hallmark of B. pertussis infection is paroxysmal cough, and it seems likely that local tissue damage is responsible for this cough. However, the total duration of the cough in typical pertussis is longer than the period during which local damage would be expected to last. Therefore, it seems possible that there is another, unidentified toxin that contributes to the continued paroxysmal cough.
In contrast to many other severe bacterial diseases in which systemic manifestations are most important, B. pertussis infection is unique in that there are no direct physically evident systemic events. Encephalopathy occurs, but this most probably is a secondary event due to anoxia associated with coughing paroxysms (149). The most pronounced systemic laboratory manifestation is leukocytosis with lymphocytosis, which is due to PT. PT may also cause hyperinsulinemia, and this may manifest in some young infants as hypoglycemia (156, 712).
Some researchers have suggested that clinical pertussis is a PT-mediated disease (623, 624, 661, 662). Although this idea is still entertained by some, there is little evidence to support it. Contradicting this notion is the observation that paroxysmal cough, the main manifestation of pertussis, is clearly not due to PT. This opinon is based on the fact that human infections with B. parapertussishu, which does not express PT, also elicit an identical proxosymal cough (143, 149).
Another area of interest has been the effect of pertussis vaccines with active PT in the susceptibility of animals to other infections (575). These effects are discussed here even though they may be due to other biologically active components of whole-cell vaccines (LPS or CyaA) or to combinations of factors. While increased susceptibility has been observed in some model systems, increased resistance has occured in others (1, 12, 19, 45, 326, 423, 440, 575, 605, 823). Two investigators found that mice were more susceptible to fatal infections with Proteus vulgaris, Pasteurella multocida, Pseudomonas fluorescens, and Escherichia coli following immunization with pertussis vaccines than were unimmunized mice (12, 423). In another study, it was found that vaccinated mice had an increased susceptibility to influenza virus infection (605). In contrast, Landy found that B. pertussis LPS increased the resistance of mice to Salmonella enterica serovar Typhi (440). Bell and Munoz found that B. pertussis extracts increased the resistance of mice to rabies virus infection, and Winters et al. noted that pertussis vaccine rendered normally sensitive mice resistant to fatal adenovirus infections (575, 823). Pertussis vaccine was also found to increase the resistance in animals to Crytococcus and Candida infections, and B. pertussis LPS fragments were found to offer protection against encephalomyocarditis virus, Semliki Forest virus, and influenza A and B viral infections in mice (1, 19, 326).
In the first blinded controlled study in Sweden with acellular pertussis vaccines, four deaths were associated with invasive bacterial disease in the vaccine groups (3, 738). Both vaccines in this trial contained residual amounts of active PT. Because of the possibility of increased susceptibility to invasive bacterial infections relating to DTP immunization, one of us (J.D.C.) participated in two large case-control studies of two different populations (57, 194). In neither study was there evidence of an increased risk of invasive bacterial disease following DTP immunization (DTP vaccines contain both active PT and LPS), and in one of the studies there was an apparent decreased risk of invasive disease following immunization (57). In the other study, a second analysis looked at the occurrence of any illness in the period, before and after immunization. In this analysis there was no increase in the occurrence of infectious illnesses in the postimmunization period compared with the preimmunization period (194).
Following infection, antibodies develop to many B. pertussis antigens including PT, FHA, PRN, FIM2/3, CyaA, and LPS (149, 153, 346, 347, 490, 666, 757, 758, 767). Agglutinating antibodies (agglutinins) develop specifically to FIM2/3, PRN, and LPS. Neutralizing antibody to PT also develops. Using ELISA, the qualitative and quantitative differences between class-specific antibodies (IgA, IgE, IgG, and IgM) can be determined. In general, IgG and IgM antibodies, but not IgA antibodies, develop against vaccine antigens following primary immunization (146, 332, 579, 757, 821). Interestingly, persons who have been primed by infection respond to immunization with not just an IgG response but also an IgA response (446). Specific secretory IgA antibodies to the various B. pertussis antigens can be detected in nasopharyngeal secretions and saliva of previously infected persons (288, 843).
Infection with B. pertussis and immunization with DTP and DTaP vaccines clearly elicit protection of various degrees and durations against pertussis. The past literature suggested that immunity after B. pertussis infection was lifelong whereas vaccine-induced immunity was relatively short lived (137, 141, 146, 244, 439, 695). Extensive studies during the last 30 years document the limited duration of immunity following immunization, and additional careful review of old literature and the more recent study of pertussis in adults indicate that immunity following disease is also relatively short-lived. An analysis of surveillance data from the prevaccine era of reported pertussis would suggest that pertussis was a rarity in adults (141). However, the experts at the time clearly recognized that atypical pertussis was not uncommon in adults and that these illnesses were reinfections (141, 442, 478, 492).
More recently, studies in Germany (where pertussis was epidemic because pertussis immunization was not routinely carried out) found numerous cases of pertussis in adults. Interestingly, many of these adults had had pertussis during childhood (695, 828). One of us (J.D.C.) had the opportunity to observe and study pertussis in adults in the United States and also in Germany. In general, pertussis in German adults tended to be more typical and severe than cases observed in the United States. This suggested that vaccine-induced immunity was actually better than disease-induced immunity. Studies of IgG antibody to PT, FHA, PRN, FIM2, and agglutinins in similarly aged young adults in the United States and Germany found that the geometric mean titers (GMTs) in the Americans were two- to four-fold higher than those noted in the Germans (146). This suggested that priming by vaccine was better that priming by infection.
In addition to serum and secretory antibody responses following infection or immunization, cell-mediated immune responses to the various B. pertussis antigens occur regularly (16-18, 34, 60, 94, 451, 547-549, 679-681, 766, 845). Studies with the mouse respiratory infection model indicate that cellular immunity plays a major role in bacterial clearance and augments the effects of antibody by predominantly Th1 cell stimulation (547, 548). In humans a cellular immune response occurs shortly after the onset of a natural infection with B. pertussis (816). A Th1 response to PT, FHA, and PRN is preferentially induced. Immunization with a whole-cell pertussis vaccine also resulted in a Th1 response whereas the response to acellular pertussis vaccines was more heterogeneous, with the stimulation of both Th1 and Th2 cells. Several studies of murine and other rodent animal models also suggest a complementary role for humoral and cell-mediated immunity in protection against Bordetella infection (503, 547-549). Persistent memory T and B cells lead to anamnestic antibody responses, which are important in long-term immunity (485).
CLINICAL MANIFESTATIONS
B. pertussis
Several factors known to affect the clinical manifestations of B. pertussis include patient age, previous immunization or infection, presence of passively acquired antibody, and antibiotic treatment (149). Additional factors which may also play a role in clinical manifestations include the number of organisms at exposure, host genetic and acquired factors, and the genotype of the organism.
The incubation period is most commonly 7 to 10 days. However, it was noted that in the household setting, 22% of secondary cases occurred more than 28 days after the onset of illness in the primary case (334). This suggests either a more prolonged incubation time or a delay in exposure within the household.
Classic illness.
Classic illness most often occurs as a primary infection in unimmunized children (141, 147, 149, 155). The illness lasts 6 to 12 weeks or longer and has three stages: catarrhal, paroxysmal, and convalescent. Initially, in the catarrhal stage, there is rhinorrhea, lacrimation, and mild cough, similar to events which occur with rhinovirus infections. Over a 7- to 14-day period, the cough worsens in both frequency and degree. The temperature is normal or occasionally mildly elevated. The paroxysmal stage, which has its onset during the second week of illness, is characterized by repeated coughing fits with 5 to 10 or more forceful coughs during a single expiration (a paroxysm). At the end of a paroxysm, there is a massive inspiratory effort during which the classic whoop occurs. In conjunction with a paroxysm, cyanosis, bulging eyes, protrusion of the tongue, salivation, lacrimation, and distention of neck veins may occur. The paroxysms are associated with tenacious mucus, but the production of purulent sputum does not occur. Posttussive vomiting is common.
The paroxysmal episodes usually occur in groups, with multiple group episodes occurring every hour both night and day. Following a group of paroxysmal episodes, the children are exhausted and may appear apathetic. Weight loss may occur because of frequent vomiting and because of the refusal to eat by the child because he or she recognizes that eating often triggers paroxysms. Interestingly, between paroxysms the affected children may appear normal without any respiratory distress.
Common complications of classic pertussis include pneumonia, otitis media, seizures, and encephalopathy. The pneumonia may be a primary event in response to B. pertussis infection or may be due to a secondary infection with other pathogens. Seizures and encephalopathy are most probably due to cerebral hypoxia related to severe paroxysms. In association with paroxysms, interstitial or subcutaneous emphysema may result from rupture of alveoli. Other complications include subarachnoid and intraventricular hemorrhage, subdural and spinal epidural hematoma, ulcer or laceration of the frenulum of the tongue, epistaxis, melena, subconjuctival hemorrhage, rupture of the diaphragm, umbilical and inguinal hernia, rectal prolapse, apnea, rib fracture, severe alkalosis with associated tetanic seizures, and dehydration.
The paroxysmal stage lasts for 2 to 8 weeks and sometimes longer. The transition to the convalescent stage is gradual and is associated with an initial decrease in the frequency of the paroxysms and subsequently a decrease in the severity of the events as well. The convalescent stage usually lasts for 1 to 2 weeks but is occasionally prolonged.
It is important to note that children who have had classic pertussis often have a reccurrence of typical coughing paroxysms when they have respiratory viral infections. Most children with classic pertussis which resulted from a primary B. pertussis infection have an elevated white blood cell count with an absolute lymphocytosis. Unless there are complications as noted above, the physical examination in pertussis is normal except for the coughing episodes. Neither fever nor pharyngitis is typical of pertussis.
Mild illness and asymptomatic infection.
In household contact studies, asymptomatic infections in family members are common (203, 474, 475). In one study, 52 (46%) of 114 household contacts who remained well and 23 (43%) of 53 of those with mild respiratory illnesses (rhinorrhea, tearing, sneezing, conjunctivitis, fever, hoarseness, sore throat, or cough of <2 weeks' duration) had laboratory evidence of B. pertussis infection (203). Most of the silent infections or mild respiratory illnesses noted above occurred in previously vaccinated children and adults or in adults who had previously had B. pertussis infections. In another recent study, 21 (5.3%) of 399 apparently healthy infants who were controls in the study had evidence of B. pertussis infection by PCR assay (335). Follow-up information was available for 15 of these subjects; 4 had cough illnesses, and 11 remained asymptomatic.
In addition to asymptomatic infections and trivial respiratory infections as noted above, a substantial number of both unvaccinated and previously vaccinated children have mild cases of pertussis (333, 336, 337, 693, 719). In one study it was noted that 47% of 247 subjects had cough illnesses which lasted ≤28 days (333). A continuation of the above study involved 2592 culture-positive, previously unvaccinated children; of these children, 38% had cough illnesses of ≤28 days and in 17% had cough illnesses of ≤21 days (336). In another study, in which PCR as well as culture was used diagnostically, it was found that 32% of the subjects had cough illnesses which lasted ≤4 weeks (693). Of this group, however, the majority (57%) had paroxysmal coughing; 32% also had whoops.
Infants.
Most deaths due to B. pertussis infection occur in infants, and severe morbidity is most common in this age group (35, 44, 112, 136, 147, 156, 185, 186, 270, 335, 338, 339, 360, 510, 512, 537, 583, 588, 619, 630, 669, 670, 712, 751, 790). In the United States from 1997 through 2000, there were 7,203 cases of reported pertussis in infants younger than 6 months of age. Of this group, 63.1% were hospitalized, 11.8% had pneumonia, 1.4% had seizures, 0.2% had encephalopathy, and 0.8% died. In the 6- to 11-month age group, 28.1% were hospitalized, 8.6% had pneumonia, 0.7% had seizures, 0.1% had encephalopathy, and <0.1% died (112).
The source of infection in infants is frequently an adolescent or adult family member (35, 56, 186, 200). In a recent study of 616 infants with pertussis, the source was identified in 264 cases (43%) (56). Of this group, mothers were the source of 32% of infections and another family member was the source in 43%. Of the source persons, 20% were 10 to 19 years of age and 56% were adults.
Neonatal infection is particularly severe, with up to a 3% risk of death (44, 156, 165, 360, 512). The initial finding is frequently apnea, and although the babies cough, their cough is so faint that it often goes unrecognized. Seizures due to hypoxia resulting from apnea are common. Severe pulmonary hypertension, the cause of which is unknown, is a frequent cause of death (510, 630, 790). In young infants, the severity of disease and risk of death correlates directly with the white blood cell count and in particular the number of lymphocytes (44, 156, 338, 512, 537). White blood cell counts in the range of 30,000 to >100,000 cells/ml are common. Coinfections with adenoviruses or respiratory syncytial virus are relatively frequent (44, 186, 459, 712). Other risk factors for fatal disease in young infants are premature birth and the presence of pneumonia (537, 790).
The relationship between B. pertussis infection and sudden infant death syndrome (SIDS) is interesting but far from clear. In a study done more than 20 years ago, it was found that infant deaths due to B. pertussis infection were often misdiagnosed as respiratory viral infections (136). Similarly, in another study of the same population it was observed that many deaths attributed to SIDS were in fact related to B. pertussis infection (588). In a more recent study, Heininger et al. found evidence of B. pertussis DNA in nasopharyngeal swabs from 9 (18%) of 51 infants who had experienced sudden unexpected deaths (339). As a follow-up to this study, a carefully controlled study was performed in which specimens for PCR assay were collected from 254 infants who had experienced sudden unexpected deaths and from 441 matched controls (335). The rate of PCR positivity was 5.1% in the sudden-death cases and 5.3% in the controls. The high rate of infection in the controls was a surprise but does not negate the possibility that the B. pertussis infections in the SIDS cases may have contributed to the fatalities.
Adults.
During the last two decades, a number of studies have indicated that B. pertussis infections in adolescents and adults are common (55, 200, 271, 354, 390, 397, 534, 550, 586, 634, 665, 675, 695, 739, 759, 788, 828, 835). There has also been an increase in the number reported cases of pertussis in adolescents and adults in concert with these studies (112, 135, 199, 232, 309, 702, 710, 838). All adults and most adolescents who have B. pertussis infections have had a previous B. pertussis infection, have been vaccinated, or both (146, 200, 206). Previous infection or previous immunization tends to modify illness in adults. Nevertheless, adolescents and adults can have symptomatic infection, mild disease, or classic pertussis. The experience of one of us (J.D.C.) and the results of several studies suggest that adults who were primed by previous infection (as opposed to priming by immunization) are more likely to have typical pertussis.
In a U.S. study of 27 adolescents and adults, the following clinical findings were noted: (i) the median duration of cough was 42 days, with a range from 27 to 66 days; (ii) all subjects had paroxysmal cough; (iii) 26% of the subjects had whooping; (iv) 56% had post-tussive vomiting; and (v) 100% had post-tussive gagging (739). In another study, the attending doctors failed to diagnose pertussis in 31 university students who showed laboratory evidence of Bordetella infection (550). Instead, their diagnoses included upper respiratory tract infection (39%), bronchitis (48%), and others (16%). In this group of patients with pertussis, the median duration of cough illness prior to being seen was 21 days; 94% of patients had one or more coughing episodes per hour, and 90% of the coughing fits had a staccato or paroxysmal quality. Only two findings in this study differentiated patients with Bordetella infection from those with cough illnesses without evidence of Bordetella infection. Patients with pertussis were less likely to have a productive cough (3% versus 21%) and were less likely to have an antibiotic prescribed at the time of the visit (39% versus 64%). In contrast to the two U.S. studies, the findings in two German studies noted more typical illness (634, 695). It should be noted that most of the German adults had not been immunized during childhood whereas most of the adolescents and adults in the U.S. studies had.
In a household contact study in Germany relating to a pediatric vaccine efficiency trial, there were 79 adults with laboratory-confirmed B. pertussis infections (634). Of this group, 80% coughed for ≥3 weeks and in 63% the cough was paroxysmal, 53% had post-tussive choking or vomiting. Complications included pneumonia, rib fracture, inguinal hernia, and severe weight loss. Unique sweating episodes were noted in 5% of the ill subjects (634).
In another adult study in conjunction with a cohort vaccine efficiency trial in children, 64 laboratory-confirmed cases were noted (695). Of this group, 70% had paroxysms, 38% had whooping, 66% had post-tussive phlegm, and 17% had post-tussive vomiting. In adults, fainting may occur in association with coughing fits (205).
B. parapertussishu
B. parapertussis infection in humans can cause unrecognized infection, mild pertussis, or classic pertussis (51, 222, 314, 330, 340, 363, 444, 465, 468, 498, 499, 545). B. parapertussishu was first isolated in the United States and during the first half of the 20th century was studied in Michigan, New York, and California, as well as in Denmark (222, 445, 545). After that, little attention was paid to B. parapertussishu in the United States and Europe until the end of the century. At this time, in conjunction with vaccine efficacy trials, extensive studies comparing illness due to B. pertussis with that due to B. parapertussishu have been performed in Sweden, Italy, and Germany (51, 340, 465, 498, 499). In addition, a similar non-vaccine-related study was carried out in Finland (330).
In the first of these studies, illnesses in 38 children with B. parapertussishu infections were compared with B. pertussis illnesses in 76 children matched by sex, season, and age (340). Comparative findings (B. pertussis versus B. parapertussishu) showed the following: cough for >4 weeks, 57% versus 37% (P = 0.06); whooping, 80% versus 59% (P = 0.07); whooping for >2 weeks, 26% versus 18% (P = 0.05); paroxysms, 90% versus 83% (P = 0.5); fever (temperature ≥ 38°C), 9% versus 0%; post-tussive vomiting, 47% versus 42%; and mean leukocyte and lymphocyte counts, 12,500/mm3 and 7,600/mm3 versus 7,800/mm3 and 3,500/mm3 (P < 0.0001), respectively.
In a study in Italy, Mastrantonia et al. identified 76 children with B. parapertussishu infections and found that in this group, 100% had cough, 76% had paroxysms, 33% had whooping, 42% had post-tussive vomiting, 29% had apnea, and 12% had cyanosis (499). With the exception of the frequency of paroxysms, the frequency of the other manifestations were all less common than those noted in children with B. pertussis infections. Similar findings were noted in a study in Munich, Germany, where illnesses in 64 children with B. parapertussishu infections were compared with B. pertussis illnesses in 116 children (465).
The results in some older studies have been less conclusive. This is probably because concomitant infections with B. pertussis and B. parapertussishu are fairly common and difficult to interpret (363, 389, 535).
B. bronchiseptica
B. bronchiseptica causes respiratory infections in many different mammals including mice, rats, guinea pigs, skunks, opossums, rabbits, raccoons, cats, dogs, ferrets, foxes, pigs, hedgehogs, sheep, koalas, leopards, horses, lesser bushbabies, and occasionally humans (283). The most important and best described natural infections are in dogs and pigs. Infections in laboratory animals have also provided a wealth of information for understanding B. bronchiseptica pathogenesis (23, 48, 83, 93, 199, 201, 224, 275, 283, 409, 427, 509, 511, 646, 671, 713, 794, 834).
Swine.
In pigs, infection with B. bronchiseptica may be asymptomatic or may be associated with upper respiratory tract disease characterized by sneezing and coughing (275). This is followed by a deformity of the bony structures of the nose (atrophic rhinitis). Disease in pigs usually occurs during infancy. Most cases occur in animals that are 3 to 8 weeks of age, but animals that are slightly older (11 to 13 weeks of age) may also develop turbinate atrophy. Pigs with atrophic rhinitis have a shortening of the upper jaw and a twisting of the snout to one side. In some very young pigs the turbinate damage may not persist due to regeneration of the bone.
Dogs.
Infectious tracheobronchitis of dogs (kennel cough) is a highly contagious respiratory disease (427). The illness may be mild with only a dry hacking cough or severe with a paroxysmal dry or mucoid cough, accompanied by ocular and nasal discharge. Dogs with severe disease frequently have pneumonia. Post-tussive retching and vomiting occur (283). The illness lasts 1 to 3 weeks, and deaths due to pneumonia are not uncommon.
Laboratory animals.
Outbreaks of respiratory disease have occurred in animals in commercial facilities which produce animals for research (283). Illness can vary from nasal discharge, sneezing, loss of appetite, and weight loss (rabbit catarrh) to bronchopneumonia and septicemia (93, 646, 713).
Humans.
In 1991, Woolfrey and Moody reviewed human illnesses associated with B. bronchiseptica infections (831). Subsequently there have been many additional case reports, and these have most recently been summarized by Ner et al. (587). In 1910 McGowan studied 13 laboratory workers exposed to various animals with B. bronchiseptica infections (511). While all of these workers had nasal symptoms, B. bronchiseptica was isolated from only one of them. This worker constantly handled rabbits and guinea pigs and had severe chronic nasal symptoms (catarrh) over an 18-month period. The illness was intractable and had acute exacerbations. During an exacerbation, a pure culture of B. bronchiseptica was grown from “a mass of muco-pus hanging down over the soft palate.” In 1926 Brown described a mild pertussis-like illness in a 5-year-old girl whose illness commenced about 10 to 12 days after she had been given a rabbit with mild “snuffles” (79). B. bronchiseptica was isolated from this child as well as from the rabbit.
In the review by Woolfrey and Moody (831), they described an analysis of the results in 23 papers as well as two of their own experiences (77, 79, 82, 88, 125, 126, 191, 241, 262, 267, 400, 405, 431, 432, 604, 714, 733, 822). Of this group of 25 patients, 56% had a compromising factor and all but 3 (12%) had a known exposure to animals. A recent paper by Ner et al. (587) notes 20 additional reports and presents a detailed description of six patients (43, 65, 129, 154, 188, 202, 212, 227, 261, 282, 476, 477, 613, 614, 650, 748, 786, 797, 824, 847). Over half of the recent cases of B. bronchiseptica illness have involved human immunodeficiency virus-infected patients. In one report of nine patients, all had had at least one AIDS-defining condition before the B. bronchiseptica infection (212). Pneumonia usually occurs in AIDS patients as well as in other immunocompromised patients and is frequently cavitary. Disseminated infections are known to occur. Other respiratory manifestations include sinusitis and bronchitis.
Normal children exposed to farm animals or pets usually have pertussis-like illnesses.
B. holmesii
B. holmesii was identified as a Bordetella sp. in 1995 and was initially noted as a cause of septicemia (814). Subsequent studies noted further septicemic illnesses as well as respiratory infections (294, 467, 508, 560, 591, 678, 752, 839). Of particular interest were the results of studies of persons with pertussis-like illnesses in Massachusetts from 1995 through 1998 (839). The investigators isolated B. holmesii from nasopharyngeal specimens from 33 patients suspected of having pertussis. Of the 23 patients with available clinical data, 100% had cough, 61% had paroxysms, 26% had post-tussive vomiting, and 9% had whooping.
DIAGNOSIS
Differential Diagnosis of Bordetella Infections
Infections in humans.
In classic pertussis, the clinical diagnosis should be made without difficulty based on the paroxysomal cough with post-tussive vomiting and whooping, absolute lymphocytosis, and lack of significant fever (149). However, the etiologic diagnosis of illness due to B. pertussis versus B. parapertussishu requires definitive laboratory study. Many other infectious agents cause illnesses with cough that can be confused with Bordetella infections. Most important in this regard are Mycoplasma pneumoniae, Chlamydia pneumoniae, adenoviruses, and other respiratory viruses (33, 136, 147, 161, 166, 196, 314, 584, 829). In addition, spasmodic attacks of coughing may be observed in children with bronchiolitis, bacterial pneumonia, cystic fibrosis, or tuberculosis. The cough associated with sinusitis can also be confused with that caused by Bordetella spp., as can the cough associated with an airway foreign body.
Infection in animals.
In dogs and laboratory animals, the clinical manifestations of B. bronchiseptica are the same as those associated with tracheobronchitis. There are many viral and bacterial causes of tracheobronchitis, so that in isolated cases, laboratory study is necessary to diagnose B. bronchiseptica infection. In general, the same is true for the early stages of illness in pigs.
Specific Diagnosis of B. pertussis Infections
An excellent, detailed account of the laboratory diagnosis of Bordetella infections is presented by Loeffelhalz in the eighth edition of the Manual of Clinical Microbiology (473).
Many practical problems markedly affect the sensitivity and specificity of the laboratory diagnosis of pertussis. These include delay in specimen collection, poor specimen collection technique, specimen transport problems, laboratory medium, problems, laboratory inexperience, laboratory contamination, equipment expense, and the conventional need for two serum samples for serologic diagnosis. In addition, there may also be confusion in the interpretation of serologic results.
The sensitivity and specificity of the laboratory diagnosis of B. pertussis infection can equal those for many other bacterial infections, with the proper performance of culture, PCR, and ELISA to measure increases in IgG and IgA antibody titers to PT in paired serum samples.
Access to diagnostic or laboratory methods is a major problem in both developed and developing countries. In developed countries, in which pertussis is apparently well controlled by immunization, few laboratories are equipped for the routine diagnosis of B. pertussis infection. Few laboratories maintain fresh culture media for diagnosis, and kits for specimen collection and transport are not routinely available. B. pertussis serologic testing using acceptable techniques is rarely available. Commercial laboratories provide an array of B. pertussis ELISA techniques, but, in general, there is no evidence of sensitivity or specificity related to serum specimens from patients. Furthermore, PCR is not routinely available.
In developing countries, laboratory services and resources vary markedly from country to country. However, the facilities for the routine culture of B. pertussis are frequently more readily available and laboratory workers are more knowledgeable than in many developed countries, in which pertussis is controlled. Routine serologic diagnostic services and PCR are generally not available.
There is currently no evidence of failure to detect new B. pertussis variants by culture, PCR, or serologic testing. The experience throughout the vaccine era suggests that pertussis variants are unlikely to be a future problem. Surveillance studies using pulsed-field gel electrophoresis are likely to be useful in identifying variant strains that would affect PCR and/or serologic diagnoses (306).
Laboratory techniques for the determination of B. pertussis infections have existed for over 90 years. A specific medium for the culture of B. pertussis was described in 1906 (63), and the demonstration of serum agglutinating antibody for diagnosis was noted in 1916 (635). In the present era, the extensive acellular pertussis vaccine efficacy trials and other epidemiological studies have made it possible to evaluate multiple methods for the laboratory diagnosis of B. pertussis infections (229, 293, 310, 315, 317, 337, 493, 536, 693, 719, 722, 740, 781). Common laboratory diagnostic methods currently include culture, direct antigen detection (direct fluorescent-antibody [DFA] test) PCR, and serologic demonstration (ELISA with many B. pertussis antigens and agglutination) by measuring rises in titer or high single serum values. Factors such as past exposure to the bacterium, age, antibiotic administration, immunization, timing of specimens, and laboratory sophistication can affect the sensitivity and specificity of the individual tests. The greatest sensitivity is obtained when culture is supplemented by PCR and serologic testing.
Culture of B. pertussis.
B. pertussis is a fastidious small (0.2- by 0.7-μm), faintly staining, gram-negative coccobacillus. Suboptimal culture results can occur because of inadequate specimen collection and transport, as well as poor laboratory methods. Methods for specimen collection, transport and culture have been well described (272, 273, 276, 359, 418, 473, 572, 827).
(i) Specimen collection.
B. pertussis colonizes the ciliated epithelial cells in the upper and lower respiratory tracts. Therefore, a specimen for culture should be obtained from the surface of respiratory ciliated epithelial cells of the upper respiratory tract. Specimens obtained from the throat, sputum, or anterior nose, which are not lined with ciliated epithelium, are not adequate (495).
Two methods have been used successfully in the collection of specimens; these are nasopharyngeal swab and nasopharyngeal aspiration. In young children, nasal wash specimens may also be satisfactory; however, dilution may be a problem, and the method has not been adequately evaluated in the diagnosis of B. pertussis infection (313). For nasopharyngeal swabs, cotton and rayon should not be used because they contain fatty acids that are toxic to B. pertussis. Calcium alginate is the preferred swab material, although Dacron is acceptable. The swab shaft should be a fine, flexible wire.
The correct use of a nasopharyngeal swab is an unpleasant experience for the patient, and this unpleasantness can lead to suboptimal specimen collection. For optimal results, the tip of the swab must come into contact with the ciliated cells of the respiratory epithelium. Failure to achieve this is a major cause of negative cultures. Although there are data suggesting that nasopharyngeal aspiration leads to a higher isolation rate of B. pertussis, this method is generally less practical in the clinical setting.
(ii) Specimen transport.
Immediate culture of a specimen is preferred but is not always practical in the clinical setting (367). For successful transport, the transport medium must prevent the loss of B. pertussis and inhibit the growth of other organisms that obscure the identification of B. pertussis. The transport medium of choice is Regan-Lowe agar (half-strength charcoal agar supplemented with horse blood and cephalexin), a nutritive medium that inhibits the growth of the normal nasopharyngeal flora. Preincubation of this medium at 36°C overnight before shipment of the specimen may increase the yield of B. pertussis but may also result in a greater growth rate of other bacterial or fungal contaminants. Nonnutritive bacteriological transport media, such as Ames medium, can be used if they contain charcoal and the period between specimen collection and culture is less than 24 h.
(iii) Culture.
Methods for culture are well described (272, 273, 359, 362, 418, 473, 572). Although many types of culture medium have allowed the successful isolation of B. pertussis from clinical specimens, charcoal agar (Regan-Lowe agar) supplemented with 10% horse blood and cephalexin (40 mg/liter) is currently the medium of choice (572). In situations when culture plates are inoculated directly without transport, it is also advisable to inoculate an enrichment medium and then replate following 48 h of incubation. Satisfactory enrichment media include Regan-Lowe transport medium and Stainer-Scholte broth.
Although Bordet-Gengou agar is frequently used for culture, the need for this medium to be freshly made makes it less practical than charcoal agar (which has an 8-week shelf life) in most laboratories. Since cephalexin inhibits some B. pertussis strains, some laboratories inoculate specimens onto charcoal agar both with and without this antibiotic. Agar plates are incubated at 35 to 36°C in high-humidity ambient air. B. pertussis is catalase and oxidase positive and urease negative and is identified by specific antiserum via agglutination or fluorescence. Cultures are usually examined daily for 7 days. However, Katzko et al. found that an increased yield of positive results occurred if they held the cultures for an additional 5 days (406).
The main reasons for failure of bacterial growth in culture from correctly collected and transported specimens are bacterial and fungal contamination and the lack of fresh media.
(iv) DFA testing of nasopharyngeal secretions.
The use of DFA for the rapid diagnosis of B. pertussis and B. parapertussishuinfections has been recently reviewed (572). This method has been used for 40 years because it is rapid and inexpensive and can provide a positive result when cultures are negative due to antibiotic use. However, DFA is an insensitive method since it does not employ amplification and lacks specificity because of cross-reactions with members of the normal nasopharyngeal flora (229). As noted by Loeffelholz, commercially available antibodies are polyclonal (Becton Dickinson) or monoclonal, identifying a lipooligosaccharide eptiope (Accu-Mab; Altachem Pharma, Edmonton, Alberta, Canada) (473). Both products have similar low sensitivity compared with culture, but the Canadian product appears to have greater specificity (518, 572). False-positive results with polyclonal antibodies are due to several organisms of the oral and nasopharyngeal flora including unencapsulated Haemophilus influenzae, diphtherioids, and anaerobic or facultatively anaerobic bacterial species (229).
(v) Detection of B. pertussis by PCR.
The use of PCR has made the rapid diagnosis of many infectious diseases possible, and its use in the diagnosis of pertussis infection is rapidly evolving (6, 81, 229, 337, 463, 520, 572, 652, 653, 693, 781). Key factors for the successful application of PCR in the diagnosis of infection by Bordetella spp. involve sample collection and preparation, primer selection and amplification conditions, detection, and internal and external positive and negative controls. Aspects of these factors have been summarized by Müller et al. (572).
Calcium alginate swabs should not be used for PCR specimens because of inhibitory factors present in the fiber, and aspirate specimens need to be treated with a mucolytic agent to remove PCR-inhibiting substances. The use of a Dacron swab with a fine, flexible wire shaft is recommended. Following swabbing, the swab should be shaken vigorously in 0.4 ml of sterile 0.9% saline solution in a vial, the swab should be discarded, and the vial should be sealed (693). Primers have been derived from four chromosomal regions: (i) the promoter region of the genes encoding PT, (ii) a DNA region upstream of the poron gene, (iii) repeated insertion sequences, and (iv) the adenylate cyclase toxin gene, cyaA. All except cyaA primers are specific for B. pertussis. Common primers include IS481, which detects both B. pertussis and B. holmesii; IS1001, which detects both B. parapertussis and B. holmesii; and PTp1 and PTp2, which amplify a 191-bp DNA fragment from the PT promoter region and is B. pertussis specific (158, 210, 229, 234, 373, 572, 627, 651-653, 693, 756).
A number of detection systems have been used that differ considerably in expense and sensitivity. During the last 15 years, a number of PCR assays have been evaluated by comparing results with culture and clinically typical pertussis. Overall, this diagnostic tool has the advantage of a much higher sensitivity compared with conventional culture. In a prospective study, in which swabs for PCR and culture were obtained simultaneously from 555 individuals with cough illness, the use of PCR increased the identification of B. pertussis infections by almost fourfold, from 28 to 111 (693). In a similar but larger study, Schmidt-Schläpfer et al. (694) found a 2.6-fold increase in the detection of B. pertussis by PCR compared with culture. Only a few studies have been reported in which the sensitivity and specificity of PCR in the diagnosis of B. pertussis infection were determined by comparison with serologically identified cases (337, 463, 466, 652, 781). In one recent study, PCR results were compared with serologic diagnoses, and PCR had a sensitivity of 61% and a specificity of 88% (337). Similar findings have been observed in other studies. False-positive results are a potential problem associated with PCR in the diagnosis of pertussis and other respiratory illnesses (6, 520, 572). False-positive results can occur if specimens for PCR are opened in the pertussis laboratory before going to the PCR laboratory (J. Cherry, unpublished data). In addition, they can occur as a result of contamination of the air in a room where DTP immunization is carried out (754).
(vi) Serologic diagnosis of B. pertussis infection.
Natural infection with B. pertussis is followed by an increase in the concentrations in serum of IgA, IgG, and IgM antibodies to specific antigens as well as to preparations of the whole organism (255, 289, 293, 310, 490, 519, 536, 572, 601, 719, 826). Prior to the development of ELISA techniques, the main serologic test for the diagnosis of pertussis was the demonstration of a fourfold increase in agglutinating-antibody titer. The antibodies measured in this test are directed against FIM2/3, PRN, and LPS. Experience suggests that this test had reasonably good specificity but lacked sensitivity. The mainstay of the serologic diagnosis of pertussis during the last 15 years has been ELISA, using specific B. pertussis proteins as antigens. Standardized techniques have been developed, and antibodies are quantitated by the reference line computer programme and reference sera from the Center for Biologics Evaluation and Research, U.S. Food and Drug Administration. The precision of the test is such that intra-assay coefficients of variation have been reduced to <10%, which makes a twofold increase in titer significant.
In contrast to natural infection, the primary immunization of children induces mainly IgM and IgG antibodies. Serologic diagnosis of pertussis may be suspected by the demonstration of an increase in agglutinin titer or the use of ELISA, showing an increase in IgA or IgG antibody titer to PT, FHA, PRN, FIM, or to sonicated whole organisms in two serum samples collected 2 to 4 weeks apart. It is now clear that antibody responses to FHA and PRN also occur following other Bordetella infections, so that isolated increases in titers of antibody against these antigens are not specific for B. pertussis infection. In addition, high titers of antibody to FHA may be the result of cross-reacting epitopes of nonencapsulated H. influenzae, M. pneumoniae, C. pneumoniae, and perhaps other bacteria. Some culture-positive patients, particularly children younger than 3 months, fail to develop measurable antibodies.
The primary problem in the serologic diagnosis of B. pertussis infection by ELISA is the delay in obtaining the acute-phase specimen. In patients with reinfections, a rapid increase in titer occurs, so that with a delayed acute-phase sample, the titer is likely to have already peaked and further titer increases between the acute-phase and convalescent-phase sera may not be observed. However, for those not recently immunized, this problem can be circumvented by using single-serum ELISA. Specifically, patients with illness will have ELISA titers that are significantly higher than GMT, of sera from well controls (493, 550).
The greatest sensitivity and specificity for the serological diagnosis of B. pertussis infection is achieved by ELISA and measurement of IgG and IgA antibodies to PT. A significant rise in titer (greater than or equal to twofold) between acute-phase and convalescent-phase sera needs to be demonstrated. In adolescents and adults, single high values of IgG or IgA antibodies to PT also indicate infection. Although IgA antibody to PT is more indicative of a recent antibody response, it is less consistent than a PT IgG response (781). The younger the child, the less consistent the IgA antibody response. Simondon et al. (707) noted that a significant fall in titer is also diagnostic of infection.
Specific Diagnosis of Other Bordetella Infections
The same transport and culture methods used for B. pertussis can be used for other Bordetella subspecies. In addition, the other subspecies are generally less fastidious and grow on blood and MacConkey agars (473). B. holmesii and B. bronchiseptica are inhibited by cephalexin, and so the isolation of these organisms will be missed if Regan-Lowe transport medium is used and if cephalexin is used in the culture media. The use of methicillin or oxacillin in place of cephalexin should allow the growth of B. holmesii and B. bronchiseptica (508, 831).
B. parapertussis, B. bronchiseptica, and B. holmesii can all be identified in respiratory secretions by PCR (158, 210, 234, 627, 651, 652, 756, 787). Several methods, involving different primers and organism-specific oligonucleotide probes or restriction enzyme cleavage patterns, have been developed for routine laboratory testing.
TREATMENT
A number of antibiotics have in vitro activity against B. pertussis (33, 39-41, 52, 361, 364-366). The mainstay of treatment over the last 30 years has been oral erythromycin. Erythromycin administration during the catarrhal stage of illness shortens the duration of symptoms and eliminates the organism from the upper respiratory tract within 5 days of initiation of therapy in most instances (41, 52, 308). Since untreated patients with pertussis are contagious for 2 to 4 weeks or more, erythromycin treatment significantly shortens the period of individual contagiousness. Initiation of erythromycin treatment after the paroxysmal stage has begun is generally thought not to benefit the patient in regard to either duration or severity of illness. However, in one small open randomized study, the children who were treated with erythromycin developed significantly fewer whoops than did children in the control group, even though most had reached the paroxysmal state at the time of onset of treatment (52). In addition, it was the feeling of one of us (J.D.C.), based on studies of German children, that treatment early in the paroxysmal phase of illness was also beneficial (333). The dose for pediatric patients is 40 to 50 mg/kg/day given every 6 h for 14 days. In 1997 the findings in a relatively large study suggested that a 7-day course of treatment with erythromycin was as effective as a 14-day course (316). Although uncommon, the use of erythromycin in neonates has been associated with the occurrence of hypertrophic pyloric stenosis (357). To our knowledge, the dose for adults has never been adequately studied, but 1 to 2 g/day given every 6 h has been used. It is the opinion of one of us (J.D.C.) that the lower dose (1 g/day) is not optimal; the gastrointestinal side effects of erythromycin in adults, even with the lower dose, make it a less than an optimal choice (139).
During the last decade, three B. pertussis isolates have been found to be resistant to erythromycin (429, 449, 459). Of these three erythromycin-resistant B. pertussis strains, two were studied for resistance to trimethoprim-sulfamethoxazole and found to be sensitive. It is likely that erythromycin-resistant strains are also resistant to other macrolides, but this was demonstrated for only one of the isolates (459). At present, there is no evidence of an emerging erythromycin resistance pattern in B. pertussis isolates (361, 429) and there is no evidence to suggest that resistant strains are contributing to the increase in reported pertussis in recent years. However, since PCR is now being used in many laboratories for the diagnosis of B. pertussis illness, the possibility of missing resistant strains is a possible problem. Since B. pertussis is likely to be sensitive to trimethoprim-sulfamethoxazole, this agent can be used in children who cannot tolerate erythromycin or in situations of demonstrated resistance (365).
The newer macrolides (azithromycin and clarithromycin) are also effective for the treatment of pertussis (11, 20, 441, 448, 497, 617). Although the dose and duration of treatment with these two macrolides have not been well studied, we suggest the following based on the available data: azithromycin at 10 mg/kg on day 1 and 5 mg/kg on days 2 to 5 as a single dose for 5 days for children and 500 mg on day 1 and 250 mg on days 2 to 5 for adults; clarithromycin at 15 to 20 mg/kg/day in two divided doses for 7 days for children and 1 g/day in two doses for 7 days for adults.
Humans infected with B. parapertussishu or B. holmesii should also respond to the macrolide therapy indicated above. In contrast, however, B. bronchiseptica is usually resistant to erythromycin (831). Most B. bronchiseptica strains are sensitive to aminoglycosides, extended-spectrum third-generation penicillins, tetracyclines, quinolones, and trimethoprim-sulfamethoxazole. Therefore, for outpatient management, children can be treated orally with trimethoprim-sulfamethoxazole and adults can be treated with the same drug or a tetracycline or quinolone.
VACCINATION AND PREVENTION
B. pertussis Vaccines
Since pertussis was such a severe disease with high mortality, attempts to create vaccines for both treatment and prevention were made soon after B. pertussis was first isolated (136, 147, 216, 442, 481, 482). The initial vaccines consisted of killed whole B. pertussis organisms. Early on, it was recognized that the production of serum antibodies and clinical protection in vaccine recipients correlated directly with the number of organisms in the vaccine. It was also realized at this time that clinical toxicity also correlated directly with the number of organisms in the vaccine.
In the 1930s, many candidate pertussis vaccines were developed and used for the treatment and prevention of pertussis in limited studies. These initial vaccines were prepared by many different methods; the products included whole-cell vaccines that contained culture media, whole cells that were washed, mixed vaccines that contained other bacteria from the upper respiratory tract flora as well as B. pertussis cells, fractionated vaccines (extracted vaccines), “detoxified vaccines,” and vaccine enriched with “toxic factors.” In his book, Lapin reviewed 29 studies of a number of candidate vaccines which were performed between 1933 and 1942 (442). It was recognized during early vaccine development that alterations in the conditions of culture, such as the use of human blood rather than horse blood, resulted in products that were less reactogenic but contained larger numbers of bacterial cells.
In the mid-1940s, Kendrick et al. (416) developed a laboratory test which could be used to predict vaccine efficacy. Prior to this time, efficacy could be determined only in human trials. This test (the mouse potency test) employed intraperitoneal vaccination of young mice with dilutions of test vaccine and a standard vaccine. The animals were challenged 14 to 17 days later by the intracerebral inoculation of 100,000 live bacteria. Potency was determined by comparing survival in the two vaccine groups at 14 days. A World Health Organization potency unit was established such that vaccines were required to contain greater than 4 international units (IU) per dose and the immunization dose was three doses (12 IU) (833). In the United States, the potency of DTP vaccines is based on the number of protective units in 1.5 ml of a specific vaccine lot (159). The vaccine must have an approximate minimum potency of 12 units per 1.5 ml. This is based on either a single test estimate of no less than 8 units or a 2, 3, 4 test geometric mean estimate of no less than 9.6, 10.8, or 12 units, respectively. The maximum allowed potency is 36 units per 1.5 ml.
Vaccines standardized by the mouse potency test were extensively evaluated in trials conducted by the British Medical Research Council after World War II, and the results of these studies validated the mouse potency test as a surrogate for vaccine efficacy (523-525). The toxicity of whole-cell vaccines was evaluated using the mouse weight gain test.
Beginning in the mid-1940s, routine immunizations of children with pertussis vaccines was started in the United States, and this continued until the replacement of whole-cell vaccines with acellular pertussis vaccine in the late 1990s (136, 147, 149, 410-417). Initial vaccines were monocomponent whole-cell pertussis vaccines, but by 1947 combination vaccines with diphtheria and tetanus toxoids (DTP) were available and recommended. During the 1950s, other countries also started performing routine pertussis immunization. In the early years, reactogenicity of pertussis vaccines and the temporal association of immunization with catastrophic neurologic events and deaths created major problems for many national programs. As a result, vaccine manufacturers tried to make their vaccines “safer.” These attempts in the United States had some successes, but one vaccine was later shown to have poor efficacy (293, 310). In Sweden, where there was great concern about “vaccine encephalopathy,” the vaccine was changed and by 1979 was found to be ineffective; its use was therefore discontinued (670).
From 1962 until 1977, a DTP vaccine with an extracted pertussis component (TriSlogan; Eli Lilly Co.) was available in the United States (147, 167, 807). This crude DTaP vaccine was prepared by chemical extraction from whole bacteria, and the cellular debris was removed by centrifugation. This vaccine was extensively used because it was thought to be less reactogenic, but few data support this assumption.
At present, DTP vaccines are still routinely used in the developing world and many developed countries, whereas DTP vaccines with acellular pertussis components (DTaP vaccines) have replaced DTP vaccines in many developed countries.
Whole-cell DTP vaccines. (i) Reactogenicity.
The reactogenicity of DTP vaccines has been extensively evaluated by one of us (J.D.C.) in numerous research papers, chapters, and reviews (26-28, 30, 130, 133, 136, 137, 140, 142, 143, 145, 147, 149, 160, 236, 346, 458). Only a brief summary of these analyses and related studies is presented here.
From January 1978 to December 1979, a study involving 15,752 doses of DTP and 784 doses of DT was carried out in the Los Angeles area (26-32, 160). Children in this study were evaluated for reactions that occurred within 48 h of vaccination. In general, all common local and systemic reactions were more common in DTP recipients that in DT recipients. Redness, swelling, and pain at the injection occurred in 37.4, 40.7, and 50.9%, respectively, of DTP recipients but in only 7.6, 7.6, and 9.9%, respectively, of DT recipients. The percentage of these reactions in DTP vaccinees increased from the first dose to the fifth dose. Fever (≥38°C) occurred in 46.5% of DTP recipients and in only 9.3% of DT recipients. Over the first four doses, the rate of fever increased from 39.6 to 54.2%. Drowsiness, fretfulness, vomiting, anorexia, and persistent crying were all more common in DTP vaccinees than in DT recipients. With the exception of anorexia, these systemic reactions decreased in frequency from the first to the fifth DTP doses. The overall rates for these systemic events in DTP vaccinees were as follows: drowsiness, 31.5%; fretfulness, 53.4%; vomiting, 6.2%; anorexia, 20.9%; and persistent crying, 3.1%.
Other more notable events in DTP vaccinees in this study, which were not frequent enough to compare statistically with similar events in DT recipients, were the following: high-pitched, unusual cry, 0.1%; convulsions, 0.06%; and hypotonic-hyporesponsive episodes (shock, collapse), 0.06%. However, none of the DT vaccinees had similar events.
Throughout the entire pertussis vaccine era, there has been concern about the temporally related occurrence of severe neurologic disease and death and DTP vaccination (4, 5, 9, 22, 25, 42, 47, 50, 54, 80, 86, 87, 95, 106, 108, 110, 130, 133, 136, 140, 142, 143, 145, 147, 178, 195, 207, 209, 213, 214, 223, 233, 236, 237, 258, 259, 281, 295, 297-301, 312, 318, 320, 323, 345, 351-353, 355, 358, 368, 376, 379, 382, 398, 399, 408, 428, 435, 480, 488, 526, 538-543, 559, 566, 568, 570, 628, 629, 637, 706, 712, 716, 720, 721, 723-729, 741, 742, 744, 755, 760, 795, 796). Over 70 years ago, Madsen (481) noted the deaths of two newborns shortly after receiving pertussis immunization, and in 1948, Byers and Moll reported a series of 15 patients in whom severe neurologic disease had its onset after immunization (87). By 1979, more than 1,000 patients with neurologic damage in association with pertussis immunization had been reported (160). In these initial case reports and small studies, no data were available to allow rate calculations and comparison with unvaccinated subjects. In addition, alternative causes for the neurologic events were rarely studied.
During the period from 1967 to 1980, population studies were undertaken to determine the frequency of neurologic events following pertussis vaccination. None of these studies were controlled, however, so that all rate estimates included children with temporally related neurologic disease that may have been caused by other factors. The first well done study, and the most definitive to date, was a prospective case-control study (National Childhood Encephalopathy Study [NCES]) that evaluated all hospital admissions of children from 2 to 36 months of age with acute serious neurologic illnesses (9). This study occurred in England, Wales, and Scotland between 1976 and 1979. The results of this study have been analyzed and reanalyzed on multiple occasions and, in our opinion, present conclusive evidence against a causal relationship between DTP immunization and brain damage.
The initial results of the NCES noted a statistically significant association between pertussis immunization and neurologic illness. Hospitalized patients with acute neurologic illness were about twice as likely to have been vaccinated with a pertussis vaccine during the week before the event than were the controls for the matching period. However, the causal inference based on this study must be questioned because when the period is increased from 7 days to 1 month preceding the event onset or the comparable period in the controls, the frequency of pertussis immunization is the same (140, 142). This indicates that the DTP immunization called attention to or brought out an event that was to occur anyway but was moved forward in time.
A further analysis of the NCES which was restricted to infants with infantile spasms (an identifiable seizure disorder of infancy) failed to find a statistical association between pertussis immunization and the event (47). Finally, an analysis of the NCES data with the exclusion of infantile spasm cases was interpreted by the investigators to indicate a cause-and-effect relationship. Specifically, it was suggested that the risk of permanent brain damage following pertussis immunization was 1 per 330,000 vaccine doses and the risk of any encephalopathy following immunizations was 1 per 140,000 vaccinations (539-541). However, as demonstrated by Stephenson (723) and MacRae (480), both of these estimates are incorrect. In regard to any encephalopathy, the risk estimate is an artifact due to the inclusion of nine children with febrile convulsions. In regard to the increase risk of brain damage, it is noted that vaccinees and controls had the same rate of pertussis immunization during the 1-month period, indicating a redistribution of events over time and not a cause-and-effect relationship.
During a period of extensive study of neurologic events temporally related to pertussis immunization, it became apparent that what was being called pertussis vaccine encephalopathy was not an encephalitis-like event but instead was the first seizure or seizures of infantile epilepsy. During the late 1980s, four carefully performed studies were carried out in the United States and Denmark (142, 259, 296, 706, 795). Collectively in these studies about 1 million pertussis immunizations were evaluated to see if they were a causative factor in epilepsy. No evidence of a causative relationship was found. Finally, a 10-year active surveillance study (1993 to 2002) in Canada found no evidence of encephalopathy following >6.5 million doses of pertussis vaccines (559). To summarize, it is our opinion that there is no such entity as “pertussis vaccine encephalopathy.”
SIDS has its peak age of occurrence at about 10 weeks of age, and since the first dose of DTP in the United States is administered to infants at 2 months of age the temporal association of immunization and the occurrence of SIDS was to be expected. However, in the late 1970s and 1980s there was considerable media coverage which inferred a cause-and-effect relationship (178). The impetus for this view followed the occurrence of a time cluster of four deaths due to SIDS in Tennessee in 1974 which occurred within 24 h after DTP vaccination (107). This was extensively studied by the Centers for Disease Control and Prevention (CDC), and a weak statistical association with one lot of a DTP vaccine was noted. However, the data from this study were carefully evaluated by the investigators and a panel of outside consultants, who concluded that there was no causal relationship between the specific vaccine lot and the SIDS cases.
During the same period, two retrospective studies of limited populations suggested that DTP immunization may have been causally related to SIDS (25, 760). However, it was noted that there was considerable bias in these investigations (568). At the same time, a case-control study in Sheffield, England, found no association between DTP immunization and SIDS (755). One further relatively small study in the state of Washington was thought by the authors to indicate a causal relationship between DTP and SIDS (796). However, the sample was small, there were only four cases within 3 days of immunization, and the authors deleted nonimmunized SIDS victims and their controls in the analysis process.
Three large controlled studies present convincing data against a cause-and-effect relationship between DTP immunization and SIDS (295, 355, 716). The first of these investigations was conducted in Norway over an 8-year period (716). The investigators compared the observed dates of SIDS occurrence in 222 infants with the expected frequency distribution of SIDS and found no evidence indicating that DTP immunization was a causative factor. The second study was a large case-control study in the United States, involving 800 cases (355). In this study the SIDS victims were less likely to have received DTP immunization than the controls in the comparative periods. This negative association between DTP immunization and SIDS was noted in the Washington state study, the study in Norway, and a recent analysis from a German investigation (335). The third large study which failed to show a cause-and-effect relationship between DTP immunization and SIDS was carried out in Tennessee and involved a cohort of 129,834 children who were born in four urban Tennessee counties during the period from 1974 through 1984 (295). In this large cohort there was no increased risk of SIDS after DTP immunization compared with a period distant from immunization. In summary, it is clear to us that DTP immunization is not a causative factor in SIDS.
(ii) Vaccine efficacy.
The use of whole-cell pertussis vaccines and whole-cell pertussis component DTP vaccines has clearly been highly efficacious (136, 147, 149). In the prevaccine era, the average yearly rate of reported pertussis in the United States was 157 per 100,000 population. Following the routine immunization of children, this rate had fallen to <1 per 100,000 population in the 1970s. Of interest, however, is that no formal efficacy trials were ever carried out in the United States on any individual DTP vaccines that were used during the last 50 years.
In 1987, Fine and Clarkson reviewed the literature for efficacy data and found 43 papers dating from 1923 to 1983 (245). These studies were carried out mainly in the United Kingdom and the United States, but data from Denmark, Sweden, Hungary, New Zealand, and Japan were also noted. In the United States, four household contact studies and one case-control study were reported for the periods between 1979 and 1983 (78, 109, 111). The reported efficacy in these investigations varied from 64 to 96%. The highest efficacy estimate was noted in the case-control study. These were all CDC studies, and during the periods studied, vaccines from four different manufacturers (Wyeth, Lederle, Connaught, and Parke-Davis) were in use.
From mid-1982 to mid-1983, Blennow et al. carried out a nonblinded but prospective cohort study involving 1,140 infants in Sweden (58). In this trial, 525 infants received three doses of a plain whole-cell vaccine (Pertussis Vaccine Wellcome; Wellcome) licensed in the United Kingdom and 615 unvaccinated infants served as controls. The subsequent attack rate was 1.5% (8 of 525) among vaccinated children and 7.6% (47 of 615) among the controls (P < 0.001). The vaccine efficacy was 80% (95% confidence interval [CI] = 58 to 90). The vaccine efficacy was 93% (95% CI = 72 to 98) in preventing pertussis with a cough duration of 4 weeks or more.
A more definitive CDC study of DTP vaccine efficacy was carried out from 1984 through 1986 in three urban areas (Baltimore, Md.; Denver, Colo.; and Milwaukee, Wis.) of the United States (602). A total of 347 children aged 1 through 4 years were exposed in the household to a primary case. To be included in the study, a household had to have a culture or serologically confirmed case or an illness that met the Council of State and Territorial Epidemiologists case definition for endemic pertussis (≥14 days of cough and either vomiting, whooping, or paroxysms). In this study, efficacy was calculated by using many different case definitions and by using all households and households with laboratory-confirmed cases. In addition, efficacy rates were examined by the number of vaccine doses and severity of disease in primary cases and in household contacts. The efficacy varied from a low of 59% (95% CI = 24 to 78) to a high of 97% (95% CI = 86 to 99). In general, and as expected, the calculated efficacy increased directly with increased duration of cough and the addition of paroxysms and whooping to the case definition. When any cough illness was considered, the efficacy was 64% (95% CI = 49 to 75).
Vaccine efficacy correlated directly with the number of vaccine doses the vaccinee received. It was 18% for one DTP dose, 48% for two DTP doses, 58% for three DTP doses, and 68% for four or more DTP doses.
A Los Angeles household contact study was carried out between July 1987 and October 1990 (200). In this study, immunization data were available for 103 household contacts who were 15 years of age or younger. Efficacy values were 37% (95% CI = 21 to 50) for any respiratory illness; 66% (95% CI = 49 to 77) for clinical pertussis (a cough illness lasting for at least 2 weeks with paroxysms, whooping, or post-tussive vomiting and without another apparent cause); and 89% (95% CI = 73 to 95) for laboratory-confirmed pertussis. At the time of this study, the only DTP vaccines available were those manufactured by Lederle and Connaught.
The most definitive studies of vaccine efficacy occurred between 1990 and 1995 in six vaccine efficacy trials in four countries in which various DTaP vaccines were evaluated and DTP vaccines were used as comparative controls (293, 310, 334, 464, 697, 708, 719). These trials (which are discussed more completely below in the section on DTaP vaccine efficacy) included three cohort trials, two household contact studies, and one case-control study. The DTP vaccines were all licensed vaccines produced by Connaught and; Lederle (United States), Pasteur Mérieux Sérums and Vaccines (France), SmithKlineBeecham Biologicals (Belgium), and Behringwerke (Germany). The subjects in all studies received three doses of vaccine at about 2, 4 and 6 months of age, and in two studies a fourth dose was administered in the second year of life.
As noted in Table 3, all vaccines except the Connaught vaccine had excellent efficacy values. The Connaught values are surprisingly low and hard to reconcile with the values in the U.S. studies presented above, since the Connaught vaccine enjoyed widespread use in the United States during these study periods. However, in the 1980s because of concerns relating to vaccine reactions, manufacturers tried variations in production techniques to make their whole-cell vaccines less reactogenic. In this venture, Lederle was able to reduce the cell count in their vaccine but nevertheless retain potency. We assume, without any proof, that Connaught also made attempts to produce a less reactogenic vaccine. We do know, however, that the Connaught DTP vaccine used in a Tennessee study in 1988 to 1989 elicited good antibody responses to PT, FHA, PRN, and FIM in 16 vaccinated infants whereas the Connaught DTP vaccine used in the vaccine efficacy trials in Sweden and Italy in 1992 produced only minimal responses to PT, FHA, and PRN (24, 293, 310).
TABLE 3.
Efficacy of DTP vaccines in six trials conducted in four countries from 1990 to 1995
| Study location (reference) | Vaccine manufacturer | % Efficacy againsta:
|
|
|---|---|---|---|
| Mild and typical pertussis | Typical pertussis | ||
| Senegal (708) | Pasteur Mérieux Sérums et Vaccins | 92 (86-99) | |
| Sweden (310) | Connaught USA | 41 (30-51) | 48 (37-58) |
| Italy (293) | Connaught USA | 23 (1-40) | 36 (14-52) |
| Germany (719) | Lederle | 83 (76-88) | 93 (89-96) |
| Germany (697) | Behringwerke AG or SmithKline Beecham Biologicals | 81 (68-89) | 89 (77-95) |
| Germany (464) | Behringwerke AG | 96 (71-100) | |
95% CI is given in parentheses.
Acellular pertussis component DTP vaccines.
Some of the candidate vaccines reviewed by Lapin in 1943 were crude DTaP vaccines (442). In addition, a DTP vaccine with an extracted (fluid) pertussis component (TriSlogen) was available in the United States from 1962 to 1977 (147). This vaccine enjoyed considerable use even though its content was never determined and its efficacy was never formally studied. As technology became available in the 1970s, it was noted that PT, FHA, and LPS were liberated into liquid medium during culture (147, 149, 346, 688). These antigens could be concentrated and separated by density gradient centrifugation. Although there was limited knowledge at the time about the function and importance of various B. pertussis antigens, it was thought early on that toxoided PT was the most important antigen to be included in an acellular vaccine and that LPS was a major cause of vaccine reactions and therefore should be removed (623, 688).
Sato et al. in Japan were the first to describe the production of aceilular pertussis component vaccines which contained known components in identifiable quantities (688). Following Sato's lead, DTaP vaccines were developed by six manufacturers in Japan and, because of epidemic pertussis, were put into immediate routine use in Japan in 1981 (151, 422, 592). Use of these vaccines during the last 23 years has significantly controlled epidemic pertussis in Japan.
The use of first-generation Japanese-made DTaP vaccines was limited to Japan because adequate efficacy, immunogenicity, and reactogenicity data were not available on any single vaccine or on vaccine use in early infancy. However, the successes in Japan stimulated extensive studies and trials in Japan, United States, Europe, and Africa, which were carried out over a 15-year period from 1980 to 1995. Immunogenicity and reactogenicity studies were carried out on all candidate acellular pertussis vaccines and DTaP vaccines. Subsequently, nine definitive efficacy trials were carried out with 11 different vaccines.
(i) Reactogenicity.
To meet regulatory requirements, numerous phase II and III studies with candidate DTaP vaccines have been carried out. Since all DTaP vaccines do not contain LPS, or contain only trace amounts, it is not surprising that all DTaP vaccines are, in general, less reactogenic than whole-cell DTP vaccines. The most definitive study of common vaccine reactions was a National Institute of Allergy and Infectious Diseases (NIAID)-sponsored study which was carried out in the six NIAID-supported Vaccine Treatment Evaluation Units (VTEU) located in five geographic regions of the United States (198). In this study, the reactogenicity of 13 candidate DTaP vaccines given as the primary series at 2, 4, and 6 months of age was evaluated. There were 2,200 subjects who received one of the 13 candidate DTaP vaccines or a DTP control vaccine following a double-blind protocol. Between 113 and 217 infants received three doses of one of the 13 DTaP products, and 370 infants received the comparative DTP vaccine. The results of this study were presented in detail in a supplement to Pediatrics (197). Of the 13 candidate vaccines, 7 were later evaluated in phase III efficacy trials. Two additional vaccines which were not evaluated in the NIAID study were also evaluated in efficacy trials. The composition of the seven vaccines noted above as well as the two additional vaccines not studied are presented in Table 4. As can be seen, there is considerable variation among the vaccines in the number of B. pertussis antigens and their amounts, the amount of adjuvant (aluminum), and the amounts of diphtheria and tetanus toxoids.
TABLE 4.
Composition of nine DTaP vaccines evaluated in efficacy trialsa
| Vaccineb | Amt of B. pertussis antigens (μg/dose)
|
Amt. of aluminum (mg/dose) | Preservative | Flocculationc
|
||||
|---|---|---|---|---|---|---|---|---|
| PT | FHA | PRN | FIM | Diphtheria toxoid | Tetanus toxoid | |||
| Certivad | 40 | 0.50 | Thimerosal | 25 | 7 | |||
| Tripediad | 23.4 | 23.4 | 0.17 | Thimerosal | 6.7 | 5 | ||
| PM-2e | 25 | 25 | 0.30 | Thimerosal | 15 | 5 | ||
| SKB-2e | 25 | 25 | 0.50 | Phenoxyethanol | 25 | 10 | ||
| Acelluvax | 5 | 2.5 | 2.5 | 0.35 | Thimerosal | 25 | 10 | |
| Infanrixd | 25 | 25 | 8 | 0.50 | Phenoxyethanol | 25 | 10 | |
| ACEL-IMMUNEd | 3.5 | 35 | 2 | 0.8f | 0.23 | Thimerosal | 9 | 5 |
| DAPTACELd | 10 | 5 | 3 | 5g | 0.33 | Phenoxyethanol | 15 | 5 |
| Daptacel-like (enhanced) | 20 | 20 | 3 | 5g | 0.33 | Phenoxyethanol | 15 | 5 |
In the overall study of the 13 candidate vaccines, local reactions (redness, swelling, and pain), fever, fussiness, drowsiness, anorexia, and the use of antipyretics were all more frequently detected in DTP recipients than in DTaP vaccinees (Table 5) (198). The rate of vomiting was similar in DTaP and DTP vaccine recipients. Over the course of the three-dose series, the frequency of fever, redness, and swelling increased whereas that of drowsiness decreased in DTaP vaccine recipients.
TABLE 5.
Percentage of DTaP- and DTP-vaccinated infants reported to have local or systemic reactions within 3 days of immunizationa
| Category | % of infants with reaction to:
|
|
|---|---|---|
| DTaPb | DTPc | |
| Systemic | ||
| Fever (temp > 100°F) | ||
| First dose | 4.2 | 27.3 |
| Second dose | 11.3 | 34.1 |
| Third dose | 15.8 | 37.7 |
| Antipyretic use | ||
| First dose | 39.3 | 60.5 |
| Second dose | 36.7 | 59.8 |
| Third dose | 36.3 | 61.4 |
| Fussiness | ||
| First dose | 6.6 | 20.6 |
| Second dose | 7.7 | 23.5 |
| Third dose | 6.7 | 17.3 |
| Drowsy | ||
| First dose | 29.9 | 43.5 |
| Second dose | 17.6 | 31.0 |
| Third dose | 12.9 | 24.6 |
| Anorexia | ||
| First dose | 9.3 | 19.5 |
| Second dose | 8.9 | 16.5 |
| Third dose | 8.9 | 14.3 |
| Vomiting | ||
| First dose | 6.3 | 7.0 |
| Second dose | 4.5 | 4.5 |
| Third dose | 4.2 | 5.3 |
| Local (injection site) | ||
| Redness | ||
| First dose | 13.5 | 49.4 |
| Second dose | 17.1 | 47.7 |
| Third dose | 21.5 | 47.6 |
| Swelling | ||
| First dose | 8.7 | 39.7 |
| Second dose | 12.1 | 34.1 |
| Third dose | 13.3 | 35.7 |
| Pain | ||
| First dose | 3.8 | 27.3 |
| Second dose | 2.0 | 18.7 |
| Third dose | 2.1 | 15.8 |
There were only minor differences between some of the reaction categories among the seven DTaP vaccines that were later evaluated in efficacy trials. In general, the two vaccines with the smallest amounts of diphtheria toxoid (ACEL-IMMUNE and Tripedia) were less likely to be associated with fever, redness, or swelling after the third dose than were the other five vaccines with greater amounts of this toxoid.
A subsequent study evaluated reaction rates for the same 13 vaccines following a fourth dose at 15 to 20 months of age (615). Overall, when rates in DTP recipients were compared with the collective rates in DTaP vaccinees, it was found that DTP recipients had a greater frequency of irritability and injection site redness, swelling, and pain. When the reaction rates in recipients of the seven DTaP vaccines that were used in efficacy trials were compared, there were considerable differences. Similar to the findings after the third dose, the two vaccines with the smaller amounts of diphtheria toxoid (ACEL-IMMUNE and Tripedia) were also less likely to be associated with fever, irritability, and redness, swelling, and pain at the injection site after the fourth dose. They were also less likely to be associated with severe irritability or marked (>50-mm diameter area) redness at the injection site.
In the NIAID study, it was noted that 20 children had entire thigh swelling in the leg where the fourth dose of a DTaP vaccine was injected (656). This reaction was noted to have a significant linear association with the amount of diphtheria toxoid in the DTaP vaccine, and it was not observed after receipt of either ACEL-IMMUNE or Tripedia, the two vaccines with the smaller amounts of diphtheria toxoid. Also, lesser degrees of swelling (>50 mm but less than the entire limb) correlated with the vaccine PT content after dose 4 and the aluminum content after dose 5.
In several additional studies, a high frequency of relatively large reactions (redness and swelling) at the injection site were noted following four and five doses of DTaP vaccines (278, 616, 692, 696, 711, 764). In all these studies except one, the DTaP vaccines contained either 15 or 25 limits of flocculation (Lf) of diphtheria toxoid. Interestingly, the NIAID VTEU study results indicate that vaccines with high concentrations of both PT and diphtheria toxoid were the most likely to cause redness and swelling of >50 mm in diameter. The three vaccines with the lowest rates of redness and swelling of >50 mm in diameter were Tripedia, Acelluvax, and ACEL-IMMUNE.
The efficacy trials carried out in the early 1990s allowed the gathering of data relating to less common and more clinically significant vaccine-associated events (157, 293, 310, 331, 464, 768, 772). Overall, persistent crying, temperature of ≥40.5°C, hypotonic-hyporesponsive episodes, and convulsions were all less frequent during the primary series following DTaP immunization than following DTP immunization. For example, the likelihood of persistent crying for ≥3 h, temperature of ≥40.5°C, hypotonic- hyporesponsive episodes, and seizures in the Italian trial was, respectively, 7, 7, 17, and 6 times more likely following DTP immunization than following one of the two DTaP vaccines (157). Similar findings were noted in the Stockholm (Sweden) trial, except that the occurrence of convulsions was similar in DTP and DTaP recipients. In the Erlangen (Germany) trial, the likelihood of persistent inconsolable crying, temperature of ≥40.5°C, and convulsions were four, three, and four times more common, respectively, in DTP recipients than in DTaP vaccinees (772). Only one child in this trial, a DTP recipient, had a hypotonic-hyporesponsive episode. It is clear from the above that true but infrequent severe reactions following DTP immunization (persistent crying, temperature of ≥40.5°C, hypotonic-hyporesponsive episodes, and the induction of febrile convulsions in children prone to febrile convulsions) are significantly reduced in infants following immunization with DTaP vaccines.
(ii) Vaccine efficacy.
As noted above, the first DTaP vaccines were developed at the Japanese National Institutes of Health in the late 1970s (151, 592, 688). First-generation DTaP vaccines produced by six companies were put into routine use in Japan in 1981 despite the lack of proof of efficacy of any of the six vaccines (149). Subsequently, six small household contact studies were published, and the calculated efficacy varied from 78 to 92% (592). However, in none of the studies were vaccines from a single manufacturer evaluated. Later, one household contact study carried out by multiple investigators evaluated a single vaccine (the Takeda vaccine) (569). In this study, efficacy against all infections was 81% and efficacy against typical infections was 98%. In retrospect, all of these studies had significant problems relating to the method of diagnosis, the method of case ascertainment, and observer bias. However, the biggest problem was that no vaccinated infants were studied; immunization was instituted after the second birthday.
Since adequate data were not available on any single vaccine or on vaccine use in infancy, a prospective double-blind study was carried out in Sweden in the mid-1980s (3). In this trial, which was supported by NIAID, two acellular pertussis vaccines were studied. A control group received a placebo, but no whole-cell pertussis vaccine control was used in the trial. For reasons which are not entirely clear today, the 2-, 4-, 6-month primary immunization schedule was not followed. Rather, two doses of vaccine were administered. The first dose was given to infants 5 to 11 months of age, and the second dose followed the first by 7 to 13 weeks. One vaccine (JNIH-7) was a PT toxoid (6 μg of protein nitrogen per dose), and the other vaccine contained toxoided PT and FHA (3.75 μg of protein nitrogen per dose for each antigen). Depending on the case definition, the efficacy of the PT toxoid varied from a high of 54% (95% CI = 26 to 72) to a low of 32% (95% CI = 6 to 51). The efficacy of the two-component PT toxoid/FHA vaccine varied from a high of 69% (95% CI = 47 to 82) and a low of 45% (95% CI = 22 to 62).
Three further analyses of data from this trial were subsequently published (735-737). These included household contact substudy data, cases diagnosed serologically, and analyses using many different clinical case definitions. As might be expected, the calculated efficacy increased when the case definition required paroxysmal cough of a long duration as well as laboratory confirmation.
Since (i) no whole-cell pertussis vaccine had been included in the initial trial in Sweden, (ii) the efficacies of the PT toxoid and the PT toxoid/FHA vaccines were lower than expected, and (iii) there were still no efficacy data relating to the first year of life, a number of trials with seven of the vaccines evaluated for immunogenicity and reactogenicity in the NIAID VTEU study as well as two additional candidate vaccines were planned and carried out in the early 1990s. These vaccines and their contents are listed in Table 4. Because of the confusion related to the variation of efficacy depending on the case definition, it was felt by leading investigators that a universal case definition should be developed. With this goal, a World Health Organization (WHO) committee met in January 1991 in Geneva (832). Resulting from this meeting was the WHO primary case definition. This definition or a slight variation of it was used in six of the eight subsequent efficacy trials which were carried out. The WHO case definition required an illness with ≥21 days of spasmodic cough and either culture-confirmed B. pertussis infection or serologic evidence of infection as indicated by a significant rise in IgA or IgG ELISA antibody against PT or FHA in paired sera or, as an alternative, contact with a case of culture-confirmed pertussis in the vaccinee's household with onset within 28 days before or after the onset of the cough illness in the study subject.
Not all members of the WHO committee, including one of us (J.D.C.), agreed with this primary case definition (131, 149). A definition which discarded bona fide cases seemed illogical at the time, and this is even more apparent today. With this definition, vaccines that lessen the severity of disease but do not prevent disease will have calculated efficacies similar to those of much better vaccines that prevent mild disease as well as typical disease.
As an example of how illogical the WHO case definition was, one need only look at data from the original Swedish trial (3, 735-737). In recipients of JNIH-7 vaccine (the PT toxoid), there were 23 culture-confirmed cases with 1 day or more of coughing spasms. When ≥21 days of coughing spasms is required for the definition of a case, there were only 12 cases; 48% of the cases have been removed from the data set. Similarly with JNIH-6 PT/FHA vaccine recipients, 4 (29%) of 14 cases are removed from the data set by the more rigorous definition. There were 39 placebo recipients with spasmodic cough for ≥1 day with culture confirmation. When ≥21 days of spasmodic cough is required, 4 cases (10%) are removed from the data set.
Prior to the onset of the different efficacy trials, there was considerable concern relating to the study methodology. It was felt by many that reliable data could be obtained only in trials which were cohort in nature and completely double-blinded and that both placebo and DTP controls were included. This of course was a major ethical problem in countries where DTP vaccines were available and their use was recommended. In the end, only two trials (Stockholm no. 1 and Italy) followed this format (293, 310). In Sweden the Göteborg trial was double-blinded but there was no DTP vaccine control and the schedule of immunization was 3, 5, and 12 months rather than 2, 4, and 6 months (preferred for comparing efficacy with other studies) (768). The second, later Stockholm study was double-blinded but did not contain a placebo arm (597). In addition, in this trial two different vaccination schedules were employed (2, 4, and 6 months and 3, 5, and 12 months).
In Germany, three trials were carried out and all were faced with the problem that a double-blinded control group (given DT vaccine) was not ethical (334, 464, 697, 719). However, since at the time the majority of children were not being vaccinated, it was relatively easy to obtain DT controls. Because of the fear of DTP vaccines in Germany, it was difficult to perform a cohort study with double-blind administration of DTP or DTaP. Therefore, only one of the three German studies (Erlangen) was a cohort study with a double-blinded comparison of DTP and DTaP and an unblinded DT group (719). The Mainz study was a household contact study in which primary cases in households in six areas of Germany were identified and prospective follow-up of young children in the families was carried out (697).
The Munich study was a case-control study in which controls were selected randomly from records in the offices of participating physicians (464). Major weaknesses of this study were that it was a case-control evaluation (which inflates efficacy) and that laboratory diagnosis did not include serologic testing (245). In both the Munich and Erlangen trials, the vaccinees received a fourth dose of vaccine in the second year of life.
Since the use of a DT control group was clearly not ethical, the Senegal trial initially was a double-blind study in which a DTP vaccine was compared with the candidate DTaP vaccine (708). Subsequently, a household contact analysis was added so that cases in unvaccinated children could be compared with cases in vaccinees.
In the study in which one of us (J.D.C.) was the co-principal investigator in Erlangen, Germany, Wyeth-Lederle made a considerable effort in correcting for the biases of the unblinded DT group. However, there was no evidence that use of the unblinded DT group led to an artificial increase in efficacy. In fact, as noted in the substudy household contact analysis, the attack rate in DT subjects was lower than expected due to the use of prophylactic macrolides (334).
In the course of the Erlangen study, it became apparent to one of us (J.D.C.) that the most significant bias in all efficacy trials, including double-blind placebo-controlled trials, was observer bias (150). Specifically, if vaccines make disease less typical but do not prevent illness, then if the observers (such as parents and physicians) “know pertussis” and initiate study only if they think the illness is pertussis, atypical cases will be missed and efficacy will be inflated. This type of bias can be reduced if the vaccinees are monitored regularly by scheduled phone calls and all children with cough illnesses lasting >7 days are evaluated. In this regard, the Erlangen protocol was the most satisfactory of all the cohort trials since telephone calls were made every 2 weeks. In Italy, scheduled telephone calls were made monthly, and in Stocklholm no. 1, scheduled calls were made every 6 to 8 weeks (293, 310). Apparently, scheduled telephone calls were not made in the Götenburg trial (719, 768).
A measure of this type of observed bias can be made in the trials in which efficacy data for mild as well as typical disease were presented. Specifically, for DT recipients about 18 to 25% more cases are expected if mild and typical cases are compared with just typical cases (333, 336). In Italy, Erlangen, Stockholm no. 1, and Götenburg, differences of 20, 18, 12, and 4%, respectively, were noted (149, 293, 310, 768). This indicates that observer bias was greatest in the Götenburg trial and least in Erlangen and Italy.
A summary of the efficacy data from the seven trials conducted in the early 1990s is presented in Table 6. In general, three- and four- or five-component vaccines (vaccines that contain PRN and FIM as well as PT and FHA) have greater efficacy against both mild and typical pertussis than do PT or PT-plus-FHA vaccines.
TABLE 6.
Vaccine efficacy data for eight acellular pertussis vaccines evaluated in seven trials carried out in the 1990s
| Location (reference) | Design | Vaccine used | Schedule | % Efficacy
|
|
|---|---|---|---|---|---|
| Typical pertussis | Mild and typical pertussis | ||||
| Sweden (Göteborg)a (768) | Double-blind prospective cohort | Certiva | 3 doses (3, 5, 12 mo) | 71 | 54 |
| Sweden (Stockholm)a (310) | Double-blind prospective cohort | SKB-2 | 3 doses (2, 4, 6 mo) | 59 | 42 |
| Daptacel | 85 | 78 | |||
| Italy (Rome) (293) | Double-blind prospective cohort | Acelluvax | 3 doses (2, 4, 6 mo) | 84 | 71 |
| Infanrix | 84 | 71 | |||
| Germany (Erlangen) (719) | Prospective cohort | ACEL-IMMUNE | 4 doses (3, 4, 5, 6, 15-18 mo) | 83 | 72 |
| Germany (Mainz) (697) | Household contact | Infanrix | 3 doses (3, 4, 5 mo) | 89 | 81 |
| Germany (Munich)a,b (464) | Case control | Tripedia | 4 doses (2, 4, 6, 15-25 mo) | 80, 93 | |
| Senegalc (708) | Household contact | Triavax | 3 doses | 74 | 31 |
Significant observer bias occurred in this trial.
Laboratory diagnosis based on culture only; 80% efficacy was against cough illness of 21 or more days, and 93% efficacy was against the WHO case definition.
The 31% efficacy was based on 21 days or more of cough illness; 74% efficacy was against the WHO case definition.
The final study, done in Sweden, was a comparative but blinded study without a DT control group (597). In a head-to-head comparison, the enhanced Daptacel-like vaccine had similar efficacy to that of the effective DTP vaccine used in the United Kingdom and was significantly more efficacious than the three-component Acelluvax vaccine. In the same trial, Acelluvax was more efficacious than the two-component SKB-2 vaccine.
B. bronchiseptica Vaccines
Dogs (kennel cough).
A number of kennel cough vaccines are available in the United States and recently the American Animal Hospital Association Canine Vaccine Task Force 2003 presented recommendations (23, 89a; Intra-Trac II Product Insert [http://medi-vet.com/IntraTracII.aspx]). The following vaccines are among those available: killed whole-cell B. bronchiseptica (KWC Bb), live avirulent Bb (LABb), LABb/live attenuated parainfluenza virus (LAPV), and LABb/LAPV/live attenuated adenovirus type 2 (CAV-2). The KWC Bb vaccine is given to puppies at 6 to 8 and 10 to 12 weeks of age and then annually. Initial immunization of older animals is two doses 4 weeks apart. The LABb/LAPV can be given at 3 weeks of age with a second dose 3 weeks later and then administered annually. The LAPV/LABb/CAV-2 vaccine is given at >8 weeks of age and is followed by annual single doses. Controlled data for vaccine efficacies are not available.
Swine (atrophic rhinitis).
A number of atrophic rhinitis vaccines are available (23, 201, 484). These include killed or nonpathogenic strains of B. bronchiseptica with various preparations of Pasteurella multocida. No efficacy data are available. Recommendations stress vaccination of sows prior to delivery, and of piglets shortly after birth and again at 3 to 4 months of age.
EPIDEMIOLOGY: IMPLICATIONS FOR THE CONTROL OF HUMAN INFECTIONS
B. pertussis Epidemiology
There is much confusion today relating to the epidemiology of pertussis. The main cause of this confusion is the failure to recognize that there are major differences in the dynamics of reported pertussis compared to the dynamics of B. pertussis infection (132). For practical purposes, there are two vastly different epidemiologies. The first is the epidemiology of reported clinical pertussis and, the second is the epidemiology of B. pertussis infection. These are considered separately below.
Observed (reported pertussis). (i) Incidence.
In the United States in the prevaccine era, the average yearly incidence of reported pertussis was 157 cases per 100,000 population (136). In England and Wales in the prevaccine era, the average yearly incidence of reported pertussis was 230 per 100,000 population. It was realized at the time that only 18% of cases were reported in the United States, suggesting that the actual rate was in the range of 872 cases per 100,000 population. In the prevaccine era, pertussis was an ever-present disease and in addition there were epidemic cycles every 2 to 5 years (on average about every 3 years). In the United States, the average interval between epidemic peaks in the prevaccine era (1922 to 1942) was similar to that in the early vaccine era (1962 to 1982) and the present vaccine era (1983 to 2004) (136, 144). Fine and Clarkson carefully studied the interepidemic interval in England and Wales for the 32-year period from 1950 to 1982 and found that it did not change significantly (244).
With the introduction and widespread use of pertussis vaccines in the 1940s and early 1950s, the rate of reported pertussis fell approximately 150-fold (Fig. 3). For the 7-year period between 1976 and 1982, the rate of reported pertussis in the United States remained between 0.5 and 1.0 case per 100,000 population (136). From 1982 to the present, there has been a modest linear increase in the rate of reported pertussis, which reached 3.1 cases per 100,000 population in 2002 (144) (Fig. 4). The reason for this upward trend is unknown, but in our opinion it is most probably due to a greater awareness of pertussis by physicians, public health professionals, and the public. Another contributing factor may be the decreased efficacy of one of the two DTP vaccines in use from around 1988 until 1995 and more recently due to the use of DTaP vaccines which, with one exception, are less efficacious than most DTP vaccines (24, 131, 152, 290, 293, 310).
FIG. 3.
Number of cases of pertussis in the United States from 1940 to 2002 (http://www.cdc.gov/nip/ed/slides/pertussis8p.ppt).
FIG. 4.
Number of cases of pertussis in the United States from 1980 to 2002 (http://www.cdc.gov/nip/ed/slides/pertussis8p.ppt).
Throughout history, reported pertussis was a disease of children. In the prevaccine era, ∼95% of cases were noted in children younger than 10 years (136). Data from Massachusetts from the period from 1933 to 1939 revealed the following percent distribution by age group: <1 year, 7.5%; 1 to 4 years, 41.1%; 5 to 9 years, 46%; 10 to 14 years, 4.1%; and ≥15 years, 0.9%. Similar prevaccine era data from England and Wales for the period from 1945 to 1949 revealed the following percent distribution by age group: <1 year, 10.4%; 1 to 4 years, 56.9%; 5 to 9 years, 29.2%; 10 to 14 years, 2.0%; and ≥15 years, 1.4%.
With the marked reduction in reported pertussis resulting from universal pediatric immunization, there was a dramatic shift in the percent age distribution. For the period from 1978 to 1981 in the United States, when the rate was <1 case per 100,000 population, the following percent distribution by age group was noted: <1 year, 53.5%; 1 to 4 years, 26.5%; 5 to 9 years, 8.2%; 10 to 14 years, 5.4%; and ≥15 years, 6.5% (136).
Over the last 20 years, in conjunction with the modest increase in reported pertussis, there has been an increase in reported pertussis in adolescents and adults (144). During the period from 1997 to 2000, the following percent distribution by age group was observed: <1 year, 29.4%; 1 to 4 years, 11.1%; 5 to 9 years, 9.8%; 10 to 19 years, 29.4%; and ≥20 years, 20.4% (109) (Fig. 5).
FIG. 5.
Age distribution and incidence of reported cases of pertussis in the United States from 1997 to 2000 (http://www.cdc.gov/nip/ed/slides/pertussis8p.ppt).
(ii) Mortality.
Pertussis was a major cause of death in the prevaccine era (136). In the period from 1926 to 1930, there were 36,013 reported deaths from pertussis in the United States. Mortality due to pertussis is markedly age related; the vast majority of deaths occur in infants. However in the prevaccine and early vaccine era, some deaths were noted in older children. For example, the mean annual pertussis death rate in the United States from 1940 to 1948 was 64 per 100,000 for infants, 6.4 per 100,000 for children 1 to 4 years of age, and 0.2 per 100,000 for children 5 to 14 years of age. During this period, more reported deaths in the first year of life resulted from pertussis than from measles, scarlet fever, diphtheria, poliomyelitis, and meningitis combined. Recent studies suggest that pertussis is an occasional factor in deaths in older adults (112, 124a, 534).
In the vaccine era, pertussis mortality declined following the curve of the decline in reported pertussis (136). In contrast, in the prevaccine era, pertussis mortality was falling whereas the incidence of reported pertussis was constant (567).
During the period from 1997 to 2000, there were 62 reported pertussis deaths in the United States (112). Of these, 56 (90%) occurred during the first 6 months of life. Two deaths (3.6%) were noted in children 5 to 9 years of age, and two deaths (3.6%) were reported in adults.
(iii) Sex and race.
Historically, one of the most remarkable features of reported pertussis was that the attack rate in females was higher than in males (136). The male/female ratio of reported pertussis cases in children aged 0 to 9 years in England and Wales from 1945 to 1982 was 0.88 (95% CI = 0.84 to 0.92). Interestingly, the reported attack rate in infant boys and girls during this period was almost equal. Data obtained in the United States during the early vaccine era was similar to the data noted above for England and Wales. Recent data from 1999 to 2002 in the United States also noted more cases in females than in males (113-116). The male/female ratio of reported pertussis cases for this 4-year period is 0.85.
In the prevaccine era, reported pertussis attack rates in the United States did not vary appreciably by race (285). Interestingly, recent data from the United States suggest considerable differences in attack rates by race. During the period from 1999 to 2002, the highest attack rates occurred in American Indians or Alaska Natives and the lowest occurred in Asian or Pacific Islanders (113-116). The reported attack rates in whites were consistently higher than those in blacks. For example, in 2002 the following rates per 100,000 were reported: American Indian or Alaska Natives, 4.17; Asian or Pacific Islanders, 1.00; blacks, 1.55; and whites, 3.71 (116).
(iv) Season and geographic areas.
Reported pertussis is noted in all populated areas of the world. However, reporting varies considerably. In the prevaccine era and early vaccine era, no seasonal pattern was observed for epidemic pertussis (136). For the 23-year period from 1980 to 2003, pertussis has been reported in every month of every year (96-105, 113-124). In general, however, more cases are reported during the second half of each year. Between 1980 and 1986, the peak months of reported pertussis were August, September, and October. Since 1987, the peak month of reported pertussis has been December. However, surprisingly, the smallest number of reported cases occurred in January. During the 4-year period from 1999 to 2002, the number of reported pertussis cases in December was 5.8 times the number of subsequent cases in January. This large difference seems biologically unlikely, and therefore it seems that the large number of cases in December may reflect a reporting bias rather than a true increase in the number of cases. Taking this into consideration, it appears that the true pattern from 1987 to 2002 is similar to that noted for the period 1980 to 1986: most cases are observed in August, September, and October.
At the Hospital for Sick Children, Toronto, Canada, between 1980 and 1990 the peak incidence of cases occurred in August, September, and October (286). In Britian the peak months of reported pertussis have been August and September (710). In the United States from 1990 through 1999, reported pertussis in infants peaked each year in the period from July to September (790).
B. pertussis infection.
During the last 20 years, the study of adolescent and adult B. pertussis infections has shed considerable light on the epidemiology of B. pertussis infections. As noted above, the cyclic pattern of epidemic pertussis is similar today to what it was in the prevaccine era. This pattern is different from that of other diseases which have been controlled by immunization (135, 149, 550). For example, with the control of measles, the interepidemic cycle lengthened. This was because the circulation of measles virus had been reduced in addition to the control of the disease. With pertussis, however, it was pointed out by Fine and Clackson 22 years ago that immunization controlled disease but did not decrease the circulation of B. pertussis (244). It was also noted in the 1970s that the source of infection in hospitalized infants was most often an adult (583). The above observations led one of us (J.D.C.) as well as others to conclude that B. pertussis infection was endemic in adolescents and adults (135, 149, 550). This adolescent and adult reservoir of sporadic infections is the source of B. pertussis infections in nonimmune children. The traditional cyclic pattern occurs because it takes a few years for a significant number of susceptables in the population to develop so that continued transmission will occur.
The development of the ability to measure IgG and IgA antibodies to B. pertussis antigens by ELISA made it possible to accurately study adolescent and adult B. pertussis infections. During the last 20 years, three types of studies of adolescent and adult populations have been carried out. These studies have determined: (i) the percentage of prolonged cough illnesses that are due to B. pertussis infections, (ii) the rate of infections, and (iii) the rate of infections with cough illness. In addition, surveys of IgA antibody in various populations has indicated the age-related occurrence of unrecognized B. pertussis infections. IgA antibody studies can be used for this purpose in both vaccinated and nonvaccinated populations because IgA antibody to B. pertussis antigens is not stimulated by primary immunization.
(i) Percentage of cough illnesses due to B. pertussis in adolescents and adults.
Prolonged cough illness was evaluated in 13 studies published between 1987 and 2002 (Table 7) (55, 271, 390, 397, 550, 586, 665, 675, 695, 739, 788, 828, 835). These studies, in six countries, involved subjects with cough illnesses seen between 1983 and 1999. The primary mode of diagnosis was the measurement of IgG or IgA antibodies to one or more B. pertussis antigens. Diagnosis was made by the demonstration of a significant antibody titer rise between acute-phase and convalescent-phase sera to one or more antigens or the presence of a significantly high single serum titer as determined by comparison of titers in well controls. In addition to serologic study, diagnosis was attempted by culture, PCR, and DFA. The individual studies were done under variable conditions, which affected the results. Some studies were done by following a formal protocol over a relatively long period, whereas others were done during pertussis outbreaks. The latter, of course, is a possible major bias in that the investigators might study only subjects they thought had pertussis and might not study prolonged cough illnesses that they did not think were pertussis.
TABLE 7.
Percentage of prolonged cough illnesses in adolescents and adults as a result of infections with serologica PCR, or culture evidence of Bordetella infections
| Author (reference) | Location | Yr | % of illness due to Bordetella |
|---|---|---|---|
| Jackson et al. (390) | Seattle | 1983-1987 | 15 |
| Robertson et al. (665) | New South Wales | 1985-1986 | 26 |
| Mink et al. (550) | Los Angeles | 1986-1989 | 26 |
| Schmitt-Grohé et al. (695) | Germany | 1992-1994 | 32 |
| Wright et al. (835) | Nashville | 1992-1994 | 21 |
| Wirsing von König et al. (828) | Germany | 1992-1994 | 31 |
| Rosenthal et al. (675) | Chicago | 1993-1994 | 26 |
| Jansen et al. (397) | San Diego | 1993-1994 | 17 |
| Nennig et al. (586) | San Francisco | 1994-1995 | 12 |
| Strebel et al. (739) | Minneapolis/St. Paul | 1995-1996 | 13 |
| Birbebaek et al. (55) | Denmark | 1995-1997 | 17 |
| Vincent et al. (788) | Korea | 1997-1998 | 50 |
| Gilberg et al. (271) | Paris | 1999 | 52 |
Significant rise in ELISA titer or high titer to PT, FHA, PRN, or FIM, or significant agglutinin titer or titer rise.
As noted in Table 7, the percentage of cough illnesses with laboratory evidence of Bordetella infection varied between a low of 12% and a high of 52%. The median value was 26%. A major factor which affected the results of these studies was the number of antigens used in the ELISAs. From several recent studies, it has become clear that infections with other Bordetella subspecies can cause IgG and IgA antibody responses to FHA and PRN and to a lesser extent FIM (149, 719). Other studies suggest that there may be cross-reacting antibody responses to FHA and perhaps PRN due to M. pneumoniae and C. pneumoniae infections (390, 550, 788). In addition, other infectious agents such as H. influenzae may also have FHA-like antigens that can result in high titers due to cross-reactivity (788).
Due to the above, it may be more appropriate to evaluate only PT antibody to determine B. pertussis infections in studies of prolonged cough illnesses. Table 8 lists 11 studies for which specific PT ELISA data were available (55, 271, 397, 550, 586, 675, 695, 739, 788, 828, 835). Using only PT, the variation is between 1 and 52%. In evaluating these data, it is important to know which studies were carried out during pertussis outbreaks and which were not related to outbreaks. All studies with the higher percentages (17 to 52%) were done during pertussis outbreaks, whereas all the others except one (695) were performed in nonoutbreak situations. The median value is 13%, and it appears that the one very low value (1%) may have been the result of a laboratory assay problem (397). The data in the studies by Mink et al., Wright et al., Nennig et al., and Strebel et al. strongly support a frequency of 12 to 16% of prolonged cough illnesses as being due to B. pertussis infection (550, 586, 739, 835). Since some persons with pertussis due to B. pertussis infection fail to mount a serum antibody response to PT but do have a response to FHA, the use of only PT may underestimate the true rate of prolonged cough illnesses due to B. pertussis (719).
TABLE 8.
Percentage of prolonged cough illnesses in adolescents and adults as a result of B. pertussisa infections
| Author (reference) | Location | Yr | % of illness due to B. pertussis |
|---|---|---|---|
| Mink et al. (550) | Los Angeles | 1986-1989 | 13 |
| Schmitt-Grohé et al. (695) | Germany | 1991-1994 | ∼11 |
| Wright et al. (835) | Nashville | 1992-1994 | 16 |
| Wirsing von König et al. (828) | Germany | 1992-1994 | 26 |
| Rosenthal et al. (675) | Chicago | 1993-1994 | 26 |
| Jansen et al. (397) | San Diego | 1993-1994 | 1 |
| Nennig et al. (586) | San Francisco | 1994-1995 | 12 |
| Strebel et al. (739) | Minneapolis/St. Paul | 1995-1996 | 13 |
| Birbebaek et al. (55) | Denmark | 1995-1997 | 17 |
| Vincent et al. (788) | Korea | 1997-1998 | 7 |
| Gilberg et al. (271) | Paris | 1999 | 52 |
Significant rise in IgA or IgG antibody titer or high titer to PT, or culture or PCR positive.
(ii) Rate of B. pertussis infections.
There are limited data available from which to access the rate of infections. There are four studies in which sera from a number of subjects were available over time (184, 206, 354; b J. Ward, J. Cherry, S. Chang, S. Partridge, W. Keitel, K. Edwards, M. Lee, J. Treanor, D. Greenberg, S. Barenkamp, D. Bernstein, R. Edelman, and R. Rabinovich, submitted for publication). In two studies two sera per subject were available, and in the other two studies multiple sera over 3- and 5-year intervals could be comparatively evaluated. In these studies, the same problem existed in regard to false-positives due to the use of FHA, PRN, and FIM. In Table 9, specific data for ELISA-measured increases in the titer of antibody to PT over time are presented. The rates varied from ∼1 to 8%. The two studies with the lower rates involved only two sera per subject, whereas the 3% rate involved three sera per year over a 3-year period and the 8% rate involved two sera per year over a 5-year period. This later study was reevaluated by one of us (J.D.C.) because of concerns that some of the seroconversions may have been due to nonspecific PT polyclonal responses rather than true rises in antibody titers (206). Removal of low values resulted in a rate of 6.7 per 100 person-years.
TABLE 9.
Rate of B. pertussis infections in adolescents and adultsa
| Author (reference) | Location | Yr | Annual rate (%) |
|---|---|---|---|
| Deville et al. (206) | Los Angeles, Calif. | 1984-1989 | 8 |
| Cromer et al. (184) | Columbus, Ohio | 1985-1990 | ∼1 |
| Hodder et al. (354) | Cleveland, Ohio | 1989-1992 | 3 |
| Ward et al., submitted | Eight U.S. cities | 1997-1999 | 1.3 |
Infections were determined by the demonstration of a significant rise in serum antibody titer to PT in successive serum samples.
(iii) Rate of cough illnesses due to B. pertussis infections.
In several of the prolonged cough illness studies, attempts were made to determine population rates of cough illnesses due to B. pertussis infection. In three initial studies the rates were calculated to be 64, 133, and 176 per 100,000 population (550, 586, 695). All three investigations were hampered by imprecise denominators. Subsequently, two prospective studies were carried out (739, 800) (Table 10). The first study revealed a rate of 507 per 100,000 population, and the second had a rate of 370 per 100,000 population. In addition, the Hodder et al. study in Cleveland included infection data and respiratory illness data over a 3-year period (354). The data in this study suggest that the rate could be as high as 1,500 per 100,000 population. However, this high value assumes that the respiratory illnesses during the periods of seroconversion were due to B. pertussis.
TABLE 10.
Rate of B. pertussis infections in adolescents and adultsa
| Author (reference) | Location | Yr | Annual rate (%) |
|---|---|---|---|
| Strebel et al. (739) | Minneapolis/St. Paul | 1995-1996 | 0.5 |
| Ward et al. (800) | Eight U.S. cities | 1997-1999 | 0.37 |
| Hodder et al. (354) | Cleveland, Ohio | 1989-1992 | 1.5 |
B. pertussis infection diagnosed by culture, PCR, or serologic study.
B. parapertussishu Epidemiology
Incidence and mortality.
In the prevaccine and early vaccine eras, B. parapertussishu infections were noted in three areas of the United States (California, Michigan, and New York) and in England, France, Czechoslovakia, Bulgaria, Denmark, Mexico, Chile, Australia, Japan, Spain, Portugal, Hungary; Yugoslavia, and Finland (51, 222, 314, 330, 340, 363, 444, 445, 465, 468, 498, 499, 545). However, most studies compared the percentage of cases of pertussis due to either B. pertussis or B. parapertussishu, and population rates were not determined. Nonetheless, from available data in Denmark, an average yearly rate can be calculated for the period from 1950 to 1957 for children aged 0 to 9 years (444, 445). The average yearly rate for pertussis due to B. parapertussishu was 73 per 100,000. For the same period it was 1,569 per 100,000 for pertussis due to B. pertussis infection.
Eldering and Kendrick (222) studied pertussis in the Grand Rapids area of Michigan for a 16-year period (1935 to 1950). Of 4,483 Bordetella isolates, 106 (2.4%) were B. parapertussishu. In Czechoslovakia during a 3-year period (1967 to 1969), Borska and Simkovicova noted rates of infection of 2.66 to 2.69% among preschool children and 0.33 to 1.11% among school children (66). In this study specimens were collected every three months from all children. Of the children with positive cultures, 70.5% had clinical symptoms; of this group, the majority (64.7%) had only very mild symptoms.
In the present era, the DTaP vaccine efficacy trials in the early 1990s revealed considerable evidence of the frequency of B. parapertussishu infections in young children. In the Erlangen trial, there was laboratory evidence of B. pertussis infections in 103 control subjects (DT recipients) and B. parapertussishu infections in 27 control subjects (719). The B. parapertussishu illness rate was 0.9 case per 100 person years. A total of 21% of all cases were due to B. parapertussishu.
Of the Bordetella isolates from study subjects in the other trials, 20, 12.2, 8, 2.1, and 2.1% were found to be B. parapertussishu in Munich, Italy, Stockholm, Mainz, and Gothenburg, respectively (499).
Agglutinating-antibody studies using B. parapertussishu as the antigen suggested that infections are common in all age groups and that the majority of these infections are unrecognized clinically (252, 545, 793). Miller et al. found B. parapertussishu agglutinins in the sera of 40% of children who had not had clinical pertussis and who had not received pertussis vaccine (545). Vysoka-Burianova found agglutinating antibodies to B. parapertussishu in the sera of 59% of 6- to 9-year-old children (793).
In contrast to the findings in Europe and the prevaccine era in the United States, B. parapertussishu isolates in the United States during the last 30 years have been uncommon. Enhanced surveillance activities by the CDC have processed over 4,000 B. pertussis isolates during the last 8 years. During the same time period there were only 10 B. parapertussishu isolates, and, interestingly, all of these were from Ohio (G. Sanden, personal communication).
Similar to B. pertussis, there appear to be epidemic cycles of B. parapertussishu infections. In Denmark during the period between 1950 and 1957 there were three peaks, suggesting a 3-year cycle (445). Further surveillance by Lautrop over a 20-year period suggested peaks every fourth year (444). He also noted that the B. pertussis and B. parapertussishu peaks did not occur concomitantly. In the study in Erlangen, there were no identified cases of pertussis due to B. parapertussishu between April 1991 and April 1992. Following this, there were B. parapertussishu-caused illnesses each month through March 1993 (340).
Clinical disease due to B. parapertussishu infection is most common during the first 5 years of life. In Denmark, 65% of the cases occurred in children younger than 5 years and 96.1% occurred in children younger than 10 years (444). In other studies, the vast majority of B. parapertussishu symptomatic infections have been noted in children (51, 66, 330, 340, 363, 465, 498). In a study in Finland, 12 cases were noted in persons aged 16 years or older (330). In contrast to B. pertussis infection, death due to B. parapertussishu infection is rare. Zwelzer and Wheeler noted two deaths in infants from whom B. parapertussishu was isolated at autopsy (848). Both of these very young infants had bronchopneumonia (848).
Sex, race, season, and geographic areas.
Unfortunately there are no data available from the larger B. parapertussishu studies on the incidence of clinical disease by sex (66, 444, 445). In four relatively recent studies, more girls than boys had pertussis due to B. parapertussishu infection (51, 340, 498, 825). Overall in these four studies there were 228 cases, and 122 (54%) were noted in girls (male/female ratio = 0.87). These findings are similar to those noted above for pertussis due to B. pertussis infection.
No data are available in regard to B. parapertussishu illness by race. In a 3-year study in Italy in conjunction with a DTaP vaccine efficacy trial, the seasonality of B. parapertussishu illnesses was similar to that of B. pertussis illnesses (499). An increase in the number of cases was noted from April through July. In examining the epidemic curves in Denmark for the period 1950 through 1957, there were four peak periods, all of which were winter peaks (445). B. parapertussis infection appears to occur worldwide, but in recent years it has been noted most often in Europe (51, 330, 340, 465, 498, 499, 825).
Interrelationship between B. parapertussishu and B. pertussis infections.
As noted above, during the early studies in Denmark it was found that epidemics of illness due to B. pertussis and B. parapertussis were not concomitant (445). However, during Lautrop's investigation he noted 79 persons who had bacteriologically confirmed infections with both B. pertussis and B. parapertussishu. In about one-third of the studied subjects, the infections with the two organisms occurred simultaneously. In sequential infections, the first infection was with B. parapertussishu in all but four instances. During the 7-year observation period, two successive infections with B. parapertussis were not encountered. More recent studies have noted both mixed infections and sequential infections with B. pertussis and B. parapertussishu (51, 330, 389, 535, 719, 753). From the available data, there is no evidence of more or less severe disease in children with concommitant infections with both organisms than would occur with B. pertussis infection. In addition, in sequential infections there is no evidence that the first infection affected the manifestations of the second infection.
B. bronchiseptica Epidemiology
Although infection with B. bronchiseptica has been associated with respiratory disease in at least 18 mammals, little is known about its epidemiology in nature (38, 64, 79, 211, 215, 240, 243, 249, 260, 267, 283, 291, 407, 426, 455, 500, 511, 516, 673, 698, 715, 747). The primary host of B. bronchiseptica is not known, and little is known about intra- and interspecies transmission in the wild. Most experience over the last 90 years has been gained by the study of domesticated animals living in closed quarters. Transmission from animal to animal is by direct contact with respiratory secretions, fomites, and perhaps by aerosol (23, 765). Porter et al. have shown that the organism can grow in lakewater, which suggests that B. bronchiseptica may occur as a free-living organism (632, 633). If this is the case, then transmission to multiple animal species could occur without direct contact.
A major difficulty in the study of the epidemiology of B. bronchiseptica in laboratory animal research colonies, kennels, and pens is the high rate of asymptomatic infection with prolonged shedding of the organism. In some guinea pig colonies, the incidence of asymptomatic infection can be as high as 20% (23). High asymptomatic infection rates also occur in rabbit colonies, and most conventionally managed swine herds are infected with B. bronchiseptica (23, 201).
B. holmesii Epidemiology
B. holmesii appears to be a rare human pathogen, whose epidemiology is presently not known (508, 814, 839).
LONG-TERM GOALS OF PERTUSSIS PREVENTION
Eradication of B. pertussis Circulation
The ultimate long-term goal of the prevention of a disease by immunization should always be the elimination of the infectious agent. This is theoretically possible with all human infections in which there is no animal reservoir (e.g., rabies) or environmental reservoir (e.g., tetanus). This goal was achieved with smallpox in 1978 and may soon be achieved with all three types of polio (134, 138). In addition, toxigenic strains of Corynebacterium diphtheriae have been eliminated from large geographic regions of the world (815).
The ultimate long-term goal for the prevention of pertussis due to B. pertussis infection should also be the elimination of the circulation of the organism. However, it is readily apparent that this goal is not realistic in the foreseeable future because of numerous obstacles such as lack of funding, understanding, and commitment. Similar to the experience with diphtheria, however, it does seem possible to us that the circulation of B. pertussis could be stopped in countries with aggressive, comprehensive immunization programs.
As noted above, the universal immunization of infants and children such as in the United States with pertussis vaccines prevents more than 95% of all reported illnesses. However, with the present increased awareness of pertussis, the absolute number of reported cases of pertussis has increased substantially during the last two decades (144). It is apparent today that the reservoir of B. pertussis in the population is symptomatic infections in adolescents and adults of all ages. This is not a new phenomenon (it was present in the prevaccine era), but it is more apparent today with the control of disease in vaccinated children (141). Clinical studies of prolonged cough illnesses and serologic surveillance studies indicate that all age groups and all geographic areas are involved.
The availability of DTaP vaccines leads to the possibility of adolescent and adult booster immunizations. In addition, two specific adolescent and adult DTaP vaccines have been developed and are licensed in several countries. The compositions of these two vaccines are presented in Table 11.
TABLE 11.
Contents of two DTaP vaccines formulated for adolescents and adults
| Antigen | Aventis (Adacel)a amt or dose | GSK (Boostrix)b amt or dose |
|---|---|---|
| Diphtheria toxoid | 2 Lf | 2.5 Lf |
| Tetanus toxoid | 5 Lf | 5 Lf |
| PT toxoid | 2.5 μg | 8 μg |
| FHA | 5 μg | 8 μg |
| PRN | 3 μg | 2.5 μg |
| FIM2/3 | 5 μg | |
| 2-Phenoxyethanol | 0.6% | 2.5 mg |
Aventis: Product information, September 2002.
GlaxoSmithKline (GSK): Product information, November 2003.
With the goal of the elimination of the circulation of B. pertussis, an immunization program must include both adolescents and all ages of adults in addition to universal childhood immunization. The duration of protection and of the expected decrease in circulation of B. pertussis following booster immunizations in adults is not known. It is clear, however, that the decay in the level of antibodies following a booster dose in adults varies by antigen (446). Specifically, antibody to PT falls substantially during an 18-month period postvaccination whereas titers to PRN and FHA have considerably lengthened decay curves. Using the serum antibody decay curves in adolescents and adults who received one dose of an adult-formulated aP vaccine, Le et al. predicted the duration of the time that the IgG GMT of antibody to the various antigens would remain above the limits of quantitation of their ELISA (446). This analysis suggested that the GMT for PT would fall below 6 ELISA units (Eu)/ml in 2.3 years, whereas the GMT for PRN would stay above 8 Eu/ml for 9.1 years. Since there is evidence that a low level (≥7 Eu/ml) of antibody to PRN is highly protective, it seems probable that an interval between booster doses of 10 years would be effective (148, 736). In this regard, one concern relates to what is being measured with respect to antibody to PRN. In the serologic correlates of immunity studies, the protected subjects were young children who had recently been immunized with PRN-containing vaccines. The antibodies to PRN in these subjects were specifically due to the direct immunologic response to B. pertussis PRN.
For the adults, however, the delayed antibody decay pattern suggests that the measured antibody may be the result of exposure to cross-reacting antigens and not just the result of the specific immunization. For example, the PRN of other Bordetella species is slightly different from that of B. pertussis. In addition, it seems possible that cross-reacting antibodies to PRN may also be stimulated by infections with M. pneumoniae and perhaps C. pneumoniae (550, 788). With these possibilities in mind, it seems possible that the antibody to PRN that was measured following adolescent and adult immunization may not be as functionally specific against B. pertussis as that which followed primary immunization in young children. If this were the case, the protection following adolescent and adult booster immunizations would probably be of shorter duration than the 10-year projected duration.
Since adults should receive dT boosters every 10 years, it is reasonable to assume that such a schedule with a DTaP vaccine could be effective. As noted above, the demonstrated projected decay pattern of IgG antibody to PRN following adult booster immunization supports a 10-year booster schedule. To be effective, a universal pertussis immunization program (infants, children, adolescents, and adults) would need to elicit both individual protection and herd immunity. Experience indicates that the pediatric aspects of this proposed program are presently in place. The adolescent portion of this program also seems attainable through the development of school-based programs. Immunization of adults with boosters every 10 years is a difficult goal and presently impossible. However, innovative ways can be developed to reach this goal. Of necessity in this regard will be active committees (similar to the Committee of Infectious Diseases of the American Academy of Pediatrics) involving internists, family practitioners, and obstetricians. Work-related immunization programs could capture a substantial number of adults, and if these programs could include spouses they may well reach enough of the population to induce herd immunity. Clearly for success a new public health commitment will be required.
Lesser Goals
At present, multiple committees, working groups, and task forces are addressing the future control of pertussis with adolescent and adult immunization. In general, these groups have shied away from universal adult immunization, presumably because it is presently logistically impossible. In general, most groups favor a universal adolescent booster dose and various attempts to reach adults who, if infected, would spread infection to infants too young to be adequately immunized. Two recent modeling studies support a booster program involving adolescents (645, 784). This approach could be expected to reduce the number of B. pertussis illnesses in infants but not have a major effect on the circulation of B. pertussis. B. pertussis would continue to circulate in persons aged 25 to over 75 years. With school-based immunization programs, a high proportion of adolescents could be immunized. However, selective immunization of adults for other diseases (e.g., influenza) has not had high compliance rates, and there is no reason to expect better results with DTaP vaccines.
Infant and Childhood DTaP Immunization Schedules
The present infant and childhood immunization schedule evolved using DTP vaccines and has been effective. The same schedule is now used with DTaP vaccines, and it is not optimal. In general, good DTP vaccines contained more antigens than the present DTaP vaccines but the concentrations of the antigens in the DTP vaccines were modest. In contrast, the specific antigens (PT, FHA, PRN, and FIM) in DTaP vaccines are present in higher concentrations than their counterparts in DTP vaccines. Furthermore, the two good DTaP vaccines available in the United States contain significantly larger amounts of diphtheria toxoid than did the former U.S. DTP vaccines (759a, 759b). The excessive amounts of diphtheroid toxoid (i.e., 25 Lf and 15 Lf) in the DTaP vaccines are responsible for marked local reactions in children who received booster doses (656). In addition, one of the two vaccines has a large amount of PT, which contributes to local reactions with booster doses (759b).
The vaccine efficacy trials in Sweden and Italy demonstrate good antibody responses and protection for more than 5 years following three doses of vaccine at 2, 4, and 6 months of age and no booster dose during the second year of life (596, 684, 685). These data indicate that with these two vaccines, a booster dose in the second year of life may be unnecessary and is the cause of excessive local reactions with the fourth and fifth doses. Although further study may be necessary, it is clear that we do not need five doses of the present DTaP vaccines in childhood. The simplest change is to omit the dose in the second year of life. Another approach which was demonstrated to give a good primary response was a schedule of 3, 5, and 12 months of age (597).
Following either schedule, a booster dose at 5 years of age should provide good protection until the time of an adolescent booster at 13 to 15 years of age.
FUTURE RESEARCH
Pathogenesis of Disease
Although much has been accomplished relating to Bordetella spp. and their illnesses during the last two decades, there is still much that is not known. A fundamental question is why people and animals infected with the four Bordetella subspecies discussed in this review have such isolated prolonged cough illnesses. The cough in pertussis is truly unique. It is difficult to believe that this cough is solely due to local damage to ciliated epithelial cells, because it continues over an extensive period with the appearance of being completely normal between paroxysms. There are clinical similarities to tetanus, suggesting that there may well be an as yet undiscovered toxin which is common to respiratory Bordetella spp. Careful investigation of the commonly expressed unknown proteins of Bordetella may shed light on this issue.
Present animal model systems are not adequate for the study of coughs. Since other primates have pertussis-like illnesses, studies of these animals by using various B. pertussis strains with various deletions might be useful. In addition, human volunteer studies are being planned.
Another area of interest is the possible relationship between B. pertussis strain differences and clinical manifestations of disease. Careful analysis of different protein variations can be analyzed by disease severity.
Further study of Bvg− and Bvgi phase organisms in more natural circumstances such as primate and human volunteer studies with B. pertussis and studies of more natural swine populations with B. bronchiseptica should be useful.
Better Vaccines
Basic research on previously known virulence factors has greatly enhanced our understanding of Bordetella pathogenesis and the host response to infection. Sequence information obtained from the Bordetella Genome Project has further accelerated the discovery of novel virulence factors. Above all, comparative analyses of the genomes as well as the pathogenic and environmental life cycles of various Bordetella subspecies have provided crucial insights into the infection mechanisms employed by Bordetella. As with most fields, information obtained from such research has facilitated the development of new vaccines. To avoid the side effects associated with DTP vaccines, scientists and clinicians have developed two generations of efficacious DTaP vaccines generally free of such alarming side effects. However, pertussis vaccine efficacy trials conducted throughout the 1990s clearly demonstrated the generally greater efficacy of DTP control vaccines over their counterpart first- and second-generation DTaP vaccines (464, 697, 708, 719). These observations suggest that the inclusion of additional antigens in the next generation of DTaP vaccines could improve vaccine efficacy.
Current DTaP vaccines are single-component (PT toxoid), two-component (PT and FHA), three-component (PT, FHA, and PRN), four-component (PT, FHA, PRN, and FIM2), and five-component (PT, FHA, PRN, and FIM2/3) vaccines. Of these vaccines, only a five-component vaccine has been shown to be as efficacious as one highly immungenic DTP vaccine (597). FIM2/3 serve as important adjuvants for inducing a protective immune response (148, 503, 506, 597, 736). The role of FHA in generating anti-Bordetella immunity has come into question; however, the discovery of fhaS and fhaL suggests that their gene products could overcome the action of anti-FHA antibodies.
Inclusion of CyaA in an aP vaccine concoction has also been suggested; however, anti-CyaA antibodies could cross-react with RTX-family hemolysins generated by other members of the microflora. For this very reason, tracheal cytotoxin, a by-product of bacterial cell wall synthesis, would also not make a good vaccine candidate. In contrast, additional surface-associated proteins (e.g., autotranporters such as BrkA, Vag8, and SphB1) serve as promising vaccine components. Antibodies generated against SphB1, for instance, could target agglutination via SphB1-FHA interactions. Alternatively, antibody-mediated blocking of SphB1 function could impede proper maturation and secretion of FHA.
The suitability of adding purified LPS to an aP vaccine concoction has also been a subject of discussion. While active B. pertussis LPS is present in all DTP vaccines in different concentrations and is a major contributor to local and systemic reactions with these vaccines (147, 149), B. pertussis infection, interestingly, is not accompanied by the usual LPS toxicity (fever and shock). Thus, genetically modified LPS may be used as a putative vaccine component, serving as an antigen and/or an adjuvant.
Most recently, the intriguing possibility of type III secretion serving as a potent virulence factor in human disease was presented (507). Until this report, type III secretion was considered to be B. bronchiseptica specific. Since B. pertussis expresses PT, which, like the TTSS, displays immunosuppressive phenotypes, it was assumed not to require a functional TTSS for pathogenesis. Mattoo et al. showed that although type III-specific proteins were not expressed by B. pertussis in vitro, transcription of all TTSS genes was surprisingly intact and regulated in a manner similar to that seen for B. bronchiseptica. It seems unlikely that B. pertussis would expend the energy required to transcribe the entire bsc and btr loci (which consist of over 26 genes), unless the products of these genes were required for pathogenesis. It was therefore proposed that B. pertussis may express type III secretion in vivo (507). If this is so, proteins secreted by this system would serve as good vaccine candidates, provided that they are also antigenic. A type III-secreted effector for B. bronchiseptica has recently been identified (603). Preliminary results suggest that this effector is functionally conserved in B. pertussis as well, thus validating the inclusion of this effector in the vaccine concoctions for Bordetella-mediated human and animal infections. Another good, and perhaps better, type III-secreted vaccine candidate is Bsp22. This 22-kDa protein is unique to Bordetella, highly conserved throughout the sequenced Bordetella strains, secreted in copious amounts by the Bordetella TTSS, and highly antigenic based on experiments conducted with mouse, rat and rabbit models (507, 840, 841). While Bsp22 is secreted by the TTSS, it appears not to serve as an effector; instead, it appears to be a component of the type III secretion apparatus and specifically associates with the type III secretion needle (505). Thus, antibodies targeted against Bsp22 could be ideal for opsonization and therefore for prevention of infection by Bordetella.
Asymptomatic carriers play a critical role in the spread of B. bronchiseptica infection. Analysis of various B. bronchiseptica virulence factor deletion mutants have mainly revealed defects in lower respiratory tract colonization in several animal models. Thus, identification of a virulence factor(s) specifically involved in nasal colonization may be important for the development of a B. bronchiseptica vaccine that could prevent carriage. Most recently, the BtrS extracytoplasmic function sigma factor, which regulates type III secretion, has been shown to represent a regulon that functions downstream of BvgAS and controls the expression of several factors including Vag8 (507). We expect that BtrS may also control the expression of one or more factors that play a role in nasal colonization, since a B. bronchiseptica BtrS deletion mutant is deficient in persistent colonization of the entire upper respiratory tract in the rat model (505). Incidentally, this defect in nasal colonization is not due to the absence of Vag8, because a Vag8 deletion mutant is indistinguishable from wild-type B. bronchiseptica in its ability to colonize the nasal cavity (A. K. Wykert, R. Deora, S. Mattoo, and J. F. Miller, unpublished data). Thus, identification and inclusion of these BtrS-regulated nasal colonization determinants may present another avenue for designing strategies to curb the spread of B. bronchiseptica infection.
Finally, understanding the proposed role of the Bvgi phase in transmission may also help to improve the ability of DTaP vaccines in preventing B. bronchiseptica carriage and spread. While antibodies against Bvg+ phase-specific factors may help to block the establishment and persistence of infection, antibodies against Bvgi phase-specific factors may prevent B. bronchiseptica from switching to a readily transmissible phase in vivo.
Role of B. holmesii in Human Disease
The findings in Massachusetts in 1995 through 1998 of pertussis-like illness due to B. holmesii is of interest and suggests that illness due to this agent may be overlooked. Increased awareness that this organism could be responsible for culture-negative cases of pertussis should be encouraged. Culture-negative samples should be studied by PCR and also recultured in media without cephalexin.
More Complete Epidemiologic Study
Presently, there is much misunderstanding relating to B. pertussis epidemiology because of the failure to recognize sporadic, endemic cases of pertussis in adolescents and adults. The use of single-serum ELISA on sera from persons with prolonged cough illnesses should be systematically studied in all age groups throughout the world.
Acknowledgments
We appreciate the veterinary research input provided by Marcelo A. Couto and the encouragement and assistance provided by Jeffery F. Miller. We are also grateful to Laura Wennstrom for her invaluable assistance.
REFERENCES
- 1.Abrahams, I. 1966. Further studies on acquired resistance to murine cryptococcosis: enhancing effect of Bordetella pertussis. J. Immunol. 96:525-529. [PubMed] [Google Scholar]
- 2.Abramson, T., H. Kedem, and D. A. Relman. 2001. Proinflammatory and proapoptotic activities associated with Bordetella pertussis filamentous hemagglutinin. Infect. Immun. 69:2650-2658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ad Hoc Group for the Study of Pertussis Vaccines. 1988. Placebo-controlled trial of two acellular pertussis vaccines in Sweden—protective efficacy and adverse events. Lancet i:955-960. [PubMed] [Google Scholar]
- 4.Advisory Panel of the Committee on Safety of Medicines. 1981. The collection of data relating to adverse reactions in pertussis vaccine, p. 27, Whooping cough. Reports from the Committee on Safety of Medicines and the Joint Committee on Vaccination and Immunization. Department of Health and Social Security, Her Majesty's Stationery Office, London, United Kingdom.
- 5.Advisory Panel of the Committee on Safety of Medicines. 1981. Report on the assessment of the summarized histories of 50 cases of reported serious reactions following immunization with vaccines containing pertussis antigen, p. 6. Whooping cough. Reports from the Committee on Safety of Medicines and the Joint Committee on Vaccination and Immunization. Department of Health and Social Security, Her Majesty's Stationery Office, London, United Kingdom.
- 6.Aintablian, N., P. Walpita, and M. H. Sawyer. 1998. Detection of Bordetella pertussis and respiratory synctial virus in air samples from hospital rooms. Infect. Control Hosp. Epidemiol. 19:918-923. [DOI] [PubMed] [Google Scholar]
- 7.Akerley, B. J., P. A. Cotter, and J. F. Miller. 1995. Ectopic expression of the flagellar regulon alters development of the Bordetella-host interaction. Cell 80:611-620. [DOI] [PubMed] [Google Scholar]
- 8.Akerley, B. J., D. M. Monack, S. Falkow, and J. F. Miller. 1992. The bvgAS locus negatively controls motility and synthesis of flagella in Bordetella bronchiseptica. J. Bacteriol. 174:980-990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alderslade, R., M. H. Bellman, N. S. B. Rawson, and D. L. Miller. 1981. The national childhood encephalopathy study, p. 79. Whooping cough. Reports from the Committee on Safety of Medicines and the Joint Committee on Vaccination and Immunization. Department of Health and Social Security, Her Majesty's Stationery Office, London, United Kingdom.
- 10.Andersen, E. K. 1953. Serological studies on H. pertussis, H. parapertussis, and H. bronchisepticus. Acta Pathol. Microbiol. Scand. 33:202-224. [DOI] [PubMed] [Google Scholar]
- 11.Aoyama, T., K. Sunakawa, S. Iwata, Y. Takeuchi, and R. Fujii. 1996. Efficacy of short-term treatment of pertussis with clarithromycin and azithromycin. J. Pediatr. 129:761-764. [DOI] [PubMed] [Google Scholar]
- 12.Arch, R. N., and I. A. Parfentjev. 1957. The effect of Hemophilus pertussis sensitization on the increase of susceptibility of mice to infection by a saprophyte. J. Infect. Dis. 101:31-34. [DOI] [PubMed] [Google Scholar]
- 13.Arico, B., and R. Rappuoli. 1987. Bordetella parapertussis and Bordetella bronchiseptica contain transcriptionally silent pertussis toxin genes. J. Bacteriol. 169:2847-2853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Asakawa, S., and S. Iwasa. 1982. The effect of Bordetella pertussis lymphocytosis-promoting factor (LPF) on antibody response in mice: its enhancing and suppressive effects. Jpn. J. Med. Sci. Biol. 35:25-29. [DOI] [PubMed] [Google Scholar]
- 15.Athanassiades, T. J. 1977. Adjuvant effect of Bordetella pertussis vaccine to sheep erythrocytes in mice: enhancement of cell-mediated immunity by subcutaneous administration of adjuvant and antigen. Infect. Immun. 18:416-423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ausiello, C. M., R. Lande, F. Urbani, B. Di Carlo, P. Stefanelli, S. Salmaso, P. Mastrantonio, and A. Cassone. 2000. Cell-mediated immunity and antibody responses to Bordetella pertussis antigens in children with a history of pertussis infection and in recipients of an acellular pertussis vaccine. J. Infect. Dis. 181:1989-1995. [DOI] [PubMed] [Google Scholar]
- 17.Ausiello, C. M., R. Lande, F. Urbani, A. la Sala, P. Stefanelli, S. Salmaso, P. Mastrantonio, and A. Cassone. 1999. Cell-mediated immune responses in four-year-old children after primary immunization with acellular pertussis vaccines. Infect. Immun. 67:4064-4071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ausiello, C. M., F. Urbani, A. la Sala, R. Lande, and A. Cassone. 1997. Vaccine- and antigen-dependent type 1 and type 2 cytokine induction after primary vaccination of infants with whole-cell or acellular pertussis vaccines. Infect. Immun. 65:2168-2174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ayme, G., M. Caroff; R. Chaby, N. Haeffner-Cavaillon, A. Le Dur, M. Moreau, M. Muset, M. C. Mynard, M. Roumiantzeff, D. Schulz, and L. Szabo. 1980. Biological activities of fragments derived from Bordetella pertussis endotoxin: isolation of a nontoxic, Shwartzman-negative lipid A possessing high adjuvant properties. Infect. Immun. 27:739-745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bace, A., T. Zrnic, J. Begovac, N. Kuzmanovic, and J. Culig. 1999. Short-term treatment of pertussis with azithromycin in infants and young children. Eur. J. Clin. Microbiol. Infect. Dis. 18:296-298. [DOI] [PubMed] [Google Scholar]
- 21.Badr-El-Din, M. K., G. H. Aref, H. Mazloum, Y. A. El-Towesy, A. S. Kassem, M. A. Abdel-Moneim, and A. A. Abbassy. 1976. The beta-adrenergic receptors in pertussis. J. Trop. Med. Hyg. 79:213-217. [PubMed] [Google Scholar]
- 22.Baird, H. W., III, and L. G. Borofsky. 1957. Infantile myoclonic seizures. J. Pediatr. 50:332-339. [DOI] [PubMed] [Google Scholar]
- 23.Baker, D. G. 2003. Natural pathogens of laboratory animals: their effects on research. ASM Press, Washington, D.C.
- 24.Baker, J. D., S. A. Halperin, K. Edwards, B. Miller, M. Decker, and D. Stephens. 1992. Antibody response to Bordetella pertussis antigens after immunization with American and Canadian whole-cell vaccines. J. Pediatr. 121:523-527. [DOI] [PubMed] [Google Scholar]
- 25.Baraff, L. J., W. J. Ablon, and R. C. Weiss. 1983. Possible temporal association between diphtheria-tetanus toxoid-pertussis vaccination and sudden infant death syndrome. Pediatr. Infect. Dis. J. 2:7-11. [DOI] [PubMed] [Google Scholar]
- 26.Baraff, L. J., and J. D. Cherry. 1979. Nature and rates of adverse reactions associated with pertussis immunization, p. 291-296. In C. R. Manclark and J. C. Hills (ed.), International Symposium on Pertussis. U.S. Department of Health, Education, and Welfare, Government Printing Office, Washington, D.C.
- 27.Baraff, L. J., J. D. Cherry, and C. L. Cody. 1980. Pertussis vaccine project: rates, nature and etiology of adverse reactions associated with DTP vaccine. Bureau of Biologics, accession no. PB81-140-634. Department of Commerce, National Technical Information Service, Springfield, Va.
- 28.Baraff, L. J., J. D. Cherry, C. L. Cody, S. M. Marcy, and C. R. Manclark. 1985. DTP vaccine reactions: effect of prior reactions on rate of subsequent reactions. Dev. Biol. Stand. 61:423-428. [PubMed] [Google Scholar]
- 29.Baraff, L. J., J. D. Cherry, and S. M. Marcy. 1986. DTP reactions: relationship of manufacturer lot, potency and endotoxin to reaction rates, abstracted. Pediatr. Res. 20:877. [Google Scholar]
- 30.Baraff, L. J., C. L. Cody, and J. D. Cherry. 1984. DTP-associated reactions: an analysis by injection site, manufacturer, prior reactions, and dose. Pediatrics 73:31-36. [PubMed] [Google Scholar]
- 31.Baraff, L. J., R. D. Leake, D. G. Burstyn, T. Payne, C. L. Cody, C. R. Manclark, and J. W. St Geme, Jr. 1984. Immunologic response to early and routine DTP immunization in infants. Pediatrics 73:37-42. [PubMed] [Google Scholar]
- 32.Baraff, L. J., W. D. Shields, L. Beckwith, G. Strome, S. M. Marcy, J. D. Cherry, and C. R. Manclark. 1988. Infants and children with convulsions and hypotonic-hyporesponsive episodes following diphtheria-tetanus-pertussis immunization: follow-up evaluation. Pediatrics 81:789-794. [PubMed] [Google Scholar]
- 33.Baraff, L. J., J. Wilkins, and P. F. Wehrle. 1978. The role of antibiotics, immunizations, and adenoviruses in pertussis. Pediatrics 61:224-230. [PubMed] [Google Scholar]
- 34.Barnard, A., B. P. Mahon, J. Watkins, K. Redhead, and K. H. Mills. 1996. Th1/Th2 cell dichotomy in acquired immunity to Bordetella pertussis: variables in the in vivo priming and in vitro cytokine detection techniques affect the classification of T-cell subsets as Th1, Th2 or Th0. Immunology 87:372-380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Baron, S., E. Njamkepo, E. Grimprel, P. Begue, J. C. Desenclos, J. Drucker, and N. Guiso. 1998. Epidemiology of pertussis in French hospitals in 1993 and 1994: thirty years after a routine use of vaccination. Pediatr. Infect. Dis. J. 17:412-418. [DOI] [PubMed] [Google Scholar]
- 36.Barry, E. M., A. A. Weiss, I. E. Ehrmann, M. C. Gray, E. L. Hewlett, and M. S. Goodwin. 1991. Bordetella pertussis adenylate cyclase toxin and hemolytic activities require a second gene, cyaC, for activation. J. Bacteriol. 173:720-726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Basar, T., V. Havlicek, S. Bezouskova, M. Hackett, and P. Sebo. 2001. Acylation of lysine 983 is sufficient for toxin activity of Bordetella pertussis adenylate cyclase: substitutions of alanine 140 modulate acylation site selectivity of the toxin acyltransferase CyaC. J. Biol. Chem. 276:348-354. [DOI] [PubMed] [Google Scholar]
- 38.Baskerville, M., M. Wood, and A. Baskerville. 1983. An outbreak of Bordetella bronchiseptica pneumonia in a colony of common marmosets (Callithrix jacchus). Lab. Anim. 17:350-355. [DOI] [PubMed] [Google Scholar]
- 39.Bass, J. W. 1986. Erythromycin for treatment and prevention of pertussis. Pediatr. Infect. Dis. J. 5:154-157. [DOI] [PubMed] [Google Scholar]
- 40.Bass, J. W. 1985. Pertussis: current status of prevention and treatment. Pediatr. Infect. Dis. J. 4:614-619. [DOI] [PubMed] [Google Scholar]
- 41.Bass, J. W., E. L. Klenk, J. B. Kotheimer, C. C. Linnemann, and M. H. Smith. 1969. Antimicrobial treatment of pertussis. J. Pediatr. 75:768-781. [DOI] [PubMed] [Google Scholar]
- 42.Bassili, W. R., and G. T. Stewart. 1976. Epidemiological evaluation of immunisation and other factors in the control of whooping-cough. Lancet i:471-474. [DOI] [PubMed] [Google Scholar]
- 43.Bauwens, J. E., D. H. Spach, T. W. Schacker, M. M. Mustafa, and R. A. Bowden. 1992. Bordetella bronchiseptica pneumonia and bacteremia following bone marrow transplantation. J. Clin. Microbiol. 30:2474-2475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Beiter, A., K. Lewis, E. F. Pineda, and J. D. Cherry. 1993. Unrecognized maternal peripartum pertussis with subsequent fatal neonatal pertussis. Obstet. Gynecol. 82:691-693. [PubMed] [Google Scholar]
- 45.Reference deleted.
- 46.Bellalou, J., H. Sakamoto, D. Ladant, C. Geoffroy, and A. Ullmann. 1990. Deletions affecting hemolytic and toxin activities of Bordetella pertussis adenylate cyclase. Infect. Immun. 58:3242-3247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bellman, M. H., E. M. Ross, and D. L. Miller. 1983. Infantile spasms and pertussis immunisation. Lancet i:1031-1034. [DOI] [PubMed] [Google Scholar]
- 48.Bemis, D. A., L. E. Carmichael, and M. J. Appel. 1977. Naturally occurring respiratory disease in a kennel caused by Bordetella bronchiseptica. Cornell Vet. 67:282-293. [PubMed] [Google Scholar]
- 49.Bemis, D. A., and J. R. Kennedy. 1981. An improved system for studying the effect of Bordetella bronchiseptica on the ciliary activity of canine tracheal epithelial cells. J. Infect. Dis. 144:349-357. [DOI] [PubMed] [Google Scholar]
- 50.Berg, J. M. 1958. Neurological complications of pertussis immunization. Br. Med. J. 30:24-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bergfors, E., B. Trollfors, J. Taranger, T. Lagergård, V. Sundh, and G. Zackrisson. 1999. Parapertussis and pertussis: differences and similarities in incidence, clinical course, and antibody responses. Int. J. Infect. Dis. 3:140-146. [DOI] [PubMed] [Google Scholar]
- 52.Bergquist, S. O., S. Bernander, H. Dahnsjo, and B. Sundelof. 1987. Erythromycin in the treatment of pertussis: a study of bacteriologic and clinical effects. Pediatr. Infect. Dis. J. 6:458-461. [DOI] [PubMed] [Google Scholar]
- 53.Bernales, R., J. Eastman, and J. Kaplan. 1976. Quantitation of circulating T and B lymphocytes in children with whooping cough. Pediatr. Res. 10:965-967. [DOI] [PubMed] [Google Scholar]
- 54.Bernier, R. H., J. A. Frank, Jr., T. J. Dondero, Jr., and P. Turner. 1982. Diphtheria-tetanus toxoids-pertussis vaccination and sudden infant deaths in Tennessee. J. Pediatr. 101:419-421. [DOI] [PubMed] [Google Scholar]
- 55.Birkebaek, N. H., M. Kristiansen, T. Seefeldt, J. Degn, A. Moller, I. Heron, P. L. Andersen, J. K. Moller, and L. Ostergard. 1999. Bordetella pertussis and chronic cough in adults. Clin. Infect. Dis. 29:1239-1242. [DOI] [PubMed] [Google Scholar]
- 56.Bisgard, K. M., F. B. Pascual, K. R. Ehresmann, C. A. Miller, C. Cianfrini, C. E. Jennings, C. A. Rebmann, J. Gabel, S. L. Schauer, and S. M. Lett. 2004. Infant pertussis: who was the source? Pediatr. Infect. Dis. J. 23:985-989. [DOI] [PubMed] [Google Scholar]
- 57.Black, S. B., J. D. Cherry, H. R. Shinefield, B. Fireman, P. Christenson, and D. Lampert. 1991. Apparent decreased risk of invasive bacterial disease after heterologous childhood immunization. Am. J. Dis. Child. 145:746-749. [PubMed] [Google Scholar]
- 58.Blennow, M. S., S. Hedenskog, and M. Grantstrom. 1988. Protective effect of acellular pertussis vaccines. Eur. J. Clin. Microbiol. Infect. Dis. 7:381. [DOI] [PubMed] [Google Scholar]
- 59.Bloemen, P. G., M. C. Van den Tweel, P. A. Henricks, F. Engels, M. J. Van de Velde, F. J. Blomjous, and F. P. Nijkamp. 1996. Stimulation of both human bronchial epithelium and neutrophils is needed for maximal interactive adhesion. Am. J. Physiol. 270:L80-L87. [DOI] [PubMed] [Google Scholar]
- 60.Blumberg, D. A., E. Pineda, L. P. Smith, P. Chatfield, C. M. Mink, P. D. Christenson, and J. D. Cherry. 1990. Cell-mediated immune responses in patients with pertussis and in asymptomatic exposed contacts, p. 175-178. Sixth International Symposium on Pertussis, Bethesda, Md.
- 61.Bokoch, G. M., and A. G. Gilman. 1984. Inhibition of receptor-mediated release of arachidonic acid by pertussis toxin. Cell 39:301-308. [DOI] [PubMed] [Google Scholar]
- 62.Bordet, J., and O. Gengou. 1909. L'endotoxine coquelucheuse. Ann. Inst. Pasteur 23:415-419. [Google Scholar]
- 63.Bordet, J., and O. Gengou. 1906. Le microbe de la coqueluche. Ann. Inst. Pasteur 20:48-68. [Google Scholar]
- 64.Bordon, D., and W. Kulp. 1939. A study of rat pneumonia. J. Bacteriol. 37:351-352. [Google Scholar]
- 65.Borras Sans, M., J. Bonal, J. Bonet, J. Arnal, F. Roca, and A. Caralps. 1991. Bordetella bronchiseptica septicemia in a hemodialysis patient. Nephron 59:676. [DOI] [PubMed] [Google Scholar]
- 66.Borska, K., and M. Simkovicova. 1972. Studies on the circulation of Bordetella pertussis and Bordetella parapertussis in populations of children. J. Hyg. Epidemiol. Microbiol. Immunol. 16:159-172. [PubMed] [Google Scholar]
- 67.Boschwitz, J. S., J. W. Batanghari, H. Kedem, and D. A. Relman. 1997. Bordetella pertussis infection of human monocytes inhibits antigen-dependent CD4 T cell proliferation. J. Infect. Dis. 176:678-686. [DOI] [PubMed] [Google Scholar]
- 68.Boschwitz, J. S., H. G. van der Heide, F. R. Mooi, and D. A. Relman. 1997. Bordetella bronchiseptica expresses the fimbrial structural subunit gene fimA. J. Bacteriol. 179:7882-7885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Boucher, P. E., A. E. Maris, M. S. Yang, and S. Stibitz. 2003. The response regulator BvgA and RNA polymerase alpha subunit C-terminal domain bind simultaneously to different faces of the same segment of promoter DNA. Mol. Cell 11:163-173. [DOI] [PubMed] [Google Scholar]
- 70.Boucher, P. E., and S. Stibitz. 1995. Synergistic binding of RNA polymerase and BvgA phosphate to the pertussis toxin promoter of Bordetella pertussis. J. Bacteriol. 177:6486-6491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Boucher, P. E., M. S. Yang, D. M. Schmidt, and S. Stibitz. 2001. Genetic and biochemical analyses of BvgA interaction with the secondary binding region of the fha promoter of Bordetella pertussis. J. Bacteriol. 183:536-544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bradford, P. G., and R. P. Rubin. 1985. Pertussis toxin inhibits chemotactic factor-induced phospholipase C stimulation and lysosomal enzyme secretion in rabbit neutrophils. FEBS Lett. 183:317-320. [DOI] [PubMed] [Google Scholar]
- 73.Bradford, W. L., and B. Slavin. 1937. An organism resembling Hemophilus pertussis with special reference to color changes produced by its growth upon certain media. Am. J. Public Health 27:1277-1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Brandt, S. J., R. W. Dougherty, E. G. Lapetina, and J. E. Niedel. 1985. Pertussis toxin inhibits chemotactic peptide-stimulated generation of inositol phosphates and lysosomal enzyme secretion in human leukemic (HL-60) cells. Proc. Natl. Acad. Sci. USA 82:3277-3280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Brennan, M. J., Z. M. Li, J. L. Cowell, M. E. Bisher, A. C. Steven, P. Novotny, and C. R. Manclark. 1988. Identification of a 69-kilodalton nonfimbrial protein as an agglutinogen of Bordetella pertussis. Infect. Immun. 56:3189-3195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Brito, G. A., M. H. Souza, A. A. Melo-Filho, E. L. Hewlett, A. A. Lima, C. A. Flores, and R. A. Ribeiro. 1997. Role of pertussis toxin A subunit in neutrophil migration and vascular permeability. Infect. Immun. 65:1114-1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Brooksaler, F., and J. D. Nelson. 1967. Pertussis. A reappraisal and report of 190 confirmed cases. Am. J. Dis. Child. 114:389-396. [DOI] [PubMed] [Google Scholar]
- 78.Broome, C. V., and D. W. Fraser. 1981. Pertussis in the United States, 1979: a look at vaccine efficacy. J. Infect. Dis. 144:187-190. [DOI] [PubMed] [Google Scholar]
- 79.Brown, J. H. 1926. Bacillus bronchisepticus infection in a child with symptoms of pertussis. Bull. Johns Hopkins Hosp. 38:147-153. [Google Scholar]
- 80.Buck, C. 1977. Whooping-cough vaccination. Lancet i:746-747. [PubMed] [Google Scholar]
- 81.Buck, G. E. 1996. Detection of Bordetella pertussis by rapid-cycle PCR and colorimetric microwell hybridization. J. Clin. Microbiol. 34:1355-1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Buggy, B. P., F. C. Brosius III, R. M. Bogin, C. A. Koller, and D. R. Schaberg. 1987. Bordetella bronchiseptica pneumonia in a patient with chronic lymphocytic leukemia. South. Med. J. 80:1187-1189. [DOI] [PubMed] [Google Scholar]
- 83.Burner, D. W., and J. H. Gillespie. 1973. The genus Bordetella, p. 193-196. In D. W. Burner and J. H. Gillespie (ed.), Hagan's infectious diseases of domestic animals—with special reference to etiology, diagnosis, and biologic therapy, 6th ed. Cornell University Press, London, United Kingdom.
- 84.Burns, D. L., S. Fiddner, A. M. Cheung, and A. Verma. 2004. Analysis of subassemblies of pertussis toxin subunits in vivo and their interaction with the ptl transport apparatus. Infect. Immun. 72:5365-5372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Burns, V. C., E. J. Pishko, A. Preston, D. J. Maskell, and E. T. Harvill. 2003. Role of Bordetella O antigen in respiratory tract infection. Infect. Immun. 71:86-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Butler, N. R., J. Golding, M. Haslum, and S. Stewart-Brown. 1982. Recent findings from the 1970 child health and education study: preliminary communication. J. R. Soc. Med. 75:781-784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Byers, R. K., and F. C. Moll. 1948. Encephalopathies following prophylactic pertussis vaccine. Pediatrics 1:437-457. [PubMed] [Google Scholar]
- 88.Byrd, L. H., L. Anama, M. Gutkin, and H. Chmel. 1981. Bordetella bronchiseptica peritonitis associated with continuous ambulatory peritoneal dialysis. J. Clin. Microbiol. 14:232-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Cahill, E. S., D. T. O'Hagan, L. Illum, and K. Redhead. 1993. Mice are protected against Bordetella pertussis infection by intranasal immunization with filamentous haemagglutinin. FEMS Microbiol. Lett. 107:211-216. [DOI] [PubMed] [Google Scholar]
- 89a.Carine Vaccine Task Force. 2003. Canine vaccination guidelines, recommendations, and supporting literature. Report, American Animal Hospital Association, Lakewood, Colo. [DOI] [PubMed]
- 90.Carbonetti, N. H., G. V. Artamonova, C. Andreasen, E. Dudley, R. M. Mays, and Z. E. Worthington. 2004. Suppression of serum antibody responses by pertussis toxin after respiratory tract colonization by Bordetella pertusis and identification of an immunodominant lipoprotein. Infect. Immun. 72:3350-3358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Carbonetti, N. H., G. V. Artamonova, R. M. Mays, and Z. E. Worthington. 2003. Pertussis toxin plays an early role in respiratory tract colonization by Bordetella pertussis. Infect. Immun. 71:6358-6366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Caroff, M., R. Chaby, D. Karibian, J. Perry, C. Deprun, and L. Szabo. 1990. Variations in the carbohydrate regions of Bordetella pertussis lipopolysaccharides: electrophoretic, serological and structural features. J. Bacteriol. 172:1121-1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Carter, G. R., M. M. Chengappa, A. W. Roberts, G. W. Claus, and Y. Rikihisa. 1995. Bordetella and Moraxella, p. 194-198. In G. R. Carter, M. M. Chengappa, A. W. Roberts, G. W. Claus, and Y. Rikihisa (ed.), Essentials of veterinary microbiology, 5th ed. Williams & Wilkins, Philadalphia, Pa.
- 94.Cassone, A., C. M. Ausiello, F. Urbani, R. Lande, M. Giuliano, A. La Sala, A. Piscitelli, S. Salmaso, and The Progetto Pertosse-CMI Working Group. 1997. Cell-mediated and antibody responses to Bordetella pertussis antigens in children vaccinated with acellular or whole-cell pertussis vaccines. Arch. Pediatr. Adolesc. Med. 151:283-289. [DOI] [PubMed] [Google Scholar]
- 95.Celermajer, J. M., and J. Brown. 1969. The neurological complications of pertussis. Med. J. Aust. 53:1066-1069. [DOI] [PubMed] [Google Scholar]
- 96.Centers for Disease Control. 1981. Annual summary 1980. Reported morbidity & mortality in the United States. Morb. Mortal. Wkly. Rep. 29:1-128. [PubMed] [Google Scholar]
- 97.Centers for Disease Control. 1982. Annual summary 1981. Reported morbidity & mortality in the United States. Morb. Mortal. Wkly. Rep. 30:1-132. [PubMed] [Google Scholar]
- 98.Centers for Disease Control. 1983. Annual summary 1982. Reported morbidity & mortality in the United States. Morb. Mortal. Wkly. Rep. 31:1-149. [PubMed] [Google Scholar]
- 99.Centers for Disease Control. 1986. Annual summary 1984. Reported morbidity and mortality in the United States. Morb. Mortal. Wkly. Rep. 33:1-135. [PubMed] [Google Scholar]
- 100.Centers for Disease Control. 1990. Summary of notifiable diseases in the United States, 1989. Morb. Mortal. Wkly. Rep. 38:1-59. [PubMed] [Google Scholar]
- 101.Centers for Disease Control. 1985. Summary of notifiable diseases in the United States, 1985. Morb. Mortal. Wkly. Rep. 34:1-21. [PubMed] [Google Scholar]
- 102.Centers for Disease Control. 1987. Summary of notifiable diseases, United States, 1986. Morb. Mortal. Wkly. Rep. 35:1-57. [PubMed] [Google Scholar]
- 103.Centers for Disease Control. 1988. Summary of notifiable diseases, United States, 1987. Morb. Mortal. Wkly. Rep. 36:1-59. [PubMed] [Google Scholar]
- 104.Centers for Disease Control. 1989. Summary of notifiable diseases, United States, 1988. Morb. Mortal. Wkly. Rep. 37:1-57. [PubMed] [Google Scholar]
- 105.Centers for Disease Control. 1991. Summary of notifiable diseases, United States, 1990. Morb. Mortal. Wkly. Rep. 39:1-61. [PubMed] [Google Scholar]
- 106.Centers for Disease Control. 1984. Adverse events following immunization: surveillance report no. 1, 1979-1982. Centers for Disease Control, Atlanta, Ga.
- 107.Centers for Disease Control. 1979. DTP vaccination and sudden infant deaths—Tennessee. Morb. Mortal. Wkly. Rep. 28:131. [Google Scholar]
- 108.Centers for Disease Control. 1979. DTP vaccination follow-up—Tennessee. Morb. Mortal. Wkly. Rep. 28:134. [Google Scholar]
- 109.Centers for Disease Control. 1984. Pertussis—United States, 1982 and 1983. Morb. Mortal. Wkly. Rep. 33:573-575. [PubMed] [Google Scholar]
- 110.Centers for Disease Control. 1987. Pertussis immunization: family history of convulsions and use of antipyretics—supplementary ACIP statement. Morb. Mortal. Wkly. Rep. 36:281-282. [PubMed] [Google Scholar]
- 111.Centers for Disease Control. 1982. Pertussis surveillance, 1979-1981. Morb. Mortal. Wkly. Rep. 31:333-336. [PubMed] [Google Scholar]
- 112.Centers for Disease Control and Prevention. 2002. Pertussis—United States, 1997-2000. Age distribution and incidence of reported cases. http://www.cdc.gov/nip/ed/slides/pertussis8p.ppt.
- 113.Centers for Disease Control and Prevention. 2000. Summary of notifiable diseases—United States, 1999. Morb. Mortal. Wkly. Rep. 48:13. [Google Scholar]
- 114.Centers for Disease Control and Prevention. 2001. Summary of notifiable diseases—United States, 2000. Morb. Mortal. Wkly. Rep. 49:1-100. [PubMed] [Google Scholar]
- 115.Centers for Disease Control and Prevention. 2002. Summary of notifiable diseases—United States, 2001. Morb. Mortal. Wkly. Rep. 50:1-108. [PubMed] [Google Scholar]
- 116.Centers for Disease Control and Prevention. 2004. Summary of notifiable diseases—United States, 2002. Morb. Mortal. Wkly. Rep. 51:1-84. [PubMed] [Google Scholar]
- 117.Centers for Disease Control and Prevention. 1992. Summary of notifiable diseases, United States, 1991. Morb. Mortal. Wkly. Rep. 40:1-63. [PubMed] [Google Scholar]
- 118.Centers for Disease Control and Prevention. 1993. Summary of notifiable diseases, United States, 1992. Morb. Mortal. Wkly. Rep. 41:1-73. [PubMed] [Google Scholar]
- 119.Centers for Disease Control and Prevention. 1994. Summary of notifiable diseases, United States, 1994. Morb. Mortal. Wkly. Rep. 43:1-80. [PubMed] [Google Scholar]
- 120.Centers for Disease Control and Prevention. 1996. Summary of notifiable diseases, United States, 1995. Morb. Mortal. Wkly. Rep. 44:1-87. [PubMed] [Google Scholar]
- 121.Centers for Disease Control and Prevention. 1994. Summary of notifiable diseases, United States, 1993. Morb. Mortal. Wkly. Rep. 42:1-73. [PubMed] [Google Scholar]
- 122.Centers for Disease Control and Prevention. 1997. Summary of notifiable diseases, United States, 1996. Morb. Mortal. Wkly. Rep. 45:1-87. [PubMed] [Google Scholar]
- 123.Centers for Disease Control and Prevention. 1998. Summary of notifiable diseases, United States, 1997, Morb. Mortal, Wkly. Rep. 46:1-87. [PubMed] [Google Scholar]
- 124.Centers for Disease Control and Prevention. 1999. Summary of notifiable Diseases, United States, 1998. Morb. Mortal. Wkly. Rep. 47:1-92. [PubMed] [Google Scholar]
- 124a.Centers for Disease Control and Prevention. 2004. Fatal case of unsuspected pertusis diagnosed from a blood culture—Minnesota, 2003. Morb. Mortal, Wkly. Rep. 53:131-132. [PubMed] [Google Scholar]
- 125.Chang, K. C., R. M. Zakhein, C. T. Cho, and J. C. Montgomery. 1975. Posttraumatic purulent meningitis due to Bordetella bronchiseptica. J. Pediatr. 86:639-640. (Letter). [DOI] [PubMed] [Google Scholar]
- 126.Chang, S. M. 1950. Pertussis due to Brucella bronchoseptica. Case report. Pediatrics 6:227-228. [PubMed] [Google Scholar]
- 127.Charles, I., N. Fairweather, D. Pickard, J. Beesley, R. Anderson, G. Dougan, and M. Roberts. 1994. Expression of the Bordetella pertussis P.69 pertactin adhesin in Escherichia coli: fate of the carboxy-terminal domain. Microbiology 140:3301-3308. [DOI] [PubMed] [Google Scholar]
- 128.Charles, I. G., G. Dougan, D. Pickard, S. Chatfield, M. Smith, P. Novotny, P. Morrissey, and N. F. Fairweather. 1989. Molecular cloning and characterization of protective outer membrane protein P.69 from Bordetella pertussis. Proc. Natl. Acad. Sci. USA 86:3554-3558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Chauncey, J. B., and D. R. Schaberg. 1990. Interstitial pneumonia caused by Bordetella bronchiseptica in a heart transplant patient. Transplantation 49:817-819. [PubMed] [Google Scholar]
- 130.Cherry, J. D. 1993. Acellular pertussis vaccines—a solution to the pertussis problem. J. Infect. Dis. 168:21-24. [DOI] [PubMed] [Google Scholar]
- 131.Cherry, J. D. 1997. Comparative efficacy of acellular pertussis vaccines: an analysis of recent trials. Pediatr. Infect. Dis. J. 16:S90-S96. [DOI] [PubMed] [Google Scholar]
- 132.Cherry, J. D. 2003. Comparison of the epidemiology of the disease pertussis vs. the epidemiology Bordtella pertussis infection. Pediatr. Res. 53:324A. [Google Scholar]
- 133.Cherry, J. D. 1986. The controversy about pertussis vaccine, p. 216-238. In J. S. Remington and M. N. Swartz (ed.), Current clinical topics in infectious diseases. McGraw-Hill Book Co., New York, N.Y.
- 134.Cherry, J. D. 2004. Enteroviruses and parechoviruses, p. 1984. In R. D. Feigin, J. D. Cherry, G. J. Demmler, and S. L. Kaplan (ed.), Textbook of pediatric infectious diseases, 5th ed. The W. B. Saunders Co., Philadelphia, Pa.
- 135.Cherry, J. D. 1999. Epidemiological, clinical, and laboratory aspects of pertussis in adults. Clin. Infect. Dis. 28(Suppl. 2):S112-S117. [DOI] [PubMed] [Google Scholar]
- 136.Cherry, J. D. 1984. The epidemiology of pertussis and pertussis immunization in the United Kingdom and the United States: a comparative study. Curr. Probl. Pediatr. 14:1-78. [DOI] [PubMed] [Google Scholar]
- 137.Cherry, J. D. 1996. Historical review of pertussis and the classical vaccine. J. Infect. Dis. 174(Suppl. 3):S259-S63. [DOI] [PubMed] [Google Scholar]
- 138.Cherry, J. D. 2004. Measles, p. 2283-2304. In R. D. Feigin, J. D. Cherry, G. J. Demmler, and S. L. Kaplan (ed.), Textbook of pediatric infectious diseases, 5th ed. The W. B. Saunders Co., Philadelphia, Pa.
- 139.Cherry, J. D. 1995. Nosocomial pertussis in the nineties. Infect. Control Hosp. Epidemiol. 16:553-555. [DOI] [PubMed] [Google Scholar]
- 140.Cherry, J. D. 1989. Pertussis and the vaccine controversy, p. 47-63. In R. K. Root, J. M. Friffiss, K. S. Warren, et al. (ed.), Immunization. Churchill Livingstone, New York, N.Y.
- 141.Cherry, J. D. 1999. Pertussis in the preantibiotic and prevaccine era, with emphasis on adult pertussis. Clin. Infect. Dis. 28(Suppl. 2):S107-S111. [DOI] [PubMed] [Google Scholar]
- 142.Cherry, J. D. 1990. ‘Pertussis vaccine encephalopathy’: it is time to recognize it as the myth that it is. JAMA 263:1679-1680. [PubMed] [Google Scholar]
- 143.Cherry, J. D. 1992. Pertussis: the trials and tribulations of old and new pertussis vaccines. Vaccine 10:1033-1038. [DOI] [PubMed] [Google Scholar]
- 144.Cherry, J. D. 2003. The science and fiction of the “resurgence” of pertussis. Pediatrics 112:405-406. [DOI] [PubMed] [Google Scholar]
- 145.Cherry, J. D., L. J. Baraff, and E. Hewlett. 1989. The past, present, and future of pertussis. The role of adults in epidemiology and future control. West. J. Med. 150:319-328. [PMC free article] [PubMed] [Google Scholar]
- 146.Cherry, J. D., T. Beer, S. A. Chartrand, J. DeVille, E. Beer, M. A. Olsen, P. D. Christenson, C. V. Moore, and K. Stehr. 1995. Comparison of values of antibody to Bordetella pertussis antigens in young German and American men. Clin. Infect. Dis. 20:1271-1274. [DOI] [PubMed] [Google Scholar]
- 147.Cherry, J. D., P. A. Brunell, G. S. Golden, and D. T. Karson. 1988. Report of the task force on pertussis and pertussis immunization—1988. Pediatrics 81:939. [Google Scholar]
- 148.Cherry, J. D., J. Gornbein, U. Heininger, and K. Stehr. 1998. A search for serologic correlates of immunity to Bordetella pertussis cough illnesses. Vaccine 16:1901-1906. [DOI] [PubMed] [Google Scholar]
- 149.Cherry, J. D., and U. Heininger. 2004. Pertussis and other Bordetella infections, p. 1588-1608. In R. D. Feigin, J. D. Cherry, G. J. Demmler, and S. Kaplan (ed.), Textbook of pediatric infectious diseases, 5th ed. The W. B. Saunders Co, Philadelphia, Pa.
- 150.Cherry, J. D., U. Heininger, K. Stehr, and P. Christenson. 1998. The effect of investigator compliance (observer bias) on calculated efficacy in a pertussis vaccine trial. Pediatrics 102:909-912. [DOI] [PubMed] [Google Scholar]
- 151.Cherry, J. D., and E. A. Mortimer, Jr. 1987. Acellular and whole-cell pertussis vaccines in Japan: report of a visit by US scientists. JAMA 257:1375-1376. [PubMed] [Google Scholar]
- 152.Cherry, J. D., and P. Olin. 1999. The science and fiction of pertussis vaccines. Pediatrics 104:1381-1383. [DOI] [PubMed] [Google Scholar]
- 153.Cherry, J. D., D. X. Xing, P. Newland, K. Patel, U. Heininger, and M. J. Corbel. 2004. Determination of serum antibody to Bordetella pertussis adenylate cyclase toxin in vaccinated and unvaccinated children and in children and adults with pertussis. Clin. Infect. Dis. 38:502-507. [DOI] [PubMed] [Google Scholar]
- 154.Choy, K. W., N. M. Wulffraat, T. F. Wolfs, S. P. Geelen, C. A. Kraaijeveld, and A. Fleer. 1999. Bordetella bronchiseptica respiratory infection in a child after bone marrow transplantation. Pediatr. Infect. Dis. J. 18:481-483. [DOI] [PubMed] [Google Scholar]
- 155.Christie, A. B. 1980. Infectious diseases: epidemiology and clinical practice, 3rd ed. p. 659. Churchill-Livingstone, London, United Kingdom.
- 156.Christie, C. D., and R. S. Baltimore. 1989. Pertussis in neonates. Am. J. Dis. Child. 143:1199-1202. [DOI] [PubMed] [Google Scholar]
- 157.Ciofi degli Atti, M. L., and P. Olin. 1997. Severe adverse events in the Italian and Stockholm I pertussis vaccine clinical trials. Dev. Biol. Stand. 89:77-81. [PubMed] [Google Scholar]
- 158.Cloud, J. L., W. C. Hymas, A. Turlak, A. Croft, U. Reischl, J. A. Daly, and K. C. Carroll. 2003. Description of a multiplex Bordetella pertussis and Bordetella parapertussis LightCycler PCR assay with inhibition control. Diagn. Microbiol. Infect. Dis. 46:189-195. [DOI] [PubMed] [Google Scholar]
- 159.Code of Federal Regulations. 1987. Food and Drugs, Title 21. Office of the Federal Register. National Archives and RecordsService, General Services Administration, Washington, D.C.
- 160.Cody, C. L., L. J. Baraff, J. D. Cherry, S. M. Marcy, and C. R. Manclark. 1981. Nature and rates of adverse reactions associated with DTP and DT immunizations in infants and children. Pediatrics 68:650-660. [PubMed] [Google Scholar]
- 161.Collier, A. M., J. D. Connor, and W. R. Irving, Jr. 1966. Generalized type 5 adenovirus infection associated with the pertussis syndrome. J. Pediatr. 69:1073-1078. [DOI] [PubMed] [Google Scholar]
- 162.Cone, T. E. J. 1970. Whooping cough is first described as a disease sui generis by Baillou in 1640. Pediatrics 46:522. [PubMed] [Google Scholar]
- 163.Confer, D. L., and J. W. Eaton. 1982. Phagocyte impotence caused by an invasive bacterial adenylate cyclase. Science 217:948-950. [DOI] [PubMed] [Google Scholar]
- 164.Confer, D. L., A. S. Slungaard, E. Graf, S. S. Panter, and J. W. Eaton. 1984. Bordetella adenylate cyclase toxin: entry of bacterial adenylate cyclase into mammalian cells. Adv. Cyclic Nucleotide Protein Phosphorylation Res. 17:183-187. [PubMed] [Google Scholar]
- 165.Congeni, B. L., D. M. Orenstein, and G. A. Nankervis. 1978. Three infants with neonatal pertussis: because of its atypical presentations, pertussis in the neonate may easily be overlooked. Clin. Pediatr. 17:113-118. [DOI] [PubMed] [Google Scholar]
- 166.Conner, J. D. 1970. Evidence for an etiological role of adenoviral infection in pertussis syndrome. N. Engl. J. Med. 283:390-394. [DOI] [PubMed] [Google Scholar]
- 167.Conner, J. S., and J. F. Speers. 1963. A comparison between undesirable reactions to extracted pertussis antigen and to whole-cell antigen in DPT combinations. J. Iowa Med. Soc. 53:340-343. [PubMed] [Google Scholar]
- 168.Reference deleted.
- 169.Cookson, B. T., H. L. Cho, L. A. Herwaldt, and W. E. Goldman. 1989. Biological activities and chemical composition of purified tracheal cytotoxin of Bordetella pertussis. Infect. Immun. 57:2223-2229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Cookson, B. T., A. N. Tyler, and W. E. Goldman. 1989. Primary structure of the peptidoglycan-derived tracheal cytotoxin of Bordetella pertussis. Biochemistry 28:1744-1749. [DOI] [PubMed] [Google Scholar]
- 171.Cookson, B. T., P. Vandamme, L. C. Carlson, A. M. Larson, J. V. Sheffield, K. Kersters, and D. H. Spach. 1994. Bacteremia caused by a novel Bordetella species, “B. hinzii.” J. Clin. Microbiol. 32:2569-2571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Cornelis, G. R., and F. Van Gijsegem. 2000. Assembly and function of type III secretory systems. Annu. Rev. Microbiol. 54:735-774. [DOI] [PubMed] [Google Scholar]
- 173.Costerton, J. W., P. S. Stewart, and E. P. Greenberg. 1999. Bacterial biofilms: a common cause of persistent infections. Science 284:1318-1322. [DOI] [PubMed] [Google Scholar]
- 174.Cotter, P. A., and J. F. Miller. 2001. Bordetella, p. 619-674. In E. A. Groisman (ed.), Principles of bacterial pathogenesis. Academic Press, Ltd., London, United Kingdom.
- 175.Cotter, P. A., and J. F. Miller. 1994. BvgAS-mediated signal transduction: analysis of phase-locked regulatory mutants of Bordetella bronchiseptica in a rabbit model. Infect. Immun. 62:3381-3390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Cotter, P. A., and J. F. Miller. 1997. A mutation in the Bordetella bronchiseptica bvgS gene results in reduced virulence and increased resistance to starvation, and identifies a new class of Bvg-regulated antigens. Mol. Microbiol. 24:671-685. [DOI] [PubMed] [Google Scholar]
- 177.Cotter, P. A., M. H. Yuk, S. Mattoo, B. J. Akerley, J. Boschwitz, D. A. Relman, and J. F. Miller. 1998. Filamentous hemagglutinin of Bordetella bronchiseptica is required for efficient establishment of tracheal colonization. Infect. Immun. 66:5921-5929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Coulter, H. L., and B. L. Fisher. 1985. DPT: a shot in the dark. Harcourt Brace Jovanovich, New York, N.Y.
- 179.Coutte, L., S. Alonso, N. Reveneau, E. Willery, B. Quatannens, C. Locht, and F. Jacob-Dubuisson. 2003. Role of adhesin release for mucosal colonization by a bacterial pathogen. J. Exp. Med. 197:735-742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Coutte, L., R. Antoine, H. Drobecq, C. Locht, and F. Jacob-Dubuisson. 2001. Subtilisin-like autotransporter serves as maturation protease in a bacterial secretion pathway. EMBO J. 20:5040-5048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Coutte, L., E. Willery, R. Antoine, H. Drobecq, C. Locht, and F. Jacob-Dubuisson. 2003. Surface anchoring of bacterial subtilisin important for maturation function. Mol. Microbiol. 49:529-539. [DOI] [PubMed] [Google Scholar]
- 182.Covacci, A., and R. Rappuoli. 1993. Pertussis toxin export requires accessory genes located downstream from the pertussis toxin operon. Mol. Microbiol. 8:429-434. [DOI] [PubMed] [Google Scholar]
- 183.Cowell, J. L., E. L. Hewlett, and C. R. Manclark. 1979. Intracellular localization of the dermonecrotic toxin of Bordetella pertussis. Infect. Immun. 25:896-901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Cromer, B. A., J. Goydos, J. Hackell, J. Mezzatesta, C. Dekker, and E. A. Mortimer. 1993. Unrecognized pertussis infection in adolescents. Am. J. Dis. Child. 147:575-577. [DOI] [PubMed] [Google Scholar]
- 185.Crowcroft, N. S., N. Andrews, C. Rooney, M. Brisson, and E. Miller. 2002. Deaths from pertussis are underestimated in England. Arch. Dis. Child. 86:336-338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Crowcroft, N. S., R. Booy, T. Harrison, L. Spicer, J. Britto, Q. Mok, P. Heath, I. Murdoch, M. Zambon, R. George, and E. Miller. 2003. Severe and unrecognised: pertussis in UK infants. Arch. Dis. Child. 88:802-806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Crowcroft, N. S., C. Stein, P. Duclos, and M. Birmingham. 2003. How best to estimate the global burden of pertussis? Lancet Infect. Dis. 3:413-418. [DOI] [PubMed] [Google Scholar]
- 188.Cuesta, J., T. Hermosilla, B. Gros, S. Zabala, and M. C. Garcia. 1991. Pneumonia caused by Bordetella bronchiseptica in a patient with Crohn's disease. An. Med. Interna 8:525-526. (In Spanish.) [PubMed] [Google Scholar]
- 189.Cummings, C. A., M. M. Brinig, P. W. Lepp, S. van de Pas, and D. A. Relman. 2004. Bordetella species are distinguished by patterns of substantial gene loss and host adaptation. J. Bacteriol. 186:1484-1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Dahlback, M., H. Bergstrand, R. Pauwels, and H. Bazin. 1983. The nonspecific enhancement of allergy. III. Precipitation of bronchial anaphylactic reactivity in primed rats by injection of alum or B. pertussis vaccine: relation of response capacity to IgE and IgG2a antibody levels. Allergy 38:261-271. [DOI] [PubMed] [Google Scholar]
- 191.Dale, A. J. D., and J. E. Geraci. 1961. Mixed cardiac valvular infections: report of case and review of literature. Proc. Staff Meet, Mayo Clin. 36:288-294. [Google Scholar]
- 192.Dale, C., G. R. Plague, B. Wang, H. Ochman, and N. A. Moran. 2002. Type III secretion systems and the evolution of mutualistic endosymbiosis. Proc. Natl. Acad. Sci. USA 99:12397-12402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Reference deleted.
- 194.Davidson, M., G. W. Letson, J. I. Ward, A. Ball, L. Bulkow, P. Christenson, and J. D. Cherry. 1991. DTP immunization and susceptibility to infectious diseases. Is there a relationship? Am. J. Dis. Child. 145:750-754. [PubMed] [Google Scholar]
- 195.Davis, L. E., D. G. Burstyn, and C. R. Manclark. 1984. Pertussis encephalopathy with a normal brain biopsy and elevated lymphocytosis-promoting factor antibodies. Pediatr. Infect. Dis. 3:448-451. [DOI] [PubMed] [Google Scholar]
- 196.Davis, S. F., R. W. Sutter, P. M. Strebel, C. Orton, V. Alexander, G. N. Sanden, G. H. Cassell, W. L. Thacker, and S. L. Cochi. 1995. Concurrent outbreaks of pertussis and Mycoplasma pneumoniae infection: clinical and epidemiological characteristics of illnesses manifested by cough. Clin. Infect. Dis. 20:621-628. [DOI] [PubMed] [Google Scholar]
- 197.Decker, M. D., and K. M. Edwards (ed.). 1995. Report of the nationwide multicenter acellular pertussis trial. Pediatrics 96:(Suppl.):547-603.7659474 [Google Scholar]
- 198.Decker, M. D., K. M. Edwards, M. C. Steinhoff, M. B. Rennels, M. E. Pichichero, J. A. Englund, E. L. Anderson, M. A. Deloria, and G. F. Reed. 1995. Comparison of 13 acellular pertussis vaccines: adverse reactions. Pediatrics 96:557-566. [PubMed] [Google Scholar]
- 199.Deeb, B. J., R. F. DiGiacomo, B. L. Bernard, and S. M. Silbernagel. 1990. Pasteurella multocida and Bordetella bronchiseptica infections in rabbits. J. Clin. Microbiol. 28:70-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Deen, J. L., C. A. Mink, J. D. Cherry, P. D. Christenson, E. F. Pineda, K. Lewis, D. A. Blumberg, and L. A. Ross. 1995. Household contact study of Bordetella pertussis infections. Clin. Infect. Dis. 21:1211-1219. [DOI] [PubMed] [Google Scholar]
- 201.De Jong, M. F. 1992. (Progressive) atrophic rhinitis, p. 415-435. In D. J. Taylor (ed.), Diseases of swine, 7th ed., Wolfe, Ames, Iowa.
- 202.de la Fuente, J., C. Albo, A. Rodriguez, B. Sopena, and C. Martinez. 1994. Bordetella bronchiseptica pneumonia in a patient with AIDS. Thorax 49:719-720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Deora, R. 2002. Differential regulation of the Bordetella bipA gene: distinct roles for different BvgA binding sites. J. Bacteriol. 184:6942-6951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Deora, R., H. J. Bootsma, J. F. Miller, and P. A. Cotter. 2001. Diversity in the Bordetella virulence regulon: transcriptional control of a Bvg-intermediate phase gene. Mol. Microbiol. 40:669-683. [DOI] [PubMed] [Google Scholar]
- 205.De Serres, G., R. Shadmani, B. Duval, N. Boulianne, P. Dery, M. Douville Fradet, L. Rochette, and S. A. Halperin. 2000. Morbidity of pertussis in adolescents and adults. J. Infect. Dis. 182:174-179. [DOI] [PubMed] [Google Scholar]
- 206.Deville, J. G., J. D. Cherry, P. D. Christenson, E. Pineda, C. T. Leach, T. L. Kuhls, and S. Viker. 1995. Frequency of unrecognized Bordetella pertussis infections in adults. Clin. Infect. Dis. 21:639-642. [DOI] [PubMed] [Google Scholar]
- 207.Dick, G. 1974. Convulsive disorders in young children. Proc. R. Soc. Med. 67:15. [PMC free article] [PubMed] [Google Scholar]
- 208.Di Fabio, J. L., M. Caroff, D. Karibian, J. C. Richards, and M. B. Perry. 1992. Characterization of the common antigenic lipopolysaccharide O-chains produced by Bordetella bronchiseptica and Bordetella parapertussis. FEMS Microbiol. Lett. 76:275-281. [DOI] [PubMed] [Google Scholar]
- 209.Dolgopol, V. B. 1941. Changes in the brain in pertussis with convulsions. Arch. Neurol. Psychiatry 46:477-503. [Google Scholar]
- 210.Dragsted, D. M., B. Dohn, J. Madsen, and J. S. Jensen. 2004. Comparison of culture and PCR for detection of Bordetella pertussis and Bordetella parapertussis under routine laboratory conditions. J. Med. Microbiol. 53:749-754. [DOI] [PubMed] [Google Scholar]
- 211.Dunne, H. W., D. C. Kradel, and R. B. Doty. 1961. Bordetella bronchiseptica (Brucella bronchiseptica) in pneumonia in young pigs. J. Biochem. (Tokyo) 139:897-899. [PubMed] [Google Scholar]
- 212.Dworkin, M. S., P. S. Sullivan, S. E. Buskin, R. D. Harrington, J. Olliffe, R. D. MacArthur, and C. E. Lopez. 1999. Bordetella bronchiseptica infection in human immunodeficiency virus-infected patients. Clin. Infect. Dis. 28:1095-1099. [DOI] [PubMed] [Google Scholar]
- 213.Edsall, G. 1970. Comment, p. 170, International Symposium on Pertussis, Bilthoven, 1969. Immunobiologic standards, vol. 13. S. Karger, New York, N.Y.
- 214.Edsall, G. 1975. Present status of pertussis vaccination. Practitioner 215:310-314. [PubMed] [Google Scholar]
- 215.Edwards, J. T. G. 1957. The European hedgehog, p. 310-314. In A. N. Warden and W. Lane-Pelter (ed.), Universities Federation for Animal Welfare handbook on the care and management of laboratory animals, 2nd ed. Universities Federation for Animal Welfare, London, United Kingdom.
- 216.Edwards, K. M., and M. D. Decker. 2004. Pertussis vaccine, p. 471-528. In S. Plotkin and W. A. Orenstein (ed.), Vaccines, 4th ed. Elsevier, Philadelphia, Pa.
- 217.Edwards, K. M., E. Lawrence, and P. F. Wright. 1986. Diphtheria, tetanus, and pertussis vaccine. A comparison of the immune response and adverse reactions to conventional and acellular pertussis components Am. J. Dis. Child. 140:867-871. [DOI] [PubMed] [Google Scholar]
- 218.Edwards, K. M., B. D. Meade, M. D. Decker, G. F. Reed, M. B. Rennels, M. C. Steinhoff, E. L. Anderson, J. A. Englund, M. E. Pichichero, and M. A. Deloria. 1995. Comparison of 13 acellular pertussis vaccines: overview and serologic response. Pediatrics 96:548-557. [PubMed] [Google Scholar]
- 219.Eldering, G., C. Hornbeck, and J. Baker. 1957. Serological study of Bordetella pertussis and related species. J. Bacteriol. 74:133-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Eldering, G., and P. Kendrick. 1938. Bacillus parapertussis: a species resembling both Bacillus pertussis and Bacillus bronchiseptica but identical with neither. J. Bacteriol. 35:561-572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Eldering, G., and P. Kendrick. 1937. A group of cultures resembling both Bacillus pertussis and Bacillus bronchiseptica but identical with neither. J. Bacteriol. 33:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Eldering, G., and P. Kendrick. 1952. Incidence of parapertussis in the Grand Rapids area as indicated by 16 years' experience with diagnostic cultures. Am. J. Public Health 42:27-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Ellenberg, J. H., D. G. Hirtz, and K. B. Nelson. 1984. Age at onset of seizures in young children. Ann. Neurol. 15:127-134. [DOI] [PubMed] [Google Scholar]
- 224.Elliott, H. 1991. Bordetella bronchiseptica in a closed cat colony. Vet. Rec. 129:474-475. [DOI] [PubMed] [Google Scholar]
- 225.Emsley, P., I. G. Charles, N. F. Fairweather, and N. W. Isaacs. 1996. Structure of Bordetella pertussis virulence factor P.69 pertactin. Nature 381:90-92. [DOI] [PubMed] [Google Scholar]
- 226.Emsley, P., G. McDermott, I. G. Charles, N. F. Fairweather, and N. W. Isaacs. 1994. Crystallographic characterization of pertactin, a membrane-associated protein from Bordetella pertussis. J. Mol. Biol. 235:772-773. [DOI] [PubMed] [Google Scholar]
- 227.Espino Aguilar, R., F. Gascon Luna, J. Amor Trucios, I. Mongil Ruiz, F. Garcia Caballero, and C. de la Torre Cecilia. 1992. Bacteremia caused by Bordetella bronchiseptica in the course of inflammatory tinea capitis. An. Esp. Pediatr. 36:323-325. (In Spanish.) [PubMed] [Google Scholar]
- 228.Everest, P., J. Li, G. Douce, I. Charles, J. De Azavedo, S. Chatfield, G. Dougan, and M. Roberts. 1996. Role of the Bordetella pertussis P.69/pertactin protein and the P.69/pertactin RGD motif in the adherence to and invasion of mammalian cells. Microbiology 142:3261-3268. [DOI] [PubMed] [Google Scholar]
- 229.Ewanowich, C. A., L. W. Chui, M. G. Paranchych, M. S. Peppler, R. G. Marusyk, and W. L. Albritton. 1993. Major outbreak of pertussis in northern Alberta, Canada: analysis of discrepant direct fluorescent-antibody and culture results by using polymerase chain reaction methodology. J. Clin. Microbiol. 31:1715-1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Ezzell, J. W., W. J. Dobrogosz, W. E. Kloos, and C. R. Manclark. 1981. Phase-shift markers in the genus Bordetella: loss of cytochrome d-629 in phase IV variants. Microbios 31:171-181. [PubMed] [Google Scholar]
- 231.Farizo, K. M., T. G. Cafarella, and D. L. Burns. 1996. Evidence for a ninth gene, ptll, in the locus encoding the pertussis toxin secretion system of Bordetella pertussis and formation of a Ptll-PtlF complex. J. Biol. Chem. 271:31643-31649. [DOI] [PubMed] [Google Scholar]
- 232.Farizo, K. M., S. L. Cochi, E. R. Zell, E. W. Brink, S. G. Wassilak, and P. A. Patriarca. 1992. Epidemiological features of pertussis in the United States, 1980-1989. Clin. Infect. Dis. 14:708-719. [DOI] [PubMed] [Google Scholar]
- 233.Farmer, T. W. 1975. Convulsive disorders, syncope and headache, p. 44-74. In T. W. Farmer (ed.), Pediatric neurology, 2nd ed. Harper & Row, Hagerstown, Md.
- 234.Farrell, J. D., M. McKeon, D. Daggard, M. J. Loeffelholz, C. J. Thompson, and T. K. S. Mukkur. 2000. Rapid-Cycle PCR method to detect Bordetella pertussis that fulfills all consensus recommendations for use of PCR in diagnosis of pertussis. J. Clin. Microbiol. 38:4499-4502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Farthing, J. R. 1971. The role of Bordetella pertussis as an adjuvant to antibody production. Br. J. Exp. Pathol. 42:614-622. [PMC free article] [PubMed] [Google Scholar]
- 236.Feigin, R. D., and J. D. Cherry. 1987. Pertussis, p. 1227-1238. In R. D. Feigin and J. D. Cherry (ed.), Textbook of pediatric infectious diseases, 2nd ed. The W. B. Saunders Co., Philadelphia, Pa.
- 237.Fenichel, G. M. 1983. The pertussis vaccine controversy. The danger of case reports. Arch. Neurol. 40:193-194. [DOI] [PubMed] [Google Scholar]
- 238.Fernandez, R. C., and A. A. Weiss. 1994. Cloning and sequencing of a Bordetella pertussis serum resistance locus. Infect. Immun. 62:4727-4738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Fernandez, R. C., and A. A. Weiss. 1996. Susceptibilities of Bordetella pertussis strains to antimicrobial peptides. Antimicrob. Agents Chemother. 40:1041-1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Ferry, N. S. 1912. Bacillus bronchisepticus (bronchicanis): the cause of distemper in dogs and a similar disease in other animals. Vet. J. 68:376-391. [Google Scholar]
- 241.Ferry, N. S. 1917. Canine distemper. Proc. Wis. Vet. Med. Assoc. 1917:80-88. [Google Scholar]
- 242.Ferry, N. S. 1911. Etiology of canine distemper. J. Infect. Dis. 8:399-420. [Google Scholar]
- 243.Ferry, N. S. 1910. A preliminary report of the bacterial findings in canine distemper. Am. Vet. Rev. 37:499-504. [Google Scholar]
- 244.Fine, P. E., and J. A. Clarkson. 1982. The recurrence of whooping cough: possible implications for assessment of vaccine efficacy. Lancet i:666-669. [DOI] [PubMed] [Google Scholar]
- 245.Fine, P. E., and J. A. Clarkson. 1987. Reflections on the efficacy of pertussis vaccines. Rev. Infect. Dis. 9:866-883. [DOI] [PubMed] [Google Scholar]
- 246.Finger, H. 1974. Bordetella pertussis as adjuvant, p. 132-166. In 4th International Convocation on Immunology, Buffalo, N.Y.
- 247.Finn, T. M., and D. F. Amsbaugh. 1998. Vag8, a Bordetella pertussis bvg-regulated protein. Infect. Immun. 66:3985-3989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Finn, T. M., and L. A. Stevens. 1995. Tracheal colonization factor: a Bordetella pertussis secreted virulence determinant. Mol. Microbiol. 16:625-634. [DOI] [PubMed] [Google Scholar]
- 249.Fisk, S. K., and O. A. Soave. 1973. Bordetella bronchiseptica in laboratory cats from central California. Lab. Anim. Sci. 23:33-35. [PubMed] [Google Scholar]
- 250.Flak, T. A., and W. E. Goldman. 1996. Autotoxicity of nitric oxide in airway disease. Am. J. Respir. Crit. Care Med. 154:S202-S206. [DOI] [PubMed] [Google Scholar]
- 251.Flak, T. A., and W. E. Goldman. 1999. Signalling and cellular specificity of airway nitric oxide production in pertussis. Cell. Microbiol. 1:51-60. [DOI] [PubMed] [Google Scholar]
- 252.Flosdorf, E. W., A. Bondi, H. Felton, and A. C. McGuiness. 1942. Studies with hemophilus pertussis. J. Pediatr. 21:625-634. [Google Scholar]
- 253.Reference deleted.
- 254.French-Constant, R., N. Waterfield, P. Daborn, S. Joyce, H. Bennett, C. Au, A. Dowling, S. Boundy, S. Reynolds, and D. Clarke. 2003. Photorhabdus: towards a functional genomic analysis of a symbiont and pathogen. FEMS Microbiol. Rev. 26:433-456. [DOI] [PubMed] [Google Scholar]
- 255.Friedman, R. L. 1988. Pertussis: the disease and new diagnostic methods. Clin. Microbiol. Rev. 1:365-376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Frolich, J. 1897. Beitrag zur pathologie des keuchustens. J. Klinderkrankh. 4:53-58. [Google Scholar]
- 257.Fuchslocher, B., L. L. Millar, and P. A. Cotter. 2003. Comparison of bipA alleles within and across Bordetella species. Infect. Immun. 71:3043-3052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Fulginiti, V. A. 1983. Sudden infant death syndrome, diphtheria-tetanus toxoid-pertussis vaccination and visits to the doctor: chance association or cause and effect? Pediatr. Infect. Dis. J. 2:5-6. [DOI] [PubMed] [Google Scholar]
- 259.Gale, J. L., P. B. Thapa, S. G. Wassilak, J. K. Bobo, P. M. Mendelman, and H. M. Foy. 1994. Risk of serious acute neurological illness after immunization with diphtheria-tetanus-pertussis vaccine. A population-based case-control study. JAMA 271:37-41. [PubMed] [Google Scholar]
- 260.Gallagher, G. L. 1965. Isolation of Bordetella bronchiseptica from horses. Vet. Rec. 77:632-633. [PubMed] [Google Scholar]
- 261.Garcia San Miguel, L., C. Quereda, M. Martinez, P. Martin-Davila, J. Cobo, and A. Guerrero. 1998. Bordetella bronchiseptica cavitary pneumonia in a patient with AIDS. Eur. J. Clin. Microbiol. Infect. Dis. 17:675-676. [DOI] [PubMed] [Google Scholar]
- 262.Gardner, P., W. B. Griffin, M. N. Swartz, and L. J. Kunz. 1970. Nonfermentative gram-negative bacilli of nosocomial interest. Am. J. Med. 48:735-749. [DOI] [PubMed] [Google Scholar]
- 263.Gentry-Weeks, C. R., B. T. Cookson, W. E. Goldman, R. B. Rimler, S. B. Porter, and R. Curtiss III. 1988. Dermonecrotic toxin and tracheal cytotoxin, putative virulence factors of Bordetella avium. Infect. Immun. 56:1698-1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Gerlach, G., F. von Wintzingerode, B. Middendorf, and R. Gross. 2001. Evolutionary trends in the genus Bordetella. Microbes Infect. 3:61-72. [DOI] [PubMed] [Google Scholar]
- 265.Geuijen, C. A., R. J. Willems, M. Bongaerts, J. Top, H. Gielen, and F. R. Mooi. 1997. Role of the Bordetella pertussis minor fimbrial subunit, FimD, in colonization of the mouse respiratory tract. Infect. Immun. 65:4222-4228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Geuijen, C. A., R. J. Willems, and F. R. Mooi. 1996. The major fimbrial subunit of Bordetella pertussis binds to sulfated sugars. Infect. Immun. 64:2657-2665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Ghosh, H. K., and J. Tranter. 1979. Bordetella bronchicanis (bronchiseptica) infection in man: review and a case report. J. Clin. Pathol. 32:546-548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Giardina, P. C., L. A. Foster, J. M. Musser, B. J. Akerley, J. F. Miller, and D. W. Dyer. 1995. bvg Repression of alcaligin synthesis in Bordetella bronchiseptica is associated with phylogenetic lineage. J. Bacteriol. 177:6058-6063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Gifford, C. G., E. C. Gonsior, G. V. Villacorte, A. Bewtra, and R. G. Townley. 1985. Pertussis booster vaccination and immediate hypersensitivity. Ann. Allergy 54:483-485. [PubMed] [Google Scholar]
- 270.Gil, A., I. Oyaguez, P. Carrasco, and A. Gonzalez. 2001. Hospital admissions for pertussis in Spain, 1995-1998. Vaccine 19:4791-4794. [DOI] [PubMed] [Google Scholar]
- 271.Gilberg, S., E. Njamkepo, I. P. Du Chatelet, H. Partouche, P. Gueirard, C. Ghasarossian, M. Schlumberger, and N. Guiso. 2002. Evidence of Bordetella pertussis infection in adults presenting with persistent cough in a French area with very high whole-cell vaccine coverage. J. Infect. Dis. 186:415-418. [DOI] [PubMed] [Google Scholar]
- 272.Gilchrist, M. J. R. 1991. Bordetella, p. 471-477. In A. Balows, W. J. Hausler, Jr., K. L. Herrmann, H. D. Isenberg, and H. J. Shadomy (ed.), Manual of clinical microbiology, 5th ed. American Society for Microbiology, Washington, D.C.
- 273.Gilchrist, M. J. R., and C. C. Linneman. 1988. Pertussis, p. 403-410. In A. Balows, W. J. Hausler, Jr., M. Ohashi, and A. Turano (ed.), Laboratory diagnosis of infectious diseases: principles and practice. Springer-Verlag, New York, N.Y.
- 274.Giles, C. J. 1992. Bordetellosis, p. 436-445. In D. J. Taylor (ed.), Diseases of swine, 7th ed, Wolfe, Ames, Iowa.
- 275.Gillespie, J. H., and J. F. Timoney. 1981. The genus Bordetella, p. 113-115. In J. H. Gillespie and J. F. Timoney (ed.), Hagan and Bruner's infectious diseases of domestic animals—with reference to etiology, pathogenicity, immunity, epidemiology, diagnosis, and biologic therapy, 7th ed. Cornell University Press, London, United Kingdom.
- 276.Gilligan, P. H., and M. C. Fisher. 1984. Importance of culture in laboratory diagnosis of Bordetella pertussis infections. J. Clin. Microbiol. 20:891-893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Glaser, P., D. Ladant, O. Sezer, F. Pichot, A. Ullmann, and A. Danchin. 1988. The calmodulin-sensitive adenylate cyclase of Bordetella pertussis: cloning and expression in Escherichia coli. Mol. Microbiol. 2:19-30. [PubMed] [Google Scholar]
- 278.Gold, M. S., S. Noonan, M. Osbourn, S. Precepa, and A. E. Kempe. 2003. Local reactions after the fourth dose of acellular pertussis vaccine in South Australia. Med. J. Aust. 179:191-194. [DOI] [PubMed] [Google Scholar]
- 279.Goldman, W. E. 1988. Tracheal cytotoxin of Bordetella pertussis, p. 237-246. In A. C. Wardlaw and R. Parton (ed.), Pathogenesis and immunity in pertussis. John Wiley & Sons, Inc., New York, N.Y.
- 280.Goldman, W. E., D. G. Klapper, and J. B. Baseman. 1982. Detection, isolation, and analysis of a released Bordetella pertussis product toxic to cultured tracheal cells. Infect. Immun. 36:782-794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Goldsmith, M. F. 1984. AMA offers recommendations for vaccine injury compensation. JAMA 252:2937-2939, 2942-2943. [DOI] [PubMed] [Google Scholar]
- 282.Gomez, L., M. Grazziutti, D. Sumoza, M. Beran, and K. Rolston. 1998. Bacterial pneumonia due to Bordetella bronchiseptica in a patient with acute leukemia. Clin. Infect. Dis. 26:1002-1003. [DOI] [PubMed] [Google Scholar]
- 283.Goodnow, R. A. 1980. Biology of Bordetella bronchiseptica. Microbiol. Rev. 44:722-738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Goodwin, M. S., and A. A. Weiss. 1990. Adenylate cyclase toxin is critical for colonization and pertussis toxin is critical for lethal infection by Bordetella pertussis in infant mice. Infect. Immun. 58:3445-3447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Gordon, J. E., and R. I. Hood. 1951. Whooping cough and its epidemiological anomalies. Am. J. Med. Sci. 222:333-361. [DOI] [PubMed] [Google Scholar]
- 286.Gordon, M., H. D. Davies, and R. Gold. 1994. Clinical and microbiologic features of children presenting with pertussis to a Canadian pediatric hospital during an eleven-year period. Pediatr. Infect. Dis. J. 13:617-622. [DOI] [PubMed] [Google Scholar]
- 287.Graeff-Wohlleben, H., H. Deppisch, and R. Gross. 1995. Global regulatory mechanisms affect virulence gene expression in Bordetella pertussis. Mol. Gen. Genet. 247:86-94. [DOI] [PubMed] [Google Scholar]
- 288.Granström, G., P. Askelof, and M. Granström. 1988. Specific immunoglobulin A to Bordetella pertussis antigens in mucosal secretion for rapid diagnosis of whooping cough. J. Clin. Microbiol. 26:869-874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Granström, M., G. Granström, A. Lindfors, and P. Askelof. 1982. Serologic diagnosis of whooping cough by an enzyme-linked immunosorbent assay using fimbrial hemagglutinin as antigen. J. Infect. Dis. 146:741-745. [DOI] [PubMed] [Google Scholar]
- 290.Grant, C. C., and J. D. Cherry. 2002. Keeping pace with the elusive Bordetella pertussis. J. Infect. 44:7-12. [DOI] [PubMed] [Google Scholar]
- 291.Graves, I. L. 1968. Bordetella bronchiseptica isolated from a fatal case of bronchopnuemonia in an African green monkey. Lab. Anim. Care 18:405-406. [PubMed] [Google Scholar]
- 292.Gray, M. C., G. M. Donato, F. R. Jones, T. Kim, and E. L. Hewlett. 2004. Newly secreted adenylate cyclase toxin is responsible for intoxication of target cells by Bordetella pertussis. Mol. Microbiol. 53:1709-1719. [DOI] [PubMed] [Google Scholar]
- 293.Greco, D., S. Salmaso, P. Mastrantonio, M. Giuliano, A. E. Tozzi, A. Anemona, M. Ciofi degli Atti, A. Giammanco, P. Panei, W. Blackwelder, D. Klein, S. Wassilak, and The Progetto Pertosse Working Group. 1996. A controlled trial of two acellular vaccines and one whole-cell vaccine against pertussis. N. Engl. J. Med. 334:341-348. [DOI] [PubMed] [Google Scholar]
- 294.Greig, J. R., S. S. Gunda, and J. T. C. Kwan. 2001. Bordetella holmesii bacteraemia in an individual on haemodialysis. Scand. J. Infect. Dis. 33:716-717. [DOI] [PubMed] [Google Scholar]
- 295.Griffin, M. R., W. A. Ray, J. R. Livengood, and W. Schaffner. 1988. Risk of sudden infant death syndrome after immunization with the diphtheria-tetanus-pertussis vaccine. N. Engl. J. Med. 319:618-623. [DOI] [PubMed] [Google Scholar]
- 296.Griffin, M. R., W. A. Ray, E. A. Mortimer, G. M. Fenichel, and W. Schaffner. 1990. Risk of seizures and encephalopathy after immunization with the diphtheria-tetanus-pertussis vaccine. JAMA 263:1641-1645. [PubMed] [Google Scholar]
- 297.Griffith, A. H. 1979. The case for immunization. Scott. Med. J. 24:42-46. [DOI] [PubMed] [Google Scholar]
- 298.Griffith, A. H. 1979. Discussion of part 5, p. 304. International Symposium on Pertussis. National Institutes of Health, Bethesda, Md.
- 299.Griffith, A. H. 1981. Medicine and the media—vaccination against whooping cough. J. Biol. Stand. 9:475-482. [DOI] [PubMed] [Google Scholar]
- 300.Griffith, A. H. 1978. Reactions after pertussis vaccine: a manufacturer's experiences and difficulties since 1964. Br. Med. J. 1:809-815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Grist, N. R. 1977. Vaccination against whooping-cough. Lancet i:358. [Google Scholar]
- 302.Gross, R., N. H. Carbonetti, R. Rossi, and R. Rappuoli. 1992. Functional analysis of the pertussis toxin promoter. Res. Microbiol. 143:671-681. [DOI] [PubMed] [Google Scholar]
- 303.Guedin, S., E. Willery, C. Locht, and F. Jacob-Dubuisson. 1998. Evidence that a globular conformation is not compatible with FhaC-mediated secretion of the Bordetella pertussis filamentous haemagglutinin. Mol. Microbiol. 29:763-774. [DOI] [PubMed] [Google Scholar]
- 304.Guedin, S., E. Willery, J. Tommassen, E. Fort, H. Drobecq, C. Locht, and F. Jacob-Dubuisson. 2000. Novel topological features of FhaC, the outer membrane transporter involved in the secretion of the Bordetella pertussis filamentous hemagglutinin. J. Biol. Chem. 275:30202-30210. [DOI] [PubMed] [Google Scholar]
- 305.Gueirard, P., and N. Guiso. 1993. Virulence of Bordetella bronchiseptica: role of adenylate cyclase-hemolysin. Infect. Immun. 61:4072-4078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Guiso, N., C. Boursaux-Eude, C. Weber, S. Z. Hausman, H. Sato, M. Iwaki, K. Kamachi, T. Konda, and D. L. Burns. 2001. Analysis of Bordetella pertussis isolates collected in Japan before and after introduction of acellular pertussis vaccines. Vaccine 19:3248-3252. [DOI] [PubMed] [Google Scholar]
- 307.Gulbenkian, A., L. Schobert, Nixon, and Tabachnick, II. 1968. Metabolic effects of pertussis sensitization in mice and rats. Endocrinology 83:885-892. [DOI] [PubMed] [Google Scholar]
- 308.Güris, D. 2000. Treatment and chemoprophylaxis. Guidelines for the control of pertussis outbreaks. Centers for Disease Control and Prevention, Atlanta, Ga.
- 309.Guris, D., P. M. Strebel, B. Bardenheier, M. Brennan, R. Tachdjian, E. Finch, M. Wharton, and J. R. Livengood. 1999. Changing epidemiology of pertussis in the United States: increasing reported incidence among adolescents and adults, 1990-1996. Clin. Infect. Dis. 28:1230-1237. [DOI] [PubMed] [Google Scholar]
- 310.Gustafsson, L., H. O. Hallander, P. Olin, E. Reizenstein, and J. Storsaeter. 1996. A controlled trial of a two-component acellular, a five-component acellular, and a whole-cell pertussis vaccine. N. Engl. J. Med. 334:349-355. [DOI] [PubMed] [Google Scholar]
- 311.Hackett, M., L. Guo, J. Shabanowitz, D. F. Hunt, and E. L. Hewlett. 1994. Internal lysine palmitoylation in adenylate cyclase toxin from Bordetella pertussis. Science 266:433-435. [DOI] [PubMed] [Google Scholar]
- 312.Haire, M., D. S. Dane, and G. Dick. 1977. Reactions to combined vaccines containing killed Bordetella pertussis. Med. Officer 117:55. [Google Scholar]
- 313.Hall, C. B., and R. G. Douglas, Jr. 1975. Clinically useful method for the isolation of respiratory syncytial virus. J. Infect. Dis. 131:1-5. [DOI] [PubMed] [Google Scholar]
- 314.Hallander, H. O., J. Gnarpe, H. Gnarpe, and P. Olin. 1999. Bordetella pertussis, Bordetella parapertussis, Mycoplasma pneumoniae, Chlamydia pneumoniae and persistent cough in children. Scand. J. Infect. Dis. 31:281-286. [DOI] [PubMed] [Google Scholar]
- 315.Hallander, H. O., E. Reizenstein, B. Renemar, G. Rasmuson, L. Mardin, and P. Olin. 1993. Comparison of nasopharyngeal aspirates with swabs for culture of Bordetella pertussis. J. Clin. Microbiol. 31:50-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Halperin, S. A., R. Bortolussi, J. M. Langley, B. Miller, and B. J. Eastwood. 1997. Seven days of erythromycin estolate is as effective as fourteen days for the treatment of Bordetella pertussis infections. Pediatrics 100:65-71. [DOI] [PubMed] [Google Scholar]
- 317.Halperin, S. A., R. Bortolussi, and A. J. Wort. 1989. Evaluation of culture, immunofluorescence, and serology for the diagnosis of pertussis. J. Clin. Microbiol. 27:752-757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Halpern, S. R., and D. Halpern. 1955. Reactions from DPT immunization and its relationship to allergic children. J. Pediatr. 47:60-67. [DOI] [PubMed] [Google Scholar]
- 319.Hannik, C. A., and H. Cohen. 1979. Changes in plasma insulin concentration and temperature of infants after pertussis vaccination, p. 297-299. In C. R. Manclark and J. C. Hills (ed.), International symposium on pertussis. U.S. Department of Health, Education, and Welfare publication NIH 79-1830. Government Printing Office, Washington, D.C.
- 320.Hansard. 1977. House of Commons Report, p. 1233, vol. 925. Her Majesty's Stationery Office, London, United Kingdom.
- 321.Hanski, E., and Z. Farfel. 1985. Bordetella pertussis invasive adenylate cyclase. Partial resolution and properties of its cellular penetration. J. Biol. Chem. 260:5526-5532. [PubMed] [Google Scholar]
- 322.Hardie, K. R., J. P. Issartel, E. Koronakis, C. Hughes, and V. Koronakis. 1991. In vitro activation of Escherichia coli prohaemolysin to the mature membrane-targeted toxin requires HlyC and a low molecular-weight cytosolic polypeptide. Mol. Microbiol. 5:1669-1679. [DOI] [PubMed] [Google Scholar]
- 323.Harker, P. 1977. Primary immunisation and febrile convulsions in Oxford 1972-5. Br. Med. J. 2:490-493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Harvill, E. T., P. A. Cotter, M. H. Yuk, and J. F. Miller. 1999. Probing the function of Bordetella bronchiseptica adenylate cyclase toxin by manipulating host immunity. Infect. Immun. 67:1493-1500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Harvill, E. T., A. Preston, P. A. Cotter, A. G. Allen, D. J. Maskell, and J. F. Miller. 2000. Multiple roles for Bordetella lipopolysaccharide molecules during respiratory tract infection. Infect. Immun. 68:6720-6728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Hasenclever, H. F., and E. J. Corley. 1968. Enhancement of acquired resistance in murine candidiasis by Bordetella pertussis vaccine. Sabouraudia 6:289-295. [PubMed] [Google Scholar]
- 327.Hausman, S. Z., J. D. Cherry, U. Heininger, C. H. Wirsing von König, and D. L. Burns. 1996. Analysis of proteins encoded by the ptx and ptl genes of Bordetella bronchiseptica and Bordetella parapertussis. Infect. Immun. 64:4020-4026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Hazenbos, W. L., C. A. Geuijen, B. M. van den Berg, F. R. Mooi, and R. van Furth. 1995. Bordetella pertussis fimbriae bind to human monocytes via the minor fimbrial subunit FimD. J. Infect. Dis. 171:924-929. [DOI] [PubMed] [Google Scholar]
- 329.Hazenbos, W. L., B. M. van den Berg, C. W. Geuijen, F. R. Mooi, and R. van Furth. 1995. Binding of FimD on Bordetella pertussis to very late antigen-5 on monocytes activates complement receptor type 3 via protein tyrosine kinases. J. Immunol. 155:3972-3978. [PubMed] [Google Scholar]
- 330.He, Q., M. K. Viljanen, H. Arvilommi, B. Aittanen, and J. Mertsola. 1998. Whooping cough caused by Bordetella pertussis and Bordetella parapertussis in an immunized population. JAMA 280:635-637. [DOI] [PubMed] [Google Scholar]
- 331.Heijbel, H., F. Rasmussen, and P. Olin. 1997. Safety evaluation of one whole-cell and three acellular pertussis vaccines in Stockholm trial II. Dev. Biol. Stand. 89:99-100. [PubMed] [Google Scholar]
- 332.Heininger, U., J. D. Cherry, P. D. Christenson, T. Eckhardt, U. Goering, P. Jakob, W. Kasper, D. Schweingel, S. Laussucq, J. G. Hackell, J. R. Mezzatesta, J. V. Scott, and K. Stehr. 1994. Comparative study of Lederle Takeda acellular and Lederle whole-cell pertussis-component diphtheria-tetanus-pertussis vaccines in infants in Germany. Vaccine 12:81-86. [DOI] [PubMed] [Google Scholar]
- 333.Heininger, U., J. D. Cherry, T. Eckhardt, C. Lorenz, P. Christenson, and K. Stehr. 1993. Clinical and laboratory diagnosis of pertussis in the regions of a large vaccine efficacy trial in Germany. Pediatr. Infect. Dis. J. 12:504-509. [DOI] [PubMed] [Google Scholar]
- 334.Heininger, U., J. D. Cherry, K. Stehr, S. Schmitt-Grohé, M. Überall, S. Laussucq, T. Eckhardt, M. Meyer, J. Gornbein, and the Pertussis Vaccine Study Group. 1998. Comparative Efficacy of the Lederle/Takeda acellular pertussis component DTP (DTaP) vaccine and Lederle whole-cell component DTP vaccine in German children after household exposure. Pediatrics 102:546-553. [DOI] [PubMed] [Google Scholar]
- 335.Heininger, U., W. J. Kleemann, J. D. Cherry, and S. S. Group. 2004. A controlled study of the relationship between Bordetella pertussis infection and sudden unexpected deaths in German infants. Pediatrics 114:e9-e15. [DOI] [PubMed] [Google Scholar]
- 336.Heininger, U., K. Klich, K. Stehr, and J. D. Cherry. 1997. Clinical findings in Bordetella pertussis infections: results of a prospective multicenter surveillance study. Pediatrics 100:e10. [DOI] [PubMed] [Google Scholar]
- 337.Heininger, U., G. Schmidt-Schlapfer, J. D. Cherry, and K. Stehr. 2000. Clinical validation of a polymerase chain reaction assay for the diagnosis of pertussis by comparison with serology, culture, and symptoms during a large pertussis vaccine efficacy trial. Pediatrics 105:e31. [DOI] [PubMed] [Google Scholar]
- 338.Heininger, U., K. Stehr, and J. D. Cherry. 1992. Serious pertussis overlooked in infants. Eur. J. Pediatr. 151:342-343. [DOI] [PubMed] [Google Scholar]
- 339.Heininger, U., K. Stehr, G. Schmidt-Schlapfer, R. Penning, R. Vock, W. Kleemann, and J. D. Cherry. 1996. Bordetella pertussis infections and sudden unexpected deaths in children. Eur. J. Pediatr. 155:551-553. [DOI] [PubMed] [Google Scholar]
- 340.Heininger, U., K. Stehr, S. Schmitt-Grohé, C. Lorenz, R. Rost, P. D. Christenson, M. Überall, and J. D. Cherry. 1994. Clinical characteristics of illness caused by Bordetella parapertussis compared with illness caused by Bordetella pertussis. Pediatr. Infect. Dis. J. 13:306-309. [DOI] [PubMed] [Google Scholar]
- 341.Heiss, L. N., T. A. Flak, J. R. Lancaster, Jr., M. L. McDaniel, and W. E. Goldman. 1993. Nitric oxide mediates Bordetella pertussis tracheal cytotoxin damage to the respiratory epithelium. Infect. Agents. Dis. 2:173-177. [PubMed] [Google Scholar]
- 342.Heiss, L. N., S. A. Moser, E. R. Unanue, and W. E. Goldman. 1993. Interleukin-1 is linked to the respiratory epithelial cytopathology of pertussis. Infect. Immun. 61:3123-3128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Hellwig, S. M., M. E. Rodriguez, G. A. Berbers, J. G. van de Winkel, and F. R. Mooi. 2003. Crucial role of antibodies to pertactin in Bordetella pertussis immunity. J. Infect. Dis. 188:738-742. [DOI] [PubMed] [Google Scholar]
- 344.Henderson, I. R., and J. P. Nataro. 2001. Virulence functions of autotransporter proteins. Infect. Immun. 69:1231-1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Hennessen, W., and U. Quast. 1979. Adverse reactions after pertussis vaccination. Dev. Biol. Stand. 43:95-100. [PubMed] [Google Scholar]
- 346.Hewlett, E. L., and J. D. Cherry. 1990. New and improved vaccines against pertussis, p. 231-250. In G. C. Woodrow and M. M. Levine (ed.), New generation vaccines. Marcel Dekker, Inc., New York, N.Y.
- 347.Hewlett, E. L., and J. D. Cherry. 1997. New and improved vaccines against pertussis, p. 387-416. In M. M. Levine, G. C. Woodrow, J. B. Kaper, and G. S. Cobon (ed.), New generation vaccines, 2nd ed. Marcel Dekker, Inc., New York, N.Y.
- 348.Hewlett, E. L., and V. M. Gordon. 1988. Adenylate cyclase toxin of Bordetella pertussis, p. 193-209. In A. C. Wardlaw and R. Parton (ed.), Pathogenesis and immunity in pertussis. John Wiley & Sons, Inc., New York, N.Y.
- 349.Hewlett, E. L., V. M. Gordon, J. D. McCaffery, W. M. Sutherland, and M. C. Gray. 1989. Adenylate cyclase toxin from Bordetella-pertussis: identification and purification of the holotoxin molecule. J. Biol. Chem. 264:19379-19384. [PubMed] [Google Scholar]
- 350.Hewlett, E. L., and N. J. Maloney. 1994. Adenylyl cyclase toxin from Bordetella pertussis, p. 948-950. In B. Iglewski, J. Moss, A. T. Tu, and M. Vaughan (ed.), Handbook of natural toxins, vol. 8. Marcel Dekker, Inc., New York, N.Y. [Google Scholar]
- 351.Hinman, A. R. 1986. DTP vaccine litigation. Am. J. Dis. Child. 140:528-530. [DOI] [PubMed] [Google Scholar]
- 352.Hinman, A. R., and J. P. Koplan. 1984. Pertussis and pertussis vaccine. Reanalysis of benefits, risks, and costs. JAMA 251:3109-3113. [DOI] [PubMed] [Google Scholar]
- 353.Hirtz, D. G., K. B. Nelson, and J. H. Ellenberg. 1983. Seizures following childhood immunizations. J. Pediatr. 102:14-18. [DOI] [PubMed] [Google Scholar]
- 354.Hodder, S. L., J. D. Cherry, E. A. Mortimer, Jr., A. B. Ford, J. Gornbein, and K. Papp. 2000. Antibody responses to Bordetella pertussis antigens and clinical correlations in elderly community residents. Clin. Infect. Dis. 31:7-14. [DOI] [PubMed] [Google Scholar]
- 355.Hoffman, H. J., J. C. Hunter, K. Damus, J. Pakter, D. R. Peterson, G. van Belle, and E. G. Hasselmeyer. 1987. Diphtheria-tetanus-pertussis immunization and sudden infant death: results of the National Institute of Child Health and Human Development Cooperative Epidemiological Study of Sudden Infant Death Syndrome risk factors. Pediatrics 79:598-611. [PubMed] [Google Scholar]
- 356.Holmes, W. H. 1940. Whooping-cough, or pertussis, p. 394-414. In W. H. Holmes (ed.), Bacillary and rickettsial infections: acute and chronic. Macmillan, New York, N.Y.
- 357.Honein, M. A., L. J. Paulozzi, I. M. Himelright, B. Lee, J. D. Cragan, L. Patterson, A. Correa, S. Hall, and J. D. Erickson. 1999. Infantile hypertrophic pyloric stenosis after pertussis prophylaxis with erythromycin: a case review and cohort study. Lancet 354:2101-2105. [DOI] [PubMed] [Google Scholar]
- 358.Hooker, J. M. 1981. A laboratory study of the toxicity of some diphtheria-tetanus-pertussis vaccines. J. Biol. Stand. 9:493-506. [DOI] [PubMed] [Google Scholar]
- 359.Hoppe, J. E. 1988. Methods for isolation of Bordetella pertussis from patients with whooping cough. Eur. J. Clin. Microbiol. Infect. Dis. 7:616-620. [DOI] [PubMed] [Google Scholar]
- 360.Hoppe, J. E. 2000. Neonatal pertussis. Pediatr Infect Dis J 19:244-7. [DOI] [PubMed] [Google Scholar]
- 361.Hoppe, J. E. 1998. State of art in antibacterial susceptibility of Bordetella pertussis and antibiotic treatment of pertussis. Infection 26:242-246. [DOI] [PubMed] [Google Scholar]
- 362.Hoppe, J. E. 1996. Update of epidemiology, diagnosis, and treatment of pertussis. Eur. J. Clin. Microbiol. Infect. Dis. 15:189-193. [DOI] [PubMed] [Google Scholar]
- 363.Hoppe, J. E. 1999. Update on respiratory infection caused by Bordetella parapertussis. Pediatr. Infect. Dis. J. 18:375-381. [DOI] [PubMed] [Google Scholar]
- 364.Hoppe, J. E., and A. Eichhorn. 1989. Activity of new macrolides against Bordetella pertussis and Bordetella parapertussis. Eur. J. Clin. Microbiol. Infect. Dis. 8:653-654. [DOI] [PubMed] [Google Scholar]
- 365.Hoppe, J. E., U. Halm, H. J. Hagedorn, and A. Kraminer-Hagedorn. 1989. Comparison of erythromycin ethylsuccinate and co-trimoxazole for treatment of pertussis. Infection 17:227-231. [DOI] [PubMed] [Google Scholar]
- 366.Hoppe, J. E., and A. Haug. 1988. Antimicrobial susceptibility of Bordetella pertussis, part I. Infection 16:126-130. [DOI] [PubMed] [Google Scholar]
- 367.Hoppe, J. E., and J. Schwaderer. 1989. Direct plating versus use of transport medium for detection of Bordetella species from nasopharyngeal swabs. Eur. J. Clin. Microbiol. Infect. Dis. 8:264-265. [DOI] [PubMed] [Google Scholar]
- 368.Hopper, J. M. H. 1961. Illness after whooping cough vaccination. Med. Officer 106:241. [Google Scholar]
- 369.Horiguchi, Y., T. Nakai, and K. Kume. 1991. Effects of Bordetella bronchiseptica dermonecrotic toxin on the structure and function of osteoblastic clone MC3T3-el cells. Infect. Immun. 59:1112-1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 370.Horiguchi, Y., T. Nakai, and K. Kume. 1989. Purification and characterization of Bordetella bronchiseptica dermonecrotic toxin. Microb. Pathog. 6:361-368. [DOI] [PubMed] [Google Scholar]
- 371.Horiguchi, Y., T. Senda, N. Sugimoto, J. Katahira, and M. Matsuda. 1995. Bordetella bronchiseptica dermonecrotizing toxin stimulates assembly of actin stress fibers and focal adhesions by modifying the small GTP-binding protein rho. J. Cell Sci. 108:3243-3251. [DOI] [PubMed] [Google Scholar]
- 372.Horiguchi, Y., N. Sugimoto, and M. Matsuda. 1993. Stimulation of DNA synthesis in osteoblast-like MC3T3-E1 cells by Bordetella bronchiseptica dermonecrotic toxin. Infect. Immun. 61:3611-3615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Houard, S., C. Hackel, A. Herzog, and A. Bollen. 1989. Specific identification of Bordetella pertussis by the polymerase chain reaction. Res. Microbiol. 140:477-487. [DOI] [PubMed] [Google Scholar]
- 374.Hueck, C. J. 1998. Type III protein secretion systems in bacterial pathogens of animals and plants. Microbiol. Mol. Biol. Rev. 62:379-433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 375.Hughes, C., J. P. Issartel, K. Hardie, P. Stanley, E. Koronakis, and V. Koronakis. 1992. Activation of Escherichia coli prohemolysin to the membrane-targetted toxin by HlyC-directed ACP-dependent fatty acylation. FEMS Microbiol. Immunol. 5:37-43. [DOI] [PubMed] [Google Scholar]
- 376.Hull, D. 1981. Interpretation of the contraindications to whooping cough vaccination. Br. Med. J. (Clin. Res. Ed.) 283:1231-1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 377.Iida, T., and T. Okonogi. 1971. Lienotoxicity of Bordetella pertussis in mice. J. Med. Microbiol. 4:51-61. [DOI] [PubMed] [Google Scholar]
- 378.Ilic, D., Y. Furuta, S. Kanazawa, N. Takeda, K. Sobue, N. Nakatsuji, S. Nomura, J. Fujimoto, M. Okada, and T. Yamamoto. 1995. Reduced cell motility and enhanced focal adhesion contact formation in cells from FAK-deficient mice. Nature 377:539-544. [DOI] [PubMed] [Google Scholar]
- 379.Illingworth, R. 1982. Toxicity of pertussis vaccine. Br. Med. J. (Clin. Res. Ed.) 285:210-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 380.Reference deleted.
- 381.Reference deleted.
- 382.Ipp, M. M., R. Gold, S. Greenberg, M. Goldbach, B. B. Kupfert, D. D. Lloyd, D. C. Maresky, N. Saunders, and S. A. Wise. 1987. Acetaminophen prophylaxis of adverse reactions following vaccination of infants with diphtheria-pertussis-tetanus toxoids-polio vaccine. Pediatr. Infect. Dis. J. 6:721-725. [DOI] [PubMed] [Google Scholar]
- 383.Irie, Y., S. Mattoo, and M. H. Yuk. 2004. The Bvg virulence control system regulates biofilm formation in Bordetella bronchiseptica. J. Bacteriol. 186:5692-5698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 384.Ishibashi, Y., S. Claus, and D. A. Relman. 1994. Bordetella pertussis filamentous hemagglutinin interacts with a leukocyte signal transduction complex and stimulates bacterial adherence to monocyte CR3 (CD11b/CD18). J. Exp. Med. 180:1225-1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 385.Ishibashi, Y., and A. Nishikawa. 2002. Bordetella pertussis infection of human respiratory epithelial cells up-regulates intercellular adhesion molecule-1 expression: role of filamentous hemagglutinin and pertussis toxin. Microb. Pathog. 33:115-125. [DOI] [PubMed] [Google Scholar]
- 386.Ishibashi, Y., and A. Nishikawa. 2003. Role of nuclear factor-kappa B in the regulation of intercellular adhesion molecule 1 after infection of human bronchial epithelial cells by Bordetella pertussis. Microb. Pathog. 35:169-177. [DOI] [PubMed] [Google Scholar]
- 387.Ishibashi, Y., D. A. Relman, and A. Nishikawa. 2001. Invasion of human respiratory epithelial cells by Bordetella pertussis: possible role for a filamentous hemagglutinin Arg-Gly-Asp sequence and alpha5beta1 integrin. Microb. Pathog. 30:279-288. [DOI] [PubMed] [Google Scholar]
- 388.Issartel, J. P., V. Koronakis, and C. Hughes. 1991. Activation of Escherichia coli prohaemolysin to the mature toxin by acyl carrier protein-dependent fatty acylation. Nature 351:759-761. [DOI] [PubMed] [Google Scholar]
- 389.Iwata, S., T. Aoyama, A. Goto, H. Iwai, Y. Sato, H. Akita, Y. Murase, T. Oikawa, T. Iwata, S. Kusano, et al. 1991. Mixed outbreak of Bordetella pertussis and Bordetella parapertussis in an apartment house. Dev. Biol. Stand. 73:333-341. [PubMed] [Google Scholar]
- 390.Jackson, L. A., J. D. Cherry, S. P. Wang, and J. T. Grayston. 2000. Frequency of serological evidence of Bordetella infections and mixed infections with other respiratory pathogens in university students with cough illnesses. Clin. Infect. Dis. 31:3-6. [DOI] [PubMed] [Google Scholar]
- 391.Jacob-Dubuisson, F., C. Buisine, N. Mielcarek, E. Clement, F. D. Menozzi, and C. Locht. 1996. Amino-terminal maturation of the Bordetella pertussis filamentous haemagglutinin. Mol. Microbiol. 19:65-78. [DOI] [PubMed] [Google Scholar]
- 392.Jacob-Dubuisson, F., C. El-Hamel, N. Saint, S. Guedin, E. Willery, G. Molle, and C. Locht. 1999. Channel formation by FhaC, the outer membrane protein involved in the secretion of the Bordetella pertussis filamentous hemagglutinin. J. Biol. Chem. 274:37731-37735. [DOI] [PubMed] [Google Scholar]
- 393.Jacob-Dubuisson, F., B. Kehoe, E. Willery, N. Reveneau, C. Locht, and D. A. Relman. 2000. Molecular characterization of Bordetella bronchiseptica filamentous haemagglutinin and its secretion machinery. Microbiology 146:1211-1221. [DOI] [PubMed] [Google Scholar]
- 394.Jacobs, C., B. Joris, M. Jamin, K. Klarsov, J. Van Beeumen, D. Mengin-Lecreulx, J. van Heijenoort, J. T. Park, S. Normark, and J. M. Frere. 1995. AmpD, essential for both beta-lactamase regulation and cell wall recycling, is a novel cytosolic N-acetylmuramyl-l-alanine amidase. Mol. Microbiol. 15:553-559. [DOI] [PubMed] [Google Scholar]
- 395.Janeway, C. A., Jr., P. Travers, M. Walport, and J. D. Capra. 1999. Immunological memory, p. 402-412. In P. Austin and E. Lawrence (ed.), Immunobiology: the immune system in health and disease, 4th ed. Elsevier, New York, N.Y.
- 396.Janicot, M., F. Fouque, and B. Desbuquois. 1991. Activation of rat liver adenylate cyclase by cholera toxin requires toxin internalization and processing in endosomes. J. Biol. Chem. 266:12858-12865. [PubMed] [Google Scholar]
- 397.Jansen, D. L., G. C. Gray, S. D. Putnam, F. Lynn, and B. D. Meade. 1997. Evaluation of pertussis in U.S. Marine Corps trainees: Clin. Infect. Dis. 25:1099-1107. [DOI] [PubMed] [Google Scholar]
- 398.Joint Committee on Vaccination and Immunisation. 1977. Whooping cough vaccination: review of the evidence on whooping cough vaccination. Department of Health and Social Security, London, United Kingdom.
- 399.Joint Committee on Vaccination and Immunisation. 1975. Whooping cough vaccine. Br. Med. J. 3:687-688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 400.Jones, M. 1950. Subacute bacterial endocarditis of nonstreptococcic etiology, a review of the literature of the thirteen-year period 1936-1948 inclusive. Am. Heart J. 40:106-116. [DOI] [PubMed] [Google Scholar]
- 401.Kania, S. A., S. Rajeev, E. H. Burns, Jr., T. F. Odom, S. M. Holloway, and D. A. Bemis. 2000. Characterization of fimN, a new Bordetella bronchiseptica major fimbrial subunit gene. Gene 256:149-155. [DOI] [PubMed] [Google Scholar]
- 402.Kaslow, H. R., and D. L. Burns. 1992. Pertussis toxin and target eukaryotic cells: binding, entry, and activation. FASEB J. 6:2684-2690. [DOI] [PubMed] [Google Scholar]
- 403.Katada, T., M. Tamura, and M. Ui. 1983. The A protomer of islet-activating protein, pertussis toxin, as an active peptide catalyzing ADP-ribosylation of a membrane protein. Arch. Biochem. Biophys. 224:290-298. [DOI] [PubMed] [Google Scholar]
- 404.Kattar, M. M., J. F. Chavez, A. P. Limaye, S. L. Rassoulian-Barrett, S. L. Yarfitz, L. C. Carlson, Y. Houze, S. Swanzy, B. L. Wood, and B. T. Cookson. 2000. Application of 16S rRNA gene sequencing to identify Bordetella hinzii as the causative agent of fatal septicemia. J. Clin. Microbiol. 38:789-794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 405.Katzenstein, D. A., L. Ciofalo, and M. C. Jordan. 1984. Bordetella bronchiseptica bacteremia. West. J. Med. 140:96-98. [PMC free article] [PubMed] [Google Scholar]
- 406.Katzko, G., M. Hofmeister, and D. Church. 1996. Extended incubation of cultureplate improves recovery of Bordetella spp. J. Clin. Microbiol. 34:1536-1564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 407.Keegan, J. J. 1920. The pathology of epidemic pneumonia in mice and guinea pigs. Arch. Intern. Med. 26:570-593. [Google Scholar]
- 408.Keens, T. G., S. L. Ward, E. P. Gates, D. I. Andree, and L. D. Hart. 1985. Ventilatory pattern following diphtheria-tetanus-pertussis immunization in infants at risk for sudden infant death syndrome. Am. J. Dis. Child. 139:991-994. [DOI] [PubMed] [Google Scholar]
- 409.Keil, D. J., and B. Fenwick. 1998. Role of Bordetella bronchiseptica in infectious tracheobronchitis in dogs. J. Am. Vet. Med. Assoc. 212:200-207. [PubMed] [Google Scholar]
- 410.Kendrick, P. L. 1975. Can whooping cough be eradicated? J. Infect. Dis. 132:707-712. [DOI] [PubMed] [Google Scholar]
- 411.Kendrick, P. L. 1943. A field study of alum-precipitated combined pertussis vaccine and diphtheria toxoid for active immunization. Am. J. Hyg. 38:193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 412.Kendrick, P. L. 1940. Secondary familial attack rates from pertussis in vaccinated and unvaccinated children. Am. J. Hyg. 32:89-91. [Google Scholar]
- 413.Kendrick, P. L. 1943. Use of alum-treated pertussis vaccine, and of alum-precipitated combined pertussis vaccine and diphtheria toxoid for active immunization. Am. J. Hyg. 32:615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 414.Kendrick, P. L., and G. Eldering. 1936. Progress report on pertussis immunization. Am. J. Public Health 28:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 415.Kendrick, P. L., and G. Eldering. 1939. A study in active immunization against pertussis. Am. J. Hyg. 29:133. [Google Scholar]
- 416.Kendrick, P. L., G. Eldering, M. K. m. Dixon, et al. 1947. Mouse protection tests in the study of pertussis vaccine. Am. J. Public Health 37:803-810. [PubMed] [Google Scholar]
- 417.Kendrick, P. L., G. Eldering, and M. Thompson. 1946. Reinforcing or “booster” injection of pertussis vaccine in previously immunized children of kindergarten age. Am. J. Dis. Child. 72:382. [DOI] [PubMed] [Google Scholar]
- 418.Kerr, J. R., and R. C. Matthews. 2000. Bordetella pertussis infection: pathogenesis, diagnosis, management, and the role of protective immunity. Eur. J. Clin. Microbiol. Infect. Dis. 19:77-88. [DOI] [PubMed] [Google Scholar]
- 419.Khelef, N., A. Zychlinsky, and N. Guiso. 1993. Bordetella pertussis induces apoptosis in macrophages: role of adenylate cyclase-hemolysin. Infect. Immun. 61:4064-4071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 420.Kimbrough, T. G., and S. I. Miller. 2002. Assembly of the type III secretion needle complex of Salmonella typhimurium. Microbes Infect. 4:75-82. [DOI] [PubMed] [Google Scholar]
- 421.Kimura, A., K. T. Mountzouros, D. A. Relman, S. Falkow, and J. L. Cowell. 1990. Bordetella pertussis filamentous hemagglutinin: evaluation as a protective antigen and colonization factor in a mouse respiratory infection model. Infect. Immun. 58:7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 422.Kimura, M., and H. Kuno-Sakai. 1988. Pertussis vaccines in Japan. Acta Paediatr. Jpn. 30:143-153. [DOI] [PubMed] [Google Scholar]
- 423.Kind, L. S. 1959. Sensitivity of pertussis inoculated mice to endotoxin. J. Immunol. 82:32-37. [PubMed] [Google Scholar]
- 424.Kirimanjeswara, G. S., P. B. Mann, and E. T. Harvill. 2003. Role of antibodies in immunity to Bordetella infections. Infect. Immun. 71:1719-1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 425.Knapp, S., and J. J. Mekalanos. 1988. Two trans-acting regulatory genes (vir and mod) control antigenic modulation in Bordetella pertussis. J. Bacteriol. 170:5059-5066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 426.Kohn, D. F., and D. E. Haines. 1977. Bordetella bronchiseptica infection in the lesser bushbaby (Galago senegalensis). Lab. Anim. Sci. 27:279-280. [PubMed] [Google Scholar]
- 427.Kontor, E. J., R. J. Wegrzyn, and R. A. Goodnow. 1981. Canine infectious tracheobronchitis: effects of an intranasal live canine parainfluenza-Bordetella bronchiseptica vaccine on viral shedding and clinical tracheobronchitis (kennel cough). Am. J. Vet. Res. 42:1694-1698. [PubMed] [Google Scholar]
- 428.Koplan, J. P., S. C. Schoenbaum, M. C. Weinstein, and D. W. Fraser. 1979. Pertussis vaccine—an analysis of benefits, risks and costs. N. Engl. J. Med. 301:906-911. [DOI] [PubMed] [Google Scholar]
- 429.Korgenski, E. K., and J. A. Daly. 1997. Surveillance and detection of erythromycin resistance in Bordetella pertussis isolates recovered from a pediatric population in the Intermountain West region of the United States. J. Clin. Microbiol. 35:2989-2991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 430.Kotob, S. I., S. Z. Hausman, and D. L. Burns. 1995. Localization of the promoter for the ptl genes of Bordetella pertussis which encode proteins essential for secretion of pertussis toxin. Infect. Immun. 63:3227-3230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 431.Krepler, P., and H. Flamm. 1958. Bordetella bronchiseptica as causative agent of human diseases. Wien. Klin. Wochenschr. 70:641-644. (In German.) [PubMed] [Google Scholar]
- 432.Kristensen, K. H., and H. Lautrop. 1962. A family epidemic caused by the whooping-cough bacterium Bordetella bronchiseptica. Ugeskr. Laeger. 124:303-308. (In Danish.) (In Danish.) [PubMed] [Google Scholar]
- 433.Kubori, T., Y. Matsushima, D. Nakamura, J. Uralil, M. Lara-Tejero, A. Sukhan, J. E. Galan, and S. I. Aizawa. 1998. Supramolecular structure of the Salmonella typhimurium type III protein secretion system. Science 280:602-605. [DOI] [PubMed] [Google Scholar]
- 434.Kuldau, G. A., G. De Vos, J. Owen, G. McCaffrey, and P. Zambryski. 1990. The virB operon of Agrobacterium tumefaciens pTiC58 encodes 11 open reading frames. Mol. Gen. Genet. 221:256-266. [DOI] [PubMed] [Google Scholar]
- 435.Kulenkampff, M., J. S. Schwartzman, and J. Wilson. 1974. Neurological complications of pertussis inoculation. Arch. Dis. Child. 49:46-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 436.Lacerda, H. M., G. D. Pullinger, A. J. Lax, and E. Rozengurt. 1997. Cytotoxic necrotizing factor 1 from Escherichia coli and dermonecrotic toxin from Bordetella bronchiseptica induce p21(rho)-dependent tyrosine phosphorylation of focal adhesion kinase and paxillin in Swiss 3T3 cells. J. Biol. Chem. 272:9587-9596. [DOI] [PubMed] [Google Scholar]
- 437.Lacey, B. W. 1960. Antigenic modulation of Bordetella pertussis. J. Hyg. 58:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 438.Lad, P. M., C. V. Olson, and P. A. Smiley. 1985. Association of the N-formyl-Met-Leu-Phe receptor in human neutrophils with a GTP-binding protein sensitive to pertussis toxin. Proc. Natl. Acad. Sci. USA 82:869-873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 439.Lambert, H. J. 1965. Epidemiology of a small pertussis outbreak in Kent County, Michigan. Public Health Rep. 80:365-369. [PMC free article] [PubMed] [Google Scholar]
- 440.Landy, M. 1956. Increase in resistance following administration of bacterial lipopolysaccharides. N. Y. Acad. Sci. 66:292-303. [Google Scholar]
- 441.Langley, J. M., S. A. Halperin, F. D. Boucher, and B. Smith. 2004. Azithromycin is as effective as and better tolerated than erythromycin estolate for the treatment of pertussis. Pediatrics 114:e96-e101. [DOI] [PubMed] [Google Scholar]
- 442.Lapin, J. H. 1943. Whooping cough. Charles C Thomas, Springfield, Ill.
- 443.Lasfargues, A., M. Caroff, and R. Chaby. 1993. Structural features involved in the mitogenic activity of Bordetella pertussis lipopolysaccharides for spleen cells of C3H/HeJ mice. FEMS Immunol. Med. Microbiol. 7:119-129. [DOI] [PubMed] [Google Scholar]
- 444.Lautrop, H. 1971. Epidemics of parapertussis. 20 years' observations in Denmark. Lancet i:1195-1198. [DOI] [PubMed] [Google Scholar]
- 445.Lautrop, H. 1958. Observations on parapertussis in Denmark, 1950-1957. Acta Pathol. Microbiol. Scand. 43:255-266. [DOI] [PubMed] [Google Scholar]
- 446.Le, T., J. D. Cherry, S. J. Chang, M. D. Knoll, M. L. Lee, S. Barenkamp, D. Bernstein, R. Edelman, K. M. Edwards, D. Greenberg, W. Keitel, J. Treanor, and J. I. Ward. 2004. Immune responses and antibody decay following immunization of adolescents and adults with an acellular pertussis vaccine: APERT study. J. Infect. Dis. 190:535-544. [DOI] [PubMed] [Google Scholar]
- 447.Lebbar, S., J. M. Cavaillon, M. Caroff, A. Ledur, H. Brade, R. Sarfati, and N. Haeffner-Cavaillon. 1986. Molecular requirement for interleukin 1 induction by lipopolysaccharide-stimulated human monocytes: involvement of the heptosyl-2-keto-3-deoxyoctulosonate region. Eur. J. Immunol. 16:87-91. [DOI] [PubMed] [Google Scholar]
- 448.Lebel, M. H., and S. Mehra. 2001. Efficacy and safety of clarithromycin versus erythromycin for the treatment of pertussis: a prospective, randomized, single blind trial. Pediatr. Infect. Dis. J. 20:1149-1154. [DOI] [PubMed] [Google Scholar]
- 449.Lee, B. 2000. Progressive respiratory distress in an infant treated for presumed pertussis. Pediatr. Infect. Dis. J. 19:475, 492-493. [DOI] [PubMed] [Google Scholar]
- 450.Lee, C. A. 1997. Type III secretion systems: machines to deliver bacterial proteins into eukaryotic cells? Trends Microbiol. 5:148-156. [DOI] [PubMed] [Google Scholar]
- 451.Leef, M., K. L. Elkins, J. Barbic, and R. D. Shahin. 2000. Protective immunity to Bordetella pertussis requires both B cells and CD4(+) T cells for key functions other than specific antibody production. J. Exp. Med. 191:1841-1852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 452.Lehrer, S. B., J. H. Vaughan, and E. M. Tan. 1975. Adjuvant activity of the histamine-sensitizing factor of Bordetella pertussis in different strains of mice. Int. Arch. Allergy Appl. Immunol. 49:796-813. [DOI] [PubMed] [Google Scholar]
- 453.Lehrer, S. B., J. H. Vaughn, and E. M. Tan. 1976. Enhancement of reaginic and hemagglutinating antibody production by an extract of Bordetella pertussis containing histamine sensitizing factor. J. Immunol. 116:178-183. [PubMed] [Google Scholar]
- 454.Leslie, P. H., and A. D. Gardner. 1931. The phases of Haemophilus pertussis. J. Hyg. 31:423-434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 455.Letcher, J., E. Weisenberg, and A. Jonas. 1993. Bordetella bronchiseptica pneumonia in a koala. J. Am. Vet. Med. Assoc. 202:985-987. [PubMed] [Google Scholar]
- 456.Levine, S., E. J. Wenk, H. B. Devlin, R. E. Pieroni, and L. Levine. 1966. Hyperacute allergic encephalomyelitis: adjuvant effect of pertussis vaccines and extracts. J. Immunol. 97:363-368. [PubMed] [Google Scholar]
- 457.Lewis, K. 2001. Riddle of biofilm resistance. Antimicrob. Agents Chemother. 45:999-1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 458.Lewis, K., S. C. Jordan, J. D. Cherry, R. S. Sakai, and C. T. Le. 1986. Petechiae and urticaria after DTP vaccination: detection of circulating immune complexes containing vaccine-specific antigens. J. Pediatr. 109:1009-1012. [DOI] [PubMed] [Google Scholar]
- 459.Lewis, K., M. A. Saubolle, F. C. Tenover, M. F. Rudinsky, S. D. Barbour, and J. D. Cherry. 1995. Pertussis caused by an erythromycin-resistant strain of Bordetella pertussis. Pediatr. Infect. Dis. J. 14:388-391. [DOI] [PubMed] [Google Scholar]
- 460.Li, J., N. F. Fairweather, P. Novotny, G. Dougan, and I. G. Charles. 1992. Cloning, nucleotide sequence and heterologous expression of the protective outer-membrane protein P.68 pertactin from Bordetella bronchiseptica. J. Gen. Microbiol. 138:1697-1705. [DOI] [PubMed] [Google Scholar]
- 461.Li, L. J., G. Dougan, P. Novotny, and I. G. Charles. 1991. P.70 pertactin, an outer-membrane protein from Bordetella parapertussis: cloning, nucleotide sequence and surface expression in Escherichia coli. Mol. Microbiol. 5:409-417. [DOI] [PubMed] [Google Scholar]
- 462.Li, Z. M., J. L. Cowell, M. J. Brennan, D. L. Burns, and C. R. Manclark. 1988. Agglutinating monoclonal antibodies that specifically recognize lipooligosaccharide A of Bordetella pertussis. Infect. Immun. 56:699-702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 463.Lichtinghagen, R., R. Diedrich-Glaubitz, and B. von Hörsten. 1994. Identification of Bordetella pertussis in nasopharyngeal swabs using the polymerase chain reaction: evaluation of detection methods. Eur. J. Clin. Chem. Clin. Biochem. 32:161-167. [DOI] [PubMed] [Google Scholar]
- 464.Liese, J. G., C. K. Meschievitz, E. Harzer, J. Froeschle, P. Hosbach, J. E. Hoppe, F. Porter, S. Stojanov, K. Niinivaara, A. M. Walker, and B. H. Belohradsky. 1997. Efficacy of a two-component acellular pertussis vaccine in infants. Pediatr. Infect. Dis. J. 16:1038-1044. [DOI] [PubMed] [Google Scholar]
- 465.Liese, J. G., C. Renner, S. Stojanov, and B. H. Belohradsky. 2003. Clinical and epidemiological picture of B. pertussis and B. parapertussis infections after introduction of acellular pertussis vaccines. Arch. Dis. Child. 88:684-687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 466.Lind-Brandberg, L., C. Welinder-Olsson, T. Lagergård, J. Taranger, B. Trollfors, and G. Zackrisson. 1998. Evaluation of PCR for diagnosis of Bordetella pertussis and Bordetella parapertussis infections. J. Clin. Microbiol. 36:679-683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 467.Lindquist, S. W., D. J. Weber, M. E. Mangum, D. G. Hollis, and J. Jordan. 1995. Bordetella holmesii sepsis in an asplenic adolescent. Pediatr. Infect. Dis. J. 14:813-815. [PubMed] [Google Scholar]
- 468.Linnemann, C. C., and E. B. Perry. 1977. Bordetella parapertussis. Recent experience and a review of the literature. Am. J. Dis. Child. 131:560-563. [DOI] [PubMed] [Google Scholar]
- 469.Linnemann Jr., C. C. 1979. Host-parasite interactions in pertussis, publication NIH 79-1830, p. 3-18. International Symposium on Pertussis, Bethesda, Md.
- 470.Livey, I., C. J. Duggleby, and A. Robinson. 1987. Cloning and nucleotide sequence analysis of the serotype 2 fimbrial subunit gene of Bordetella pertussis. Mol. Microbiol. 1:203-209. [DOI] [PubMed] [Google Scholar]
- 471.Locht, C., M. C. Geoffroy, and G. Renauld. 1992. Common accessory genes for the Bordetella pertussis filamentous hemagglutinin and fimbriae share sequence similarities with the papC and papD gene families. EMBO J. 11:3175-3183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 472.Locht, C., and J. M. Keith. 1986. Pertussis toxin gene: nucleotide sequence and genetic organization. Science 232:1258-1264. [DOI] [PubMed] [Google Scholar]
- 473.Loeffelholz, M. J. 2003. Bordetella, p. 780-788. In P. R. Murray, E. J. Baron, J. H. Jorgensen, M. A. Pfaller, and R. H. Yolken (ed.), Manual of clinical microbiology, 8th ed. ASM Press, Washington, D.C.
- 474.Long, S. S., H. W. Lischner, A. Deforest, and J. L. Clark. 1990. Serologic evidence of subclinical pertussis in immunized children. Pediatr. Infect. Dis. J. 9:700-705. [DOI] [PubMed] [Google Scholar]
- 475.Long, S. S., C. J. Welkon, and J. L. Clark. 1990. Widespread silent transmission of pertussis in families: antibody correlates of infection and symptomatology. J. Infect. Dis. 161:480-486. [DOI] [PubMed] [Google Scholar]
- 476.Lo Re, V., III, P. J. Brennan, J. Wadlin, R. Weaver, and I. Nachamkin. 2001. Infected branchial cleft cyst due to Bordetella bronchiseptica in an immunocompetent patient. J. Clin. Microbiol. 39:4210-4212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 477.Lorenzo-Pajuelo, B., J. L. Villanueva, J. Rodriguez-Cuesta, N. Vergara-Irigaray, M. Bernabeu-Wittel, A. Garcia-Currel, and G. Martinez de Tejada. 2002. Cavitary pneumonia in an AIDS patient caused by an unusual Bordetella bronchiseptica variant producing reduced amounts of pertactin and other major antigens. J. Clin. Microbiol. 40:3146-3154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 478.Luttinger, P. 1916. The epidemiology of pertussis. Am. J. Dis. Child. 12:290-315. [Google Scholar]
- 479.Lyons, A. B. 1997. Pertussis toxin pretreatment alters the in vivo cell division behaviour and survival of B lymphocytes after intravenous transfer. Immunol. Cell Biol. 75:7-12. [DOI] [PubMed] [Google Scholar]
- 480.MacRae, K. D. 1988. Epidemiology, encephalopathy, and pertussis vaccines, p. 302-311. FEMS-Symposium Pertussis: Proceedings of a Conference Organized by the Society of Microbiology and Epidemiology of the GDR., Berlin, Germany.
- 481.Madsen, T. 1933. Vaccination against whooping cough. JAMA 101:187. [Google Scholar]
- 482.Madsen, T. 1925. Whooping cough: its bacteriology, diagnosis, prevention and treatment. Boston Med. Surg. J. 192:50-60. [Google Scholar]
- 483.Magyar, T., N. Chanter, A. J. Lax, J. M. Rutter, and G. A. Hall. 1988. The pathogenesis of turbinate atrophy in pigs caused by Bordetella bronchiseptica. Vet. Microbiol. 18:135-146. [DOI] [PubMed] [Google Scholar]
- 484.Magyar, T., V. L. King, and F. Kovács. 2002. Evaluation of vaccines for atrophic rhinitis--a comparison of three challenge models. Vaccine 20:1797-1802. [DOI] [PubMed] [Google Scholar]
- 485.Mahon, B. P., M. T. Brady, and K. H. Mills. 2000. Protection against Bordetella pertussis in mice in the absence of detectable circulating antibody: implications for long-term immunity in children. J. Infect. Dis. 181:2087-2091. [DOI] [PubMed] [Google Scholar]
- 486.Maitland, H. B., R. Kohn, and A. D. Macdonald. 1955. The histamine-sensitizing property of Haemophilus pertussis. J. Hyg. 53:196-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 487.Mallory, F. B., and A. A. Horner. 1912. Pertussis: the histological lesion in the respiratory tract. J. Med. Res. XXVII:115-123. [PMC free article] [PubMed] [Google Scholar]
- 488.Malmgren, B., B. Vahlquist, and R. Zetterstrom. 1960. Complications of immunization. Br. Med. J. 5215:1800-1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 489.Manclark, C. R., and J. L. Cowell. 1984. Pertussis, p. 69-106. In R. Germanier (ed.), Bacterial vaccines. Academic Press, Inc., New York, N.Y.
- 490.Manclark, C. R., B. D. Meade, and D. G. Burstyn. 1986. Serological response to Bordetella pertussis, p. 388-394. In N. R. Rose, A. Friedman, and J. L. Fahey (ed.), Manual of clinical and laboratory immunology, 3rd ed. American Society for Microbiology, Washington, D.C.
- 491.Mann, P. B., M. J. Kennett, and E. T. Harvill. 2004. Toll-like receptor 4 is critical to innate host defense in a murine model of bordetellosis. J. Infect. Dis. 189:833-836. [DOI] [PubMed] [Google Scholar]
- 492.Mannerstedt, G. 1934. Pertussis in adults. J. Pediatr. 5:596-600. [Google Scholar]
- 493.Marchant, C. D., A. M. Loughlin, S. M. Lett, C. W. Todd, L. H. Wetterlow, R. Bicchieri, S. Higham, P. Etkind, E. Silva, and G. R. Siber. 1994. Pertussis in Massachusetts, 1981-1991: incidence, serologic diagnosis, and vaccine effectiveness. J. Infect. Dis. 169:1297-305. [DOI] [PubMed] [Google Scholar]
- 494.Marchitto, K. S., S. G. Smith, C. Locht, and J. M. Keith. 1987. Nucleotide sequence homology to pertussis toxin gene in Bordetella bronchiseptica and Bordetella parapertussis. Infect. Immun. 55:497-501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 495.Marcon, M. J., A. C. Hamoudi, H. J. Cannon, and M. M. Hribar. 1987. Comparison of throat and nasopharyngeal swab specimens for culture diagnosis of Bordetella pertussis infection. J. Clin. Microbiol. 25:1109-1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 496.Martinez de Tejada, G., J. F. Miller, and P. A. Cotter. 1996. Comparative analysis of the virulence control systems of Bordetella pertussis and Bordetella bronchiseptica. Mol. Microbiol. 22:895-908. [DOI] [PubMed] [Google Scholar]
- 497.Martinez, S. M., C. A. Kemper, D. Haiduven, S. H. Cody, and S. C. Deresinski. 2001. Azithromycin prophylaxis during a hospitalwide outbreak of a pertussis-like illness. Infect. Control Hosp. Epidemiol. 22:781-783. [DOI] [PubMed] [Google Scholar]
- 498.Mastrantonio, P., M. Giuliano, P. Stefanelli, T. Sofia, L. De Marzi, G. Tarabini, M. Quarto, and A. Moiraghi. 1997. Bordetella parapertussis infections. Dev. Biol. Stand. 89:255-259. [PubMed] [Google Scholar]
- 499.Mastrantonio, P., P. Stefanelli, M. Giuliano, Y. Herrera Rojas, M. Ciofi degli Atti, A. Anemona, and A. E. Tozzi. 1998. Bordetella parapertussis infection in children: epidemiology, clinical symptoms, and molecular characteristics of isolates. J. Clin. Microbiol. 36:999-1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 500.Mather, E. C., B. Addison, D. Owens, C. J. Bierschwal, and C. E. Martin. 1973. Bordetella bronchiseptica associated with infertility in a mare. J. Am. Vet. Med. Assoc. 163:76-77. [PubMed] [Google Scholar]
- 501.Mathov, D. 1962. Effect of Haemophilus pertussis vaccine on human beings. Acta Allergol. 17:400-408. [Google Scholar]
- 502.Matsuzawa, T., A. Fukui, T. Kashimoto, K. Nagao, K. Oka, M. Miyake, and Y. Horiguchi. 2004. Bordetella dermonecrotic toxin undergoes proteolytic processing to be translocated from a dynamin-related endosome into the cytoplasm in an acidification-independent manner. J. Biol. Chem. 279:2866-2872. [DOI] [PubMed] [Google Scholar]
- 503.Mattoo, S., P. A. Cotter, and J. F. Miller. 2000. Differential roles of Bordetella virulence factors as inducers and modulators of the host immune response, p. 254. Proc. 100th Gen. Meet. Am. Soc. Microbiol. 2000. American Society for Microbiology, Washington, D.C.
- 504.Mattoo, S., A. K. Foreman-Wykert, P. A. Cotter, and J. F. Miller. 2001. Mechanisms of Bordetella pathogenesis. Front. Biosci. 6:E168-E186. [DOI] [PubMed] [Google Scholar]
- 505.Mattoo, S., and J. F. Miller. 2004. BtrV, a gram-positive anti-anti-sigma factor, exerts posttranscirptional control on the type III secretion apparatus components of Bordetella bronchiseptica, p. 113. Proc. 104th Gen. Meet. Am. Soc. Microbiol. 2004. American Society for Microbiology, Washington, D.C.
- 506.Mattoo, S., J. F. Miller, and P. A. Cotter. 2000. Role of Bordetella bronchiseptica fimbriae in tracheal colonization and development of a humoral immune response. Infect. Immun. 68:2024-2033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 507.Mattoo, S., M. H. Yuk, L. L. Huang, and J. F. Miller. 2004. Regulation of type III secretion in Bordetella. Mol. Microbiol. 52:1201-1214. [DOI] [PubMed] [Google Scholar]
- 508.Mazengia, E., E. A. Silva, J. A. Peppe, R. Timperi, and H. George. 2000. Recovery of Bordetella holmesii from patients with pertussis-like symptoms: use of pulsed-field gel electrophoresis to characterize circulating strains. J. Clin. Microbiol. 38:2330-2333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 509.McCandlish, I. A., H. Thompson, H. J. Cornwell, and N. G. Wright. 1978. A study of dogs with kennel cough. Vet. Rec. 102:293-301. [DOI] [PubMed] [Google Scholar]
- 510.McEniery, J. A., R. G. Delbridge, and D. M. Reith. 2004. Infant pertussis deaths and the management of cardiovascular compromise. J. Paediatr. Child Health 40:230-232. [DOI] [PubMed] [Google Scholar]
- 511.McGowan, J. P. 1911. Some observations on a laboratory epidemic, principally among dogs and cats, in which the animals affected presented the symptoms of the disease called “distemper.” J. Pathol. Bacteriol. 15:372-430. [Google Scholar]
- 512.McGregor, J., J. W. Ogle, and G. Curry-Kane. 1986. Perinatal pertussis. Obstet. Gynecol. 68:582-586. [PubMed] [Google Scholar]
- 513.McGuirk, P., P. A. Johnson, E. J. Ryan, and K. H. Mills. 2000. Filamentous hemagglutinin and pertussis toxin from Bordetella pertussis modulate immune responses to unrelated antigens. J. Infect. Dis. 182:1286-1289. [DOI] [PubMed] [Google Scholar]
- 514.McGuirk, P., B. P. Mahon, F. Griffin, and K. H. Mills. 1998. Compartmentalization of T cell responses following respiratory infection with Bordetella pertussis: hyporesponsiveness of lung T cells is associated with modulated expression of the co-stimulatory molecule CD28. Eur. J. Immunol. 28:153-163. [DOI] [PubMed] [Google Scholar]
- 515.McGuirk, P., and K. H. Mills. 2000. Direct anti-inflammatory effect of a bacterial virulence factor: IL-10-dependent suppression of IL-12 production by filamentous hemagglutinin from Bordetella pertussis. Eur. J. Immunol. 30:415-422. [DOI] [PubMed] [Google Scholar]
- 516.McKenzie, R. A., A. D. Wood, and P. J. Blackall. 1979. Pneumonia associated with Bordetella bronchiseptica in captive koalas. Aust. Vet. J. 55:427-430. [DOI] [PubMed] [Google Scholar]
- 517.McMillan, D. J., M. Shojaei, G. S. Chhatwal, C. A. Guzman, and M. J. Walker. 1996. Molecular analysis of the bvg-repressed urease of Bordetella bronchiseptica. Microb. Pathog. 21:379-394. [DOI] [PubMed] [Google Scholar]
- 518.McNicol, P., S. Giercke, M. Gray, D. Martin, B. Brodeur, M. S. Peppler, T. Williams, and G. Hammond. 1995. Evaluation and validation of a monoclonal immunofluorescent reagent for direct detection of Bordetella pertussis. J. Clin. Microbiol. 33:2868-2871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 519.Meade, B., C. M. Mink, and C. R. Manclark. 1990. Serodiagnosis of pertussis, p. 322-329. Proceedings of the Sixth International Symposium on Pertussis.
- 520.Meade, B. D., and A. Bollen. 1994. Recommendations for use of the polymerase chain reaction in the diagnosis of Bordetella pertussis infections. J. Med. Microbiol. 41:51-55. [DOI] [PubMed] [Google Scholar]
- 521.Meade, B. D., P. D. Kind, J. B. Ewell, P. P. McGrath, and C. R. Manclark. 1984. In vitro inhibition of murine macrophage migration by Bordetella pertussis lymphocytosis-promoting factor. Infect. Immun. 45:718-725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 522.Meade, B. D., P. D. Kind, and C. R. Manclark. 1984. Lymphocytosis-promoting factor of Bordetella pertussis alters mononuclear phagocyte circulation and response to inflammation. Infect. Immun. 46:733-739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 523.Medical Research Council. 1951. The prevention of whooping cough by vaccination. Br. Med. J. 1:1464-1471. [PMC free article] [PubMed] [Google Scholar]
- 524.Medical Research Council. 1959. Vaccination against whooping cough. Br. Med. J. 1:994-1000. [PMC free article] [PubMed] [Google Scholar]
- 525.Medical Research Council. 1956. Vaccination against whooping cough: relation between protection in children and results of laboratory tests. Br. Med. J. 2:454-462. [PMC free article] [PubMed] [Google Scholar]
- 526.Melchior, J. C. 1977. Infantile spasms and early immunization against whooping cough. Danish survey from 1970 to 1975. Arch. Dis. Child. 52:134-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 527.Melton, A. R., and A. A. Weiss. 1993. Characterization of environmental regulators of Bordetella pertussis. Infect. Immun. 61:807-815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 528.Melton, A. R., and A. A. Weiss. 1989. Environmental regulation of expression of virulence determinants in Bordetella pertussis. J. Bacteriol. 171:6206-6212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 529.Menozzi, F. D., P. E. Boucher, G. Riveau, C. Gantiez, and C. Locht. 1994. Surface-associated filamentous hemagglutinin induces autoagglutination of Bordetella pertussis. Infect. Immun. 62:4261-4269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 530.Menozzi, F. D., C. Gantiez, and C. Locht. 1991. Interaction of the Bordetella pertussis filamentous hemagglutinin with heparin. FEMS Microbiol. Lett. 62:59-64. [DOI] [PubMed] [Google Scholar]
- 531.Merkel, T. J., C. Barros, and S. Stibitz. 1998. Characterization of the bvgR locus of Bordetella pertussis. J. Bacteriol. 180:1682-1690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 532.Merkel, T. J., P. E. Boucher, S. Stibitz, and V. K. Grippe. 2003. Analysis of bvgR expression in Bordetella pertussis. J. Bacteriol. 185:6902-6912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 533.Merkel, T. J., and S. Stibitz. 1995. Identification of a locus required for the regulation of bvg-repressed genes in Bordetella pertussis. J. Bacteriol. 177:2727-2736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 534.Mertens, P. L., F. S. Stals, J. F. Schellekens, A. W. Houben, and J. Huisman. 1999. An epidemic of pertussis among elderly people in a religious institution in The Netherlands. Eur. J. Clin. Microbiol. Infect. Dis. 18:242-247. [DOI] [PubMed] [Google Scholar]
- 535.Mertsola, J. 1985. Mixed outbreak of Bordetella pertussis and Bordetella parapertussis infection in Finland. Eur. J. Clin. Microbiol. 4:123-128. [DOI] [PubMed] [Google Scholar]
- 536.Mertsola, J., O. Ruuskanen, T. Kuronen, O. Meurman, and M. K. Viljanen. 1990. Serologic diagnosis of pertussis: evaluation of pertussis toxin and other antigens in enzyme-linked immunosorbent assay. J. Infect. Dis. 161:966-971. [DOI] [PubMed] [Google Scholar]
- 537.Mikelova, L. K., S. A. Halperin, D. Scheifele, B. Smith, E. Ford-Jones, W. Vaudry, T. Jadavji, B. Law, and D. Moore. 2003. Predictors of death in infants hospitalized with pertussis: a case-control study of 16 pertussis deaths in Canada. J. Pediatr. 143:576-581. [DOI] [PubMed] [Google Scholar]
- 538.Miles, R. N., and G. P. Hosking. 1983. Pertussis: should we immunise neurologically disabled and developmentally delayed children? Br. Med. J. (Clin. Res. Ed.) 287:318-320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 539.Miller, D., J. Wadsworth, J. Diamond, and E. Ross. 1985. Pertussis vaccine and whooping cough as risk factors in acute neurological illness and death in young children. Dev. Biol. Stand. 61:389-394. [PubMed] [Google Scholar]
- 540.Miller, D. L., R. Alderslade, and E. M. Ross. 1982. Whooping cough and whooping cough vaccine: the risks and benefits debate. Epidemiol. Rev. 4:1-24. [DOI] [PubMed] [Google Scholar]
- 541.Miller, D. L., E. M. Ross, R. Alderslade, M. H. Bellman, and N. S. Rawson. 1981. Pertussis immunisation and serious acute neurological illness in children. Br. Med. J. (Clin. Res. Ed.) 282:1595-1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 542.Miller, H. 1956. Discussion on the neurological complications of the acute specific fevers. Proc. R. Soc. Med. 49:139-146. [PMC free article] [PubMed] [Google Scholar]
- 543.Miller, H. G., and J. B. Stanton. 1954. Neurological sequelae of prophylactic inoculation. Q. J. Med. 23:1-27. [PubMed] [Google Scholar]
- 544.Miller, J. F., S. A. Johnson, W. J. Black, D. T. Beattie, J. J. Mekalanos, and S. Falkow. 1992. Constitutive sensory transduction mutations in the Bordetella pertussis bvgS gene. J. Bacteriol. 174:970-979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 545.Miller, J. J. J., T. M. Saito, and R. J. Silverberg. 1941. Parapertussis. J. Pediatr. 19:229-240. [Google Scholar]
- 546.Miller, J. J. J., R. J. Silverberg, T. M. Saito, et al. 1943. An agglutinative reaction for Hemophilus pertussis. II. Its relation to clinical immunity. J. Pediatr. 22:644-651. [Google Scholar]
- 547.Mills, K. H., A. Barnard, J. Watkins, and K. Redhead. 1993. Cell-mediated immunity to Bordetella pertussis: role of Th1 cells in bacterial clearance in a murine respiratory infection model. Infect. Immun. 61:399-410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 548.Mills, K. H., M. Brady, E. Ryan, and B. P. Mahon. 1998. A respiratory challenge model for infection with Bordetella pertussis: application in the assessment of pertussis vaccine potency and in defining the mechanism of protective immunity. Dev. Biol. Stand. 95:31-41. [PubMed] [Google Scholar]
- 549.Mills, K. H., M. Ryan, E. Ryan, and B. P. Mahon. 1998. A murine model in which protection correlates with pertussis vaccine efficacy in children reveals complementary roles for humoral and cell-mediated immunity in protection against Bordetella pertussis. Infect. Immun. 66:594-602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 550.Mink, C. M., J. D. Cherry, P. Christenson, K. Lewis, E. Pineda, D. Shlian, J. A. Dawson, and D. A. Blumberg. 1992. A search for Bordetella pertussis infection in university students. Clin. Infect. Dis. 14:464-471. [DOI] [PubMed] [Google Scholar]
- 551.Mink, C. M., C. H. O'Brien, S. Wassilak, A. Deforest, and B. D. Meade. 1994. Isotype and antigen specificity of pertussis agglutinins following whole-cell pertussis vaccination and infection with Bordetella pertussis. Infect. Immun. 62:1118-1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 552.Mink, C. M., M. Uhari, D. A. Blumberg, M. Knip, K. Lewis, P. D. Christenson, M. Toyoda, S. C. Jordan, S. R. Levin, and J. D. Cherry. 1990. Metabolic and hematologic effects and immune complex formation related to pertussis immunization. Pediatr. Res. 27:353-357. [DOI] [PubMed] [Google Scholar]
- 553.Mizushima, Y., M. Mori, T. Ogita, and T. Nakamura. 1979. Adjuvant for IgE antibody and islet-activating protein in Bordetella pertussis. Int. Arch. Allergy Appl. Immunol. 58:426-429. [DOI] [PubMed] [Google Scholar]
- 554.Mobberley-Schuman, P. S., B. Connelly, and A. Weiss. 2003. Phagocytosis of Bordetella pertussis incubated with convalescent serum. J. Infect. Dis. 187:1646-1653. [DOI] [PubMed] [Google Scholar]
- 555.Molski, T. F., P. H. Naccache, M. L. Marsh, J. Kermode, E. L. Becker, and R. I. Sha'afi. 1984. Pertussis toxin inhibits the rise in the intracellular concentration of free calcium that is induced by chemotactic factors in rabbit neutrophils: possible role of the “G proteins” in calcium mobilization. Biochem. Biophys. Res. Commun. 124:644-650. [DOI] [PubMed] [Google Scholar]
- 556.Montaraz, J. A., P. Novotny, and J. Ivanyi. 1985. Identification of a 68-kilodalton protective protein antigen from Bordetella bronchiseptica. Infect. Immun. 47:744-751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 557.Mooi, F. R., W. H. Jansen, H. Brunings, H. Gielen, H. G. van der Heide, H. C. Walvoort, and P. A. Guinee. 1992. Construction and analysis of Bordetella pertussis mutants defective in the production of fimbriae. Microb. Pathog. 12:127-135. [DOI] [PubMed] [Google Scholar]
- 558.Mooi, F. R., H. G. van der Heide, A. R. ter Avest, K. G. Welinder, I. Livey, B. A. van der Zeijst, and W. Gaastra. 1987. Characterization of fimbrial subunits from Bordetella species. Microb. Pathog. 2:473-484. [DOI] [PubMed] [Google Scholar]
- 559.Moore, D. L., N. Le Saux, D. Scheifele, and S. A. Halperin. 2004. Lack of evidence of encephalopathy related to pertussis vaccine: active surveillance by IMPACT, Canada, 1993-2002. Pediatr. Infect. Dis. J. 23:568-571. [DOI] [PubMed] [Google Scholar]
- 560.Morris, J. T., and M. Myers. 1998. Bacteremia due to Bordetella holmesii. Clin. Infect. Dis. 27:912-913. [DOI] [PubMed] [Google Scholar]
- 561.Morse, S. I. 1976. Biologically active components and properties of Bordetella pertussis. Adv. Appl. Microbiol. 20:9-26. [DOI] [PubMed] [Google Scholar]
- 562.Morse, S. I. 1977. Lymphocytosis-promoting factor of Bordetella pertussis: isolation, characterization, and biological activity. J. Infect. Dis. 136(Suppl):S234-S238. [DOI] [PubMed] [Google Scholar]
- 563.Morse, S. I. 1965. Studies on the lymphocytosis induced in mice by Bordetella pertussis. J. Exp. Med. 121:49-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 564.Morse, S. I., and K. K. Bray. 1969. The occurrence and properties of leukocytosis and lymphocytosis-stimulating material in the supernatant fluids of Bordetella pertussis cultures. J. Exp. Med. 129:523-550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 565.Morse, S. I., and J. H. Morse. 1976. Isolation and properties of the leukocytosis- and lymphocytosis-promoting factor of Bordetella pertussis. J. Exp. Med. 143:1483-1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 566.Mortimer, E. A., Jr. 1980. Pertussis immunization: problems, perspectives, prospects. Hosp. Pract. 15:103-107, 111-112, 117-118. [DOI] [PubMed] [Google Scholar]
- 567.Mortimer, E. A., Jr., and P. K. Jones. 1979. An evaluation of pertussis vaccine. Rev. Infect. Dis. 1:927-934. [DOI] [PubMed] [Google Scholar]
- 568.Mortimer, E. A., Jr., P. K. Jones, and L. Adelson. 1983. DTP and SIDS. Pediatr. Infect. Dis. J. 2:492-493. [DOI] [PubMed] [Google Scholar]
- 569.Mortimer, E. A., Jr., M. Kimura, J. D. Cherry, H. Kuno-Sakai, M. G. Stout, C. L. Dekker, R. Hayashi, Y. Miyamoto, J. V. Scott, T. Aoyama, et al. 1990. Protective efficacy of the Takeda acellular pertussis vaccine combined with diphtheria and tetanus toxoids following household exposure of Japanese children. Am. J. Dis. Child. 144:899-904. [DOI] [PubMed] [Google Scholar]
- 570.Mortimer, E. A., Jr., and P. K. Jones. 1979. Pertussis vaccine in the United States: the benefit-risk ratio, p. 250, International Symposium on Pertussis. National Institutes of Health, Bethesda, Md.
- 571.Mountzouros, K. T., A. Kimura, and J. L. Cowell. 1992. A bactericidal monoclonal antibody specific for the lipooligosaccharide of Bordetella pertussis reduces colonization of the respiratory tract of mice after aerosol infection with B. pertussis. Infect. Immun. 60:5316-5318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 572.Müller, F. M., J. E. Hoppe, and C. H. Wirsing von König. 1997. Laboratory diagnosis of pertussis: state of the art in 1997. J. Clin. Microbiol. 35:2435-2443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 573.Munoz, J. 1963. Comparison of Bordetella pertussis cells and Freund's adjuvant with respect to their antibody inducing and anaphylactogenic properties. J. Immunol. 90:132-139. [PubMed] [Google Scholar]
- 574.Munoz, J. 1971. Protein toxins from Bordetella pertussis, p. 271-300. In S. Kadis, T. C. Montie, and S. A. Ajl (ed.), Microbiol toxins, vol. IIA. Academic Press, Inc., New York, N.Y. [Google Scholar]
- 575.Munoz, J., and R. K. Bergman. 1977. Bordetella pertussis — immunological and other biological activities, vol. 4. Marcel Dekker, Inc., New York, N.Y.
- 576.Munoz, J., and R. K. Bergman. 1968. Histamine-sensitizing factors from microbial agents, with special reference to Bordetella pertussis. Bacteriol. Rev. 32:103-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 577.Munoz, J. J. 1988. Action of pertussigen (pertussis toxin) on the host immune system in pathogenesis and immunity in pertussis, p. 173-192. In A. C. Wardlaw and R. Parton (ed.), Pathogenesis and immunity in pertussis. John Wiley & Sons, Ltd., New York, N.Y.
- 578.Munoz, J. J., M. G. Peacock, and W. J. Hadlow. 1987. Anaphylaxis or so-called encephalopathy in mice sensitized to an antigen with the aid of pertussigen (pertussis toxin). Infect. Immun. 55:1004-1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 579.Nagel, J., and E. J. Poot-Scholtens. 1983. Serum IgA antibody to Bordetella pertussis as an indicator of infection. J. Med. Microbiol. 16:417-426. [DOI] [PubMed] [Google Scholar]
- 580.Nakai, T., A. Sawata, and K. Kume. 1985. Intracellular locations of dermonecrotic toxins in Pasteurella multocida and in Bordetella bronchiseptica. Am. J. Vet. Res. 46:870-874. [PubMed] [Google Scholar]
- 581.Nakase, Y., and M. Endoh. 1988. Heat-labile toxin of Bordetella pertussis, p. 217-229. In A. C. Wardlaw and R. Parton (ed.), Pathogenesis and immunity in pertussis. John Wiley & Sons, Inc., New York, N.Y.
- 582.Nakase, Y., M. Tateishi, K. Sekiya, and T. Kasuga. 1970. Chemical and biological properties of the purified O antigen of Bordetella pertussis. Jpn. J. Microbiol. 14:1-8. [DOI] [PubMed] [Google Scholar]
- 583.Nelson, J. D. 1978. The changing epidemiology of pertussis in young infants. The role of adults as reservoirs of infection. Am. J. Dis. Child. 132:371-373. [DOI] [PubMed] [Google Scholar]
- 584.Nelson, K. E., F. Gavitt, M. D. Batt, C. A. Kallick, K. T. Reddi, and S. Levin. 1975. The role of adenoviruses in the pertussis syndrome. J. Pediatr. 86:335-341. [DOI] [PubMed] [Google Scholar]
- 585.Nencioni, L., M. G. Pizza, G. Volpini, M. T. De Magistris, F. Giovannoni, and R. Rappuoli. 1991. Properties of the B oligomer of pertussis toxin. Infect. Immun. 59:4732-4734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 586.Nennig, M. E., H. R. Shinefield, K. M. Edwards, S. B. Black, and B. H. Fireman. 1996. Prevalence and incidence of adult pertussis in an urban population. JAMA 275:1672-1674. [PubMed] [Google Scholar]
- 587.Ner, Z., L. A. Ross, M. V. Horn, T. G. Keens, E. F. MacLaughlin, V. A. Starnes, and M. S. Woo. 2003. Bordetella bronchiseptica infection in pediatric lung transplant recipients. Pediatr. Transplant. 7:413-417. [DOI] [PubMed] [Google Scholar]
- 588.Nicoll, A., and A. Gardner. 1988. Whooping cough and unrecognised postperinatal mortality. Arch. Dis. Child. 63:41-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 589.Nicosia, A., A. Bartoloni, M. Perugini, and R. Rappuoli. 1987. Expression and immunological properties of the five subunits of pertussis toxin. Infect. Immun. 55:963-967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 590.Nicosia, A., M. Perugini, C. Franzini, M. C. Casagli, M. G. Borri, G. Antoni, M. Almoni, P. Neri, G. Ratti, and R. Rappuoli. 1986. Cloning and sequencing of the pertussis toxin genes: operon structure and gene duplication. Proc. Natl. Acad. Sci. USA 83:4631-4635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 591.Njamkepo, E., F. Delisle, I. Hagege, G. Gerbaud, and N. Guiso. 2000. Bordetella holmesii isolated from a patient with sickle cell anemia: analysis and comparison with other Bordetella holmesii isolates. Clin. Microbiol. Infect. 6:131-136. [DOI] [PubMed] [Google Scholar]
- 592.Noble, G. R., R. H. Bernier, E. C. Esber, M. C. Hardegree, A. R. Hinman, D. Klein, and A. J. Saah. 1987. Acellular and whole-cell pertussis vaccines in Japan. Report of a visit by US scientists. JAMA 257:1351-1356. [PubMed] [Google Scholar]
- 593.O'Brien, A. D., T. J. Standiford, K. A. Bucknell, S. E. Wilcoxen, and R. Paine III. 1999. Role of alveolar epithelial cell intercellular adhesion molecule-l in host defense against Klebsiella pneumoniae. Am. J. Physiol. 276:L961-L970. [DOI] [PubMed] [Google Scholar]
- 594.Ohgitani, T., T. Okabe, and N. Sasaki. 1991. Characterization of haemagglutinin from Bordetella bronchiseptica. Vaccine 9:653-658. [DOI] [PubMed] [Google Scholar]
- 595.Okajima, F., and M. Ui. 1984. ADP-ribosylation of the specific membrane protein by islet-activating protein, pertussis toxin, associated with inhibition of a chemotactic peptide-induced arachidonate release in neutrophils. A possible role of the toxin substrate in Ca2+-mobilizing biosignaling. J. Biol. Chem. 259:13863-13871. [PubMed] [Google Scholar]
- 596.Olin, P., L. Gustafsson, L. Barreto, L. Hessel, T. C. Mast, A. V. Rie, H. Bogaerts, and J. Storsaeter. 2003. Declining pertussis incidence in Sweden following the introduction of acellular pertussis vaccine. Vaccine 21:2015-2021. [DOI] [PubMed] [Google Scholar]
- 597.Olin, P., F. Rasmussen, L. Gustafsson, H. O. Hallander, H. Heijbel, and the Ad Hoc Group for the Study of Pertussis Vaccines. 1997. Randomised controlled trial of two-component, three-component, and five-component acellular pertussis vaccines compared with whole-cell pertussis vaccine. Lancet 350:1569-1577. [DOI] [PubMed] [Google Scholar]
- 598.Oliver, D. C., G. Huang, and R. C. Fernandez. 2003. Identification of secretion determinants of the Bordetella pertussis BrkA autotransporter. J. Bacteriol. 185:489-495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 599.Oliver, D. C., G. Huang, E. Nodel, S. Pleasance, and R. C. Fernandez. 2003. A conserved region within the Bordetella pertussis autotransporter BrkA is necessary for folding of its passenger domain. Mol. Microbiol. 47:1367-1383. [DOI] [PubMed] [Google Scholar]
- 600.Olson, L. C. 1975. Pertussis: Medicine (Baltimore) 54:427-469. [DOI] [PubMed]
- 601.Onorato, I. M., and S. G. Wassilak. 1987. Laboratory diagnosis of pertussis: the state of the art. Pediatr. Infect. Dis. J. 6:145-151. [DOI] [PubMed] [Google Scholar]
- 602.Onorato, I. M., S. G. Wassilak, and B. Meade. 1992. Efficacy of whole-cell pertussis vaccine in preschool children in the United States. JAMA 267:2745-2749. [PubMed] [Google Scholar]
- 603.Panina, E., M. Han, S. Mattoo, M. H. Yuk, and J. F. Miller. 2004. Identification of a Bordetella type III secreted effector protein, p. 78. Proc. 104th Gen. Meet. Am. Soc. Microbiol. 2004. American Society for Microbiology, Washington, D.C.
- 604.Papasian, C. J., N. J. Downs, R. L. Talley, D. J. Romberger, and G. R. Hodges. 1987. Bordetella bronchiseptica bronchitis. J. Clin. Microbiol. 25:575-577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 605.Parfentjev, I. A. 1955. Bacterial allergy increases susceptibility to influenza virus in mice. Proc. Soc. Exp. Biol. Med. 90:373-375. [DOI] [PubMed] [Google Scholar]
- 606.Parfentjev, I. A. 1948. Histamine shock in mice sensitized with Hemophilus pertussis vaccine. J. Pharmacol. Exp. Ther. 92:411-413. [PubMed] [Google Scholar]
- 607.Parfentjev, I. A., and W. L. Schleyer. 1949. The influence of histamine on the blood sugar level of normal and sensitized mice. Arch. Biochem. Biophys. 20:341-346. [PubMed] [Google Scholar]
- 608.Parkhill, J., M. Sebaihia, A. Preston, L. D. Murphy, N. Thomson, D. E. Harris, M. T. Holden, C. M. Churcher, S. D. Bentley, K. L. Mungall, A. M. Cerdeno-Tarraga, L. Temple, K. James, B. Harris, M. A. Quail, M. Achtman, R. Atkin, S. Baker, D. Basham, N. Bason, I. Cherevach, T. Chillingworth, M. Collins, A. Cronin, P. Davis, J. Doggett, T. Feltwell, A. Goble, N. Hamlin, H. Hauser, S. Holroyd, K. Jagels, S. Leather, S. Moule, H. Norberczak, S. O'Neil, D. Ormond, C. Price, E. Rabbinowitsch, S. Rutter, M. Sanders, D. Saunders, K. Seeger, S. Sharp, M. Simmonds, J. Skelton, R. Squares, S. Squares, K. Stevens, L. Unwin, S. Whitehead, B. G. Barrell, and D. J. Maskell. 2003. Comparative analysis of the genome sequences of Bordetella pertussis, Bordetella parapertussis and Bordetella bronchiseptica. Nat. Genet. 35:32-40. [DOI] [PubMed] [Google Scholar]
- 609.Parton, R. 1985. Effect of prednisolone on the toxicity of Bordetella pertussis for mice. J. Med. Microbiol. 19:391-400. [DOI] [PubMed] [Google Scholar]
- 610.Pauwels, R., M. Van der Straeten, B. Platteau, and H. Bazin. 1983. The non-specific enhancement of allergy. I. In vivo effects of Bordetella pertussis vaccine on IgE synthesis. Allergy 38:239-246. [DOI] [PubMed] [Google Scholar]
- 611.Pearson, R. D., P. Symes, M. Conboy, A. A. Weiss, and E. L. Hewlett. 1987. Inhibition of monocyte oxidative responses by Bordetella pertussis adenylate cyclase toxin. J. Immunol. 139:2749-2754. [PubMed] [Google Scholar]
- 612.Peppler, M. S. 1984. Two physically and serologically distinct lipopolysaccharide profiles in strains of Bordetella pertussis and their phenotype variants. Infect. Immun. 43:224-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 613.Peraire, J., C. Manso, E. Vidal, and C. Richart. 1996. Bordetella bronchiseptica in a patient with prostatic adenocarcinoma. Enferm. Infecc. Microbiol. Clin. 14:458-459. [PubMed] [Google Scholar]
- 614.Petrocheilou-Paschou, V., K. Georgilis, E. Kostis, H. Prifti, N. Zakopoulos, and S. Stamatelopoulos. 2000. Bronchitis caused by Bordetella bronchiseptica in an elderly woman. Clin. Microbiol. Infect. 6:147-148. [DOI] [PubMed] [Google Scholar]
- 615.Pichichero, M. E., M. A. Deloria, M. B. Rennels, E. L. Anderson, K. M. Edwards, M. D. Decker, J. A. Englund, M. C. Steinhoff, A. Deforest, and B. D. Meade. 1997. A safety and immunogenicity comparison of 12 acellular pertussis vaccines and one whole-cell pertussis vaccine given as a fourth dose in 15- to 20-month-old children. Pediatrics 100:772-788. [DOI] [PubMed] [Google Scholar]
- 616.Pichichero, M. E., K. M. Edwards, E. L. Anderson, M. B. Rennels, J. A. Englund, D. E. Yerg, W. C. Blackwelder, D. L. Jansen, and B. D. Meade. 2000. Safety and immunogenicity of six acellular pertussis vaccines and one whole-cell pertussis vaccine given as a fifth dose in four- to six-year-old children. Pediatrics 105:e11. [DOI] [PubMed] [Google Scholar]
- 617.Pichichero, M. E., W. J. Hoeger, and J. R. Casey. 2003. Azithromycin for the treatment of pertussis. Pediatr. Infect. Dis. J. 22:847-849. [DOI] [PubMed] [Google Scholar]
- 618.Pieroni, R. E., D. L. Stevens, A. Stojanovic, and L. Levine. 1971. Investigation of cutaneous histamine sensitivity in children with pertussis. Int. Arch. Allergy Appl. Immunol. 41:940-944. [DOI] [PubMed] [Google Scholar]
- 619.Pilorget, H., A. Montbrun, T. Attali, I. Tiran-Rajaofera, C. Bony, C. Brayer, S. Samperiz, and J. L. Alessandri. 2003. Malignant pertussis in the young infant. Arch. Pediatr. 10:787-790. (In French.) [DOI] [PubMed] [Google Scholar]
- 620.Pishko, E. J., D. J. Betting, C. S. Hutter, and E. T. Harvill. 2003. Bordetella pertussis acquires resistance to complement-mediated killing in vivo. Infect. Immun. 71:4936-4942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 621.Pishko, E. J., G. S. Kirimanjeswara, M. R. Pilione, L. Gopinathan, M. J. Kennett, and E. T. Harvill. 2004. Antibody-mediated bacterial clearance from the lower respiratory tract of mice requires complement component C3. Eur. J. Immunol. 34:184-193. [DOI] [PubMed] [Google Scholar]
- 622.Pittman, M. 1951. Comparison of the histamine sensitizing property with the protective activity of pertussis vaccines for mice. J. Infect. Dis. 89:300-304. [DOI] [PubMed] [Google Scholar]
- 623.Pittman, M. 1984. The concept of pertussis as a toxin-mediated disease. Pediatr. Infect. Dis. J. 3:467-486. [DOI] [PubMed] [Google Scholar]
- 624.Pittman, M. 1979. Pertussis toxin: the cause of the harmful effects and prolonged immunity of whooping cough. A hypothesis. Rev. Infect. Dis. 1:401-412. [DOI] [PubMed] [Google Scholar]
- 625.Pittman, M. 1951. Sensitivity of mice to histamine during respiratory infection by Hemophilus pertussis. Proc. Soc. Exp. Biol. Med. 77:70-74. [DOI] [PubMed] [Google Scholar]
- 626.Pizza, M., M. Bugnoli, R. Manetti, A. Covacci, and R. Rappuoli. 1990. The subunit S1 is important for pertussis toxin secretion. J. Biol. Chem. 265:17759-17763. [PubMed] [Google Scholar]
- 627.Poddar, S. K. 2003. Detection and discrimination of B. pertussis and B. holmesii by real-time PCR targeting IS481 using a beacon probe and probe-target melting analysis. Mol. Cell. Probes 17:91-98. [DOI] [PubMed] [Google Scholar]
- 628.Pollock, T. M., E. Miller, J. Y. Mortimer, and G. Smith. 1984. Symptoms after primary immunisation with DTP and with DT vaccine. Lancet ii:146-149. [DOI] [PubMed] [Google Scholar]
- 629.Pollock, T. M., and J. Morris. 1983. A 7-year survey of disorders attributed to vaccination in North West Thames region. Lancet i:753-757. [DOI] [PubMed] [Google Scholar]
- 630.Pooboni, S., N. Roberts, C. Westrope, D. R. Jenkins, H. Killer, H. C. Pandya, and R. K. Firmin. 2003. Extracorporeal life support in pertussis. Pediatr. Pulmonol. 36:310-315. [DOI] [PubMed] [Google Scholar]
- 631.Porter, J. F., K. Connor, and W. Donachie. 1994. Isolation and characterization of Bordetella parapertussis-like bacteria from ovine lungs. Microbiology 140:255. [DOI] [PubMed] [Google Scholar]
- 632.Porter, J. F., R. Parton, and A. C. Wardlaw. 1991. Growth and survival of Bordetella bronchiseptica in natural waters and in buffered saline without added nutrients. Appl. Environ. Microbiol. 57:1202-1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 633.Porter, J. F., and A. C. Wardlaw. 1993. Long-term survival of Bordetella bronchiseptica in lakewater and in buffered saline without added nutrients. FEMS Microbiol. Lett. 110:33-36. [DOI] [PubMed] [Google Scholar]
- 634.Postels-Multani, S., H. J. Schmitt, C. H. Wirsing von König, H. L. Bock, and H. Bogaerts. 1995. Symptoms and complications of pertussis in adults. Infection 23:139-142. [DOI] [PubMed] [Google Scholar]
- 635.Povitzky, O. R., and E. Worth. 1916. Agglutination in pertussis: its characteristics and its comparative value in clinical diagnosis, and in determination of genus and species. Arch. Intern. Med. 17:279-292. [Google Scholar]
- 636.Prasad, S. M., Y. Yin, E. Rodzinski, E. I. Tuomanen, and H. R. Masure. 1993. Identification of a carbohydrate recognition domain in filamentous hemagglutinin from Bordetella pertussis. Infect. Immun. 61:2780-2785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 637.Prensky, A. L. 1974. Pertussis vaccination. Dev. Med. Child Neurol. 16:539-543. [DOI] [PubMed] [Google Scholar]
- 638.Preston, A., J. Parkhill, and D. J. Maskell. 2004. The Bordetellae: lessons from genomics. Nat. Rev. Microbiol. 2:379-390. [DOI] [PubMed] [Google Scholar]
- 639.Preston, A., R. Thomas, and D. J. Maskell. 2002. Mutational analysis of the Bordetella pertussis wlb LPS biosynthesis locus. Microb. Pathog. 33:91-95. [DOI] [PubMed] [Google Scholar]
- 640.Preston, N. W. 1965. Effectiveness of pertussis vaccines. Br. Med. J. 2:11-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 641.Preston, N. W. 1988. Pertussis today, p. 1-18. In A. C. Wardlaw, and R. Parton (ed.), Pathogenesis and immunity in pertussis. John Wiley & Sons, Inc., New York, N.Y.
- 642.Preston, N. W. 1976. Prevalent serotypes of Bordetella pertussis in non-vaccinated communities. J. Hyg. 77:85-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 643.Preston, N. W. 1963. Type-specific immunity against whooping cough. Br. Med. J. 3:724-726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 644.Preston, N. W., and T. N. Stanbridge. 1972. Efficacy of pertussis vaccines: a brighter horizon. Br. Med. J. 3:448-451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 645.Purdy, K. W., J. W. Hay, M. F. Botteman, and J. I. Ward. 2004. Evaluation of strategies for use of acellular pertussis vaccine in adolescents and adults: a cost-benefit analysis. Clin. Infect. Dis. 39:20-28. [DOI] [PubMed] [Google Scholar]
- 646.Quinn, P. J., M. E. Carter, B. K. Markey, and G. R. and Carter. 1994. Bordetella species, p. 280-283. In P. J. Quinn, M. E. Carter, B. K. Markey, and G. R. Carter (ed.), Clinical veterinary microbiology: Wolfe Publishing, London, United Kingdom.
- 647.Rambow, A. A., R. C. Fernandez, and A. A. Weiss. 1998. Characterization of BrkA expression in Bordetella bronchiseptica. Infect. Immun. 66:3978-3980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 648.Rankin, S., and E. Rozengurt. 1994. Platelet-derived growth factor modulation of focal adhesion kinase (p125FAK) and paxillin tyrosine phosphorylation in Swiss 3T3 cells. Bell-shaped dose response and cross-talk with bombesin. J. Biol. Chem. 269:704-710. [PubMed] [Google Scholar]
- 649.Reed, C. E., M. Benner, S. D. Lockey, T. Enta, S. Makino, and R. H. Carr. 1972. On the mechanism of the adjuvant effect of Bordetella pertussis vaccine. J. Allergy Clin. Immunol. 49:174-182. [DOI] [PubMed] [Google Scholar]
- 650.Reina, J., A. Bassa, I. Llompart, N. Borrell, J. Gomez, and A. Serra. 1991. Pneumonia caused by Bordetella bronchiseptica in a patient with a thoracic trauma. Infection 19:46-48. [DOI] [PubMed] [Google Scholar]
- 651.Reischl, U., N. Lehn, G. N. Sanden, and M. J. Loeffelholz. 2001. Real-time PCR assay targeting IS481 of Bordetella pertussis and molecular basis for detecting Bordetella holmesii. J. Clin. Microbiol. 39:1963-1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 652.Reizenstein, E., B. Johansson, L. Mardin, J. Abens, R. Mollby, and H. O. Hallander. 1993. Diagnostic evaluation of polymerase chain reaction discriminative for Bordetella pertussis, B. parapertussis, and B. bronchiseptica. Diagn. Microbiol. Infect. Dis. 17:185-191. [DOI] [PubMed] [Google Scholar]
- 653.Reizenstein, E., L. Lindberg, R. Mollby, and H. O. Hallander. 1996. Validation of nested Bordetella PCR in pertussis vaccine trial. J. Clin. Microbiol. 34:810-815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 654.Relman, D., E. Tuomanen, S. Falkow, D. T. Golenbock, K. Saukkonen, and S. D. Wright. 1990. Recognition of a bacterial adhesion by an integrin: macrophage CR3 (alpha M beta 2, CD11b/CD18) binds filamentous hemagglutinin of Bordetella pertussis. Cell 61:1375-1382. [DOI] [PubMed] [Google Scholar]
- 655.Relman, D. A., M. Domenighini, E. Tuomanen, R. Rappuoli, and S. Falkow. 1989. Filamentous hemagglutinin of Bordetella pertussis: nucleotide sequence and crucial role in adherence. Proc. Natl. Acad. Sci. USA 86:2637-2641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 656.Rennels, M. B., M. A. Deloria, M. E. Pichichero, G. A. Losonsky, J. A. Englund, B. D. Meade, E. L. Anderson, M. C. Steinhoff, and K. M. Edwards. 2000. Extensive swelling after booster doses of acellular pertussis-tetanus-diphtheria vaccines. Pediatrics 105:e12. [DOI] [PubMed] [Google Scholar]
- 657.Reference deleted.
- 658.Rhea, L. J. 1915. The comparative pathology of the tracheal and bronchial lesions produced in man by B. pertussis (whooping-cough) and those produced in dogs by B. bronchisepticus (canine distemper). J. Med. Res. 32:471-474. [PMC free article] [PubMed] [Google Scholar]
- 659.Rhodes, C., M. Gray, J. Watson, T. Muratore, S. Kim, E. Hewlett, and C. Grisham. 2001. Structural Consequences of divalent metal binding by the adenylyl cyclase toxin of Bordetella pertussis. Arch. Biochem. Biophys. 395:169-176. [DOI] [PubMed] [Google Scholar]
- 660.Riboli, B., P. Pedroni, A. Cuzzoni, G. Grandi, and F. de Ferra. 1991. Expression of Bordetella pertussis fimbrial (fim) genes in Bordetella bronchiseptica: fimX is expressed at a low level and vir-regulated. Microb. Pathog. 10:393-403. [DOI] [PubMed] [Google Scholar]
- 661.Robbins, J. B. 1984. Towards a new vaccine for pertussis, p. 176-183. In L. Leive and D. Schlessinger (ed.), Microbiology—1984. American Society for Microbiology, Washington, D.C.
- 662.Robbins, J. B., M. Pittman, B. Trollfors, T. A. Lagergård, J. Taranger, and R. Schneerson. 1993. Primum non nocere: a pharmacologically inert pertussis toxoid alone should be the next pertussis vaccine. Pediatr. Infect. Dis. J. 12:795-807. [PubMed] [Google Scholar]
- 663.Roberts, M., I. Cropley, S. Chatfield, and G. Dougan. 1993. Protection of mice against respiratory Bordetella pertussis infection by intranasal immunization with P.69 and FHA. Vaccine 11:866-872. [DOI] [PubMed] [Google Scholar]
- 664.Roberts, M., N. F. Fairweather, E. Leininger, D. Pickard, E. L. Hewlett, A. Robinson, C. Hayward, G. Dougan, and I. G. Charles. 1991. Construction and characterization of Bordetella pertussis mutants lacking the vir-regulated P.69 outer membrane protein. Mol. Microbiol. 5:1393-1404. [DOI] [PubMed] [Google Scholar]
- 665.Robertson, P. W., H. Goldberg, B. H. Jarvie, D. D. Smith, and L. R. Whybin. 1987. Bordetella pertussis infection: a cause of persistent cough in adults. Med. J. Aust. 146:522-525. [DOI] [PubMed] [Google Scholar]
- 666.Robinson, A., L. A. Ashworth, and L. I. Irons. 1989. Serotyping Bordetella pertussis strains. Vaccine 7:491-494. [DOI] [PubMed] [Google Scholar]
- 667.Robinson, A., L. I. Irons, and L. A. Ashworth. 1985. Pertussis vaccine: present status and future prospects. Vaccine 3:11-22. [DOI] [PubMed] [Google Scholar]
- 668.Rogel, A., J. E. Schultz, R. M. Brownlie, J. G. Coote, R. Parton, and E. Hanski. 1989. Bordetella pertussis adenylate cyclase: purification and characterization of the toxic form of the enzyme. EMBO J. 8:2755-2760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 669.Romano, M. J., M. D. Weber, M. E. Weisse, and B. L. Siu. 2004. Pertussis pneumonia, hypoxemia, hyperleukocytosis, and pulmonary hypertension: improvement in oxygenation after a double volume exchange transfusion. Pediatrics 114:e264-e266. [DOI] [PubMed] [Google Scholar]
- 670.Romanus, V., R. Jonsell, and S. O. Bergquist. 1987. Pertussis in Sweden after the cessation of general immunization in 1979. Pediatr. Infect. Dis. J. 6:364-371. [DOI] [PubMed] [Google Scholar]
- 671.Roop, R. M., Jr., H. P. Veit, R. J. Sinsky, S. P. Veit, E. L. Hewlett, and E. T. Kornegay. 1987. Virulence factors of Bordetella bronchiseptica associated with the production of infectious atrophic rhinitis and pneumonia in experimentally infected neonatal swine. Infect. Immun. 55:217-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 672.Rose, T., P. Sebo, J. Ballalou, and D. Ladant. 1995. Interaction of calcium with Bordetella pertussis adenylate cyclase toxin. Characterization of multiple calcium-binding sites and calcium-induced conformational changes. J. Biol. Chem. 270:26370-26376. [DOI] [PubMed] [Google Scholar]
- 673.Rosenow, E. C. 1931. The relation of streptococci to the filterable virus of encephalitis of the fox. J. Infect. Dis. 48:304-334. [Google Scholar]
- 674.Rosenthal, R. S., W. Nogami, B. T. Cookson, W. E. Goldman, and W. J. Folkening. 1987. Major fragment of soluble peptidoglycan released from growing Bordetella pertussis is tracheal cytotoxin. Infect. Immun. 55:2117-2120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 675.Rosenthal, S., P. Strebel, P. Cassiday, G. Sanden, K. Brusuelas, and M. Wharton. 1995. Pertussis infection among adults during the 1993 outbreak in Chicago. J. Infect. Dis. 171:1650-1652. [DOI] [PubMed] [Google Scholar]
- 676.Rossi, C., J. Homan, C. Bauche, H. Hamdi, D. Ladant, and J. Chopineau. 2003. Differential mechanisms for calcium-dependent protein/membrane association as evidenced from SPr-Binding studies on supported biomimetic membranes. Biochemistry 42:15273-15283. [DOI] [PubMed] [Google Scholar]
- 677.Roy, C. R., and S. Falkow. 1991. Identification of Bordetella pertussis regulatory sequences required for transcriptional activation of the fhaB gene and autoregulation of the bvgAS operon. J. Bacteriol. 173:2385-2392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 678.Russell, F. M., J. M. Davis, M. J. Whipp, P. H. Janssen, P. B. Ward, J. R. Vyas, M. Starr, S. M. Sawyer, and N. Curtis. 2001. Severe Bordetella holmesii infection in a previously healthy adolescent confirmed by gene sequence analysis. Clin. Infect. Dis. 33:129-130. [DOI] [PubMed] [Google Scholar]
- 679.Ryan, M., L. Gothefors, J. Storsaeter, and K. H. Mills. 1997. Bordetella pertussis-specific Th1/Th2 cells generated following respiratory infection or immunization with an acellular vaccine: comparison of the T cell cytokine profiles in infants and mice. Dev. Biol. Stand. 89:297-305. [PubMed] [Google Scholar]
- 680.Ryan, M., G. Murphy, L. Gothefors, L. Nilsson, J. Storsaeter, and K. H. Mills. 1997. Bordetella pertussis respiratory infection in children is associated with preferential activation of type 1 T helper cells. J. Infect. Dis. 175:1246-1250. [DOI] [PubMed] [Google Scholar]
- 681.Ryan, M., G. Murphy, E. Ryan, L. Nilsson, F. Shackley, L. Gothefors, K. Øymar, E. Miller, J. Storsaeter, and K. H. Mills. 1998. Distinct T-cell subtypes induced with whole cell and acellular pertussis vaccines in children. Immunology 93:1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 682.Sako, W. 1947. Studies on pertussis immunization. J. Pediatr. 30:29-40. [DOI] [PubMed] [Google Scholar]
- 683.Sakurai, Y., H. Suzuki, and E. Terada. 1993. Purification and characterisation of haemagglutinin from Bordetella bronchiseptica. J. Med. Microbiol 39:388-392. [DOI] [PubMed] [Google Scholar]
- 684.Salmaso, S., P. Mastrantonio, A. E. Tozzi, P. Stefanelli, A. Anemona, M. L. Ciofi degli Atti, and A. Giammanco. 2001. Sustained efficacy during the first 6 years of life of 3-component acellular pertussis vaccines administered in infancy: the Italian experience. Pediatrics 108:E81. [DOI] [PubMed] [Google Scholar]
- 685.Salmaso, S., P. Mastrantonio, S. G. Wassilak, M. Giuliano, A. Anemona, A. Giammanco, A. E. Tozzi, M. L. Ciofi degli Atti, D. Greco, and the Stage II Working Group. 1998. Persistence of protection through 33 months of age provided by immunization in infancy with two three-component acellular pertussis vaccines. Vaccine 16:1270-1275. [DOI] [PubMed] [Google Scholar]
- 686.Sanyal, R. K. 1960. Histamine sensitivity in children after pertussis infection. Nature 185:537-538. [DOI] [PubMed] [Google Scholar]
- 687.Sato, H., and Y. Sato. 1985. Protective antigens of Bordetella pertussis mouse-protection test against intracerebral and aerosol challenge of B. pertussis. Dev. Biol. Stand. 61:461-467. [PubMed] [Google Scholar]
- 688.Sato, Y., M. Kimura, and H. Fukumi. 1984. Development of a pertussis component vaccine in Japan. Lancet i:122-126. [DOI] [PubMed] [Google Scholar]
- 689.Sauer, L. W., and L. Hambrecht. 1929. Experimental whooping cough. Am. J. Dis. Child. 37:732-744. [Google Scholar]
- 690.Saukkonen, K., C. Cabellos, M. Burroughs, S. Prasad, and E. Tuomanen. 1991. Integrin-mediated localization of Bordetella pertussis within macrophages: role in pulmonary colonization. J. Exp. Med. 173:1143-1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 691.Schaeffer, L. M., F. X. McCormack, H. Wu, and A. A. Weiss. 2004. Bordetella pertussis lipopolysaccharide resists the bactericidal effects of pulmonary surfactant protein A. J. Immunol. 173:1959-1965. [DOI] [PubMed] [Google Scholar]
- 692.Scheifele, D. W., S. A. Halperin, and A. C. Ferguson. 2001. Assessment of injection site reactions to an acellular pertussis-based combination vaccine, including novel use of skin tests with vaccine antigens. Vaccine 19:4720-4726. [DOI] [PubMed] [Google Scholar]
- 693.Schlapfer, G., J. D. Cherry, U. Heininger, M. Überall, S. Schmitt-Grohé, S. Laussucq, M. Just, and K. Stehr. 1995. Polymerase chain reaction identification of Bordetella pertussis infections in vaccinees and family members in a pertussis vaccine efficacy trial in Germany. Pediatr. Infect. Dis. J. 14:209-214. [DOI] [PubMed] [Google Scholar]
- 694.Schmidt-Schlapfer, G., J. G. Liese, F. Porter, S. Stojanov, M. Just, and B. H. Belohradsky. 1997. Polymerase chain reaction (PCR) compared with conventional identification in culture for detection of Bordetella pertussis in 7153 children. Clin. Microbiol. Infect. 3:462-467. [DOI] [PubMed] [Google Scholar]
- 695.Schmitt-Grohé, S., J. D. Cherry, U. Heininger, M. A. Überall, E. Pineda, and K. Stehr. 1995. Pertussis in German adults. Clin. Infect. Dis. 21:860-866. [DOI] [PubMed] [Google Scholar]
- 696.Schmitt, H. J., K. Beutel, A. Schuind, M. Knuf, S. Wagner, S. Muschenborn, H. Bogaerts, H. L. Bock, and R. Clemens. 1997. Reactogenicity and immunogenicity of a booster dose of a combined diphtheria, tetanus, and tricomponent acellular pertussis vaccine at fourteen to twenty-eight months of age. J. Pediatr. 130:616-623. [DOI] [PubMed] [Google Scholar]
- 697.Schmitt, H. J., C. H. Wirsing von König, A. Neiss, H. Bogaerts, H. L. Bock, H. Schulte-Wissermann, M. Gahr, R. Schult, J. U. Folkens, W. Rauh, and R. Clemens. 1996. Efficacy of acellular pertussis vaccine in early childhood after household exposure. JAMA 275:37-41. [PubMed] [Google Scholar]
- 698.Seibold, H. R., E. A. Perrin, Jr., and A. C. Garner. 1970. Pneumonia associated with Bordetella bronchiseptica in Callicebus species primates. Lab. Anim. Care 20:456-461. [PubMed] [Google Scholar]
- 699.Sekiya, K. 1983. Effects of Bordetella pertussis components on IgE and IgG1 responses. Microbiol. Immunol. 27:905-915. [DOI] [PubMed] [Google Scholar]
- 700.Sekura, R. D., F. Fish, C. R. Manclark, B. Meade, and Y. L. Zhang. 1983. Pertussis toxin. Affinity purification of a new ADP-ribosyltransferase. J. Biol. Chem. 258:14647-14651. [PubMed] [Google Scholar]
- 701.Sen, D. K., S. Arora, S. Gupta, and R. K. Sanyal. 1974. Studies of adrenergic mechanisms in relation to histamine sensitivity in children immunized with Bordetella pertussis vaccine. J. Allergy Clin. Immunol. 54:25-31. [DOI] [PubMed] [Google Scholar]
- 702.Senzilet, L. D., S. A. Halperin, J. S. Spika, M. Alagaratnam, A. Morris, and B. Smith. 2001. Pertussis is a frequent cause of prolonged cough illness in adults and adolescents. Clin. Infect. Dis. 32:1691-1697. [DOI] [PubMed] [Google Scholar]
- 703.Seufferlein, T., and E. Rozengurt. 1994. Lysophosphatidic acid stimulates tyrosine phosphorylation of focal adhesion kinase, paxillin, and p130. Signaling pathways and cross-talk with platelet-derived growth factor. J. Biol. Chem. 269:9345-9351. [PubMed] [Google Scholar]
- 704.Seufferlein, T., and E. Rozengurt. 1994. Sphingosine induces p125FAK and paxillin tyrosine phosphorylation, actin stress fiber formation, and focal contact assembly in Swiss 3T3 cells. J. Biol. Chem. 269:27610-27617. [PubMed] [Google Scholar]
- 705.Seufferlein, T., and E. Rozengurt. 1995. Sphingosylphosphorylcholine rapidly induces tyrosine phosphorylation of p125FAK and paxillin, rearrangement of the actin cytoskeleton and focal contact assembly. Requirement of p21rho in the signaling pathway. J. Biol. Chem. 270:24343-24351. [DOI] [PubMed] [Google Scholar]
- 706.Shields, W. D., C. Nielsen, D. Buch, V. Jacobsen, P. Christenson, B. Zachau-Christiansen, and J. D. Cherry. 1988. Relationship of pertussis immunization to the onset of neurologic disorders: a retrospective epidemiologic study. J. Pediatr. 113:801-805. [DOI] [PubMed] [Google Scholar]
- 707.Simondon, F., I. Iteman, M. P. Preziosi, A. Yam, and N. Guiso. 1998. Evaluation of an immunoglobulin G enzyme-linked immunosorbent assay for pertussis toxin and filamentous hemagglutinin in diagnosis of pertussis in Senegal. Clin. Diagn. Lab. Immunol. 5:130-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 708.Simondon, F., M. P. Preziosi, A. Yam, C. T. Kane, L. Chabirand, I. Iteman, G. Sanden, S. Mboup, A. Hoffenbach, K. Knudsen, N. Guiso, S. Wassilak, and M. Cadoz. 1997. A randomized double-blind trial comparing a two-component acellular to a whole-cell pertussis vaccine in Senegal. Vaccine 15:1606-1612. [DOI] [PubMed] [Google Scholar]
- 709.Skinner, J. A., A. Reissinger, H. Shen, and M. H. Yuk. 2004. Bordetella type III secretion and adenylate cyclase toxin synergize to drive dendritic cells into a semimature state. J. Immunol. 173:1934-1940. [DOI] [PubMed] [Google Scholar]
- 710.Skowronski, D. M., G. De Serres, D. MacDonald, W. Wu, C. Shaw, J. Macnabb, S. Champagne, D. M. Patrick, and S. A. Halperin. 2002. The changing age and seasonal profile of pertussis in Canada. J. Infect. Dis. 185:1448-1453. [DOI] [PubMed] [Google Scholar]
- 711.Skowronski, D. M., V. P. Remple, J. Macnabb, K. Pielak, D. M. Patrick, S. A. Halperin, and D. Scheifele. 2003. Injection-site reactions to booster doses of acellular pertussis vaccine: rate, severity, and anticipated impact. Pediatrics 112:e453. [DOI] [PubMed] [Google Scholar]
- 712.Smith, C., and H. Vyas. 2000. Early infantile pertussis; increasingly prevalent and potentially fatal. Eur. J. Pediatr. 159:898-900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 713.Smith, T. 1913. Some bacteriological and environmental factors in the pneumonias of lower animals with special reference to the guinea-pig. J. Med. Res. 29:291-323. [PMC free article] [PubMed] [Google Scholar]
- 714.Snell, J. J. S. 1973. The distribution and identification of non-fermenting bacteria. Public Health Lab. Serv. Monograph Ser. 4:1-45. [Google Scholar]
- 715.Snyder, S. B., S. K. Fisk, J. G. Fox, and O. A. Soave. 1973. Respiratory tract disease associated with Bordetella bronchiseptica infection in cats. J. Am. Vet. Med. Assoc. 163:293-294. [PubMed] [Google Scholar]
- 716.Solberg, L. 1985. DPT immunization, visit to child health center and sudden infant death syndrome (SIDS). Oslo Health Council, Oslo, Norway.
- 717.Spangrude, G. J., F. Sacchi, H. R. Hill, D. E. Van Epps, and R. A. Daynes. 1985. Inhibition of lymphocyte and neutrophil chemotaxis by pertussis toxin. J. Immunol. 135:4135-4143. [PubMed] [Google Scholar]
- 718.Spears, P. A., L. M. Temple, D. M. Miyamoto, D. J. Maskell, and P. E. Orndorff. 2003. Unexpected similarities between Bordetella avium and other pathogenic Bordetellae. Infect. Immun. 71:2591-2597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 719.Stehr, K., J. D. Cherry, U. Heininger, S. Schmitt-Grohé, M. Überall, S. Laussucq, T. Eckhardt, M. Meyer, R. Engelhardt, and P. Christenson. 1998. A comparative efficacy trial in Germany in infants who received either the Lederle/Takeda acellular pertussis component DTP (DTaP) vaccine, the Lederle whole-cell component DTP vaccine, or DT vaccine. Pediatrics 101:1-11. [DOI] [PubMed] [Google Scholar]
- 720.Steinman, L., A. Weiss, N. Adelman, M. Lim, J. Oehlert, R. Zuniga, E. Hewlett, and S. Falkow. 1985. Murine model for pertussis vaccine encephalopathy: role of the major histocompatibility complex; antibody to albumin and to Bordetella pertussis and pertussis toxin. Dev. Biol. Stand. 61:439-446. [PubMed] [Google Scholar]
- 721.Steinman, L., A. Weiss, N. Adelman, M. Lim, R. Zuniga, J. Oehlert, E. Hewlett, and S. Falkow. 1985. Pertussis toxin is required for pertussis vaccine encephalopathy. Proc. Natl. Acad. Sci. USA 82:8733-8736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 722.Steketee, R. W., D. G. Burstyn, S. G. Wassilak, W. N. Adkins, Jr., M. B. Polyak, J. P. Davis, and C. R. Manclark. 1988. A comparison of laboratory and clinical methods for diagnosing pertussis in an outbreak in a facility for the developmentally disabled. J. Infect. Dis. 157:441-449. [DOI] [PubMed] [Google Scholar]
- 723.Stephenson, J. B. 1988. A neurologist looks at neurological disease temporally related to DTP immunization. Tokai J. Exp. Clin. Med. 13(Suppl):157-164. [PubMed] [Google Scholar]
- 724.Stetler, H. C., W. A. Orenstein, K. J. Bart, E. W. Brink, J. P. Brennan, and A. R. Hinman. 1985. History of convulsions and use of pertussis vaccine. J. Pediatr. 107:175-179. [DOI] [PubMed] [Google Scholar]
- 725.Stewart, G. J. 1979. Toxicity of pertussis vaccine: frequency and probability of reactions. J. Epidemiol. Commun. Health 33:150-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 726.Stewart, G. J. 1983. Whooping cough and pertussis vaccine. Br. Med. J. (Clin. Res. Ed.) 287:1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 727.Stewart, G. T. 1979. Infection and immunization. Scott. Med. J. 24:47-52. [DOI] [PubMed] [Google Scholar]
- 728.Stewart, G. T. 1979. Pertussis vaccine: the United Kingdom's experience, p. 262-278. International Symposiuom on Pertussis. National Institutes of Health, Bethesda, Md.
- 729.Stewart, G. T. 1977. Vaccination against whooping-cough. Efficacy versus risks. Lancet i:234-237. [DOI] [PubMed] [Google Scholar]
- 730.Stibitz, S., and M. S. Yang. 1991. Subcellular localization and immunological detection of proteins encoded by the vir locus of Bordetella pertussis. J. Bacteriol. 173:4288-4296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 731.Stockbauer, K. E., A. K. Foreman-Wykert, and J. F. Miller. 2003. Bordetella type III secretion induces caspase 1-independent necrosis. Cell. Microbiol. 5:123-132. [DOI] [PubMed] [Google Scholar]
- 732.Stockbauer, K. E., B. Fuchslocher, J. F. Miller, and P. A. Cotter. 2001. Identification and characterization of BipA, a Bordetella Bvg− intermediate phase protein. Mol. Microbiol. 39:65-78. [DOI] [PubMed] [Google Scholar]
- 733.Stoll, D. B., S. A. Murphey, and S. K. Ballas. 1981. Bordetella bronchiseptica infection in stage IV Hodgkin's disease. Postgrad. Med. J. 57:723-724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 734.Storsaeter, J., W. C. Blackwelder, and H. O. Hallander. 1992. Pertussis antibodies, protection, and vaccine efficacy after household exposure. Am. J. Dis. Child. 146:167-172. [DOI] [PubMed] [Google Scholar]
- 735.Storsaeter, J., H. Hallander, C. P. Farrington, P. Olin, R. Mollby, and E. Miller. 1990. Secondary analyses of the efficacy of two acellular pertussis vaccines evaluated in a Swedish phase III trial. Vaccine 8:457-461. [DOI] [PubMed] [Google Scholar]
- 736.Storsaeter, J., H. O. Hallander, L. Gustafsson, and P. Olin. 1998. Levels of anti-pertussis antibodies related to protection after household exposure to Bordetella pertussis. Vaccine 16:1907-1916. [DOI] [PubMed] [Google Scholar]
- 737.Storsaeter, J., and P. Olin. 1992. Relative efficacy of two acellular pertussis vaccines during three years of passive surveillance. Vaccine 10:142-144. [DOI] [PubMed] [Google Scholar]
- 738.Storsaeter, J., P. Olin, B. Renemar, T. Lagergård, R. Norberg, V. Romanus, and M. Tiru. 1988. Mortality and morbidity from invasive bacterial infections during a clinical trial of accllular pertussis vaccines in Sweden. Pediatr. Infect. Dis. J. 7:637-645. [DOI] [PubMed] [Google Scholar]
- 739.Strebel, P., J. Nordin, K. Edwards, J. Hunt, J. Besser, S. Burns, G. Amundson, A. Baughman, and W. Wattigney. 2001. Population-based incidence of pertussis among adolescents and adults, Minnesota, 1995-1996. J. Infect. Dis. 183:1353-1359. [DOI] [PubMed] [Google Scholar]
- 740.Strebel, P. M., S. L. Cochi, K. M. Farizo, B. J. Payne, S. D. Hanauer, and A. L. Baughman. 1993. Pertussis in Missouri: evaluation of nasopharyngeal culture, direct fluorescent antibody testing, and clinical case definitions in the diagnosis of pertussis. Clin. Infect. Dis. 16:276-285. [DOI] [PubMed] [Google Scholar]
- 741.Ström, J. 1967. Further experience of reactions, especially of a cerebral nature, in conjunction with triple vaccination: a study based on vaccinations in Sweden 1959-65. Br. Med. J. 4:320-323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 742.Ström, J. 1960. Is universal vaccination against pertussis always justified? Br. Med. J. 2:1184. [PMC free article] [PubMed] [Google Scholar]
- 743.Stronk, M. G., and M. Pittman. 1955. The influence of pertussis vaccine on histamine sensitivity of rabbits and guinea pigs and on the blood sugar in rabbits and mice. J. Infect. Dis. 96:152-161. [DOI] [PubMed] [Google Scholar]
- 744.Stuart-Harris, C. H. 1979. Experiences of pertussis in the United Kingdom, p. 256-261, International Symposium on Pertussis. National Institutes of Health, Bethesda, Md.
- 745.Suko, M., T. Ogita, H. Okudaira, and Y. Horiuchi. 1977. Preferential enhancement of IgE antibody formation by Bordetella pertussis. Int. Arch. Allergy Appl. Immunol. 54:329-337. [DOI] [PubMed] [Google Scholar]
- 746.Suzuki, I., Y. Kumazawa, T. Miyazaki, and K. Mizunoe. 1978. Modulation of the antibody response to sheep erythrocytes in murine spleen cell cultures by a T cell mitogen extracted from Bordetella pertussis. Microbiol. Immunol. 22:47-51. [DOI] [PubMed] [Google Scholar]
- 747.Switzer, W. P., C. J. Maré, and E. D. Hubbard. 1966. Incidence of Bordetella bronchiseptica in wildlife and man in Iowa. Am. J. Vet. Res. 27:1134-1136. [PubMed] [Google Scholar]
- 748.Tamion, F., C. Girault, V. Chevron, M. Pestel, and G. Bonmarchand. 1996. Bordetella bronchoseptica pneumonia with shock in an immunocompetent patient. Scand. J. Infect. Dis. 28:197-198. [DOI] [PubMed] [Google Scholar]
- 749.Tamura, M., K. Nogimori, S. Murai, M. Yajima, K. Ito, T. Katada, M. Ui, and S. Ishii. 1982. Subunit structure of islet-activating protein, pertussis toxin, in conformity with the A-B model. Biochemistry 21:5516-5522. [DOI] [PubMed] [Google Scholar]
- 750.Tamura, M., K. Nogimori, M. Yajima, K. Ase, and M. Ui. 1983. A role of the B-oligomer moiety of islet-activating protein, pertussis toxin, in development of the biological effects on intact cells. J. Biol. Chem. 258:6756-6761. [PubMed] [Google Scholar]
- 751.Tanaka, M., C. R. Vitek, F. B. Pascual, K. M. Bisgard, J. E. Tate, and T. V. Murphy. 2003. Trends in pertussis among infants in the United States, 1980-1999. JAMA 290:2968-2975. [DOI] [PubMed] [Google Scholar]
- 752.Tang, Y. W., M. K. Hopkins, C. P. Kolbert, P. A. Hartley, P. J. Severance, and D. H. Persing. 1998. Bordetella holmesii-like organisms associated with septicemia, endocarditis, and respiratory failure. Clin. Infect. Dis. 26:389-392. [DOI] [PubMed] [Google Scholar]
- 753.Taranger, J., B. Trollfors, T. Lagergård, and G. Zackrisson. 1994. Parapertussis infection followed by pertussis infection. Lancet 334:1703. [DOI] [PubMed] [Google Scholar]
- 754.Taranger, J., B. Trollfors, L. Lind, G. Zackrisson, and K. Beling- Holmquist. 1994. Environmental contamination leading to false-positive polymerase chain reaction for pertussis. Pediatr. Infect. Dis. J. 13:936-937. (Letter.) [DOI] [PubMed] [Google Scholar]
- 755.Taylor, E. M., and J. L. Emery. 1982. Immunisation and cot deaths. Lancet ii:721. [DOI] [PubMed] [Google Scholar]
- 756.Templeton, K. E., S. A. Scheltinga, A. van der Zee, B. M. Diederen, A. M. van Kruijssen, H. Goossens, E. Kuijper, and E. C. Claas. 2003. Evaluation of real-time PCR for detection of and discrimination between Bordetella pertussis, Bordetella parapertussis, and Bordetella holmesii for clinical diagnosis. J. Clin. Microbiol. 41:4121-4126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 757.Thomas, M. G., L. A. Ashworth, E. Miller, and H. P. Lambert. 1989. Serum IgG, IgA, and IgM responses to pertussis toxin, filamentous hemagglutinin, and agglutinogens 2 and 3 after infection with Bordetella pertussis and immunization with whole-cell pertussis vaccine. J. Infect. Dis. 160:838-845. [DOI] [PubMed] [Google Scholar]
- 758.Thomas, M. G., K. Redhead, and H. P. Lambert. 1989. Human serum antibody responses to Bordetella pertussis infection and pertussis vaccination. J. Infect. Dis. 159:211-218. [DOI] [PubMed] [Google Scholar]
- 759.Thomas, P. F., P. B. McIntyre, and B. B. Jalaludin. 2000. Survey of pertussis morbidity in adults in western Sydney. Med. J. Aust. 173:74-76. [DOI] [PubMed] [Google Scholar]
- 759a.Thomson Healthcare. 2004. Daptacel, p. 786-792. In Physicians' desk reference, 58th ed. Thomson Healthcare, Montrale, N.J.
- 759b.Thomson Healthcare. 2004. Infanrix, p. 1532-1537. In Physicians' desk reference, 58th ed. Thomson Healthcare, Montrale, N.J.
- 760.Torch, W. 1982. Diphtheria-pertussis-tetanus (DTP) immunization: a potential cause of the sudden infant death syndrome (SIDS). Neurology 32:A169. [Google Scholar]
- 761.Torrey, J. C., and A. H. Rahe. 1912. Studies in canine distemper. J. Med. Res. 27:291-364. [PMC free article] [PubMed] [Google Scholar]
- 762.Tosi, M. F., J. M. Stark, C. W. Smith, A. Hamedani, D. C. Gruenert, and M. D. Infeld. 1992. Induction of ICAM-1 expression on human airway epithelial cells by inflammatory cytokines: effects on neutrophil-epithelial cell adhesion. Am. J. Respir. Cell Mol. Biol. 7:214-221. [DOI] [PubMed] [Google Scholar]
- 763.Toyota, T., Y. Kai, M. Kakizaki, A. Sakai, Y. Goto, M. Yajima, and M. Ui. 1980. Effects of islet-activating protein (IAP) on blood glucose and plasma insulin in healthy volunteers (phase 1 studies). Tohoku J. Exp. Med. 130:105-116. [DOI] [PubMed] [Google Scholar]
- 764.Tozzi, A. E., A. Anemona, P. Stefanelli, S. Salmaso, M. L. Atti, P. Mastrantonio, and A. Giammanco. 2001. Reactogenicity and immunogenicity at preschool age of a booster dose of two three-component diphtheria-tetanus-acellular pertussis vaccines in children primed in infancy with acellular vaccines. Pediatrics 107:E25. [DOI] [PubMed] [Google Scholar]
- 765.Trahan, C. J., E. H. Stephenson, J. W. Ezzell, and W. C. Mitchell. 1987. Airborne-induced experimental Bordetella bronchiseptica pneumonia in strain 13 guinea pigs. Lab. Anim. 21:226-232. [DOI] [PubMed] [Google Scholar]
- 766.Tran Minh, N. N., Q. He, K. Edelman, R. M. Olander, M. K. Viljanen, H. Arvilommi, and J. Mertsola. 1999. Cell-mediated immune responses to antigens of Bordetella pertussis and protection against pertussis in school children. Pediatr. Infect. Dis. J. 18:366-370. [DOI] [PubMed] [Google Scholar]
- 767.Trollfors, B., T. Lagergård, J. Taranger, E. Bergfors, R. Schneerson, and J. B. Robbins. 2001. Serum immunoglobulin G antibody responses to Bordetella pertussis lipooligosaccharide and B. parapertussis lipopolysaccharide in children with pertussis and parapertussis. Clin. Diagn. Lab. Immunol. 8:1015-1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 768.Trollfors, B., J. Taranger, T. Lagergård, L. Lind, V. Sundh, G. Zackrisson, C. U. Lowe, W. Blackwelder, and J. B. Robbins. 1995. A placebo-controlled trial of a pertussis-toxoid vaccine. N. Engl. J. Med. 333:1045-1050. [DOI] [PubMed] [Google Scholar]
- 769.Tuomanen, E. 1988. Bordetella pertussis adhesins, p. 75-94. In A. C. Wardlaw and R. Parton (ed.), Pathogenesis and immunity in pertussis. John Wiley & Sons, Inc., New York, NY.
- 770.Tuomanen, E., J. Nedelman, J. O. Hendley, and E. Hewlett. 1983. Species specificity of Bordetella adherence to human animal ciliated respiratory epithelial cells. Infect. Immun. 42:692-695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 771.Tuomanen, E., and A. Weiss. 1985. Characterization of two adhesins of Bordetella pertussis for human ciliated respiratory-epithelial cells. J. Infect. Dis. 152:118-125. [DOI] [PubMed] [Google Scholar]
- 772.Überall, M. A., K. Stehr, J. D. Cherry, U. Heininger, S. Schmitt-Grohé, S. Laussucq, T. Eckhardt, and The Pertussis Vaccine Study Group. 1997. Severe adverse events in a comparative efficacy trial in Germany in infants receiving either the Lederle/Takeda acellular pertussis component DTP (DTaP) vaccine, the Lederle whole-cell component DTP (DTP) or DT vaccine. Dev. Biol. Stand. 89:83-89. [PubMed] [Google Scholar]
- 773.Uhl, M. A., and J. F. Miller. 1994. Autophosphorylation and phosphotransfer in the Bordetella pertussis BvgAS signal transduction cascade. Proc. Natl. Acad. Sci. USA 91:1163-1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 774.Uhl, M. A., and J. F. Miller. 1996. Central role of the BvgS receiver as a phosphorylated intermediate in a complex two-component phosphorelay. J. Biol. Chem. 271:33176-33180. [DOI] [PubMed] [Google Scholar]
- 775.Uhl, M. A., and J. F. Miller. 1996. Integration of multiple domains in a two-component sensor protein: the Bordetella pertussis BvgAS phosphorelay. EMBO J. 15:1028-1036. [PMC free article] [PubMed] [Google Scholar]
- 776.Ui, J. 1990. Pertussis toxin as a valuable probe for G-protein involvement in signal transduction, p. 45-77. In J. Moss and M. Vaughan (ed.), ADP-ribosylating toxins and G-proteins: insights into signal transduction. American Society for Microbiology, Washington, D.C. [DOI] [PubMed]
- 777.Vandamme, P., M. Heyndrickx, M. Vancanneyt, B. Hoste, P. De Vos, E. Falsen, K. Kersters, and K. H. Hinz. 1996. Bordetella trematum sp. nov., isolated from wounds and ear infections in humans, and reassessment of Alcaligenes denitrificans Ruger and Tan 1983. Int. J. Syst. Bacteriol. 46:849-858. [DOI] [PubMed] [Google Scholar]
- 778.Vandebriel, R. J., S. M. Hellwig, J. P. Vermeulen, J. H. Hoekman, J. A. Dormans, P. J. Roholl, and F. R. Mooi. 2003. Association of Bordetella pertussis with host immune cells in the mouse lung. Microb. Pathog. 35:19-29. [DOI] [PubMed] [Google Scholar]
- 779.van den Akker, W. M. 1997. Bordetella bronchiseptica has a BvgAS-controlled cytotoxic effect upon interaction with epithelial cells. FEMS Microbiol. Lett. 156:239-244. [DOI] [PubMed] [Google Scholar]
- 780.van den Akker, W. M. 1998. Lipopolysaccharide expression within the genus Bordetella: influence of temperature and phase variation. Microbiology 144:1527-1535. [DOI] [PubMed] [Google Scholar]
- 781.van der Zee, A., C. Agterberg, M. Peeters, F. Mooi, and J. Schellekens. 1996. A clinical validation of Bordetella pertussis and Bordetella parapertussis polymerase chain reaction comparison with culture and serology using samples from patients with suspected whooping cough from a highly immunized population. J. Infect. Dis. 174:89-96. [DOI] [PubMed] [Google Scholar]
- 782.van der Zee, A., H. Groenendijk, M. Peeters, and F. R. Mooi. 1996. The differentiation of Bordetella parapertussis and Bordetella bronchiseptica from humans and animals as determined by DNA polymorphism mediated by two different insertion sequence elements suggests their phylogenetic relationship. Int. J. Syst. Bacteriol. 46:640-647. [DOI] [PubMed] [Google Scholar]
- 783.van der Zee, A., F. Mooi, J. Van Embden, and J. Musser. 1997. Molecular evolution and host adaptation of Bordetella spp. phylogenetic analysis using multilocus enzyme electrophoresis and typing with three insertion sequences. J. Bacteriol. 179:6609-6617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 784.Van Rie, A., and H. W. Hethcote. 2004. Adolescent and adult pertussis vaccination: computer simulations of five new strategies. Vaccine 22:3154-3165. [DOI] [PubMed] [Google Scholar]
- 785.Verghese, M. W., C. D. Smith, and R. Snyderman. 1985. Potential role for a guanine nucleotide regulatory protein in chemoattractant receptor mediated polyphosphoinositide metabolism, Ca++ mobilization and cellular responses by leukocytes. Biochem. Biophys. Res. Commun. 127:450-457. [DOI] [PubMed] [Google Scholar]
- 786.Viejo, G., P. de la Iglesia, L. Otero, M. I. Blanco, B. Gomez, D. De Miguel, A. Del Valle, and B. De la Fuente. 2002. Bordetella bronchiseptica pleural infection in a patient with AIDS. Scand. J. Infect. Dis. 34:628-629. [DOI] [PubMed] [Google Scholar]
- 787.Vielemeyer, O., J. Y. Crouch, S. C. Edberg, and J. G. Howe. 2004. Identification of Bordetella pertussis in a critically ill human immunodeficiency virus-infected patient by direct genotypical analysis of Gram-stained material and discrimination from B. holmesii by using a unique recA gene restriction enzyme site. J. Clin. Microbiol. 42:847-849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 788.Vincent, J. M., J. D. Cherry, W. F. Nauschuetz, A. Lipton, C. M. Ono, C. N. Costello, L. K. Sakaguchi, G. Hsue, L. A. Jackson, R. Tachdjian, P. A. Cotter, and J. A. Gornbein. 2000. Prolonged afebrile nonproductive cough illnesses in American soldiers in Korea: a serological search for causation. Clin. Infect. Dis. 30:534-539. [DOI] [PubMed] [Google Scholar]
- 789.Viprey, V., A. Del Greco, W. Golinowski, W. J. Broughton, and X. Perret. 1998. Symbiotic implications of type III protein secretion machinery in Rhizobium. Mol. Microbiol. 28:1381-1389. [DOI] [PubMed] [Google Scholar]
- 790.Vitek, C. R., F. B. Pascual, A. L. Baughman, and T. V. Murphy. 2003. Increase in deaths from pertussis among young infants in the United States in the 1990s. Pediatr. Infect. Dis. J. 22:628-634. [DOI] [PubMed] [Google Scholar]
- 791.von Wintzingerode, F., G. Gerlach, B. Schneider, and R. Gross. 2002. Phylogenetic relationships and virulence evolution in the genus Bordetella. Curr. Top. Microbiol. Immunol. 264:177-199. [PubMed] [Google Scholar]
- 792.von Wintzingerode, F., A. Schattke, R. A. Siddiqui, U. Rosick, U. B. Gobel, and R. Gross. 2001. Bordetella petrii sp. nov., isolated from an anaerobic bioreactor, and emended description of the genus Bordetella. Int. J. Syst. Evol. Microbiol. 51:1257-1265. [DOI] [PubMed] [Google Scholar]
- 793.Vysok' a-Burianov'a, B. 1963. Contemporary problems in the epidemiology of whooping cough. J. Hyg. Epidemiol. Microbiol. Immunol. 33:472-481. [PubMed] [Google Scholar]
- 794.Wagener, J. S., R. Sobonya, L. Minnich, and L. M. Taussig. 1984. Role of canine parainfluenza virus and Bordetella bronchiseptica in kennel cough. Am. J. Vet. Res. 45:1862-1866. [PubMed] [Google Scholar]
- 795.Walker, A. M., H. Jick, D. R. Perera, T. A. Knauss, and R. S. Thompson. 1988. Neurologic events following diphtheria-tetanus-pertussis immunization. Pediatrics 81:345-349. [PubMed] [Google Scholar]
- 796.Walker, A. M., H. Jick, D. R. Perera, R. S. Thompson, and T. A. Knauss. 1987. Diphtheria-tetanus-pertussis immunization and sudden infant death syndrome. Am. J. Public Health 77:945-951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 797.Wallet, F., T. Perez, S. Armand, B. Wallaert, and R. J. Courcol. 2002. Pneumonia due to Bordetella bronchiseptica in a cystic fibrosis patient: 16S rRNA sequencing for diagnosis confirmation. J. Clin. Microbiol. 40:2300-2301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 798.Reference deleted.
- 799.Ward, J. E., Jr., E. M. Dale, E. W. Nester, and A. N. Binns. 1990. Identification of a VirB10 protein aggregate in the inner membrane of Agrobacterium tumefaciens. J. Bacteriol. 172:5200-5210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 800.Ward, J., and APERT Study Group. 2001. Pertussis epidemiology and acellular pertussis vaccine efficacy in older children: NIH APERT Multicenter Pertussis Trial. Ped. Res. 49:240A. [Google Scholar]
- 801.Wardlaw, A. C., and R. Parton. 1982. Bordetella pertussis toxins. Pharmacol. Ther. 19:1-53. [DOI] [PubMed] [Google Scholar]
- 802.Wardlaw, A. C., and R. Parton. 1988. Pathogenesis and immunity in pertussis. John Wiley & Sons, Inc., New York, N.Y.
- 803.Wardlaw, A. C., and R. Parton. 1983. Pertussis vaccine, vol. 2. Academic Press, Inc., New York, N.Y.
- 804.Wardlaw, A. C., R. Parton, R. K. Bergman, and J. J. Munoz. 1979. Loss of adjuvanticity in rats for the hyperacute form of allergic encephalomyelitis and for reaginic antibody production in mice of a phenotypic variant of Bordetella pertussis. Immunology 37:539-545. [PMC free article] [PubMed] [Google Scholar]
- 805.Watanabe, M., and M. Nagai. 2003. Role of systemic and mucosal immune responses in reciprocal protection against Bordetella pertussis and Bordetella parapertussis in a murine model of respiratory infection. Infect. Immun. 71:733-738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 806.Watanabe, M., H. Takimoto, Y. Kumazawa, and K. Amano. 1990. Biological properties of lipopolysaccharides from Bordetella species. J. Gen. Microbiol. 136:489-493. [DOI] [PubMed] [Google Scholar]
- 807.Weihl, C., H. D. Riley, and J. H. Lapin. 1963. Extracted pertussis antigen. A clinical appraisal. Am. J. Dis. Child. 106:210-215. [DOI] [PubMed] [Google Scholar]
- 808.Weingart, C. L., P. S. Mobberley-Schuman, E. L. Hewlett, M. C. Gray, and A. A. Weiss. 2000. Neutralizing antibodies to adenylate cyclase toxin promote phagocytosis of Bordetella pertussis by human neutrophils. Infect. Immun. 68:7152-7155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 809.Weingart, C. L., and A. A. Weiss. 2000. Bordetella pertussis virulence factors affect phagocytosis by human neutrophils. Infect. Immun. 68:1735-1739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 810.Weiss, A. A., and M. S. Goodwin. 1989. Lethal infection by Bordetella pertussis mutants in the infant mouse model. Infect. Immun. 57:3757-3764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 811.Weiss, A. A., and E. L. Hewlett. 1986. Virulence factors of Bordetella pertussis. Annu. Rev. Microbiol. 40:661-686. [DOI] [PubMed] [Google Scholar]
- 812.Weiss, A. A., F. D. Johnson, and D. L. Burns. 1993. Molecular characterization of an operon required for pertussis toxin secretion. Proc. Natl. Acad. Sci. USA 90:2970-2974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 813.Welch, R. A. 1991. Pore-forming cytolysins of gram-negative bacteria. Mol. Microbiol. 5:521-528. [DOI] [PubMed] [Google Scholar]
- 814.Weyant, R. S., D. G. Hollis, R. E. Weaver, M. F. Amin, A. G. Steigerwalt, S. P. O'Connor, A. M. Whitney, M. I. Daneshvar, C. W. Moss, and D. J. Brenner. 1995. Bordetella holmesii sp. nov. a new gram-negative species associated with septicemia. J. Clin. Microbiol. 33:1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 815.Wharton, M., and C. R. Vitek. 2004. Diphtheria toxoid, p. 211-228. In S. A. Plotkin and W. A. Orenstein (ed.), Vaccines, 4th ed. The W. B. Saunders Co., Philadelphia, Pa.
- 816.Wiertz, E. J., H. G. Loggen, H. C. Walvoort, and J. G. Kreeftenberg. 1989. In vitro induction of antigen specific antibody synthesis and proliferation of T lymphocytes with acellular pertussis vaccines, pertussis toxin and filamentous haemagglutinin in humans. J. Biol. Stand. 17:181-190. [DOI] [PubMed] [Google Scholar]
- 817.Willems, R., A. Paul, H. G. van der Heide, A. R. ter Avest, and F. R. Mooi. 1990. Fimbrial phase variation in Bordetella pertussis: a novel mechanism for transcriptional regulation. EMBO J. 9:2803-2809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 818.Willems, R. J., C. Geuijen, H. G. van der Heide, G. Renauld, P. Bertin, W. M. van den Akker, C. Locht, and F. R. Mooi. 1994. Mutational analysis of the Bordetella pertussis fim/fha gene cluster: identification of a gene with sequence similarities to haemolysin accessory genes involved in export of FHA. Mol. Microbiol. 11:337-347. [DOI] [PubMed] [Google Scholar]
- 819.Willems, R. J., H. G. van der Heide, and F. R. Mooi. 1992. Characterization of a Bordetella pertussis fimbrial gene cluster which is located directly downstream of the filamentous haemagglutinin gene. Mol. Microbiol. 6:2661-2671. [DOI] [PubMed] [Google Scholar]
- 820.Wilson, R., R. Read, M. Thomas, A. Rutman, K. Harrison, V. Lund, B. Cookson, W. Goldman, H. Lambert, and P. Cole. 1991. Effects of Bordetella pertussis infection on human respiratory epithelium in vivo and in vitro. Infect. Immun. 59:337-345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 821.Winsnes, R., T. Lonnes, B. Mogster, and B. P. Berdal. 1985. Antibody responses after vaccination and disease against leukocytosis promoting factor, filamentous hemagglutinin, lipopolysaccharide and a protein binding to complement-fixing antibodies induced during whooping cough. Dev. Biol. Stand. 61:353-365. [PubMed] [Google Scholar]
- 822.Winsser, J. 1960. A study of Bordetella bronchiseptica. Proc. Anim. Care Panel 10:87-104. [Google Scholar]
- 823.Winters, A. L., D. W. Baggett, W. R. Benjamin, H. K. Brown, and T. W. Klein. 1985. Resistance to adenovirus infection after administration of Bordetella pertussis vaccine in mice. Infect. Immun. 47:587-591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 824.Winters, J. L., W. N. O'Connor, R. A. Broughton, and J. A. Noonan. 1992. Bordetella bronchiseptica pneumonia in a patient with Down syndrome: a case report and review. Pediatrics 89:1262-1265. [PubMed] [Google Scholar]
- 825.Wirsing von König, C. H., and H. Finger. 1994. Role of pertussis toxin in causing symptoms of Bordetella parapertussis infection. Eur. J. Clin. Microbiol. Infect. Dis. 13:455-458. [DOI] [PubMed] [Google Scholar]
- 826.Wirsing von König, C. H., D. Gounis, S. Laukamp, H. Bogaerts, and H. J. Schmitt. 1999. Evaluation of a single-sample serological technique for diagnosing pertussis in unvaccinated children. Eur. J. Clin. Microbiol. Infect. Dis. 18:341-345. [DOI] [PubMed] [Google Scholar]
- 827.Wirsing von König, C. H., J. E. Hoppe, A. Tacken, and H. Finger. 1990. Detection of Bordetella pertussis in clinical specimens, p. 315-320. Proceedings of the 6th International Symposium on Pertussis. DHHS no. FDA 90-1164. Department of Health and Human Services, Washington, D.C.
- 828.Wirsing von König, C. H., S. Postels-Multani, H. L. Bock, and H. J. Schmitt. 1995. Pertussis in adults: frequency of transmission after household exposure. Lancet 346:1326-1329. [DOI] [PubMed] [Google Scholar]
- 829.Wirsing von König, C. H., H. Rott, H. Bogaerts, and H. J. Schmitt. 1998. A serologic study of organisms possibly associated with pertussis-like coughing. Pediatr. Infect. Dis. J. 17:645-649. [DOI] [PubMed] [Google Scholar]
- 830.Wolff, J., G. H. Cook, A. R. Goldhammer, and S. A. Berkowitz. 1980. Calmodulin activates prokaryotic adenylate cyclase. Proc. Natl. Acad. Sci. USA 77:3841-3844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 831.Woolfrey, B. F., and J. A. Moody. 1991. Human infections associated with Bordetella bronchiseptica. Clin. Microbiol. Rev. 4:243-255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 832.World Health Organization. 1991. WHO meeting on case definition of pertussi: Geneva, 10-11 January 1991. Issue no. MIN/EP1/PERT/91.1. WHO Geneva, Switzerland.
- 833.World Health Organization, and Expert Committee on Biological Standardization. 1964. Requirements for pertussis vaccine. Requirements for biological substances, no. 8. 16th Report. Technical report series no. 274. World Health Organization, Geneva, Switzerland.
- 834.Wright, N. G., H. Thompson, D. Taylor, and H. J. Cornwell. 1973. Bordetella bronchiseptica: a re-assessment of its role in canine respiratory disease. Vet. Rec. 93:486-487. [DOI] [PubMed] [Google Scholar]
- 835.Wright, S. W., K. M. Edwards, M. D. Decker, and M. H. Zeldin. 1995. Pertussis infection in adults with persistent cough. JAMA 273:1044-1046. [PubMed] [Google Scholar]
- 836.Xu, Y., and J. T. Barbieri. 1996. Pertussis toxin-catalyzed ADP-ribosylation of Gi-2 and Gi-3 in CHO cells is modulated by inhibitors of intracellular trafficking. Infect. Immun. 64:593-599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 837.Xu, Y., and J. T. Barbieri. 1995. Pertussis toxin-mediated ADP-ribosylation of target proteins in Chinese hamster ovary cells involves a vesicle trafficking mechanism. Infect. Immun. 63:825-832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 838.Yih, W. K., S. M. Lett, F. N. des Vignes, K. M. Garrison, P. L. Sipe, and C. D. Marchant. 2000. The increasing incidence of pertussis in Massachusetts adolescents and adults, 1989-1998. J. Infect. Dis. 182:1409-1416. [DOI] [PubMed] [Google Scholar]
- 839.Yih, W. K., E. A. Silva, J. Ida, N. Harrington, S. M. Lett, and H. George. 1999. Bordetella holmesii-like organisms isolated from Massachusetts patients with pertussis-like symptoms. Emerg. Infect. Dis. 5:441-443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 840.Yuk, M. H., E. T. Harvill, P. A. Cotter, and J. F. Miller. 2000. Modulation of host immune responses, induction of apoptosis and inhibition of NF-kappaB activation by the Bordetella type III secretion system. Mol. Microbiol. 35:991-1004. [DOI] [PubMed] [Google Scholar]
- 841.Yuk, M. H., E. T. Harvill, and J. F. Miller. 1998. The BvgAS virulence control system regulates type III secretion in Bordetella bronchiseptica. Mol. Microbiol. 28:945-959. [DOI] [PubMed] [Google Scholar]
- 842.Yuk, M. H., U. Heininger, G. Martinez de Tejada, and J. F. Miller. 1998. Human but not ovine isolates of Bordetella parapertussis are highly clonal as determined by PCR-based RAPD fingerprinting. Infection 26:270-273. [DOI] [PubMed] [Google Scholar]
- 843.Zackrisson, G., T. Lagergård, B. Trollfors, and I. Krantz. 1990. Immunoglobulin A antibodies to pertussis toxin and filamentous hemagglutinin in saliva from patients with pertussis. J. Clin. Microbiol. 28:1502-1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 844.Zaretzky, F. R., M. C. Gray, and E. L. Hewlett. 2002. Mechanism of association of adenylate cyclase toxin with the surface of Bordetella pertussis: a role for toxin-filamentous haemagglutinin interaction. Mol. Microbiol. 45:1589-1598. [DOI] [PubMed] [Google Scholar]
- 845.Zepp, F., M. Knuf, P. Habermehl, J. H. Schmitt, C. Rebsch, P. Schmidtke, R. Clemens, and M. Slaoui. 1996. Pertussis-specific cell-mediated immunity in infants after vaccination with a tricomponent acellular pertussis vaccine. Infect. Immun. 64:4078-4084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 846.Zhang, Y. L., and R. D. Sekura. 1991. Purification and characterization of the heat-labile toxin of Bordetella pertussis. Infect. Immun. 59:3754-3759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 847.Zuabi, T., A. Faivisevitz, and M. L. Alkan. 1999. Severe pneumonia caused by Bordetella bronchiseptica. Harefuah 137:189-190, 263. (In Hebrew.) [PubMed] [Google Scholar]
- 848.Zuelzer, W. W., and W. E. Wheeler. 1946. Parapertussis pneumonia. J. Pediatr. 29:493-497. [DOI] [PubMed] [Google Scholar]