Abstract
Objective: The aim of this study was to examine the information-seeking behaviors (e.g., information resource usage patterns, access to types of sources and to medical libraries, and use of particular information technologies) of members in a primary care practice-based research network (PBRN) to inform future efforts supporting primary care practitioners in their daily care of patients.
Methods: Every primary care practitioner who was a member of the Kentucky Ambulatory Network—including family practitioners, general practitioners, nurse practitioners, and physician assistants—was surveyed. The cross-sectional survey included twenty-six questions to investigate the information-seeking behavior of primary care practitioners.
Results: The response rate was 51% (59 of 116). Most practitioners (58%) stated they sought information to support patient care several times per week, and most (68%) noted they do this while the patient waited. Many practitioners (40%) never or almost never perform literature searches from online sources such as MEDLINE, although 44% said they did so a few times per month. A significant correlation between use of online sources and use of print sources suggests that those who seek online information more frequently than those who do not also seek information from print sources frequently, and vice versa. Access to medical libraries was also reported as high.
Conclusions: Consistent with previous studies, the primary care practitioners in this rural PBRN reported more frequent use of print and interpersonal sources compared to online sources. There appeared to be, however, a clear difference between those practitioners who are more likely to seek information, regardless of format, and those who are less inclined. Future interventions will need to address such barriers as time, cost, and information-seeking skills.
INTRODUCTION
Supporting the information needs of primary care providers is critical to enhancing health in the United States, because Americans, particularly those in rural communities, rely heavily on them for health care [1–3]. Primary care has defining characteristics (e.g., first-contact, comprehensiveness, accessibility, integration of services, sustained partnerships with patients over time, and orientation toward communities or populations served) that result in a very high complexity of practice content and great diversity of practice settings [4–6]. Moreover, primary care is comprised of a number of health professions, including family physicians, general practitioners, nurse practitioners, and physician assistants, as well as obstetricians, gynecologists, and pediatricians. Thus, as implied by recent reports from the Institute of Medicine [7, 8], the breadth and complexity of information and knowledge required to deliver excellent primary care services means that health information professionals must use innovative approaches if they are to meet the needs of these clinicians. Specifically, these approaches should address the barriers to timely and accurate access to both patient-specific and knowledge-based information that is critical to quality care.
The aim of this study was to assess the information-seeking behaviors and preferences of clinicians in a primary care practice-based research network (PBRN; described further below). The authors examined issues such as primary care practitioners' information resource usage patterns, access or barriers to different types of sources and to medical libraries, and use of particular information technologies. We suggest that the results of our survey will inform future efforts in supporting primary care practitioners in their daily care of patients.
Information needs in primary care
Previous studies have examined information needs and information-seeking behaviors in various primary care settings [9–16], including use of the Internet [17, 18]. A common finding in many of these studies has been the primary care providers' preference for print, ready reference, and interpersonal sources such as colleagues. This preference may be due, as noted by Gorman, to the fact that the main goal of the clinician and patient is to improve the patient's health rather than seek more information, which leads to a certain tolerance of uncertainty and the need to make the best judgment with the information at hand [9].
It has also been shown that information needs, information seeking, and source preference are consistent between rural and nonrural primary care practitioners, although rural physicians have noted a lack of access to some sources [11]. Dorsch and others who have studied rural health professionals' information needs have described similar problems with access to information, noting such barriers as: lack of time, isolation, inadequate library access, lack of equipment, lack of skills, costs, and inadequate Internet infrastructure [12–14, 19].
Information overload is considered one of the key barriers to accessing the best evidence for decision making and effective knowledge updating and is being addressed through evidence-based medicine (EBM) methods. Therefore, access to, and use of, evidence-based information resources by practitioners is receiving increased attention. Studies have shown low rates of access and use of evidence-based information resources such as the Cochrane library among practitioners, and there is a general call for better means of accessing evidence by general practitioners [20, 21]. A more recent study of family practitioners has shown similar success rates between experienced and inexperienced searchers of EBM sources to answer clinical questions; however, the practical use of these sources have been questioned due to lengthy search times [22]. Given the inherent difficulties in EBM regarding the harvesting and processing of the vast amounts of available literature, EBM is also viewed as a critical research problem in medical informatics [23], with some calling for informatics specialists to explore new approaches to facilitating incorporation of EBM principles in computer-based clinical decision support systems [24].
In addition, concerns exist related to the use of, or limited access to, the Internet to support the information needs of practitioners. Although nearly ubiquitous, Internet use varies, as does quality of access. For instance, Moffat et al. have reported 92% of general practitioners had Internet access, but 86% said it was restricted to one computer [25]. Use of MEDLINE in rural Washington has been reported to be higher than expected, but print and interpersonal sources are still dominant [26]. A recent study suggested that, although the Internet is playing an increasingly important role in physicians' continuing education and delivery of care, the aforementioned barriers of time, information-seeking skills, and information overload remain key challenges [27].
Generally, there appears to be consensus that quality in primary care can be positively affected by better information services and related enabling technologies. To do this, however, implies the need for a clearer description of primary care practitioners' information-seeking behaviors to better direct these efforts. Networks of practices formed to specifically support research in primary care offer one window through which we can examine this special health information context.
Practice-based research networks (PBRNs)
Primary care PBRNs offer special contexts in which to address the information needs of primary care providers. The goal of these networks is to bring together frontline caregivers serving broad populations and to study and disseminate innovations aimed at improving the quality, efficiency, and/or safety of primary health care [28, 29]. Thus, PBRNs offer a unique “laboratory” for investigating primary care information needs and related problems in real-world practices serving a very broad array of patients in a variety of contexts. PBRNs can also provide an excellent vehicle for translating advances in health information services and research into practice, because the member practitioners tend to be open to innovation and their practices are good settings in which to test translation and dissemination strategies.
The Kentucky Ambulatory Network (KAN)
The Kentucky Ambulatory Network (KAN) is an emerging PBRN established in 2000. Its overarching missions are to advance knowledge and to promote best practices at the primary care level through collaborative research in appropriate settings and the translation of new knowledge into practice. In so doing, KAN seeks to broadly represent primary care practices in Kentucky, many of which are in rural communities. KAN is administered through the Department of Family Practice and Community Medicine at the University of Kentucky (UK) in Lexington. Most of its member clinicians are family practitioners located in central and eastern Kentucky, primarily in small private practices. KAN also includes a broad array of health services researchers and other academicians at UK and the University of Louisville (U of L).
At the time of our survey, KAN membership included 116 community-based clinicians at 68 practice sites scattered throughout central and eastern Kentucky, with 80% located in rural areas, based on US census definitions. KAN also included 37 university-based faculty members from UK and U of L, at the time of the survey. The 116 community-based clinicians included family physicians, general internists, pediatricians, a preventive medicine physician, nurse practitioners, and physician assistants.
A major goal of KAN has been to develop a practice-based research infrastructure. At present, KAN lacks an integrated informatics infrastructure to support its mission. Here, we refer to data-collection and management tools, such as an electronic medical record, as well as rapid access to high-quality evidence-based medical knowledge at the point of care, in clinician- and patient-friendly formats. Our need to develop such an infrastructure drove us to investigate the current state of informatics in our network [30], as well as the information-seeking preferences and behaviors of our clinician members.
METHODS
We used a cross-sectional design that employed surveys of primary care practitioners (including physicians, nurse practitioners, and physician assistants) to help determine their current attitudes, knowledge, and behaviors related to use of medical knowledge sources in the primary care setting. We excluded practitioners at academic centers to achieve a sample of practices more representative of the primary care practicing population in the state as a whole.
Following a review of the literature, a survey instrument was developed that included up to twenty-six questions primarily related to the knowledge and use of information resources, both online and in print, that might be used by practitioners in their day-to-day care of patients <http://www.mc.uky.edu/kan/currentresearchprojects.htm>. Feedback on wording of questions and overall design of the survey was solicited from UK Department of Family Practice faculty and staff, as well as other experts in survey design and research at UK.
The study protocol was approved by the UK Institutional Review Board. The KAN research nurse called each practice manager to alert them that surveys would be arriving via express mail. Surveys were then sent to all KAN community-based clinicians. A cover letter described the aims of the study, explained that response to the survey implied consent to participate, and assured participants that all individual responses would be kept confidential. Surveys were coded to track nonresponders. A follow-up mailing to nonresponders was done one month after the initial mailing. The project research assistant telephoned nonresponders approximately one month after the second mailing as the final attempt to increase the response rate.
Basic descriptive data were collected and analyzed. All statistical analyses were performed using SPSS v11.5.
RESULTS
Demographics
Of the 116 practitioner surveys sent, 59 were returned for a response rate of approximately 51%, an adequate response rate [31], particularly given the extremely limited time practitioners have for responding to surveys and the fact that many of these practitioners, by virtue of being KAN members, were already active in some form of research. A comparison of responders and nonresponders showed that they were similar in terms of types of practices and other demographic characteristics.
Approximately 60% of the respondents were male and 40% female. Thirty-five of all practitioner surveys (30%) were mailed to females, with 22 (63%) returned; 82 (71%) were sent to males, with 35 (43%) returned. Overall, 16 nurses or physician assistants (62%) sent their surveys back, whereas 41 physicians (46%) did. Most of the nurses were female (4 males and 22 females). Neither information about respondents' race or ethnicity nor information about respondents' ages was collected. Year of graduation from professional training was determined for physicians. The median graduation year was 1994, with a range of 1958 to 2001. The number of patients seen per week ranged from 25 to 270, with a mean of 106. The average number of hours spent caring for patients per week was 43, with a range of 0 to 80.
Use of and barriers to use of information resources in practices
As a general information-needs question, clinicians were asked how often they sought information from colleagues, print resources, or online resources (excluding drug dosing or drug interactions information) to care for their patients. Fifty-eight percent stated they did this several times per week, 18% daily, 22% rarely, and 2% never. When asked whether they did this while a patient waited, 68% said yes and 32% no. Also, respondents were asked to rank, from 1 to 3, their main barriers to seeking health information. The number one barrier for most was lack of time (76%); the top three other common barriers were cost (33% of respondents), format of information sources (22% of respondents), and information-seeking skills (25% of respondents).
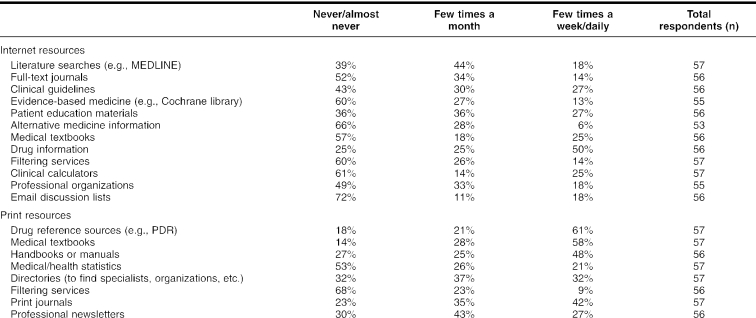
Table 1 shows the frequency of use of various Internet and print resources. The results in this table reveal an overall pattern of moderate online information resource usage as compared to print resources, perhaps due to the barriers mentioned above. As noted in the studies cited earlier, the preference for ready reference and interpersonal sources remains high with primary care practitioners. Use of EBM resources, as well as alternative medicine sources, appears fairly low, however.
Table 1 Information sources used by primary care practitioners
A paired samples t test was conducted to measure the relationship between practitioner use of print and online sources. Data were treated as ordinal (Never = 1, Almost never = 2, Few times a month = 3, Few times a week = 4, and Daily = 5), and responses to use of each resource were averaged for each respondent. The analysis revealed a statistically significant relationship (t(56) = −4.66; P < 0.0001; two-tailed) between seeking information from print resources and seeking information from online sources, with a significant positive correlation between the two types of sources (0.327; P < 0.013). In other words, individuals who seek information more frequently (that is, whose average responses for each source are closer to 5) from online sources also sought information more frequently from print sources. The inverse was true for those who sought information less frequently (response averages closer to 1) from either print or electronic sources. Chi-square analyses did not reveal statistically significant associations between practitioners' date of graduation from most recent medical education and use of either electronic or print resources.
Approximately 48% of practitioners stated they had access to a small medical library, 46% to a hospital library, and 21% to a university medical library. About 14% said they had no immediate medical library access. More than 55% stated they could access a library via the Internet; 57% of respondents reported having access to 2 or more types of medical libraries; and 29% had access to just 1 type. Thirty-three percent said they used the library sometimes, 28% frequently, 21% rarely, and 7% never.
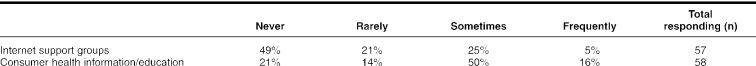
Approximately 60% of practitioners reported having an email account, and 40% did not. When asked if they believed that the use of email to communicate with patients enhanced medical practice, 34% agreed, 7% strongly agreed, 24% disagreed, 9% strongly disagreed, and 27% said they did not know. Also, 52% said that patients often discussed with them information they received from the Internet, 47% said this seldom occurred, and 2% said never. A majority (59%) of practitioners felt that patients who sought health information via the Internet were more informed than patients who did not, 38% said they were about the same, and 3% said they seemed less informed. When asked how often (never, rarely, sometimes, frequently) they prescribed particular Internet resources (either Internet support groups or consumer health education information) to patients, practitioners answered as shown in Table 2.
Table 2 Frequency of prescribing Internet health resources to patients
DISCUSSION
Our study showed that primary care practitioners in a largely rural PBRN reported that they did not use online information resources as much as print resources. However, the frequency of seeking information was fairly high (particularly considering that the question asked respondents to exclude when they sought information on drug dosing or interactions), and it was encouraging that primary care providers stated they had information needs arising during patient visits that they felt they could satisfy using a variety of sources, while the patient waited. Of course consistent with the studies noted earlier, time, cost, and skills emerged as major barriers to seeking information, but the respondents in our study reported a fair level of use of available resources.
Despite increased availability of EBM-related resources, however, few practitioners stated they used such resources. Our data did not indicate the reasons for this, but we might speculate that it could be the result of a general lack of awareness of user-friendly sources or that there was not strong agreement about the importance of EBM in the day-to-day care of patients. The study conducted by Byrnes et al. showed that, prior to a training intervention, 43% of participants believed EBM to be important in providing optimum care, but the number jumped to 79% immediately following the intervention and stayed about the same (78%) three months later [32]. Also, the same study showed an increase in participants' self-assessed information-seeking behavior, such as increased confidence when searching MEDLINE or increased frequency of searching the Internet for work-related information. A study conducted with rural physicians in Canada also showed an improvement in the frequency of use of the Internet to address patient-related information needs following a training intervention [33]. These studies suggest that training and education to improve practitioners' awareness and efficacious use of Internet-based knowledge will likely continue to be a fruitful area for research and interventions.
Of interest in our study was that there appeared to be two groups of information seekers: those who sought information from more sources and more frequently and those who pursued information less frequently, regardless of the source, including both print and online formats. Unfortunately, the data from this survey did not afford the opportunity to learn more about the differences between these two groups. For instance, individual information-seeking style could be an indicator of one's proclivity to seek information not readily available. As noted by Cullen [34], a practitioner's cognitive style or self-image as a health professional might determine the types of sources sought (e.g., whether one might seek out scientific literature as opposed to summaries of that literature).
Patient-oriented Internet resources were not recommended frequently by the practitioners in our study. Yet, given the demands of the consumer health movement, individuals might feel compelled to seek information related to doctor visits to be more informed participants in their own care. The number of Internet searches related to health has increased astoundingly over the past years, and evidence shows that many do so either before or following a visit with their doctors [35]. Our study showed that more than half of the clinicians reported that most of their patients discussed information obtained from the Internet with them and that most clinicians perceived these patients to be more informed than others. To help their patients find and effectively use quality information, primary care physicians need to become more familiar with what their patients are using to inform their health-related decisions.
CONCLUSIONS
The critical challenges implied by the results of our study require innovative approaches to enhancing access to information resources. The PBRN examined in this study is one of 111 primary care PBRNs in the United Sates as of July 2004 [36]. Because by definition PBRNs are designed to facilitate research to further knowledge of primary care practice, they offer a particularly interesting context to design and evaluate new models for information services.
As one possibility, we propose a tailored or individualized approach to enhancing information seeking and use in primary care. For instance, we know that various practitioners noted a lack of knowledge about available information resources, as well as the skills to access them successfully. Thus, a series of brief, individualized training sessions (designed in conjunction with health sciences librarians as part of an outreach program) for practitioners could help develop information-seeking skills and, ultimately, lead to an increased sense of efficacy in information seeking. As noted previously, similar interventions have been proved to be effective. Individualized training might also address barriers to use that are more fundamental, such as improved understanding of EBM principles and resources while taking into account an individual practitioner's cognitive style and self-image.
Improving clinicians' access to information and their competence to use, find, and apply evidence-based knowledge in their practices will have a blunted impact without attention to motivational factors. These factors can be addressed through establishing payment-for-performance programs currently being explored by large health care purchasers and payers and/or through requiring clinicians to demonstrate the application in their practices of activities that are evidence based to improve quality. Licensure and certification sanctions can drive these requirements [37]. The American Board of Family Practice is instituting just such a requirement for maintaining board certification [38].
Certainly, technology offers many promises for enhancing access and use of various knowledge-based sources. The lack of knowledge about sources or the significant time it takes to seek answers from multiple sources, each with its own interface and architecture, can be major barriers. Thus, tools that integrate source access into a single interface should be further investigated for less time to be spent negotiating any particular resource. That is, a more standardized interface would allow access to multiple, disparate sources without having to have special skills to search and synthesize the information from each. Such services might be informed by existing outreach services provided by medical libraries, particularly because access to and use of a medical library of some sort was relatively strong in our study. Moreover, the fact that many say they can access a library via the Internet is encouraging for developing or enhancing information access services.
Footnotes
* Support for this project comes from the Agency for Healthcare Research and Quality (AHRQ) grant number R21 HS13487-01.
Contributor Information
James E. Andrews, Email: jandrews@cas.usf.edu.
Kevin A. Pearce, Email: kpearce@email.uky.edu.
Carol Ireson, Email: clires@uky.edu.
Margaret M. Love, Email: mlove@email.uky.edu.
REFERENCES
- Green LA, Fryer GE, Yawn BP, Lanier D, and Dovey SM. The ecology of medical care revisited. N Engl J Med. 2001 Jun; 344(26):2021–5. [DOI] [PubMed] [Google Scholar]
- Fryer GE, Green LA, Dovey SM, and Phillips RI. The United States relies on family physicians unlike any other specialty. Am Fam Physician. 2001 May; 63(9):1669–703. [PubMed] [Google Scholar]
- Council on Graduate Education. Physician distribution and health care challenges in rural and inner-city areas. 10th report. US Department of Health and Human Services, 1998. [Google Scholar]
- Declaration of Alma-Ata. International conference on primary health care. Alma-Ata,. USSR; 6–12 Sep 1978. [Google Scholar]
- Institute of Medicine. Primary care: America's health in a new era. Donalson MS, Yordy KP, Lohr KN, Vanselow NA, eds. Washington, DC: National Academies Press, 1996. [PubMed] [Google Scholar]
- US Department of Health and Human Services. Ambulatory care visits to physician offices, hospital outpatient departments and emergency departments: United States 1997. Vital and Health Statistics 1999;series 13:no. 143. [PubMed] [Google Scholar]
- Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington, DC: National Academies Press, 2001. [PubMed] [Google Scholar]
- Kohn L, Corrigan J, and Donaldson ME. To err is human: building a safer health system. Washington, DC: National Academies Press, 2000. [PubMed] [Google Scholar]
- Gorman P. Information seeking of primary care physicians: conceptual models and empirical studies. In: Wilson TD, Allen DK, eds. Information behaviour: proceedings of the second international conference on research in information needs, seeking and use in different contexts. Sheffield and London, UK: Taylor Graham, 13/15 Aug 1998. [Google Scholar]
- Gorman PN. Information needs of physicians. J Am Soc Inf Sci. 1995 Dec; 46(10):729–36. [Google Scholar]
- Gorman P.. Information needs in primary care: a survey of rural and nonrural primary care physicians. Medinfo. 2001;10(Pt1):338–2. [PubMed] [Google Scholar]
- Dorsch JL. Information needs of rural health professionals: a review of the literature. Bull Med Libr Assoc. 2000 Oct; 88(4):346–54. [PMC free article] [PubMed] [Google Scholar]
- Dee C, Blazek R. Information needs of the rural physician: a descriptive study. Bull Med Libr Assoc. 1993 Jul; 81(3):259–64. [PMC free article] [PubMed] [Google Scholar]
- Dawes M, Sampson U. Knowledge management in clinical practice: a systematic review of information seeking behavior in physicians. Int J Med Inf. 2003 Aug; 71(9):9–15. [DOI] [PubMed] [Google Scholar]
- Haug JD. Physicians' preferences for information sources: a meta-analytic study. Bull Med Libr Assoc. 1997 Jul; 85(3):223–32. [PMC free article] [PubMed] [Google Scholar]
- Ely JW, Levy BT, and Hartz A. What clinical information resources are available in family practice? J Fam Pract. 1999 Feb; 48(2):135. [PubMed] [Google Scholar]
- Cullen RJ. In search of evidence: family practitioners' use of the Internet for clinical information. J Med Libr Assoc. 2002 Oct; 90(4):370–9. [PMC free article] [PubMed] [Google Scholar]
- Westberg EE, Miller RA. The basis for using the Internet to support the information needs of primary care. J Am Med Inform Assoc. 1999 Jan; 6(1):6–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundeen GW, Tenopir C, and Wemager P. Information needs of rural health care practitioners in Hawaii. Bull Med Libr Assoc. 1994 Apr; 82(2):197–205. [PMC free article] [PubMed] [Google Scholar]
- Carney PA, Poor DA, Schifferdecker KE, Gephart DS, Brooks B, and Nierenberg DW. Computer use among community-based primary care physician preceptors. Acad Med. 2004 Jun; 79(6):580–90. [DOI] [PubMed] [Google Scholar]
- Young JM, Ward JE. General practitioners' use of evidence databases. Med J Aust. 1999 Jan; 170(2):56–8. [PubMed] [Google Scholar]
- Schwartz K, Northrup J, Israel N, Crowell K, Lauder N, and Neale AV. Use of on-line evidence-based resources at the point of care. Fam Med. 2003 Apr; 35(4):251–6. [PubMed] [Google Scholar]
- Bakken S. An informatics infrastructure is essential for evidence-based practice. J Am Med Inform Assoc. 2001 May; 8(3):199–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sim I, Gorman P, Greenes RA, Haynes RB, Kaplan B, Lehmann H, and Tang PC. Clinical decision support systems for the practice of evidence-based medicine. J Am Med Inform Assoc. 2001 Nov; 8(6):527–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffat MO, Moffat KJ, and Cano V. General practitioners and the Internet: a questionnaire survey of Internet connectivity and use in Lothian. Health Bull. 2001 Mar; 59(2):120–6. [PubMed] [Google Scholar]
- Chimoskey SJ, Norris TE. Use of MEDLINE by rural physicians in Washington State. J Am Med Inform Assoc. 1999 Jul; 6(4):332–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett NL, Casebeer LL, Kristofco RE, and Strasser SM. Physicians' Internet information-seeking behaviors. J Contin Educ Health Prof. 2004 Winter; 24(1):31–8. [DOI] [PubMed] [Google Scholar]
- Nutting PA, Beasley JW, and Werner JJ. Practice-based research networks answer primary care questions. JAMA. 1999 Feb; 281(8):686–8. [DOI] [PubMed] [Google Scholar]
- AHRQ. Primary care practice-based research networks. [Fact sheet, Jun 2001]. AHRQ publication No. 01-P020. Rockville, MD: Agency for Healthcare Research and Quality. (Available from: <http://www.ahrq.gov/research/pbrnfact.htm>. [cited 4 Nov 2003].). [Google Scholar]
- Andrews JE, Pearce K, Ireson C, Sydney S.. Current state of information technology use in a U.S. primary care practice-based research network (PBRN) Inform Prim Care. 2004;12(1):11–8. doi: 10.14236/jhi.v12i1.103. [DOI] [PubMed] [Google Scholar]
- Babbie E. The practice of social research. 9th ed. Stamford, CT: Wadsworth, 2001. [Google Scholar]
- Byrnes JA, Kulick TA, and Schwartz DG. Information-seeking behavior changes in community-based teaching practices. J Med Libr Assoc. 2004 Jul; 92(3):334–40. [PMC free article] [PubMed] [Google Scholar]
- Kronick J, Blake C, Munoz E, Heilbrunn L, Dunikowski L, and Milne WK. Improving on-line skills and knowledge: a randomized trial of teaching rural physicians to use on-line medical information. Can Fam Physician. 2003 Mar; 49:312–7. [PMC free article] [PubMed] [Google Scholar]
- Cullen RJ. In search of evidence: family practitioners' use of the Internet for clinical information. J Med Libr Assoc. 2002 Oct; 90(4):370–9. [PMC free article] [PubMed] [Google Scholar]
- Case DO, Johnson JD, Andrews JE, and Allard S. From two-step flow to the Internet: the changing array of sources for genetics information seeking. JASIST. 2004 Jun; 55(8):660–9. [Google Scholar]
- National Program Office, Department of Family Medicine, University of Colorado Health Sciences Center. Prescription for health. [Web document]. Aurora, CO: The Office. [rev. 7 Dec 2004; cited 12 Dec 2004]. <http://www.prescriptionforhealth.org>. [Google Scholar]
- Donen N. Mandatory practice self appraisal: moving toward outcomes-based continuing education. J Eval Clin Pract. 1999 Aug; 5(3):297–303. [DOI] [PubMed] [Google Scholar]
- American Board of Family Practice. About the maintenance of certification program for family physicians. [Web document]. Lexington, KY. <https://www.abfp.org/MOC/about.aspx>. [Google Scholar]