Abstract
A 5 year old, neutered male, domestic shorthaired cat had acute left hemiparesis and Horner's syndrome. Magnetic resonance imaging (MRI) revealed a loss of the normal signal from the nucleus pulposus of the intervertebral disc at C3/4, narrowing of the ventral subarachnoid space and slight dorsal displacement of the spinal cord and a focal hyperintense lesion affecting the left side of the spinal cord at the same level. The presumptive diagnosis was focal spinal cord oedema associated with intervertebral disc extrusion. A traumatic aetiology was suspected. The cat was treated conservatively and improved gradually over a period of 6 months.
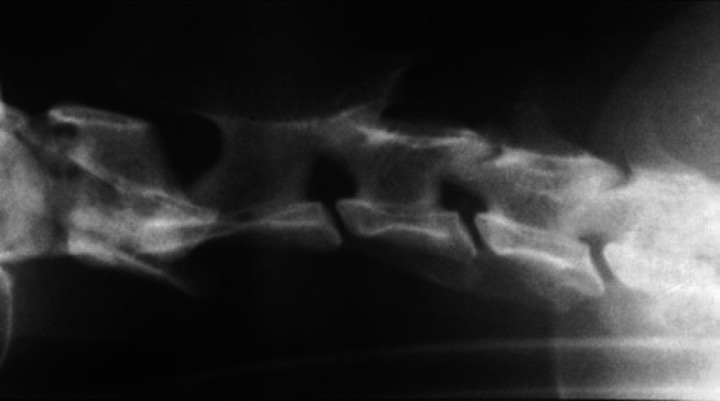
A 5-year-old, neutered male, domestic shorthaired cat was found unable to walk after being missing for 12 h. No signs of trauma were identified on physical examination. Survey radiography of the cervical spine revealed a narrowed intervertebral disc space at C3/4 (Fig 1). The cat was referred without any treatment to the Queen Mother Hospital for Animals, Royal Veterinary College within 24 h of the onset of clinical signs.
Fig 1.
Lateral radiograph of the cervical region. The inter-vertebral space at C3/4 appears slightly narrowed and there is a faint opacity superimposed on the intervertebral foramen, possibly reflecting extruded disc material.
The cat was recumbent with normal mental status. There was left hemiparesis and absence of conscious proprioception affecting the left thoracic and pelvic limbs. Muscle tone was slightly reduced in the left thoracic limb and slightly increased in the left pelvic limb. Withdrawal reflexes were reduced in the left thoracic limb but patellar and withdrawal reflexes were exaggerated in the left pelvic limb. Muscle tone and reflexes on the right were normal. Panniculus reflex was intact and deep pain perception was judged normal in all limbs. No signs of pain were detected on palpation of the entire spine, including gentle manipulation of the neck. There was mild anisocoria, protrusion of the left third eyelid and miosis of the left eye that appeared more marked in dim light. Pupillary light reflexes and a fundic examination were normal. The left pinna felt warmer than the right. Administering 10% phenylephrine eye drops into each eye resulted in mydriasis of the left pupil occurring in 55 min, compatible with first order Horner's syndrome (Petersen-Jones 1995). On the basis of the neurological signs, the presumptive diagnosis was left sided cervical spinal cord lesion.
The cat was anaesthetised for MRI of the cervical spinal cord (Philips Gyroscan NT 1.5 Tesla). In T2-weighted images there was a loss of the normal signal from the nucleus pulposus of the intervertebral disc at C3/4 and a focal hyperintense lesion affecting the left side of the spinal cord at the same level (Fig 2). Narrowing of the ventral subarachnoid space and slight dorsal displacement of the spinal cord at C3/4 was identified on sagittal images compatible with an extradural sign on the ventral aspect (Fig 2). T1-weighted images of the cord appeared normal. There was a minor increase in signal intensity affecting the cord at C3/4 after intravenous gadolinium oxide (Gadoteric acid, Dotarem). On the basis of these findings, the presumptive diagnosis was focal spinal cord oedema associated with intervertebral disc extrusion at C3/4.
Fig 2.
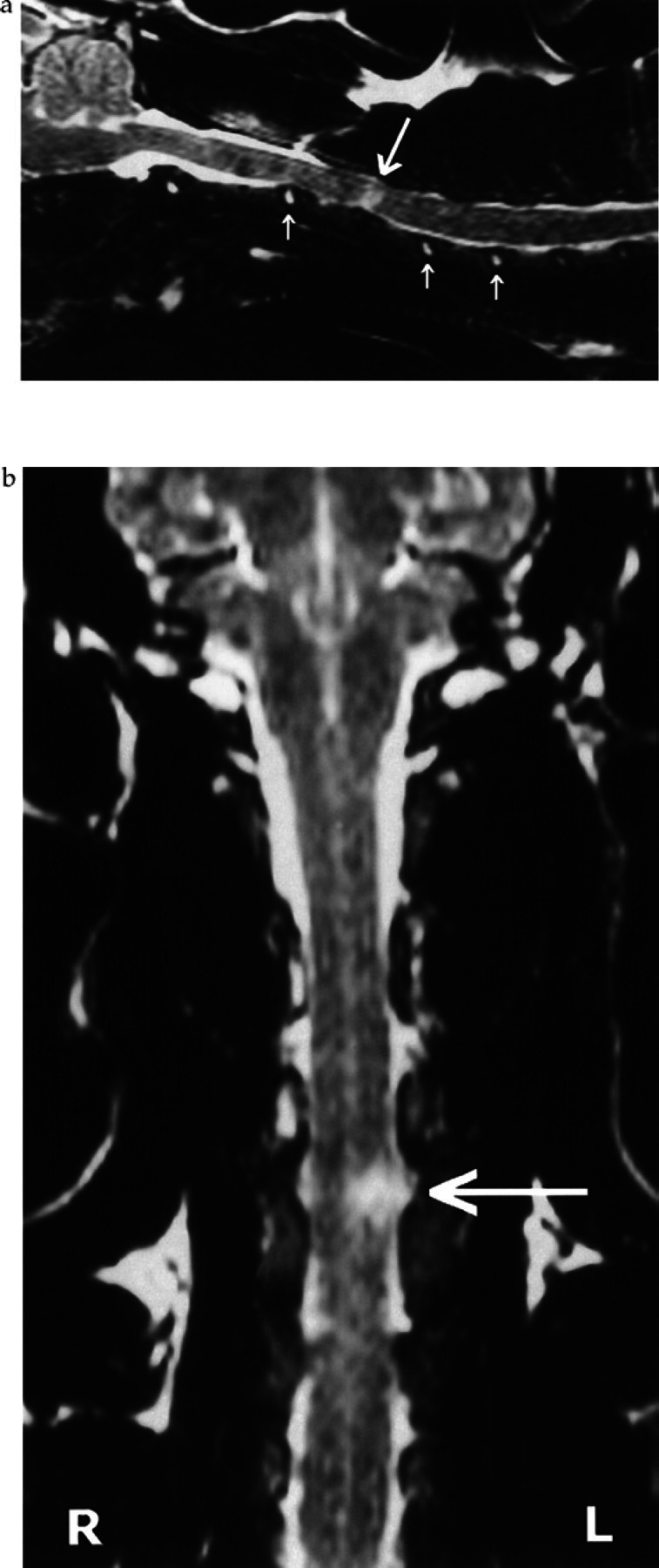
Sagittal (A) and dorsal (B) T2-weighted MR spin-echo images (TR ms, TE ms) of the cervical spine. The hyperintense signal that represents the normal nucleus pulposus is visible at intervertebral spaces throughout the cervical region (small arrows) with exception of C3/4. Narrowing of the ventral subarachnoid space and slight dorsal displacement of the cord at C3/4 suggests an extradural lesion on its ventral aspect. A focal hyperintense lesion compatible with oedema or necrosis is visible on both images affecting the left side of the spinal cord at C3/4 (large arrow).
Cerebrospinal fluid (CSF) collected from the cisterna magna had a neutrophilic pleiocytosis (greater than 99% non-degenerate neutrophils), occasional large mononuclear cells and moderate number of erythrocytes. The total cell count was 166 nucleated cells/mm3 (normal less than 5 cells/mm3) and 539 erythrocytes/mm3 (normal 0/mm3). Total protein level was elevated at 0.29 g/l (normal less than 0.25 g/l). No microorganisms were identified. The CSF analysis was considered compatible with an acute, moderate inflammatory process.
The cat was treated with prednisolone (initially 1 mg/kg every 12 h) using a reducing dose over a period of 3 weeks. The cat improved gradually. Mild left hemiparesis was the only abnormality detected when re-examined 6 m later.
Discussion
Degeneration and dorsal protrusion of the intervertebral discs is a common finding in cats at necropsy (King et al 1958, King & Smith 1960a, b & c, 1964); however, few cats ever have clinical signs of spinal cord disease secondary to intervertebral disc protrusion. Sporadic case reports have described cats with either a Hansen type I disc extrusion (Hoerlein 1978, Seim & Nafe 1981, Gilmore 1983, Bagley et al 1995, Sparkes & Skerry 1990, Kathmann et al 2000) or type II protrusion (Heavner 1971, Littlewood et al 1984).
In the present case, the acute onset neurological signs, narrowed C3/4 intervertebral disc space, MRI abnormalities and ipsilateral spinal cord signs all support a diagnosis of traumatic disc extrusion, which is an uncommon diagnosis in the cat (Hoerlein 1978). Although we have no direct evidence of a traumatic incident affecting the cat in this report, this seems a strong possibility. The clinical signs in the present case are similar to those described in a series of dogs that had trauma affecting the cervical spine (Griffiths 1970). All dogs had a variable degree of hemiparesis, Horner's syndrome, hyperthermia of the ipsilateral side and, in some cases, there was positional dystonia. In addition, each dog had a narrowed cervical intervertebral space identified radiographically without evidence of disc calcification or other degenerative changes.
Lesions affecting the lateral tectotegmentospinal tracts within C1-T3 cord segments may result in a sympathetic paralysis of the entire ipsilateral side of the head, body and limbs (DeLahunta 1983) and, therefore, may result in unilateral Horner's syndrome and hyperthermia because of peripheral vasodilatation. It is uncertain whether the degree of Horner's syndrome is related to the severity of cord injury, recovery time or prognosis. It is reported that Horner's syndrome is rarely associated with C1–5 cord disease because lesions severe enough to cause the syndrome usually cause respiratory failure leading to death (Raw 1994); however, in our experience, Horner's syndrome, or at least a partial Horner's syndrome (for example, ipsilateral miosis without any iris pathology), is a moderately frequent finding in animals with cervical spinal cord lesions.
The CSF analysis in the present case is interesting. Presence of erythrocytes and neutrophilic pleiocytosis can be associated with high-velocity–low-volume disc extrusion (author's unpublished data). In Griffiths' report (1970), CSF was collected from only one case, which revealed numerous erythrocytes; however, no comment was made about nucleated cell count or cytology. Similarly, CSF analysis was not reported in the study by Yarrow & Jeffery (2000).
The principles of diagnosis and treatment for cats with suspected disc protrusion are similar to those applied to dogs (Bagley et al 1995). Surgery to remove extruded disc material from the vertebral canal is indicated if there is radiographic evidence of significant extradural compression (Kathmann et al 2000); however, a small volume of extruded disc material may be dispensed in the epidural fat and may be difficult to identify surgically (Sanders et al 1999). Also, it has been stated that surgery may be less beneficial if there is a very small amount of disc material in the vertebral canal, or if the extruded disc material has penetrated the dura and entered the spinal cord (Schrader 1989). In the present case, the degree of impingement on the cord, assessed by MRI suggested the presence of only a small amount of extruded disc material. Because of this, and because we believed the left-sided intra-parenchymal cord lesion to be responsible for the clinical signs, conservative management is more appropriate in this case.
Use of steroid therapy in animals with acute disc extrusion remains a controversial subject. There is evidence that use of methylprednisolone sodium succinate is beneficial for humans with acute spinal cord injury (Bracken et al 1992); however, these results have not been reproduced in dogs or cats. In dogs with this particular type of high-velocity-low-volume disc extrusion, the prognosis for return of motor function is good if deep pain perception is intact (Griffiths 1970, Yarrow & Jeffery 2000). Nevertheless, some neurological deficits, such as ipsilateral weakness or incontinence, may be permanent.
The principal diagnostic imaging techniques for investigating clinical signs of spinal cord disease in dogs or cats are survey radiography and myelography, although computed X-ray tomography and MRI are used increasingly (Sharp et al 1995, Bagley et al 1995, Kneissl & Schedlbauer 1997, Levitski et al 1999, Olby et al 2000). In the present case, MRI was chosen rather than myelography because of the potential to identify lesions affecting any anatomical component of the cervical spine including the vertebrae, intervertebral discs and spinal cord. Loss of hydration of the nucleus pulposus, which is recognised as a reduced signal on T2-weighted images, is a common finding that indicates either degeneration or protrusion (Flanders et al 1992, Kioumehr & Ziegler 1998). Similarly, the combination of increased signal on T2-weighted images and normal T1-weighted images of the spinal cord, as observed in this cat, is compatible with a non-haemorrhagic spinal cord contusion (Flanders et al 1992, Kioumehr & Ziegler 1998). The location of the lesion based on neurological signs, the survey radiographic findings and the close proximity of the disc lesion, extradural sign and intramedullary lesion on MRI all support the conclusion that extrusion of a small volume of a nucleus pulposus at C3/4 was the cause of clinical signs in this cat.
References
- Bagley RS, Tucker RL, Moore MP, Harrington ML. (1995) Radiographic diagnosis: intervertebral disc extrusion in a cat. Veterinary Radiology & Ultrasound 36, 380–382. [Google Scholar]
- Bracken MB, Shepard MJ, Collins WF, Jr., et al. (1992) Methylprednisolone or naloxone treatment after acute spinal cord injury: 1-year follow-up data. Results of the second National Acute Spinal Cord Injury Study. Journal of Neurosurgery 76, 23–31. [DOI] [PubMed] [Google Scholar]
- DeLahunta A. (1983) In: Veterinary Neuroanatomy and Clinical Neurology (2nd edn). WB Saunders, Philadelphia, pp 116–120. [Google Scholar]
- Flanders AE, Tartaglino LM, Friedman DP, Aquilone LF. (1992) Magnetic resonance imaging in acute spinal injury. Seminars in Roentgenology 27, 271–298. [DOI] [PubMed] [Google Scholar]
- Gilmore DR. (1983) Extrusion of a feline intervertebral disc. Veterinary Medicine/Small Animal Clinician 78, 207–209. [Google Scholar]
- Griffiths IR. (1970) A syndrome produced by dorso-lateral ‘explosions’ of the cervical intervertebral discs. The Veterinary Record 87, 737–741. [DOI] [PubMed] [Google Scholar]
- Heavner JE. (1971) Intervertebral disc syndrome in the cat. Journal of the American Veterinary Medical Association 159, 425–427. [PubMed] [Google Scholar]
- Hoerlein BF. (1978) Disc disorders in cats. In: Canine neurology, (3rd edn). Hoerlein B.F (ed.) WB Saunders, Philadelphia, pp. 551–555. [Google Scholar]
- Kathmann I, Cizinauskas S, Rytz U, Lang J, Jaggy A. (2000) Spontaneous lumbar intervertebral disc protrusion in cats: literature review and case presentations. Journal of Feline Medicine and Surgery 2, 207–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King AS, Smith RN, Kon VM. (1958) Protrusion of the intervertebral disc in the cat. The Veterinary Record 70, 509–512. [Google Scholar]
- King AS, Smith RN. (1960a) Disc protrusions in the cat: distribution of dorsal protrusions along the vertebral column. The Veterinary Record 72, 335–337. [Google Scholar]
- King AS, Smith RN. (1960b) Disc protrusion in the cat: age incidence of dorsal protrusions. The Veterinary Record 72, 381–382. [Google Scholar]
- King AS, Smith RN. (1960c) Disc protrusion in the cat: ventral protrusions and radial splits. Research in Veterinary Science 1, 310–307. [Google Scholar]
- King AS, Smith RN. (1964) Degeneration of the intervertebral disc in the cat. Acta Orthopaedica Scandinavica 34, 139–158. [DOI] [PubMed] [Google Scholar]
- Kioumehr F, Ziegler JW. (1998) Magnetic resonance imaging of the spine. In: The MRI manual, 2nd edn. Lufkin RB. (ed.) Mosby, London, pp. 213–232. [Google Scholar]
- Kneissl S, Schedlbauer B. (1997) Sagittal computed tomography of the feline spine. Veterinary Radiology & Ultrasound 38, 282–283. [DOI] [PubMed] [Google Scholar]
- Levitski RE, Lipsitz D, Chauvet AE. (1999) Magnetic resonance imaging of the cervical spine in 27 dogs. Veterinary Radiology & Ultrasound 40, 332–341. [DOI] [PubMed] [Google Scholar]
- Littlewood JD, Herrtage ME, Palmer AC. (1984) Intervertebral disc protrusion in a cat. Journal of Small Animal Practice 25, 119–127. [Google Scholar]
- Olby NJ, Muñana KR, Sharp NJH, Thrall DE. (2000) The computed tomographic appearance of acute thoracolumbar intervertebral disc herniations in dogs. Veterinary Radiology & Ultrasound 41, 396–402. [DOI] [PubMed] [Google Scholar]
- Petersen-Jones SM. (1995) Abnormalities of eyes and vision. In: Manual of Small Animal Neurology (2nd edn) Wheeler SJ. (ed.) British Small Animal Veterinary Association, Cheltenham, pp. 136. [Google Scholar]
- Raw ME. (1994) Horner's syndrome in the dog and cat. Veterinary Annual 34, 181–188. [Google Scholar]
- Sanders S, Bagley RS, Tucker RL, Nelson NR. (1999) Radiographic diagnosis: focal spinal cord malacia in a cat. Veterinary Radiology & Ultrasound 40, 122–125. [DOI] [PubMed] [Google Scholar]
- Schrader SC. (1989) Neurosurgery. In: The Cat, Diseases and Management, volume 2, Sherding RG. (ed.) Churchill Livingstone, New York, pp 1225–1245. [Google Scholar]
- Seim HB, Nafe LA. (1981) Spontaneous intervertebral disc extrusion with associated myelopathy in a cat. Journal of the American Animal Hospital Association 17, 201–204. [Google Scholar]
- Sharp NJH, Cofone M, Robertson ID, DeCarlo A, Smith GK, Thrall DE. (1995) Computed tomography in the evaluation of caudal cervical spondylomyelopathy of the Dobermann Pinscher. Veterinary Radiology & Ultrasound 36, 100–108. [Google Scholar]
- Sparkes AH, Skerry TM. (1990) Successful management of a prolapsed intervertebral disc in a Siamese cat. Feline Practice 18, 7–9. [Google Scholar]
- Yarrow TG, Jeffery ND. (2000) Dura mater laceration associated with acute paraplegia in three dogs. Veterinary Record 146, 138–139. [DOI] [PubMed] [Google Scholar]