Abstract
Background/purpose
External cervical resorption (ECR) is an aggressive form of root resorption, which etiology is unclear and its prognosis remains unpredictable. The purpose of this study was to investigate the prognosis and potential prognostic factors of ECR-affected teeth after surgical intervention for external repair with/without root canal treatment.
Materials and methods
Treated ECR cases from 2009 to 2019 were collected retrospectively. The survival of the teeth and the status of root resorption were assessed during the follow-up period. Potential prognostic factors were analyzed with log-rank test and Kaplan–Meier statistics.
Results
A total of 42 treated ECR-affected teeth were enrolled. The two-year survival rate was 71.20% [54.16%, 93.59%]. Persistent root resorption was the main complication after treatment. Patients with multiple ECR-affected teeth had greater recurrent potential than patients with solitary ECR-affected teeth. Prolonged calcium hydroxide dressing may contribute to a more favorable clinical outcome. Gender, age, tooth position and the need for root canal treatment did not show statistically significant effect on the prognosis.
Conclusion
The current surgical method was able to arrest ECR in most cases. However, the case type (the number of ECR-affected teeth per patient) could highly affect the prognosis of the teeth. Clinicians should consider long-term calcium hydroxide dressing in case of pulp involvement to achieve better results.
Keywords: External cervical resorption, Root canal treatment, Surgical repair, Calcium hydroxide, Recurrence
Introduction
External cervical resorption (ECR) is an aggressive form of root resorption (RR), which initiates from the external cervical area of the tooth. Its aetiology is mostly related to traumatic injury and orthodontic treatment.1, 2, 3 Some other factors such as tooth bleaching, periodontal treatment, and probably systemic disease problems were also possible aetiology.2,4,5 Typically, early ECR-affected teeth are asymptomatic and show no obvious visual signs.6 Probing depth more than three millimetres and chronic gingival abscess are occasionally noted at the mature stages. A scalloped-like radiolucency with well-defined or irregular border can be noted around the cervix of the tooth.7,8 The diagnosis of ECR is achieved by medical and dental history taking, clinical examination, and radiographic assessment.9
ECR is managed by various approaches depending on the location, extent, size, accessibility of the lesion, and proximity of the decay to the root canal system.1,6,9, 10, 11 Surgical repair alone is commonly performed in mild ECR, while surgical or non-surgical repair combined with endodontic treatment is indicated in case that the lesion approaches near the pulp and in case of pulp and periapical pathosis. Intentional replantation and orthodontic extrusion are also feasible.6,12,13 Severe tooth structure loss in advanced cases make the tooth unrestorable; thus, periodic review or tooth extraction is often suggested.6
The treatment of ECR is in fact really challenging. One main treatment goal of ECR is to arrest the resorptive process. However, recurrence of resorption after treatment were reported in previous studies1,14 and several case reports.15,16 Tooth fracture was another complication after treatment.1 The invasion of biological width may be another concern because the restorations are placed close to the bone margin.17 Although the treatment recommendation for ECR has now been established according to Heithersay or Patel's classification, the treatment outcome and prognosis of disease remains unpredictable, especially those cases in advanced stages.
Up to now, there is still limited studies inspected the treatment outcomes and analyzed the prognostic factors of ECR cases.1,11,14,18 The purpose of our study was to investigate the prognosis of ECR-affected teeth after surgical intervention for external repair with/without root canal treatment (RCT) and to analyze the potential prognostic factors, in order to help clinicians in clinical decision, treatment planning, and improving the treatment procedures.
Materials and methods
Case collection and screening
This study was conducted with the approval of the Research Ethic Committee of National Taiwan University Hospital (IRB number: 201909004RINB). As described in our previous study,4 63 ECR-affected teeth from 31 patients from 2009 to 2019 were collected in the Department of Dentistry, National Taiwan University Hospital. The diagnosis was confirmed by 3 individual observers through radiographic examination, and consensus was reached through discussion in case of disagreement.
Inclusion and exclusion criteria
The included ECR cases should be treated with surgical intervention by certified endodontic or periodontal specialists, or by post-graduate dentists under specialist training program. The patients were recalled every three to six months for clinical and radiographic evaluation. A minimal of three-month follow-up after the completion of treatment was required. The exclusion criteria were: teeth extracted soon after the discovery of disease, ECR-affected teeth treated through an internal repaired only, teeth which were undergoing clinical observation and did not receive any forms of repair, and teeth which received surgical treatment but had soon lost from follow-up.
Data registration
Excel 2016 (Microsoft, Seattle, WA, USA) was used for data registration. The following information was recorded: age, gender, case type, affected tooth position, pulp vitality, probing depth, type of restorative material, and duration of intracanal calcium hydroxide dressing before repair. The case type was defined by the cumulated incidence of ECR-affected teeth in the same patient at the latest follow-up. A patient with a single ECR-affected tooth was classified as a “solitary ECR case,” whereas a patient with more than one ECR-affected tooth was classified as a “multiple ECR case.”
Treatment procedure
For lesions distant from the pulp (mainly Heithersay class I, or Patel 1–2/A-B/d), surgical repair was performed first.1,6 The vitality of the tooth would then be monitored during the follow-up visits, to determine the need of subsequent RCT. The main surgical procedure was described below.
-
1)
Administration of local anaesthesia
-
2)
Elevation of full-thickness flap
-
3)
Removal of the granulation tissue
-
4)
Gentle cavity preparation to avoid perforating the root canal
-
5)
Restoration with composite resin, glass ionomers, mineral trioxide aggregate (MTA), Biodentine, or in combinations.
For lesions near the pulp (Heithersay class II to IV lesions in general, or Patel 1–2/A-C/p), RCT were mainly initiated prior to the surgery (Fig. 1). If the lesions extended intraosseously, osteotomy was performed to expose the entire cavity and facilitate the approach of dental instruments. Enamel matrix derivative (Emdogain, Biora AB/Straumann, Switzerland) was occasionally conducted for periodontal tissue regeneration. A second surgery may be arranged if the resorption continued after the first surgery.
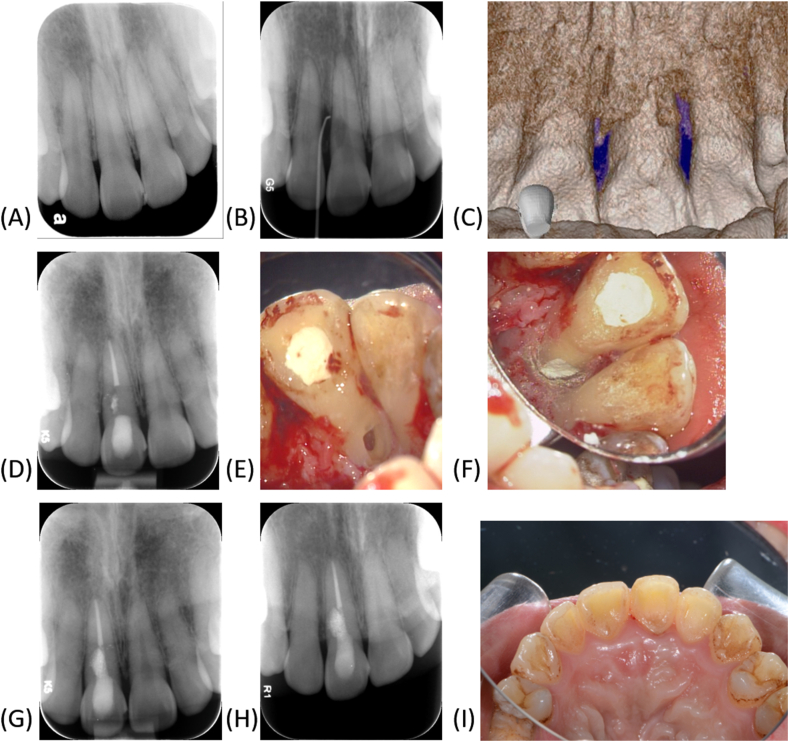
Figure 1.
A case of ECR-affected incisor with previous traumatic history. (A) The patient asked for assessment of maxillary anterior teeth after dental trauma. The mesial incisal angle was chipped away. No obvious cervical resorption was noted. (B) One year later the patient came to our department with a chief complaint of gingival swelling in maxillary anterior area for two weeks. A gutta percha point traced to the ECR in tooth 11 through the sinus tract. (C) CBCT showed that ECR was located at the disto-palatal side of the tooth. (D) Root canal treatment (RCT) was performed first and the gutta percha was removed below the resorption cavity. (E) Surgery was arranged. The granulated tissue was removed and the cavity was prepared. (F) The cavity was repaired with MTA and the root canal was backfilled with gutta percha. (G) Radiograph taken after the treatment. (H) 14-month follow-up. No recurrent ECR was noted in the radiograph. (I) The treatment also achieved esthetic results.
Outcome assessment
The outcome of teeth was assessed from two aspects, including the survival status of the teeth and the status of root resorption. A “survived” tooth was defined as a tooth remaining in situ. Extracted teeth were seen as “non-survived” and their reasons for extraction were noted down. The survival time for a tooth was defined as the time interval from the earliest visit, which ECR was diagnosed, to the last clinical visit (for survived tooth) or to the date of tooth extraction (for non-survived tooth).
The resorption status of all teeth was evaluated radiographically. The radiographic series of each tooth was provided to two individual observers, which were asked to compare the later radiographs to the initial ones. The individual observers determine whether the resorption was “arrested” or still continuing after the treatment. Additionally, some cases received a surgical retreatment after the first treatment course failed. In consequence, these cases underwent a second-round of evaluation for their resorption status, to determine the outcome of the retreatment. Afterwards, McNemar test and Kappa statistics were used to evaluate the inter-observer agreement. A third observer would decree the results when disagreement occurred. The arrested time for an arrested ECR was defined as the time interval from the date of the operation to the date when the latest radiograph was taken, while the arrested time for a persisting ECR was defined as the time interval from the date of the operation, to the earliest post-operative radiograph which the progression of resorption was detected. The earliest radiographs were decided by the three observers through discussion.
Statistical analysis
The statistical analysis was performed with R version 3.6.1 (The R Foundation for Statistical Computing, Vienna, Austria) through the R commander and RcmdrPlugin.survival Package.19 Survival analysis was used to evaluate the survival rate and resorption status among these teeth. Log-rant test was conducted to establish the relationship between tooth survival, resorption status, and various potential prognostic factors. P-value <0.05 was considered statistically significant. The Kaplan–Meier curves were plotted with R and STATA.
The relationship between various factors and the resorption status after surgical retreatment was not tested statistically, considering the small sample size. Only the resorption status after the initial treatment course was analyzed for the potential prognostic factors.
Results
A total of 63 ECR-affected teeth were collected within the period of 2009–2019. 42 teeth were enrolled, while the other 21 teeth were excluded. Among the 42 teeth, 10 had received a surgical retreatment. All these teeth could be divided into two groups: RCT group and non-RCT prior to a surgical intervention. The survival rate for RCT group was 76.0%, and that for non-RCT group was 76.5%. The resorption status for RCT group was 24.0%, and that for non-RCT group was 47.1%.
Tooth survival
The average follow-up period was 24.4 months (±13.5). The survival rates at 6, 12, and 24 months were 95.00% [88.48%, 100.00%], 92.36% [84.41%, 100.00%], and 71.20% [54.16%, 93.59%]. The Kaplan–Meier curves were presented in Fig. 2A. Altogether 10 teeth were extracted during the follow-up period. 8 teeth were extracted in consideration of the extensive and persisting resorption. Another 2 teeth were extracted due to tooth fracture. Respectively, they fractured around 11 months and 24 months during the post-operative period.
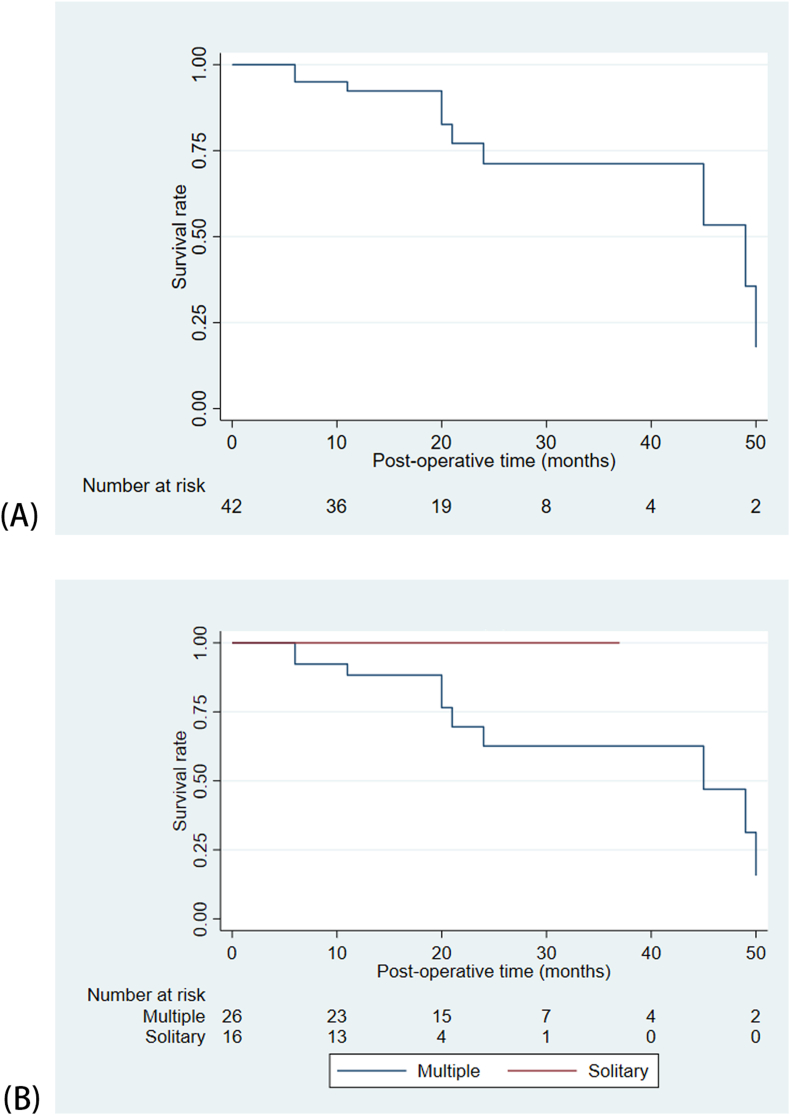
Figure 2.
Kaplan–Meier curves of the survival rate (A) Overall survival rate (42 teeth) (B) Classified according to case type.
Prognostic factors on tooth survival (Table 1)
Table 1.
Relationship between various potential predisposing factors and the survival of 42 ECR-affected teeth after initial treatment and retreatment.
| No. of ECR teeth | No. of survived teeth | P-value(Log-rank test) | |
|---|---|---|---|
| Sex | |||
| Male | 26 | 20 | 0.155 |
| Female | 16 | 12 | |
| Age | |||
| >40 years of age | 17 | 13 | 0.296 |
| <40 years of age | 25 | 19 | |
| Case type (number of ECR-affected teeth per patient) | |||
| Multiple | 26 | 16 | 0.090 |
| Solitary | 16 | 16 | |
| Tooth type | |||
| Anterior teeth | 24 | 17 | 0.108 |
| Posterior teeth | 18 | 15 | |
| Dental arch | |||
| Maxillary teeth | 35 | 25 | 0.406 |
| Mandibular teeth | 7 | 7 | |
| Probing depth before treatment | |||
| >3 mm | 24 | 20 | 0.908 |
| <3 mm | 18 | 12 | |
| Need for root canal treatment | |||
| Yes | 25 | 19 | 0.292 |
| No | 17 | 13 | |
| Duration of Ca(OH)2 dressing before repaira | |||
| >2 weeks | 14 | 14 | 0.059 |
| <2 weeks | 11 | 5 | |
| Restorative material | |||
| Composite resin or GI | 22 | 17 | 0.261 |
| MTA or Biodentine | 11 | 9 | |
| Othersb | 9 | 6 |
ECR, external cervical resorption; GI, glass ionomer cement; MTA, mineral trioxide aggregate.
Only include ECR cases which root canal treatment were needed.
Use two kinds of materials or just perform root planning without restoration.
All factors were not statistically significant. However, all of the non-survived teeth belong to Multiple-affected case type although the factor exhibited no statistical significance (P = 0.090, Fig. 2B). The duration of calcium hydroxide dressing before repair showed marginally statistical significance (P = 0.059).
Resorption status (Table 2)
Table 2.
Resorption status of the 42 ECR-affected teeth.
| Teeth after initial treatment (n = 42) | Teeth after surgical retreatment (n = 10) | ||
|---|---|---|---|
| Number of arrested root resorption | 28 | 4 | |
| Number of persisting root resorption | 14 | 6 | |
| Time interval (months) for detection of persisting ECR after treatment | |||
| Minimum | 2 | 6 | |
| First quartile | 8 | 7 | |
| Median | >38 | 10 | |
| Third quartile | >38 | >34 | |
| Maximum | 21 | 31 | |
The 2 observers had a 92.31% of proportion of agreement on deciding whether the resorption was arrested or still persistent. No statistically significant difference was found under McNemar test (P = 0.134). The Kappa value was 0.839.
The arrested rates after the first repair at 6, 10, and 12 months were 80.20% [68.80%,93.50%], 74.85% [62.48%, 89.68%], and 72.08% [59.29%, 87.63%]. The arrested rates after surgical retreatment at 6 and 10 months were 88.89% [70.56%, 100%] and 40% [17.07%, 93.76%]. The log-rank test showed that there was no statistically significant difference in the arrested rates after the initial repair and after the retreatment (P = 0.258). The progress of resorption was detected between 2 and 21 months during the follow-up period. The first quartile and median times required to detect the progress of resorption after the first treatment were 8 months and greater than 38 months, and 7 and 10 months after surgical retreatment.
Prognostic factors on resorption status (Table 3)
Table 3.
Relationship between various potential predisposing factors and the resorption status for 42 teeth after the initial treatment course.
| No. of teeth | No. of persisting root resorption teeth | P-value(Log-rank test) | |
|---|---|---|---|
| Sex | |||
| Male | 26 | 10 | 0.392 |
| Female | 16 | 4 | |
| Age | |||
| >40 years of age | 17 | 7 | 0.501 |
| <40 years of age | 25 | 7 | |
| Case type (number of ECR-affected teeth per patient) | |||
| Multiple | 26 | 14 | 0.001 |
| Solitary | 16 | 0 | |
| Tooth type | |||
| Anterior teeth | 24 | 7 | 0.537 |
| Posterior teeth | 18 | 7 | |
| Dental arch | |||
| Maxillary teeth | 35 | 14 | 0.111 |
| Mandibular teeth | 7 | 0 | |
| Probing depth before treatment | |||
| >3 mm | 24 | 6 | 0.387 |
| <3 mm | 18 | 8 | |
| Need for root canal treatment | |||
| Yes | 25 | 6 | 0.256 |
| No | 17 | 8 | |
| Duration of Ca(OH)2 dressing before repaira | |||
| >2 weeks | 14 | 0 | 0.003 |
| <2 weeks | 11 | 6 | |
| Restorative material | |||
| Composite resin or GI | 22 | 9 | 0.396 |
| MTA or Biodentine | 11 | 2 | |
| Others | 9 | 3 |
ECR, external cervical resorption; GI, glass ionomer cement; MTA, mineral trioxide aggregate.
Cases which did not require root canal treatment were excluded.
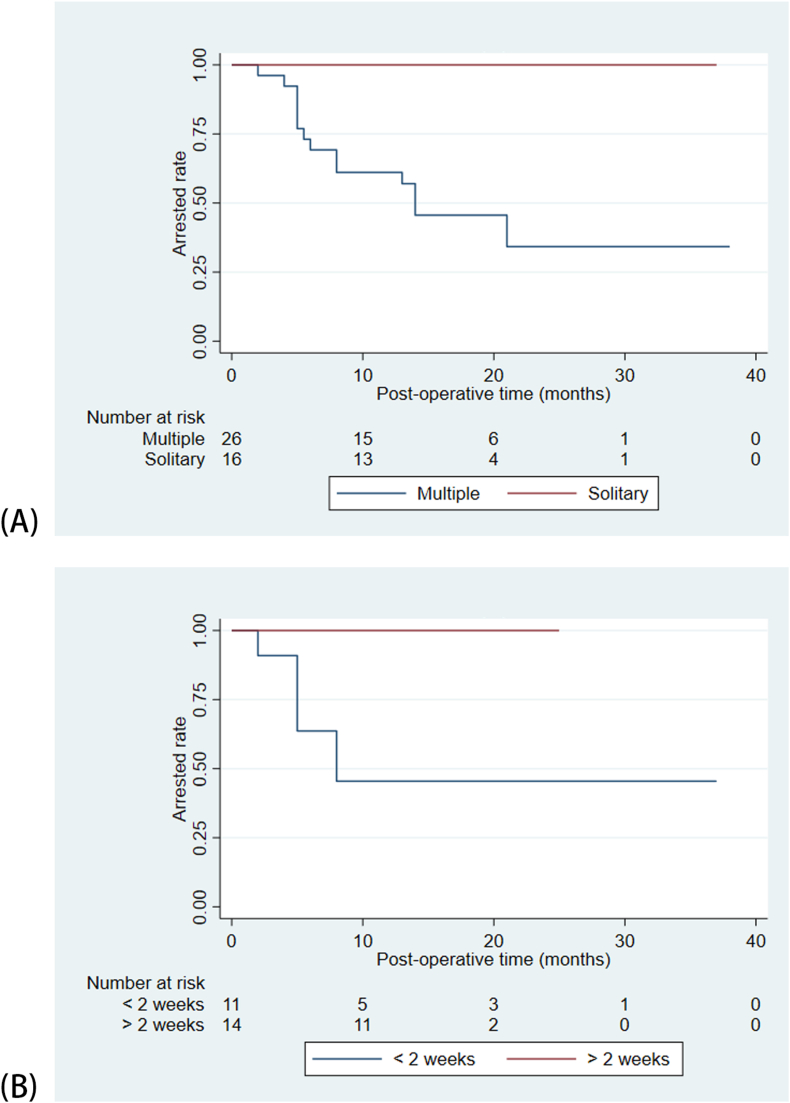
Log-rank test revealed a significant relationship between resorption status and the following variables: case type (P = 0.001), and duration of Ca(OH)2 dressing before repair (P = 0.003). Patients with solitary ECR-affected tooth (SEAT) had better outcome than patients with multiple ECR-affected teeth (MEAT) (Fig. 3A). No progression of resorption was detected in any of patients with SEAT and the overall arrested rate for patients with MEAT was 34.21%. Duration of intracanal dressing greater than 2 weeks had better prognosis than that less than 2 weeks (Fig. 3B). Sex, age, tooth position, need for RCT, and choice of restorative did not significantly affect the progression of resorption.
Figure 3.
Kaplan–Meier curves of the resorption status (A) Case type (B) Duration of calcium hydroxide dressing.
Discussion
Very limited studies had been conducted on the prognosis of ECR. Our study has given an insight into the outcome of treated ECR cases, and pointed out several associated prognostic factors, which may aid clinicians in clinical decision and treatment planning.
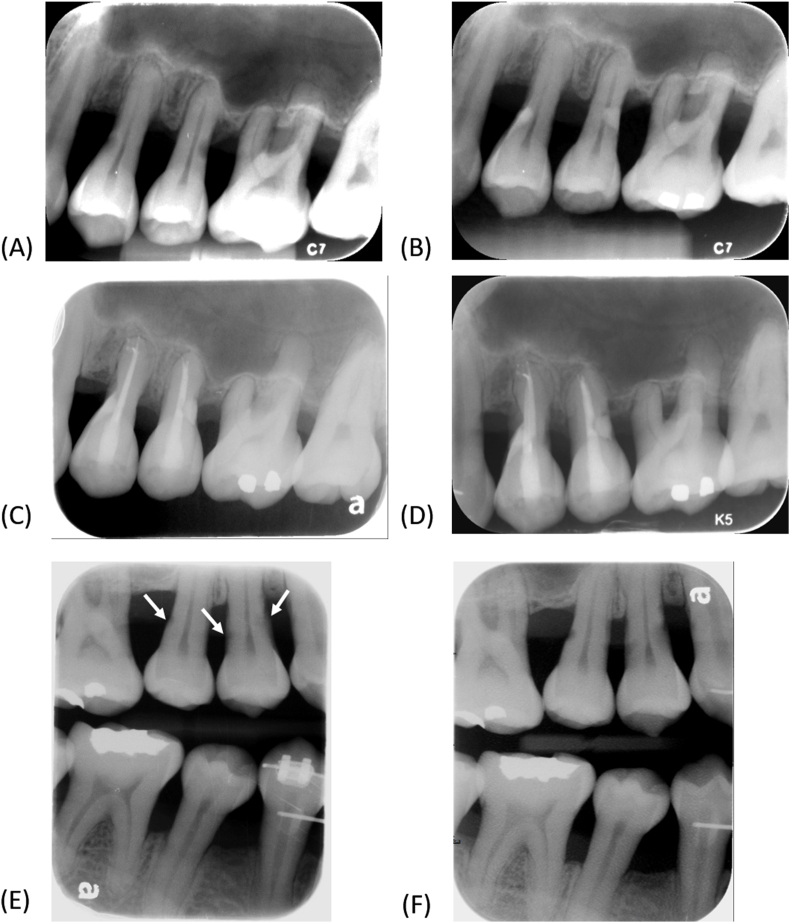
Persistent root resorption (RR) is currently the most serious concern for treatment failure (Fig. 4).1,14,15,20 In this study, the persisting resorption were mainly detected within one year after the treatment, with a median time from 5 to 8 months. However, the speed of RR varied from case by case. 2 months were enough to detect the persisting resorption in aggressive cases, while 2 years of time may be needed for chronic cases. Currently no reliable method is available to predict whether an ECR is rapidly or slowly growing. We recommend that all patients should be monitored every 1–3 months during the first year post-operatively, so that a surgical retreatment can be arranged timely before the situation gets worse.
Figure 4.
An aggressive ECR case with multiple affected teeth. (A) Initial radiograph revealed ECR in teeth 24 and 25. (B) Surgical repair was performed. The resorbed area was restored with glass ionomer cement. (C) Pulp necrosis developed and root canal treatments were completed four months after the surgery. (D) ECR recurred on the proximal surfaces of tooth 24 one year after the surgery. (E) ECR seemed to be initiating on the proximal surfaces of teeth 14 and 15 (white arrows) during the follow up period of teeth 24 and 25. (F) The resorption became obvious within one year.
The arrested rate after the first surgical attempt was 66.7%. This data was slightly lower than the previous studies14 probably related to the compositions of cases. Interestingly, we've found that ECRs in patients with MEAT have an extreme tendency to continue RR after treatment, while all cases in patients with SEAT have successfully stopped ECR from progressing (Fig. 3A). The different clinical responses imply that the nature of disease in these two groups of patients can be distinct. It has been reported that ECR in SEAT patients is more related to local stimuli, such as dental trauma and orthodontics.2,4,5 Conversely, the etiology of ECR in MEAT is more obscured and could be related to some generalized factors, such as thyroid or parathyroid disorders,4,20,21 autoimmune disease,22 elevated alkaline phosphatase,23 drug-induced and rebound effects after cessation of anti-resorptive treatment,24 viral infections, inherited genetic variants, and hormonal changes.24,25 Probably an underlying problem is kept stimulating the development of ECR, contributing to its high recurrent potential.
Our results also suggest that prolonged calcium hydroxide dressing has a positive effect on controlling ECR (Fig. 3B). Studies had shown that its hydroxyl ions can pass through the dentinal tubules as well as the perforation site, creating an alkaline environment in the periodontal tissue.26,27 Osteoclasts could barely resorb any hard tissue in pH value greater than 7.3.28 In addition, the formation of clastic cells is critically oriented by the osteoprotegerin (OPG)/receptor activator of nuclear factor Kappa B ligand (RANKL) ratio. Calcium hydroxide is able to increase the OPG expression, up-regulate the OPG/RANKL ratio, and thus prohibit the clastogenesis.29 Bacterial endotoxin can also be detoxified by calcium hydroxide, leading to an interference in the lipopolysaccharide-stimulated pathway.30,31 Studies have proposed that calcium hydroxide could prevent and inhibit inflammatory root resorption,32 yet very little studies investigated its role in ECR. In this present study, prolonged calcium hydroxide dressing could potentially reduce the recurrence of resorption in cases with pulp involvement. It is speculated that calcium hydroxide can influence the periodontal tissue through the thin dentin structure at root resorption site, and exhibit an anti-resorptive action.
Gender, tooth position, the necessity of RCT and the choice of restorative material showed no statistically significant difference on resorption control. Heithersay found that the recurrent potential increases as the ECR progresses from class I to IV.1 We found contradictive results that ECR could recur at any stage, including mild ECR, in which RCT is not required. Its recurrence seemed to be irrelevant to its size.
All ECR cases were managed through surgical (external) approach in the present study. With the surgical approach, clinicians can be more confident of the complete removal of the granulation tissue. Also, the contour of the root surface can be more properly established. In fact, non-surgical (internal) approach has been advocated to repair the cervical destruction.3,6,33 The development of endodontic microscope and ultrasonic instruments have made the non-surgical approach more feasible. This approach enables the treatment of ECR in the posterior teeth and in proximal tooth surfaces, where surgical approach would be challenging. However, it is quite doubtful whether the resorptive tissue can be removed completely or not. Moreover, many other treatment modalities had been also reported, including surgical approach followed by internal approach,34 orthodontic extrusion,12,13 intentional replantation,6,13 vital pulp therapy,35 and Nd-YAG laser therapy.36 Clinicians should make their treatment planning according to the individual clinical circumstances and their clinical skills.
In this study, most ECR-affected teeth were successfully retained after treatment. Common complications included persistent root resorption. Preoperatively, case type was the most critical prognostic factor. Patients with multiple ECR-affected teeth tended to have strong recurrent potential. Intraoperatively, our study highlighted the need of long-term calcium hydroxide dressing before repairing the resorption sit, in case of pulp involvement. Postoperatively, persisting ICRs were mainly detected within the first year after treatment. Various clinical and radiographic parameters should be considered to achieve more favorable clinical outcome.
Declaration of competing interest
The authors have no conflicts of interest relevant to this article.
Acknowledgments
This study was supported by National Taiwan University Hospital [grant numbers 109-004632, 111-S0261].
Contributor Information
Jiiang-Huei Jeng, Email: jhjeng@kmu.edu.tw.
Yi-Ling Tsai, Email: tyl.endo@gmail.com.
References
- 1.Heithersay G.S. Treatment of invasive cervical resorption an analysis of results using topical application of trichloracetic acid. Quintessence Int. 1999;30:96–110. [PubMed] [Google Scholar]
- 2.Mavridou A.M., Bergmans L., Barendregt D., Lambrechts P. Descriptive analysis of factors associated with external cervical resorption. J Endod. 2017;43:1602–1610. doi: 10.1016/j.joen.2017.05.026. [DOI] [PubMed] [Google Scholar]
- 3.Patel S., Lambrechts P., Shemesh H., Mavridou A. European Society of Endodontology position statement: external cervical resorption. Int Endod J. 2018;51:1323–1326. doi: 10.1111/iej.13008. [DOI] [PubMed] [Google Scholar]
- 4.Jeng P.Y., Lin L.D., Chang S.H., et al. Invasive cervical resorption - distribution, potential predisposing factors and clinical characteristics. J Endod. 2020;46:475–482. doi: 10.1016/j.joen.2020.01.011. [DOI] [PubMed] [Google Scholar]
- 5.Irinakis E., Aleksejuniene J., Shen Y., Haapasalo M. External cervical resorption: a retrospective case-control study. J Endod. 2020;46:1420–1427. doi: 10.1016/j.joen.2020.05.021. [DOI] [PubMed] [Google Scholar]
- 6.Patel S., Krastl G., Weiger R., et al. ESE position statement on root resorption. Int Endod J. 2023;56:792–801. doi: 10.1111/iej.13916. [DOI] [PubMed] [Google Scholar]
- 7.Patel S., Saberi N., Pimental T., Teng P.H. Present status and future directions: root resorption. Int Endod J. 2022;55(Suppl 4):892–921. doi: 10.1111/iej.13715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patel S., Mavridou A.M., Lambrechts P., Saberi N. External cervical resorption-part 1: histopathology, distribution and presentation. Int Endod J. 2018;51:1205–1223. doi: 10.1111/iej.12942. [DOI] [PubMed] [Google Scholar]
- 9.Mavridou A.M., Rubbers E., Schryvers A., et al. A clinical approach strategy for the diagnosis, treatment and evaluation of external cervical resorption. Int Endod J. 2022;55:347–373. doi: 10.1111/iej.13680. [DOI] [PubMed] [Google Scholar]
- 10.Patel S., Foschi F., Condon R., Pimentel T., Bhuva B. External cervical resorption: part 2 - management. Int Endod J. 2018;51:1224–1238. doi: 10.1111/iej.12946. [DOI] [PubMed] [Google Scholar]
- 11.Irinakis E., Haapasalo M., Shen Y., Aleksejuniene J. External cervical resorption - treatment outcomes and determinants: a retrospective cohort study with up to 10 years of follow-up. Int Endod J. 2022;55:441–452. doi: 10.1111/iej.13717. [DOI] [PubMed] [Google Scholar]
- 12.Schwartz R.S., Robbins J.W., Rindler E. Management of invasive cervical resorption: observations from three private practices and a report of three cases. J Endod. 2010;36:1721–1730. doi: 10.1016/j.joen.2010.06.011. [DOI] [PubMed] [Google Scholar]
- 13.Espona J., Roig E., Duran-Sindreu F., Abella F., Machado M., Roig M. Invasive cervical resorption: clinical management in the anterior zone. J Endod. 2018;44:1749–1754. doi: 10.1016/j.joen.2018.07.020. [DOI] [PubMed] [Google Scholar]
- 14.Jebril A., Aljamani S., Jarad F. The surgical management of external cervical resorption: a retrospective observational study of treatment outcomes and classifications. J Endod. 2020;46:778–785. doi: 10.1016/j.joen.2020.03.006. [DOI] [PubMed] [Google Scholar]
- 15.Kim Y., Lee C.Y., Kim E., Roh B.D. Invasive cervical resorption: treatment challenges. Restor Dent Endod. 2012;37:228–231. doi: 10.5395/rde.2012.37.4.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wu J., Lin L.Y., Yang J., et al. Multiple idiopathic cervical root resorption: a case report. Int Endod J. 2016;49:189–202. doi: 10.1111/iej.12440. [DOI] [PubMed] [Google Scholar]
- 17.Venuti L. Operating protocols of external root cervical resorption. G Ital Endod. 2015;29:9–29. [Google Scholar]
- 18.DeLuca S., Choi A., Pagni S., Alon E. External cervical resorption: relationships between classification, treatment, and 1-Year outcome with evaluation of the Heithersay and Patel classification systems. J Endod. 2023;49:469–477. doi: 10.1016/j.joen.2023.03.005. [DOI] [PubMed] [Google Scholar]
- 19.Fox J., Carvalho M.S. The RcmdrPlugin.survival package: extending the R commander interface to survival analysis (R package version 1.0-1) J Stat Software. 2012;49:1–32. [Google Scholar]
- 20.Neely A.L., Thumbigere-Math V., Somerman M.J., Foster B.L. A familial pattern of multiple idiopathic cervical root resorption with a 30-year follow-up. J Periodontol. 2016;87:426–433. doi: 10.1902/jop.2015.150536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Neely A.L., Gordon S.C. A familial pattern of multiple idiopathic cervical root resorption in a father and son: a 22-year follow-up. J Periodontol. 2007;78:367–371. doi: 10.1902/jop.2007.060155. [DOI] [PubMed] [Google Scholar]
- 22.Arroyo-Bote S., Bucchi C., Manzanares M.C. External cervical resorption: a new oral manifestation of systemic sclerosis. J Endod. 2017;43:1740–1743. doi: 10.1016/j.joen.2017.03.040. [DOI] [PubMed] [Google Scholar]
- 23.Iwamatsu-Kobayashi Y., Satoh-Kuriwada S., Yamamoto T., et al. A case of multiple idiopathic external root resorption: a 6-year follow-up study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100:772–779. doi: 10.1016/j.tripleo.2004.11.047. [DOI] [PubMed] [Google Scholar]
- 24.Chu E.Y., Deeb J.G., Foster B.L., Hajishengallis E., Somerman M.J., Thumbigere-Math V. Multiple idiopathic cervical root resorption: a challenge for a transdisciplinary medical-dental team. Front Dent Med. 2021;2 doi: 10.3389/fdmed.2021.652605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang N., Zhang M., Zhu J., Zhu Y., Wu J. Multiple idiopathic cervical root resorption: a systematic review. Oral Dis. 2022 doi: 10.1111/odi.14406. (in press) [DOI] [PubMed] [Google Scholar]
- 26.Fulzele P., Baliga S., Thosar N., Pradman D. Evaluation of calcium ion, hydroxyl ion release and pH levels in various calcium hydroxide based intracanal medicaments: an in vitro study. Contemp Clin Dent. 2011;2:291–295. doi: 10.4103/0976-237X.91791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shetty S., Manjunath M.K., Tejaswi S. An in-vitro evaluation of the pH change through root dentin using different calcium hydroxide preparations as an intracanal medicament. J Clin Diagn Res. 2014;8:ZC13–ZC16. doi: 10.7860/JCDR/2014/9374.4950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arnett T.R. Extracellular pH regulates bone cell function. J Nutr. 2008;138:415S–418S. doi: 10.1093/jn/138.2.415S. [DOI] [PubMed] [Google Scholar]
- 29.Han B., Wang X., Liu J., et al. Influence of calcium hydroxide–ioaded microcapsules on osteoprotegerin and receptor activator of Nuclear Factor Kappa B ligand activity. J Endod. 2014;40:1977–1982. doi: 10.1016/j.joen.2014.08.008. [DOI] [PubMed] [Google Scholar]
- 30.Silva L., Nelson-Filho P., Leonardo M.R., Rossi M.A., Pansani C.A. Effect of calcium hydroxide on bacterial endotoxin in vivo. J Endod. 2002;28:94–98. doi: 10.1097/00004770-200202000-00011. [DOI] [PubMed] [Google Scholar]
- 31.Jiang J., Zuo J., Chen S.H., Shannon Holliday L. Calcium hydroxide reduces lipopolysaccharide-stimulated osteoclast formation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:348–354. doi: 10.1067/moe.2003.18. [DOI] [PubMed] [Google Scholar]
- 32.Mohammadi Z., Dummer P.M.H. Properties and applications of calcium hydroxide in endodontics and dental traumatology. Int Endod J. 2011;44:697–730. doi: 10.1111/j.1365-2591.2011.01886.x. [DOI] [PubMed] [Google Scholar]
- 33.Shemesh A., Itzhak J.B., Solomon M. Minimally invasive treatment of class 4 invasive cervical resorption with internal approach: a case series. J Endod. 2017;43:1901–1908. doi: 10.1016/j.joen.2017.04.026. [DOI] [PubMed] [Google Scholar]
- 34.Fernandes M., Menezes L., Ataide I.D. Management of invasive cervical resorption using a surgical approach followed by an internal approach after 2 months due to pulpal involvement. J Conserv Dent. 2017;20:214–218. doi: 10.4103/0972-0707.218312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Asgary S., Nourzadeh M., Verma P., Lamar Hicks M., Nosrat A. Vital pulp therapy as a conservative approach for management of invasive cervical resorption: a case series. J Endod. 2019;45:1161–1167. doi: 10.1016/j.joen.2019.05.020. [DOI] [PubMed] [Google Scholar]
- 36.Hashizume H., Kitahara N. A case report of the healing ability of low-density Nd: YAG laser irradiation and MTA compaction on invasive cervical root resorption. J Jpn Endod Assoc. 2017;35:133–137. [Google Scholar]