Abstract
There are different kinds of benign and malignant lesions in the oral cavity. Clinically, definite diagnosis can be confirmed only by doing adequate surgical biopsy and subsequent histopathological examination. Inadequate biopsy technique, unsuitable selection of the location for biopsy, inappropriate tissue handling and record of patients' information may lead to artifacts and misdiagnosis by the oral pathologists. Soft tissue stabilization is a challenge during oral surgery procedures. It needs the cooperation of operator, assistants, and patients to overcome the difficulty and ensure the successful outcome. In this article, we reviewed the procedures for clinical surgical biopsy, and raised three current tissue stabilization methods including fingers and gauze stabilization, stabilization with chalazion forceps and adapted instruments, and stabilization with retraction sutures. Moreover, some limitations were also presented. Clinician should examine the clinical characteristics of the oral lesion, the surrounding anatomical structures, and their own clinical experience and preference to select the appropriate tool. More understanding of these biopsy and tissue stabilization methods can effectively improve the biopsy procedures and obtain adequate tissues for histopathological examination and subsequent issue of an accurate pathological report.
Keywords: Oral biopsy, Pressure forceps, Retractor, Soft tissue, Tissue stabilization methods
Introduction
Oral biopsy surgery is a common procedure in dental practice that involves the incision, excision or punch of oral mucosal tissue for histopathological evaluation.1 Any suspected oral soft tissue lesions should be biopsied and subjected to histopathological examination by oral and maxillofacial pathologists.2 Clinical studies in different countries have found that aphthous ulcer, trauma-related lesions, herpes simplex virus-associated lesions are most commonly found lesions in children. Biopsy reports show that mucocele, fibrous lesion, and pyogenic granuloma are the most commonly observed biopsied oral mucosal lesions in children.3 In adults, aphthous ulcer, lichen planus, herpes simplex labialis/stomatitis, oral candidiasis, fibroma, mucocele, leukoplakia, erythroplakia, oral cancer and more others are regularly found in clinical dental practice.4 There are also various oral benign and malignant soft tissue diseases such as reactive, infectious, inflammatory, immune-related, and premalignant/malignant lesions.1 This is especially true in Taiwan, due to different oral habits such as tobacco smoking, alcohol consumption, and betel quid chewing,5, 6, 7 that increase the exposure of oral cavity to various chemical carcinogens and oral cancer initiation, promotion, and progression.8, 9, 10, 11, 12 Although most dentists are able to detect suspicious oral lesions, only 9.9%–11.3% of general dentists have confidence in performing biopsies by themselves.13,14 Dentists who were reluctant to do such procedures explained that they did not have the experience, skills or appropriate clinical tools to do the oral biopsy procedures.14 Other studies found that majority of dentists had never or hardly performed any oral biopsy in the dental school,15, 16, 17 emphasizing the importance of postgraduate training and self-directed learning on this topic. Clinicians might have tried to perform a biopsy but eventually obtained samples with minimal diagnostic value.17 Poor biopsy technique, inadequate selection of region for biopsy, and improper tissue handling and documentation of clinical information may lead to artifacts and misdiagnosis of oral lesions of the patients.2
Accuracy of oral soft tissue biopsy diagnosis
While many dentists and oral surgeons considered the oral biopsy surgery to be very simple, this was possibly due to the adequate judgement of histopathological specimens by the experienced pathologists. However, possible underdiagnosis or overdiagnosis has been reported. The agreement of clinical diagnosis with pathological diagnosis are generally high regarding to periapical lesions, oral potentially malignant disorders, and non-neoplastic proliferative lesions (89.3–92.6% of agreement). Marked disagreement between clinical impression and histopathological report was found mainly in the mesenchymal tumors (25%) and cysts (44.2%).18 A study conducted in the Department of Oral and Maxillofacial Surgery, Massachusetts General Hospital, Boston, MA, USA from January 2005 to December 2012 has found a 11.1% (30 cases) discordant diagnosis rate between the initial incisional biopsy diagnosis and final definitive resection diagnosis for various oral lesions.19 The major reasons for discordant diagnosis are sampling error (60%), pathologists' discrepancy (23.3%), insufficient tissue of biopsy (13.3%), and inflammation-obscuring diagnosis (3.4%).19 Our previous study also showed that in 242 cases of oral leukoplakia found in the National Taiwan University Hospital, 200 cases with single site biopsy demonstrated a 56% agreement rate between provisional biopsy and final definitive diagnosis, with an underdiagnosis of incisional biopsy specimens in 29.5% of the patients.20 The underdiagnosis rate of 42 oral leukoplakia cases with multiple sites of biopsy was only 11.9%, but non-homogeneous oral leukoplakia cases showed a higher rate of underdiagnosis of biopsy specimens,20 suggesting that obtaining sufficient and representative biopsy samples are important for an accurate histopathological diagnosis. Accurate biopsy and subsequent histopathological examination are further shown to be critical for the early definite diagnosis of pemphigus vulgaris for early treatment by medical doctors.21,22 Clinically, 90% of oral ulcers in pemphigus vulgaris patients are often misdiagnosed as an aphthous ulcer.21 Biopsy and histopathological examination of minor salivary gland is also suggested to be useful for early diagnosis of Sjögren's syndrome,23 and adequate grading system is useful to decrease the misdiagnosis of lip biopsy sample for Sjögren's syndrome.24 So special attention should be considered about the incisional biopsy for large and heterogeneous lesions to avoid underdiagnosis and overdiagnosis. Understanding the confounding factors may improve technique modification and the overall accuracy of the diagnosis of oral biopsy sample.
General principles of oral biopsy
Clinically, the dentists or oral surgeons should evaluate the patients' medical and dental history. Systemic diseases such as seizure, asthma, cardiovascular diseases (myocardial infarction, angina pectoris, etc.), stroke, rheumatoid fever, human immunodeficiency virus (HIV) disease, tuberculosis, hepatitis, and more others should be carefully reviewed.25 They should also understand the patients' oral habits (betel quid chewing, tobacco smoking, alcohol consumption), and ask about the history of the oral lesion, to further evaluate the duration and growth rate of the lesion. The size, depth, location, color, consistency, surface texture, mobility, and other clinical characteristics shall be thoroughly assessed to obtain possible diagnosis (impression) of the oral lesions. Before biopsy surgery, informed consent should be signed by the patients with understanding the possible complications of oral biopsy procedure including pain, discomfort, bleeding, swelling, infection, and even scarring and esthetic concern after the procedure, especially when the lesion is localized in the lip.25 Excisional biopsy should be avoided if oral malignancy is the possible concern, to preserve the border of malignant lesion for definite extirpation by the oral and maxillofacial surgeon.1 On the other hand, incisional biopsy is often used for oral lesions with possible malignancy or for the large lesions.1 However, possible underdiagnosis of oral premalignant lesion and malignant lesion by incisional biopsy was reported.20,26 Agent of local anesthesia should not be injected directly into the lesional tissues. This is particularly true for biopsy of immune-related mucocutaneous disorders.27 Sharp surgical scalpel is required for optimal biopsy results, because crushing of tissues by tissue forceps, electrosurgery or laser may lead to artifactual tissue alterations. The #15 sharp scalpel blade is the most popularly-used instrument for oral biopsy. Presence of severe inflammation may also distort the tissues for cytomorphological examination.28 Moreover, enough size and amounts of tissue are better to be obtained for adequate histopathological examination to reach an accurate and definitive diagnosis.28,29 However, clinically the locations of oral lesions, such as the floor of mouth, esthetic zone of the lip, gingiva, and the mental area, may potentially hinder the biopsy tissues' sampling due to access, hemostasis, and possibly injury to submandibular duct or mental nerve.28
Steps of the biopsy surgery include selection of biopsy sites, preparation of operation field, anesthesia, tissue stabilization, incision or excision of the lesion, handling of biopsy tissues, hemostasis, and surgical wound closure.30, 31, 32 Tissue stabilization plays a crucial role in the oral biopsy procedure, as it is highly related to the visibility and accessibility of the surgical field. A good tissue stabilization keeps the targeted tissue in place and prevents it from shifting or moving during the biopsy procedure. Thus, tissue stabilization increases the accuracy of incision, prevents damage to the surrounding tissues, facilitates suturing, and shortens the duration of the biopsy procedure. However, the oral cavity is a complex and narrow space. Oral and perioral tissues, such as the tongue, cheeks, and lips, are often soft, mobile and moistened with saliva, which poses a challenge for an effective tissue stabilization. To overcome these challenges, various instruments and techniques have been reported in the literature. The aim of this article also tried to explore the different methods for tissue stabilization during the oral biopsy surgery, to evaluate their advantages and disadvantages, and to provide valuable insights that could assist clinicians in making decisions for optimizing the success of oral biopsy surgery.
Preliminary examination of the oral lesions
Examination of intraoral lesions usually includes a thorough health and dental history, and physical and radiographic examinations.30,33,34 During this process, clinicians gather detailed information about the patients' oral habits, lesion's history, and clinical features. Radiographs are particularly useful for determining whether the lesions involve the bone or not, or have an intraosseous origin.
After conducting a thorough assessment, clinicians may obtain some presumptive diagnosis and determine the need for a biopsy. Methods including incisional, excisional and punch biopsies are selected based on the size and clinical appearance of the oral lesions. If a biopsy is deemed necessary, potential risks or complications associated with the biopsy procedure should be identified to ensure its safety and effectiveness. The type of anesthesia, the method for tissue stabilization, and the type of biopsy being performed should be considered in advance. Exposure of the surgical field is especially important due to the limited space of the oral cavity for the biopsy procedures. Various methods are available for tissue stabilization, including grasping the tissue with fingers or gauze, utilizing tissue retractors or chalazion forceps, and applying retraction sutures.25,30,35 Each method has its pros and cons (Table 1). The anatomical location, clinical features of the lesion, the type of biopsy, and the available instruments should be considered for selection of an appropriate method.
Table 1.
Common methods for oral tissue stabilization and their advantages and disadvantages.
| Methods | Advantages | Disadvantages |
|---|---|---|
| Fingers and gauze | Cost-effective No specialized equipment Help eliminate bleeding by applied pressure |
The lips and tongue may be slippery and difficult to grip. Risk of sharps injuries (avoid using this method in patients with blood-borne pathogens) |
| Chalazion forceps and their modifications | Easy to apply and remove Reduce bleeding Improve visibility Less risk of sharps injuries |
May slip off or cause discomfort/bruising if not used properly One type of forceps does not suit for all cases. Different types of forceps may be required. |
| Retraction sutures | Strong retraction force (especially for the tongue) Help pathologists orientate the specimens |
Potential histological artifacts Possible laceration of the tissue Risk of damaging the nerves, veins, and arteries |
It is noteworthy that clinical expertise, surgical experiences, and clinical interest can vary among clinicians. Although some general dentists may feel confident in performing biopsies, patients who have significant systemic diseases, oral lesions with malignant potentials, or cases with greater surgical difficulties (such as the lesions that are close to vital structures) may be more challenging.30,33 Referral to an oral and maxillofacial surgeon is recommended for optimal care and further treatment of such cases.36
Stabilization with fingers and gauze
One of the most common techniques for tissue stabilization involves holding and retracting the lips, cheeks or tongue firmly with the fingers.30,31 This method is cost effective and does not require any specialized equipment. Clinicians or assistants manipulate the cheek and the lip by placing their thumbs inside the mouth adjacent to the lesion, and positioning the other fingers on the external surface, pushing the tissue inward to elevate the lesion (Fig. 1). This method can also aid in hemostasis by compressing the bleeding area and reducing the blood flow.
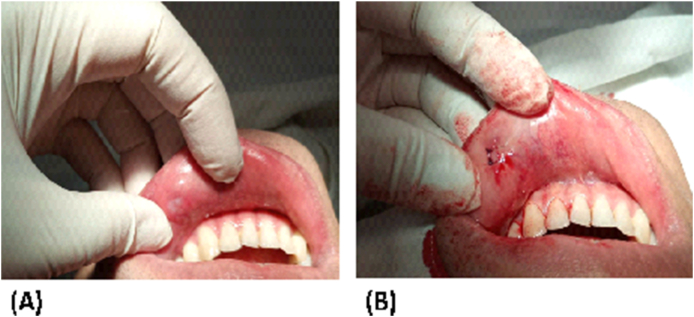
Figure 1.
A dome-shape mucosal swelling over the left lower lip. The lesion was pushed inward with the middle and ring fingers to facilitate the excision. The scalpel should be manipulated carefully to avoid iatrogenic sharp injuries on the stabilizing fingers.
To reinforce stabilization, a gauze can be placed between the fingers and the tissue to facilitate the grip and remove saliva and blood.30,31,35 Gauze is especially useful for stabilizing the tongue (Fig. 2). The tip of the tongue is grasped and pulled outward to improve visibility and surgical accessibility. Simultaneously, the patient is asked to relax his or her tongue to minimize undesired movements.
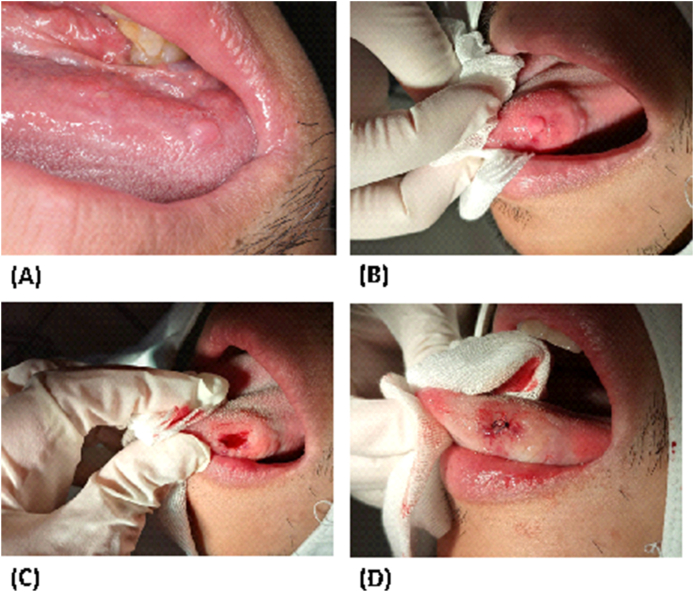
Figure 2.
(A) A pink papule over the left tongue border, (B) The tip of the tongue was grasped manually with a gauze, (C) After the excision, (D) After suturing
This method has several drawbacks despite its popularity. At first, grasping the tissue can be complicated due to the fluid and the nature of the mucosa. Although gauzes can temporarily remove surrounding fluid, the newly secreted saliva moistens the mucosa again. Secondly, the tongue is a very strong muscular structure. Retracting the tongue can be challenging as it may disgust the patient and trigger the gag reflex.35 This reflex is likely elicited by external stimulation at the base of the tongue.37
Sharp injuries, although very rare, could unexpectedly occur. A needle-stick injury or scalpel injury on the stabilizing fingers could transmit microbiomes such as hepatitis B virus, hepatitis C virus, and HIV from the patient to the surgical team members.38,39 The dentist and the assistants must exercise with caution throughout the surgical procedure to prevent such events. Several studies have demonstrated the efficacy of double gloving on reducing the perforation of inner gloves and the risk of cross-contamination.40,41 Mischke et al.40 summarized the results from 34 randomized clinical trials and revealed that double gloves provide superior protection compared to single gloves. The use of three pairs of gloves or gloves made of special materials seemed to offer extra protection but the potential loss of dexterity and the additional cost should be considered. Nevertheless, if the patient is known to be a carrier of infectious blood-borne pathogen before the surgery, it is advisable to avoid using fingers and gauze for stabilization. Instead, alternative methods should be employed to ensure safety.
Although the literature suggests that the “assistant” rather than the dentist holds the tissue for stabilization,30,31,42 we suggest that clinicians hold the tissue by themselves with their non-dominant hand, and operate the blade with the dominant hand. Meanwhile, the assistance aids the incision with a tissue tweezer and removes the fluid with a suction tube. Under this circumstance, the clinician has better control of the soft tissue, increases the accuracy of the blade, and reduces the risk of sharps injury.
Stabilization with chalazion forceps and adapted instruments
The use of toothed tissue forceps to grasp tissue specimens should be avoided, because the instrument may penetrate specimens, produce voids, tears, and compression of the surrounding tissues.2,27 The chalazion forceps, invented in the nineteenth century, was initially designed to remove chalazia, painless lumps in the eyelid. However, it has become a practical tool to aid oral biopsy, especially for oral lesions on the lip and buccal mucosa.25,42, 43, 44, 45 The advantages of chalazion forceps include speed, stabilization of tissues, increase tissue visibility and dissection, and reduce the artifact.46 Byrne et al.45 demonstrated that the lower lip biopsy for sicca syndrome with the aid of chalazion forceps has a 100% diagnostic accuracy and none of their patients experiences any complications. On the contrary, the lower lip biopsies without using a chalazion forceps results in paresthesia in 11% of cases from a meta-analytic study.47
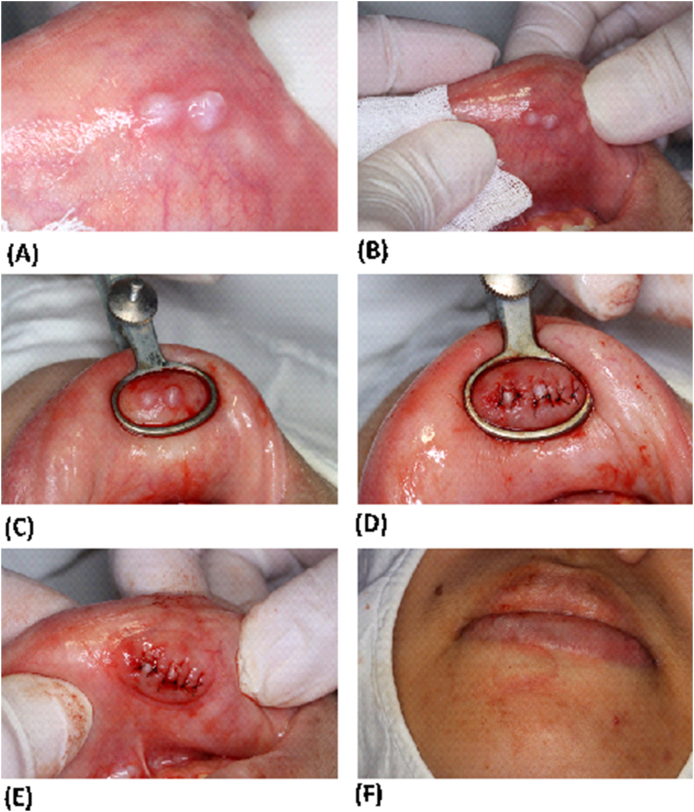
A chalazion forceps (Fig. 3) has a forceps-like handle, a thumbscrew in the middle, and a working end composed of a flat, solid, oval plate, and a ring-like aperture. To use these forceps, the targeted tissue is encircled by the ring-like aperture and then the thumbscrew is tightened (Fig. 3C). It is important not to overtightening the screw, as this may cause discomfort or bruising. With appropriate tightening force, the forceps can provide a firm and secure grip on the oral tissue. Additionally, the pressure from the forceps creates a local ischemic condition that helps reduce intraoperative bleeding and improve visualization of the underlying tissue. After excision and suturing, the thumbscrew is loosened and the forceps is removed.
Figure 3.
Use of a chalazion forceps for the lower lip biopsy. (A) Two whitish, fluctuant papules at the center of the lower lip. The patient stated that she had visited an otolaryngologist and an incision was done by the doctor to release the fluid. However, the swelling soon occurred again. (B) Stabilization and elevation of the lesion with fingers. (C) A chalazion forceps was used in this case. (D) Primary closure with interrupted sutures. (E and F) Surgical site after removal of the chalazion forceps.
Despite its advantages, the traditional chalazion forceps has several limitations.46,48 Firstly, its small, round aperture constrains the size and shape of the surgical field, while its flat, solid plate on the working end does not follow the contour of the oral soft tissue. In addition, its handle is too small to be hold, and the assistant's hand is positioned too close to the surgical area, which increases the risk of iatrogenic scalpel injuries. Its design also forces the assistant to hold it in an unergonomic way.
Several improvements have been proposed for the traditional chalazion forceps. For example, the B forceps, S forceps, and Saliclick smart lip holder are designed to overcome these limitations.46, 47, 48 The B forceps and S forceps have longer handles that make them more convenient to use. The B forceps has larger plates on the working end, providing greater contact area with the tissue and thus increases the stability. It also replaces the thumbscrew with an auto-pressure system for easy application and removal. The S forceps has a wider and ovoid aperture at the working end that amplifies the surgical field. Also, the flat plate is replaced with a convex plate to elevate and compress the tissue. The Saliclick lip holder is similar in size with the conventional forceps, but it has a bigger plate to increase its retention. It also incorporates the auto-pressure system to make it more user-friendly. As claimed by their designers, these modifications can greatly improve the overall performance of these tools. For the lichen planus lesion, the biopsy specimens taken with the B forceps are shown to have less artifacts (tissue fragmentation, fissures, or hemorrhages) histologically than conventional method.49 Chalazion forceps are very useful for biopsy of salivary glands, especially the minor salivary gland for diagnosis of Sjögren's syndrome.50
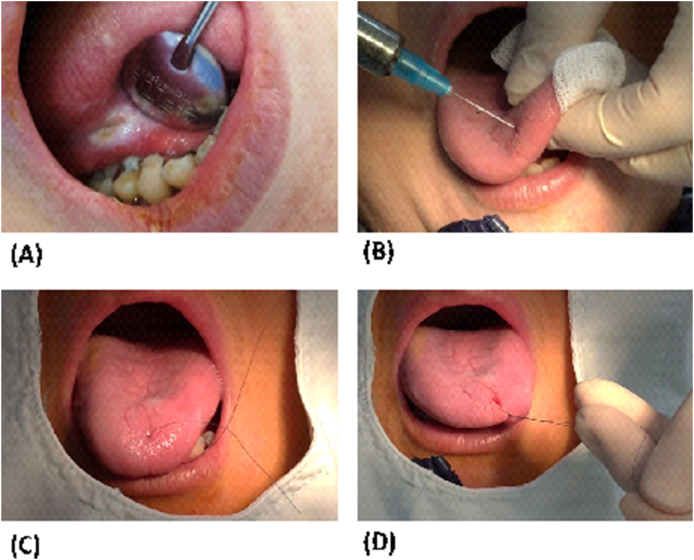
Stabilization with retraction sutures
Retraction sutures are commonly used in surgical procedures to stabilize tissue and improve visualization of the surgical site.25,30,31,35 Retraction sutures have two main applications. One is to elevate and orientate the lesion to be excised (Fig. 4), and the other is to retract and stabilize the tongue (Fig. 5). In both cases, the retraction sutures should be strong enough to hold the tissue in place. A 2-0 suture may be more favorable than 4-0 or 5-0 suture to facilitate the grasp.35,51 Silk is more favorable than nylon due to the friction.35,51,52
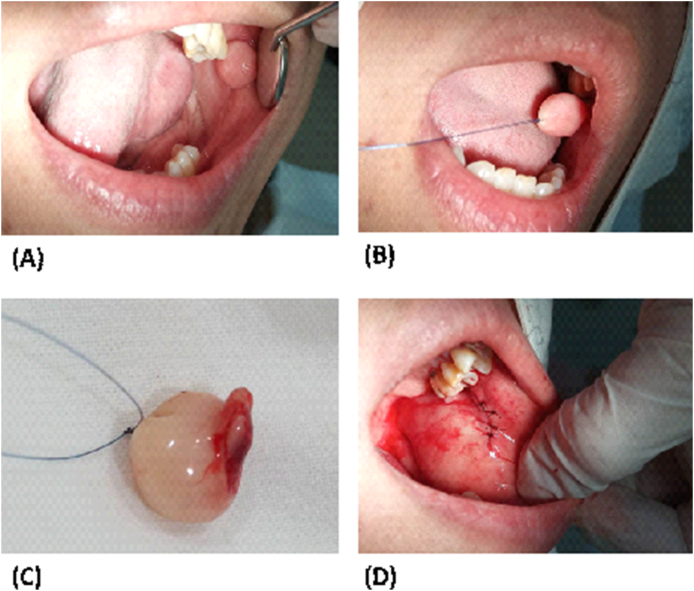
Figure 4.
(A) Fibromatous nodule over the left cheek. Clinical impression of an irritation fibroma was made. (B) The lesion was elevated using a retraction suture (C) The excised specimen. The suture should be placed deeper into the tissue to avoid laceration of the mucosa. (D) Post-operative photograph.
Figure 5.
Retraction of the tongue using a retraction suture. (A) A painful, ulcerative lesion persisted for at least 3 weeks in the ventral surface of the tongue. (B) Local anesthesia was administered. (C and D) A knot was tied with 4-0 nylon suture. Note that the use of thin, nylon suture for retraction may result in laceration of the surrounding tissue.
The first application is to place a suture within the tissue to be removed (Fig. 4). The end of the suture can be grabbed manually or suspended with a hemostat or a towel clip. This technique is quite commonly used for excision of an irritation fibroma. It not only helps the clinicians to stabilize the tissue, but also helps the pathologist for orientating the sample. However, these sutures may cause some histological artifacts such as splitting the epithelium from the connective tissue, fragmentation, and formation of pseudocyst, resulting in misinterpretation or misdiagnosis.53, 54, 55 It is recommended to tie a loose knot close to the specimen, because a tight knot may crush the superficial tissue.56 Excessive traction forces or stitches which run too superficially may lead to laceration or crush of the specimen.57 Thus, the suture should be deep enough and the force should be well controlled.
The second application is to offer secure stabilization of the tongue (Fig. 5). This technique may not be necessary in minor cases to avoid under efforts. The decision on how to stabilize the tongue should be predicated upon the clinical characteristics of the lesion. For instance, when the lesion is small, well defined, benign-appearing, and situated anteriorly on the tongue, a simple approach can be taken. In this case, stabilization with fingers and gauzes, or with chalazion forceps may be enough for conducting a biopsy. Conversely, in cases where the lesion is sizable, potentially malignant, or with poor accessibility, the use of retraction sutures may provide better stability.
Several techniques for retracting the tongue with sutures have been described. The simplest technique is to pull the tongue with a single suture (Fig. 5). Local anesthesia is first administered at the site where the suture will be inserted (Fig. 5B) and at the biopsy region. A suture is then placed deeply into the tissue, away from the lateral border of the tongue. A knot is tied once the suture has pierced through the tongue (Fig. 5D). However, this technique carries the risk of damaging the veins, arteries and nerves on the ventral surfaces of the tongue due to the suture running through the middle of the tongue.35,51
Another technique involves using two retraction sutures simultaneously to provide additional stability and ensure safety.30,51 Both sutures are placed in the anterior third, with one on the left side and the other on the right side. These sutures are then pulled concomitantly to orientate and stabilize the tongue tissue. Recently a novel but atraumatic approach has been proposed.35 It combines the use of nasogastric tube with retraction sutures. The tube is cut into halves and placed on the dorsal and ventral surface of the tongue, respectively. The authors claimed that the tube can serve as a shield between the suture and the tongue; thus, it can prevent unnecessary trauma to the tongue tissue.
Other surgical tools
Other tools can also be helpful during major and minor oral surgeries. The dental mirror, as well as several types of surgical retractor can help retract the tongue and cheek. Choosing the appropriate retractor for the specific surgical site is essential, as the retractors vary in size and design.25,51 These instruments are especially useful when biopsy sites are located in the mouth floor. Cotton rolls can also be inserted to the lingual sulci to move the tongue aside and assist in moisture control.25 A mouth gag or a bite block can be helpful when lesions are localized in the posterior area of the mouth.
Adson forceps (fine-tip forceps) can also grasp and lift the specimen during biopsy.56 However, it is crucial to use the forceps cautiously to avoid tearing, compression, or the formation of pseudocyst in the specimen.53,55 The specimen should be handled gently and grasped in an area less critical for the pathological examination.
It is noteworthy that careful manipulation of the specimen is essential at any stages - before, during, and after the biopsy surgery - to prevent the production of artifacts.54,55 A large amount of infiltrative anesthesia could result in vacuolation and even separation of the epithelium from the connective tissue.55 Thermal damage caused by laser or electric scalpel could lead to tissue cauterization, making the specimen uninterpretable.58 Excision without adequate margin not only renders its diagnostic value, but also increases the risk of recurrence in aggressive pathologic lesions. In contrast, artifacts created by the stabilizing instrument may have a relatively small effect on the histopathological examination and interpretation.
Conclusion
Soft tissue stabilization can be a challenging process during oral surgery. It often involves the cooperation of the operator and the assistants to overcome these challenges and ensure a successful clinical outcome for the patients. Fingers, gauzes, chalazion forceps, retraction sutures, etc. may be helpful in stabilizing the oral tissues. However, none of these instruments is completely perfect and can serve in all cases. Clinicians should consider the clinical characteristics of the oral lesion, the surrounding anatomy, and their own experience and preference to select an appropriate tool for the soft tissue stabilization during the biopsy procedure.
Declaration of competing interest
All authors declare there are no conflict of interest for this submission.
Acknowledgments
This study was supported by grants from Chang Gung Memorial Hospital (CMRPF1M0081, CMRPF1N0061), and the Ministry of Science and Technology (MOST107-2314-B-255-009-MY3, MOST107-2314-B-255-008-MY2, MOST108-2314-B-002-043-MY3, MOST110-2314-B255-002-MY3, MOST110-2314-B-255-003-MY3, MOST111-2314-B002-109-MY3, and MOST111-2314-B002-107-MY3), Kaohsiung Medical University & Hospital (KMU-Q111004, KMU-110KK040, KMUH-DK(A)-111002, KMUH111-1T09) and Kaohsiung Veterans General Hospital.
Contributor Information
Chun-Feng Chen, Email: 261463@gmail.com.
Jiiang-Huei Jeng, Email: jhjeng@ntu.edu.tw, jhjeng@kmu.edu.tw.
References
- 1.Shanti R.M., Tanaka T., Stanton D.C. Oral biopsy techniques. Dermatol Clin. 2020;38:421–427. doi: 10.1016/j.det.2020.05.003. [DOI] [PubMed] [Google Scholar]
- 2.Kumaraswamy K.L., Vidhya M., Rao P.K., Mukunda A. Oral biopsy: oral pathologist's perspective. J Cancer Res Therapeut. 2012;8:192–198. doi: 10.4103/0973-1482.98969. [DOI] [PubMed] [Google Scholar]
- 3.Hong C.H.L., Dean D.R., Hull K., et al. World workshop on oral medicine VII: relative frequency of oral mucosal lesions in children, a scoping review. Oral Dis. 2019;25(Suppl 1):193–203. doi: 10.1111/odi.13112. [DOI] [PubMed] [Google Scholar]
- 4.Randall D.A., Wilson Westmark N.L., Neville B.W. Common oral lesions. Am Fam Physician. 2022;105:369–376. [PubMed] [Google Scholar]
- 5.Alsharif S.A., Alsharif A.T., Krsoum M.A., et al. Trend analysis of head and neck neoplasms between 2012-2018 in patients residing in Al-Madinah, Saudi Arabia: a retrospective study. Eur J Dermatol. 2021;15:509–514. doi: 10.1055/s-0040-1722090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang Y.P., Chen H.M., Kuo R.C., et al. Oral verrucous hyperplasia: histologic classification, prognosis, and clinical implications. J Oral Pathol Med. 2009;38:651–656. doi: 10.1111/j.1600-0714.2009.00790.x. [DOI] [PubMed] [Google Scholar]
- 7.Yang Y.H., Lien Y.C., Ho P.S., et al. The effect of chewing areca/betel quid with and without cigarette smoking on oral submucous fibrosis and oral mucosal lesions. Oral Dis. 2005;11:88–94. doi: 10.1111/j.1601-0825.2004.01061.x. [DOI] [PubMed] [Google Scholar]
- 8.Ko Y.C., Huang Y.L., Lee C.H., Chen M.J., Lin L.M., Tsai C.C. Betel quid chewing, cigarette smoking and alcohol consumption related to oral cancer in Taiwan. J Oral Pathol Med. 1995;24:450–453. doi: 10.1111/j.1600-0714.1995.tb01132.x. [DOI] [PubMed] [Google Scholar]
- 9.Jeng J.H., Chang M.C., Hahn L.J. Role of areca nut in betel quid-associated chemical carcinogenesis: current awareness and future perspectives. Oral Oncol. 2001;37:477–492. doi: 10.1016/s1368-8375(01)00003-3. [DOI] [PubMed] [Google Scholar]
- 10.Chang M.C., Chiang C.P., Lin C.L., Lee J.J., Hahn L.J., Jeng J.H. Cell-mediated immunity and head and neck cancer: with special emphasis on betel quid chewing habit. Oral Oncol. 2005;41:757–775. doi: 10.1016/j.oraloncology.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 11.Yeh C.Y., Lin C.L., Chang M.C., et al. Differences in oral habit and lymphocyte subpopulation affect malignant transformation of patients with oral precancer. J Formos Med Assoc. 2016;115:263–268. doi: 10.1016/j.jfma.2015.07.017. [DOI] [PubMed] [Google Scholar]
- 12.Yeh C.Y., Chen H.M., Chang M.C., et al. Cytotoxicity and transformation of C3H10T1/2 cells induced by areca nut components. J Formos Med Assoc. 2016;115:108–112. doi: 10.1016/j.jfma.2015.01.004. [DOI] [PubMed] [Google Scholar]
- 13.Hashim R., Abo-Fanas A., Al-Tak A., et al. Early detection of oral cancer- Dentists' knowledge and practices in the United Arab Emirates. Asian Pac J Cancer Prev APJCP. 2018;19:2351–2355. doi: 10.22034/APJCP.2018.19.8.2351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Anandani C., Metgud R., Ramesh G., Singh K. Awareness of general dental practitioners about oral screening and biopsy procedures in Udaipur, India. Oral Health Prev Dent. 2015;13:523–530. doi: 10.3290/j.ohpd.a32993. [DOI] [PubMed] [Google Scholar]
- 15.Tong K.N. Uniformed Services University of the Health Sciences; Maryland, United States: 2019. Evaluation of the importance of soft tissue biopsy in military dentistry (Master's thesis) [Google Scholar]
- 16.Budhraja N.J., Shenoi S.R., Iqbal M.A. Knowledge and attitude of the general dentists towards oral biopsy procedure: a cross-sectional study. Acta Sci Dent Sci. 2019:35–39. [Google Scholar]
- 17.López Jornet P., Velandrino Nicolás A., Martínez Beneyto Y., Fernández Soria M. Attitude towards oral biopsy among general dentists in Murcia. Med Oral Patol Oral Cir Bucal. 2007;12:E116–E121. [PubMed] [Google Scholar]
- 18.Mendez M., Haas A.N., Rados P.V., Filho M.S., Carrard V.C. Agreement between clinical and histopathologic diagnoses and completeness of oral biopsy forms. Braz Oral Res. 2016;30:e94. doi: 10.1590/1807-3107BOR-2016.vol30.0094. [DOI] [PubMed] [Google Scholar]
- 19.Chen S., Forman M., Sadow P.M., August M. The diagnostic accuracy of incisional biopsy in the oral cavity. J Oral Maxillofac Surg. 2016;74:959–964. doi: 10.1016/j.joms.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 20.Lee J.J., Hung H.C., Cheng S.J., et al. Factors associated with underdiagnosis from incisional biopsy of oral leukoplakic lesions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:217–225. doi: 10.1016/j.tripleo.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 21.Daneshpazhooh M., Chams-Davatchi C.C., Ramezani A., Moinedin F., Memami M.R. Abortive aphthous-like oral lesions: an underreported initial presentation of pemphigus vulgaris. J Eur Acad Dermatol Venereol. 2009;23:157–159. doi: 10.1111/j.1468-3083.2008.03007.x. [DOI] [PubMed] [Google Scholar]
- 22.Daltaban O., Ozcentik A., Akman Karakas A., Ustun K., Hatipoglu M., Uzun S. Clinical presentation and diagnostic delay in pemphigus vulgaris: a prospective study from Turkey. J Oral Pathol Med. 2020;49:681–686. doi: 10.1111/jop.13052. [DOI] [PubMed] [Google Scholar]
- 23.Costa S., Quintin-Roue I., Lesourd A., et al. Reliability of histopathological salivary gland biopsy assessment in Sjögren’s syndrome: a multicenter cohort study. Rheumatology. 2015;54:1056–1064. doi: 10.1093/rheumatology/keu453. [DOI] [PubMed] [Google Scholar]
- 24.Langerman A.J., Blair E.A., Sweiss N.J., Taxy J.B. Utility of lip biopsy in the diagnosis and treatment of Sjögren’s syndrome. Laryngoscope. 2007;117:1004–1008. doi: 10.1097/MLG.0b013e31804654f7. [DOI] [PubMed] [Google Scholar]
- 25.Davari P., Fazel N. Practical pearls for oral procedures. Clin Dermatol. 2016;34:440–448. doi: 10.1016/j.clindermatol.2016.02.016. [DOI] [PubMed] [Google Scholar]
- 26.Pentenero M., Carrozzo M., Pagano M., et al. Oral mucosal dysplastic lesions and early squamous cell carcinomas: underdiagnosis from incisional biopsy. Oral Dis. 2003;9:68–72. doi: 10.1034/j.1601-0825.2003.02875.x. [DOI] [PubMed] [Google Scholar]
- 27.Jain N. Essentials before sending biopsy specimens: a surgeon's perspective and pathologists concern. J Maxillofac Oral Surg. 2011;10:361–364. doi: 10.1007/s12663-011-0234-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McNamara K.K., Kalmar J.R. Pearls and pitfalls in the diagnosis of small oral biopsies. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2023;40:313–320. doi: 10.1053/j.semdp.2023.03.001. [DOI] [PubMed] [Google Scholar]
- 29.Lazzarotto B., Garcia C., Martinelli-Klay C., Lombardi T. Biopsy of the oral mucosa: does size matter? J Stomatol Oral Maxillofac Surg. 2022;123:e385–e389. doi: 10.1016/j.jormas.2022.02.005. [DOI] [PubMed] [Google Scholar]
- 30.Ellis E. In: Tucker MR. Contemporary oral and maxillofacial surgery. 7th ed. Hupp J.R., Ellis E., editors. Elservier; Philadelphia, PA: 2019. Principles of differential diagnosis and biopsy. [Google Scholar]
- 31.Avon S.L., Klieb H.B.E. Oral soft-tissue biopsy: an overview. J Can Dent Assoc. 2012;78:c75. [PubMed] [Google Scholar]
- 32.Zaragan M. Clinicians' role in the occurrence of oral biopsy artifacts as a potential diagnostic dilemma. Dent Med Probl. 2019;56:299–306. doi: 10.17219/dmp/108597. [DOI] [PubMed] [Google Scholar]
- 33.Zargaran M. A review of biopsy in dentistry: principles, techniques, and considerations. J Dent Mater Tech. 2014;3:47–54. [Google Scholar]
- 34.Kalmar J.R., McNamara K.K. In: Peterson's principles of oral and maxillofacial surgery. Miloro M., Ghali G.E., Larsen P.E., Waite P., editors. Springer; Cham: 2022. Differential diagnosis of oral disease. [Google Scholar]
- 35.Papadogeorgakis N., Kalfarentzos E., Fouzas M. An atraumatic method to retract the tongue during oral surgery procedures: a technical note. J Maxillofac Oral Surg. 2021;20:319–321. doi: 10.1007/s12663-020-01369-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kaner K.H. Referral and management considerations for a biopsy: why choose the oral and maxillofacial surgeon. Dent Clin. 2020;64:241–247. doi: 10.1016/j.cden.2019.08.013. [DOI] [PubMed] [Google Scholar]
- 37.Akarslan Z.Z., Biçer A.Z. Utility of the gagging problem assessment questionnaire in assessing patient sensitivity to dental treatments. J Oral Rehabil. 2012;39:948–955. doi: 10.1111/j.1365-2842.2012.02321.x. [DOI] [PubMed] [Google Scholar]
- 38.Elseviers M.M., Arias-Guillen M., Gorke A., Arens H.J. Sharps injuries amongst healthcare workers: review of incidence, transmissions and costs. J Ren Care. 2020;40:150–156. doi: 10.1111/jorc.12050. [DOI] [PubMed] [Google Scholar]
- 39.Lokest U., Srinidhi D., Sudhakara Reddy K. Post exposure prophylaxis to occupational injuries for general dentist. J Indian Prosthodont Soc. 2014;14:1–3. doi: 10.1007/s13191-012-0176-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mischke C., Verbeek J.H., Saarto A., Lavoie M.C., Pahwa M., Ijaz S. Gloves, extra gloves or special types of gloves for preventing percutaneous exposure injuries in healthcare personnel. Cochrane Database Syst Rev. 2014;7:CD009573. doi: 10.1002/14651858.CD009573.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang Z., Gao X., Ruan X., Zheng B. Effectiveness of double-gloving method on prevention of surgical glove perforations and blood contamination: a systematic review and meta-analysis. J Adv Nurs. 2021;77:3630–3643. doi: 10.1111/jan.14824. [DOI] [PubMed] [Google Scholar]
- 42.Bhat S., Periasamy S., Murugaiyan A. Chalazion forceps-An instrument used for mucocele and biopsy of oral lesions: a literature review. J Res Med Dent Sci. 2020;8:138–141. [Google Scholar]
- 43.Syed M.I., Ilan O., Rutka J.A. A simple technique for minor salivary gland and oral biopsy in the clinic: Our experience. Clin Otolaryngol. 2015;40:403–404. doi: 10.1111/coa.12335. [DOI] [PubMed] [Google Scholar]
- 44.Shah L., Fogden S. Use of a chalazion clamp for intraoral biopsies: a technical note. Br J Oral Maxillofac Surg. 2019;58:105–106. doi: 10.1016/j.bjoms.2019.10.307. [DOI] [PubMed] [Google Scholar]
- 45.Byrne L.O., Ramli R., Khoo S.G. The accuracy of dry surgical field sublabial biopsy in the diagnosis of sicca syndrome. J Laryngol Otol. 2021;135:834–838. doi: 10.1017/S0022215121002073. [DOI] [PubMed] [Google Scholar]
- 46.Bermejo-Fenoll A., López-Jornet P. Instrument for biopsy of oral lesions: an improved chalazion forceps. Dermatol Surg. 2006;32:1493–1495. doi: 10.1111/j.1524-4725.2006.32360.x. [DOI] [PubMed] [Google Scholar]
- 47.Varela-Centelles P., Sánchez-Sánchez M., Costa-Bouzas J., Seoane-Romero J.M., Seoane J., Takkouche B. Neurological adverse events related to lip biopsy in patients suspicious for Sjögren’s syndrome: a systematic review and prevalence meta-analysis. Rheumatology. 2014;53:1208–1214. doi: 10.1093/rheumatology/ket485. [DOI] [PubMed] [Google Scholar]
- 48.Dumusc A., Bannert B., Kollert F., et al. Use of a smart lip holder for minimally invasive minor salivary gland biopsy. BMJ Innov. 2021;7:445–447. [Google Scholar]
- 49.Bermejo-Fenoll A., Lopez-Jornet M.P., Jimenez-Torres M.J., Camacho-Alonso F., Orduna-Domingo A. Biopsy of the buccal mucosa in oral lichen planus: the traditional method versus the use of a new pressure forceps. J Am Dent Assoc. 2007;138:957–962. doi: 10.14219/jada.archive.2007.0292. [DOI] [PubMed] [Google Scholar]
- 50.Varela-Centelles P., Seoane-Romero J.M., Sánchez-Sánchez M., González-Mosquera A., Diz-Dios P., Seoane J. Minor salivary gland biopsy in Sjögren’s syndrome: a review and introduction of a new tool to ease the procedure. Med Oral Patol Oral Cir Bucal. 2014;19:e20–e23. doi: 10.4317/medoral.19131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vyas T. Biopsy of oral lesion – a review article. J Adv Med Dent Sci Res. 2018;6:27–35. [Google Scholar]
- 52.Tajirian A.L., Goldberg D.J. A review of sutures and other skin closure materials. J Cosmet Laser Ther. 2010;12:296–302. doi: 10.3109/14764172.2010.538413. [DOI] [PubMed] [Google Scholar]
- 53.Seoane J., Varela-Centelles P., Ramirez J.R., Romero M.A., De La Cruz A. Artefacts produced by suture traction during incisional biopsy of oral lesion. Clin Otolaryngol Allied Sci. 2022;27:549–553. doi: 10.1046/j.1365-2273.2002.00619.x. [DOI] [PubMed] [Google Scholar]
- 54.Rastogi V., Puri N., Arora S., Kaur G., Yadav L., Sharma R. Artefacts: a diagnostic dilemma – a review. J Clin Diagn Res. 2013;7:2408–2413. doi: 10.7860/JCDR/2013/6170.3541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Khan S., Tijare M., Jain M., Desai A. Artifacts in histopathology: a potential cause of misinterpretation. J Dent Sci. 2014;2:23–31. [Google Scholar]
- 56.Oliver R.J., Sloan P., Pemberton M.N. Oral biopsies: methods and applications. Br Dent J. 2004;196:329–333. doi: 10.1038/sj.bdj.4811075. [DOI] [PubMed] [Google Scholar]
- 57.Mota-Ramiréz A., Silvestre F.J., Simó J.M. Oral biopsy in dental practice. Med Oral Patol Oral Cir Bucal. 2007;12:E504–E510. [PubMed] [Google Scholar]
- 58.Baggish M.S., Barash F., Noel Y., Brooks M. Comparison of thermal injury zones in loop electrical and laser cervical excisional conization. Am J Obstet Gynecol. 1992;166:545–548. doi: 10.1016/0002-9378(92)91668-z. [DOI] [PubMed] [Google Scholar]