SUMMARY
When choosing a voluntary blood donor (VBD), it is important to ensure the donor health, and at the same time to produce a quality and safe blood product. The donor selection process leads to donor rejection related to their current health condition. The aim of this study was to determine gender differences in VBDs, to examine the reasons for their rejection, and to determine the share of permanently and temporarily deferred VBD, especially due to low hemoglobin levels. The research was conducted in eastern Croatia in the 2014 to 2018 period. The study included 144,041 blood donations from a total of 80,418 VBDs, of which 83.3% of donations were from male VBDs and 16.7% from female VBDs. There were 11.46% of temporarily deferred and permanently rejected donors. Out of all temporarily deferred donors and possible reasons for deferral, the largest share of deferrals referred to a reduced hemoglobin level, which accounted for 54% in female VBD and 46% in male VBD. Female VBDs made up to one-third of total VBDs and account for one-sixth of total blood donations. Low hemoglobin was the most common reason for VBD deferral. Gender and age are related to blood hemoglobin levels in rejected and accepted donors. Female VBDs represent a potential reservoir for increasing the total number of VBDs.
Key words: Blood donor, Gender differences, Deferral, Hemoglobin
Introduction
A voluntary blood donor (VBD) is a person who donates blood, plasma or cellular components of blood according to the principles of voluntariness, solidarity, anonymity and free of charge (1). Blood is a national treasure of every country, and a VBD is an indirect, active participant in the treatment of patients, or an active link between the healthy part of society and patients. A precondition for donating blood is good health of the person donating blood, but there are situations where donor’s health is impaired, and donor must be temporarily or permanently deferred. According to the Recommendations of the Council of Europe (European Committee, European Directorate for the Quality of Medicines (EDQM), Guide to the Preparation Use and Quality Assurance of Blood Components, 18th Edition) and Good Manufacturing Practices (Good Manufacturing Practices for Blood Establishment, GMP), basic criteria need to be met so that a person can become a VBD (1).
The selection of VBD is important primarily to protect the health of donors, and consequently to ensure the quality and safety of blood products for transfusion treatment (2-4). The hemovigilance system in transfusion medicine is constantly considering the criteria for selecting VBDs. According to the EDQM guidelines and European Union (EU) Blood Directives that have been transposed into Croatian legislation, the basic criteria in selecting VBD are general condition, body weight (≥55 kg), age, body temperature (<37 °C), pulse (50-100 min), pressure (systolic 100-180 mm Hg, diastolic 60-110 mm Hg) and hemoglobin value (men 135 g/L, women 125 g/L). Men can donate blood every 3 months, and women every 4 months or platelets every month. According to the criteria for selecting VBDs, donors may be temporarily or permanently deferred. Depending on their health condition, temporarily deferred donors are deferred for a certain period depending on the reason of deferral. Permanently deferred donors are those who are prevented from further blood donation to preserve the health of voluntary donors and the health of recipients. Due to the reduced hemoglobin concentration, a significant number of VBDs are temporarily deferred, which may have an impact on self-sufficiency and blood supply (5, 6).
The aim of the study was to determine demographic characteristics and reasons for deferral of VBDs in eastern Croatia in the 2014-2018 period, with emphasis on temporary deferrals due to low hemoglobin levels. Our goal was to review hemoglobin concentrations among temporary deferred blood donors and determine their distribution in the predefined age groups. The purpose was to identify which age groups of donors were affected most by the low levels of hemoglobin and, therefore, should be monitored and further tested to determine their iron levels or potential anemia. It is known that hemoglobin concentration is related to iron levels and regular blood donors may develop anemia after blood donation despite the acceptable hemoglobin concentration during donor selection (7-11). In order to safeguard donor’s health, it is important to analyze such data and systematically monitor donors at the national level (12, 13).
Subjects and Methods
The study population included all VBDs, those who donated whole blood units, and those who did not donate blood due to temporary or permanent deferral in the 2014-2018 period. Department of Transfusion Medicine in Osijek collected blood in the eastern Croatia region that consists of 4 counties: Osijek-Baranja County, Vukovar-Srijem County, Virovitica-Podravina County and Brod-Posavina County. Data were collected prospectively and obtained from the national e-Delphyn IT transfusion program. Data on the number of donors, whole blood donations, and reasons for temporary and permanent deferral of VBDs were extracted from the database. The research was designed as a retrospective study.
During the study period, a validated quantitative method for determination of hemoglobin concentration from capillary blood on a Hemo Control analyzer (EKF, Barleben, Germany) was used, as described in the literature (14). The devices are calibrated and regularly preventively maintained according to the manufacturer’s recommendations.
Ethics
All the procedures in the study were in accordance with ethical standards of the institutional or regional board on human experimentation and Helsinki Declaration from 1975, as revised in 1983. Ethical approval for this study was obtained from Ethics Committee of Osijek University Hospital Center, Osijek, Croatia (R1-1954-412020).
Statistical methods
Statistical analysis was done with SPSS software package for Windows (version 9.0, Carry, New York, USA). The following tests were used: t-test, Pearson’s χ2-test, simple analysis of variance (ANOVA, Bonferroni post-hoc test), Fisher exact test, and Spearman’s correlation coefficient.
Results
During the 2014-2018 study period, a total of 80,418 donors, 60,423 (66.91%) males and 19,995 (33.09%) females, donated 144,041 blood donations. Annual data showed a higher participation of females in 2017 and 2018, and of males in 2014, 2015 and 2016. These differences were statistically nonsignificant (χ2-test, p<0.001). The highest number of males were in the 26-55 age group, while the highest number of females were in the ≤25 age group (χ2-test, p<0.001) (Table 1). Males donated 119,920 (83.3%) donations and females 24,121 (16.7%) donations. Although females constituted one-third of the overall donor pool, they accounted for only one-sixth of all blood donations (Table 2).
Table 1. Annual number of blood donors by age and gender in the 2014-2018 period.
| Age group (yrs) | Number (%) of participants according to gender | p* | ||
|---|---|---|---|---|
| VBD male | VBD female | Total | ||
| 2014 | <0.001 | |||
| ≤25 | 782 (6.7) | 643 (19.1) | 1425 (9.5) | |
| 26-35 | 2906 (24.9) | 1026 (30.4) | 3932 (26.1) | |
| 36-45 | 3095 (26.5) | 687 (20.4) | 3782 (25.1) | |
| 46-55 | 2768 (23.7) | 550 (16.3) | 3318 (22) | |
| 56-65 | 1745 (14.9) | 393 (11.7) | 2138 (14.2) | |
| ≥66 | 385 (3.3) | 71 (2.1) | 456 (3) | |
| Total | 11681 (100) | 3370 (100) | 15051 (100) | |
| 2015 | <0.001 | |||
| ≤25 | 1032 (8.4) | 910 (23.1) | 1942 (11.9) | |
| 26-35 | 3227 (26.1) | 1141 (28.9) | 4368 (26.8) | |
| 36-45 | 3291 (26.7) | 809 (20.5) | 4100 (25.2) | |
| 46-55 | 2788 (22.6) | 626 (15.9) | 3414 (21) | |
| 56-65 | 1690 (13.7) | 391 (9.9) | 2081 (12.8) | |
| ≥66 | 319 (2.6) | 65 (1.6) | 384 (2.4) | |
| Total | 12347 (100) | 3942 (100) | 16289 (100) | |
| 2016 | <0.001 | |||
| ≤25 | 1343 (11.2) | 1060 (28) | 2403 (15.2) | |
| 26-35 | 3086 (25.7) | 965 (25.5) | 4051 (25.7) | |
| 36-45 | 3158 (26.3) | 759 (20) | 3917 (24.8) | |
| 46-55 | 2608 (21.7) | 598 (15.8) | 3206 (20.3) | |
| 56-65 | 1530 (12.8) | 363 (9.6) | 1893 (12) | |
| ≥66 | 267 (2.2) | 41 (1.1) | 308 (2) | |
| Total | 11992 (100) | 3786 (100) | 15778 (100) | |
| 2017 | <0.001 | |||
| ≤5 | 1741 (14.3) | 1394 (31.7) | 3135 (18.9) | |
| 26-35 | 3108 (25.5) | 1029 (23.4) | 4137 (24.9) | |
| 36-45 | 3104 (25.5) | 896 (20.3) | 4000 (24.1) | |
| 46-55 | 2562 (21) | 689 (15.6) | 3251 (19.6) | |
| 56-65 | 1448 (11.9) | 364 (8.3) | 1812 (10.9) | |
| ≥66 | 220 (1.8) | 31 (0.7) | 251 (1.5) | |
| Total | 12183 (100) | 4403 (100) | 16586 (100) | |
| 2018 | <0.001 | |||
| ≤25 | 1949 (15.9) | 1529 (34) | 3478 (20.8) | |
| 26-35 | 3220 (26.4) | 1005 (22.4) | 4225 (25.3) | |
| 36-45 | 3061 (25) | 938 (20.9) | 3999 (23.9) | |
| 46-55 | 2477 (20.3) | 679 (15.1) | 3156 (18.9) | |
| 56-65 | 1332 (10.9) | 316 (7) | 1648 (9.9) | |
| ≥66 | 181 (1.5) | 27 (0.6) | 208 (1.2) | |
| Total | 12220 (100) | 4494 (100) | 16714 (100) | |
*χ2-test; VBD = voluntary blood donor
Table 2. Annual number of donations by donor age and gender in the 2014-2018 period.
| Age group (yrs) | Number (%) of participants according to gender | p* | ||
|---|---|---|---|---|
| VBD male | VBD female | Total | ||
| ≤25 | 9213 (7.7) | 5161 (21.4) | 14374 (10) | <0.001 |
| 26-35 | 29308 (24.4) | 5844 (24.2) | 35152 (24.4) | |
| 36-45 | 33151 (27.6) | 5199 (21.6) | 38350 (26.6) | |
| 46-55 | 28831 (24) | 4545 (18.8) | 33376 (23.2) | |
| 56-65 | 16842 (14) | 2999 (12.4) | 19841 (13.8) | |
| ≤66 | 2575 (2.1) | 373 (1.5) | 2948 (2) | |
| Total | 119920 (100) | 24121 (100) | 144041 (100) | |
*χ2-test; VBD = voluntary blood donor
Of all VBDs donating in the study period, the number of deferrals was 16,161 (11.46%), of which 9,165 (56.7%) were males and 6,996 (43.3%) females. The percentage of deferred VBDs did not differ significantly between male and female donors throughout the study period. During 2017 and 2018, there were significantly more deferred female VBDs compared to male VBDs (χ2-test, p<0.001) (Table 3).
Table 3. Annual number of deferred blood donors by gender in the 2014-2018 period.
| Year | Number (%) of participants in regard to gender | p* | ||
|---|---|---|---|---|
| VBD male | VBD female | Total | ||
| 2014 | 1746 (19.1) | 1162 (16.6) | 2908 (18) | <0.001 |
| 2015 | 1449 (15.8) | 1133 (16.2) | 2582 (16) | |
| 2016 | 2270 (24.8) | 1438 (20.6) | 3708 (22.9) | |
| 2017 | 1855 (20.2) | 1679 (24) | 3534 (21.9) | |
| 2018 | 1845 (20.1) | 1584 (22.6) | 3429 (21.2) | |
| Total | 9165 (100) | 6996 (100) | 16161 (100) | |
*χ2-test; VBD = voluntary blood donor
Out of 271 permanently deferred donors, 197 (72.7%) were males, yielding a statistically significant gender difference in permanently deferred donors annually (χ2-test, p=0.04) (Table 4).
Table 4. Permanently deferred VBDs by age and gender.
| Year | Number (%) of participants in regard to gender | p* | ||
|---|---|---|---|---|
| VBD male | VBD female | Total | ||
| 2014 | 34 (17.3) | 10 (13.5) | 44 (16.2) | 0.04 |
| 2015 | 37 (18.8) | 10 (13.5) | 47 (17.3) | |
| 2016 | 38 (19.3) | 9 (12.2) | 47 (17.3) | |
| 2017 | 26 (13.2) | 21 (28.4) | 47 (17.3) | |
| 2018 | 62 (31.5) | 24 (32.4) | 86 (31.7) | |
| Total | 197 (100) | 74 (100) | 271 (100) | |
*χ2-test; VBD = voluntary blood donor
Among temporarily deferred donors, there were significantly more females than males in the ≤25 age group (χ2-test, p=0.04) (Table 5).
Table 5. Temporarily deferred VBDs by age and gender.
| Age group (yrs) | Number (%) of participants according to gender | p* | ||
|---|---|---|---|---|
| VBD male | VBD female | Total | ||
| 2014 | <0.001 | |||
| ≤25 | 363 (20.8) | 497 (42.8) | 860 (29.6) | |
| 26-35 | 296 (17) | 236 (20.3) | 532 (18.3) | |
| 36-45 | 416 (23.8) | 214 (18.4) | 630 (21.7) | |
| 46-55 | 371 (21.2) | 154 (13.3) | 525 (18.1) | |
| 56-65 | 289 (16.6) | 59 (5.1) | 348 (12) | |
| ≥66 | 11 (0.6) | 2 (0.2) | 13 (0.4) | |
| Total | 1746 (100) | 1162 (100) | 2908 (100) | |
| 2015 | <0.001 | |||
| ≤25 | 371 (25.6) | 513 (45.3) | 884 (34.2) | |
| 26-35 | 297 (20.5) | 273 (24.1) | 570 (22.1) | |
| 36-45 | 306 (21.1) | 198 (17.5) | 504 (19.5) | |
| 46-55 | 280 (19.3) | 116 (10.2) | 396 (15.3) | |
| 56-65 | 175 (12.1) | 33 (2.9) | 208 (8.1) | |
| ≥66 | 20 (1.4) | 0 | 20 (0.8) | |
| Total | 1449 (100) | 1133 (100) | 2582 (100) | |
| 2016 | <0.001 | |||
| ≤25 | 417 (18.4) | 543 (37.8) | 960 (25.9) | |
| 26-35 | 525 (23.1) | 316 (22) | 841 (22.7) | |
| 36-45 | 510 (22.5) | 332 (23.1) | 842 (22.7) | |
| 46-55 | 461 (20.3) | 176 (12.2) | 637 (17.2) | |
| 56-65 | 330 (14.5) | 69 (4.8) | 399 (10.8) | |
| ≥66 | 27 (1.2) | 2 (0.1) | 29 (0.8) | |
| Total | 2270 (100) | 1438 (100) | 3708 (100) | |
| 2017 | <0.001 | |||
| ≤25 | 386 (20.8) | 698 (41.6) | 1084 (30.7) | |
| 26-35 | 414 (22.3) | 379 (22.6) | 793 (22.4) | |
| 36-45 | 395 (21.3) | 359 (21.4) | 754 (21.3) | |
| 46-55 | 369 (19.9) | 176 (10.5) | 545 (15.4) | |
| 56-65 | 255 (13.7) | 65 (3.9) | 320 (9.1) | |
| ≥66 | 36 (1.9) | 2 (0.1) | 38 (1.1) | |
| Total | 1855 (100) | 1679 (100) | 3534 (100) | |
| 2018 | <0.001 | |||
| ≤25 | 398 (21.6) | 659 (41.6) | 1057 (30.8) | |
| 26-35 | 430 (23.3) | 351 (22.2) | 781 (22.8) | |
| 36-45 | 373 (20.2) | 301 (19) | 674 (19.7) | |
| 46-55 | 345 (18.7) | 215 (13.6) | 560 (16.3) | |
| 56-65 | 257 (13.9) | 55 (3.5) | 312 (9.1) | |
| ≥66 | 42 (2.3) | 3 (0.2) | 45 (1.3) | |
| Total | 1845 (100) | 1584 (100) | 3429 (100) | |
*χ2-test; VBD = voluntary blood donor
The most frequent reason for deferral was a low hemoglobin concentration (39% of all deferred donors), followed by blood pressure (26%) and respiratory problems (3%), whereas all other particular reasons accounted for less than 3%.
The total number of temporarily deferred donors due to hemoglobin concentration was 5773, including 3102 (54%) females and 2671 (46%) males. Of all temporarily deferred female donors, 44.82% (3102/6921) were due to low hemoglobin levels. Among temporarily deferred males, 34.55% (2671/7731) were due to low hemoglobin levels (Tables 6 and 7).
Table 6. Temporarily deferred male VBDs according to the reason for deferral in the 2014-2018 period.
| Male VBDs – temporarily deferred | Number (%) of participants according to age | p* | ||||||
|---|---|---|---|---|---|---|---|---|
| ≤25 (n=1916) |
26 - 35 (n=1559) |
36 -45 (n=1665) |
46 -55 (n=1504) |
56 -65 (n=965) |
≥ 66 (n=122) |
Total (n=7731) |
||
| Alcoholism | 5 (0.3) |
21 (1.3) | 30 (1.8) |
57 (3.8) |
30 (3.1) | 2 (1.6) | 145 (1.9) | <0.001 |
| Endocrinologic system diseases | 4 (0.2) |
10 (0.6) | 13 (0.8) | 5 (0.3) |
2 (0.2) |
0 | 34 (0.4) |
0.07 |
| Genitourinary tract diseases | 9 (0.5) |
8 (0.5) |
15 (0.9) |
9 (0.6) |
14 (1.5) |
0 | 55 (0.7) |
0.04 |
| Skin and subcutaneous tissue disorders | 13 (0.7) |
27 (1.7) |
17 (1) |
7 (0.5) |
6 (0.6) |
0 | 70 (0.9) |
0.002 |
| Digestive system diseases | 32 (1.7) | 51 (3.3) | 61 (3.7) | 61 (4.1) | 44 (4.6) | 1 (0.8) | 250 (3.2) | <0.001 |
| Respiratory diseases | 140 (7.3) | 91 (5.8) | 56 (3.4) | 40 (2.7) | 22 (2.3) | 1 (0.8) | 350 (4.5) | <0.001 |
| Cardiovascular diseases | 45 (2.3) | 17 (1.1) | 24 (1.4) | 32 (2.1) | 33 (3.4) | 2 (1.6) | 153 (2) | 0.001 |
| Nerve and mental diseases | 9 (0.5) |
13 (0.8) | 22 (1.3) | 13 (0.9) | 9 (0.9) |
1 (0.8) | 67 (0.9) | 0.18 |
| DAT positive – temporarily | 0 | 0 | 0 | 1 (0.1) |
1 (0.1) |
0 | 2 (0.03) | 0.47 |
| Malaria testing | 14 (0.7) | 70 (4.5) | 77 (4.6) | 13 (0.9) | 2 (0.2) |
0 | 176 (2.3) | <0.001 |
| Blood pressure | 715 (37.3) | 319 (20.5) | 308 (18.5) | 330 (21.9) | 210 (21.8) | 31 (25.4) | 1913 (24.7) | <0.001 |
| Neurological diseases | 20 (1) |
15 (1) |
5 (0.3) |
10 (0.7) | 6 (0.6) |
2 (1.6) | 58 (0.8) | 0.09 |
| Low hemoglobin concentration | 314 (16.4) | 621 (39.8) | 760 (45.6) | 382 (25.4) | 573 (59.4) | 21 (17.2) | 2671 (34.5) | <0.001 |
| Giving up before donation | 25 (1.3) | 31 (2) |
6 (0.4) |
8 (0.5) |
6 (0.6) |
2 (1.6) | 78 (1) |
<0.001 |
| Operative procedures | 64 (3.3) | 70 (4.5) | 66 (4) |
57 (3.8) | 34 (3.5) | 4 (3.3) | 295 (3.8) | 0.62 |
| Miscellaneous | 531 (27.7) | 499 (32) | 494 (29.7) | 380 (25.3) | 302 (31.3) | 29 (23.8) | 2235 (28.9) | <0.001 |
| Injuries and poisoning | 9 (0.5) |
14 (0.9) | 15 (0.9) | 13 (0.9) | 10 (1) |
2 (1.6) | 63 (0.8) | 0.45 |
| Risky behavior | 3 (0.2) |
5 (0.3) |
5 (0.3) |
1 (0.1) |
0 | 0 | 14 (0.2) | 0.30 |
| Infectious and parasitic diseases | 34 (1.8) | 23 (1.5) | 18 (1.1) | 10 (0.7) | 4 (0.4) |
2 (1.6) | 91 (1.2) | 0.008 |
| DAT positive – temporarily | 0 | 0 | 0 | 1 (0.1) |
1 (0.1) |
0 | 2 (0.03) | 0.47 |
| Faint | 1 (0.1) |
1 (0.1) |
0 | 0 | 0 | 0 | 2 (0.03) | 0.78 |
| Temporarily deferred AST/ALT | 0 | 2 (0.1) |
2 (0.1) |
1 (0.1) |
1 (0.1) |
0 | 6 (0.1) |
0.76 |
| Vaccines | 0 | 6 (0.4) |
1 (0.1) |
3 (0.2) |
0 | 0 | 10 (0.1) | 0.02 |
| Malignancies | 0 | 1 (0.1) |
1 (0.1) |
0 | 0 | 0 | 2 (0.03) |
0.73 |
Fisher exact test; VBD = voluntary blood donor; DAT = direct antiglobulin test; AST = aspartate aminotransferase; ALT = alanine aminotransferase
Table 7. Temporarily deferred female VBDs according to the reason for deferral in the 2014-2018 period.
| Female VBD – temporarily deferred | Number (%) of participants according to age | p* | ||||||
|---|---|---|---|---|---|---|---|---|
| -25 (n=2953) |
26 – 35 (n=1533) |
36 – 45 (n=1403) |
46 – 55 (n=772) |
56 – 65 (n=244) |
≥ 66 (n=16) |
Total (n=6921) |
||
| Alcoholism | 0 | 2 (0.1) |
0 | 1 (0.1) |
0 | 0 | 3 (0.04) |
0.31 |
| Diseases of the endocrinological system | 18 (0.6) |
16 (1) |
21 (1.5) |
17 (2.2) |
4 (1.6) |
0 | 76 (1.1) |
0.003 |
| Diseases of the genitourinary tract | 21 (0.7) |
13 (0.8) |
15 (1.1) |
11 (1.4) |
3 (1.2) |
0 | 63 (0.91) |
0.49 |
| Skin and subcutaneous tissue disorders | 19 (0.6) |
3 (0.2) |
5 (0.4) |
7 (0.9) |
1 (0.4) |
0 | 35 (0.51) |
0.20 |
| Diseases of the digestive system | 15 (0.5) |
21 (1.4) |
14 (1) |
19 (2.5) |
6 (2.5) |
0 | 75 (1.08) |
<0.001 |
| Respiratory diseases | 58 (2) |
28 (1.8) |
8 (0.6) |
7 (0.9) |
1 (0.4) |
0 | 102 (1.47) | 0.003 |
| Cardiovascular diseases | 28 (0.9) |
3 (0.2) |
11 (0.8) |
14 (1.8) |
8 (3.3) |
0 | 64 (0.92) |
<0.001 |
| Nerve and mental diseases | 8 (0.3) |
5 (0.3) |
13 (0.9) |
12 (1.6) |
5 (2) |
0 | 43 (0.62) |
<0.001 |
| Blood pressure | 1121 (38) | 394 (25.7) | 259 (18.5) | 123 (15.9) | 51 (20.9) | 0 | 1948 (28.15) | <0.001 |
| Period, pregnancy, abortion, breastfeeding | 74 (2.5) |
70 (4.6) |
31 (2.2) |
3 (0.4) |
0 | 0 | 178 (2.57) | <0.001 |
| Faint before blood donation | 1 (0.03) |
0 | 0 | 0 | 0 | 0 | 1 (0.01) |
0.93 |
| Low hemoglobin concentrations | 1079 (36.5) | 707 (46.1) | 816 (58.2) | 403 (52.2) | 91 (37.3) | 6 (37.5) | 3102 (44.82) | <0.001 |
| Giving up before donation | 17 (0.6) |
9 (0.6) |
5 (0.4) |
1 (0.1) |
2 (0.8) |
0 | 34 (0.49) |
<0.001 |
| Operative procedures | 30 (1) |
18 (1.2) |
13 (0.9) |
16 (2.1) |
7 (2.9) |
1 (6.3) |
85 (1.23) |
0.009 |
| Miscellaneous | 426 (14.4) | 217 (14.2) | 178 (12.7) | 126 (16.3) | 63 (25.8) | 5 (31.3) | 1015 (14.67) | <0.001 |
| Infectious and parasitic diseases | 22 (0.7) |
7 (0.5) |
4 (0.3) |
2 (0.3) |
2 (0.8) |
0 | 37 (0.53) |
0.32 |
| Malaria testing | 5 (0.2) |
13 (0.8) |
3 (0.2) |
4 (0.5) |
0 | 0 | 25 (0.36) |
0.009 |
| Malignancies | 0 | 0 | 1 (0.1) |
1 (0.1) |
0 | 0 | 2 (0.03) |
0.42 |
| Neurological diseases | 15 (0.5) |
4 (0.3) |
5 (0.4) |
2 (0.3) |
0 | 0 | 26 (0.38) |
0.67 |
| Temporarily deferred AST/ALT | 1 (0.03) |
0 | 0 | 0 | 0 | 0 | 1 (0.01) |
0.93 |
| Risky behaviour | 1 (0.03) |
0 | 0 | 0 | 0 | 0 | 1 (0.01) |
0.93 |
| Vaccines | 1 (0.03) |
0 | 0 | 1 (0.1) |
0 | 0 | 2 (0.03) |
0.60 |
| Injuries and poisoning | 4 (0.1) |
2 (0.1) |
1 (0.1) |
2 (0.3) |
1 (0.4) |
0 | 10 (0.14) |
0.78 |
Fisher exact test; VBD = voluntary blood donor; DAT = direct antiglobulin test; AST = aspartate aminotransferase; ALT = alanine aminotransferase
There were a significantly higher mean hemoglobin concentration in male donors accepted for blood donation than in female in each study year (Student’s t-test, p<0.001) (Table 8).
Table 8. Differences in hemoglobin concentration of accepted donors according to gender by years.
| Year | Hemoglobin (g), arithmetic mean (standard deviation) |
Difference | 95% confidence interval | p* | |
|---|---|---|---|---|---|
| VBD male | VBD female | ||||
| 2014 | 152.49 (10.84) | 137.59 (9.1) | 14.9 | 14.6-15.2 | <0.001 |
| 2015 | 149.56 (8.36) | 136.06 (7.55) | 13.5 | 13.3-13.7 | <0.001 |
| 2016 | 153.81 (10.99) | 138.24 (9.6) | 15.6 | 15.3-15.9 | <0.001 |
| 2017 | 153.34 (10.84) | 137.25 (9.09) | 16.1 | 15.8-16.4 | <0.001 |
| 2018 | 154.82 (10.79) | 137.84 (9.18) | 16.9 | 16.7-17.3 | <0.001 |
VBD = voluntary blood donor
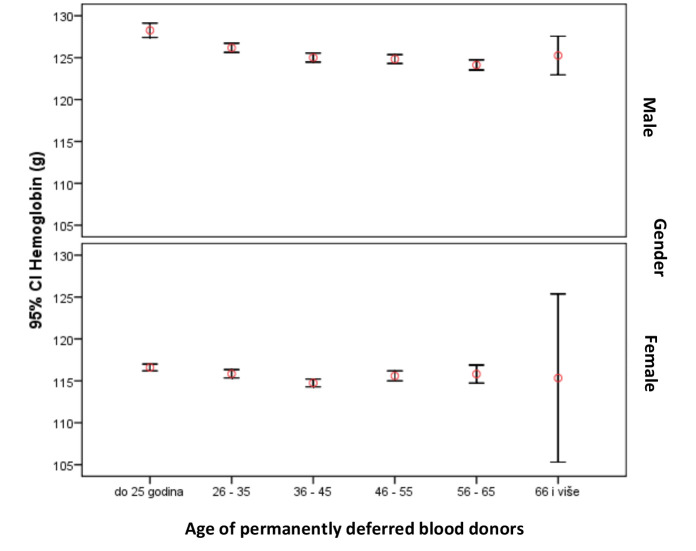
Similarly, hemoglobin concentration in temporarily deferred female donors due to low hemoglobin levels was significantly lower as compared with male donors each year (Student’s t-test, p<0.001) (Table 9, Fig. 1).
Table 9. Differences in hemoglobin concentration in temporarily deferred VBDs according to gender by years.
| Year | Hemoglobin (g), arithmetic mean (standard deviation) |
Difference | 95% confidence interval | p* | |
|---|---|---|---|---|---|
| VBD male | VBD female | ||||
| 2014 | 126.02 (7.74) | 116.22 (6.39) | 9.8 | 8.9-10.6 | <0.001 |
| 2015 | 126.15 (8.86) | 115.51 (7.72) | 10.6 | 9.3-11.9 | <0.001 |
| 2016 | 124.98 (7.34) | 115.41 (7.04) | 9.6 | 8.9-10.2 | <0.001 |
| 2017 | 125.07 (6.47) | 115.42 (6.35) | 9.7 | 8.9-10.3 | <0.001 |
| 2018 | 125.22 (7.01) | 116.5 (6.06) | 8.7 | 7.9-9.5 | <0.001 |
*Student’s t-test; VBD = voluntary blood donor
Fig. 1.
Hemoglobin concentration in permanently deferred voluntary blood donors according to age and gender.
Hemoglobin concentrations were higher in male VBDs regardless of whether they were accepted or temporarily deferred donors (Tables 10 and 11). Repeated measurements in younger male donors temporarily deferred due to low hemoglobin levels showed significantly higher hemoglobin concentrations compared to older age groups (ANOVA, Bonferroni post-hoc test, p<0.001). Also, there were significant age differences in hemoglobin concentrations among temporarily deferred female donors (ANOVA, p<0.001).
Table 10. Hemoglobin concentration of temporarily deferred male VBDs by age.
| Male VBD age group (yrs) | n | Arithmetic mean (standard deviation) |
(F, df) | p* |
|---|---|---|---|---|
| ≤25 | 295 | 128.26 (7.43) | (15.5; 5) | <0.001 |
| 26-35 | 610 | 126.17 (6.79) | ||
| 36-45 | 748 | 125.01 (7.5) | ||
| 46-55 | 697 | 124.83 (7.08) | ||
| 56-65 | 595 | 124.13 (7.58) | ||
| ≥66 | 32 | 125.25 (6.4) |
*ANOVA (post-hoc Bonferroni); VBD = voluntary blood donor
Table 11. Hemoglobin concentration in temporarily deferred female VBDs according to age.
| Female VBD age group (yrs) | n | Arithmetic mean (standard deviation) |
(F; df) | p* |
|---|---|---|---|---|
| ≤25 | 1053 | 116.59 (6.73) | (7.1;5) | <0.001 |
| 26-35 | 716 | 115.84 (6.75) | ||
| 36-45 | 793 | 114.75 (6.73) | ||
| 46-55 | 440 | 115.59 (6.35) | ||
| 56-65 | 99 | 115.81 (5.41) | ||
| ≥66 | 3 | 115.33 (4.04) |
*ANOVA (post-hoc Bonferroni); VBD = voluntary blood donor
Discussion
Determination of hemoglobin concentration is one of the factors in the process of selecting a donor and an important prerequisite for protecting donor health, while ensuring a quality blood product with sufficient hemoglobin content in the red blood cell concentrate. According to the European Union Recommendations, the concentration of hemoglobin for blood donation must be at least 125 g/L in women and at least 135 g/L in men. After donating 450 mL of blood, male donors lose 242±17 mg and females 217±11 mg of iron (15).
Data on donor distribution by gender in our study showed a significantly higher proportion of males (66.91%) as compared to data from Western European countries (16, 17). The proportion of female donors in our study of 33.09% is similar to data from Italy and Greece where this share is around 30%. Conversely, in most EU countries, there is an equal donor gender distribution (16). In some EU countries, the frequency of women donating blood is higher, such as in Spain 46%, Portugal 43%, Belgium 45%, the Netherlands 50%, Denmark 50%, France 50%, the United Kingdom 53%, and Finland 55%. We observed a lower number of donors in 2016 (15,778) as compared with 2015, 2017 and 2018. This can be explained by the increased migration of the younger and working population to Western European countries (17). The lower contribution of female donors in our study than in Western European countries can be explained by insufficient promotion of blood donation to target groups, since according to Newman, women are more willing to donate blood than men (18).
Most of the donors in our study were aged between 26 to 55 years. Male donors were evenly distributed over this age range, while the number of female donors decreased with age. A higher proportion of female (21.4%) than male (7.7%) donors was recorded in the ≤25 age group, which is in line with the results of similar studies (18-20). The age and gender distribution of donors in our study is comparable to the results from the United Kingdom (21). Similar to our study, the United Kingdom study on more than 1.8 million whole blood donations found a high frequency of female donors under the age of 25 and gradual decline over years. This can be explained by the fact that female donors in the reproductive period have long breaks in donating blood due to pregnancy and breastfeeding, which could be a possible reason for stopping donating blood (19-23). Given that women generally have a lower body mass than males, they always give a higher portion of blood volume than men when the uniform volume of whole blood is collected. Therefore, they have more frequent adverse reactions during and after donation, which is recognized as a reason for stopping regular blood donation (23).
In our study, female donors accounted for one-third of total VBD population, but for only one-sixth of total blood donations. This was due to a greater number of donor deferrals, but also longer intervals between regular donations prescribed for women. A study conducted in the United States in 2015 showed that deferrals may cause loss of potential donors because of disappointment with the inability to donate blood. Such a phenomenon is particularly pronounced in female donors deferred due to low hemoglobin concentration during menstruation or pregnancy, which can cause iron deficiency (24). Therefore, more frequent temporary deferral of female donors may lead to their loss from the donor pool.
In our study, the overall deferral rate was 11.46%, which is comparable to deferral rates of 11.5% and 11.6% in India (25, 26) or 8.7% in Nigeria (27), as well as 14% in Cyprus (28), 6% in Luxembourg (28) and 9.49% in Romania (28). The rate of permanently deferred donors in our study was 1.7%. This percentage is similar to the percentage in EU countries, e.g., Luxembourg 0.63% (29) but lower than in other non-European countries, e.g., Iran 11.4% (29) and as high as 37.1% in India (25). This indicates high awareness among EU donors regarding donor selection criteria.
In our study cohort, deferral rate due to low hemoglobin concentration was 4.00%. Data for 2014 show a 5.64% deferral rate due to hemoglobin concentration at the national level, which is comparable to 6.5% reported from India (24), whereas in the EU, the rate ranged from 0.11% to 7% (26).
Of all deferrals in our study, 36.3% were due to low hemoglobin concentration, which was the most common reason for temporary deferral. These results coincide with data from Slovenia (30%) and Romania (30.6%) (28), and even higher from India (55.8%) (26). The percentage of temporarily deferred donors due to low hemoglobin concentration was 44.2% among females and 34.5% among males. These differences between genders were statistically nonsignificant, unlike some other studies where this percentage was 77.9% of female donors versus 37.0% of male donors (26).
In regard to gender, in our region, the share of deferral was 12.86% among female donors and 2.22% among male donors, which is comparable to data for Croatia from 2014, where the share of deferral was 15.9% among female donors and 3.24% among male donors (27).
According to EU Directives 2004/33/EC and EDQM guidelines, hemoglobin concentration for donors should be >135 g/L in men and >125 g/L in women, whereas in other countries, these values differ by 5-10 g/L5. In the United States and Europe, it has been found that 10%-20% of women normally have hemoglobin concentration in the range of 120-125 g/L and, although not anemic, do not meet the criteria for blood donation. The same trend is observed in men, with the values of 125-136 g/L5.
In our study, hemoglobin concentrations in female donors were significantly lower as compared to male donors in both accepted donors and temporarily deferred ones (Student ‘s t-test, p<0.001). Female donors generally have lower hemoglobin concentrations, which is the reason for their more frequent deferral, and thus withdrawal from regular blood donation (12). Temporarily deferred male donors in our study had hemoglobin values from 124.98 g/L to 126.15 g/L. Such levels of hemoglobin would make them eligible blood donors in North American countries. However, studies have shown that these hemoglobin concentrations indicate anemia in men (13, 33). Hemoglobin concentrations in temporarily deferred female donors from our cohort ranged from 115.41 g/L to 116.5 g/L, which indicates anemia according to the currently valid World Health Organization criteria.
Younger male VBDs had significantly higher hemoglobin concentrations as compared to all other age groups (+3 g/L), which can be explained by the fact that hemoglobin levels fall with age in men, who are therefore more often deferred due to low hemoglobin concentration (30-36). These values also coincide with data reported by Beutler and Waalen (+1 g/L), although in their analysis, this difference was not statistically significant (37).
Our study showed that the most significant proportion of blood donor deferrals was temporary deferral due to decreased or low hemoglobin concentration.
Hemoglobin concentrations in deferred and accepted donors were gender and age dependent. Thus, we believe that donor age and gender should be evaluated regularly in order to determine real characteristics of blood donors related to temporary deferral due to reduced hemoglobin concentration. Iron and ferritin levels should be checked in blood donors who are frequently deferred due to low hemoglobin concentration, particularly in frequent regular donors and donors who alternately donate cell components on cell separators in combination with a 450 mL whole blood donation.
This study showed that the female part of the population certainly represented a potential reservoir for increasing the total number of VBDs.
The results of this retrospective study indicated that donors in this region should be screened for serum iron and ferritin levels, in particular frequent regular donors. In order to preserve donor health and regular blood supply, educational material on diet and iron supplements should be developed, which in turn will help prevent reduction in the number of temporarily deferred VBDs due to low hemoglobin concentration.
References
- 1.Council of Europe. Guide to the preparation, use and quality assurance of blood components, 18th Edition, European Directorate for the Quality of Medicines, (EDQM) & HealthCare, Strasbourg, France, 2015. [Google Scholar]
- 2.Karp JK, King KE. International variation in volunteer whole blood donor eligibility criteria. Transfusion. 2010;50(2):507–13. 10.1111/j.1537-2995.2009.02392.x [DOI] [PubMed] [Google Scholar]
- 3.Samardžija M, Drenjančević D, Miletić M, Slavulj B, Jukić I, Zibar L, et al. The impact of positive anti-HBC marker on permanent deferral of voluntary blood donors in Eastern Croatia and estimation of occult hepatitis B virus infection rate. Acta Clin Croat. 2020;59(1):126–34. 10.20471/acc.2020.59.01.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Magnussen K, Hasselbalch HC, Ullum H, Bjerrum OW. Characterization of blood donors with high haemoglobin concentration. Vox Sang. 2013. February;104(2):110–4. [x.] 10.1111/j.1423-0410.2012.01644.x [DOI] [PubMed] [Google Scholar]
- 5.Eder A, Goldman M, Rossmann S, Waxman D, Bianco C. Selection criteria to protect the blood donor in North America and Europe: past (dogma), present (evidence), and future (hemovigilance). Transfus Med Rev. 2009;23(3):205–20. 10.1016/j.tmrv.2009.03.003 [DOI] [PubMed] [Google Scholar]
- 6.Starčević A, Mavrinac M, Katalinić N, Balen S. Are Croatian blood donors obese? Acta Clin Croat. 2020;59(3):455–62. 10.20471/acc.2020.59.03.09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Magnussen K, Ladelund S. Handling low hemoglobin and iron deficiency in a blood donor population: 2 years’ experience. Transfusion. 2015;55:2473–8. 10.1111/trf.13152 [DOI] [PubMed] [Google Scholar]
- 8.Delaney M, Schellhase KG, Young S, Geiger S, Fink A, Mast AE. Blood center practice and education for blood donors with anemia. Transfusion. 2011;51:929–36. 10.1111/j.1537-2995.2010.02919.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mast AE, Bialkowski W, Bryant BJ, Wright DJ, Birch R, Kiss JE, et al. A randomized, blinded, placebo-controlled trial of education and iron supplementation for mitigation of iron deficiency in regular blood donors. Transfusion. 2016. June;56(6 Pt 2):1588–97. 10.1111/trf.13469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kasraian L, Negarestani N. Rates and reasons for blood donor deferral, Shiraz, Iran. A retrospective study. Sao Paulo Med J. 2015;133(1):36–42. 10.1590/1516-3180-2013-7110002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Di Angelantonio E, Thompson SG, Kaptoge S, Moore C, Walker M, Armitage J, et al. INTERVAL Trial Group . Efficiency and safety of varying the frequency of whole blood donation (INTERVAL): a randomised trial of 45 000 donors. Lancet. 2017. November 25;390(10110):2360–71. 10.1016/S0140-6736(17)31928-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goldman M, Uzicanin S, Osmond L, Scalia V, O’Brien SF. A large national study of ferritin testing in Canadian blood donors. Transfusion. 2017. March;57(3):564–70. 10.1111/trf.13956 [DOI] [PubMed] [Google Scholar]
- 13.Lobier M, Castrén J, Niittymäki P, Palokangas E, Partanen J, Arvas M. The effect of donation activity dwarfs the effect of lifestyle, diet and targeted iron supplementation on blood donor iron stores. PLoS One. 2019. August 13;14(8):e0220862. 10.1371/journal.pone.0220862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Avcioglu G, Nural C, Yilmaz FM, Baran P, Erel Ö, Yilmaz G. Comparison of noninvasive and invasive point-of-care testing methods with reference method for hemoglobin measurement. J Clin Lab Anal. 2018;32(3):e22309. 10.1002/jcla.22309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Simon TL. Iron, iron everywhere but not enough to donate. Transfusion. 2002;42(6):664. 10.1046/j.1537-2995.2002.00121.x [DOI] [PubMed] [Google Scholar]
- 16.Bani M, Giussani B. Gender differences in giving blood: a review of the literature. Blood Transfus. 2010;8(4):278–87. 10.2450/2010.0156-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Magnussen K, Bork N, Asmussen L. The effect of a standardized protocol for iron supplementation to blood donors low in hemoglobin concentration. Transfusion. 2008;48(4):749–54. 10.1111/j.1537-2995.2007.01601.x [DOI] [PubMed] [Google Scholar]
- 18.Newman BH. Adjusting our management of female blood donors: the key to an adequate blood supply. Transfusion. 2004;44:591–6. 10.1111/j.0041-1132.2004.04014.x [DOI] [PubMed] [Google Scholar]
- 19.Misje AH, Bosnes V, Heier HE. Gender differences in presentation rates, deferrals and return behaviour among Norwegian blood donors. Vox Sang. 2010;98:e241–8. 10.1111/j.1423-0410.2009.01267.x [DOI] [PubMed] [Google Scholar]
- 20.Schreiber GB, Sharma UK, Wright DJ, et al. Retrovirus Epidemiology Donor Study . First year donation patterns predict long term commitment for first time donors. Vox Sang. 2005;88:114–21. 10.1111/j.1423-0410.2005.00593.x [DOI] [PubMed] [Google Scholar]
- 21.Lattimore S, Wickenden C, Brailsford RS. Blood donors in England and North Wales: demography and patterns of donation. Transfusion. 2015;55:91–9. 10.1111/trf.12835 [DOI] [PubMed] [Google Scholar]
- 22.Piersma TW, Merz EM, Bekkers R, de Kort W, Andersen S, Hjalgrim H, et al. Life events and donor lapse among blood donors in Denmark. Vox Sang. 2019. November;114(8):795–807. 10.1111/vox.12842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Prados Madrona D, Fernández Herrera MD, Jiménez DP, Giraldo SG, Robles Campos R. Women as whole blood donors offers, donations and deferrals in the province of Huelva, south-western Spain. Blood Transfus. 2014;12 Suppl 1:s11–20. 10.2450/2012.0117-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mast AE, Schlumpf KS, Wright DJ, Custer B, Spencer B, Murphy EL, et al. Demographic correlates of low hemoglobin deferral among prospective whole blood donors. Transfusion. 2010;50(8):1794–802. 10.1111/j.1537-2995.2010.02649.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shrivastava M, Shah N, Navaid S, Agarwal K, Sharma G. Blood donor selection and deferral pattern as an important tool for blood safety in a tertiary care hospital. Asian J Transfus Sci. 2016;10:122–6. 10.4103/0973-6247.187938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Agnihotri N. Whole blood donor deferral analysis at a center in Western India. Asian J Transfus Sci. 2010. July 1;4(2):116–22. 10.4103/0973-6247.67035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Birjandi F, Gharehbaghian A, Delavari A, Rezaie N, Maghsudlu M. Blood donor deferral pattern in Iran. Arch Iran Med. 2013. November;16(11):657–60. [PubMed] [Google Scholar]
- 28.Okoroiwu HU, Enosakhare AA. Blood donor’s deferral prevalence and causes in a tertiary health care hospital, southern Nigeria. BMC Health Serv Res. 2019. July 22;19(1):510. 10.1186/s12913-019-4352-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vuk T, Magnussen K, De Kort W, Follea G, Liumbruno G, Schennach H, et al. International forum: an investigation ot iron status in blood donors. Blood Transfus. 2017. January;15(1):20–41. 10.2450/2016.0101-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.World Health Organisation. Worldwide Prevalence of Anaemia 1993-2005. Geneva: WHO, 2008. [Google Scholar]
- 31.Cook JD, Flowers CH, Skikne BS. The quantitative assessment of body iron. Blood. 2003;101:3359–64. 10.1182/blood-2002-10-3071 [DOI] [PubMed] [Google Scholar]
- 32.Blanc B, Finch CA, Hallberg L, et al. Nutritional anaemias. Report of a WHO Scientific Group. WHO Tech Rep Ser. 1968;405:1–40. [PubMed] [Google Scholar]
- 33.Mast AE. Low hemoglobin deferral in blood donors. Transfus Med Rev. 2014;28:18–22. 10.1016/j.tmrv.2013.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pan WH, Habicht JP. The non-iron-deficiency-related difference in hemoglobin concentration distribution between blacks and whites and between men and women. Am J Epidemiol. 1991. December 15;134(12):1410–6. 10.1093/oxfordjournals.aje.a116046 [DOI] [PubMed] [Google Scholar]
- 35.Johnson-Spear MA, Yip R. Haemoglobin difference between black and white women with comparable iron status: justification for race-specific anaemia criteria. Am J Clin Nutr. 1994;60:117–21. 10.1093/ajcn/60.1.117 [DOI] [PubMed] [Google Scholar]
- 36.Spekman MLC, Tilburg TG, Merz EM. Do deferred donors continue their donations? A large‐scale register study on whole blood donor return in the Netherlands. Transfusion. 2019;59:3657–65. 10.1111/trf.15551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Beutler E, Waalen J. The definition of anemia: what is the lower limit of normal of the blood hemoglobin concentration? Blood. 2006;107:1747–50. 10.1182/blood-2005-07-3046 [DOI] [PMC free article] [PubMed] [Google Scholar]