Abstract
Background
Research continues to show an association between oral health and systemic health, further stressing the importance of effective daily plaque removal via toothbrushing to maintain periodontal health and overall well-being. This investigation was undertaken to compare the efficacy of oscillating-rotating, sonic, and manual toothbrushes in reducing gingivitis and plaque in randomised controlled trials (RCTs) with up to 6 months’ follow-up.
Methods
This meta-analysis was conducted from a single database (Procter & Gamble Oral Care Clinical Archive) including RCTs from 2007 to 2022. Three authors independently assessed study eligibility. Disagreements concerning selected studies were resolved by discussion with an expert colleague. Direct and indirect treatment comparisons along with transition rates to gingival health were calculated using participant-level data. Transition-to-health time was calculated using data from all time points. Subregion analyses evaluated number of bleeding sites and plaque reduction.
Results
This meta-analysis included 21 gingivitis RCTs and 25 plaque RCTs. Relative to manual and sonic brushes, oscillating-rotating brushes had a higher percentage of participants who transitioned to gingival health (72% vs 21% and 54%; P < .001). Compared with manual and sonic brushes, respectively, oscillating-rotating brushes demonstrated greater bleeding site reductions (by 52% and 29%; P < .001) and superior plaque reductions (by 19% and 5%; P < .001). Oscillating-rotating brushes provided faster transitions to health than sonic brushes and showed greater efficacy across subregions. The most advanced oscillating-rotating brush demonstrated statistically significantly greater efficacy compared with traditional oscillating-rotating, manual, and sonic brushes when analysed separately. Risk of bias was deemed low for all studies.
Conclusions
Oscillating-rotating toothbrushes offer superior results for transition to health, gingivitis, and plaque reduction compared with manual and sonic brushes. The most advanced oscillating-rotating model offers enhanced efficacy vs traditional models.
Key words: Biofilm, Bacteria, Prevention and control, Toothbrushing, Gingival disease, periodontitis
Introduction
Bacterial plaque triggers gingivitis, an oral inflammatory response marking the onset of periodontal disease,1 which is a widespread global issue.2 Effective toothbrushing removes dental plaque3 to prevent and reverse gingivitis, thereby reducing the risk of periodontitis, which has been associated with systemic conditions such as cardiovascular disease, diabetes, and Alzheimer's disease.4 Therefore, for the individual, removing plaque and preventing gingivitis have the potential to improve not only oral health but also whole-body health. For society, a cost-benefit analysis5 established that the economic burden of periodontitis is mitigated better by a strategy of prevention than of treatment. Prevention also ameliorates the environmental burden of dentistry, contributing towards an ecologically sustainable dental practice over time.6
Twice-daily brushing with a fluoride toothpaste is accepted as the basic standard of care for at-home plaque removal. Whilst a well-designed manual toothbrush can provide thorough plaque removal, the effectiveness of this device is highly sensitive to users’ brushing behaviour and compliance with professional guidance.7 Over time, a variety of toothbrush designs have been developed to optimise plaque control, including electric toothbrushes. Electric brushes have demonstrated consistently greater gingivitis reduction and plaque removal compared with manual brushes in systematic reviews.3,8, 9, 10 An 11-year observational study also found that electric toothbrush users exhibited reduced clinical attachment loss progression and periodontal pocket depth as well as greater tooth retention compared with manual brush users.11
Electric toothbrushes have evolved to include built-in timers, pressure sensors, expanded brushing modes, and Bluetooth-connected apps to increase brushing time and thoroughness.12,13 The majority of contemporary electric toothbrushes are classified as sonic (side-to-side motion) or oscillating-rotating (O-R). Evidence shows greater gingivitis and plaque reduction for the latter technology.8,14, 15, 16, 17 A prior meta-analysis assessed the gingivitis- and plaque-reducing effects of O-R vs manual and sonic electric toothbrushes.15 That analysis focused on 20 randomised controlled trials (RCTs) evaluating plaque and 16 RCTs assessing gingivitis, all of which were conducted between 2007 and 2017. Access to participant-level data was required from every study to assess the relationship between baseline and end-of-treatment gingivitis levels for each tested toothbrush. In 2020, an O-R brush model (iO; Oral-B iO, Procter & Gamble) was introduced with a linear magnetic drive replacing the traditional O-R gear-based mechanical drive system. The linear magnetic drive produces micro-vibrations at bristle tips, which might augment plaque removal.12
In light of the significant design changes associated with the latest O-R model, this investigation was undertaken to extend the reach of the prior meta-analysis and compare the efficacy of O-R toothbrushes, including the latest model, with manual negative control and sonic positive control toothbrushes in reducing gingivitis and plaque in RCTs with up to 6 months’ follow-up. It also offers new perspectives on the data. Whilst the previous analysis characterised gingivitis solely by number of bleeding sites, the new analysis additionally reflects changes in patients’ modified gingival index (MGI) scores. New by-region analyses of number of bleeding sites and Rustogi Modified Navy Plaque scores shed light on brush efficacy in hard-to-reach areas. Additionally, the current study analyses participant-level data from all time points in each study (vs only baseline and final time points) to assess how quickly patients transitioned to a gingival health state. Finally, this new meta-analysis includes toothbrushing efficacy evaluations over a longer usage period (up to 6 months), whereas the prior meta-analysis included studies up to 3 months.
Materials and methods
This study was conducted in accordance with the PRISMA statement18 and is registered on ClinicalTrials.gov (NCT05594004). All RCTs included in this analysis were conducted according to protocols approved by Ethics Committees and in compliance with the International Conference on Harmonization (ICH) and Good Clinical Practice (GCP) principles.
Search process
The authors searched the Procter & Gamble Oral Care Clinical Archive for eligible RCTs from 2007 to 2022, which includes new studies and those in the prior meta-analysis.15 Trials in the archive were reviewed to determine their eligibility for inclusion in the meta-analysis. This meta-analysis was not associated with a systematic review because individual participant-level data were required.
Eligibility criteria
Studies that met the following criteria were eligible: (1) up to 6 months’ duration; (2) randomised and controlled, parallel-group, and examiner-blinded design; (3) reported plaque and/or gingivitis outcomes after an intervention with comparator control group(s); and (4) examiner-based. Digital imaging studies were excluded. All individual studies excluded participants with severe periodontal disease, as characterised by purulent exudate, generalised mobility, and/or severe recession.
Study selection and data collection
Three authors (RA, JG, YZ) independently assessed study eligibility. Disagreements concerning selected studies were resolved by discussion with an expert colleague. From selected studies, the following data were collected for both intervention and control groups: study name, year, country, and design; age and sex of each participant; experimental and comparator treatments; timing of follow-up visits; and outcome measurements (participant-level data).
Risk of bias assessment
The quality of each RCT was assessed using the Cochrane risk-of-bias tool (RoB2) for randomised parallel-group trials.19
Statistical analysis
Gingivitis data were expressed in terms of number of bleeding sites and MGI score.20 As in the previous meta-analysis,15 the number of bleeding sites was calculated using the Löe-Silness Gingival Index, Gingival Bleeding Index, Papillary Bleeding Index, or Mazza Gingival Index within each study. If there was more than 1 follow‐up visit in the trial, the final assessment up to and including the 6-month visit was used for data extraction for all analyses except the time-to-transition-to-health analysis, which included all assessments. One-step, participant-level meta-analysis used a mixed model for direct and indirect treatment comparisons and for identification of participant-level covariates.21 Study and treatment were included as random effects, allowing for different treatment-effect sizes by study. Baseline gingivitis score and separate interactions with study and treatment were also modelled to allow the relationship between baseline and end-of-treatment gingivitis score to differ by study and treatment. The 1-step model allowed for between-study variability of the residual variance (Equation 9).22 Adjusted treatment mean gingivitis scores with standard error bars and estimated mean difference between treatments with P values and 95% confidence intervals (CIs) were included in the bar plots with tables. Percentage changes from control were calculated using adjusted mean scores. Similar analyses were also generated for lingual, buccal, molar, molar-lingual, and molar-buccal subregions.
Classification of gingival status as healthy (<10% bleeding sites), localised gingivitis (10%−30% bleeding sites), or generalised gingivitis (>30% bleeding sites) was based on gingivitis case definitions established in 2017.1 Rates of transition between classes were calculated for each treatment, and odds ratios were generated with 95% CIs. To assess time to reaching gingival health status, all interim time point bleeding data were used for the time-to-event analysis with event defined as transition to gingival health (<10% bleeding sites). The cumulative incidence of event (F(t)) is described as the probability that an event has occurred by time t, ie, F(t) = 1-S(t)= Pr(T ≤ t) with S(t) as the survival function. The cumulative incidence curve is therefore the complement of the survival curve which can be estimated from Kaplan–Meier estimator. Data are considered as censored when a participant does not experience a transition to health by the end of the study. The cumulative incidence curve is plotted with 95% CIs for each treatment and overall treatment comparison is generated using the Log-rank test.23
Per the prior meta-analysis,15 plaque data, expressed as Turesky Modification of the Quigley-Hein Index or the Rustogi Modified Navy Plaque Index, were standardised by dividing each study's mean treatment difference by the respective standard deviation.24 Direct and indirect comparisons of treatments were accomplished by network meta-analysis; the requisite assumptions of homogeneity, transitivity, and treatment rank credibility were confirmed as satisfied. Network meta-analysis produced treatment differences with P values, 95% CIs, and P scores based on point estimates and standard errors of the frequentist network meta-analysis estimates. P scores were calculated as averaged 1-sided P values and used to rank the treatments25; larger P scores indicate greater certainty that a given treatment has better antiplaque efficacy. Percentage change from control was calculated by the weighted percentage change from the control from each study with weights calculated from the random-effects model using within-study variance and between-study variance. A 1-step meta-analysis on Rustogi Modified Navy Plaque Index was also done for lingual, buccal, molar, molar-lingual, molar-buccal, interproximal, interproximal-anterior, interproximal-molar, and gingival subregions.
Summary-level and network meta-analyses used the “metafor” and “net Meta” packages in R version 3.2.3.26,27 Participant-level time to event analysis used “survival” and “surd miner” packages in the same R version. All other participant-level analyses were conducted using SAS 9.4 (SAS Institute).
Results
Clinical trials overview
This meta-analysis represents 21 RCTs from 3 countries, involving 2655 participants, wherein gingivitis was assessed. Eight trials compared O-R brushes with manual brushes; 13 trials compared O-R brushes with sonic brushes. There were 25 RCTs from 3 countries, involving 3019 participants, wherein plaque was assessed. Eleven trials compared O-R brushes with manual brushes; 14 trials compared O-R brushes with sonic brushes28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49 (see Table 1).
Table 1.
Randomised controlled trials included in the meta-analyses, listed in reverse chronological order.
| Study | Location | Duration | Population, inclusion criteria | Outcomes measures | Control toothbrush |
|---|---|---|---|---|---|
| Grender et al28 | Ontario, Canada | 12 weeks | Adults N = 100 BS: 20–90 MGI: 1.75–2.5 RMNPI: >0.5 |
GBI, MGI, RMNPI | Manual: Oral-B Indicator |
| Grender et al29 | Ontario, Canada | 12 weeks | Adults N = 100 BS: 20–90 MGI: 1.75–2.5 RMNPI: >0.5 |
GBI, MGI, RMNPI | Manual: Oral-B Indicator |
| Goyal et al30 | Ontario, Canada | 6 months | Adults N = 110 BS: 20–90 MGI: 1.75–2.5 RMNPI: >0.5 |
GBI, MGI, RMNPI | Sonicare DiamondClean |
| Adam et al31 | Ontario, Canada | 8 weeks | Adults N = 90 BS: 20–90 MGI: 1.75–2.5 RMNPI: >0.5 |
GBI, MGI, RMNPI | Sonicare DiamondClean |
| Grender et al32 | Ontario, Canada | 8 weeks | Adults N = 110 BS: ≥20 MGI: ≥1.75 RMNPI: >0.5 |
GBI, MGI, RMNPI | Manual: ADA reference |
| Ccahuana-Vasquez et al33 | Ontario, Canada | 5 weeks | Adults N = 150 BS: ≥10 MGI: 1.75–2.3 RMNPI: ≥0.5 |
GBI, MGI, RMNPI | Manual: ADA reference |
| Ccahuana-Vasquez et al34 | Ontario, Canada | 8 weeks | Adults N = 148 BS: ≥10 MGI: 1.75–2.3 RMNPI: ≥0.5 |
GBI, MGI, RMNPI | Sonicare DiamondClean |
| Erbe et al35 | Mainz, Germany | 2 weeks | Adolescents N = 59 TMQHPI: ≥1.75 |
TMQHPI | Manual: Oral-B 35 Indicator |
| Adam et al36 | Indiana, USA | 8 weeks | Adults N = 95 TMQHPI |
TMQHPI | Manual: ADA reference |
| Li et al37 | Beijing, China | 3 months | Adults N = 123 BS: ≥15 |
Mazza GI | Manual: Lion Dentor Systema |
| Ccahuana-Vasquez et al38 | Ontario, Canada | 8 weeks | Adults N = 148 BS: ≥10 MGI: 1.75–2.3 RMNPI: ≥0.5 |
GBI, MGI, RMNPI | Sonicare DiamondClean |
| Goyal 2015, unpublished | Ontario, Canada | 4 weeks | Adults N = 97 RMNPI: ≥0.5 |
GBI, MGI, TMQHPI | Sonicare DiamondClean |
| Klukowska et al39 | Indiana, USA | 6 weeks | Adults N = 94 TMQHPI ≥1.75 |
TMQHPI | Manual: ADA reference |
| Klukowska et al40 | Ontario, Canada | 12 weeks | Adults N = 127 BS: ≥10 MGI: 1.75–2.3 RMNPI: ≥0.5 |
GBI, MGI, RMNPI | Sonicare FlexCare Platinum |
| Klukowska et al41 | Nevada, USA | 6 weeks | Adults N = 128 BS: ≥10 MGI: 1.75–2.3 RMNPI: ≥0.5 |
GBI, MGI, RMNPI | Colgate ProClinical A1500 |
| Klukowska et al42 | Ontario, Canada | 6 weeks | Adults N = 128 BS: ≥10 MGI: 1.75–2.3 RMNPI: ≥0.5 |
GBI, MGI, RMNPI | Sonicare DiamondClean |
| Büchel et al43 | Jena, Germany | 4 weeks | Adults N = 129 TMQHPI: ≥1.75 |
TMQHPI | Colgate ProClinical C200 |
| Milleman 2014, unpublished | Indiana, USA | 4 weeks | Adults N = 97 BS: ≥20 TMQHPI: ≥1.8 |
GBI, MGI, TMQHPI | Manual: ADA reference |
| Klukowska et al44 | Ontario, Canada | 4 weeks | Adults N = 99 BS: ≥10 MGI: 1.75–2.3 RMNPI: ≥0.5 |
GBI, MGI, RMNPI | Manual: ADA reference |
| Klukowska et al45 | Nevada, USA | 12 weeks | Adults N = 127 BS: ≥10 MGI: 1.75–2.3 RMNPI: ≥0.5 |
GBI, MGI, RMNPI | Colgate ProClinicalA1500 |
| Sigusch 2013, unpublished | Jena, Germany | 6 weeks | Adults N = 99 TMQHPI: ≥1.75 |
TMQHPI | Manual: ADA reference |
| Klukowska et al46 | Ontario, Canada | 12 weeks | Adults N = 130 BS: ≥10 MGI: 1.75–2.3 RMNPI: ≥0.5 |
GBI, MGI, RMNPI | Sonicare DiamondClean |
| Klukowska et al47 | Ontario, Canada | 4 weeks | Adults N = 117 MGI: 1.75–2.3 RMNPI: ≥0.5 |
GBI, MGI, RMNPI | Manual: ADA reference |
| Williams et al48 | Missouri, USA | 10 weeks | Adults N = 165 for LSGI; N = 176 for TMQHPI BS: ≥20 LSGI: ≥1.1 TMQHPI: ≥1.75 |
LSGI; TMQHPI | Sonicare FlexCare |
| Goyal et al49 | Ontario, Canada | 12 weeks | Adults N = 173 MGI: 1.73–2.3 |
GBI, MGI, RMNPI | Sonicare FlexCare |
| Putt 2007, unpublished | Indiana, USA | 12 weeks | Adults N = 188 PBI: ≥1.1 TMQHPI: ≥1.75 |
PBI, TMQHPI | Sonicare FlexCare |
GBI: Gingival Bleeding Index; LSGI: Löe-Silness Gingival Index; Mazza GI: Mazza Gingival Index; MGI: Modified Gingival Index; PBI: Papillary Bleeding Index; RMNPI: Rustogi Modified Navy Plaque Index; TMQHPI: Turesky Modification of Quigley-Hein Plaque Index.
Gingival bleeding sites
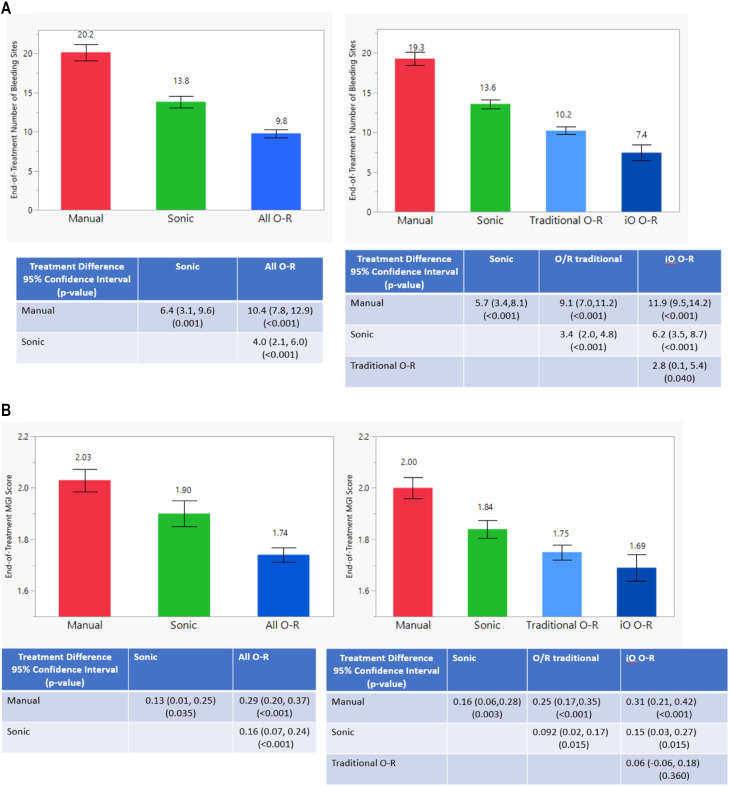
Figure 1A shows adjusted mean number of gingival bleeding sites at end of treatment per brush group. In studies assessing the effects of all O-R brushes (ie, iO O-R studies and traditional O-R studies combined) on gingivitis vs manual and sonic brushes, participants using an O-R brush had an average of 10.4 (95% CI, 7.8–12.9) fewer bleeding sites compared with a manual brush and 4.0 (95% CI, 2.1–6.0) fewer bleeding sites vs a sonic brush (P < .001) at end of treatment. These reductions equate to a 52% and 29% bleeding reduction benefit for O-R technology vs the respective controls. When the iO O-R brush subgroup was analysed separately, it demonstrated the fewest bleeding sites, followed by traditional O-R, sonic, and manual brushes, in that order (P ≤ .04). Study participants using an iO O-R brush had a bleeding reduction benefit of 62% vs manual, 46% vs sonic, and 27% vs traditional O-R. The use of a sonic brush yielded a reduction in average number of bleeding sites of 6.4 vs manual (P = .001) and a 32% bleeding reduction.
Fig. 1.
A, Adjusted mean end-of-treatment number of bleeding sites (standard error), treatment differences, confidence intervals, and P values using 1-step meta-analysis on subject-level data. B, Adjusted mean end-of-treatment modified gingival index (MGI) scores (standard error), treatment differences, confidence intervals, and P values using 1-step meta-analysis on subject-level data.
Baseline bleeding-by-treatment interaction term was significant (P < .001) in the subject-level 1-step meta-analysis model, indicating that the effect of an O-R electric brush compared with that of the control depends on the number of baseline bleeding sites. The specific nature of this relationship is summarised in Supplementary Figure 1. The figure shows that the relative efficacy across brushes remains consistent, with iO O-R being the most effective and manual being the least effective, regardless of baseline bleeding level. The figure also demonstrates that the benefit of an O-R brush increases as baseline bleeding increases.
In the transition-to-health analysis, 72% of all O-R brush users with gingivitis at baseline transitioned to healthy gingival status at end of treatment compared with 54% of sonic brush users and 21% of manual brush users (P < .001). Participants with baseline gingivitis had 9.5 times better odds (95% CI, 7.0–13.0) of transitioning to gingival health status using O-R compared with a manual toothbrush and 2.2 times better odds (95% CI, 1.7–2.7) vs a sonic toothbrush. When subgroups of O-R users were analysed separately, 88% of participants using iO O-R and 65% of participants using traditional O-R transitioned from baseline gingivitis to a state of gingival health (P < .001; Table 2). A more detailed analysis showing transitions across generalised gingivitis, localised gingivitis, and gingival health is shown in Table 3.
Table 2.
Changes from baseline: baseline bleeding percentage vs postbaseline bleeding percentage.
| Postbaseline |
||||
|---|---|---|---|---|
| Baseline | Total (n) | Gingival health | Gingivitis | |
| All O-R | Gingival health | 487 | 479 (98%) | 8 (2%) |
| Gingivitis | 842 | 606 (72%) | 236 (28%) | |
| O-R subgroups: iO O-R | Gingival health | 0 | 0 (0%) | 0 (0%) |
| Gingivitis | 255 | 225 (88%) | 30 (12%) | |
| Traditional O-R | Gingival health | 487 | 479 (98%) | 8 (2%) |
| Gingivitis | 587 | 381 (65%) | 206 (35%) | |
| Manual | Gingival health | 132 | 132 (100%) | 0 (0%) |
| Gingivitis | 315 | 67 (21%) | 248 (79%) | |
| Sonic | Gingival health | 344 | 321 (93%) | 23 (7%) |
| Gingivitis | 535 | 290 (54%) | 245 (46%) | |
Data shown use 2 classifications: gingival health (<10% bleeding sites) and gingivitis (≥10% bleeding sites).
O-R, oscillating-rotating.
Table 3.
Changes from baseline: baseline bleeding percentage vs postbaseline bleeding percentage.
| Postbaseline |
|||||
|---|---|---|---|---|---|
| Baseline | Total (n) | Gingival health | Localised gingivitis | Generalised gingivitis | |
| All O-R | Gingival health | 487 | 479 (98%) | 8 (2%) | 0 (0%) |
| Localised gingivitis Generalised gingivitis |
693 149 |
570 (82%) 36 (24%) |
121 (17%) 88 (59%) |
2 (1%) 25 (17%) |
|
| O-R subgroups: iO O-R | Gingival health | 0 | 0 (0%) | 0 (0%) | 0 (0%) |
| Localised gingivitis Generalised gingivitis |
220 35 |
212 (96%) 13 (37%) |
8 (4%) 19 (54%) |
0 (0%) 3 (9%) |
|
| Traditional O-R | Gingival health | 487 | 479 (98%) | 8 (2%) | 0 (0%) |
| Localised gingivitis Generalised gingivitis |
473 114 |
358 (73%) 23 (20%) |
113 (24%) 69 (61%) |
2 (1%) 22 (19%) |
|
| Manual | Gingival health | 132 | 132 (100%) | 0 (0%) | 0 (0%) |
| Localised gingivitis Generalised gingivitis |
233 82 |
63 (27%) 4 (4%) |
167 (72%) 39 (48%) |
3 (1%) 39 (48%) |
|
| Sonic | Gingival health | 344 | 321 (93%) | 23 (7%) | 0 (0%) |
| Localised gingivitis Generalised gingivitis |
457 78 |
283 (62%) 7 (9%) |
166 (36%) 52 (67%) |
8 (2%) 19 (24%) |
|
Data shown use 3 classifications: gingival health (<10% bleeding sites), localised gingivitis (10%–30% bleeding sites), and generalised gingivitis (>30% bleeding sites).
O-R, oscillating-rotating.
Figure 1B shows adjusted mean MGI scores at end of treatment for each brush group. A reduction in the average MGI score of 0.29 (95% CI, 0.20–0.37) and 0.16 (95% CI, 0.07–0.24) was observed for all O-R brushes vs manual and sonic brushes, respectively (P < .001), representing a 14% and 8% benefit for O-R technology vs the respective controls. When the iO O-R brush subgroup was analysed separately, it demonstrated a comparable MGI score to traditional O-R (3% difference; P = .36). The iO O-R and traditional O-R subgroups both showed a statistically significantly lower MGI score vs manual (16% and 13%, respectively) and sonic brushes (8% and 5%, respectively; P ≤ .015 for all comparisons). The sonic brush MGI reduction vs manual was 0.13 (P = .035), a 6% MGI reduction.
Plaque: Network meta-analysis allowed for both direct and indirect comparisons of the treatments with respect to standardised mean plaque score (Table 4). O-R brushes, relative to manual brushes, reduced the average standardised plaque score by 1.85 (95% CI, 1.45–2.26), a reduction of 19%. Relative to sonic brushes, all O-R brushes reduced the average standardised plaque score by 0.57 (95% CI, 0.23–0.92), a reduction of 5%. Sonic brushes, relative to manual brushes, reduced the average standardised average plaque score by 1.28 (95% CI, 0.74–1.81), a reduction of 13%. Standardised plaque scores showed that the iO O-R brush produced the lowest plaque score, followed by the traditional O-R, sonic, and manual brushes (P < .001).
Table 4.
Network meta-analysis on standardised plaque score: standardised mean differences, 95% confidence intervals, and treatment P scores.
| SMD* (95% confidence interval) |
Sonic | All O-R | P score |
|---|---|---|---|
| Manual | −1.28 (−1.81 to −0.74) | −1.85 (−2.26 to −1.45) | .00 |
| Sonic | −0.57 (−0.92 to −0.23) | .50 | |
| All O-R | 1.00 | ||
| SMD* (95% confidence interval) |
Sonic | Traditional O-R | iO O-R | P score |
|---|---|---|---|---|
| Manual | −1.17 (−1.67 to −0.67) | −1.63 (−2.04 to −1.22) | −2.45 (−3.04 to −1.85) | .00 |
| Sonic | −0.46 (−0.79 to −0.13) | −1.28 (−1.90 to −0.65) | .33 | |
| Traditional O-R | −0.82 (−1.45 to −0.19) | .67 | ||
| iO O-R | 1.00 |
O-R, oscillating-rotating; SMD, standardised mean difference.
All pairwise comparisons are statistically significant (P < .001).
Regional analysis: Analyses of lingual, buccal, molar, molar-buccal, and molar-lingual subregions were conducted for number of bleeding sites (Supplementary Figure 2A). Statistically significant differences in favour of all O-R brushes persisted across all analysed subregions (P < .001).
Plaque scores were analysed for the same subregions listed above, along with interproximal, interproximal-anterior, interproximal-molar, and gingival surfaces (Supplementary Figure 2B). Statistically significant benefits persisted across all analysed subregions for O-R vs manual. O-R showed statistically significant differences vs sonic for lingual, buccal, interproximal, interproximal-anterior, and interproximal-molar subregions (P ≤ .028).
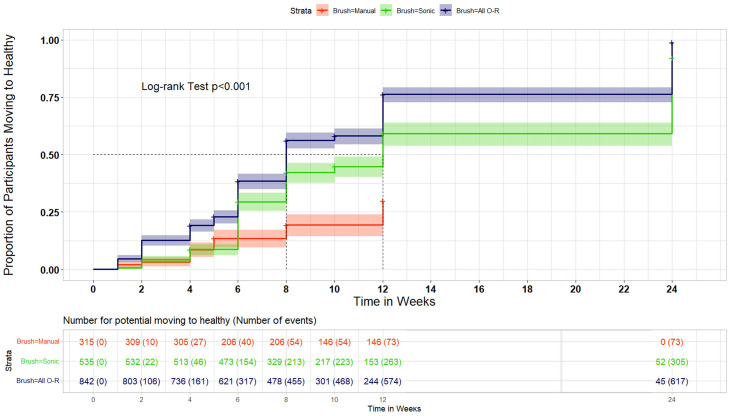
Time to transition to health: By 12 weeks, a higher percentage of O-R brush users (76.3%; 95% CI, 72.8%−79.4%) than manual brush users (29.8%; 95% CI, 23.9%−35.9%) or sonic brush users (59.2%; 95% CI, 54%−64.1%) transitioned from baseline gingivitis to a state of gingival health (Figure 2). Using the data from all time points, and assessing them cumulatively, the median time to transition to a state of health was 8 weeks for O-R brush users and 12 weeks for sonic brush users.
Fig. 2.
Percentage of participants transitioning to healthy gingival status over time.
Risk of bias
Risk of bias in each trial was deemed low for all 5 domains (Supplementary Figure 3). Every study was randomised and examiner-blind, and the allocation sequence was unknown during enrollment and treatment assignment, mitigating bias associated with the randomisation process. Each study was also analysed using the per-protocol population to assess the outcome of adhering to intervention, minimising bias associated with deviations from the intended interventions. Bias due to missing outcome data was addressed by availability of data for all, or the vast majority of, participants. Examiners were blinded to treatment and used credentialed clinical measures to assess efficacy, minimising bias in the measurement of the outcome domain. Finally, each study had a prespecified analysis plan that included results irrespective of outcome to mitigate bias in the selection of the reported result.
Discussion
Results of this meta-analysis confirm consistently greater plaque removal and gingivitis-reduction efficacy of O-R brushes relative to manual and sonic brushes. One factor potentially contributing to efficacy differences is brush head design. O-R brushes have a small, round head, similar to a prophy cup, which contours to the shape of each tooth. Manual toothbrushes typically have a large, rectangular shape, and sonic toothbrushes have preserved a more traditional head shape.
Additionally, for the first time this study demonstrates that the most advanced O-R model provides enhanced bleeding site reduction efficacy relative to traditional O-R brushes. The novel design of the iO O-R brush might contribute to its enhanced effectiveness vs other, “traditional” O-R toothbrushes with respect to transitions to gingival health and bleeding site reduction. The iO O-R toothbrush incorporates a linear magnetic drive system that directs energy to brush filaments tips—eliminating intrinsic losses of energy that are incurred with use of mechanical drive systems in earlier models of oscillating rotating brushes—inducing micro-vibrations at the site of plaque removal.12 The superiority of this brush vs manual28,29,50 and sonic30,31 brushes has already been demonstrated in studies of plaque and gingivitis reduction after as much as 6 months of use; the current results further confirm evidence of the iO brush as an effective oral health tool.
Notably, the relative percentage bleeding site reductions for O-R vs manual and sonic were greater than the respective relative percentage of plaque reduction at the same regions. A given relative reduction in plaque corresponded to a larger relative reduction in the number of bleeding sites. This is consistent with results of previous research suggesting that plaque toxicity may be more important than quantity. The species profile of bacterial plaque, which shows a characteristic, progingivitis shift as early as 24 hours after the cessation of oral hygiene, precedes and correlates with the onset of gingivitis symptoms.51 The pathogenic effect of plaque may be independent of total plaque mass due, at least in part, to lipopolysaccharides that are present on the uniquely problematic subsets of plaque bacteria.52
The results of this meta-analysis are consistent with those of multiple other systematic reviews and meta-analyses. Whilst some groups have reported little to no efficacy difference between O-R and sonic brushes, including high-frequency models, with respect to plaque or gingivitis reduction,53,54 a large body of independently conducted research supports the superior performance of O-R brushes vs sonic as well as manual brushes.8, 9, 10,14,16,17 The consistently lower plaque effects seen for manual toothbrushes vs electric toothbrushes illustrate that whilst a skilled user can achieve thorough plaque removal with a manual toothbrush, it is difficult to do in practice.7
A limitation of the RCTs included in this meta-analysis is the lack of double-blinding due to logistical challenges associated with concealing toothbrush identity. However, all trials were examiner-blinded. Another limitation is that every trial did not have a positive and negative control toothbrush. The fact that all trials were supported by a single manufacturer and the meta-analysis was not conducted in conjunction with a systematic review might be considered a potential limitation. However, access to participant-level data for each study not only was necessary to complete the set of analyses but also provided the advantage of producing distinctive assessments such as the transition-to-health segmentations. Risk of bias was deemed low for all studies using the Cochrane RoB2 assessment tool.19 All studies were randomised, controlled, and examiner-blinded and used credentialed research standards. The majority of studies were conducted at independent sites according to ICH/GCP standards. Findings for 22 of 26 total studies have been published in peer-reviewed journals,28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49 mitigating across-study risk of bias. All studies were analysed per a prespecified analysis plan using the per-protocol population to evaluate the effect of complying with intervention. The scale and rigour of the dataset supports its validity and reproducibility, and the clinical methods are validated. A core strength of these analyses is the large and diverse population, making the findings applicable to the broader global population.
The O-R brush examined in the current meta-analysis features an interactive app. The few studies to date that explored such apps suggest that they lead to brushing behaviour (eg, brushing coverage, time, pressure) and oral health improvements.55, 56, 57 Future research could further explore behaviour and health benefits of toothbrush apps. Another area for further investigation is regimen research. Whilst O-R electric brush technology provides significant advances in plaque removal, antibacterial dentifrice and rinse can inhibit plaque regrowth between brushing sessions to enhance plaque control.58,59
In conclusion, this meta-analysis shows that O-R toothbrushes provide significantly better plaque and gingivitis reduction and a faster transition to health than sonic or manual brushes. Relative to other O-R brushes, the most advanced O-R model produces a significantly greater rate of transition to gingival health and significantly greater reductions in number of bleeding sites and plaque scores.
Author contributions
All authors have made substantial contributions to the conception and design of the study. YZ and JG led data collection and analysis. All authors were involved in data interpretation, drafting the manuscript and revising it critically and have given final approval of the version to be published.
Funding
Procter & Gamble funded the analysis and medical writing assistance.
Conflict of interest
Drs Zou and Grender are employees of The Procter & Gamble Company. Dr Adam is an employee of Procter & Gamble Service GmbH. Dr Levin has done consulting work for The Procter & Gamble Company.
Acknowledgements
The authors are grateful to Marisa DeNoble Loeffler, MS, for medical writing assistance.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.identj.2023.06.009.
Appendix. Supplementary materials
REFERENCES
- 1.Chapple ILC, Mealey BL, Van Dyke TE, et al. Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium: consensus report of workgroup 1 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol. 2018;89(Suppl 1):S74–S84. doi: 10.1002/JPER.17-0719. [DOI] [PubMed] [Google Scholar]
- 2.Herrera D, Meyle J, Renvert S, Jin L, FDI Global Periodontal Health Project Task Team . FDI World Dental Federation; 2018. White paper on prevention and management of periodontal diseases for oral health and general health.https://fdiworlddental.org/sites/default/files/2020-11/gphp-2018-white_paper-en.pdf Available from: Accessed 5 May 2023. [Google Scholar]
- 3.Van der Weijden F, Slot D. Efficacy of homecare regimens for mechanical plaque removal in managing gingivitis a meta review. J Clin Periodontol. 2015;42:S77–S91. doi: 10.1111/jcpe.12359. [DOI] [PubMed] [Google Scholar]
- 4.Kurtzman GM, Horowitz RA, Johnson R, Prestiano RA, Klein BI. The systemic oral health connection: biofilms. Medicine (Baltimore) 2022;101(46):e30517. doi: 10.1097/MD.0000000000030517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bishop C. Time to take gum disease seriously: the societal and economic impact of periodontitis. The economist intelligence unit. Available from: https://eiuperspectives.economist.com/healthcare/time-take-gum-disease-seriously-societal-and-economic-impact-periodontitis. Accessed 18 April 2023.
- 6.FDI World Dental Federation. Sustainability in dentistry. Available from: https://www.fdiworlddental.org/sustainability-dentistry. Accessed 4 April 2023.
- 7.Ebel S, Blättermann H, Weik U, Margraf-Stiksrud J, Deinzer R. High plaque levels after thorough toothbrushing: what impedes efficacy? JDR Clin Trans Res. 2019;4(2):135–142. doi: 10.1177/2380084418813310. [DOI] [PubMed] [Google Scholar]
- 8.Elkerbout T, Slot D, Rosema N, Van der Weijden G. How effective is a powered toothbrush as compared to a manual toothbrush? A systematic review and meta-analysis of single brushing exercises. Int J Dent Hyg. 2020;18:17–26. doi: 10.1111/idh.12401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thomassen T, Van der Weijden FGA, Slot DE. The efficacy of powered toothbrushes: a systematic review and network meta-analysis. Int J Dent Hyg. 2022;20:3–17. doi: 10.1111/idh.12563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yaacob M, Worthington H, Deacon S, et al. Powered versus manual toothbrushing for oral health. Cochrane Database Syst Rev. 2014 doi: 10.1002/14651858.CD002281.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pitchika V, Pink C, Völzke H, Welk A, Kocher T, Holtfreter B. Long-term impact of powered toothbrush on oral health: 11-year cohort study. J Clin Periodontol. 2019;46(7):713–722. doi: 10.1111/jcpe.13126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Adam R. Introducing the Oral-B iO electric toothbrush: next generation oscillating-rotating technology. Int Dent J. 2020;70:S1–S6. doi: 10.1111/idj.12570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Delaurenti M, Ward M, Souza S, et al. The effect of use of a sonic power toothbrush and a manual toothbrush control on plaque and gingivitis. J Clin Dent. 2017;28(1 Spec No A):A1–A6. [PubMed] [Google Scholar]
- 14.Clark-Perry D, Levin L. Systematic review and meta-analysis of randomized controlled studies comparing oscillating-rotating and other powered toothbrushes. J Am Dent Assoc. 2020;151 doi: 10.1016/j.adaj.2019.12.012. 265-25.e6. [DOI] [PubMed] [Google Scholar]
- 15.Grender J, Adam R, Zou Y. The effects of oscillating-rotating electric toothbrushes on plaque and gingival health: a meta-analysis. Am J Dent. 2020;33:3–11. [PubMed] [Google Scholar]
- 16.van der Sluijs E, Slot DE, Hennequin-Hoenderdos NL, Valkenburg C, van der Weijden F. The efficacy of an oscillating-rotating power toothbrush compared to a high-frequency sonic power toothbrush on parameters of dental plaque and gingival inflammation: a systematic review and meta-analysis. Int J Dent Hyg. 2023;21(1):77–94 doi: 10.1111/idh.12597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van der Sluijs E, Slot DE, Hennequin-Hoenderdos NL, Valkenburg C, van der Weijden F. Dental plaque score reduction with an oscillating-rotating power toothbrush and a high-frequency sonic power toothbrush: a systematic review and meta-analysis of single-brushing exercises. Int J Dent Hyg. 2021;19:78–92. doi: 10.1111/idh.12463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6 doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 20.Lobene R, Weatherford T, Ross N, Lamm R, Menaker L. A modified gingival index for use in clinical trials. Clin Prev Dent. 1986;8(1):3–6. [PubMed] [Google Scholar]
- 21.Burke DL, Ensor J, Riley RD. Meta-analysis using individual participant data: one-stage and two-stage approaches, and why they may differ. Stat Med. 2017;36(5):855–875. doi: 10.1002/sim.7141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Riley RD, Lambert PC, Staessen JA, et al. Meta-analysis of continuous outcomes combining individual patient data and aggregate data. Stat Med. 2008;27:1870–1893. doi: 10.1002/sim.3165. [DOI] [PubMed] [Google Scholar]
- 23.Schwender H, Hosmer DW, Lemeshow S, May S. Applied survival analysis: regression modeling of time-to-event data. Stat Paper. 2012;53:247–248. [Google Scholar]
- 24.Borenstein M, Hedges LV, Higgins PT, Rothstein HR. John Wiley & Sons, Ltd; Chichester: 2009. Introduction to meta-analysis. [Google Scholar]
- 25.Rücker G, Schwarzer G. Ranking treatments in frequentist network meta-analysis works without resampling methods. BMC Med Res Methodol. 2015;15:58. doi: 10.1186/s12874-015-0060-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.R Core Team. R: a language and environment for statistical computing. Available from: https://www.R-project.org. Accessed 30 April 2023.
- 27.Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36:1–48. [Google Scholar]
- 28.Grender J, Goyal CR, Qaqish J, Timm H, Adam R. A 12-week randomized controlled trial comparing a novel electric toothbrush with an extra gentle brush head to a manual toothbrush for plaque and gingivitis reduction. Compend Contin Educ Dent. 2022;43(1):17–25. [PubMed] [Google Scholar]
- 29.Grender J, Goyal CR, Qaqish J, Timm H, Adam R. Gingival health effects with an oscillating-rotating electric toothbrush with micro-vibrations and a novel brush head designed for stain control: results from a 12-week randomized controlled trial. Am J Dent. 2022;35(5):219–226. [PubMed] [Google Scholar]
- 30.Goyal CR, Adam R, Timm H, Grender J, Qaqish J. A 6-month randomized controlled trial evaluating a novel smart-connected oscillating-rotating toothbrush versus a smart-connected sonic toothbrush for the reduction of plaque and gingivitis. Am J Dent. 2021;34:54–60. [PubMed] [Google Scholar]
- 31.Adam R, Goyal C, Qaqish J, Grender J. Evaluation of an oscillating-rotating toothbrush with micro-vibrations versus a sonic toothbrush for the reduction of plaque and gingivitis: results from a randomized controlled trial. Int Dent J. 2020;70:S16–S21. doi: 10.1111/idj.12569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Grender J, Goyal C, Qaqish J, Adam R. An 8-week randomized controlled trial comparing the effect of a novel oscillating-rotating toothbrush versus a manual toothbrush on plaque and gingivitis. Int Dent J. 2020;70:S7–15. doi: 10.1111/idj.12571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ccahuana-Vasquez R, Adam R, Conde E, et al. A 5-week randomized clinical evaluation of a novel electric toothbrush head with regular and tapered bristles versus a manual toothbrush for reduction of gingivitis and plaque. Int J Dent Hyg. 2019;17:153–160. doi: 10.1111/idh.12372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ccahuana-Vasquez R, Conde E, Cunningham P, Grender J, Goyal C, Qaqish J. An 8-week clinical comparison of an oscillating-rotating electric rechargeable toothbrush and a sonic toothbrush in the reduction of gingivitis and plaque. J Clin Dent. 2018;29:27–32. [PubMed] [Google Scholar]
- 35.Erbe C, Klees V, Ferrari-Peron P, et al. A comparative assessment of plaque removal and toothbrushing compliance between a manual and an interactive power toothbrush among adolescents: a single-center, single-blind randomized controlled trial. BMC Oral Health. 2018;18:130. doi: 10.1186/s12903-018-0588-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Adam R, Grender JM, Conde EL, et al. Superior long-term dental plaque reduction of a rechargeable oscillation-rotation toothbrush. J Dent Res. 2017;96 (Special Issue A):Abstr 877. [Google Scholar]
- 37.Li Z, He T, Li C, et al. A randomized 3-month clinical comparison of a power toothbrush to a manual toothbrush in the reduction of gingivitis. Am J Dent. 2016;29:193–196. [PubMed] [Google Scholar]
- 38.Ccahuana-Vasquez R, Conde E, Grender J, Cunningham P, Qaqish J, Goyal C. An eight-week clinical evaluation of an sscillating-rotating power toothbrush with a brush head utilizing angled bristles compared with a sonic toothbrush in the reduction of gingivitis and plaque. J Clin Dent. 2015;26(3):80–85. [PubMed] [Google Scholar]
- 39.Klukowska M, Grender JM, Conde E, Milleman KR, Milleman JL. Plaque reduction efficacy of an oscillating-rotating power brush with a novel brush head utilizing angled bristle tufts. Compend Contin Educ Dent. 2014;35(9):702–706. [PubMed] [Google Scholar]
- 40.Klukowska M, Grender J, Conde E, Ccahuana-Vasquez R, Goyal C. A randomized 12-week clinical comparison of an oscillating-rotating toothbrush to a new sonic brush in the reduction of gingivitis and plaque. J Clin Dent. 2014;25:26–31. [PubMed] [Google Scholar]
- 41.Klukowska M, Grender J, Conde E, Ccahuana-Vasquez R, Goyal C. A randomized clinical trial evaluating gingivitis and plaque reduction of an oscillating-rotating power brush with a new brush head with angled bristles versus a marketed sonic brush with self-adjusting technology. Am J Dent. 2014;27:179–184. [PubMed] [Google Scholar]
- 42.Klukowska M, Grender J, Conde E, Goyal C, Qaqish J. A six-week clinical evaluation of the plaque and gingivitis efficacy of an oscillating-rotating power toothbrush with a novel brush head utilizing angled CrissCross bristles versus a sonic toothbrush. J Clin Dent. 2014;25:6–12. [PubMed] [Google Scholar]
- 43.Büchel B, Reise M, Klukowska M, et al. A 4-week clinical comparison of an oscillating-rotating power brush versus a marketed sonic brush in reducing dental plaque. Am J Dent. 2014;27:56–60. [PubMed] [Google Scholar]
- 44.Klukowska M, Sharma NC, Grender JM, Conde E, Cunningham P, Qaqish J. Comparative anti-gingivitis efficacy of oscillation-rotation electric toothbrush vs manual toothbrush. J Dent Res. 2014;93 (Special Issue A):Abstr 1366. [Google Scholar]
- 45.Klukowska M, Grender JM, Conde E, Goyal CR. A 12-week clinical comparison of an oscillating-rotating power brush versus a marketed sonic brush with self-adjusting technology in reducing plaque and gingivitis. J Clin Dent. 2013;24:55–61. [PubMed] [Google Scholar]
- 46.Klukowska M, Grender JM, Goyal CR, Mandl C, Biesbrock AR. 12-week clinical evaluation of a rotation/oscillation power toothbrush versus a new sonic power toothbrush in reducing gingivitis and plaque. Am J Dent. 2012;25:287–292. [PubMed] [Google Scholar]
- 47.Klukowska M, Qaqish J, Grender JM, Rooney JE, Hoke PD, Cunningham P. Gingivitis reduction from a power toothbrush with novel brush head. J Dent Res. 2010;89 (Special Issue A):Abstr 3695. [Google Scholar]
- 48.Williams K, Rapley K, Haun J, et al. Comparison of rotation/oscillation and sonic power toothbrushes on plaque and gingivitis for 10 weeks. Am J Dent. 2009;22:345–349. [PubMed] [Google Scholar]
- 49.Goyal C, Qaqish J, He T, Grender J, Walters P, Biesbrock A. A randomized 12-week study to compare the gingivitis and plaque reduction benefits of a rotation-oscillation power toothbrush and a sonic power toothbrush. J Clin Dent. 2009;20:93–98. [PubMed] [Google Scholar]
- 50.Adam R, Erb J, Grender J. Randomized controlled trial assessing plaque removal of an oscillating-rotating electric toothbrush with micro-vibrations. Int Dent J. 2020;70:S22–S27. doi: 10.1111/idj.12568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Huang S, He T, Yue F, et al. Longitudinal multi-omics and microbiome meta-analysis identify an asymptomatic gingival state that links gingivitis, periodontitis, and aging. MBio. 2021;12 doi: 10.1128/mBio.03281-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Klukowska M, Haught JC, Xie S, et al. Clinical effects of stabilized stannous fluoride dentifrice in reducing plaque microbial virulence I: microbiological and receptor cell findings. J Clin Dent. 2017;28:16–26. [PubMed] [Google Scholar]
- 53.de Jager M, Rmaile A, Darch O, Bikker JW. The effectiveness of manual versus high-frequency, high-amplitude sonic powered toothbrushes for oral health: a meta-analysis. J Clin Dent. 2017;28:A13–A28. [PubMed] [Google Scholar]
- 54.El-Chami H, Younis A, Brignardello-Petersen R. Efficacy of oscillating rotating versus side-to-side powered toothbrushes on plaque and gingival index reduction: a systematic review. J Am Dent Assoc. 2021;152:115–126. doi: 10.1016/j.adaj.2020.10.002. e114. [DOI] [PubMed] [Google Scholar]
- 55.Erbe C, Klees V, Braunbeck F, et al. Comparative assessment of plaque removal and motivation between a manual toothbrush and an interactive power toothbrush in adolescents with fixed orthodontic appliances: a single-center, examiner-blind randomized controlled trial. Am J Orthod Dentofacial Orthop. 2019;155(4):462–472. doi: 10.1016/j.ajodo.2018.12.013. [DOI] [PubMed] [Google Scholar]
- 56.Thurnay S, Adam R, Meyners M. A global, in-market evaluation of toothbrushing behaviour and self-assessed gingival bleeding with use of app data from an interactive electric toothbrush. Oral Health Prev Dent. 2022;20:1–10. doi: 10.3290/j.ohpd.b2572911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tonetti MS, Deng K, Christiansen A, et al. Self-reported bleeding on brushing as a predictor of bleeding on probing: early observations from the deployment of an internet of things network of intelligent power-driven toothbrushes in a supportive periodontal care population. J Clin Periodontol. 2020;47(10):1219–1226. doi: 10.1111/jcpe.13351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Adam R, Grender J, Timm H, Qaqish J, Goyal CR. Anti-gingivitis and anti-plaque efficacy of an oral hygiene system: results from a 12-week randomized controlled trial. Compend Contin Educ Dent. 2021;42(9):e1–e4. [PubMed] [Google Scholar]
- 59.Zini A, Mazor S, Timm H, et al. Effects of an oral hygiene regimen on progression of gingivitis/early periodontitis: a randomized controlled trial. Can J Dent Hyg. 2021;55:85–94. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.