Abstract
Objectives: This study (1) examined the natural history of learning to use learning resources by medical students and residents and (2) considered whether that history is consistent with the ways in which physicians approach their learning tasks.
Methods: The authors conducted and analyzed thirty-two open-ended interviews of first-year and third-year medical students and first-year and senior residents in internal medicine, family medicine, or pediatrics.
Results and Discussion: Learning to use learning resources occurs at the same time as learning done to address instructional and clinical problems that physicians-in-training face, with all kinds of learning following well-documented stages. Skills for using resources are developed gradually and by overcoming barriers such as time constraints and existing habits.
Conclusions: Implications of the natural history of learning to use learning resources can be employed by librarians and medical teachers to facilitate self-directed learning for physicians-in-training. Specific recommendations are provided.
INTRODUCTION
The professional practice of medicine is predicated on self-directed, lifelong learning [1], so it is critical that those responsible for teaching physicians-in-training understand the skills necessary for self-directed learning and have programs in place introducing and developing these skills [2–5]. Unfortunately, development of such programs is hindered by insufficient knowledge of how physicians-in-training develop self-directed learning skills in general and how they come to use learning resources in particular.
Broadly viewed, “learning resources” include the time and energy available for mastering new skills and knowledge and the social support needed for learning. However, the authors define learning resources more narrowly as “those human and material resources that provide learners with the facts, principles, and experiences necessary to realize meaningful learning outcomes.” Examples include textbooks, senior colleagues, and electronic journals.
Use of learning resources by self-directed learners requires a number of skills defined by Knowles [6] as the ability to: (1) identify resources, (2) design a plan for resource use, (3) make resources available, and (4) work well with teachers, peers, and other resource persons. These competencies and instruction on them have been studied in physicians and physicians-in-training [7, 8]. However, these studies do not consider how students and residents learn to use learning resources in the broader context of their ongoing medical studies.
Our goals in this study are to elucidate the natural history of learning to use learning resources and to consider whether this history is consistent with the ways in which physicians approach other learning tasks [9]. Thus, we ask questions including: (1) what circumstances trigger medical students and residents to learn to use any given learning resource?; (2) how do medical students and residents learn about the resources they use?; (3) what do they learn about these resources?; and (4) what barriers do physicians-in-training encounter in learning to use new resources?
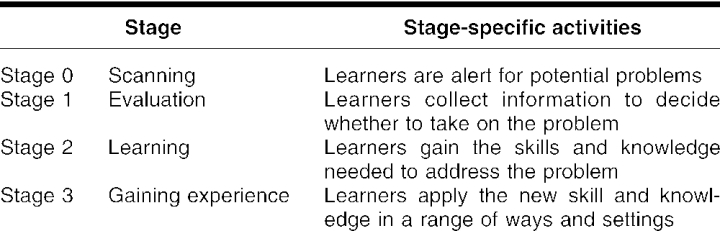
Slotnick's staged theory of physicians' learning has been selected as the theoretical framework for this study (Table 1) [9–11]. Other staged theories of physicians' learning have been suggested by Geertsma, Parker, and Whitbourne [12]; Putnum and Campbell [13] with further development by Bennett and Fox [14]; and Garcia and Newsom [15]. However, these theories are limited to learning that leads to practice change versus everyday learning that may or may not result in change of behavior. Further, Slotnick's theory is the only one that considers episodes that end early, and existing evidence suggests this theory is helpful in understanding how physicians-in-training learn [16].
Table 1 Stages of physicians' self-directed learning [9]
The natural history of learning to use learning resources will clarify why physicians-in-training are or are not able to use resources and how instruction influences when and how these resources are used. It will also explain preferences for particular resources among physicians-in-training [17, 18] and physicians [19–21]. Conclusions based on the aforementioned studies show that physicians prefer learning resources that are familiar, accessible, clinically relevant, and time efficient. The natural history of learning to use learning resources should explain how learners come to see resources as having these attributes. Finally, implications of our study bear on the development of skills for lifelong learning in medicine and should be of interest to medical educators, librarians, physicians-in-training, and physicians.
METHODS
We conducted a qualitative study using open-ended, semi-structured interviews of physicians-in-training. This study was a part of a larger project documenting physicians', residents', and medical students' approaches to learning.
Study participants were randomly selected from lists of first-year and third-year medical students of the University of Wisconsin Medical School and first-year and senior residents in internal medicine, family medicine, or pediatrics residency programs affiliated with the University of Wisconsin–Madison. We interviewed eight people in each group, because previous experiences [9, 10] suggested this number of interviewees would lead to theoretical saturation [22].
We asked respondents to describe how they approached situations (i.e., problems) where they needed new skills or knowledge without regard to whether the situations were specific (i.e., related to an individual patient) or general (i.e., related to a body of skill and knowledge). Interview questions included those specifically focused on learning resources (e.g., “when did you first start to use this [given] learning resource?”), and we anticipated that resources would also be considered in response to other questions (e.g., “what happened when you applied what you'd learned?”). To facilitate interviewees' reflection about what they were describing, we asked the same questions in different ways until interviewees could not recall any new details.
All interviews were conducted by a single researcher with each interview taking about an hour. Interviews were tape recorded, each tape was transcribed, and the transcript was proofed against the original tape. In addition, summaries of senior residents' interviews were prepared and read back to them to ensure that our interpretations were correct. However, we stopped doing this because the occasional changes identified from the feedback were minor, so these efforts were not worth the time invested.
We developed categories and subcategories of learning resources based on the transcripts of interviews with third-year medical students. These categories and subcategories and examples from each were used to create a coding dictionary for reviewing all thirty-two transcripts. The dictionary was also used to develop a database for identifying and recording learning resources used by interviewees. We added to and modified the dictionary and the database as required while reviewing the remaining twenty-four transcripts. To ensure consistency, categories and subcategories were discussed among the investigators.
We contacted fourteen first-year students; nine of them agreed to participate in the study and were interviewed. One interview recording was accidentally destroyed and not included in the data analysis. Eleven of forty third-year students were willing to participate, and the eight who responded first were interviewed. Forty-three interns and nineteen senior residents were invited to participate in the study: nine interns and nine senior residents agreed to participate, and, once again, the first eight in each group were interviewed. We anticipated that both first-year and third-year students had attended the medical school's library orientation tour at least once and that third-year students had likely used individual librarians' assistance and group training in conjunction with their course assignments and problem-based learning (PBL) sessions [23]. We did not examine library instruction offered in the medical schools attended by the residents.
STUDY RESULTS
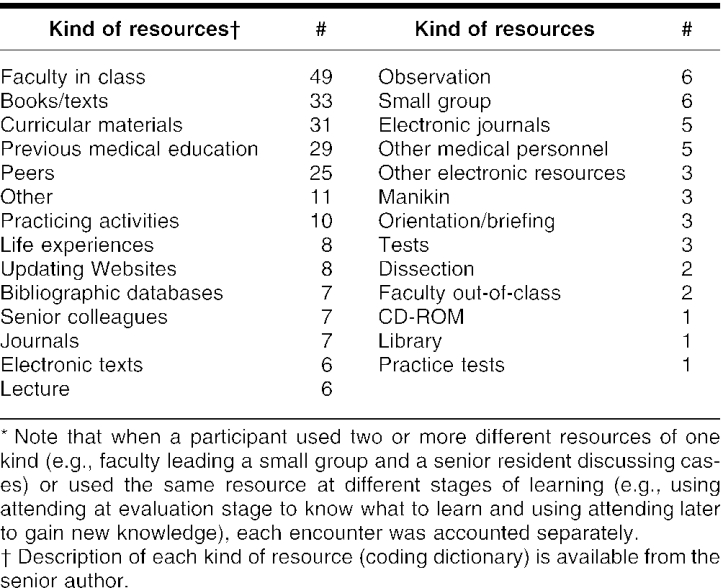
Study participants reported using twenty-seven different kinds of learning resources† (Table 2). The major categories were human resources (e.g., lectures, faculty in class, peers), electronic resources (e.g., bibliographic databases, journals accessed electronically, CD-ROM), printed resources (e.g., textbooks, journals, curricular materials), and experience (e.g., cadaver dissection, manikin intubation).
Table 2 Resources reported by study participants*
Not surprisingly, learning resources were associated with the learning environment in which they were used. For instance, first-year students utilized anatomy dissection guides in the cadaver laboratory, and both first-year and third-year students relied heavily on course syllabi. In contrast, residents, responsible for patient care, used more clinically oriented resources such as clinical specialists, bibliographic databases, and professional associations' Websites. Clearly, learning to use resources was associated with learning that addressed medical issues.
The natural history of learning to use learning resources
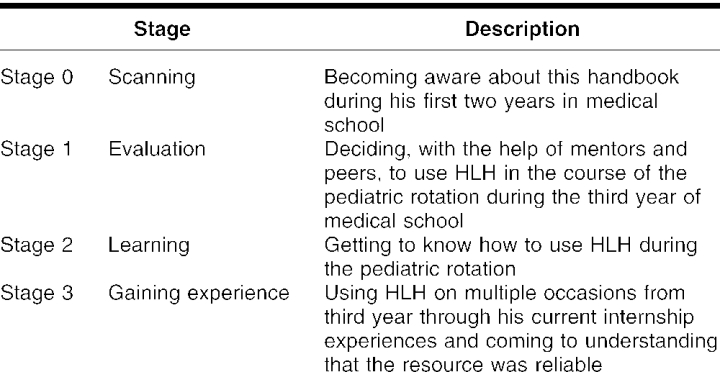
ZD‡, a family medicine intern, provides an example of how such learning occurred. He reported how he learned to use the Harriet Lane Handbook (referred to hereafter as HLH), a regularly updated compendium of diagnostic and management guidance for pediatric patients [24].
ZD first became aware of HLH through introductory clinical practice courses in his first and second years of medical school when professors mentioned it during descriptions of pediatric cases. ZD again heard about HLH from peers and mentors during discussions of pediatric patients on his third-year pediatric rotation. His recollection of HLH at that time included the criteria he used to evaluate the handbook's utility:
Harriet Lane Handbook is something that I've had, ah…referred to me by my peers and, ah, by my mentors as being a reliable source of information, ah, as not being, ah…subject to errors and, you know, it's generally been well-reviewed, so it's not something where, you know, numbers, or frequencies, or other parameters will be misquoted, it's generally, you know, [a] fairly trustworthy resource. (ZD)
Thus, ZD started to use HLH during his third year. In the course of using it, he learned that while it was good for identifying well-established treatment courses, it was not useful in producing a broad differential diagnosis. An in-depth reference text like Kliegman, Nieder, and Super's book [25] was more appropriate on those occasions. During internship when ZD assumed responsibility for patient care, he concluded that the handbook was a fairly trustworthy resource, because (1) he did not have any negative outcomes from using what he had learned from the book and (2) information available elsewhere was not in conflict with what was provided by this handbook. As a result, he made sure HLH was around when he expected to see pediatric patients.
ZD first heard about HLH in connection with pediatric cases but did not use it until he needed to know how to deal with patients' problems. He did not become comfortable with this resource, however, until he had used it multiple times to solve a variety of clinical problems. This example is typical of what we learned from other interviewees in that learning resources were commonly introduced to medical students and residents over time and through a variety of sources such as curricula, orientation, senior colleagues, and peers. Interviewees, however, did not start using these resources until they actually needed them. More specifically, learning to use basic sciences–oriented resources happened earlier in medical school, whereas clinically oriented resources were used later in medical school and during residency, when physicians-in-training become responsible for patients. In both basic and clinical instances, participants learned how to use those resources largely on their own and through experience with the resources.
A few participants reported that their first use of a new learning resource was crucial in deciding whether to use the resource again. For example, FT, a third-year student, observed, “I generally don't go back to anything that I didn't think was a help…the first time.”
Skills acquired while learning to use learning resources
First, physicians-in-training developed a range of skills as they learned how to use learning resources to address multiple needs. Besides solving clinical problems, these needs included meeting teachers' expectations (e.g., that particular resources are acceptable), demonstrating proficiency to attendings and others (e.g., residents and nurses), and satisfying other needs that varied from episode to episode (e.g., locating patients' handouts through the Internet).
Second, learning about particular learning resources contributed to learners developing strategies for using the resources. These strategies were often learned incidentally (i.e., they were not the learner's immediate focus [26]), with incidental learning to use resources having two components: “a pattern in terms of how I look for information and where I look for it” (VV, a family medicine senior resident). In other words, the process allowed students and residents to know how and in which order to use resources. Students and residents figured out where to place a new learning resource among other familiar resources by considering the resource's reliability (e.g., HLH for well-established treatment courses), accessibility (e.g., SJ, a family medicine intern, observed that residents “are right there, so they're a resource I use very often”), clinical applicability (e.g., “the quick reference guide I've used…[was] more relevant to what I see in a hospital vs…references that I find more useful and efficient in the clinic,” PK, a family medicine senior resident), and time (e.g., “that's what I was looking for…in the amount of time that I had,” UP, a third-year student, commenting on a text accessed through MD Consult).
Third, study participants also developed skills for relating information from any one resource to that gained from other resources (e.g., information from articles with feedback provided by senior colleagues). Finally, physicians-in-training learned to ensure the availability of trusted learning resources when possible (e.g., by carrying a pocket-size handbook).
Barriers to learning to use learning resources
Some medical students and residents reported hesitancies in learning to use new resources. Though lack of time was an issue (PK, a family medicine senior resident, could not find Web-based information quickly enough to avoid having patients “waiting forever”), a more commonly reported barrier was success using already familiar resources. As a case in point, VS, a pediatric senior resident, reported:
I guess I've gotten comfortable with about three or four different resources and I just go back to these resources. Not that I'm not willing to learn something new, but I think the ones that I have now are adequate for what I need in terms of my research right now.
This practical philosophy of “if it ain't broke, don't fix it” suggested that successful use of familiar resources results in resistance to considering other resources.
Physicians-in-training were also resistant or reported experiencing difficulty when use of new resources required revising the ways that they approached learning from similar resources in the past. This was the case with interns' use of human resources. Reflecting on what to do when there was no best evidence to support clinical decisions (e.g., the approach was too new to be well-studied, or equally credible sources provided conflicting recommendations) caused interns to become more epistemologically sophisticated [27] and realize that no single truth exists in medical practice:
Now that I've worked with more attendings, I realized that…everybody does things differently, there is not just one way of doing things, and it doesn't make it right or wrong, necessarily. (SJ, an intern)
This understanding represents the intern's growth from viewing senior colleagues as “gold standard” resources to a more critical perspective about human resources that the intern will need to function independently after residency training. However, this growth is often a painful experience for physicians-in-training, because they have to look at senior colleagues as less authoritative and more human. They now understand they have to rely more heavily on their own information seeking and judgments, because the suggestions of others are less reliable than they had previously understood them to be.
DISCUSSION
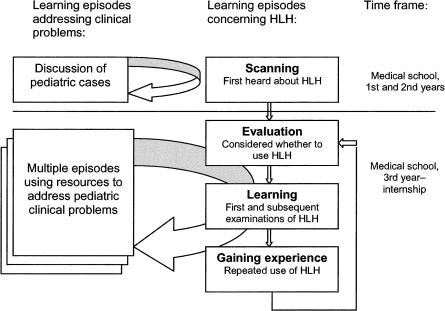
The interviewees told us that the ways they used familiar resources were most likely to develop gradually and, we assert, in stages. In particular, we found their descriptions consistent with the four stages of physicians' self-directed learning presented in the introduction. ZD's learning to use HLH, for example, can be reframed as shown in Table 3 and Figure 1.
Table 3 Stages of ZD's learning to use the Harriet Lane Handbook (HLH)
Figure 1.
The dynamics of learning to use HLH in relation to learning about clinical problems Note that each clinical problem learning episode (represented by the arrows) went through its own scanning, evaluation, learning, and gaining experience stages independently of which stage the learner was at viz learning to use HLH.
Figure 1 shows that at any given time the learner is simultaneously at one stage in learning how to use HLH and another regarding the clinical problem under consideration. ZD, for example, was at the evaluation stage in addressing a clinical problem during his third-year pediatric rotation and at the evaluation stage with HLH, when he considered the resources available to learn the solution to a clinical problem. Though he had heard of HLH before, this was the first time he considered using it. He used what he had heard from his mentors and peers in deciding to use HLH, moved to the learning stage immediately after he was introduced to the handbook, and then moved to the gaining experience stage when he applied what he found. Clearly, while this initial learning episode, focusing on a specific clinical problem, played an important role in ZD's learning to use HLH, he repeated the cycle of using HLH to solve subsequent clinical problems while still remaining at the gaining experience stage in learning to use HLH.
The stories shared by the study participants clarified the competencies of self-directed learners in using resources as defined by Knowles [6]. For instance, physicians-in-training developed strategies for attacking clinical problems, with each new resource occupying a certain place in the constellation of familiar resources as determined by its accessibility, clinical applicability, familiarity, and return on the time required by this resource—the same characteristics of learning resources that physicians prefer [20, 21, 28–30].
In addition to Knowles's four competencies, we have found that integrating information from multiple resources is an important ability that physicians-in-training develop while learning to use learning resources. We consider that development of this synthetic ability, as well as the ability to evaluate the reliability of the resource and its relevance to particular types of problems, develops concurrently with the abilities of physicians-in-training to reflect and think critically. More specifically, we agree with Brockbank and McGill [31] that reflection is the process by which experiences are considered through thoughts, feelings, or actions both in the moment (Schön's [32] reflection-in-action) and afterward (reflection-on-action). The process of critical thinking is thus a subset of reflection involving logical inquiry and problem solving leading to an evaluative decision or action (Committee on Critical Thinking and the Language Arts, National Council of Teachers of English [33]).
Returning to ZD's learning about HLH, his reflection on HLH was first seen in considering whether to use it and then in evaluating the reliability of what he learned from it. ZD's reflection relied on his senior colleagues and peers in judging the resource's reliability, because that was all his limited experiential background allowed. He simply noted, for example, that HLH was peer reviewed, and he had been told that was a good thing. Only later in medical school and during internship, when ZD's evaluation became based on his experiences (both with HLH specifically and with caring for patients more generally), could he consider the book in a more sophisticated manner. This was also the time when he began thinking critically about treatment options in HLH as they related to suggestions from other resources.
ZD's experiences and conclusions from previous research indicate that physicians-in-training develop reflection and critical thinking skills gradually [34, 35] and as a part of their personal development [27]. Thus, it would be unreasonable to expect learners' competencies in adopting learning resources to develop in a short period of time (e.g., during introductions to the medical library during the first year of medical school), and, indeed, the majority of study participants' histories of learning to use learning resources covered more than two years.
According to Hiemstra and Brockett [36], learners themselves could be sources of resistance to self-directed learning, and this was the case with our study participants. We also found that reflection and critical thinking were necessary to overcome their resistance, as was apparent in those instances cited earlier where study participants found that the resources they had selected did not work. We conceptualize the approaches learners have to using resources as “schemata”: mental structures in which a person stores knowledge about and procedures for using (in the current case) learning resources [37]. In most cases, schemata grew by “assimilation” [38], when current experiences and insights were simply incorporated into existing schemata (e.g., ZD adding to his corpus of experience using HLH). However, schemata sometimes did not work, they had to be revised (i.e., accommodated), as happened when SJ changed the way in which she used human resources.
Accommodation requires both cognitive and affective efforts, and renovating a schemata represents a barrier when it keeps physicians-in-training from learning to use new resources or makes it difficult for them to move from one stage to another in their learning. Thus, a triggering event [12, 39], commonly experienced as unsettling, is often needed to facilitate development of new, more sophisticated schemata that allow physicians-in-training to be better self-directed learners.
Study limitations and future research
This study was part of a larger project documenting the approaches of physicians-in-training to learning about medical issues; the overall study did not focus specifically on how people learn to use learning resources. Whereas interview questions facilitated interviewees' detailed responses about learning to use selected learning resources, their stories, as a result, were incomplete in regard to learning to use all the resources they mentioned. In addition, the data analyzed in this study were medical students' and residents' self-reports and were limited by their recall and their need to look professional to the interviewer.
We have no evidence bearing on the degree to which the two limitations hamper our findings. Further, and beyond replicating this study to confirm or disconfirm its findings, we believe that future research on the natural history of learning to use learning resources should address at least four questions:
Under what circumstances does learning to use a new resource require accommodation versus assimilation of schemata?
How do physicians-in-training know when they learn enough about any given learning resource?
How do physicians-in-training know they do want to use the resource again?
When do physicians-in-training stop using a familiar learning resource?
Study implications
We offer the following suggestions for educators helping physicians-in-training develop their self-directed learning skills:
-
Provide stage-appropriate instruction to help physicians-in-training learn to use learning resources:
Scanning and evaluation stages: It is important to understand that physicians-in-training learn about learning resources during these stages; they do not learn how to use these resources until the learning and gaining experience stages. Thus, orientation sessions, references to resources in course or rotation materials, library tours, library catalog instructions, computer skills trainings, and MEDLINE classes are only useful for making physicians-in-training aware of resources they may use as learners in the future. Such awareness should highlight the information that librarians and medical teachers want them to recall later when they consider where to find answers to problems they encounter.
Learning and gaining experience stages: Appropriate instruction at these stages has to integrate medical and library curricula (e.g., through librarians' involvement in morning report described by Atlas, Smigielski, Wulff, and Coleman [40] or the self-directed two-hour library open houses proposed by Walton, Westphal, Lauer, Munson, and Shedlock [41]); role modeling by attendings; assistance and feedback from medical teachers and librarians regarding use of learning resources (e.g., as components of mentorship, preceptorship, small group teaching, and journal clubs); and peer group exercises requiring physicians-in-training to reflect on their use of learning resources (e.g., students' reflections facilitated by residents). Failure to recognize that students and residents are focused on problems they face and not on learning resources predisposes against success in helping them use new resources.
-
Emphasize in instruction:
critical evaluation of learning resources (e.g., how physicians-in-training know that the resource is reliable)
self-reflection regarding information-seeking strategies and use of learning resources (e.g., how physicians-in-training recognize that they have enough information to address the problem that precipitated learning)
development of abilities to scan the environment for new learning resources (e.g., by reading and discussing journals and interacting with colleagues)
awareness of the stages that physicians-in-training go through in their learning to use learning resources and the challenges they may encounter (e.g., the need to accommodate schemata and time constraints as described by medical faculty)
-
Create supportive learning environments where:
reflection, feedback, and collaboration are welcomed;
human resources (e.g., senior colleagues, teachers, librarians) are approachable;
printed and Web-based resources are available; and
time for learning to use learning resources is ensured.
CONCLUSION
Three conclusions can be drawn from our study. First, effective use of clinically oriented learning resources is a part of being successful, self-directed, lifelong learners in medicine, and medical school and residency are critical in learning to use learning resources. Second, learning to use a learning resource is a staged process, where physicians-in-training become aware of a learning resource at the scanning stage, decide to start using this resource at the evaluation stage, learn how to use this resource at the learning stage, and advance their skills related to use of learning at the gaining experience stage. Third, knowing the stages and barriers related to skills for learning resource use is essential to consider in planning educational interventions to help physicians-in-training develop self-direction. Key points from our study are (Figure 2):
The natural history of learning to use learning resources is inseparable from the learning that physicians-in-training do to address problems they face in medical school and residency
Learning to use resources includes developing skills to identify a resource as useful for addressing the problems at hand as well as associated problems (e.g., satisfying the attending), developing a strategy for using each given resource, making a resource available, and integrating the information provided by one resource with information gained from other resources.
Learning to use a resource is well described as the staged process of scanning, evaluation, learning, and gaining experience.
Physicians-in-training use curricula, orientation sessions, senior colleagues, and peers during scanning and evaluation stages of learning to use resources, and they actually learn how to use resources and gain experience with them by practicing and reflecting on their practice.
Progress through these stages often requires years and occurs in concert with developing critical thinking and reflection skills.
The first practical experience of using a learning resource is often important for success in learning to use the resource, because it bears on whether the resource will be used again.
The lack of time to devote to a new resource, the habit of using familiar resources only, and the need to accommodate schemata concerning ways to use learning resources can be barriers to learning how to use new resources for physicians-in-training.
Figure 2.
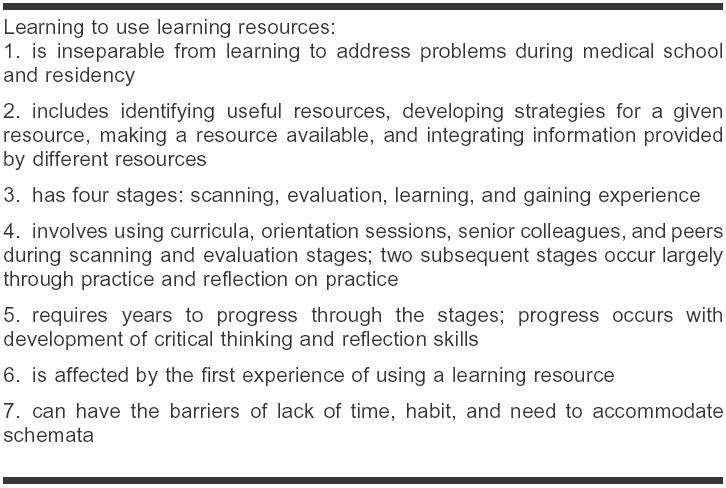
Key points learning to use learning resources
Acknowledgments
The authors gratefully acknowledge Anne Taylor-Vaisey's insightful comments on early drafts of this paper. This report is much stronger because of her efforts.
Footnotes
* This research was supported by the Educational Research and Development grant from the University of Wisconsin and approved by the University of Wisconsin Health Sciences Human Subjects Committee.
† These resources were used in learning episodes described by study participants. None of the episodes was part of problem-based learning.
‡ Interviewees are identified with randomly generated two-letter pseudonyms. The word “ah” is used to represent verbalization such as “ah,” “um,” and the like, and ellipsis (…) represents pauses and not deleted words or phrases. Words in [brackets] are added for clarification.
Contributor Information
Marianna B. Shershneva, Email: mbshershneva@wisc.edu.
Henry B. Slotnick, Email: hbslotnick@wisc.edu.
George C. Mejicano, Email: mejicano@facstaff.wisc.edu.
REFERENCES
- Hilton S, Slotnick HB. Professionalism and proto-professionalism: a new view of professionalism in physicians-in-training and physicians. Presented at: AMEE 2003 Relevance in Medical Education Conference; Bern, Switzerland; Sep 2003. [Google Scholar]
- Chessell G. Medical education: using interactive learning. J Audiov Media Med. 1994 Apr; 17(2):77–80. [DOI] [PubMed] [Google Scholar]
- Davis D, Barnes BE, and Fox R. eds. The continuing professional development of physicians: from research to practice. Chicago, IL: The American Medical Association Press, 2003. [Google Scholar]
- Merriam SB, Caffarella RS. Learning in adulthood: a comprehensive guide. 2nd ed. San Francisco, CA: Jossey-Bass Publishers, 1999. [Google Scholar]
- West DC, Pomeroy JR, Park JK, Gerstenberger EA, and Sandoval J. Critical thinking in graduate medical education: a role for concept mapping assessment? JAMA. 2000 Sep 6; 284(9):1105–10. [DOI] [PubMed] [Google Scholar]
- Knowles MS. Fostering competence in self-directed learning. In: Smith RM, ed. Learning to learn across the life span. San Francisco, CA: Jossey-Bass Publishers, 1990. [Google Scholar]
- Osman LM, Muir AL. Computer skills and attitudes to computer-aided learning among medical students. Med Educ. 1994 Sep; 28(5):381–5. [DOI] [PubMed] [Google Scholar]
- Shelstad KR, Clevenger FW. On-line search strategies of third year medical students: perceptions vs fact. J Surg Res. 1994 Apr; 56(4):338–44. [DOI] [PubMed] [Google Scholar]
- Slotnick HB. How doctors learn: physicians' self-directed learning episodes. Acad Med. 1999 Oct; 74(10):1106–17. [DOI] [PubMed] [Google Scholar]
- Slotnick HB.. How doctors know when to stop learning. Med Teach. 2000;22(2):189–96. [Google Scholar]
- Slotnick HB. How doctors learn: education and learning across the medical-school-to-practice trajectory. Acad Med. 2001 Oct; 76(10):1013–26. [DOI] [PubMed] [Google Scholar]
- Geertsma RH, Parker RC, and Whitbourne SK. How physicians view the process of change in their practice behavior. J Med Educ. 1982 Oct; 57(10 pt 1):752–61. [DOI] [PubMed] [Google Scholar]
- Putnum RW, Campbell MD. Competence. In: Fox RD, Mazmanian PE, Putnam RW, eds. Changing and learning in the lives of physicians. New York, NY: Praeger, 1989. [Google Scholar]
- Bennett NL, Fox RD. Challenges for continuing professional education. In: Curry L, Wergin JF, eds. Educating professionals: responding to new expectations for competence and accountability. San Francisco, CA: Jossey-Bass Publishers, 1993:262–78. [Google Scholar]
- Garcia R, Newsom R. Learning and change among emergency physicians. J Contin Educ Health Prof. 1996 Winter; 16(1):33–41. [Google Scholar]
- Slotnick HB, Hilton S. Evidence of professional development in the learning activities of medical students, house officers, and practicing physicians. Presented at: AMEE 2003 Relevance in Medical Education Conference; Bern, Switzerland; Sep 2003. [Google Scholar]
- Cogdill KW, Moore ME. First-year medical students' information needs and resource selection: responses to a clinical scenario. Bull Med Libr Assoc. 1997 Jan; 85(1):51–4. [PMC free article] [PubMed] [Google Scholar]
- D'Alessandro MP, Nguyen BC, and D'Alessandro DM. Information needs and information-seeking behaviors of on-call radiology residents. Acad Radiol. 1999 Jan; 6(1):16–21. [DOI] [PubMed] [Google Scholar]
- Haug JD. Physicians' preferences for information sources: a meta-analytic study. Bull Med Libr Assoc. 1997 Jul; 85(3):223–32. [PMC free article] [PubMed] [Google Scholar]
- Slotnick HB, Harris TR, and Antonenko DR. Changes in learning-resource use across physicians' learning episodes. Bull Med Libr Assoc. 2001 Apr; 89(2):194–203. [PMC free article] [PubMed] [Google Scholar]
- Verhoeven AA, Boerma EJ, and Meyboom-de Jong B. Use of informational sources by family physicians: a literature survey. Bull Med Libr Assoc. 1995 Jan; 83(1):85–90. [PMC free article] [PubMed] [Google Scholar]
- Strauss AL, Corbin JM. Basics of qualitative research: grounded theory procedures and techniques. Newbury Park, CA: Sage Publications, 1990. [Google Scholar]
- Hooper-Lane C. Personal communication. 2004. [Google Scholar]
- Gunn VL, Barone MA. eds. The Harriet Lane handbook: a manual for pediatric house officers. 16th ed. Philadelphia, PA: Mosby, 2002. [Google Scholar]
- Kliegman R, Nieder ML, and Super DM. Practical strategies in pediatric diagnosis and therapy. Philadelphia, PA: W. B. Saunders, 1996. [Google Scholar]
- Marsick VJ, Watkins KE. Informal and incidental learning. In: Merriam SB, ed. The new update on adult learning theory. San Francisco, CA: Jossey-Bass Publishers, 2001. (New Directions for Adult and Continuing Education, 89). [Google Scholar]
- King PM, Kitchener KS. Developing reflective judgment: understanding and promoting intellectual growth and critical thinking in adolescents and adults. San Francisco, CA: Jossey-Bass Publishers, 1994. [Google Scholar]
- Casebeer L, Bennett N, Kristofco R, Carillo A, and Centor R. Physician Internet medical information seeking and on-line continuing education use patterns. J Cont Educ Health Prof. 2002 Winter; 22(1):33–42. [DOI] [PubMed] [Google Scholar]
- Dee C, Blazek R. Information needs of the rural physician: a descriptive study. Bull Med Libr Assoc. 1993 Jul; 81(3):259–64. [PMC free article] [PubMed] [Google Scholar]
- Thompson ML. Characteristics of information resources preferred by primary care physicians. Bull Med Libr Assoc. 1997 Apr; 85(2):187–92. [PMC free article] [PubMed] [Google Scholar]
- Brockbank A, McGill I. Facilitating reflective learning in higher education. Buckingham, UK: Open University Press, 1998. [Google Scholar]
- Schön DA. Reflective practitioner. San Francisco, CA: Jossey-Bass Publishers, 1983. [Google Scholar]
- Fowler B. Critical thinking definitions. [Web document]. [cited 20 Jul 2003]. <http://www.kcmetro.cc.mo.us/longview/ctac/definitions.htm>. [Google Scholar]
- Scott JN, Markert RJ, and Dunn MM. Critical thinking: change during medical school and relationship to performance in clinical clerkships. Med Educ. 1998 Jan; 32(1):14–8. [DOI] [PubMed] [Google Scholar]
- Sobral DT. An appraisal of medical students' reflection-in-learning. Med Educ. 2000 Mar; 34(3):182–7. [DOI] [PubMed] [Google Scholar]
- Hiemstra R, Brockett RG. Overcoming resistance to self-direction in adult learning. San Francisco, CA: Jossey-Bass Publishers, 1994. [Google Scholar]
- West CK, Farmer JA, and Wolff PM. Instructional design: implications from cognitive science. Englewood Cliffs, NJ: Prentice Hall, 1991. [Google Scholar]
- Piaget J. Origins of intelligence in children. New York, NY: International Universities Press, 1952. [Google Scholar]
- Fox RD, Mazmanian PE, and Putnam RW. eds. Changing and learning in the lives of physicians. New York, NY: Praeger, 1989. [Google Scholar]
- Atlas MC, Smigielski EM, Wulff JL, and Coleman MT. Case studies from morning report: librarians' role in helping residents find evidence-based clinical information. Med Ref Ser Q. 2003 Fall; 22(3):1–14. [DOI] [PubMed] [Google Scholar]
- Walton L, Westphal T, Lauer B, Munson K, and Shedlock J. No more tours: how library tours of the past become today's celebrations. Med Ref Serv Q. 2001 Spring; 20(1):39–48. [DOI] [PubMed] [Google Scholar]