Abstract
Background/purpose
Accuracy of using implant length on periapical radiographs as calibration reference for measurements has not been verified. This study aimed to verify the measurements of peri-implant crestal bone level (piCBL) on periapical radiographs taken by the paralleling technique and using the implant length for calibration; and to propose a customized crownlevel position (CLP) jig to improve the measurement accuracy of piCBL.
Materials and methods
A typodont installed an implant and a screw-retained crown at maxillary central incisor was used. To simulate piCBL, a metal post was placed near the implant at the same height of implant platform. The CLP jig was designed and 3-dimensionally printed out to allow implant projected orthogonally on periapical film. Thirty periapical radiographs were taken using paralleling technique with and without the jig by three examiners. The implant axis and implant length on radiographs were acquired by image segmentation. The discrepancy of piCBL determination (ΔD) from these measurements were compared and further analyzed when using the implant length for calibration.
Results
The piCBL measurement errors were smaller when the jig was used for all examiners (P < 0.001). The inter-rater differences were insignificant. After calibration, ΔD with and without jig were 0.09 (0.07–0.11) and 0.43 (0.38–0.49) mm, respectively.
Conclusion
Conventional long-cone paralleling technique using true implant length for calibration demonstrated imprecise piCBL measurement on periapical radiographs. Transferring the implant axis to the CLP jig allowed orthogonal projection of radiography which provided reliable measurements of piCBL with an accuracy of less than 0.1 mm.
Keywords: Crown-level position jig, Orthogonal projection, peri-Implant crestal bone level, Standardized implant periapical radiograph, 3-Dimensional printing
Introduction
Peri-implant crestal bone loss after loading is a common phenomenon.1 As the minute bone change is crucial to monitor the biological and functional response of the implant, several studies had shown the necessity of comparing the bone change with a submillimeter scale.2,3 Additionally, after the first year of service, the threshold of 0.2 mm annual bone loss is considered an important success criterion in dental implants.4, 5, 6 Conventionally, peri-implant crestal bone level (piCBL) was determined on periapical films made with the long-cone paralleling technique and using the known implant length as calibration reference. However, obtaining serial radiographs of dental implant with the identical X-ray projection is difficult to achieve in daily practice because the parallelism between the projection plane and the implant axis could be different each time. Moreover, the reliability of using the true implant length for calibration to measure distances on radiographs has never been tested.
Direct reading of piCBL on radiographs was considered unreliable if the implant axis was not projected strictly parallel to the periapical film. Three-degree vertical angulation of X-ray beam to the implant axis could introduce a more than 0.2 mm of overestimated crestal bone height.7 Further, image quality, as well as the interpreter, significantly influenced the reliability of periapical radiography measurements.8 To control the radiographic quality, it is highly recommended to make implant radiographs with a commercial film holder and a position device to keep the holder vertical to the occlusal plane. However, the implant axis is usually not perpendicular to the occlusal plane, and the production of distorted images of the implant proper is not uncommon. Although, implant length9 or pitch distance8 on radiographs are commonly used as calibration references for linear measurements, distorted implant projection may cause errors in calibrated measurements. Therefore, fixture-level position jigs were recommended for making implant periapical radiographs to obtain orthogonal implant projection,10, 11, 12, 13 which provided the image with a clear thread pattern and without superimposition of the implant platform. Thus, it was considered the most accurate periapical radiograph image to evaluate piCBL7,11,12 and the misfit of implant-abutment interface.14, 15, 16 However, using fixture-level position jigs has some limitations. First, the abutment screw should be unscrewed in advance to attach the position jig to the fixture, which is time consuming.12,13 Repeatedly disconnecting and reconnecting the abutment screw could cause biological17,18 and mechanical complications.19,20 Furthermore, fixture-level position jigs cannot be applied in cases with cement-retained implant prostheses.12
Therefore, this study aimed to propose a customized crown-level position (CLP) jig to standardize implant radiography with an orthogonal projection to the implant without removing implant suprastructure, and also to examine the efficacy of using implant length as calibration reference to measure piCBL.
Material and methods
Study model preparation
A maxillary dentate typodont (Basic, KaVo Dental GmbH, Berlin, Germany) was used. The right central incisor was removed and replaced by an aluminum implant (4.1 × 10 mm RC BLT, Straumann, Basel, Switzerland). A threaded metal post was inserted in the septum parallel to the implant axis, 5 mm labial to the implant center to simulate the crestal level, and the post top was at the same height of the implant platform (Fig. 1).
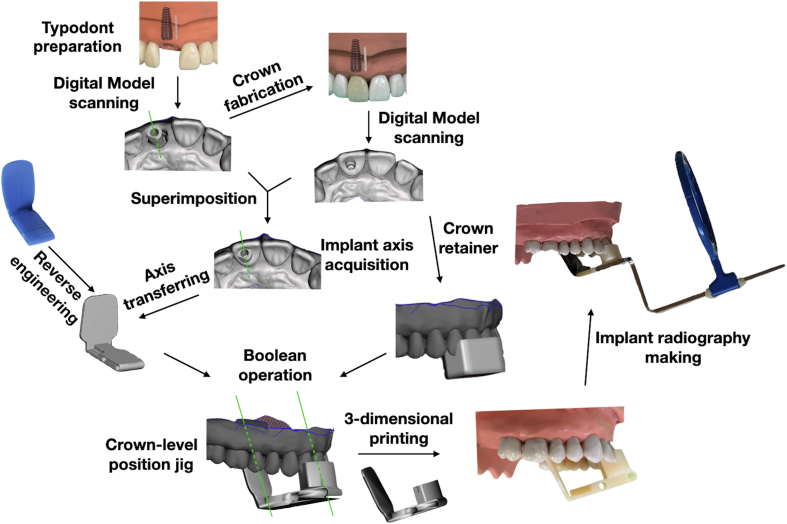
Figure 1.
Schematic flow chart of the fabrication of customized crown-level position jig for standardization of implant radiography.
Implant axis acquisition
The first digital model with a scan body (Scanbody RC, Straumann) inserted was scanned to record the axis of the implant and for making a screw-retained zirconia crown, which was implant-level model. Once the zirconia crown was delivered, the second, crown-level digital model, was scanned. The retrieved crown-level digital model was superimposed with the first scanned implant-level model in Geomagic Control X (3D Systems, Rock Hill, SC, USA) to transfer the implant axis to the crown-level model (Fig. 1).
Crown-level position jig fabrication
The CLP jig composed of a crown retainer and a periapical film holder. The film holder was built in SolidWorks (Dassault Systémes, Vélizy-Villacoublay, France) by reverse engineering the bite-block of XCP Rinn (Dentsply Sirona, York, PA, USA) to facilitate positioning indicator arm (Dentsply Sirona) perpendicular to the periapical film. The film holder was placed at the position that was parallel to implant axis, without superimposing neighboring anatomy and central ray aiming implant platform. The crown retainer covering the implant crown and adjacent teeth was designed on the crown-level digital model. Afterwards, the film holder jointing with the crown retainer and the crown-level digital model were computed under Boolean operation in Autodesk Meshmixer (Autodesk Inc., San Rafael, CA, USA). The CLP jig was then printed out by a 3D printer (Phrozen Sonic, Phrozen, Hsinchu, Taiwan) using a photopolymer resin (Enlighten AA TEMP, Enlighten Materials, Taipei, Taiwan) (Fig. 1).
Radiographic crestal bone-level measurement
Three examiners with different clinical experiences were recruited, including an intern, a resident, and a periodontist. Each examiner made 5 implant radiographs with the conventional long-cone paralleling technique and another 5 implant radiographs with paralleling technique and the position jig at different time points. All the 30 implant radiographs were made with an intraoral X-ray unit (Heliodent plus, Dentsply Sirona) set at 7 mA DC, 60 kV, and 0.25 s exposure time.
The top surface of the metal post was served as the maker to simulate buccal plate bone height near the implant. A photograph was made orthogonally to the implant platform to confirm the top of the metal post was at the same level with the platform, which denoted that the discrepancy of piCBL (ΔD) and implant platform was zero (Fig. 2A). Thereafter, the ΔD of all the 30 implant radiographs with jig (Fig. 2B) and without jig (Fig. 2C) were measured by the same examiner (J-Y Yen) using ImageJ (National Institutes of Health, Bethesda, MD, USA).
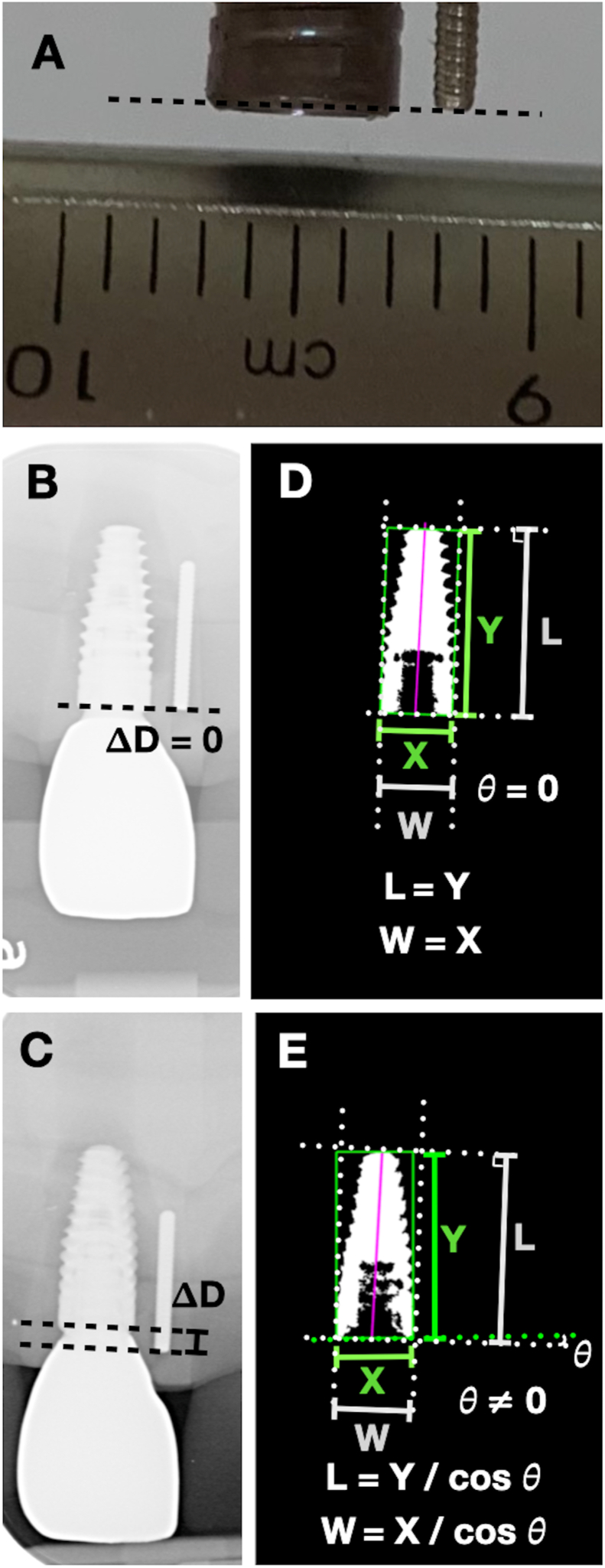
Figure 2.
Discrepancy of peri-implant crestal bone level determination (ΔD), acquisition of implant axis and the calculation of implant dimensions. (A) Orthogonal photograph showing top surface of metal rod (simulated bone crest) at the same level with implant fixture level. (B) Radiograph taken with jig showing ΔD = 0. (C) Radiograph taken without jig showing ΔD > 0. (D, E) Semi-automated image segmentation and calculations of implant dimensions with and without jig, respectively. L: implant length; W: implant width; X: width of bounding box; Y: length of bonding bounding box; θ: the deviated angle between implant axis and minimal bounding box.
piCBL measurement using implant length as calibration reference
Implant images on radiographs were verified by a semi-automated method to acquire implant axis orientation21,22 and implant dimensions23,24 using the algorithms in the Matlab (MathWorks, Natick, MA, USA) library. The acquired implant axis and the minimal bounding rectangle were then used to calculate the width and length of the implant on each radiograph (Fig. 2D and E). The true dimensions of the implant were measured in width and length with a digital caliper and serve as calibration references for distortion assessment; and the ΔD of each implant radiograph was adjusted accordingly using the implant length magnification ratio. Further, the length of metal post was derived from the image on the radiograph and compared with its true length (8.12 mm) to assess the reliability of using implant length as the calibration reference for linear measurements.
Statistical analyses
Descriptive statistics of ΔD for two techniques by three examiners were described. The ΔD measured on implant radiographs with and without CLP jig were compared by Mann–Whitney U test for three examiners. Variations of ΔD among examiners were compared using Kruskal–Wallis tests. Magnifications of the implant in width and length were compared between two radiographic techniques, respectively. Statistical analyses were performed with SPSS 25.0 for Windows (IBM Corp., Armonk, NY, USA) and the significance level was set at α = 0.05.
Results
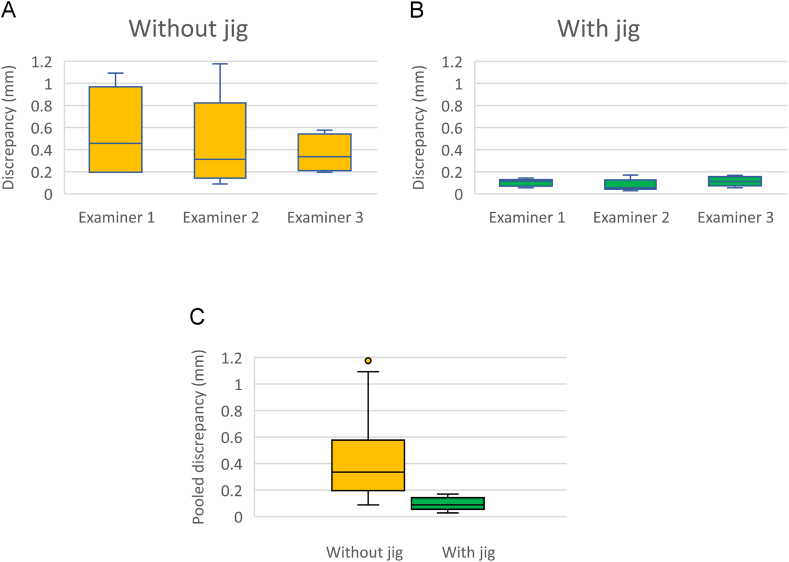
The results of the discrepancy between top surface of metal post and implant platform on radiographs were described in Table 1. It was considered a perfect radiographic shot if the ΔD was zero. The ΔD measured on radiographs made by the use of paralleling technique with the CLP jig were significantly smaller than those made without the jig for all the examiners (Fig. 3). The pooled ΔD were 0.10 ± 0.04 mm for the CLP jig radiographs, and 0.46 ± 0.34 mm for the paralleling technique radiographs without using jig. While no differences were found among the examiners when the same technique was applied.
Table 1.
Discrepancy between metal post top surface and implant platform on radiographs for parallel technique with jig and parallel technique alone for three examiners.
| Examiner | Parallel technique with jig |
Parallel technique alone |
P1 | |||
|---|---|---|---|---|---|---|
| Mean ± SD | 95% CI | Mean ± SD | 95% CI | |||
| ΔD0 (mm) | 1 | 0.10 ± 0.03 | 0.07–0.13 | 0.56 ± 0.4 | 0.21–0.91 | 0.008a |
| 2 | 0.08 ± 0.06 | 0.03–0.13 | 0.45 ± 0.43 | 0.07–0.83 | 0.016a | |
| 3 | 0.11 ± 0.05 | 0.06–0.16 | 0.37 ± 0.17 | 0.22–0.52 | 0.008a | |
| P2 | 0.416 | 0.896 | ||||
Abbreviations: CI, confidence interval; SD, standard deviation; ΔD0, original discrepancy of peri-implant crestal bone level.
P1 represents the comparison among three examiners.
P2 represents the comparison between two methods.
Statistically significant at α = 0.05.
Figure 3.
Boxplot showing the measurement discrepancy of three examiner (Examiner 1: Intern; Examiner 2: Resident; Examiner 3: Periodontist) following paralleling technique to take implant periapical radiographs. A. Without jig. B. With jig. C. Pooled data of three examiners.
The true dimensions of the implant used were 4.12 mm and 10.23 mm in width and length measured by a digital caliper, respectively. The magnification of the implant on radiograph was calculated by taking the true size of the implant as reference. The magnifications in both directions for paralleling technique with and without jig were shown in Table 2. The magnification in implant width was smaller than implant length in both techniques, and magnifications using paralleling technique with jig were statistically greater than those without jig (P < 0.05).
Table 2.
Magnification of the width and length of the implant on radiographs for parallel technique with jig and parallel technique alone.
| Magnification | Parallel technique with jig |
Parallel technique alone |
P1 | ||
|---|---|---|---|---|---|
| Mean ± SD | 95% CI | Mean ± SD | 95% CI | ||
| Implant width | 1.06 ± 0.003 | 1.059–1.062 | 1.05 ± 0.02 | 1.04–1.06 | 0.02a |
| Implant length | 1.09 ± 0.01 | 1.09–1.10 | 1.07 ± 0.03 | 1.05–1.08 | 0.003a |
| P2 | <0.001a | 0.001a | |||
Abbreviation: CI (confidence interval); SD (standard deviation).
P1 represents the comparison among three examiners.
P2 represents the comparison between two methods.
Statistically significant at α = 0.05.
Using the true implant length as calibration reference, both techniques showed an improved ΔD. The calibrated ΔD on radiographs with CLP jig was improved and significantly smaller (P < 0.001) than those on radiographs without jig (Table 3).
Table 3.
Improvement of discrepancy of peri-implant crestal bone level by implant length adjustment for parallel technique with and without jig.
| Parallel technique with jig |
Parallel technique alone |
|||
|---|---|---|---|---|
| Mean ± SD | 95% CI | Mean ± SD | 95% CI | |
| ΔD0 (mm) | 0.10 ± 0.04 | 0.076–0.121 | 0.46 ± 0.34 | 0.287–0.628 |
| ΔD1 (mm) | 0.09 ± 0.04 | 0.070–0.110 | 0.43 ± 0.33 | 0.378–0.492 |
| (ΔD0- ΔD1)/ΔD0 | 10.0% | 6.5% | ||
Abbreviations: CI (confidence interval); SD (standard deviation); ΔD0 (original discrepancy of peri-implant crestal bone level), ΔD1 (calibrated discrepancy of peri-implant crestal bone level by implant length adjustment).
Discussions
Implant length is commonly used for linear calibration of piCBL measurements on periapical radiographs, however, its reliability has never been testified. This study found that routine long-cone paralleling technique demonstrated a scattering result of piCBL measurements (Table 1). Additionally, using implant length for calibration did not effectively resolve the problem (Fig. 3). Since there is a request of precise measurement of piCBL changes in implant dentistry, especially at the early loading stage. With the calibrated ΔD of 0.43 mm revealed in the present investigation, using paralleling technique alone was not fulfilled the requests to verify the subtle yearly piCBL changes4, 5, 6 or implant-abutment misfit.15,16 The reason why the correction method is invalid may be because the magnifications of periapical radiographs in length and width directions are different (Table 2). As the collimated radiation beam of the dental X ray machine used is not a spot but a rectangle in shape.
To precisely monitor the piCBL changes fixture-level position jigs were highly recommended.10, 11, 12, 13 However, repeatedly disconnecting and re-connecting the abutment is time consuming and may damage the abutment–implant interface and abutment screw.17, 18, 19, 20 Moreover, fixture-level position jigs are not feasible in cement-type implant prostheses. Therefore, the CLP jig was designed and verified in this study. The core concept of the technique is to transfer the implant axis to the crown level before insertion of the definitive prosthesis. Taking advantage of available laboratory scanners and opensource software, the CLP jig can be designed specifically for evaluation of piCBL or interproximal contact loss of implant prostheses.25, 26, 27 Moreover, the STL file of CLP jig can be stored and printed out handily when standardized periapical radiography is indicated, which also eases the concern of preserving the jig for long-term follow-up.
The present study showed a high accuracy of piCBL measurement using a paralleling technique with the jig. The discrepancy can even be reduced to 0.09 mm by using implant length as the calibration reference. Based on the calibrated ΔD, this technique can provide high precision and accurate measurement, which shall be sufficient to discriminate a slight change of crestal bone level and interproximal contacts.
Moreover, using the conventional paralleling technique has been shown to produce a poor prediction of piCBL because of the oblique projection of the x-ray beam to the apical film. Previous animal studies demonstrate a controversial result of 1.0 mm overestimation28 and 0.4 mm underestimation29 of piCBL compared to histological measurements. A clinical study also found that peri-implant proximal bony defect measured on the implant periapical radiograph was 1.3 mm less than that measured intra-operatively.30 The ΔD measured in this study might be exaggerated as the metal post served as the piCBL was placed 5 mm labial to the implant, as the longer film-object distance will magnify the discrepancy of piCBL. However, this study confirmed the unreliable measurement of piCBL using paralleling technique without the position jig. Although, cone beam computed tomography (CBCT) has been verified in assessing bone level and osseous defect around implants,29,31 the high radiation exposure was not recommended at periodic follow-up evaluation and metal artifacts around dental implant on CBCT images might limit its application.
The proposed crown-level implant position jig could record the 3D relationship of the target implant and the periapical film plane to allow orthogonal projection of X-ray beam using the paralleling technique.32,33 These settings would not only eliminate the effect of parallax resulting from the buccal/lingual position of the implant32 but also prevent superimposition of adjacent anatomical structure at extreme sites, such as the maxillary and mandibular canine regions. However, due to their two-dimensional nature, the diagnostic value of periapical radiographs is limited in evaluating intra-bony defects or differentiate buccal and lingual bone levels. Nevertheless, periapical radiographs are still the most commonly used tool for diagnosing peri-implant defects. Future works incorporating artificial intelligent in analyzing bony defect with the standardized periapical radiographs might be of interest.
In clinical applications, the use of small-sized periapical film or horizontally placed film holder can be designed to prevent film bending or intrude patient comfort at extreme sites. It should be noted that a high prevalence of proximal contact loss of implant prosthesis, especially at mesial contact, has been reported.25, 26, 27 Therefore, the jig printed out from the previously restored digital STL file may not fully seated on the implant prosthesis if the retainer involved adjacent teeth and the relationship of them was changed at long-term follow-up. In this case, the jig can also be used to verify the stability of interproximal contacts of implant prosthesis, while minor adjustment of the jig might be necessary before making radiograph.
Transferring the implant axis to the crown level can be easily accomplished at the time the final prosthesis was inserted. However, it is challenging to transfer the implant axis of the implant prosthesis already delivered. Thus, it warrants future studies to retrieve the implant axis of the delivered implant prosthesis from periapical radiograph by using artificial intelligence to analyze implant radiographic images and provide orthogonal projection to the implant and the periapical film without removing the implant prosthesis.
In this study, the incisor implant was chosen as the study model. Because orthogonal projection of the incisor implant on periapical radiography was considered to be more difficult to achieve than the posterior implant. However, using a simulated model with only one implant and a screw-retained crown may not fully reflect the various conditions in the clinic. Testing the CLP jig for more different implant systems in different locations of the mouth merits further studies.
In conclusion, the conventional long-cone paralleling technique only slightly improved the measurement accuracy of piCBL even with the adjustment of implant length calibration. Using a custom CLP jig, standardization of implant radiography for piCBL determination has been achieved with an accuracy of 0.09 mm after implant length calibration. It is highly recommended to transfer the implant axis to the crown level before implant prothesis is inserted, which will facilitate the fabrication of CLP jig and thus benefit standardization of periapical radiographs in the long-term follow-up of implant prosthesis and peri-implant tissue.
Declaration of competing interest
The authors have no conflicts of interest relevant to this article.
Acknowledgements
The study was supported in part by the National Science and Technology Council, Taiwan (Grant No. NSTC 111-2218-E-A49-025-) and Department of Health, Taipei City Government (Grant No. 11001-62-034). The authors appreciate and are grateful for the valuable assistance and technical support provided by Chia-Feng Lu, Ping-Feng Lin and Nai-Chi Chen of Department of Biomedical Imaging and Radiological Science, College of Biomedical Science and Engineering, National Yang Ming Chiao Tung University.
References
- 1.Albrektsson T., Chrcanovic B., Ostman P.O., Sennerby L. Initial and long-term crestal bone responses to modern dental implants. Periodontol. 2000 2017;73:41–50. doi: 10.1111/prd.12176. [DOI] [PubMed] [Google Scholar]
- 2.Wang Y.C., Kan J.Y., Rungcharassaeng K., Roe P., Lozada J.L. Marginal bone response of implants with platform switching and non-platform switching abutments in posterior healed sites: a 1-year prospective study. Clin Oral Implants Res. 2015;26:220–227. doi: 10.1111/clr.12312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Salvi G.E., Gallini G., Lang N.P. Early loading (2 or 6 weeks) of sandblasted and acid-etched (SLA) ITI implants in the posterior mandible. A 1-year randomized controlled clinical trial. Clin Oral Implants Res. 2004;15:142–149. doi: 10.1111/j.1600-0501.2004.01014.x. [DOI] [PubMed] [Google Scholar]
- 4.Albrektsson T., Zarb G., Worthington P., Eriksson A.R. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1:11–25. [PubMed] [Google Scholar]
- 5.Smith D.E., Zarb G.A. Criteria for success of osseointegrated endosseous implants. J Prosthet Dent. 1989;62:567–572. doi: 10.1016/0022-3913(89)90081-4. [DOI] [PubMed] [Google Scholar]
- 6.Lekholm U., Adell R., Lindhe J., et al. Marginal tissue reactions at osseointegrated titanium fixtures. (II) A cross-sectional retrospective study. Int J Oral Maxillofac Surg. 1986;15:53–61. doi: 10.1016/s0300-9785(86)80011-4. [DOI] [PubMed] [Google Scholar]
- 7.Sewerin I.P. Errors in radiographic assessment of marginal bone height around osseointegrated implants. Scand J Dent Res. 1990;98:428–433. doi: 10.1111/j.1600-0722.1990.tb00994.x. [DOI] [PubMed] [Google Scholar]
- 8.Afrashtehfar K.I., Bragger U., Hicklin S.P. Reliability of interproximal bone height measurements in bone- and tissue-level implants: a methodological study for improved calibration purposes. Int J Oral Maxillofac Implants. 2020;35:289–296. doi: 10.11607/jomi.7763. [DOI] [PubMed] [Google Scholar]
- 9.Wakoh M., Harada T., Otonari T., et al. Reliability of linear distance measurement for dental implant length with standardized periapical radiographs. Bull Tokyo Dent Coll. 2006;47:105–115. doi: 10.2209/tdcpublication.47.105. [DOI] [PubMed] [Google Scholar]
- 10.Meijer H.J., Steen W.H., Bosman F. Standardized radiographs of the alveolar crest around implants in the mandible. J Prosthet Dent. 1992;68:318–321. doi: 10.1016/0022-3913(92)90337-a. [DOI] [PubMed] [Google Scholar]
- 11.Payne A.G., Solomons Y.F., Lownie J.F. Standardization of radiographs for mandibular implant-supported overdentures: review and innovation. Clin Oral Implants Res. 1999;10:307–319. doi: 10.1034/j.1600-0501.1999.100407.x. [DOI] [PubMed] [Google Scholar]
- 12.Galasso L. Proposed method for the standardized measurement of marginal bone height on periapical radiographs with the Branemark System. Clin Implant Dent Relat Res. 2000;2:147–151. doi: 10.1111/j.1708-8208.2000.tb00005.x. [DOI] [PubMed] [Google Scholar]
- 13.Naffah N., Chidiac J.J. A modified periapical radiographic holder used for standardized implant assessment. J Prosthet Dent. 2004;91:398. doi: 10.1016/j.prosdent.2003.12.020. [DOI] [PubMed] [Google Scholar]
- 14.Papavassiliou H., Kourtis S., Katerelou J., Chronopoulos V. Radiographical evaluation of the gap at the implant-abutment interface. J Esthetic Restor Dent. 2010;22:235–251. doi: 10.1111/j.1708-8240.2010.00345.x. [DOI] [PubMed] [Google Scholar]
- 15.Lin K.C., Wadhwani C.P., Cheng J., Sharma A., Finzen F. Assessing fit at the implant-abutment junction with a radiographic device that does not require access to the implant body. J Prosthet Dent. 2014;112:817–823. doi: 10.1016/j.prosdent.2014.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Daros P., Carneiro V.C., Siqueira A.P., de-Azevedo-Vaz S.L. Diagnostic accuracy of 4 intraoral radiographic techniques for misfit detection at the implant abutment joint. J Prosthet Dent. 2018;120:57–64. doi: 10.1016/j.prosdent.2017.08.008. [DOI] [PubMed] [Google Scholar]
- 17.Molina A., Sanz-Sanchez I., Martin C., Blanco J., Sanz M. The effect of one-time abutment placement on interproximal bone levels and peri-implant soft tissues: a prospective randomized clinical trial. Clin Oral Implants Res. 2017;28:443–452. doi: 10.1111/clr.12818. [DOI] [PubMed] [Google Scholar]
- 18.Abrahamsson I., Berglundh T., Lindhe J. The mucosal barrier following abutment dis/reconnection. An experimental study in dogs. J Clin Periodontol. 1997;24:568–572. doi: 10.1111/j.1600-051x.1997.tb00230.x. [DOI] [PubMed] [Google Scholar]
- 19.Guzaitis K.L., Knoernschild K.L., Viana M.A. Effect of repeated screw joint closing and opening cycles on implant prosthetic screw reverse torque and implant and screw thread morphology. J Prosthet Dent. 2011;106:159–169. doi: 10.1016/S0022-3913(11)60115-7. [DOI] [PubMed] [Google Scholar]
- 20.Arshad M., Mahgoli H., Payaminia L. Effect of repeated screw joint closing and opening cycles and cyclic loading on abutment screw removal torque and screw thread morphology: scanning electron microscopy evaluation. Int J Oral Maxillofac Implants. 2018;33:31–40. doi: 10.11607/jomi.5476. [DOI] [PubMed] [Google Scholar]
- 21.Rocha L., Velho L., Carvalho P.C.P. IEEE comput. XV Brazilian symposium on computer graphics and image processing. 2002. Image moments-based structuring and tracking of objects; pp. 99–105. [Google Scholar]
- 22.Jouary A., Haudrechy M., Candelier R., Sumbre G. A 2D virtual reality system for visual goal-driven navigation in zebrafish larvae. Sci Rep. 2016;6 doi: 10.1038/srep34015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Levine M.D., Nazif A.M. Dynamic measurement of computer generated image segmentations. IEEE Trans Pattern Anal Mach Intell. 1985;6:155–164. doi: 10.1109/tpami.1985.4767640. [DOI] [PubMed] [Google Scholar]
- 24.Otsu N. A threshold selection method from gray-level histograms. IEEE Trans Syst Man Cybern Syst. 1979;9:62–66. [Google Scholar]
- 25.Pang N.S., Suh C.S., Kim K.D., Park W., Jung B.Y. Prevalence of proximal contact loss between implant-supported fixed prostheses and adjacent natural teeth and its associated factors: a 7-year prospective study. Clin Oral Implants Res. 2017;28:1501–1508. doi: 10.1111/clr.13018. [DOI] [PubMed] [Google Scholar]
- 26.Yen J.Y., Kang L., Chou I.C., Lai Y.L., Lee S.Y. Risk assessment of interproximal contact loss between implant-supported fixed prostheses and adjacent teeth: a retrospective radiographic study. J Prosthet Dent. 2022;127:86–92. doi: 10.1016/j.prosdent.2020.06.023. [DOI] [PubMed] [Google Scholar]
- 27.Ren S., Lin Y., Hu X., Wang Y. Changes in proximal contact tightness between fixed implant prostheses and adjacent teeth: a 1-year prospective study. J Prosthet Dent. 2016;115:437–440. doi: 10.1016/j.prosdent.2015.08.018. [DOI] [PubMed] [Google Scholar]
- 28.Schliephake H., Wichmann M., Donnerstag F., Vogt S. Imaging of periimplant bone levels of implants with buccal bone defects. Clin Oral Implants Res. 2003;14:193–200. doi: 10.1034/j.1600-0501.2003.140209.x. [DOI] [PubMed] [Google Scholar]
- 29.Ritter L., Elger M.C., Rothamel D., et al. Accuracy of peri-implant bone evaluation using cone beam CT, digital intra-oral radiographs and histology. Dentomaxillofacial Radiol. 2014;43 doi: 10.1259/dmfr.20130088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Garcia-Garcia M., Mir-Mari J., Benic G.I., Figueiredo R., Valmaseda-Castellon E. Accuracy of periapical radiography in assessing bone level in implants affected by peri-implantitis: a cross-sectional study. J Clin Periodontol. 2016;43:85–91. doi: 10.1111/jcpe.12491. [DOI] [PubMed] [Google Scholar]
- 31.Pelekos G., Tse J.M.N., Ho D., Tonetti M.S. Defect morphology, bone thickness, exposure settings and examiner experience affect the diagnostic accuracy of standardized digital periapical radiographic images but not of cone beam computed tomography in the detection of peri-implant osseous defects: an in vitro study. J Clin Periodontol. 2019;46:1294–1302. doi: 10.1111/jcpe.13200. [DOI] [PubMed] [Google Scholar]
- 32.Malloy K.A., Wadhwani C., McAllister B., Wang M., Katancik J.A. Accuracy and reproducibility of radiographic images for assessing crestal bone height of implants using the precision implant X-ray locator (PIXRL) device. Int J Oral Maxillofac Implants. 2017;32:830–836. doi: 10.11607/jomi.5683. [DOI] [PubMed] [Google Scholar]
- 33.Lin K.C., Wadhwani C.P., Sharma A., Finzen F. A radiograph positioning technique to evaluate prosthetic misfit and bone loss around implants. J Prosthet Dent. 2014;111:163–165. doi: 10.1016/j.prosdent.2013.06.016. [DOI] [PubMed] [Google Scholar]