Abstract
Denture plaque, a biofilm that develops on denture surfaces, could contribute to many oral and systemic afflictions. Hence, a quantitative assessment of denture plaque is important to evaluate the denture hygiene of denture wearers, particularly to prevent plaque biofilm-associated diseases. The aim of this systematic review, therefore, was to review and summarize the visual denture hygiene assessment methods using denture plaque indices and with planimetries published in the literature. English language studies published up to March 2022 in four electronic databases, PubMed, Medline, Embase, and Cochrane Library, were searched, followed by a manual search of Google Scholar by two assessors. The review followed Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) whenever possible. Details of the visual assessment methods, including the types of denture assessed, its materials and its surfaces, as well as the use of a disclosing agent, were the main outcomes. Of 492 screened studies, 74 were included per the inclusion and exclusion criteria. Of these, 60 studies utilized various denture plaque indices while 18 used planimetries. 43 out of 60 studies with indices and 17 out of 18 studies with planimetries used disclosing agents for visual evaluation of plaque. A total of 21 indices were described in the included studies, of which seven graded a divided denture surface, while the remainder graded entire denture surface. Of the 18 planimetric assessments, one study quantified squares of the disclosed plaques on denture images, 16 studies quantified such pixels with computer programs, and a single study quantified points, pixels, and contour of plaque areas. In summary, denture plaque indices appear to be popular in denture plaque assessment due to their simplicity. Computerized planimetric assessment, though more time-consuming, provides a more accurate assessment of plaque load as it is less prone to subjectivity and assessor errors.
Keywords: Denture hygiene, Denture cleanliness, Denture plaque, Plaque biofilm, indices, Planimetry
Introduction
Dental prostheses such as removable partial and complete dentures are still widely used to replace missing teeth, particularly in the developed world, mainly due to the higher financial outlay of various dental implants. The former exogenous, acrylic, or metallic, appliances are well known to harbor denture plaque biofilm in retentive areas, and these are likely to contribute to afflictions such as Candida-associated denture stomatitis, and caries and periodontitis of the abutment teeth.1, 2, 3, 4 Denture plaque is essentially a biofilm comprising a complex aggregate of micro-organisms and their metabolites that accumulate on denture surfaces.2
A positive correlation between the amount of denture plaque biofilm and the severity of denture stomatitis is well established.5,6 Furthermore, denture plaque aggregates particularly in debilitated hospitalized individuals are known to correlate well with potentially fatal systemic complications such as aspiration pneumonia.1,7,8 Meanwhile, most denture wearers, especially in developing countries, have poor knowledge of denture hygiene.9 Hence, over the years, many workers have attempted to either quantitatively or semi-quantitatively assess denture hygiene to educate and motivate patients in a visually impressive manner and also to develop clinical correlates of plaque-related diseases.10,11
The presence and distribution of plaque biofilm on the denture surfaces could be assessed using either the naked eye with denture plaque assessment indices or the latter with planimetries.12 Those indices utilize a calibrated assessor for semi-quantitative grading of denture plaque biofilm. The assessor usually assesses the area of denture surfaces covered with plaque biofilm using a disclosing agent.12 More recently, however, planimetries have been employed to provide a better quantitative assessment of plaque biofilm-covered denture surfaces. Computer programs are usually used in planimetric analyses to provide a quantitative indication of the area with plaque deposition. In general, denture plaque indices are also helpful to motivate individual patients to improve their denture hygiene while the latter, more sensitive planimetric assessment methods can be used in research settings to compare the relative efficacy of denture cleansing agents and methods.
Over the last few decades, many indices and planimetries evaluating denture hygiene for clinical as well as research purposes have been used and these have been reviewed in an attempt to obtain a global oversight on denture plaque levels,2 denture hygiene,13 and denture hygiene practices.14 However, to the best of our knowledge, there is no recent comprehensive review of the subject and the current review was undertaken to provide a contemporaneous, critical account of the visual denture hygiene assessment methods described in the literature.
Methods
The review question “Which visual assessment methods have been used to measure denture plaque biofilm in previous studies?” was specifically set using a Population, Intervention, Control, and Outcomes (PICO) model (Table 1). This review was registered on the PROSPERO international prospective register of systematic reviews (CRD42023390370). The review followed the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).
Table 1.
The search strategy and tools for risk of bias assessment used in the study
| Population | Denture wearers |
| Intervention | Visual assessment methods of denture plaque-deposited area |
| Comparison/ Control | Comparison to clean or new dentures |
| Outcomes | Denture plaque deposited area |
| Searched terms | (“Denture hygiene” OR “denture cleanliness” OR “denture plaque” OR “denture care”) AND (“assessment” OR “observation” OR “study” OR “investigation” OR “score” OR “scale” OR “index” OR “method” OR “model” OR “way”) |
| Database | PubMed, Medline, Embase, and Cochrane Library |
| Filter | No filter applied |
| Search date | The most recent search was performed on March 31, 2022. |
| Risk of Bias Assessment Tools | The National Institutes of Health (NIH) quality assessment tools for controlled intervention studies/observational cohort and cross-sectional studies/before-after (Pre-Post) study with no control group/case-control studies/case series |
Literature Search
The literature in four electronic databases, PubMed, Medline, Embase, and Cochrane Library, was searched by two assessors (KMT and AWKY) independently using a defined search strategy (Table 1). Relevant references from the selected studies were retrieved and an additional hand-search via Google Scholar was performed by the same assessors to identify other potentially eligible studies. The most recent search was performed on March 31, 2022. Abovementioned two independent assessors initially screened through the titles and abstracts of retrieved studies. Duplicates of studies were removed. The shortlisted studies were then screened with full-text analysis. The inclusion criteria for this systematic review were as follows: English language studies; visual assessment of denture hygiene on removable partial or complete dentures; original clinical studies. Simulated in vitro studies, case reports and short communications, studies without statistical analysis as well as studies using assessment methods other than visual assessments were excluded. Disagreements between assessors were solved by discussion for a consensus.
Data collection, extraction, and analysis
Data extraction was performed independently by the same assessors using a pre-defined data extraction template. Inter-assessor conflicts were discussed to reach a consensus. From the materials and methods section of each selected study, details of the denture hygiene assessment including the examined samples whether the actual denture or its images, complete or partial or both dentures, maxillary or mandibular or both dentures, types of denture materials, the use of a disclosing agent, and the assessed denture surfaces were extracted (Table 2 and 3). Furthermore, details of the denture plaque indices and planimetric assessment methods were also extracted (Table 4). Any missing information was secured as much as possible by emailing the corresponding author. The screening process and data extraction were performed using Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia). The methodological quality of selected studies was assessed by an assessor (KMT) using National Institutes of Health (NIH) Study Quality Assessment Tools for respective study types.
Table 2.
A list of the 74 reviewed studies. (*studies under the same project of Zenthofer et al. 201434. #studies under the same project of Sloane et al.32)
| No. | Year | Authors | Content of study/ Purpose | Visual Assessment tools | Name of tools/studies used and referred | Examined sample (Denture/Image) | Profile of dentures assessed | Disclosing Materials (brands/ compound) | Denture surface(s) assessed |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 1970 | Budtz-Jorgensen and Bertram4 | Relationship between denture cleanliness and denture stomatitis | Index | Budtz-Jorgensen and Betram 19704 | Denture | Maxillary | Proflavine-monosulfate in 3.0 % aqueous solution | Fitting surface |
| 2 | 1977 | Budtz-Jorgensen and Kelstrup 45 | The efficiency of denture cleansers (enzymes) | Index | Budtz-Jorgensen and Betram 19704 | Denture | Maxillary | Proflavine-monosulfate in 3.0 % aqueous solution | Fitting surface |
| 3 | 1977 | Budtz-Jorgensen56 | Efficacy of enzymatic dissolvent tablet for prevention of denture plaque | Index | Budtz-Jorgensen 197756 | Image | Maxillary | Proflavine-monosulfate in 3.0 % aqueous solution | Fitting surface |
| 4 | 1978 | Budtz-Jorgensen and Knudsen67 | Efficacy of brushing with chlorhexidine or Steradent for prevention of denture plaque | Index | Budtz-Jorgensen 197756 | Image | Maxillary | Proflavine-monosulfate in 3.0 % aqueous solution | Fitting surface |
| 5 | 1981 | Abelson et al.78 | The efficiency of commercial denture cleansers | Index | Abelson et al.198178 | Denture | Any | Trace dye, The Lorvic Co. St. Louis, MO | All surfaces including teeth |
| 6 | 1982 | Ambjørnsen et al.53 | Additive index for denture plaque accumulation | Index | Ambjørnsen et al. 198253 | Denture | Maxillary | No disclosing | Fitting surface |
| 7 | 1982 | Ghalichebaf et al.68 | Effectiveness of commercial immersion-type denture cleansers | Planimetry-square counting | Square counting | Image | Maxillary | 5.0% erythrosine | Fitting surface |
| 8 | 1982 | Tarbet et al.83 | Relationship between denture hygiene and mucosal health | Index | Tarbet et al. 198283 | Denture | Maxillary | FD&C Red No. 3 | Fitting surface |
| 9 | 1982 | Augsburger and Elahi84 | Cleansing efficiency of soap-type denture cleanser | Index | Augsburger and Elahi 198284 | Denture | Maxillary | FD&C Red No. 3 (erythrosine) Lorric Corp., St. Louis, Mo. | All surfaces including teeth |
| 10 | 1983 | Budtz-Jorgensen et al.15 | Efficacy of protease enzyme denture cleansers (Alcalase) | Index | Budtz-Jorgensen et al. 198315 | Image | Maxillary | Proflavine-monosulfate in 3.0 % aqueous solution | Fitting surface |
| 11 | 1983 | Poulsen et al.16 | Evaluation of two methods of denture plaque scorings | Index | Budtz-Jorgensen et al. 198315 | Image | Maxillary | Proflavine-monosulfate in 3.0 % aqueous solution | Fitting surface |
| 12 | 1984 | Ambjørnsen et al.17 | To compare the reproducibility and reliability of different denture plaque scorings | Index | Budtz-Jorgensen 197756 | Image | Maxillary | Proflavine-monosulfate in 3.0 % aqueous solution | Fitting surface |
| Schubert and Schubert's PHI86 | |||||||||
| Ambjørnsen et al. 198253 | |||||||||
| 13 | 1986 | Murray et al.18 | Relationship between the abrasivity and cleaning power of the dentifrices-type denture cleansers | Index | Murray et al. 198618 | Denture | Both | 1.0% solution of fluorescein | All surfaces including teeth |
| 14 | 1987 | Schou et al.54 | Relationship between oral hygiene, denture plaque, and stomatitis | Index | Armbjornsen et al. 198253 | Denture | Maxillary | No disclosing | Fitting surface |
| 15 | 1990 | Cardash et al.19 | Method of monitoring denture hygiene | Index | Tarbet et al. 198283 | Image | Both | Red Cote, J.O. Butler. Co. Chicago III | Fitting surface |
| 16 | 1990 | Hoad-Reddick et al.82 | Denture cleanliness in the elderly population | Index | Hoad-Reddick et al. 199082 | Denture | Both or any | No disclosing | All surfaces including teeth |
| 17 | 1995 | McCabe et al.20 | Efficacy of two soaking denture cleansers | Index | McCabe et al. 199520 | Denture | Not mentioned | FDC blue 1, 0.25% in deionized water | All surfaces including teeth |
| 18 | 1996 | Jeganathan et al.21 | Clinically viable denture hygiene index | Index | Jeganathan et al. 199621 | Denture | Maxillary | FD&C Red No. 3 (erythrosine) | Fitting surface |
| 19 | 1996 | McCabe et al.22 | Method for denture plaque scoring | Index | McCabe et al. 199520 | Denture | Both | FDC blue 1, 0.25% in deionized water | All surfaces including teeth |
| 20 | 1996 | Keng and Lim23 | Denture plaque distribution and effectiveness of a perborate-containing denture cleanser | Index | Modified Quigley-Hein Index23 | Image | Both | Red Cote, J.O. Butler. Co. Chicago III | All surfaces including teeth |
| 21 | 1997 | Jeganathan et al.24 | Relationship between denture hygiene habits, cleanliness, wearing behavior, and stomatitis | Index | Budtz-Jorgensen and Betram 19704 | Denture | Maxillary | FD&C Red No. 3 (erythrosine) | Fitting surface |
| 22 | 2000 | Sheen and Harrison25 | A new method for assessing plaque levels on dentures by using digital imaging | Planimetry | Not mentioned the program used | Image | Maxillary | Fluorescent dye (Spectrum Chemical Mfg Corp, Gardena, Calif.) | All surfaces including teeth |
| Index | Augsburger and Elahi 198284 | Denture | Maxillary | ||||||
| 23 | 2002 | Kulak-Ozkan et al.26 | Relationship between oral hygiene habits, denture cleanliness, and stomatitis | Index | Budtz-Jorgensen and Betram 19704 | Denture | Maxillary | Proflavine-monosulfate in 0.3% aqueous solution | Fitting surface |
| 24 | 2004 | Paranhos et al.10 | Comparison of different denture plaque assessments methods | Planimetry | Image Tool 2.02 Software | Image | Maxillary | An aqueous solution of 5.0% erythrosine (Art. 1355 Erythrosine, E. Merck, Darmstadt, Germany) | Fitting surface |
| Planimetry | Digital planimeter | Image | Maxillary | ||||||
| Planimetry-point counting | Grid with equidistant points | Image | Maxillary | ||||||
| Paper weighing | NOT visual method | - | - | ||||||
| 25 | 2004 | Andrucioli et al.69 | To evaluate the effectiveness of denture cleansing paste | Planimetry | Image Tool 2.02 Software | Image | Maxillary | 1.0% sodium fluorescein | Fitting surface |
| 26 | 2005 | Kanli et al.27 | Relationship between oral hygiene habits, denture cleanliness, and stomatitis | Index | Schubert and Schubert's PHI86 | Denture | Maxillary | 5.0% erythrosine dye solution | Fitting surface |
| 27 | 2006 | Montal et al.55 | To assess oral (denture) hygiene, and treatment needs of the geriatric institution | Index | Montal et al. 200655 | Denture | Any | No disclosing | All surfaces including teeth |
| 28 | 2006 | De Visschere et al.28 | Oral hygiene of the elderly in long-term care institutions | Index | Augsburger and Elahi 198284 | Denture | Any | Methylene blue disclosing solution | Fitting and polished surfaces |
| 29 | 2006 | Dikbas et al.57 | Investigation of denture cleanliness | Index | Hoad-Reddick et al. 199082 | Denture | Both | No disclosing | All surfaces including teeth |
| 30 | 2007 | Fernandes et al.70 | Comparison of efficacy of three denture brushes | Planimetry | Adobe Photoshop 5.5 software | Image | Both | An aqueous solution of 1.0% neutral red | All surfaces including teeth |
| 31 | 2007 | Paranhos et al.29 | Distribution of biofilm on internal and external surfaces of the denture | Index | Paranhos et al. 200729 | Image | Maxillary | 1.0% neutral red solution; School of Pharmaceutical Sciences, University of Sao Paulo, Brazil | All surfaces including teeth |
| 32 | 2007 | Paranhos et al.30 | Effect of mechanical and chemical denture cleansing methods | Planimetry | Image tool 2.02 + Adobe Photoshop software 5.4 | Image | Maxillary | 1.0% neutral red solution; School of Pharmaceutical Sciences, University of Sao Paulo, Brazil | Fitting surface |
| Index | Paranhos et al.2006 | ||||||||
| 33 | 2007 | Salles et al.71 | To compare and correlate denture plaque after brushing, associated with specific paste and soap | Planimetry | Image Tool 2.0 Software | Image | Not mentioned | 1.0% neutral red solution; School of Pharmaceutical Sciences, University of Sao Paulo, Brazil | Fitting surface |
| 34 | 2009 | Coulthwaite et al.12 | To compare currently available visual and planimetric plaque measurement | Index | McCabe et al. 199520 | Image | Both | Methylene blue disclosing solution (FDC Blue #1, 0.25% in deionized water) | All surfaces including teeth |
| Planimetry | Adobe Photoshop (version 7; Adobe Systems Inc.) | Image | |||||||
| Index | Augsburger and Elahi 198284 | Image | |||||||
| 35 | 2010 | Paranhos et al.31 | Evaluation of three denture hygiene indices | Planimetry | Image Tool 2.02 Software | Image | Maxillary | 5.0% erythrosine aqueous solution | Fitting surface |
| Index | Schubert and Schubert's PHI86 | ||||||||
| Index | Jeganathan et al. 199621 | ||||||||
| Index | Budtz-Jorgensen 197756 | ||||||||
| 36 | 2010 | Souza et al.72 | Domestic use of disclosing solution for denture hygiene | Planimetry | Image Tool 2.02 Software | Image | Maxillary | 1.0% neutral red solution; School of Pharmaceutical Sciences, University of Sao Paulo, Brazil | Fitting and polished surfaces |
| 37 | 2011 | Cruz et al.73 | Effectiveness of chemical cleanser and ultrasonic device for denture hygiene | Planimetry | Image Tool 2.02 Software | Image | Maxillary | 1.0% neutral red solution | Fitting surface |
| 38 | 2012 | Puskar et al.58 | To examine the influence of gender, age, cleaning habits, and continuous wear of dentures on denture stomatitis | Index | Ambjørnsen et al. 198253 | Denture | Both | No disclosing | Fitting surface |
| 39 | 2012 | Taiwo et al.59 | Denture hygiene of elderly | Index | Taiwo et al. 201259 | Denture | Not mentioned | No disclosing | Fitting surface |
| 40 | 2012 | de Andrade et al.74 | Effect of Chlorhexidine on denture hygiene | Planimetry | Image Tool 3.0 Software | Image | Maxillary | 1.0% neutral red solution | Fitting surface |
| 41 | 2013 | Sloane et al.32# | Effect of person-centered mouth care intervention | Index | Augsburger and Elahi 198284 | Denture | Any | Not mentioned the brand or compound | Fitting and polished surfaces |
| 42 | 2014 | Mylonas et al.33 | Clinical audit in denture cleanliness | Index | Mylonas’ DCI33 | Denture | Any | Plaqsearch, Malmö, Sweden | Fitting surface |
| 43 | 2014 | Zenthöfer et al.34* | Comparison of oral health and hygiene in patients with or without dementia | Index | Wefers’ DHI85 | Denture | Both | Plaque Test; IvoclarVivadent, Schaan, Liechtenstein | All surfaces including teeth |
| 44 | 2014 | Zenthöfer et al.35* | Association of apraxia with oral hygiene | Index | Wefers’ DHI85 | Denture | Both | Plaque Test; IvoclarVivadent, Schaan, Liechtenstein | All surfaces including teeth |
| 45 | 2015 | Almas et al.36 | Simplified quantitative denture plaque index that | Index | Classification of Almas, Salameh, Kutkut, and Doubali-Denture Plaque Index (ASKD-DPI) 36 | Image | Both | Diluted erythrosine solution (Red-Cote #28 red dye) | Fitting surface |
| 46 | 2015 | Khanagar et al.37 | To assess the oral hygiene status of institutionalized dependent elders | Index | Augsburger and Elahi 198284 | Denture | Not mentioned | Plaque check disclosing solution | Fitting and polished surfaces |
| 47 | 2016 | Zenthöfer et al.38* | Improving the oral health of institutionalized dementia elders | Index | Wefers’ DHI85 | Denture | Both | Plaque Test; IvoclarVivadent, Schaan, Liechtenstein | All surfaces including teeth |
| 48 | 2016 | Mylonas et al.39 | Denture cleanliness of patients in a regional dental hospital | Index | Mylonas’ DCI33 | Denture | Any | Plaqsearch, Malmö, Sweden | Fitting surface |
| 49 | 2016 | Steinmassl et al.65 | Relationship of cognitive status to oral hygiene | Index | Wefers’ DHI85 | Denture | Both | Not mentioned about disclosing | All surfaces including teeth |
| 50 | 2016 | Zenthöfer et al.40* | Effectiveness of carers’ education on oral health and denture hygiene improvements of dementia elders | Index | Wefers’ DHI85 | Denture | Both | Plaque Test; IvoclarVivadent, Schaan, Liechtenstein | All surfaces including teeth |
| 51 | 2016 | Duyck et al.41 | Impact of denture cleaning method and overnight storage condition on denture plaque | Index | Augsburger and Elahi 198284 | Denture | Mandibular | 4.0% erythrosine disclosing solution | Fitting and polished surfaces |
| 52 | 2016 | Al-Kaisy et al.75 | Assessment of denture hygiene habit | Planimetry | Image tool 2.02 software | Image | Maxillary | Methylene blue disclosing solution (FDC Blue #1, 0.25% in deionized water) | Fitting surface |
| 53 | 2017 | Zenthöfer et al.42* | Association of dementia with poor oral health/denture hygiene and risk of periodontal disease in elderly | Index | Wefers’ DHI85 | Denture | Both | Plaque Test; IvoclarVivadent, Schaan, Liechtenstein | All surfaces including teeth |
| 54 | 2017 | Nihtila et al.60 | Effectiveness of a tailored oral health intervention | Index/ Score | Binary score (Y/N) | Denture | Not mentioned | No disclosing | Not mentioned |
| 55 | 2017 | Martori et al.43 | Relationship between denture-related factors and oral Candida colonization | Index | Jeganathan et al. 199621 | Denture | Maxillary | Erythrosine (Reveal; Henry-Schein, Melville, NY | Fitting surface |
| 56 | 2017 | Zimmerman et al.44# | Oral hygiene status and risk assessment | Index | Augsburger and Elahi 198284 | Denture | Any | Not mentioned the brand or compound | Fitting and polished surfaces |
| 57 | 2017 | Arruda et al.76 | Efficacy of denture cleanser | Planimetry | Image tool software | Image | Both | 1.0% neutral red | Fitting surface |
| 58 | 2018 | Baba et al.77 | To evaluate mechanical cleansing vs mechanical + chemical cleansing | Planimetry | Image J software | Image | Maxillary | Prospec, GC Co. | Fitting surface |
| 59 | 2018 | Ikeya et al.79 | Effects of denture cleanser | Planimetry | Adobe Photoshop vCS6 software; Adobe Systems, Inc | Image | Maxillary | Methylene blue, 0.25% m/v in distilled water; Wako Pure Chemical Industries Ltd | All surfaces including teeth |
| 60 | 2018 | Schwindling et al.46* | Oral health intervention and denture hygiene | Index | Wefers’ DHI85 | Denture | Any | Not mentioned about disclosing | All surfaces including teeth |
| 61 | 2018 | Klotz et al.47* | Oral health on the mortality of elderly people | Index | Wefers’ DHI85 | Denture | Not mentioned | Plaque Test; IvoclarVivadent, Schaan, Liechtenstein | All surfaces including teeth |
| 62 | 2018 | Guevara-Canales et al.61 | To determine whether self-perceived oral health impact and satisfaction measure | Index | Guevara-Canales et al.201861 | Denture | Both or any | No disclosing | Not mentioned |
| 63 | 2018 | Weintraub et al.48# | Improving oral hygiene in the nursing home | Index | Augsburger and Elahi 198284 | Denture | Both | Not mentioned the brand or compound | All surfaces including teeth |
| 64 | 2020 | Klotz et al.49* | To identify how changes to general health might affect the oral health | Index | Wefers’ DHI85 | Denture | Not mentioned | Plaque Test; IvoclarVivadent, Schaan, Liechtenstein | All surfaces including teeth |
| 65 | 2020 | Badaró et al.80 | Effects of three denture disinfection protocols | Planimetry | ImageTool 3.0; Informer Technologies, Inc | Image | Maxillary | No disclosing | Fitting surface |
| 66 | 2020 | Krausch-Hofmann et al.11 | Assessment of oral health conditions presented in the photograph | Index | Krausch-Hofmann et al. 202011 | Denture | Maxillary | No disclosing | Fitting surface |
| 67 | 2021 | Alqarni et al.50 | To analyze the influence of the intervention on neglected elderly | Index | Jeganathan et al. 199621 | Denture | Maxillary | Not mentioned about disclosing | Fitting surface |
| 68 | 2021 | Garg et al.51 | Impact of Sensitization on Family Caregivers | Index | Jeganathan et al. 199621 | Denture | Both or any | Not mentioned the brand or compound | Not mentioned |
| 69 | 2021 | Ng et al.52 | Effect of educational mobile application on denture hygiene | Index | Jeganathan et al. 199621 | Image | Maxillary | GC Tri Plaque ID Gel plaque disclosing agent (GC Co.) | Fitting surface |
| 70 | 2021 | Cinquanta et al.62 | Patient attitude and habits on denture hygiene | Index | Hoad-Reddick et al. 199082 | Denture | Both | No disclosing | All surfaces including teeth |
| 71 | 2021 | Wiatrak et al.66 | Effect of Tea Tree Oil Toothpaste on oral health | Index | Not mentioned | Not mentioned | Not mentioned | Not mentioned about disclosing | Not mentioned |
| 72 | 2021 | Araujo et al.81 | Effect of denture hygiene protocol | Planimetry | NIS-elements software | Image | Maxillary | 1.0% neutral red; IMBRALAB Química e Farmacêutica Ltda | Fitting surface |
| 73 | 2022 | Mousa et al.63 | Development of halitosis | Index | Ambjørgensen et al. 198253 | Denture | Both | No disclosing | Fitting and polished surfaces |
| 74 | 2022 | Peroz et al.64 | The influences of quarterly professional dental hygiene interventions | Index | Wefers’ DHI85 | Denture | Any | No disclosing | All surfaces including teeth |
Table 3.
A summary of the included visual assessment of denture hygiene studies. Four studies used both assessment methods and are hence mutually inclusive in both categories.
| Studies using denture plaque indices | Studies using planimetries | |||
|---|---|---|---|---|
| Numbers of studies | 60 | 81.1% | 18 | 24.3% |
| Examined samples | ||||
| Actual dentures | 46 | 76.7% | 0 | 0% |
| Images | 13 | 21.7% | 18 | 100% |
| Not mentioned | 1 | 1.6% | 0 | 0% |
| Types of dentures assessed | ||||
| Complete Denture | 8 | 13.3% | 10 | 55.6% |
| Partial Denture | 2 | 3.3% | 0 | 0% |
| Both complete and partial dentures | 3 | 5.0% | 0 | 0% |
| Not mentioned | 47 | 78.3% | 8 | 44.4% |
| Profile of dentures assessed | ||||
| Maxillary dentures | 23 | 38.3% | 14 | 77.8% |
| Mandibular dentures | 1 | 1.7% | 0 | 0% |
| Both maxillary and mandibular dentures | 17 | 28.3% | 3 | 16.6% |
| Maxillary or mandibular dentures | 12 | 2.0% | 0 | 0% |
| Not mentioned | 7 | 11.7% | 1 | 5.6% |
| Materials of denture assessed | ||||
| Acrylic | 13 | 21.7% | 10 | 55.6% |
| Metal | 1 | 1.7% | 0 | 0% |
| Both | 1 | 1.7% | 0 | 0% |
| Not mentioned | 45 | 75.0% | 8 | 44.4% |
| Using of disclosing agents on examined samples | ||||
| Yes | 43 | 71.6% | 17 | 94.4% |
| No (Plain) | 13 | 21.7% | 1 | 5.6% |
| Not mentioned | 4 | 6.7% | 0 | 0% |
| Denture surface(s) assessed | ||||
| Fitting (intaglio) surface only | 26 | 43.3% | 13 | 72.2% |
| Polished (cameo) surface only | 6 | 1.0% | 1 | 5.6% |
| All denture surfaces | 24 | 40.0% | 4 | 22.2% |
| Not mentioned | 4 | 6.7% | 0 | 0% |
Table 4.
Details about different denture plaque assessment indices and planimetric methods utilized to measure denture hygiene in the reviewed studies
| Year | Name of Indices/ Planimetric methods | Examined sample (Denture/Image) | Profile of dentures assessed | Disclosing (Yes/No) | Denture surface(s) assessed | Entire surface or divided assessment | Grading method on denture plaque or denture cleanliness |
|---|---|---|---|---|---|---|---|
| DENTURE PLAQUE INDICES | |||||||
| 1970 | Budtz-Jorgensen and Betram4 | Denture | Maxillary | Yes | Fitting surface | Entire | Estimated proportion/ quality |
| 1977 | Budtz-Jorgensen56 | Image | Maxillary | Yes | Fitting surface | Entire | Estimated proportion/ quality |
| 1979 | Schübert and Schübert Prosthesis Hygiene Index (PHI)86 | Image | Maxillary | Yes | Fitting surface | Divided | Estimated proportion/ quality |
| 1981 | Abelson et al.78 | Denture | Any | Yes | All surfaces including teeth | Entire | Estimated proportion/ quality |
| 1982 | Ambjørnsen et al.53 (developed from Silness and Loe plaque score 1964, Ainamo and Bay 1975) | Denture | Maxillary | No | Fitting surface | Divided | Estimated proportion/ quality |
| 1982 | Tarbet et al.83 | Image | Both | Yes | Fitting surface | Divided | Estimated area % |
| 1982 | Augsburger and Elahi84 | Denture | Maxillary | Yes | All surfaces | Divided | Estimated area % |
| 1983 | Budtz-Jorgensen et al.15 | Image | Maxillary | Yes | Fitting surface | Entire | Estimated area % |
| 1984 | Modified Quigley-Hein Index 23 | Denture | Maxillary | Yes | All surfaces including teeth | Entire | Estimated area % |
| 1986 | Murray et al.18 | Denture | Both | Yes | All surfaces including teeth | Entire | Estimated proportion/ quality |
| 1990 | Hoad-Reddick et al.82 | Denture | Both | No | All surfaces including teeth | Entire | Estimated proportion/ quality |
| 1995 | McCabe et al.20 | Denture | Not mentioned | Yes | All surfaces including teeth | Entire | Estimated proportion/ quality (upon stain, soil calculus, disclosed plaque) |
| 1996 | Jeganathan et al.21 (modified Tarbet et al.) | Denture | Maxillary | Yes | Fitting surface | Entire | Estimated area % |
| 1999 | Wefers' Denture Hygiene Index (DHI)85 | Denture | Both | Yes | All surfaces including teeth | Divided | Approximate % (the ratio of plaque-positive sites to all available sites, expressed as a percentage) |
| 2006 | Montal et al.55 | Denture | Any | No | All surfaces including teeth | Entire | Estimated proportion/ quality |
| 2007 | Paranhos et al.29 (modified Schübert and Schübert PHI) | Image | Maxillary | Yes | All surfaces including teeth | Divided | Estimated proportion/ quality |
| 2012 | Taiwo et al.59 (modified WHO assessment 1986) | Denture | Any | No | Fitting surface | Entire | Estimated proportion/ quality |
| 2014 | Mylonas et al. Denture Cleanliness Index (DCI)33 | Denture | Any | Yes | Fitting surface | Entire | Estimated area % |
| 2015 | Classification of Almas, Salameh, Kutkut, and Doubali-Denture Plaque Index (ASKD-DPI)36 | Image | Both | Yes | Fitting surface | Divided | Estimated area % |
| 2018 | Guevara-Canales et al.61 | Denture | Not mentioned | No | Not mentioned | Entire | Estimated proportion/ quality |
| 2020 | Krausch-Hofmann et al.11 | Denture | Maxillary | No | Fitting surface | Entire | Estimated proportion/ quality |
| PLANIMETRIC METHODS | |||||||
| Computerized pixel-counting | Image | Maxillary | Yes | Fitting surface | Entire | Pixels of disclosed plaque area can be automatically counted by the image analysis software. | |
| Point-counting | Image | Maxillary | Yes | Fitting surface | Entire | Disclosed denture image was projected, and superimposed by a grit of squares or equidistant points. Percentage of denture areas with disclosed squares/points could be calculated. | |
| Square-counting | Image | Maxillary | Yes | Fitting surface | Entire | ||
| Digital planimeter | Image | Maxillary | Yes | Fitting surface | Entire | A digital planimeter traced the contour of disclosed plaque area and the entire denture surface to calculate the percentage of disclosed plaque area. | |
Results
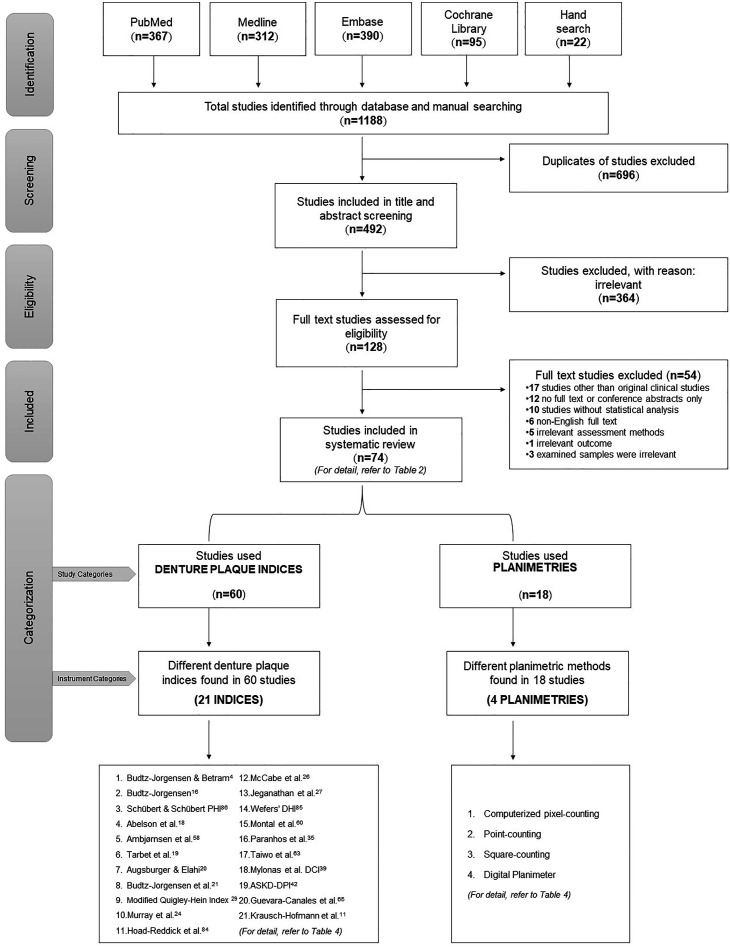
A total of 1188 studies were retrieved through the primary literature search. After the removal of duplicates and other exclusion criteria, 492 studies were screened, and of these, 128 were shortlisted for inclusion based on the screening of their titles and abstracts. The full text of shortlisted studies was assessed for eligibility, and finally, 74 studies4,10, 11, 12,15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 84 were selected for this review (Fig 1). A summary of all reviewed studies is listed in Table 2.
Figure 1.
PRISMA flowchart for search strategy together with the structure of this systematic review. (Four studies used both assessment methods and are hence mutually inclusive in both categories.)
An overwhelming, 19 studies12,20,21,25,29, 30, 31,33,39,41,63,66,73, 74, 75, 76,79,81,84 assessed acrylic dentures, and only a single study52 investigated metallic dentures, whereas another43 investigated both acrylic and metallic dentures; the remaining 53 studies4,9,10,14, 15, 16, 17, 18,21, 22, 23,25, 26, 27,31,33, 34, 35, 36, 37,39,41,43, 44, 45, 46, 47, 48, 49,50,52, 53, 54, 55, 56, 57, 58, 59,60,61,63,64,66, 67, 68, 69,70,71,76,77,79,81,82 did not specify the fabricated denture material under investigation. (Table 3) Surprisingly, eight34,35,38,40,42,46,47,49 of 74 studies reported results from the identical population by a single group of investigators in Germany, and three studies32,44,48 investigated another single cohort from the USA. (Table 2)
The totally included 74 studies were split into two sub-categories as per the assessment methods. Accordingly, 18 studies10,12,25,30,31,68, 69, 70, 71, 72, 73, 74, 75, 76, 77,79, 80, 81 used planimetries while 60 studies4,11,12,15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67,78,82, 83, 84 used denture plaque indices (Table 3 and Fig 1). Four studies12,25,30,31 used both assessment methods, hence such studies were mutually inclusive in both categories. Therefore, the total sum of studies of all categories evaluated was over 74. All but one81 of the included studies had a moderate to high risk of bias (Supplementary Table 1).
Characteristics for included studies that utilized denture plaque indices
Of the 60 studies using denture plaque indices with naked eye assessment,4,11,12,15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67,78,82, 83, 84 a vast majority 46 assessed the actual dentures, 4,11,18,20, 21, 22,24, 25, 26, 27, 28,32, 33, 34, 35,37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51,53, 54, 55,57, 58, 59, 60, 61, 62, 63, 64, 65,78,82, 83, 84 while 13 assessed only the denture images.12,15, 16, 17,19,23,29, 30, 31,36,52,56,67 One study did not mention the assessed item.66 Twenty-three studies examined the maxillary dentures only,4,11,15, 16, 17,21,24, 25, 26, 27,29, 30, 31,43,45,50,52, 53, 54,56,67,83,84 17 studies examined both the maxillary and mandibular dentures,12,18,19,22,23,34, 35, 36,38,40,42,48,57,58,62,63,65 and 12 studies examined either the maxillary or the mandibular dentures.28,32,39,44,46,51,55,61,64,74,78,82 Studies that used disclosing agents to assess denture plaque (43 studies)4,12,15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45,47, 48, 49,51,52,56,67,78,83,84 were three times more than those without disclosing agents (13 studies).11,20,53, 54, 55,57, 58, 59, 60, 61, 62, 63, 64
The fitting surface of dentures was assessed in 26 studies4,11,15, 16, 17,19,24,26,27,30, 31, 32,36,39,43,45,49,50,52, 53, 54,56,58,59,67,83 while both the denture and tooth surfaces were assessed in 24 studies.12,18,20,22,23,25,29,34,35,38,40,42,46, 47, 48, 49,55,57,62,64,65,78,82,84 The remaining six studies assessed only the fitting and polished surfaces of dentures without teeth,28,32,37,41,44,63 and four studies did not mention the surface(s) they assessed. 51,60,61,66
Characteristics for included denture plaque indices
In total, 21 indices were used for denture plaque grading by the naked eye of assessors (Table 4). The most commonly used indices were Wefers’ Denture Hygiene Index (DHI)85 which was used in 10 studies,34,35,38,40,42,46,47,49,64,65 and Augsburger and Elahi index which was used in nine studies.12,25,28,32,37,41,44,48,84
Disclosing agents for the denture plaque were utilized in 15 indices4,15,18,20,21,23,29,33,36,56,78,83, 84, 85, 86 while the remaining six indices did not utilize any disclosing agents.11,53,55,59,61,82 Ten indices were used to assess maxillary complete dentures,4,11,15,21,23,29,53,56,84,86 and nine for evaluation of maxillary and mandibular dentures.18,33,36,55,59,78,82,83,85 Two indices did not specify the type of examined dentures.20,61 Eight indices assessed all denture surfaces including denture teeth,18,20,23,29,55,78,82,85 one index assessed fitting (intaglio) and polished (cameo) surfaces;84 11 indices assessed denture fitting surface only,4,11,15,21,33,36,53,56,59,83,86 and one did not specify the surface(s) assessed.61
In general, grading indices could be classified into three types: i) subjective grading by estimating the percentage of plaque-deposited areas (7 indices),15,21,23,33,36,83,84 ii) subjective grading by estimating the proportion and quality of plaque-deposited areas (13 indices),4,11,18,29,53,55,56,59,61,78,82,86 and iii) sub-dividing the denture surfaces into areas, and quantifying the percentage of divided areas with plaque deposition (1 index).85
Seven indices divided the denture surface into areas for grading,29,36,53,83, 84, 85, 86 while the rest graded the entire denture area, mostly the fitting surface.4,11,15,18,20,21,23,33,55,56,59,61,78,82 The index proposed by Jeganathan et al.21 was used to assess metallic dentures in two studies.43,52
Planimetric assessments
Most planimetric studies assessed the fitting surface of the maxillary complete dentures. All except one planimetric assessment80 assessed the disclosed denture images i.e. 17 studies.10,12,25,30,31,68, 69, 70, 71, 72, 73, 74, 75, 76, 77,79,81 Of the 18 studies that utilized planimetric assessments, one study quantified squares,68 16 studies quantified pixels with computer programs,12,25,30,31,69, 70, 71, 72, 73, 74, 75, 76, 77,79, 80, 81 and a single study quantified points, pixels, and contour of plaque areas.10 (Table 4) Among 17 studies that utilized computerized planimetries,10,12,25,30,31,69, 70, 71, 72, 73, 74, 75, 76, 77,79, 80, 81 two most commonly used software were UTHSCSA (the University of Texas Health Science Center at San Antonio) Image tool (11 studies)10,30,31,69,71, 72, 73, 74, 75, 76,80 and Adobe Photoshop (4 studies).12,30,70,79
Comparative studies
One study compared the accuracy and reproducibility of the three indices (Schübert and Schübert Prosthesis Hygiene Index (PHI),86 Budtz-Jorgensen56 and Jeganathan et al.21) using the planimetric assessment as the gold standard.31 Another study analyzed the agreements between an index of Augsburger and Elahi84 and three planimetries.12
Since these various studies used disparate indices yielding different outcome parameters, a meta-analysis of the extracted data could not be performed.
Discussion
In general, denture hygiene or denture plaque biofilm can be visually assessed using various indices and planimetries. Our review provides a contemporaneous account of these assessment methods described in the literature up to 2022. Clearly, the fact that there are so many methodologies in use to evaluate denture plaque biofilm implies that there is no single preferred method of assessment, and the data from the current review should facilitate decision-making by future investigators and clinicians embarking on similar studies on the optimal method of denture plaque evaluation.
In this review, most studies assessed acrylic complete dentures. Only a relatively small number of studies investigated metallic dentures and this may be related to imaging issues and poor contrast of disclosed metallic surfaces that may interfere with the computerized assessment of images.
Denture plaque biofilm usually develops unevenly on denture surfaces and more biofilm growth is seen on the fitting (intaglio) surface than on the polished (cameo) surfaces.11,79 This is because the intaglio surfaces are protected from the continuous, dynamic flushing action of saliva and the muscular movements of the tongue.6 Additionally, the intaglio surfaces, in comparison to cameo surfaces, are unpolished and may contain undercut regions, especially at the area around maxillary tuberosities and palatal rugae19,30 which have limited access for a denture brush.79 This, together with the fact that the maxillary denture-bearing area is the main plaque-depository area,12 and most affected by pathologies such as denture-associated stomatitis and related fungal infections.87 These are the possible reasons why most workers have assessed the intaglio surfaces of maxillary dentures in comparison to cameo surfaces. Actually, indices that can effectively assess both maxillary and mandibular dentures should be preferable clinically as many patients have both maxillary and mandibular prostheses. Besides, the differences in plaque patterns between maxillary vs mandibular dentures were not clearly reported in reviewed studies. Moreover, there was no report of a significant difference in plaque score or plaque amount between maxillary and mandibular dentures.
Furthermore, because of different plaque growth on different denture surfaces, plaque assessment on divided areas enables assessment of localized areas of plaque deposition.17 Of the indices used, the method of Augsburger and Elahi84 where eight sub-divided areas were assessed is clearly less time-consuming12 and preferable to the method of Paranhos et al.29 where a total of 22 sub-divided areas were quantified.
Most denture plaque assessment indices were inexpensive and simple to use, being compatible with use in a clinic or community setting, thus permitting the study of a large number of subjects quickly and effectively.88 The ease and the rapidity of the assessment method are clearly important in community-level studies with large cohorts, as visual fatigue associated with prolonged assessment36 could bias the outcome. Actually, assessment of actual dentures is quicker and simpler to grade for the entire surfaces, and also possible to use a blunt probe to physically detect the plaque53,54,59 but assessors can easily confuse with any imaginary division of the denture surfaces in the assessment on divided denture-areas. Hence assessments of the denture images, captured by a camera, rather than on-site evaluation, have been suggested so that assessors evaluate the images at a later stage in a laboratory setting with no time constraints.20,22 Furthermore, denture images can be anonymized easily in this manner to reduce any potential evaluator bias. The use of such imaging also facilitates the testing and training of inter- and intra-assessor reproducibility as well as allows dividing denture surface into areas by computer. Thus the suggested imaging techniques are in general preferable to on-site naked-eye evaluations.
Disclosing the plaque on the denture surfaces is demanding because plaque is usually colorless and cannot be visible easily.89,90 Disclosing agents are surrogate visual indicators19 that are used in many denture plaque indices (15 out of 21) in this review to enhance the visibility of plaque biofilm. The dye in the disclosing agent diffuses into plaque, binds to plaque components such as proteins and polysaccharides, and is retained in the plaque.91,92 All but a single denture plaque index85 in our review were entailing subjective judgments by the assessors and hence more prone to inter- and intra-assessor measurement errors. Moreover, these indices were in the ordinal scale, which is non-continuous and semi-quantitative, meaning that only low-power categorical statistical tests could be performed.12 An index that calculates the percentage of divided areas with plaque-deposited, is more objective and permits the use of powerful statistical tests, which is preferable in this context.85
Planimetric plaque assessment methods, as opposed to the traditional naked eye methods with indices, could be considered as a relatively new development in denture plaque evaluation research.29 In principle, these methods are based on quantifying10 either point counts or divided squares68 of a projected image or tracing the contour of a disclosed plaque area using a digital planimeter.10 Then, the area with plaque deposition, in pixels, can be automatically measured using image analysis software.
As regards the surfaces studied in planimetric investigations most evaluated only the fitting surface while a few others assessed multiple surfaces such as both the intaglio and cameo surfaces, and left and right buccal surfaces.12,71,79 Such planimetric assessment of multiple denture surfaces is useful for evaluating the efficacy of denture cleansing procedures though it may lead to confusion as overlapping image surfaces in different images.
The other advantage of planimetries is that the results are provided in percentages (%), as a continuous numerical value i.e. ratio scale93 that permits more powerful statistical analyses.12 The planimetric results also correlate well with other non-visual plaque assessment methods such as plaque weight and viable microbial counts.94
However, there are some drawbacks associated with planimetries too. These include inherent artifacts due to reflected light or discoloration of the acrylic denture base. Additionally, image quality consequential to the standardization of the camera settings such as the resolution power, the exposure time, as well as background lighting are all factors that need to be considered.12,22 Other factors that affect the image quality are the angulation between the camera and the denture,25,29,69, 70, 71,76 and the denture position25 and distance all of which should be standardized.
In conclusion, computerized planimetries provide a more objective assessment of denture plaque biofilm and do not require the calibration of assessors in comparison to naked eye visual assessment methods using denture plaque indices.71,95 Although time-consuming,10,12,73 and requires additional equipment as well as effort for capturing and analyzing standard images, some have suggested that planimetries should be the method of choice for research on denture hygiene.71,73 On the contrary, the naked eye assessment using denture plaque indices are simple, and easy to interpret though subjective,22 and perhaps more practical for those without access to imaging technology, providing acceptable results in a clinical setting. The latter, we believe, is more appropriate for community-level studies. Finally, very few plaque biofilm assessments of metallic denture bases have been conducted, and further work in this area is needed.
Funding resources
This research/review did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgements
Publication made possible in part by support from The University of Hong Kong (HKU) Libraries Open Access Author Fund sponsored by the HKU Libraries.
CRediT authorship contribution statement
Khaing Myat Thu: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Resources, Data curation, Writing – original draft, Writing – review & editing, Visualization. Andy Wai Kan Yeung: Conceptualization, Methodology, Validation, Formal analysis, Writing – review & editing, Supervision. Lakshman Samaranayake: Validation, Writing – review & editing, Supervision. Walter Yu Hang Lam: Conceptualization, Methodology, Validation, Writing – review & editing, Supervision, Project administration.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.identj.2023.06.010.
Appendix. Supplementary materials
References
- 1.Kikuchi R, Watabe N, Konno T, Mishina N, Sekizawa K, Sasaki H. High incidence of silent aspiration in elderly patients with community- acquired pneumonia. Am J Respir Crit Care Med. 1994;150:251–253. doi: 10.1164/ajrccm.150.1.8025758. [DOI] [PubMed] [Google Scholar]
- 2.Nikawa H, Hamada T, Yamamoto T. Denture plaque - Past and recent concerns. J Dent. 1998;26:299–304. doi: 10.1016/s0300-5712(97)00026-2. [DOI] [PubMed] [Google Scholar]
- 3.Coulthwaite L, Verran J. Potential pathogenic aspects of denture plaque. Br J Biomed Sci. 2007;64:180–189. doi: 10.1080/09674845.2007.11732784. [DOI] [PubMed] [Google Scholar]
- 4.Budtz-Jorgensen E, Bertram U. Denture stomatitis. Acta Odontol Scand. 1970;28:71–92. doi: 10.3109/00016357009033133. [DOI] [PubMed] [Google Scholar]
- 5.Barbeau J, Se´guin J, Goulet JP, Koninck Ld, Avon SL, Lalonde B, et al. Reassessing the presence of candida albicans in denture-related stomatitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:51–59. doi: 10.1067/moe.2003.44. [DOI] [PubMed] [Google Scholar]
- 6.Samaranayake L. 5th ed. Elsevier; 2018. Essential Microbiology for Dentistry. [Google Scholar]
- 7.Imsand M, Janssens JP, Auckenthaler R, Mojon P, Budtz-Jørgensen E. Bronchopneumonia and oral health in hospitalized older patients. A pilot study. Gerodontology. 2002;19:66–72. doi: 10.1111/j.1741-2358.2002.00066.x. [DOI] [PubMed] [Google Scholar]
- 8.Kusama T, Aida J, Yamamoto T, Kondo K, Osaka K. Infrequent denture cleaning increased the risk of pneumonia among community-dwelling older adults: A population-based cross-sectional study. Sci Rep. 2019;9:13734. doi: 10.1038/s41598-019-50129-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Castellucci Barbosa L, Ferreira MRM, de Carvalho Calabrich CF, Viana AC, de Lemos MCL, Lauria RA. Edentulous patients’ knowledge of dental hygiene and care of prostheses. Gerodontology. 2008;25:99–106. doi: 10.1111/j.1741-2358.2007.00190.x. [DOI] [PubMed] [Google Scholar]
- 10.Paranhos HFO, da Silva CHL. Comparative study of methods for the quantification of biofilm on complete dentures. Braz Oral Res. 2004;18:215–223. doi: 10.1590/s1806-83242004000300007. [DOI] [PubMed] [Google Scholar]
- 11.Krausch-Hofmann S, Tran TD, Declerck D, Mello JA, Declercq A, Lesaffre E, et al. Assessment of oral health conditions presented in photographs - Is there a difference between dentists and non-dental professional caregivers? BMC Oral Health. 2020;20:188. doi: 10.1186/s12903-020-01171-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coulthwaite L, Verran J. Evaluation of in vivo denture plaque assessment methods. Br Dent J. 2009;207:E12. doi: 10.1038/sj.bdj.2009.854. [DOI] [PubMed] [Google Scholar]
- 13.Mylonas P, Milward P, McAndrew R. Denture cleanliness and hygiene: an overview. Br Dent J. 2022;233:20–26. doi: 10.1038/s41415-022-4397-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Papadiochou S, Polyzois G. Hygiene practices in removable prosthodontics: A systematic review. Int J Dent Hyg. 2018;16:179–201. doi: 10.1111/idh.12323. [DOI] [PubMed] [Google Scholar]
- 15.Budtz-Jorgensen E, Kelstrup J, Poulsen S. Reduction of formation of denture plaque by a protease (Alcalase@) Acta Odontol Scand. 1983;41:93–98. doi: 10.3109/00016358309162308. [DOI] [PubMed] [Google Scholar]
- 16.Poulsen S, Budtz-Jorgensen E, Knudsen AM, Nielsen L, Kelstrup J. Evaluation of two methods of scoring denture plaque. Acta Odontol Scand. 1983;41:283–286. doi: 10.3109/00016358309162336. [DOI] [PubMed] [Google Scholar]
- 17.Ambjørnsen E, Rise J, Haugejorden O. A study of examiner errors associated with measurement of denture plaque. Acta Odontol Scand. 1984;42:183–191. doi: 10.3109/00016358408993870. [DOI] [PubMed] [Google Scholar]
- 18.Murray ID, McCabe JF, Storer R. The relationship between the abrasivity and cleaning power of the dentifrices-type denture cleansers. Br Dent J. 1986;161:205–208. doi: 10.1038/sj.bdj.4805932. [DOI] [PubMed] [Google Scholar]
- 19.Cardash HS, Rosenberg M. An innovative method of monitoring denture hygiene. J Prosthet Dent. 1990;63:661–664. doi: 10.1016/0022-3913(90)90323-5. [DOI] [PubMed] [Google Scholar]
- 20.McCabe JF, Murray ID, Kelly PJ. The efficacy of denture cleansers. Eur J Prosthodont Restor Dent. 1995;3:203–207. [PubMed] [Google Scholar]
- 21.Jeganathan S, Thean HPY, Thong K, Chan YC, Singh M. A clinically viable index for quantifying denture plaque. Quintessence Int (Berl) 1996;27:569–573. [PubMed] [Google Scholar]
- 22.McCabe JF, Murray ID, Laurie J, Kelly PJ. A method for scoring denture plaque. Eur J Prosthodont Restor Dent. 1996;4:59–64. [PubMed] [Google Scholar]
- 23.Keng SB, Lim M. Denture plaque distribution and the effectiveness of a perborate-containing denture cleanser. Quintessence Int. 1996;27:341–345. [PubMed] [Google Scholar]
- 24.Jeganathan S, Payne JA, Thean HPY. Denture stomatitis in an elderly edentulous Asian population. J Oral Rehabil. 1997;24:468–472. doi: 10.1046/j.1365-2842.1997.00523.x. [DOI] [PubMed] [Google Scholar]
- 25.Sheen SR, Harrison A. Assessment of plaque prevention on dentures using an experimental cleanser. J Prosthet Dent. 2000;84:594–601. doi: 10.1067/mpr.2000.110498. [DOI] [PubMed] [Google Scholar]
- 26.Kulak-Ozkan Y, Kazazoglu E, Arikan A. Oral hygiene habits, denture cleanliness, presence of yeasts and stomatitis in elderly people. J Oral Rehabil. 2002;29:300–304. doi: 10.1046/j.1365-2842.2002.00816.x. [DOI] [PubMed] [Google Scholar]
- 27.Kanli A, Demirel F, Sezgin Y. Oral candidosis, denture cleanliness and hygiene habits in an elderly population. Aging Clin Exp Res. 2005;17:502–507. doi: 10.1007/BF03327418. [DOI] [PubMed] [Google Scholar]
- 28.De Visschere LM, Grooten L, Theuniers G, Vanobbergen JN. Oral hygiene of elderly people in long-term care institutions–a cross-sectional study. Gerodontology. 2006;23:195–204. doi: 10.1111/j.1741-2358.2006.00139.x. [DOI] [PubMed] [Google Scholar]
- 29.Paranhos HFO, da Silva CHL, Venezian GC, Macedo LD, de Souza RF. Distribution of biofilm on internal and external surfaces of upper complete dentures: the effect of hygiene instruction. Gerodontology. 2007;24:162–168. doi: 10.1111/j.1741-2358.2007.00177.x. [DOI] [PubMed] [Google Scholar]
- 30.Paranhos HFO, Silva-Lovato CH, Souza RF, Cruz PC, Freitas KM, Peracini A. Effects of mechanical and chemical methods on denture biofilm accumulation. J Oral Rehabil. 2007;34:606–612. doi: 10.1111/j.1365-2842.2007.01753.x. [DOI] [PubMed] [Google Scholar]
- 31.Paranhos HFO, Lovato Da Silva CH, Souza RF, Pontes KMDF. Evaluation of three indices for biofilm accumulation on complete dentures. Gerodontology. 2010;27:33–40. doi: 10.1111/j.1741-2358.2009.00285.x. [DOI] [PubMed] [Google Scholar]
- 32.Sloane PD, Zimmerman S, Chen X, Barrick AL, Poole P, Reed D, et al. Effect of a person-centered mouth care intervention on care processes and outcomes in three nursing homes. J Am Geriatr Soc. 2013;61:1158–1163. doi: 10.1111/jgs.12317. [DOI] [PubMed] [Google Scholar]
- 33.Mylonas P, Afzal Z, Attrill DC. A clinical audit of denture cleanliness in general dental practice undertaken in the west midlands. Br Dent J. 2014;217:231–234. doi: 10.1038/sj.bdj.2014.757. [DOI] [PubMed] [Google Scholar]
- 34.Zenthöfer A, Schröder J, Cabrera T, Rammelsberg P, Hassel AJ. Comparison of oral health among older people with and without dementia. Community Dent Health. 2014;31:27–31. [PubMed] [Google Scholar]
- 35.Zenthöfer A, Navratil SD, Rammelsberg P, Cabrera T, Gorenc L, Urbanowitsch N, et al. Oral health and apraxia among institutionalized elderly people - A pilot study. Acta Odontol Scand. 2014;73:150–155. doi: 10.3109/00016357.2014.961956. [DOI] [PubMed] [Google Scholar]
- 36.Almas K, Salameh Z, Kutkut A, Ai DA. A simplified technique to measure plaque on the intaglio surfaces of complete dentures. J Int Acad Periodontol. 2015;17:58–64. [PubMed] [Google Scholar]
- 37.Khanagar S, Naganandini S, Rajanna V, Naik S, Rao R, Madhuniranjanswamy MS. Oral hygiene status of institutionalised dependent elderly in India - A cross-sectional survey. Can Geriatr J. 2015;18:51–56. doi: 10.5770/cgj.18.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zenthöfer A, Cabrera T, Rammelsberg P, Hassel AJ. Improving oral health of institutionalized older people with diagnosed dementia. Aging Ment Heal. 2016;20:303–308. doi: 10.1080/13607863.2015.1008986. [DOI] [PubMed] [Google Scholar]
- 39.Mylonas P, Attrill DC, Walmsley AD. Evaluating denture cleanliness of patients in a regional dental hospital. Br Dent J. 2016;221:127–130. doi: 10.1038/sj.bdj.2016.562. [DOI] [PubMed] [Google Scholar]
- 40.Zenthöfer A, Meyer-Kühling I, Hufeland AL, Schröder J, Cabrera T, Baumgart D, et al. Carers’ education improves oral health of older people suffering from dementia – Results of an intervention study. Clin Interv Aging. 2016;11:1755–1762. doi: 10.2147/CIA.S118330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Duyck J, Vandamme K, Krausch-Hofmann S, Boon L, Keersmaecker KD, Jalon E, et al. Impact of denture cleaning method and overnight storage condition on denture biofilm mass and composition: A cross-over randomized clinical trial. PLoS One. 2016;11 doi: 10.1371/journal.pone.0145837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zenthöfer A, Baumgart D, Cabrera T, Rammelsberg P, Schro¨der J, Corcodel N, et al. Poor dental hygiene and periodontal health in nursing home residents with dementia: an observational study. Odontology. 2017;105:208–213. doi: 10.1007/s10266-016-0246-5. [DOI] [PubMed] [Google Scholar]
- 43.Martori E, Ayuso-Montero R, Willaert E, Viñas M, Peraire M, Martinez-Gomis J. Status of removable dentures and relationship with oral candida-associated factors in a geriatric population in catalonia. J Prosthodont. 2017;26:370–375. doi: 10.1111/jopr.12551. [DOI] [PubMed] [Google Scholar]
- 44.Zimmerman S, Austin S, Cohen L, Reed D, Poole P, Ward K, et al. Readily Identifiable Risk Factors of Nursing Home Residents’ Oral Hygiene: Dementia, Hospice, and Length of Stay. J Am Geriatr Soc. 2017;65:2516–2521. doi: 10.1111/jgs.15061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Budtz-Jorgensen E, Kelstrup J. Enzymes as denture cleansers. Scan J Dent Res. 1977;85:209–215. doi: 10.1111/j.1600-0722.1977.tb00555.x. [DOI] [PubMed] [Google Scholar]
- 46.Schwindling FS, Krisam J, Hassel AJ, Rammelsberg P, Zenthöfer A. Long-term success of oral health intervention among care-dependent institutionalized seniors: Findings from a controlled clinical trial. Community Dent Oral Epidemiol. 2018;46:109–117. doi: 10.1111/cdoe.12335. [DOI] [PubMed] [Google Scholar]
- 47.Klotz AL, Hassel AJ, Schröder J, Rammelsberg P, Zenthöfer A. Is compromised oral health associated with a greater risk of mortality among nursing home residents? A controlled clinical study. Aging Clin Exp Res. 2018;30:581–588. doi: 10.1007/s40520-017-0811-y. [DOI] [PubMed] [Google Scholar]
- 48.Weintraub JA, Zimmerman S, Ward K, Wretman CJ, Sloane PD, Stearns SC, et al. Improving Nursing home residents’ oral hygiene: results of a cluster randomized intervention trial. J Am Med Dir Assoc. 2018;19:1086–1091. doi: 10.1016/j.jamda.2018.09.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Klotz AL, Zajac M, Ehret J, Kilian S, Rammelsberg P, Zenthöfer A. Short-term effects of a deterioration of general health on the oral health of nursing-home residents. Clin Interv Aging. 2020;15:29–38. doi: 10.2147/CIA.S234938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Alqarni MA, Mattoo K, Dhingra S, Baba SM, Sanabani FA, Makramani BMAA, et al. Sensitizing family caregivers to influence treatment compliance among elderly neglected patients—A 2-year longitudinal study outcome in completely edentulous patients. Healthc. 2021;9:533. doi: 10.3390/healthcare9050533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Garg R, Mattoo K, Kumar L, Khalid I, Baig F, Elnager M, et al. Impact of sensitization of family caregivers upon treatment compliance among geriatric patients suffering from elder abuse and neglect. Healthc. 2021;9:226. doi: 10.3390/healthcare9020226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ng JYM, Lim TW, Tarib N, Ho TK. Effect of educational progressive web application on patient's oral and denture knowledge and hygiene: A randomised controlled trial. Health Informatics J. 2021;27:1–17. doi: 10.1177/14604582211035821. [DOI] [PubMed] [Google Scholar]
- 53.Ambjornsen E, Valderhaug J, Norheim PW, Floystrand F. Assessment of an additive index for plaque accumulation on complete maxillary dentures. Acta Odontol Scand. 1982;40:203–208. doi: 10.3109/00016358209019813. [DOI] [PubMed] [Google Scholar]
- 54.Schou L, Wight C, Cumming C. Oral hygiene habits, denture plaque, presence of yeasts and stomatitis in institutionalized elderly in Lathian, Scotland. Community Dent Oral Epidemiol. 1987;15:85–89. doi: 10.1111/j.1600-0528.1987.tb00488.x. [DOI] [PubMed] [Google Scholar]
- 55.Montal S, Tramini P, Triay JA, Valcarcel J. Oral hygiene and the need for treatment of the dependent institutionalised elderly. Gerodontology. 2006;23:67–72. doi: 10.1111/j.1741-2358.2006.00111.x. [DOI] [PubMed] [Google Scholar]
- 56.Budtz-Jorgensen E. Prevention of denture plaque formation by an enzyme denture cleanser. J Biol Buccale. 1977;5:239–244. [PubMed] [Google Scholar]
- 57.Dikbas I, Calikkocaoglu S. Investigation of the Cleanliness of Dentures in a University Hospital. Int J Prosthodont. 2006;19:294–298. [PubMed] [Google Scholar]
- 58.Puskar T, Potran M, Markovic D, Slobodan P, Danimir J, Tijana L, et al. Factors influencing the occurrence of denture stomatitis in complete dentures wearers. HealthMED. 2012;6:2780–2785. [Google Scholar]
- 59.Taiwo JO, Arigbede AO, Harcourt P. Denture hygiene of the elderly denture wearers in south east local government area in Ibadan. Nigeria. 2012;2:22–27. [Google Scholar]
- 60.Nihtilä A, Tuuliainen E, Komulainen K, Autonen-Honkonen K, Nykänen I, Hartikainen S, et al. Preventive oral health intervention among older home care clients. Age Ageing. 2017;46:846–851. doi: 10.1093/ageing/afx020. [DOI] [PubMed] [Google Scholar]
- 61.Guevara-Canales JO, Morales-Vadillo R, Sacsaquispe-Contreras SJ, Alberca-Ramos DE, Morgenstern-Orezzoli H, Cava-Vergiú CE. Association between self-perceived oral health and clinical indicators. Oral Health Prev Dent. 2018;16:33–41. doi: 10.3290/j.ohpd.a39685. [DOI] [PubMed] [Google Scholar]
- 62.Cinquanta L, Varoni EM, Barbieri C, Sardella A. Patient attitude and habits regarding removable denture home hygiene and correlation with prosthesis cleanliness: A cross-sectional study of elderly Italians. J Prosthet Dent. 2021;125 doi: 10.1016/j.prosdent.2021.01.024. 772.e1-e7. [DOI] [PubMed] [Google Scholar]
- 63.Mousa MA, Alam MK, Ganji KK, Khader Y, Lynch E, Kielbassa AM. Prospective case series on possible effects of local factors on the development of halitosis in new complete denture wearers. Quintessence Int (Berl) 2022;53:218–225. doi: 10.3290/j.qi.b2218709. [DOI] [PubMed] [Google Scholar]
- 64.Peroz I, Klein C. Influence of professional dental hygiene on oral and general health of retirement home residents: A comparative study. Clin Exp Dent Res. 2022;8:45–53. doi: 10.1002/cre2.488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Steinmassl PA, Steinmassl O, Kraus G, Dumfahrt H, Grunert I. Is Cognitive status related to oral hygiene level and appropriate for determining need for oral hygiene assistance? J Periodontol. 2016;87:41–47. doi: 10.1902/jop.2015.150349. [DOI] [PubMed] [Google Scholar]
- 66.Wiatrak K, Morawiec T, Rój R, Kownacki P, Nitecka-Buchta A, Niedzielski D, et al. Article evaluation of effectiveness of a toothpaste containing tea tree oil and ethanolic extract of propolis on the improvement of oral health in patients using removable partial dentures. Molecules. 2021;26:4071. doi: 10.3390/molecules26134071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Budtz-Jorgensen E, Knudsen AM. Chlorhexidine gel and steradent employed in cleaning dentures. Acta Odontol Scand. 1978;36:83–87. doi: 10.3109/00016357809027570. [DOI] [PubMed] [Google Scholar]
- 68.Ghalichebaf M, Graser GN, Zander HA. The efficacy of denture-cleansing agents. J Prosthet Dent. 1982;48:515–520. doi: 10.1016/0022-3913(82)90354-7. [DOI] [PubMed] [Google Scholar]
- 69.Andrucioli MCD, Dorigan De Macedo L, Panzeri H, Lara EHG, Paranhos HFO. Comparison of two cleansing pastes for the removal of biofilm from dentures and palatal lesions in patients with atrophic chronic candidiasis. Braz Dent J. 2004;15:220–224. doi: 10.1590/s0103-64402004000300011. [DOI] [PubMed] [Google Scholar]
- 70.Fernandes RAG, Lovato-Silva CH, Paranhos HFO, Ito IY. Efficacy of three denture brushes on biofilm removal from complete dentures. J Appl Oral Sci. 2007;15:39–43. doi: 10.1590/S1678-77572007000100009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Salles AES, Macedo LD, Fernandes RAG, Silva-Lovato CH, Paranhos H de FO. Comparative analysis of biofilm levels in complete upper and lower dentures after brushing associated with specific denture paste and neutral soap. Gerodontology. 2007;24:217–223. doi: 10.1111/j.1741-2358.2007.00169.x. [DOI] [PubMed] [Google Scholar]
- 72.Souza RF, Regis RR, Nascimento C, Paranhos HFO, Silva CHL. Domestic use of a disclosing solution for denture hygiene: A randomised trial. Gerodontology. 2010;27:193–198. doi: 10.1111/j.1741-2358.2009.00309.x. [DOI] [PubMed] [Google Scholar]
- 73.Cruz PC, de Andrade IM, Peracini A, Souza-Gugelmin MCM, Silva-Lovato CH, Souza RF, et al. The effectiveness of chemical denture cleansers and ultrasonic device in bio film removal from complete dentures. J Appl Oral Sci. 2011;19:668–673. doi: 10.1590/S1678-77572011000600021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.de Andrade IM, Cruz PC, Silva-Lovato CH, de Souza RF, Cristina Monteiro Souza-Gugelmin M, Paranhos HFO. Effect of chlorhexidine on denture biofilm accumulation. J Prosthodont. 2012;21:2–6. doi: 10.1111/j.1532-849X.2011.00774.x. [DOI] [PubMed] [Google Scholar]
- 75.al-Kaisy N, Saddq TH, Raouf LL. Assessment of denture hygiene habits among complete denture wearers attending Sulaimani Dental School. Sulaimani Dent J. 2016;3:69–77. [Google Scholar]
- 76.de Arruda CNF, Salles MM, Badaró MM, Oliveira VC, Macedo AP, Silva-Lovato CH, et al. Effect of sodium hypochlorite and Ricinus communis solutions on control of denture biofilm: A randomized crossover clinical trial. J Prosthet Dent. 2017;117:729–734. doi: 10.1016/j.prosdent.2016.08.035. [DOI] [PubMed] [Google Scholar]
- 77.Baba Y, Sato Y, Owada G, Minakuchi S. Effectiveness of a combination denture-cleaning method versus a mechanical method: comparison of denture cleanliness, patient satisfaction, and oral health-related quality of life. J Prosthodont Res. 2018;62:353–358. doi: 10.1016/j.jpor.2018.01.005. [DOI] [PubMed] [Google Scholar]
- 78.Abelson DC. Denture plaque and denture cleansers. J Prosthet Dent. 1981;45:376–379. doi: 10.1016/0022-3913(81)90094-9. [DOI] [PubMed] [Google Scholar]
- 79.Ikeya K, Iwasa F, Inoue Y, Fukunishi M, Takahashi N, Ishihara K, et al. Inhibition of denture plaque deposition on complete dentures by 2-methacryloyloxyethyl phosphorylcholine polymer coating: A clinical study. J Prosthet Dent. 2018;119:67–74. doi: 10.1016/j.prosdent.2017.02.012. [DOI] [PubMed] [Google Scholar]
- 80.Badaró MM, Bueno FL, Arnez RM, Oliveira VC, Macedo AP, Souza RF, et al. The effects of three disinfection protocols on candida spp., denture stomatitis, and biofilm: A parallel group randomized controlled trial. J Prosthet Dent. 2020;124:690–698. doi: 10.1016/j.prosdent.2019.09.024. [DOI] [PubMed] [Google Scholar]
- 81.Araujo CB, Ribeiro AB, Fortes CV, Bueno FL, Wever BD, Oliveira VC, et al. Effect of local hygiene protocols on denture-related stomatitis, biofilm, microbial load, and odor: A randomized controlled trial. J Prosthet Dent. 2021;128:664–673. doi: 10.1016/j.prosdent.2020.12.018. [DOI] [PubMed] [Google Scholar]
- 82.Hoad-Reddick G, Grant AA, Griffiths CS. Investigation into the cleanliness of dentures in an population. J Prosthet Dent. 1990;64:48–52. doi: 10.1016/0022-3913(90)90152-3. [DOI] [PubMed] [Google Scholar]
- 83.Tarbet WJ. Denture plaque: Quiet destroyer. J Prosthet Dent. 1982;48:647–652. doi: 10.1016/s0022-3913(82)80022-x. [DOI] [PubMed] [Google Scholar]
- 84.Augsburger RH, Elahi JM. Evaluation of seven proprietary denture cleansers. J Prosthet Dent. 1982;47:356–359. doi: 10.1016/s0022-3913(82)80079-6. [DOI] [PubMed] [Google Scholar]
- 85.Wefers KP. Der “Denture Hygiene Index” (DHI) Dent Forum. 1999;9:13–14. [Google Scholar]
- 86.Schubert VR, Schubert U. Der Prosthesnhygiene-Index (PHI)- eine Methode zur Dokumentation und Gesundheitserziehung. Stomatol DDR. 1979;29:29–31. [PubMed] [Google Scholar]
- 87.Samaranayake LP, MacFarlane TW. Wright‑ Butterworth; 1990. Oral candidosis. [Google Scholar]
- 88.Davies GN. The different requirements of periodontal indices for prevalence studies and clinical trials. Int Dent J. 1968;18:560–569. [PubMed] [Google Scholar]
- 89.Pretty IA, Edgar WM, Smith PW, Higham SM. Quantification of dental plaque in the research environment. J Dent. 2005;33:193–207. doi: 10.1016/j.jdent.2004.10.017. [DOI] [PubMed] [Google Scholar]
- 90.Mensi M, Scotti E, Sordillo A, Agosti R, Calza S. Plaque disclosing agent as a guide for professional biofilm removal: A randomized controlled clinical trial. Int J Dent Hyg. 2020;18:285–294. doi: 10.1111/idh.12442. [DOI] [PubMed] [Google Scholar]
- 91.Chetruş V, Ion IR. Dental plaque – classification, formation and identification. Int J Med Dent. 2013;17:139–143. [Google Scholar]
- 92.Gallagher IHC, Fussell SJ, Cutress TW. Mechanism of action of a two-tone plaque disclosing agent. J Periodontol. 1977;48:395–396. doi: 10.1902/jop.1977.48.7.395. [DOI] [PubMed] [Google Scholar]
- 93.Söder B, Johannsen A, Lagerlöf F. Percent of plaque on individual tooth surfaces and differences in plaque area between adjacent teeth in healthy adults. Int J Dent Hyg. 2003;1:23–28. doi: 10.1034/j.1601-5037.2003.00003.x. [DOI] [PubMed] [Google Scholar]
- 94.Verran J, Rocliffe MD. Feasibility of using automatic image analysis for measuring dental plaque in situ. J Dent. 1986;14:11–13. doi: 10.1016/0300-5712(86)90095-3. [DOI] [PubMed] [Google Scholar]
- 95.Rekola M, Scheinin A. Quantification of dental plaque through planimetric analysis. Scan J Dent Res. 1977;85:51–55. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.