Abstract
This paper examines how health care providers respond to a reference pricing insurance program that increases consumer cost sharing when consumers choose high-priced surgical providers. We use geographic variation in the population covered by the program to estimate supply-side responses. We find limited evidence of market segmentation and price reductions for providers with baseline prices above the reference price. Finally, approximately 75% of the reduction in provider prices is in the form of a positive externality that benefits a population not subject to the program.
Keywords: I11, I13, L11, Reference pricing, Provider prices, Health care markets
1. Introduction
As a means of restraining health care spending, many employers and insurers have introduced substantial changes to their insurance benefit designs. Many recent benefit designs use patient cost sharing or reduce the number of covered providers to incentivize patients to receive care from less expensive providers. While several studies document consumer responses to these benefit design changes (Parente et al., 2004; Beeuwkes Buntin et al., 2011; Buntin et al., 2006; Sood et al., 2013; Haviland et al., 2015; Gruber and McKnight, 2016; Brot-Goldberg et al., 2017), the supply-side responses are not well understood. This paper measures how firms, in this case outpatient surgery providers, respond to a particular insurance policy implemented by one of the largest purchasers of health insurance coverage in the United States, the California Public Employees’ Retirement System (CalPERS).
In January 2012, CalPERS implemented a reference pricing program for three common outpatient surgical services – cataract surgery, colonoscopy, and joint arthroscopy. The program uses a non-linear cost-sharing schedule to incentivize consumers to receive care from less expensive providers. Under the program, which was implemented for one of CalPERS three insurance options, patients who receive care at freestanding Ambulatory Surgical Centers (ASCs), which tend to have lower prices, face no change in cost sharing. However, patients who receive care at Hospital Outpatient Departments (HOPDs), which typically have higher prices, are responsible for the entire marginal cost of care above a pre-specified price threshold. Previous work shows that for each of the three surgical services, the program leads to large shifts in patient demand from expensive to less expensive providers (Robinson et al., 2015a,b,c). This paper tests whether providers respond to these changes in consumer demand by lowering prices.
To test provider responses to the program, we use detailed medical claims data covering 2009–2013 from a large insurer, Anthem Blue Cross, that provides benefits to both CalPERS and non-CalPERS consumers. Key to our identification strategy is the fact that although networks and negotiated prices at a given provider are the same for both populations, only CalPERS members are subject to the reference pricing program.1 Thus, the non-CalPERS Anthem population serves as a natural control group for the CalPERS population. In addition, due to the structure of CalPERS, there is substantial variation in the concentration of CalPERS enrollees across California. A given provider’s exposure to the reference pricing program depends on the concentration of CalPERS enrollees who are enrolled in the Anthem PPO option in that market. Our identification strategy relies on the much greater exposure that providers in high-exposure regions to the program have than providers in low-exposure regions.
Somewhat counterintuitively, we find modest price reductions for ASC providers, which is consistent with the reference pricing program increasing price competition among ASCs. We estimate that a 10% increase in exposure to the CalPERS program leads to approximately 0.6% and 0.4% reductions in ASC prices for cataract surgeries and colonoscopies, respectively. For HOPDs, we do not find a mean reduction in prices. However, we do find that a 10% increase in exposure to the program leads to a 1.7% reduction in colonoscopy prices for HOPDs with baseline prices above the reference price. Because prices are set at the insurer-level rather than the employer level, approximately 75% of the reduction in provider prices benefits the non-CalPERS population that is not subject to the program.
One concern with the reference pricing program is the potential for unintended provider responses. For example, providers that lower prices for the three surgical services of interest may correspondingly increase prices in other areas. We examine several forms of cost-shifting and alternative provider responses. We do not find evidence that providers price discriminate between the CalPERS and non-CalPERS populations, cost-shift by raising prices for other services, or change prices for other insurers. We also do not find evidence of changes in clinical quality.
This paper fits into a broader literature on how health care firms respond to changes in insurance coverage for consumers. To our knowledge, this paper is the first to demonstrate that health care providers change their negotiated prices in response to increases in consumer cost sharing. Much of the existing literature focuses on firm responses along non-price dimensions. For example, Finkelstein (2007) finds that the expansion of insurance coverage through the introduction of Medicare increased hospital entry and adaptation of new medical technologies. Likewise, Blume-Kohout and Sood (2013) find that due to low reimbursement rates, the introduction of Medicare Part D increased investments in medications for the elderly, while Freedman et al. (2015) find that the expansion of Medicaid in the 1980s and 1990s reduced neonatal care technology adoption. Similarly, both Dafny (2005) and Clemens and Gottlieb (2014) show that hospitals and physicians strategically responded to Medicare payment changes by increasing volume for services that have higher reimbursement rates. On the other hand, Duggan and Morton (2010) finds that the expansion in prescription drug coverage through Medicare Part D allowed insurers to negotiate lower prices by using tiered benefit designs. Similar to the Part D experience, the setting we study uses differential cost sharing to shift consumer demand to less-expensive providers.
The most similar paper to this study examines the effect of the CalPERS’ reference pricing program for knee and hip replacements on the two components that make up the total price-consumer and insurer payments (Brown and Robinson, 2016). Following the program’s implementation, insurer payments to both high and low-price hospitals decreased. This paper follows a similar approach but focuses on how the variation in provider exposure to the CalPERS program influences provider responses. Also, unlike Brown and Robinson (2016), this paper focuses specifically on how reference pricing changes the negotiated prices between providers and insurers rather than how the total price is distributed between consumers and insurers.
We start by providing a description of the CalPERS reference pricing program and the institutional setting. Section 3 describes the data. Section 4 examines changes in provider prices in response to the program. Section 5 considers alternative explanations for the provider price changes and Section 6 concludes.
2. Institutional background
CalPERS provides health insurance coverage to 1.4 million California state, municipal, and county employees and their dependents, making it the third largest purchaser of health services in the United States. Nearly all State of California employees and their dependents receive health insurance through CalPERS. In addition, California counties and municipalities throughout the state can choose to provide coverage to their employees and their dependents through CalPERS or to provide their own coverage. CalPERS health insurance enrollment is largely split between three plans; a Kaiser Permanente fully integrated plan, a health maintenance organization (HMO) administered by Blue Shield of California, and a preferred provider organization (PPO) plan administered by Anthem Blue Cross.
CalPERS added reference pricing to its Anthem PPO insurance plan in 2011 for knee and hip replacement surgery and expanded it to colonoscopy, cataract surgery, and joint arthroscopy in 2012.2 Reference pricing was not implemented for the Kaiser or Blue Shield HMO plans. The decision to implement reference pricing was motivated by the substantial variation in provider prices that was not accompanied by discernible differences in procedural quality. Moreover, these services are “shoppable,” non-emergent services and are the among the most routine outpatient surgical services. Patients typically have several weeks or months to make care decisions and have many provider options. Compared to other surgical services, there is a much lower quality component and risks of surgical complications are low (Robinson et al., 2015a,b; Naseri et al., 2016).
The price variation that motivated the implementation of the reference pricing program is shown in Fig. 1, which plots the distribution of provider prices among the CalPERS population for hospital outpatient departments (HOPDs) and ambulatory surgical centers (ASCs) in 2011, the year before implementation. For colonoscopies, the 25th percentile price for HOPD providers is $1666 while the 75th percentile price is $3110. The range is much narrower for ASCs, from $638 to $1457, respectively. The corresponding arthroscopy 25th and 75th price percentiles range between $2270 to $4935 for ASCs and $4081 to $9039 for HOPDs. For cataract surgery, the respective price ranges are $1102 and $2191 for ASCs and $5605 and $8261 for HOPDs.
Fig. 1.
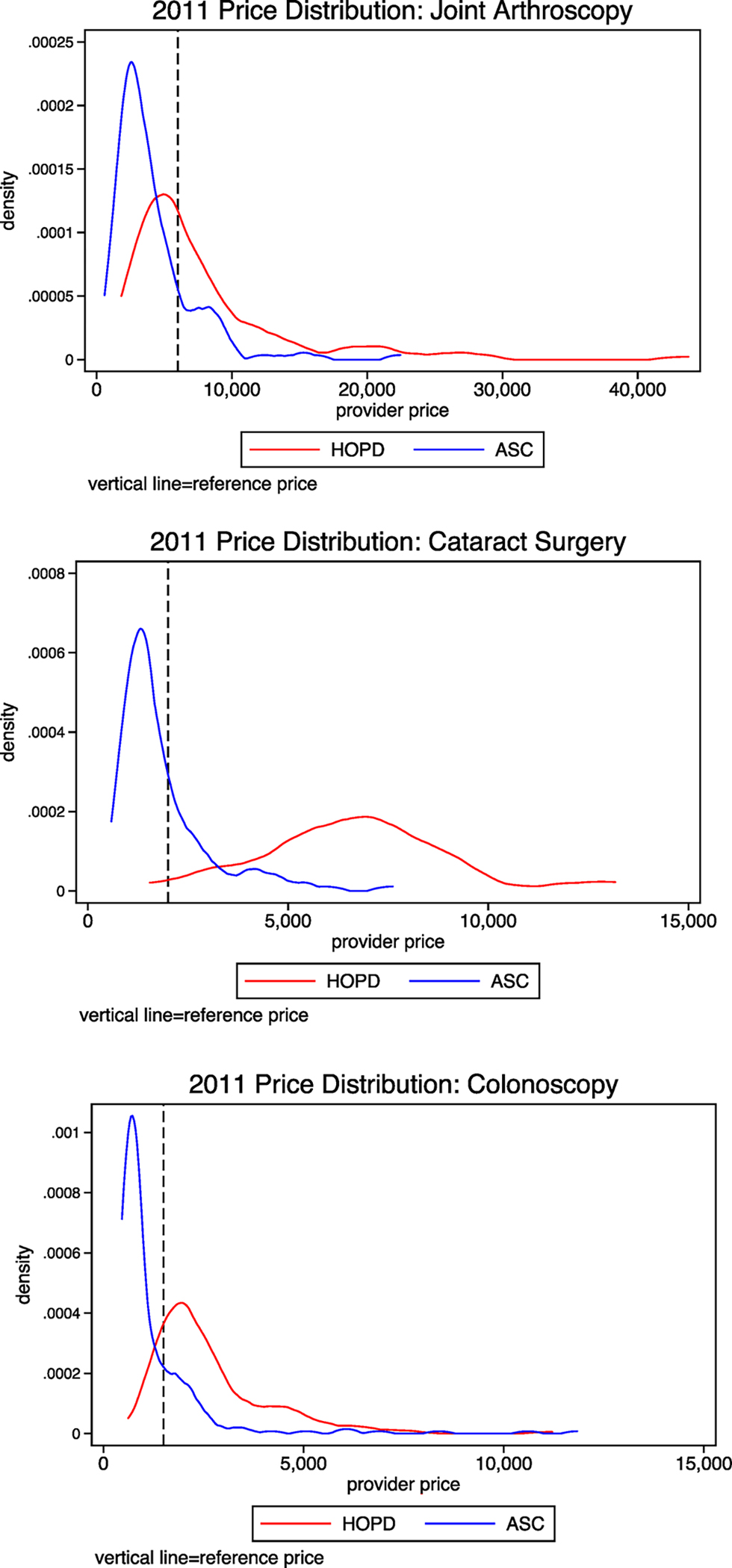
Distribution of provider prices. Each figure presents the distribution of each provider’s negotiated prices for the Anthem PPO in 2011. The blue line shows the distribution for services received at an ambulatory surgical center (ASC) and the red line shows prices for services received at an hospital outpatient department (HOPD).
Unlike HOPDs, ASCs are freestanding facilities that do not deliver emergency care or accept uninsured patients. As a result, they typically have lower fixed costs than HOPDs. The lower cost-structures are reflected in lower reimbursement rates from Medicare and most commercial insurers. ASCs also typically specialize in a few surgical procedures and can thereby operate more efficiently (Courtemanche and Plotzke, 2010; Carey et al., 2011). ASCs are often physician owned and operated. Due to their “focused factory” nature, previous studies have found that ASCs deliver slightly higher care quality than HOPDs (Casalino et al., 2003; Barro et al., 2006). Importantly for this setting, ASCs typically offer fewer services than hospitals and HOPDs. Thus, for the services that they do offer, ASCs may be more responsive to changes in patient incentives than HOPDs.
In light of this variation in prices and the fact that CalPERS was not able to link prices to observable differences in clinical outcomes or quality of care, CalPERS established reimbursement limits of $1500 for colonoscopy, $2000 for cataract surgery, and $6000 for arthroscopy services received at a HOPD. This reference price includes the entire cost of the procedure and includes any ancillary services related to the primary surgical procedure (e.g. laboratory tests and anesthesia services). The reference price also only applies to the procedure’s facility fee.3 CalPERS enrollees who receive care at a HOPD priced at or under these thresholds are responsible for standard cost-sharing payments (e.g. deductible payments, copayments, and coinsurance), but patients who receive care from HOPDs priced above the reference price are responsible for standard cost sharing for the portion up to the reference price plus the entirety of the difference in the facility price and the reference price.4 Moreover, the cost-sharing portion that covers the difference between the provider price and the reference price does not apply to out-of-pocket maximums or count towards deductible coverage.5 CalPERS enrollees receiving care at any ASC, regardless of the price, are only responsible for standard cost sharing. Nearly all ASC prices fall below the reference price and so this design makes the program easier to understand for enrollees without substantially increasing costs.
Fig. 2 uses colonoscopies as an example to illustrate how reference pricing changes consumer cost sharing. The solid line represents the case of no insurance coverage where patients are responsible for the full marginal cost of care. The dotted line represents the pre-reference pricing price schedule (“traditional coverage”). CalPERS PPO patients typically have a $500 deductible. We present the price schedule under the full deductible for simplicity. In this scenario, patients are responsible for the full marginal price up to the deductible but then only responsible for a 20% coinsurance. Under the third scenario, the dashed line, patients are responsible for the full marginal price up to $500 and then pay the 20% coinsurance until $1500. Above the $1500 reference price, they face the full marginal cost of care.
Fig. 2.
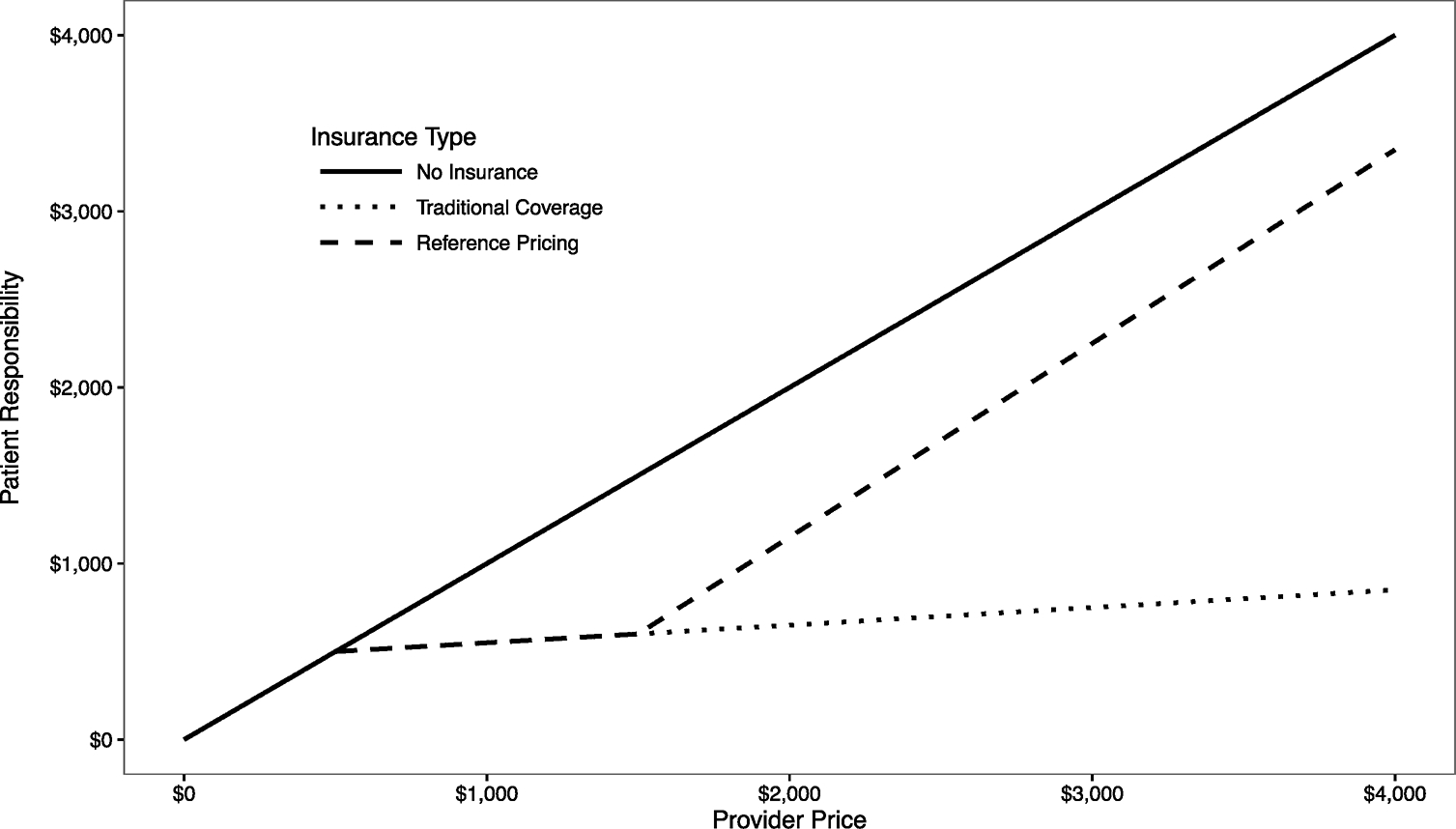
Reference pricing illustration.
Of course, providers will only change prices if consumers respond to the program. Evidence from several studies shows that the CalPERS program shifts patient volume from expensive to low-price providers. For joint arthroscopy, the reference pricing leads to a 14.3 percentage point shift in consumer volume from HOPDs to ASCs, a 17.6% reduction in the average cost per procedure, and an estimated savings of $2.3 million (Robinson et al., 2015a). The cataract program shifts demand by 8.6 percentage points and decreases average procedure costs by 18%, which leads to a $1.3 million reduction in medical spending. (Robinson et al., 2015c). Likewise, the colonoscopy reference pricing program leads to a 17.6 percentage point increase in ASC volume, a 21.0% reduction in spending, and a $7.0 million savings (Robinson et al., 2015b; Whaley et al., 2017; Aouad et al., 2018a; Aouad et al., 2018b).6
Consumers are exempted from the program if a doctor recommends care at a specific facility or if there is not an ASC within 30 miles of the patient’s home address. During the study period, patients had access to a list of ASCs but did not have information about specific provider prices. Several controls were put in place by Anthem to ensure that non-exempted CalPERS enrollees were aware of the program and did not inadvertently receive care from a HOPD. The reference pricing program builds upon a previous prior-authorization program. During the authorization, providers are informed if reference pricing applies to the patient’s service. In addition, the authorization triggers a telephone call to the patient. The call lists providers near the patient’s home zip code and whether the reference price applies to the provider. Many physicians perform surgical procedures at both ASCs and HOPDs. If a patient schedules a procedure at a HOPD with a physician who also operates at an ASC, Anthem automatically rescheduled the service to the ASC. Compliant with California Department of Insurance regulations, Anthem notified all in-network providers about the program 120 days before the January 2012 implementation.
3. Data
3.1. Medical claims
Our primary data source consists of medical claims data from two California populations that receive insurance coverage through an Anthem Blue Cross PPO. The first population consists of CalPERS enrollees, who are subject to reference pricing starting in 2012. The claims data are used to measure provider prices. The second population consists of all non-CalPERS Anthem PPO enrollees and serves as our control population. From the claims data and for both populations, we identify all knee and shoulder arthroscopy (Current Procedural Terminology (CPT) codes 23044–29999), colonoscopy (CPT codes 44389–45392), and cataract surgery (CPT codes 66982–66984) procedures.7 For both samples, we restrict the sample to procedures received at in-network providers. Within the three procedure groupings, there are several specific procedures but the reference price is the same within each procedure type. For example, cataract surgeries consist of both standard cataract surgery (CPT code 66984) and complex, non-routine cataract surgery (CPT code 66982) but both have the same reference price of $2000. For each service, we identify the primary CPT code for the procedure. Table A.1 includes a full list of the CPT codes and their frequencies.
We use the negotiated price between Anthem and each provider, the sum of insurer spending and consumer cost sharing, as our primary dependent variable.8 For a given procedure, the claims data contains observations for the primary procedure plus ancillary procedures (e.g. anesthesia services). Each of the ancillary procedures has a separate negotiated price. For each primary procedure, we use the sum of all related procedures to calculate the procedure’s bundled price because the reference price applies to this bundled price and not just the price of the primary procedure. Similarly, because the reference price only applies to the procedure’s facility fee, we only include costs from the facility portion of the claim in each procedure’s bundled price. As a test for cost-shifting, we examine the effects of the program on professional fees in Section 5.2.
For each surgical procedure, we identify the primary provider from the set of providers included in the bundle as the provider listed on the index surgical claim, the provider’s location, and whether the provider is an ASC or HOPD. The data also contains patient-level demographic information (e.g. patient age, gender, home zip code). To measure patient risk severity, we compute the patient’s weighted Charlson comorbidity score in the year prior to the procedure (Charlson et al., 1987). We also create indicators for the various chronic conditions that underlie the Charlson score.
3.1.1. Descriptive statistics
Table 1 presents summary statistics about the claims data. Colonoscopy procedures account for the majority (78%) of the procedures in the sample and also have the lowest average cost. Joint arthroscopy services have the highest price, but the reference price is set lower in the HOPD price distribution than for other services. Nearly all cataract surgeries performed at a HOPD are above the reference price. For all three services, the average patient age and percent male between ASC and HOPD patients are almost identical.
Table 1.
Descriptive statistics.
| Arthroscopy | Cataract surgery | Colonoscopy | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Mean | (sd) | Mean | (sd) | Mean | (sd) | |
|
| ||||||
| Mean price | ||||||
| ASC | $7687 | ($12,557) | $2380 | ($3319) | $1854 | ($3836) |
| HOPD | $7951 | ($6618) | $6625 | ($2896) | $2779 | ($1694) |
| Median price | ||||||
| ASC | $3730 | $1501 | $763 | |||
| HOPD | $5837 | $6162 | $2226 | |||
| 25th percentile price | ||||||
| ASC | $2284 | $1142 | $606 | |||
| HOPD | $4449 | $4754 | $1707 | |||
| 75th percentile price | ||||||
| ASC | $16,762 | $2311 | $1425 | |||
| HOPD | $9167 | $7866 | $3429 | |||
| Percent of services above reference price | ||||||
| ASC | 31.6% | (46.4%) | 31.2% | (46.3%) | 25.2% | (43.4%) |
| HOPD | 51.3% | (50.0%) | 98.4% | (12.4%) | 87.4% | (33.2%) |
| Number of procedures | ||||||
| ASC | 46,746 | 20,067 | 224,613 | |||
| HOPD | 21,901 | 5857 | 86,728 | |||
| Patient Age | ||||||
| ASC | 47.4 | (12.6) | 58.0 | (6.0) | 52.9 | (8.5) |
| HOPD | 47.5 | (12.5) | 57.4 | (6.9) | 52.7 | (9.0) |
| Male patient | ||||||
| ASC | 57.4% | (49.4%) | 44.9% | (49.7%) | 46.1% | (49.9%) |
| HOPD | 56.7% | (49.5%) | 45.9% | (49.8%) | 47.1% | (49.9%) |
3.2. Market-level exposure to the CalPERS reference pricing program
Our second data input is each market’s log-transformed exposure to CalPERS population subject to reference pricing, relative to the entire commercially insured population. To calculate each market’s exposure to the CalPERS reference pricing program, we divide the number of enrollees in the CalPERS-sponsored Anthem PPO plan that was subject to the reference pricing program by the number of individuals with commercial insurance. The denominator includes all individuals with commercial insurance, including non-CalPERS and non-Anthem plans. For each market , we define as
For simplicity, we refer to as exposure to CalPERS, rather than exposure to the CalPERS-sponsored Anthem PPO population. For both populations, we use the year before the program’s implementation, 2011, as the baseline year. The CalPERS enrollment data population is provided by the CalPERS Center for Innovation. For the commercially insured population denominator, we use the Inter-Study survey of insurers, which contains market-level information on the population sizes by insurance carrier.
We use Hospital Service Areas (HSAs) as our primary market definition. As a robustness test, we use the larger Hospital Referral Regions (HRRs) as an alternative market definition and find similar results. Both HSAs and HRRs are defined by the Dartmouth Atlas of Health Care and measure localized health care markets. California contains 209 HSAs, but only 121 HSAs match the claims data. Figure 3 shows the variation in CalPERS exposure across California. The CalPERS-sponsored Anthem PPO population is highly clustered around the Sacramento region and the specific markets in which the local governments have decided to administer benefits through CalPERS. The non-CalPERS Anthem population is more evenly distributed throughout the state. The average exposure in each HSA is 2.2% but ranges from a low of 0.003% to a high of 29.6%.
Fig. 3.
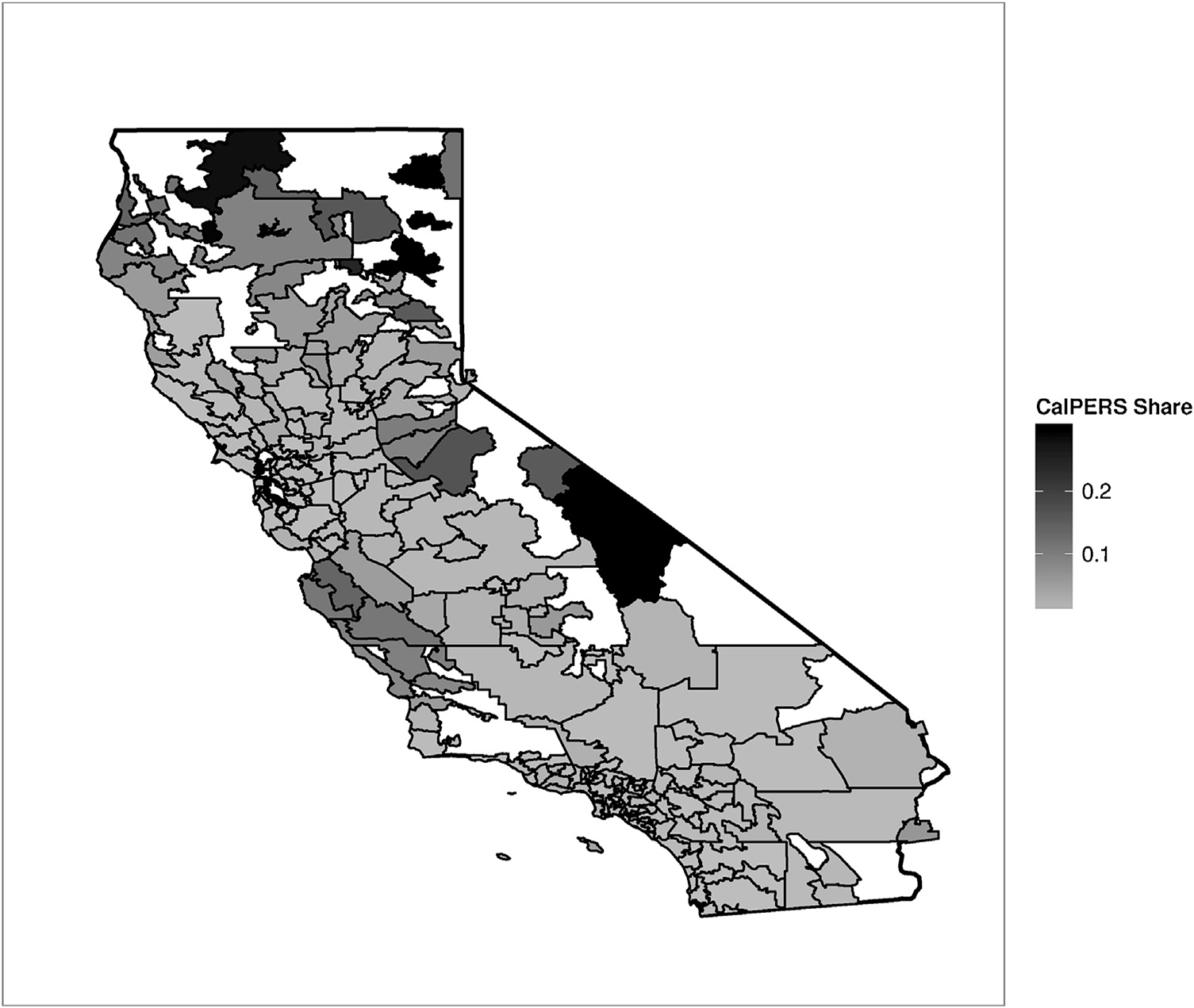
Variation in CalPERS exposure. This map shows the share of the commercially insured population that is enrolled in the CalPERS PPO subject to reference pricing.
Due to this skewness, in our primary regressions, we use the log-transformed exposure, which we calculate as , in our primary regressions.9 Using the log of CalPERS exposure also allows us to interpret our regression coefficients as elasticities. Fig. 4 plots the distribution of log-CalPERS exposure.10 The geographic variation shown in this figure is a key piece of our identification strategy. The regions with a small share of CalPERS members collectively serve as a control group for the regions with a larger share. As a result of this geographic distribution, California HOPDs and ASCs vary substantially in their exposure to the CalPERS population. Providers in markets with a smaller share of CalPERS enrollees are relatively unaffected by the program while providers for which CalPERS enrollees constitute a large share of their patient population are more affected.
Fig. 4.
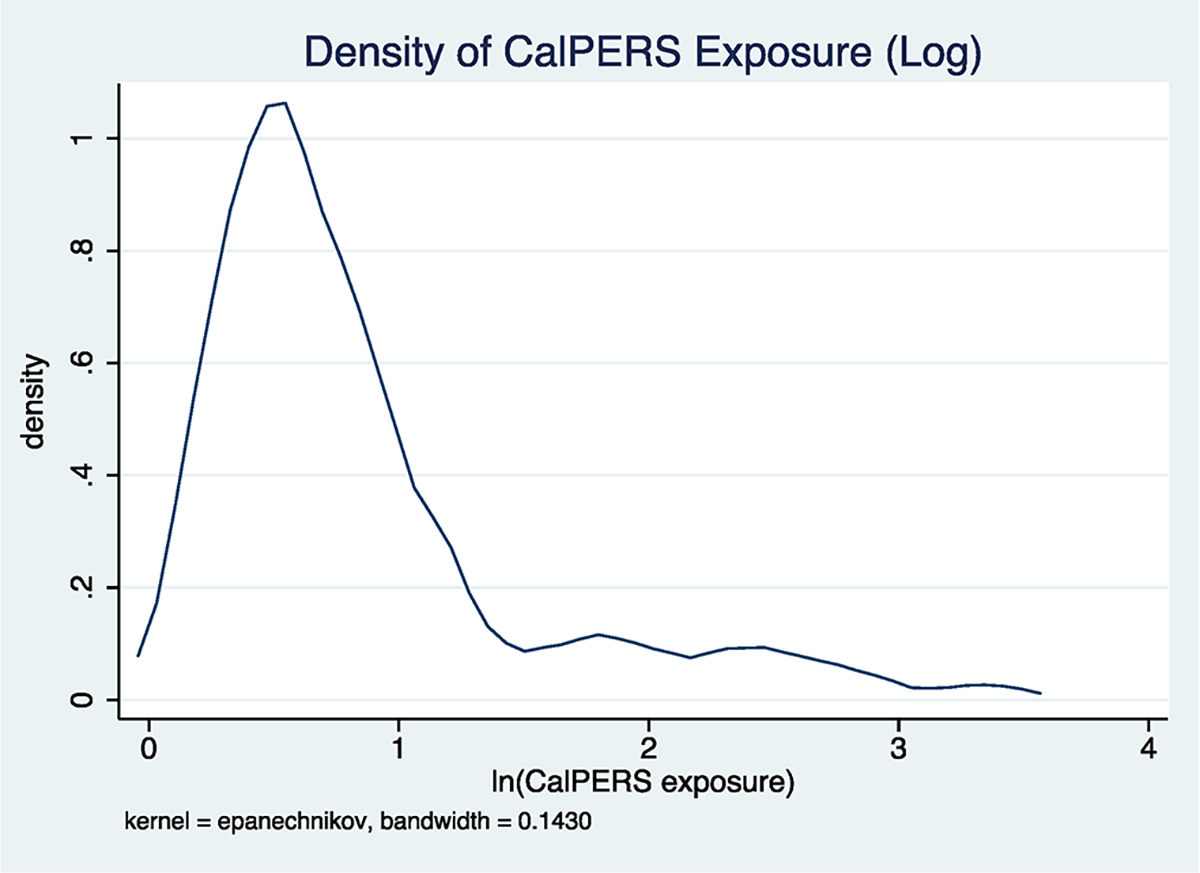
Distribution of CalPERS exposure. This figure shows the density in the log-transformed share of the commercially insured population that is enrolled in the CalPERS PPO subject to reference pricing.
4. Provider price responses
4.1. Empirical approach
To estimate provider price responses to the program, we estimate the following difference-in-differences regression:
| (1) |
In this specification, the dependent variable of measures the bundled facility price for a procedure received by patient from provider at time . The term indexes the pre (2009–2011) and post (2012–2013) implementation periods. We also include fixed effects for year and month to capture any seasonality or temporal changes in prices. The year fixed effects negate the inclusion of the main effect.
In , we include patient demographics (10-year age categories, gender, and patient HRR fixed effects). To account for differences in patient risks, we also include Charlson comorbidity scores and indicators for 17 chronic conditions. Finally, we include fixed effects for the primary CPT code for the procedure. To account for serial correlation, we cluster standard errors at the provider’s HSA.
The coefficient on the interaction of and measures the change in prices before and after the program’s implementation between high and low-exposure markets. Because the term is continuous and lies between 0 and 1, the coefficient is interpreted as the difference in prices between markets with no exposure to CalPERS (i.e., no CalPERS enrollees, so is thus equal to 0) and markets with full exposure to CalPERS (i.e., the entire commercially insured population is enrolled in CalPERS, so is thus equal to 1). Provider fixed effects in both control for time-invariant provider differences and allow for the coefficient to be interpreted as the within-provider change in prices. Because providers are matched to a single HSA, the provider fixed effects are collinear with and so we omit the main CalPERS exposure term.
A causal interpretation of the coefficient relies on the assumption that pre-implementation price trends are not correlated with CalPERS exposure and that market-level exposure to CalPERS is not correlated with other programs that might influence provider prices. This is a strong assumption as our treatment variable is not randomly assigned and is instead a function of government employment. To test the validity of this assumption, we test for pre-implementation price trends and do not find evidence of pre-trend differences based on exposure to CalPERS. We are also not aware of any other program that was implemented by CalPERS during this time period. Moreover, the low-exposure markets control for any statewide policies. In Appendix B, we test for contemporaneous changes that might impact provider prices. We find limited evidence of contemporaneous shocks, which supports our identification strategy. Finally, an economically meaningful program by an alternative employer is unlikely as no other employers have the same geographic reach across California. However, in Section 5.3, we use data from a sample of non-Anthem insurers and non-CalPERS employers as a robustness test. We do not find price changes that would support the existence of contemporaneous policies or programs.
This regression estimates the mean provider responses to the program, but the results may not be uniform. In particular, HOPD provider responses may depend on the provider’s baseline price relative to the reference price. To test for heterogeneous effects, we define equal to one if provider ’s mean price for service in 2011, the year before implementation, is above the reference price. We then estimate
| (2) |
This regression is similar to the one in Eq. (1), except that the term gives the differential effect of exposure to CalPERS by high-priced providers relative to low-priced providers.
4.2. Results
Table 2 starts by presenting price changes for both ASCs and HOPDs combined. The first column presents the arthroscopy results, the second column presents cataract surgery results, and the third column presents results for colonoscopy services. Because both the CalPERS exposure measure and prices are expressed in logs, the coefficients can be interpreted as elasticities. This table implies that a 10% increase in exposure to CalPERS leads to a 0.2% reduction in arthroscopy provider prices, but the result is not statistically significant. For cataract surgery and colonoscopy, there is a 0.7% and 0.4% reduction in provider prices, respectively. The year fixed effects indicate that overall prices increase by approximately 5% per year during the 2009–2013 study period.
Table 2.
Combined provider price responses to reference pricing.
| Arthroscopy | Cataract | Colonoscopy | |
|---|---|---|---|
| (1) | (2) | (3) | |
|
| |||
| Post × ln(CalPERS exposure) | −0.0232 | −0.0664** | −0.0359** |
| (0.0298) | (0.0309) | (0.0181) | |
| 2010 | 0.0381*** | 0.0353*** | 0.0376*** |
| (0.0100) | (0.00662) | (0.0106) | |
| 2011 | 0.127*** | 0.0728*** | 0.0813*** |
| (0.0138) | (0.0197) | (0.0101) | |
| 2012 | 0.183*** | 0.145*** | 0.175*** |
| (0.0321) | (0.0288) | (0.0232) | |
| 2013 | 0.223*** | 0.196*** | 0.208*** |
| (0.0288) | (0.0512) | (0.0246) | |
| Observations | 68,576 | 25,910 | 311,055 |
| Number of providers | 571 | 397 | 689 |
| Number of markets | 158 | 148 | 162 |
| Adjusted R2 | 0.240 | 0.184 | 0.230 |
| Mean price | 5521 | 2939 | 1542 |
This table presents the results from Eq. (1) and estimates provider price responses to the CalPERS reference pricing program. Each column separately estimates price responses for joint arthroscopy, cataract surgery, and colonoscopy procedures. In all columns, ASC and HOPD providers are combined. The dependent variable in all columns is ln(priceijtk) and each regression is estimated using OLS. Controls for month, patient age, gender, Charlson comorbidity score, indicators for 17 chronic conditions, and patient HRR fixed effects are included but not reported. Robust standard errors clustered at the Hospital Service Area level are in parentheses.
p < 0.01.
p < 0.05.
p < 0.1.
Table 3 presents provider price responses to the reference pricing program but separates ASCs and HOPDs. For ASC providers, there is a modest reduction in provider prices. For cataract surgery, a 10% increase in exposure to the program leads to a 0.6% reduction in ASC prices. For colonoscopies, there is a 0.4% reduction in ASC provider prices. While we do not find a a statistically significant effect for arthroscopies, as shown in Table A.5, we find that when disaggregating the arthroscopy procedures, there is a 0.5% reduction in ASC provider prices for knee and wrist arthroscopy, but no change for hip and shoulder arthroscopies. For all three procedures, the results for HOPD providers are neither statistically nor economically significant.
Table 3.
Provider price responses to reference pricing.
| Arthroscopy | Cataract | Colonoscopy | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
| ASC | HOPD | ASC | HOPD | ASC | HOPD | |
|
| ||||||
| Post × ln(CalPERS exposure) | −0.0219 | −0.0103 | −0.0630* | −0.0109 | −0.0404* | −0.0203 |
| (0.0366) | (0.0246) | (0.0358) | (0.0149) | (0.0217) | (0.0195) | |
| 2010 | 0.0155 | 0.0843*** | 0.0143 | 0.0895*** | 0.0237*** | 0.0744*** |
| (0.0126) | (0.00883) | (0.0129) | (0.00855) | (0.00721) | (0.0100) | |
| 2011 | 0.111*** | 0.152*** | 0.0422* | 0.160*** | 0.0580*** | 0.140*** |
| (0.0177) | (0.0107) | (0.0244) | (0.0106) | (0.0109) | (0.0125) | |
| 2012 | 0.151*** | 0.230*** | 0.108*** | 0.214*** | 0.153*** | 0.229*** |
| (0.0352) | (0.0317) | (0.0410) | (0.0174) | (0.0298) | (0.0180) | |
| 2013 | 0.190*** | 0.273*** | 0.156** | 0.273*** | 0.190*** | 0.249*** |
| (0.0319) | (0.0331) | (0.0689) | (0.0206) | (0.0307) | (0.0223) | |
| Observations | 46,696 | 21,880 | 20,065 | 5845 | 224,469 | 86,586 |
| Number of providers | 325 | 246 | 239 | 158 | 414 | 275 |
| Number of markets | 108 | 108 | 110 | 79 | 117 | 114 |
| Adjusted R2 | 0.259 | 0.211 | 0.185 | 0.283 | 0.255 | 0.177 |
| Mean price | 4409 | 7893 | 1882 | 6560 | 1067 | 2772 |
This table presents the results from Eq. (1) and estimates provider price responses to the CalPERS reference pricing program. The odd-numbered columns restrict the sample to ASC providers and the even-numbered columns restrict the sample to HOPD providers. The dependent variable in all columns is ln(priceijtk) and each regression is estimated using OLS. Controls for month, patient age, gender, Charlson comorbidity score, indicators for 17 chronic conditions, and patient HRR fixed effects are included but not reported. Robust standard errors clustered at the Hospital Service Area level are in parentheses.
p < 0.01.
p < 0.05.
p < 0.1.
To put these elasticities in perspective, moving from the HSA with the 25th percentile of CalPERS exposure to the 75th percentile is a 357% increase in the CalPERS-sponsored Anthem PPO share of the commercially insured population. Thus, the approximately −0.04 elasticity implies that implementing the reference pricing program in the 75th percentile market instead of in the 25th percentile market leads to a 14% larger reduction in ASC prices. At the median ASC price of $1501 for cataract surgery and $763 for colonoscopies, these results imply a $321 and $109 reduction in provider prices, respectively.
The slight reduction in ASC prices is somewhat counterintuitive. Appendix C presents a conceptual model that describes how the program might lead to reductions in ASC prices. This model implies that the decrease in ASC prices operates through a similar mechanism as the “generic competition paradox” in pharmaceutical markets, in which firms selling brand-name drugs avoid the segment of the market that is cross-price sensitive to generic drugs in order to focus on the segment of the market loyal to the brand-name drug (Scherer, 1993; Regan, 2008). Table C.1 presents evidence that the reduction in ASC prices is increasing in the market-level shift from HOPDs to ASCs that is induced by the program. In addition, due to cross-subsidization from other services, HOPDs are likely less sensitive to changes in consumer demand for these three services. ASCs, on the other hand, specialize in a narrow range of procedures, and thus are likely more sensitive to changes in consumer cost sharing for these services.
Table 4 presents the results from Eq. (2), which examines differences in responses by providers with baseline prices above the reference price relative to providers with prices below the reference price. The results in column 1 show that a 10% increase in exposure to the program leads to a 1.7% reduction in arthroscopy prices for ASCs that had a 2011 price above the $6000 reference price, compared to those with a 2011 price below $6000. For colonoscopies, the results are much more consistent with the expected outcomes. We do not find a differential effect for ASCs based on the provider’s baseline price. However, we do find meaningful price reductions for HOPDs with 2011 prices above the reference price. Our results imply that a 10% increase in exposure leads to a 1.7% reduction in colonoscopy prices for HOPDs above the reference price at baseline.
Table 4.
Provider price responses to reference pricing by baseline prices.
| Arthroscopy | Cataract | Colonoscopy | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
| ASC | HOPD | ASC | HOPD | ASC | HOPD | |
|
| ||||||
| Post × ln(CalPERS) | 0.0431* | 0.0119 | −0.0963* | 0.318 | −0.0422 | 0.137*** |
| (0.0236) | (0.0399) | (0.0499) | (0.319) | (0.0258) | (0.0431) | |
| Post × above | 0.226*** | −0.0105 | 0.0135 | 0.161 | 0.0368 | 0.187*** |
| (0.0674) | (0.0543) | (0.0890) | (0.178) | (0.0483) | (0.0236) | |
| Post × ln(CalPERS) above | −0.170*** | −0.0316 | 0.0674 | −0.329 | 0.0884 | −0.171*** |
| (0.0514) | (0.0496) | (0.0624) | (0.319) | (0.0748) | (0.0514) | |
| Observations | 46,696 | 21,880 | 20,065 | 5845 | 224,469 | 86,586 |
| Number of providers | 325 | 246 | 239 | 158 | 414 | 275 |
| Number of markets | 108 | 108 | 110 | 79 | 117 | 114 |
| Adjusted R2 | 0.263 | 0.212 | 0.192 | 0.283 | 0.260 | 0.181 |
| Mean price for high-priced providers | 6844 | 10,860 | 2939 | 6639 | 1943 | 2986 |
This table presents the results from Eq. (2) and estimates heterogeneous provider price responses to the CalPERS reference pricing program based on 2011 provider prices. The odd-numbered columns restrict the sample to ASC providers and the even-numbered columns restrict the sample to HOPD providers. The dependent variable in all columns is ln(priceijtk) and each regression is estimated using OLS. Controls for month, patient age, gender, Charlson comorbidity score, indicators for 17 chronic conditions, and patient HRR fixed effects are included but not reported. Robust standard errors clustered at the Hospital Service Area level are in parentheses.
p < 0.01.
p < 0.05.
p < 0.1.
At the same time, for both cataract surgery and colonoscopy, the main coefficients are positive and large in magnitude for HOPDs. For these two services, the main effects imply that HOPDs with baseline prices below the reference price increased prices, while providers above the reference price decreased prices by approximately the same amount. As shown in Table 3, these effects cancel out, and on average, the CalPERS program does not lead to changes in HOPD prices.
In contrast to the mean results presented in Table 3, these results suggest that, with the exception of arthroscopy providers, high-priced HOPDs responded to the program by lowering prices. Similarly, with the exception of arthroscopy providers, the ASC price responses do not differ by baseline provider prices. These two results are consistent with the design of the program and with consumer responses to the program. Patients have a strong financial incentive to move from providers with prices above the reference price. In contrast, the program does not change patient’s incentives to select a low-priced ASC, and so we should not expect to find a differential price response.
4.3. Parallel trends
To test for pre-implementation differences in price trends, we estimate a similar regression as Eq. (1) but replace the term with quarterly interactions that capture price differences based on exposure to the CalPERS population. We use the first quarter of the data, January-March 2009, as the reference period. The quarterly coefficients are shown in Fig. 5, which plots the quarterly differences in prices for ASCs (panel a) and HOPDs (panel b). For ASCs, there is little difference in provider prices based on exposure to CalPERS during the pre-period. However, following the implementation of reference pricing, which is indicated by the dashed line at , there is a steady decline in the log-CalPERS exposure price coefficients. For HOPDs, the confidence intervals overlap zero in all quarters and the point estimates hover around 0. In addition, the declining ASC prices over time mirror the consumer responses to the program found in previous studies, which find that for all three services, the magnitude of the consumer responses approximately doubled from the first to the second year of the program (Robinson et al., 2015a,b,c).
Fig. 5.
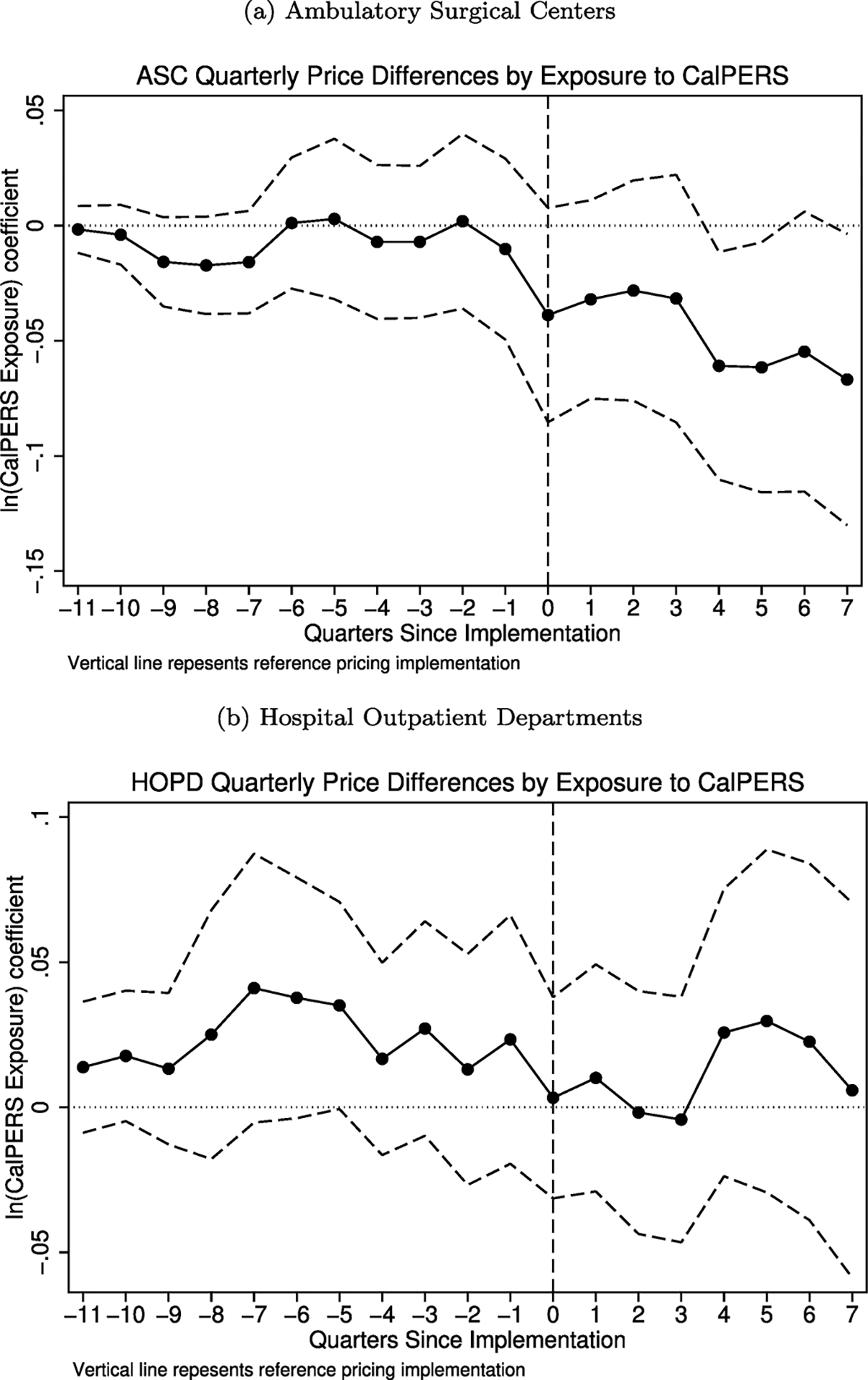
Parallel trends test. These figures plot the quarterly association between provider prices and exposure to CalPERS. The solid line represents the log-difference in prices for a 1-unit change in log-exposure to CalPERS. The dashed lines represent a 95% confidence interval. The vertical line indicates the implementation of the CalPERS reference pricing program. The top panel presents results for ambulatory surgical centers, while the bottom panel presents results for hospital outpatient departments.
Fig. 6 presents similar results, but plots the quarterly coefficients. Thus, these figures show the quarterly difference in prices between providers with 2011 prices above the reference price with providers with prices below the reference price at baseline. For ASCs, we do not find any difference in trends based on provider baseline prices. For HOPDs, there is a downward trend following the implementation of the program, but the result is not statistically significant.
Fig. 6.
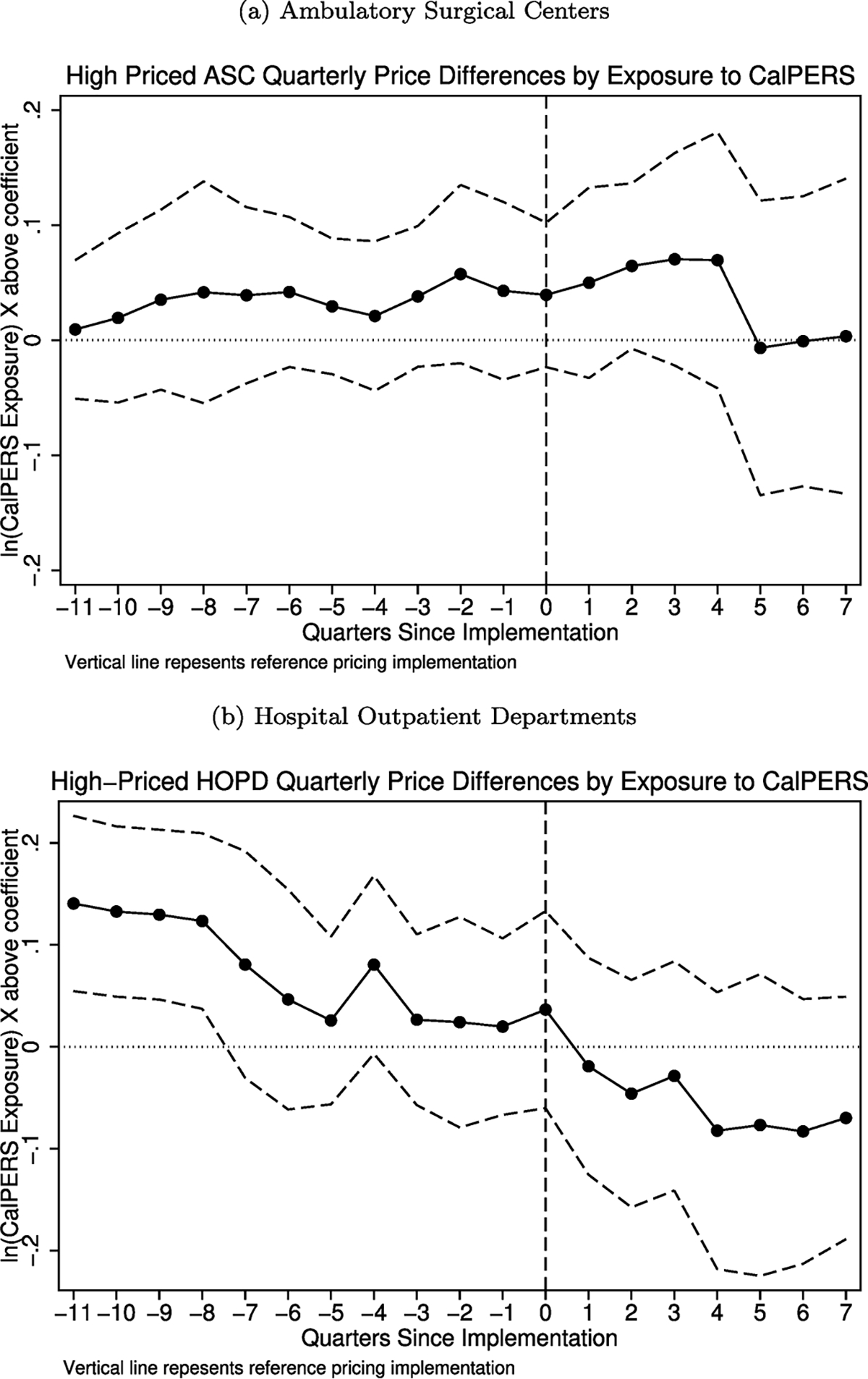
Parallel trends test: high vs. low-priced providers. These figures plot the quarterly association between provider prices and exposure to CalPERS based on each provider’s baseline price relative to the reference price. The solid line represents the log-difference in prices for a 1-unit change in log-exposure to CalPERS for a providers with a baseline price above the reference price relative to providers with prices below the reference price at baseline. The dashed lines represent a 95% confidence interval. The vertical line indicates the implementation of the CalPERS reference pricing program. The top panel presents results for ambulatory surgical centers, while the bottom panel presents results for hospital outpatient departments.
Tables A.2 and A.3 test the parallel trends separately for each procedure and find similar results. We do not find evidence of pre-trend price differences based on exposure to CalPERS. The effects are larger in the second year of the program than in the first year.
5. Alternative explanations
We next examine several alternative explanations of how providers might respond to the program. These alternative explanations may invalidate the previous results (e.g. price discrimination), change the interpretation of the results (e.g. cost-shifting or changes in quality), or provide evidence of contemporaneous shocks (e.g. changes in prices for other insurers). For all cases, we do not find substantial evidence that supports other forms of provider responses. The null results for these alternative explanations supports our interpretation of the previous results as evidence of increased price competition induced by the reference pricing program.
5.1. Do providers price discriminate?
One potential provider response to the reference pricing program is to price discriminate between patient populations and simply charge CalPERS patients a lower price while not changing prices for non-CalPERS patients. Price discrimination is a way to lessen the reduction in demand among CalPERs patients while avoiding price reductions for the larger non-CalPERS population. However, if providers respond to the program by price discriminating, our previous results may be mechanically driven simply by the location of CalPERS patients rather than any real change in provider prices. In fact, a core assumption underlying our identification strategy is that provider prices do not differ between the CalPERS and non-CalPERS populations.
To test this assumption, we estimate changes in within-provider prices between the CalPERS and non-CalPERS populations before and after the program as
| (3) |
In this regression, indicates that patient is a CalPERS enrollee. As in the previous regressions, the provider fixed effects allow for a within-provider interpretation and so the coefficient tests the hypothesis that CalPERS and non-CalPERS patients face different baseline prices at the same provider. The coefficient measures the changes in provider prices for CalPERS patients relative to non-CalPERS patients following the launch of the reference pricing program. Thus, a negative coefficient indicates that following the implementation of the reference pricing program, CalPERS and non-CalPERS patients within the Anthem PPO face different bundled prices at the same provider. We include controls for patient demographics and other characteristic that may influence prices and so this regression estimates price discrimination conditional on observed patient characteristics.
A shown in Table 5, we find little evidence supporting the price discrimination hypothesis. Following the implementation of the program, the coefficients indicate that CalPERS and non-CalPERS patients face the same prices at a given provider. With the exception of HOPD prices for joint arthroscopy, where we do not find a change in provider prices based on exposure to CalPERS, the coefficients are again small and not statistically significant. Among the ASC providers, where we find a price response in our main specification, the coefficients are all less than 1% and are not statistically significant.
Table 5.
Price discrimination between CalPERS and non-CalPERS patients.
| Arthroscopy | Cataract | Colonoscopy | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
| ASC | HOPD | ASC | HOPD | ASC | HOPD | |
|
| ||||||
| CalPERS patient | 0.0224* | 0.00844 | 0.0178* | −0.00401 | 0.00931 | 0.00282 |
| (0.0131) | (0.00957) | (0.00969) | (0.00593) | (0.00610) | (0.00596) | |
| Post × CalPERS patient | 0.00627 | −0.0446*** | −0.00615 | −0.0155 | −0.00853 | −0.00293 |
| (0.0216) | (0.0140) | (0.0199) | (0.0125) | (0.0105) | (0.00920) | |
| Observations | 46,696 | 21,880 | 20,065 | 5845 | 224,469 | 86,586 |
| Number of providers | 325 | 246 | 239 | 158 | 414 | 275 |
| Number of markets | 108 | 108 | 110 | 79 | 117 | 114 |
| Adjusted R2 | 0.259 | 0.212 | 0.178 | 0.283 | 0.254 | 0.176 |
This table presents the results from Eq. (3) and tests for price discrimination between the CalPERS and non-CalPERS populations. The odd-numbered columns restrict the sample to ASC providers and the even-numbered columns restrict the sample to HOPD providers. The dependent variable in all columns is ln(priceijtk) and each regression is estimated using OLS. Controls for year, month, patient age, gender, Charlson comorbidity score, indicators for 17 chronic conditions, and patient HRR fixed effects are included but not reported. Robust standard errors clustered at the Hospital Service Area level are in parentheses.
p < 0.01.
p < 0.05.
p < 0.1.
The lack of a consistent effect implies that providers do not respond to the reference pricing program by price discriminating between the CalPERS and non-CalPERS populations, either before or after the implementation of the reference pricing program. The absence of a meaningful baseline effect supports the use of the non-CalPERS Anthem population as a control group. In addition, the coefficients suggest that the previously discussed price changes reflect changes in underlying negotiated rates for ASCs and do not simply capture price discrimination by providers. Instead, the price responses apply to both the CalPERS and non-CalPERS populations.
Table A.6 tests this effect by limiting the sample to the non-CalPERS control population. Following the implementation of reference pricing, there is a nearly identical reduction in provider prices when restricting the sample to the non-CalPERS population. Across all markets, the non-CalPERS population constitutes 86.9% of the total Anthem PPO population. In markets with above-average exposure to CalPERS, the non-CalPERS population makes up 77.9% of the Anthem PPO population. Thus, over 75% of the price reductions caused by the CalPERS program accrue to the non-CalPERS control group.
Because provider prices are negotiated at the insurer-level rather than at the individual employer level, the much larger Anthem population captures the majority of the price reductions caused by CalPERS reference pricing program. The price changes that are induced by the CalPERS population also apply to the non-CalPERS population. As a result, the price reductions can be interpreted as a positive externality that the CalPERS reference pricing program has on other populations.
5.2. Do providers cost-shift?
The next alternative explanation we examine is cost-shifting between different types of services fees. Most surgical services are reimbursed using two separate fees, a facility fee and a professional fee. The facility fee is meant to cover the expenses for the surgical facility while the professional fee covers the physician’s cost. In this setting, the median professional fee is 44.0% of the facility fee, but ranges from a low of 14.2% for cataract surgeries performed in HOPDs to a high of 55.9% for colonoscopies performed in HOPDs. The reference price only applies to the facility fee and does not cover the professional fee. Accordingly, the provider price responses estimated so far only use the procedure’s facility price as the outcome of interest. However, one potential provider response to the reference pricing program is to lower the facility fee but increase the professional fee. Such an approach keeps the overall reimbursement level fixed but decreases the effects of the reference pricing program. If this type of cost-shifting occurs, then the price reductions we observe may be illusory as overall medical spending may not change, or may even increase.
To test for changes in professional fees, we estimate the same regression as Eq. (1) but use the professional fee as the dependent variable. A positive coefficient indicates that providers in markets with high CalPERS exposure increase their professional fees. However, as shown in Table 6, we do not find evidence that providers change professional fees. The exception is for cataract surgeries performed in HOPDs, where we find that a 3.2% reduction in professional fees for every 10% increase in CalPERS exposure. However, this result is in the opposite sign of any increase in professional fees due to cost-shifting.
Table 6.
Changes in professional fees.
| Arthroscopy | Cataract | Colonoscopy | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
| ASC | HOPD | ASC | HOPD | ASC | HOPD | |
|
| ||||||
| Post × ln(CalPERS exposure) | 0.0468 | −0.0729 | −0.0265 | −0.319*** | −0.0369 | −0.0345 |
| (0.0316) | (0.0462) | (0.0476) | (0.101) | (0.0765) | (0.0751) | |
| 2010 | −0.0547** | −0.109*** | 0.0488** | −0.0151 | −0.239*** | −0.159*** |
| (0.0261) | (0.0274) | (0.0216) | (0.0749) | (0.0222) | (0.0287) | |
| 2011 | −0.128*** | −0.127*** | 0.0470** | 0.00340 | −0.284*** | −0.176*** |
| (0.0294) | (0.0324) | (0.0190) | (0.0615) | (0.0455) | (0.0400) | |
| 2012 | −0.157*** | −0.0977 | 0.0229 | 0.259*** | −0.247*** | −0.157** |
| (0.0454) | (0.0646) | (0.0423) | (0.0851) | (0.0513) | (0.0707) | |
| 2013 | −0.130*** | −0.0298 | 0.0269 | 0.242*** | −0.256*** | −0.266** |
| (0.0414) | (0.0479) | (0.0574) | (0.0691) | (0.0512) | (0.103) | |
| Observations | 46,696 | 21,880 | 20,065 | 5845 | 224,469 | 86,586 |
| Number of providers | 325 | 246 | 239 | 158 | 414 | 275 |
| Number of markets | 108 | 108 | 110 | 79 | 117 | 114 |
| Adjusted R2 | 0.051 | 0.038 | 0.004 | 0.009 | 0.059 | 0.043 |
| Mean professional fee | 1559 | 1557 | 869 | 1046 | 525 | 580 |
This table presents the results from Eq. (1) and tests changes in professional fees as evidence of cost-shifting in responses to the CalPERS reference pricing program. The odd-numbered columns restrict the sample to ASC providers and the even-numbered columns restrict the sample to HOPD providers. The dependent variable in all columns is the log of each procedure’s professional fee. Each regression is estimated using OLS. Controls for month, patient age, gender, Charlson comorbidity score, indicators for 17 chronic conditions, and patient HRR fixed effects are included but not reported. Robust standard errors clustered at the Hospital Service Area level are in parentheses.
p < 0.01.
p < 0.05.
p < 0.1.
One limitation of the data is that we are not able to capture all forms of provider cost-shifting. Providers may also cost-shift by increasing the prices they charge Anthem patients for other services. Finally, providers may increase utilization of joint arthroscopy, cataract, and colonoscopy services. The latter form of cost-shifting is similar to several previous studies that show providers strategically induce patient demand (Gruber and Owings, 1996; Yip, 1998; Dafny, 2005; Kim and Norton, 2015).
5.3. Do providers changes prices for other insurers?
The analysis thus far has only considered the price effects for the Anthem PPO insurance plan. However, the program may lead to changes in pricing for other insurers that have implications for understanding the overall benefits of the program. If providers price discriminate by reducing prices for the Anthem PPO plan while raising prices for other insurers, then the estimated price reductions may not be welfare improving for the entire commercially insured population.
To test for spillover effects to other insurers, we use data provided by the Health Care Cost Institute (HCCI), along with companies providing data to it – Aetna, Humana, and UnitedHealthcare. The HCCI data contains medical claims from approximately 50 million individuals, which makes it one of the largest sources of claims data available to researchers. Importantly for this study, Anthem Blue Cross is not one of the three insurers that supply data to the HCCI. As a result, the HCCI data allows us to test for changes in provider prices among insurers that have not implemented the reference pricing program for any of their employer customers. The HCCI data also allows us to test for contemporaneous shocks under the assumption that any contemporaneous shocks that influence the Anthem population also impact the population that receives benefits through other large insurers.
From the HCCI data, we identify all knee and shoulder arthroscopy, cataract surgery, and colonoscopy procedures. We limit the patient population to patients enrolled in a PPO and out-patient procedures performed at either an ASC or HOPD. We then use the HCCI data to estimate the same regression as Eq. (1).
One limitation of the HCCI data is that it does not contain facility identifiers and instead includes encrypted physician National Provider Identifiers (NPIs). We are thus unable to include a fixed effect for the facility at which the procedure was performed. We instead create a unique identifier for each NPI, HSA, and facility (ASC or HOPD) combination. We use this identifier as a fixed effect to identify the within-provider changes in prices. Another limitation of the HCCI data is that the insurers represented in the HCCI data do not have a large California presence. UnitedHealth and Aetna, which are the largest and the fifth-largest insurers in the U.S., account for just 8.3% and 7.1% of the commercially insured market in California, respectively. Humana, which primarily offers Medicare Part C plans, has a market share of less than 1%. In contrast, Anthem Blue Cross has a California market share of approximately 27.8%.
As shown in Table 7, we do not find evidence that the program leads to price changes for non-Anthem insurers. In the top panel, we leverage the scope of the HCCI data and include the entire HCCI population, which includes patients from all 50 states. By including data from all states, we are able to control for differences in California-specific trends that might be leading to changes in prices. In the bottom panel, we restrict the population to California patients in order to have a more direct analogue of the primary estimation results. Due to the low market share of Aetna and United in California, the California-only sample sizes in the Panel B are substantially lower than in the Anthem data used in the primary analyses.
Table 7.
Changes in prices for non-anthem insurers.
| Arthroscopy | Cataract | Colonoscopy | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| ASC | HOPD | ASC | HOPD | ASC | HOPD | |
|
| ||||||
| Panel A: full U.S. population | ||||||
| Post × ln(exposure) | −0.0110 | −0.0727** | −0.124 | 0.0739 | 0.0331* | −0.0292 |
| (0.0648) | (0.0337) | (0.0801) | (0.101) | (0.0182) | (0.0291) | |
| Observations | 217,084 | 279,985 | 111,778 | 24,284 | 1,425,702 | 909,037 |
| Number of providers | 1158 | 1199 | 849 | 242 | 3870 | 3904 |
| R-squared | 0.144 | 0.141 | 0.072 | 0.087 | 0.045 | 0.138 |
| Panel B: California subpopulation | ||||||
| Post × ln(exposure) | −0.111 | −0.00129 | 0.187 | 0.500* | 0.0443 | 0.0559 |
| (0.111) | (0.101) | (0.133) | (0.172) | (0.0290) | (0.0588) | |
| Observations | 9980 | 1476 | 1760 | 206 | 79,142 | 22,722 |
| Number of providers | 94 | 20 | 27 | 4 | 354 | 159 |
| R-squared | 0.068 | 0.206 | 0.276 | 0.574 | 0.054 | 0.140 |
This table presents the results that use data from the Health Care Cost Institute (HCCI) to test for provider price responses to the CalPERS reference pricing program among non-Anthem insurers. The odd-numbered columns restrict the sample to ASC providers and the even-numbered columns restrict the sample to HOPD providers. The top panel uses the entire HCCI population while the bottom panel restricts the sample to the California population. The dependent variable in all columns is ln(priceijtk) and each regression is estimated using OLS. Controls for year, month, patient age, gender, Charlson comorbidity score, indicators for 17 chronic conditions, and patient HRR fixed effects are included but not reported. Robust standard errors clustered at the Hospital Service Area level are in parentheses.
p < 0.01.
p < 0.05.
p < 0.1.
For both groups, we do not find meaningful reductions in provider prices based on exposure to CalPERS. In the top panel, we find that a 10% increase in exposure to the program leads to a 0.7% reduction in HOPD prices for arthroscopy. However, in our main results, we do not find any HOPD price response for arthroscopy procedures. Similarly, we find a 0.3% increase in ASC prices for colonoscopy, but this effect is in the opposite direction of our results. Finally, in the bottom panel, we find a 5% increase in HOPD provider prices for cataract surgery. However, the HCCI data only has 206 patients and 4 cataract HOPD providers that meet our inclusion criteria. Thus, this large increase should be interpreted with caution.
We interpret the lack of a consistent effect among the non-Anthem population in the HCCI population as evidence that exposure to the CalPERS reference pricing program did not lead to changes in how providers bargain with other insurers for these three services. The lack of an effect also suggests that contemporaneous shocks that impact all insurers in the market are not present during this time period.
5.4. Do providers change quality?
The previous tests have examined changes in provider prices, but providers may also respond to the changes in consumer demand by changing quality. To test for quality responses, we use the same empirical strategy but replace the dependent variable with an indicator for procedural complications related to the surgery, . These outcomes have been previously used to examine if the CalPERS program leads to changes in complications for consumers (Robinson et al., 2015a,b; Naseri et al., 2016). A full description of the quality measures is described in Appendix D. They include complications similar to postoperative nerve injury (joint arthroscopy), retinal detachment (cataract surgery), and intestine perforations (colonoscopy). The results in Table 8 do not support the hypothesis that providers respond to the CalPERS program by changing quality. The only statistically significant coefficient is for colonoscopies performed at HOPDs, where we find a 0.4 percentage point reduction in the complication rate. None of the other coefficients are economically or statistically significant.
Table 8.
Changes in quality outcomes.
| Arthroscopy | Cataract | Colonoscopy | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
| ASC | HOPD | ASC | HOPD | ASC | HOPD | |
|
| ||||||
| Post × ln(CalPERS exposure) | 0.000245 | −0.00397 | 0.00227 | 0.0125 | −0.00178 | −0.00428* |
| (0.00177) | (0.00371) | (0.00430) | (0.0118) | (0.00113) | (0.00218) | |
| 2010 | −0.00118 | −0.00312 | 0.00583 | 0.0191** | 0.00224*** | 0.000294 |
| (0.00150) | (0.00260) | (0.00354) | (0.00725) | (0.000800) | (0.00178) | |
| 2011 | −0.00192 | −0.00107 | 0.0106** | 0.0157** | 0.00247** | 0.00145 |
| (0.00196) | (0.00296) | (0.00483) | (0.00607) | (0.00107) | (0.00168) | |
| 2012 | −0.00178 | 0.00188 | 0.00882 | 0.00879 | 0.00315** | 0.00586** |
| (0.00272) | (0.00385) | (0.00577) | (0.00638) | (0.00125) | (0.00276) | |
| 2013 | −0.00124 | 0.00168 | 0.0119* | 0.00835 | 0.00151 | 0.00462* |
| (0.00278) | (0.00410) | (0.00607) | (0.00776) | (0.00117) | (0.00257) | |
| Observations | 46,696 | 21,880 | 20,065 | 5845 | 224,469 | 86,586 |
| Number of providers | 325 | 246 | 239 | 158 | 414 | 275 |
| Number of markets | 108 | 108 | 110 | 79 | 117 | 114 |
| Adjusted R2 | 0.059 | 0.087 | 0.005 | 0.029 | 0.019 | 0.030 |
| Mean complication rate | 0.013 | 0.016 | 0.028 | 0.039 | 0.019 | 0.032 |
This table presents the results from Eq. (1). The dependent variable in all columns is the probability of having a surgical complication and each regression is estimated using OLS. Controls for month, patient age, gender, Charlson comorbidity score, indicators for 17 chronic conditions, and patient HRR fixed effects are included but not reported. Robust standard errors clustered at the Hospital Service Area level are in parentheses.
p < 0.01.
p < 0.05.
p < 0.1.
5.5. Robustness tests
As additional tests, Appendix A includes regression results that test for parallel trends by procedure and provider baseline price, use the raw exposure to CalPERS as the primary independent variable, compare price trends between markets in the top and bottom quartiles of exposure to CalPERS, define CalPERS exposure relative to the entire insured population (including Medicare and Medicaid patients), test for differences based on market concentration, include both facility and professional provider fixed effects, and test for provider entry. In all cases, the results are not meaningfully different than the main results, and indicate that the program leads to modest reductions in provider prices.
6. Conclusion
In an effort to reduce healthcare costs, many employers and payers have implemented innovative benefit designs. For “shoppable” services, insurance benefit designs such as reference pricing exploit the large variation in healthcare prices and incentivize patients to receive care from less expensive providers. While previous research has shown that the CalPERS reference pricing program does in fact lead patients to select less expensive providers, little evidence exists on how providers respond to this, or other health insurance designs.
This paper shows meaningful provider price responses to the reference pricing program. Somewhat counterintuitively, the price reductions largely apply to the lower-priced providers ASCs. The price reduction among ASCs is consistent with increased price competition among ASC providers. Because the provider price changes apply to all enrollees in the Anthem PPO, the CalPERs program leads to a sizable positive externality to the non-CalPERS population. The CalPERS population captures only approximately 25% of the price reduction, while approximately 75% of the price reduction benefits the non-CalPERS population in the form of a positive price externality. To our knowledge, this study is the first to show how targeted patient cost sharing can lead to provider price reductions.
As insurers seek to reduce health care spending, this paper suggests that for selected services, expanded use of reference pricing programs or other targeted insurance programs may have the dual effect of changing both consumer and provider behavior. While the price reductions we find in this study are relatively modest, these three services account for approximately 2.4% of the $949 billion spent by the commercially insured population. Previous estimates suggest that approximately 43% of health care spending is for shoppable services, and so expanded programs may have meaningful effects (Frost et al., 2016; Robinson et al., 2017). At the same time, few payers have the purchasing power of CalPERS. Unless they are pooled across employers, reference pricing programs for individual employers will likely have minimal effects on provider pricing behaviors.
This study is not without limitations and expanding upon this study’s limitations is important for future work. Perhaps the largest limitation is that this paper only examines provider responses in the first two years of the CalPERS reference pricing program. As both patients and providers learn more about the program, these initial responses may not be maintained. In addition, we only observe provider prices for services included in the reference pricing program. It may be possible that providers lower prices for the reference pricing-eligible services but then negotiate higher prices for non-covered services. Finally, under a model of physician-induced demand, providers may increase the volume of services performed (Cromwell and Mitchell, 1986). We do not examine the quantity effects of the program, but future work should test if the program changes utilization of services.
Despite these limitations, this study demonstrates how innovative and appropriately-constructed insurance designs can spur lead to reductions in provider prices. These results suggest that if other employers were to simultaneously implement similar reference pricing programs, the provider price reductions would likely increase and apply to a larger set of providers.
Acknowledgments
This project was supported by Grant R01 HS022098 from the Agency for Healthcare Research and Quality, R21CA919229 from the National Cancer Institute, the Bing Center for Health Economics, the National Institute for Health Care Management Foundation, and the Laura and John Arnold Foundation. Data on Anthem Blue Cross PPO enrollees were provided by Anthem, Inc. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality, CalPERS, or Anthem, Inc. The study was approved by the Institutional Review Board at the University of California, Berkeley. We thank seminar participants at IIOC 2016, Indiana University, the Chicago Health Economics Workshop, and the RAND Labor Seminar. We also thank Marion Aouad, Juan Pablo Atal, David Cowling, Paul Gertler, Josh Gottlieb, Chaoran Guo, Benjamin Handel, Daniel Miller, James Robinson, Neeraj Sood, and Katherine Yang for providing helpful comments.
Appendix A. Additional tables and figures
A.1. Parallel trends by service
We test for pre-trend differences by estimating a similar regression as Eq. (1) but replace the term with four year by exposure interactions: . We use 2009 as the reference year. As shown in Table A.2, we fail to reject differences in prices based on market-level exposure to CalPERS in the 2010 and 2011 pre-implementation years. The only exception is for joint arthroscopy procedures performed at an ASC, where we find a 0.2% decrease in prices for every 10% increase in exposure to the CalPERS program in 2010 but we do not find an effect for 2011.
In Table A.3, we use the same approach, but test for parallel trends among the providers with a 2011 price above the reference price, relative to providers below the reference price. For arthroscopy and colonoscopy, we do not find any difference in prices. However, for cataract HOPD providers, we find a 0.2 and 0.3 elasticity in 2010 and 2011, respectively. However, the elasticity increases to 0.8 and 0.7 in 2012 and 2013, respectively.
A.2. Combined facility and professional fee
The results in Table 3 use the log-transformed facility fee as the dependent variable, to which the reference price is applied, while the results in Table 6 use the log-transformed professional fee as the dependent variable. As a sensitivity test, we estimate the same set of regressions with the log-transformed combined facility and professional fees as the dependent variable. These results are similar to, but slight smaller in magnitude than, the main results in Table 3 (Table A.4).
A.3. Detailed arthroscopy services
The joint arthroscopy results pool knee, shoulder, hip, and wrist arthroscopy procedures. As a sensitivity test, we disaggregate the arthroscopy procedures into two similar arthroscopy types – hip and shoulder arthroscopy and knee and wrist arthroscopy. As shown in Table A.5, we find that the arthroscopy results are driven exclusively by changes in ASC prices for knee and wrist arthroscopy. We find no change in ASC or HOPD prices for hip and shoulder arthroscopy. For knee and wrist arthroscopy, we find that a 10% increase in CalPERS exposure leads to a 0.5% reduction in ASC prices and no change in HOPD prices. This change is consistent with the cataract surgery and colonoscopy effects.
A.4. Non-CalPERS control population
As a sensitivity test of the price discrimination hypothesis, we estimate the main difference-in-differences regression but limit the population to the non-CalPERS Anthem PPO population that was not subject to the reference pricing program. As shown in Table A.6, we find that the results for the non-CalPERS population are almost identical to the main results. Thus, the lower prices induced by the CalPERS reference pricing program benefit the population not subject to the program. Across all markets, the non-CalPERS population constitutes 86.9% of the total Anthem PPO population. In markets with above-average exposure to CalPERS, the non-CalPERS population makes up 77.9% of the Anthem PPO population. Thus, over 75% of the price reductions caused by the CalPERS program accrue to the non-CalPERS control group.
A.5. Alternative CalPERS exposure measures
A.5.1. Non log-transformed CalPERS exposure
Our main results use the log-transformed exposure to CalPERS as our primary independent variable of interest. As a robustness test, we use the raw CalPERS exposure. As shown in Fig. A.1, the raw CalPERS exposure is highly skewed. The results when using the raw share are similar to when using the log-transformed share. As shown in the first column of Table A.7, we find that every 10-percentage point increase in CalPERS exposure leads to 11.1, 11.6 and 7.0 percentage point reduction in ASC prices for joint arthroscopy, cataract surgery, and colonoscopy procedures, respectively. We do not find statistically significant reductions in prices for HOPDs.
A.5.2. Dichotomous CalPERS exposure: top quartile vs. bottom quartile
Our main results use a continuous measure of CalPERS exposure. As an additional test, we test for differences in price trends between markets in the top quartile of exposure to CalPERS (2.1%) compared to markets in the bottom quartile of exposure to CalPERS (0.5%). We define market-level exposure to CalPERS as the share of CalPERS enrollees to the commercially insured population in each market. As shown in Table A.8, the results are similar to our main results. We find that relative to the bottom quartile markets, the top quartile markets have a 9% reduction in ASC colonoscopy prices. The 11.9% reduction in cataract surgery prices at ASC providers is close to statistically significant (p = 0.103).
Table A.1.
Procedure codes included in analysis.
| CPT code | Procedure | Frequency | Description |
|---|---|---|---|
|
| |||
| 29881 | Arthroscopy | 18,775 | Arthroscopy, knee, surgical; with meniscectomy (medial OR lateral, including any meniscal shaving) |
| 29826 | Arthroscopy | 9380 | Arthroscopy, shoulder, surgical; decompression of subacromial space with partial acromioplasty, with or without coracoacromial release |
| 29880 | Arthroscopy | 8060 | Arthroscopy, knee, surgical; with meniscectomy (medial AND lateral, including any meniscal shaving) |
| 29877 | Arthroscopy | 4010 | Arthroscopy, knee, surgical; debridement/shaving of articular cartilage (chondroplasty) |
| 29822 | Arthroscopy | 2493 | Arthroscopy, shoulder, surgical; debridement, limited |
| 29875 | Arthroscopy | 2486 | Arthroscopy, knee, surgical; synovectomy, limited (eg, plica or shelf resection) (separate procedure) |
| 29876 | Arthroscopy | 2385 | Arthroscopy, knee, surgical; synovectomy, major, two or more compartments (eg, medial or lateral) |
| 29823 | Arthroscopy | 2299 | Arthroscopy, shoulder, surgical; debridement, extensive |
| 29879 | Arthroscopy | 1582 | Arthroscopy, knee, surgical; abrasion arthroplasty (includes chondroplasty where necessary) or multiple drilling or microfracture |
| 29824 | Arthroscopy | 1268 | Arthroscopy, shoulder, surgical; distal claviculectomy including distal articularsurface (Mumford procedure) |
| 29807 | Arthroscopy | 1221 | Arthroscopy, shoulder, surgical; repair of SLAP lesion |
| 29882 | Arthroscopy | 1137 | Arthroscopy, knee, surgical; with meniscus repair (medial OR lateral) |
| 29862 | Arthroscopy | 877 | Arthroscopy, hip, surgical; with debridement/shaving of articular cartilage (chondroplasty), abrasion arthroplasty, and/or resection of labrum |
| 29806 | Arthroscopy | 728 | Arthroscopy, shoulder, surgical; capsulorrhaphy |
| 29846 | Arthroscopy | 710 | Arthroscopy, wrist, surgical; excision and/or repair of triangular fibrocartilage and/or joint debridement |
| 29873 | Arthroscopy | 590 | Arthroscopy, knee, surgical; with lateral release |
| 29874 | Arthroscopy | 483 | Arthroscopy, knee, surgical; for removal of loose body or foreign body |
| 29825 | Arthroscopy | 352 | Arthroscopy, shoulder, surgical; with lysis and resection of adhesions, with or without manipulation |
| 29870 | Arthroscopy | 271 | Arthroscopy, knee, diagnostic, with or without synovial biopsy (separate procedure) |
| 29884 | Arthroscopy | 203 | Arthroscopy, knee, surgical; with lysis of adhesions, with or without manipulation (separate procedure) |
| 29820 | Arthroscopy | 175 | Arthroscopy, shoulder, surgical; synovectomy, partial |
| 29838 | Arthroscopy | 134 | Arthroscopy, elbow, surgical; debridement, extensive |
| 29883 | Arthroscopy | 131 | Arthroscopy, knee, surgical; with meniscus repair (medial AND lateral) |
| 29819 | Arthroscopy | 126 | Arthroscopy, shoulder, surgical; with removal of loose body or foreign body |
| 29834 | Arthroscopy | 109 | Arthroscopy, elbow, surgical; with removal of loose body or foreign body |
| 29821 | Arthroscopy | 100 | Arthroscopy, shoulder, surgical; synovectomy, complete |
| 29837 | Arthroscopy | 65 | Arthroscopy, elbow, surgical; debridement, limited |
| 29871 | Arthroscopy | 33 | Arthroscopy, knee, surgical; for infection, lavage and drainage |
| 29835 | Arthroscopy | 29 | Arthroscopy, elbow, surgical; synovectomy, partial |
| 29805 | Arthroscopy | 25 | Arthroscopy, shoulder, diagnostic, with or without synovial biopsy (separate procedure) |
| 29836 | Arthroscopy | 19 | Arthroscopy, elbow, surgical; synovectomy, complete |
| 29886 | Arthroscopy | 18 | Arthroscopy, knee, surgical; drilling for intact osteochondritis dissecans lesion |
| 29830 | Arthroscopy | 17 | Arthroscopy, elbow, diagnostic, with or without synovial biopsy (separate procedure) |
| 29887 | Arthroscopy | 13 | Arthroscopy, knee, surgical; drilling for intact osteochondritis dissecans lesion with internal fixation |
| 29885 | Arthroscopy | 10 | Arthroscopy, knee, surgical; drilling for osteochondritis dissecans with bone grafting, with or without internal fixation |
| 29888 | Arthroscopy | 3 | Arthroscopically aided anterior cruciate ligament repair/augmentation or reconstruction |
| 29827 | Arthroscopy | 2 | Arthroscopy, shoulder, surgical; with rotator cuff repair |
| 23044 | Arthroscopy | 1 | Arthrotomy, acromioclavicular, sternoclavicular joint, including exploration, drainage, or removal of foreign body |
| 27427 | Arthroscopy | 1 | Ligamentous reconstruction (augmentation), knee; extra-articular |
| 29840 | Arthroscopy | 1 | Arthroscopy, wrist, diagnostic, with or without synovial biopsy (separate procedure) |
| 29844 | Arthroscopy | 1 | Arthroscopy, wrist, surgical; synovectomy, partial |
| 29860 | Arthroscopy | 1 | Arthroscopy, hip, diagnostic with or without synovial biopsy (separate procedure) |
| 29999 | Arthroscopy | 1 | Unlisted procedure, arthroscopy |
| 66984 | Cataract | 22,596 | Extracapsular cataract removal with insertion of intraocular lens prosthesis (1 stage procedure) |
| 66982 | Cataract | 961 | Extracapsular cataract removal with insertion of intraocular lens prosthesis (one stage procedure), complex |
| 66983 | Cataract | 17 | Intracapsular cataract extraction with insertion of intraocular lens prosthesis (1 stage procedure) |
| 45378 | Colonoscopy | 127,894 | Colonoscopy, flexible, proximal to splenic flexure; diagnostic, with or without collection of specimen(s) by brushing or washing |
| 45380 | Colonoscopy | 98,483 | Colonoscopy, flexible, proximal to splenic flexure; with biopsy, single or multiple |
| 45385 | Colonoscopy | 40,062 | Colonoscopy, flexible, proximal to splenic flexure; with removal of tumor(s), polyp(s), or other lesion(s) by snare technique |
| 45384 | Colonoscopy | 9757 | Colonoscopy, flexible, proximal to splenic flexure; with removal of tumor(s), polyp(s), or other lesion(s) |
| 45383 | Colonoscopy | 3442 | Colonoscopy, flexible, proximal to splenic flexure; with ablation of tumor(s), polyp(s), or other lesion(s) |
| 45381 | Colonoscopy | 2101 | Colonoscopy, flexible, proximal to splenic flexure; with directed submucosal injection(s), any substance |
| 45382 | Colonoscopy | 335 | Colonoscopy, flexible, proximal to splenic flexure; with control of bleeding |
| 45386 | Colonoscopy | 154 | Colonoscopy, flexible, proximal to splenic flexure; with dilation by balloon, 1 or more strictures |
| 45391 | Colonoscopy | 95 | Colonoscopy, flexible, proximal to splenic flexure; with endoscopic ultrasound examination |
| 45379 | Colonoscopy | 61 | Colonoscopy, flexible, proximal to splenic flexure; with removal of foreign body |
| 44389 | Colonoscopy | 60 | Colonoscopy through stoma; with biopsy, single or multiple |
| 44394 | Colonoscopy | 37 | Colonoscopy through stoma; with removal of tumor(s), polyp(s), or other lesion(s) by snare technique |
| 45392 | Colonoscopy | 27 | Colonoscopy, flexible, proximal to splenic flexure; with transendoscopic ultrasound guided intramural aspiration/biopsy(s) |
| 45387 | Colonoscopy | 22 | Colonoscopy, flexible, proximal to splenic flexure; with transendoscopic stent placement (includes predilation) |
| 44392 | Colonoscopy | 12 | Colonoscopy through stoma; with removal of tumor(s), polyp(s), or other lesion(s) by hot biopsy forceps or bipolar cautery |
| 45355 | Colonoscopy | 6 | Colonoscopy, rigid or flexible, transabdominal via colotomy, single or multiple |
| 44393 | Colonoscopy | 4 | Colonoscopy through stoma; with ablation of tumor(s), polyp(s), or other lesion(s) |
| 44391 | Colonoscopy | 2 | Colonoscopy through stoma; with control of bleeding |
Table A.2.
Provider price responses to reference pricing: parallel trends.
| Arthroscopy | Cataract | Colonoscopy | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
| ASC | HOPD | ASC | HOPD | ASC | HOPD | |
|
| ||||||
| 2010 × ln(CalPERS exposure) | −0.00423 | 0.00644 | 0.0163 | 0.0148 | −0.00307 | 0.0244 |
| (0.0133) | (0.0154) | (0.0183) | (0.0162) | (0.0122) | (0.0241) | |
| 2011 × ln(CalPERS exposure) | 0.00527 | 0.0191 | −0.00166 | −0.0123 | 0.000433 | 0.00115 |
| (0.0228) | (0.0190) | (0.0323) | (0.0171) | (0.0192) | (0.0170) | |
| 2012 × ln(CalPERS exposure) | 0.00219 | −0.00128 | −0.0234 | −0.00153 | −0.0323 | −0.0231 |
| (0.0295) | (0.0329) | (0.0355) | (0.0184) | (0.0279) | (0.0174) | |
| 2010 × ln(CalPERS exposure) | −0.0467 | −0.00154 | −0.0914 | −0.0207 | −0.0505* | −0.000363 |
| (0.0624) | (0.0374) | (0.0628) | (0.0248) | (0.0291) | (0.0248) | |
| Observations | 46,696 | 21,880 | 20,065 | 5845 | 224,469 | 86,586 |
| Number of providers | 325 | 246 | 239 | 158 | 414 | 275 |
| Number of markets | 108 | 108 | 110 | 79 | 117 | 114 |
| Adjusted R2 | 0.259 | 0.211 | 0.189 | 0.283 | 0.256 | 0.177 |
This table presents the results from Eq. (1) and estimates provider price responses to the CalPERS reference pricing program. The odd-numbered columns restrict the sample to ASC providers and the even-numbered columns restrict the sample to HOPD providers. The dependent variable in all columns is ln(priceijtk) and each regression is estimated using OLS. Controls for month, patient age, gender, Charlson comorbidity score, indicators for 17 chronic conditions, and patient HRR fixed effects are included but not reported. Robust standard errors clustered at the Hospital Service Area level are in parentheses.
p < 0.01.
p < 0.05.
p < 0.1.
Table A.3.
Provider price responses to reference pricing: parallel trends.
| Arthroscopy | Cataract | Colonoscopy | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
| ASC | HOPD | ASC | HOPD | ASC | HOPD | |
|
| ||||||
| 2010 × ln(CalPERS exposure) above | −0.0313 | −0.0137 | 0.0557 | −0.225*** | −0.00402 | −0.0804 |
| (0.0301) | (0.0198) | (0.0387) | (0.0445) | (0.0161) | (0.0849) | |
| 2011 × ln(CalPERS exposure) above | −0.0188 | −0.0269 | 0.0749 | −0.334*** | −0.00542 | −0.0697 |
| (0.0275) | (0.0349) | (0.0640) | (0.0464) | (0.0191) | (0.120) | |
| 2012 × ln(CalPERS exposure) above | −0.0998* | −0.0250 | 0.112* | −0.780*** | 0.0305 | −0.152 |
| (0.0569) | (0.0410) | (0.0649) | (0.0924) | (0.0395) | (0.162) | |
| 2010 × ln(CalPERS exposure) above | −0.238*** | −0.0269 | 0.165 | −0.745*** | 0.0534 | −0.496*** |
| (0.0415) | (0.0540) | (0.117) | (0.0532) | (0.0383) | (0.171) | |
| Observations | 32,392 | 19,184 | 17,568 | 5146 | 175,453 | 81,672 |
| Number of providers | 123 | 158 | 122 | 75 | 182 | 185 |
| Number of markets | 74 | 80 | 83 | 40 | 98 | 95 |
| Adjusted R2 | 0.203 | 0.220 | 0.078 | 0.261 | 0.108 | 0.175 |
This table presents the results from Eq. (1) and estimates provider price responses to the CalPERS reference pricing program. The odd-numbered columns restrict the sample to ASC providers and the even-numbered columns restrict the sample to HOPD providers. The dependent variable in all columns is ln(priceijtk) and each regression is estimated using OLS. Controls for month, patient age, gender, Charlson comorbidity score, indicators for 17 chronic conditions, and patient HRR fixed effects are included but not reported. Robust standard errors clustered at the Hospital Service Area level are in parentheses.
p < 0.01.
p < 0.05.
p < 0.1.
A.5.3. CalPERS population relative to entire insured population
Our main results define market-level exposure to CalPERS as the share of CalPERS enrollees to the commercially insured population in each market. As a robustness test, we include Medicaid and Medicare enrollment in the denominator population, and thus define CalPERS exposure as CalPERS enrollment relative to the entire insured population. We do not use these results in our main results because providers likely respond to demand changes among the commercially insured population differently than the Medicaid or Medicare populations. As shown in Table A.9, the results are similar to our main results. The elasticity estimate for cataract surgery is slightly larger than in the main results, while the colonoscopy ASC result is similar in magnitude, but is not as precisely estimated.
A.6. Differences by market structure
We next consider differential impacts based on market structure. To do so, we calculate the Herfindahl-Hirschman Index (HHI) for each Hospital Referral Region (HRR) and procedure. We follow the FTC guidelines and classify markets with an HHI above 0.25 as concentrated markets. The distribution of HHIs for each service are shown in Fig. A.2. To test for differences in provider price responses between concentrated and competitive markets, we then estimate a triple-differences regression that interacts CalPERS exposure with an indicator for concentrated markets. As shown in Table A.10, we do not find consistent evidence that the effects differ between concentrated and non-concentrated markets.
Table A.4.
Provider price responses to reference pricing: full insured population denominator.
| Arthroscopy | Cataract | Colonoscopy | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
| ASC | HOPD | ASC | HOPD | ASC | HOPD | |
|
| ||||||
| Post × ln(CalPERS exposure) | −0.0148 | −0.00445 | −0.0467* | −0.0178 | −0.0339** | −0.0251 |
| (0.0302) | (0.0188) | (0.0268) | (0.0156) | (0.0171) | (0.0210) | |
| 2010 | −0.00835 | 0.0524*** | 0.0129 | 0.0679*** | −0.0527*** | 0.0345*** |
| (0.0116) | (0.00852) | (0.0102) | (0.0104) | (0.00782) | (0.00940) | |
| 2011 | 0.0602*** | 0.109*** | 0.0398** | 0.130*** | −0.0289*** | 0.0895*** |
| (0.0153) | (0.0106) | (0.0187) | (0.00916) | (0.0107) | (0.0119) | |
| 2012 | 0.0997*** | 0.179*** | 0.0871*** | 0.187*** | 0.0511* | 0.176*** |
| (0.0312) | (0.0234) | (0.0295) | (0.0165) | (0.0261) | (0.0206) | |
| 2013 | 0.139*** | 0.222*** | 0.124** | 0.240*** | 0.0804*** | 0.198*** |
| (0.0278) | (0.0245) | (0.0483) | (0.0196) | (0.0282) | (0.0236) | |
| Observations | 46,696 | 21,880 | 20,065 | 5845 | 224,469 | 86,586 |
| Number of providers | 325 | 246 | 239 | 158 | 414 | 275 |
| Number of markets | 108 | 108 | 110 | 79 | 117 | 114 |
| Adjusted R2 | 0.258 | 0.229 | 0.150 | 0.236 | 0.238 | 0.181 |
| Mean total (facility + professional) | 9246 | 9508 | 3250 | 7671 | 2380 | 3359 |
This table presents the results from Eq. (1) but uses the log-transformed combined facility and in professional fees as the dependent variable. The odd-numbered columns restrict the sample to ASC providers and the even-numbered columns restrict the sample to HOPD providers. The dependent variable in all columns is the log of each procedure’s professional fee. Each regression is estimated using OLS. Controls for month, patient age, gender, Charlson comorbidity score, indicators for 17 chronic conditions, and patient HRR fixed effects are included but not reported. Robust standard errors clustered at the Hospital Service Area level are in parentheses.
p < 0.01.
p < 0.05.
p < 0.1.
Table A.5.
Provider price responses to reference pricing: full insured population denominator.
| Hip-shoulder | Knee-wrist | |||
|---|---|---|---|---|
|
|
|
|||
| (1) | (2) | (3) | (4) | |
| ASC | HOPD | ASC | HOPD | |
|
| ||||
| Post × ln(CalPERS exposure) | −0.00648 | −0.0146 | −0.0512* | −0.0115 |
| (0.0406) | (0.0240) | (0.0296) | (0.0236) | |
| 2010 | 0.0101 | 0.0766*** | 0.0198 | 0.103*** |
| (0.0146) | (0.0132) | (0.0133) | (0.0103) | |
| 2011 | 0.118*** | 0.142*** | 0.0897*** | 0.165*** |
| (0.0199) | (0.0116) | (0.0192) | (0.0143) | |
| 2012 | 0.118*** | 0.219*** | 0.210*** | 0.250*** |
| (0.0365) | (0.0298) | (0.0368) | (0.0331) | |
| 2013 | 0.159*** | 0.265*** | 0.237*** | 0.282*** |
| (0.0342) | (0.0322) | (0.0327) | (0.0344) | |
| Observations | 31,990 | 14,576 | 14,706 | 7304 |
| Number of providers | 317 | 241 | 273 | 208 |
| Number of markets | 107 | 107 | 102 | 92 |
| Adjusted R2 | 0.199 | 0.178 | 0.211 | 0.162 |
| Mean price | 3944 | 3944 | 5421 | 5421 |
This table presentsthe results from the sensitivity test that disaggregates the arthroscopy services. Columns 1–2 show results for hip and shoulder arthroscopy and columns 3–4 show results for knee and wrist arthroscopy. The odd-numbered columns restrict the sample to ASC providers and the even-numbered columns restrict the sample to HOPD providers. The dependent variable in all columns is the log of each procedure’s professional fee. Each regression is estimated using OLS. Controls for month, patient age, gender, Charlson comorbidity score, indicators for 17 chronic conditions, and patient HRR fixed effects are included but not reported. Robust standard errors clustered at the Hospital Service Area level are in parentheses.
p < 0.01.
p < 0.05.
p < 0.1.
A.7. Professional provider fixed effects
As mentioned in Section 5.3, surgical procedures commonly include a facility fee, which is designed to cover the hospital’s expenses, and a professional fee, which is designed to cover the physician’s expenses. Because the reference price applies to only the facility fee, our main specification includes fixed effects for just the facility. However, many physicians perform procedures at multiple facilities. On average, each professional provider identifier is associated with 1.9 facility identifiers for arthroscopy, 1.5 for cataract surgery, and 2.1 for colonoscopy. As an additional test, we estimate a model that includes fixed effects for both the facility and provider identifiers. As shown in Table A.11, including the professional provider fixed effects does not substantially change the results from our main specification.
A.8. Provider entry
One additional alternative explanation is that the CalPERS program induces provider entry. As a test of this explanation, we estimate if increased exposure to the CalPERS program is associated with provider entry. We define entry as the first year (beyond 2009) that a provider has non-zero patient volume. As shown in Table A.12, we find no relationship between exposure to CalPERS and provider entry.
Table A.6.
Provider price responses to reference pricing: full insured population denominator.
| Arthroscopy | Cataract | Colonoscopy | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
| ASC | HOPD | ASC | HOPD | ASC | HOPD | |
|
| ||||||
| Post × ln(CalPERS exposure) | −0.0182 | −0.0101 | −0.0677* | −0.0104 | −0.0444* | −0.0197 |
| (0.0355) | (0.0260) | (0.0374) | (0.0144) | (0.0244) | (0.0204) | |
| 2010 | 0.0163 | 0.0895*** | 0.00784 | 0.0934*** | 0.0235*** | 0.0737*** |
| (0.0123) | (0.00921) | (0.0122) | (0.00924) | (0.00741) | (0.00954) | |
| 2011 | 0.111*** | 0.156*** | 0.0367* | 0.160*** | 0.0604*** | 0.139*** |
| (0.0177) | (0.0119) | (0.0212) | (0.00994) | (0.0110) | (0.0121) | |
| 2012 | 0.147*** | 0.239*** | 0.104** | 0.218*** | 0.155*** | 0.228*** |
| (0.0341) | (0.0340) | (0.0398) | (0.0171) | (0.0315) | (0.0187) | |
| 2013 | 0.186*** | 0.277*** | 0.156** | 0.274*** | 0.194*** | 0.247*** |
| (0.0317) | (0.0350) | (0.0676) | (0.0208) | (0.0323) | (0.0230) | |
| Observations | 41,818 | 19,508 | 17,145 | 5019 | 197,988 | 75,896 |
| Number of providers | 321 | 244 | 238 | 153 | 411 | 273 |
| Number of markets | 107 | 108 | 110 | 78 | 117 | 113 |
| Adjusted R2 | 0.252 | 0.209 | 0.192 | 0.282 | 0.252 | 0.177 |
This table presents the results from Eq. (1) but restricts the population to the non-CalPERS Anthem PPO control population. The odd-numbered columns restrict the sample to ASC providers and the even-numbered columns restrict the sample to HOPD providers. The dependent variable in all columns is the log of each procedure’s professional fee. Each regression is estimated using OLS. Controls for month, patient age, gender, Charlson comorbidity score, indicators for 17 chronic conditions, and patient HRR fixed effects are included but not reported. Robust standard errors clustered at the Hospital Service Area level are in parentheses.
p < 0.01.
p < 0.05.
p < 0.1.
Table A.7.
Provider price responses to reference pricing: level CalPERS exposure.
| Arthroscopy | Cataract | Colonoscopy | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
| ASC | HOPD | ASC | HOPD | ASC | HOPD | |
|
| ||||||
| Post × CalPERS exposure | −1.111 | −0.153 | −1.156* | −0.348 | −0.701** | −0.303 |
| (0.677) | (0.485) | (0.662) | (0.433) | (0.331) | (0.423) | |
| 2010 | 0.0159 | 0.0843*** | 0.0140 | 0.0895*** | 0.0237*** | 0.0744*** |
| (0.0126) | (0.00880) | (0.0129) | (0.00855) | (0.00720) | (0.0101) | |
| 2011 | 0.111*** | 0.152*** | 0.0422* | 0.160*** | 0.0578*** | 0.140*** |
| (0.0177) | (0.0107) | (0.0245) | (0.0106) | (0.0109) | (0.0125) | |
| 2012 | 0.155*** | 0.225*** | 0.0781** | 0.211*** | 0.133*** | 0.218*** |
| (0.0266) | (0.0239) | (0.0299) | (0.0141) | (0.0226) | (0.0152) | |
| 2013 | 0.193*** | 0.268*** | 0.126** | 0.270*** | 0.170*** | 0.238*** |
| (0.0275) | (0.0258) | (0.0556) | (0.0177) | (0.0243) | (0.0198) | |
| Observations | 46,696 | 21,880 | 20,065 | 5845 | 224,469 | 86,586 |
| Number of providers | 325 | 246 | 239 | 158 | 414 | 275 |
| Number of markets | 108 | 108 | 110 | 79 | 117 | 114 |
| Adjusted R2 | 0.259 | 0.211 | 0.183 | 0.283 | 0.255 | 0.177 |
This table presents the results from Eq. (1) and estimates provider price responses to the CalPERS reference pricing program. The odd-numbered columns restrict the sample to ASC providers and the even-numbered columns restrict the sample to HOPD providers. The dependent variable in all columns is ln(priceijtk) and each regression is estimated using OLS. Controls for month, patient age, gender, Charlson comorbidity score, indicators for 17 chronic conditions, and patient HRR fixed effects are included but not reported. Robust standard errors clustered at the Hospital Service Area level are in parentheses.
p < 0.01.
p < 0.05.
p < 0.1.
Table A.8.
Provider price responses to reference pricing: top quartile vs. bottom quartile.
| Arthroscopy | Cataract | Colonoscopy | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
| ASC | HOPD | ASC | HOPD | ASC | HOPD | |
|
| ||||||
| Post × top quartile CalPERS exposure | −0.0128 | −0.00205 | −0.127 | −0.0255 | −0.0904* | −0.0152 |
| (0.0491) | (0.0405) | (0.0764) | (0.0196) | (0.0455) | (0.0249) | |
| 2010 | 0.0291*** | 0.0783*** | 0.0270* | 0.0895*** | 0.0272** | 0.0868*** |
| (0.00933) | (0.0141) | (0.0141) | (0.00898) | (0.0115) | (0.0138) | |
| 2011 | 0.104*** | 0.149*** | 0.0377* | 0.170*** | 0.0791*** | 0.158*** |
| (0.0179) | (0.0123) | (0.0222) | (0.00706) | (0.0189) | (0.00757) | |
| 2012 | 0.103*** | 0.226*** | 0.0819* | 0.216*** | 0.189*** | 0.233*** |
| (0.0182) | (0.0364) | (0.0438) | (0.0148) | (0.0423) | (0.0155) | |
| 2013 | 0.106*** | 0.277*** | 0.157 | 0.258*** | 0.230*** | 0.255*** |
| (0.0189) | (0.0354) | (0.102) | (0.0173) | (0.0365) | (0.0218) | |
| Observations | 22,224 | 13,262 | 10,621 | 3186 | 94,068 | 55,155 |
| Number of providers | 151 | 151 | 111 | 95 | 195 | 166 |
| Number of markets | 48 | 54 | 53 | 38 | 49 | 58 |
| Adjusted R2 | 0.210 | 0.226 | 0.087 | 0.264 | 0.243 | 0.191 |
| Mean price | 4409 | 7893 | 1882 | 6560 | 1067 | 2772 |
This table presents the results from Eq. (1) and estimates provider price responses to the CalPERS reference pricing program, but compares price trends between markets in the top quartile of exposure to CalPERS (2.1%) to markets in the bottom quartile (0.5%). The odd-numbered columns restrict the sample to ASC providers and the even-numbered columns restrict the sample to HOPD providers. The dependent variable in all columns is ln(priceijtk) and each regression is estimated using OLS. Controls for month, patient age, gender, Charlson comorbidity score, indicators for 17 chronic conditions, and patient HRR fixed effects are included but not reported. Robust standard errors clustered at the Hospital Service Area level are in parentheses.
p < 0.01.
p < 0.05.
p < 0.1.
Table A.9.
Provider price responses to reference pricing: full insured population denominator.
| Arthroscopy | Cataract | Colonoscopy | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
| ASC | HOPD | ASC | HOPD | ASC | HOPD | |
|
| ||||||
| Post × ln(CalPERS exposure) | −0.0251 | −0.0135 | −0.0733* | −0.0112 | −0.0403 | −0.0203 |
| (0.0474) | (0.0302) | (0.0427) | (0.0170) | (0.0265) | (0.0236) | |
| 2010 | 0.0156 | 0.0843*** | 0.0141 | 0.0895*** | 0.0237*** | 0.0744*** |
| (0.0126) | (0.00881) | (0.0129) | (0.00854) | (0.00722) | (0.0101) | |
| 2011 | 0.111*** | 0.152*** | 0.0421* | 0.160*** | 0.0579*** | 0.140*** |
| (0.0177) | (0.0107) | (0.0245) | (0.0105) | (0.0109) | (0.0125) | |
| 2012 | 0.148*** | 0.230*** | 0.0986*** | 0.212*** | 0.143*** | 0.224*** |
| (0.0327) | (0.0295) | (0.0367) | (0.0153) | (0.0278) | (0.0168) | |
| 2013 | 0.186*** | 0.272*** | 0.146** | 0.271*** | 0.181*** | 0.244*** |
| (0.0297) | (0.0310) | (0.0639) | (0.0187) | (0.0287) | (0.0210) | |
| Observations | 46,696 | 21,874 | 20,062 | 5836 | 224,469 | 86,585 |
| Number of providers | 325 | 242 | 238 | 153 | 414 | 274 |
| Number of markets | 108 | 104 | 109 | 74 | 117 | 113 |
| Adjusted R2 | 0.259 | 0.211 | 0.184 | 0.283 | 0.255 | 0.177 |
| Mean price | 4409 | 7894 | 1882 | 6559 | 1067 | 2772 |
This table presents the results from Eq. (1) and estimates provider price responses to the CalPERS reference pricing program, but measures CalPERS exposure relative to the entire insured population (commercially insured, Medicare, and Medicaid). The odd-numbered columns restrict the sample to ASC providers and the even-numbered columns restrict the sample to HOPD providers. The dependent variable inall columns is ln(priceijtk) and each regression is estimated using OLS. Controls for month, patient age, gender, Charlson comorbidity score, indicators for 17 chronic conditions, and patient HRR fixed effects are included but not reported. Robust standard errors clustered at the Hospital Service Area level are in parentheses.
p < 0.01.
p < 0.05.
p < 0.1.
Table A.10.
Provider price responses to reference pricing: differences by market structure.
| Arthroscopy | Cataract | Colonoscopy | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
| ASC | HOPD | ASC | HOPD | ASC | HOPD | |
|
| ||||||
| Post × ln(CalPERS) | 0.163*** | −0.00229 | 0.0178 | −0.0346 | −0.0530 | −0.0199 |
| (0.0586) | (0.0346) | (0.0374) | (0.0216) | (0.0684) | (0.0250) | |
| Post × concentrated | 0.166** | 0.0203 | 0.173 | −0.0743 | −0.0164 | 0.0266 |
| (0.0736) | (0.0490) | (0.140) | (0.0675) | (0.0506) | (0.0935) | |
| Post × ln(CalPERS) × concentrated | −0.233*** | −0.0224 | −0.138 | 0.0710 | 0.0193 | −0.0130 |
| (0.0730) | (0.0440) | (0.0840) | (0.0478) | (0.0696) | (0.0581) | |
| Observations | 46,696 | 21,874 | 20,062 | 5836 | 224,469 | 86,585 |
| Number of providers | 325 | 242 | 238 | 153 | 414 | 274 |
| Number of markets | 108 | 104 | 109 | 74 | 117 | 113 |
| Adjusted R2 | 0.261 | 0.211 | 0.194 | 0.285 | 0.256 | 0.177 |
Table A.11.
Provider price responses to reference pricing: professional provider fixed effects.
| Arthroscopy | Cataract | Colonoscopy | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
| ASC | HOPD | ASC | HOPD | ASC | HOPD | |
|
| ||||||
| Post × ln(CalPERS exposure) | −0.00925 | −0.0105 | −0.0704* | −0.00905 | −0.0399* | −0.0258 |
| (0.0282) | (0.0250) | (0.0386) | (0.0164) | (0.0214) | (0.0191) | |
| 2010 | 0.0164 | 0.0843*** | 0.0164 | 0.0929*** | 0.0253*** | 0.0724*** |
| (0.0132) | (0.00913) | (0.0133) | (0.00889) | (0.00728) | (0.0101) | |
| 2011 | 0.112*** | 0.154*** | 0.0452* | 0.166*** | 0.0599*** | 0.143*** |
| (0.0109) | (0.0257) | (0.0122) | (0.0112) | (0.0118) | (0.0185) | |
| 2012 | 0.142*** | 0.234*** | 0.119*** | 0.214*** | 0.155*** | 0.238*** |
| (0.0313) | (0.0452) | (0.0207) | (0.0307) | (0.0184) | (0.0318) | |
| 2013 | 0.190*** | 0.274*** | 0.171** | 0.274*** | 0.194*** | 0.259*** |
| (0.0327) | (0.0765) | (0.0241) | (0.0319) | (0.0254) | (0.0329) | |
| Observations | 46,696 | 21,874 | 20,062 | 5836 | 224,469 | 86,583 |
| Number of facilities | 325 | 242 | 238 | 153 | 414 | 275 |
| Number of physicians | 1016 | 988 | 713 | 494 | 1177 | 1180 |
| Number of markets | 108 | 104 | 109 | 74 | 117 | 108 |
| Adjusted R2 | 0.813 | 0.763 | 0.895 | 0.883 | 0.906 | 0.810 |
| Mean price | 4409 | 7894 | 1882 | 6559 | 1067 | 2772 |
Table A.12.
Provider price responses to reference pricing: provider entry.
| Arthroscopy | Cataract | Colonoscopy | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
| ASC | HOPD | ASC | HOPD | ASC | HOPD | |
|
| ||||||
| Post × ln(CalPERS exposure) | −0.0180 | −0.00235 | 0.00160 | −0.0401 | −0.00212 | 0.0640 |
| (0.0326) | (0.0206) | (0.0196) | (0.0408) | (0.0526) | (0.0441) | |
| Observations | 1625 | 1230 | 1195 | 790 | 2070 | 1375 |
| Number of providers | 325 | 246 | 239 | 158 | 414 | 275 |
| Number of markets | 108 | 108 | 110 | 79 | 117 | 114 |
| Adjusted R2 | 0.056 | 0.017 | 0.031 | 0.042 | 0.033 | 0.015 |
Fig. A.1.
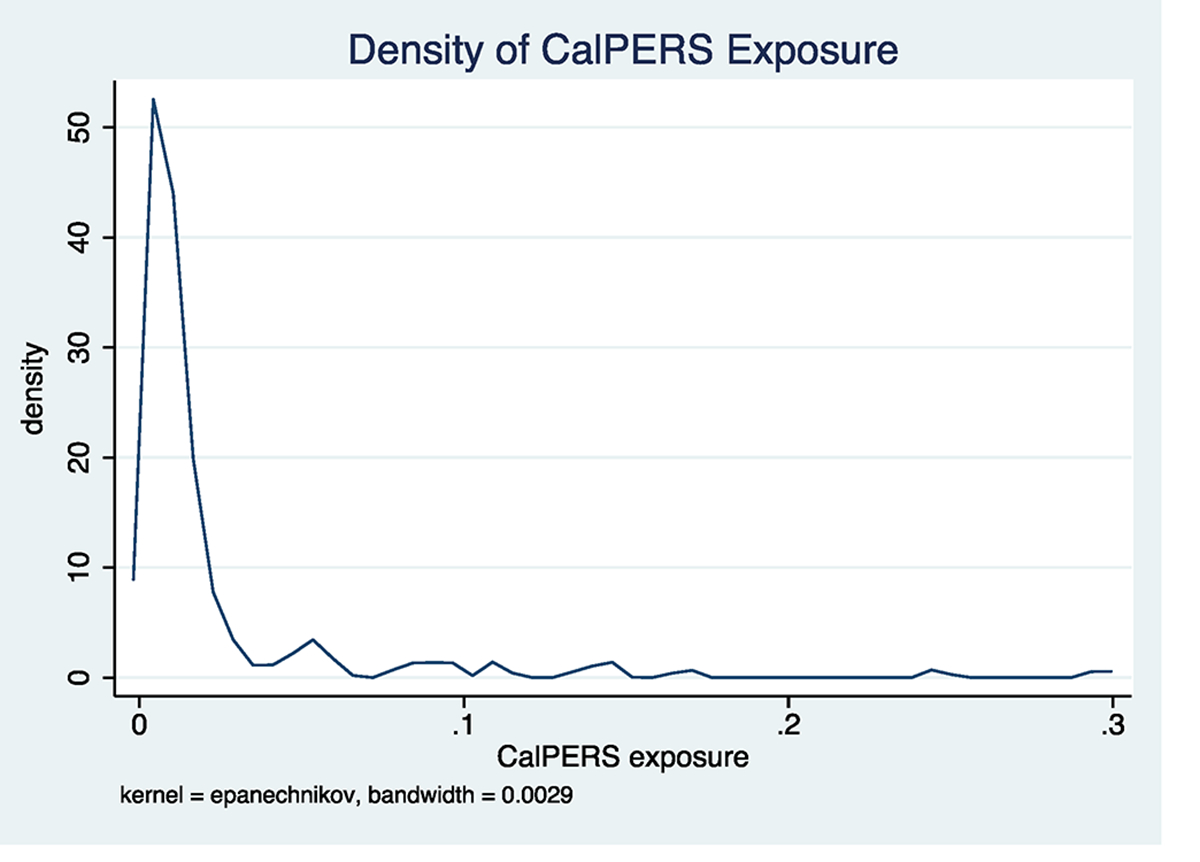
Distribution of CalPERS exposure.
Fig. A.2.

HHI distribution.
Appendix B. Contemporaneous shocks
Our empirical model assumes that no programs that potentially impact provider prices were implemented at the same time as the launch of the CalPERS reference pricing program. While we are not aware of any such program, to test for potential contemporaneous shocks, we use examine if exposure to the program is correlated with other programs that may plausibly impact the delivery system. To do so, we examine the changes in outcomes for Medicare patients and economic conditions listed in Table B.1.
For each outcome, we estimate the following difference-in-differences regression:
As in the main results, we use the log of each dependent variable so that each outcome can be interpreted as an elasticity.
Fig. B.1 presents the interaction coefficient of interest for each outcome. We find a small reduction in the share of Medicare enrollees with ambulatory visit to primary care physician. More notably, we also find a relatively strong increase in the unemployment rate. Our results imply that every 10% increase in exposure to CalPERS is associated with a 3.1% increase in the unemployment rate.
The link between the unemployment rate and exposure to CalPERS is consistent with labor market trends in California during this time period. Much of the economic growth has occurred in the large metropolitan areas – Los Angeles, San Francisco, and San Diego – where CalPERS constitutes a smaller share of the population. However, if changes in unemployment counter-cyclically influence provider prices, then this paper’s conclusion that the CalPERS reference pricing program leads to changes in ASC prices may be incorrect.
Table B.1.
Contemporaneous shocks data sources.
| Outcome | Data Source | Years | Market-Level |
|---|---|---|---|
|
| |||
| Age, sex, and race-adjusted Medicare per-enrollee spending | Dartmouth Atlas | 2009–2013 | HSA |
| Age, sex, and race-adjusted Medicare mortality rate | Dartmouth Atlas | 2009–2013 | HRR |
| Monthly unemployment rate | BLS | 2009–2013 | County |
| Share of Medicare enrollees with ambulatory visit to primary care physician | Dartmouth Atlas | 2009–2013 | HSA |
| Share of diabetic Medicare enrollees with HbA1c test and eye exam | Dartmouth Atlas | 2009–2013 | HSA |
| Share of Medicare enrollees with knee and hip replacements | Dartmouth Atlas | 2009–2012 | HRR |
Table B.2.
Association between unemployment rate and provider prices.
| Arthroscopy | Cataract | Colonoscopy | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
| ASC | HOPD | ASC | HOPD | ASC | HOPD | |
|
| ||||||
| ln(unemployment rate) | −0.0271 | 0.0392 | −0.0269 | 0.134 | −0.0406 | −0.0471 |
| (0.0590) | (0.0557) | (0.0488) | (0.0982) | (0.0541) | (0.0585) | |
| 2010 | 0.0157 | 0.0826 | 0.0160 | 0.0753 | 0.0136 | 0.0752 |
| (0.0153) | (0.0120) | (0.0131) | (0.0126) | (0.0129) | (0.0108) | |
| 2011 | 0.0385 | 0.150 | 0.0392 | 0.151 | 0.0219 | 0.138 |
| (0.0423) | (0.0117) | (0.0250) | (0.0126) | (0.0209) | (0.00867) | |
| Observations | 23,034 | 12,733 | 10,250 | 3199 | 114,992 | 50,793 |
| Number of providers | 153 | 158 | 130 | 75 | 211 | 185 |
| Number of markets | 84 | 80 | 86 | 40 | 104 | 95 |
| Adjusted R2 | 0.122 | 0.177 | 0.009 | 0.222 | 0.040 | 0.137 |
Fig. B.1.
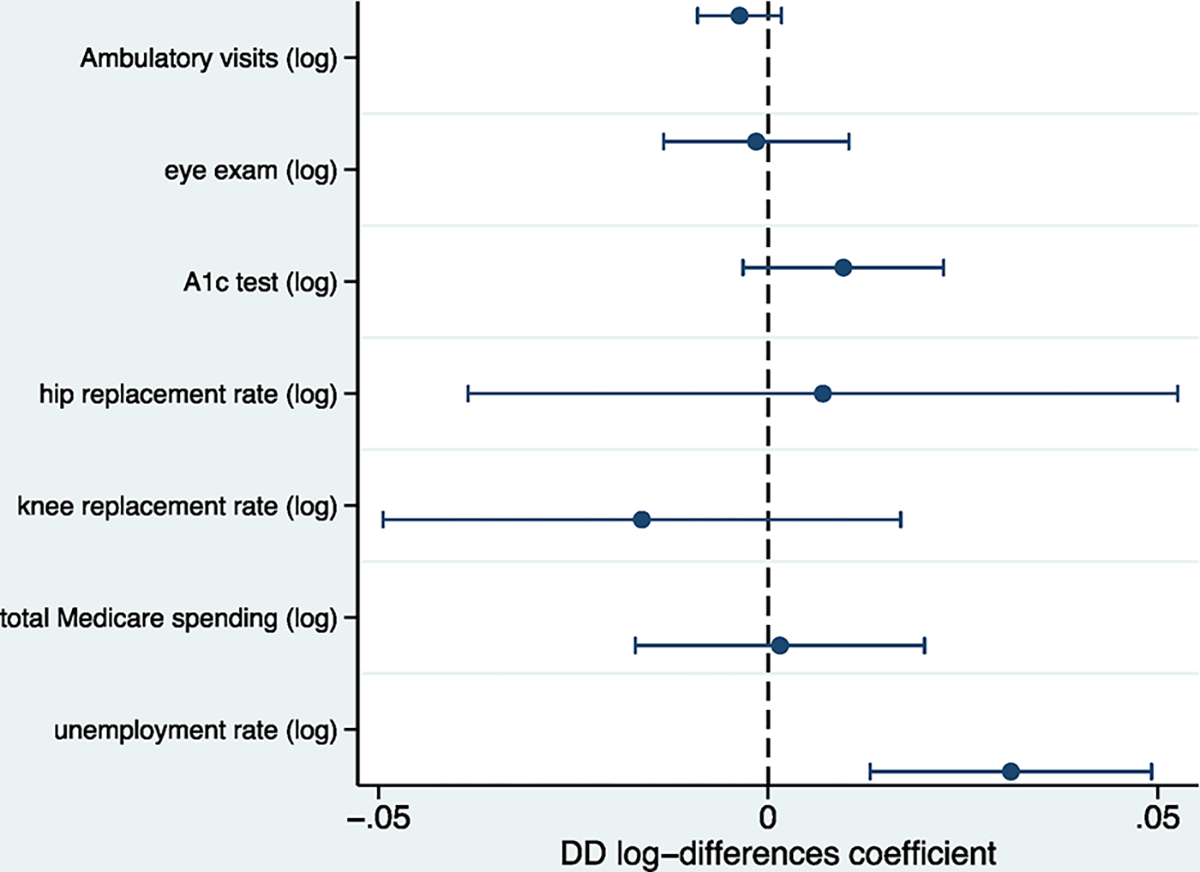
Contemporaneous shocks test.
To further examine this scenario, we test the correlation between the unemployment rate and provider prices. We estimate
To avoid contamination from the reference pricing program, we restrict the sample to the pre-implementation period (2009–2012).
Table B.2 presents these results. We do not find a statistically significant association between unemployment and provider prices. The lack of an association suggests that trends in unemployment rates do not lead to changes in provider prices.
Appendix C. Market segmentation conceptual model
We consider a stylized model of competition between two providers, indexed by , a single HOPD and a single ASC (). For each of the traditional insurance coverage () and reference pricing () time periods, each consumer receives one unit of care but faces the decision of whether to receive care from the ASC or the HOPD. Let consumer utility be given by
| (4) |
In this expression, represents the benefit of the service, captures the patient’s out-of-pocket spending for the service, while represents the benefit of receiving care at a HOPD, which is a function of patient cost sharing. We assume that the value of receiving care at the HOPD is decreasing in out-of-pocket prices, . The , and terms represent patient sensitivity to the benefits of the service, use of the HOPD, and out-of-pocket costs, respectively. Consumer cost sharing is a function of the provider’s price, , the provider type, , and the time period, and is defined as
| (5) |
where is the coinsurance rate and is the reference price. Because and .
We further assume that there are consumers that are equally split between two patient types: the segment that prefers the HOPD but is less price sensitive, the -types, and the price sensitive segment that does not value the HOPD, the -types. More formally, let but and let but . Thus, and . Importantly, providers do not observe each patient’s type.
Differences in patient valuation of HOPDs is a key feature of this model. A consumer of either type will choose the HOPD provider if and only if the benefit of receiving care at the HOPD is greater than the difference in out-of-pocket spending between the HOPD and the ASC:
| (6) |
The market share of the HOPD is thus given by
| (7)(8) |
where is the indicator function. Because there are only two providers and each consumer receives one unit of care, the ASC market share is given by .
Table C.1.
Provider price responses to reference pricing: exposure to CalPERS and consumer demand shifts.
| Arthroscopy | Cataract | Colonoscopy | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
| ASC | HOPD | ASC | HOPD | ASC | HOPD | |
|
| ||||||
| Post × ln(CalPERS exposure) × ΔHOPD | −0.106 | −0.0303 | 0.0234 | 0.0782 | −0.253*** | 0.0135 |
| (0.0873) | (0.0504) | (0.0362) | (0.0546) | (0.0768) | (0.0630) | |
| Post × ΔHOPD | 0.0836 | −0.0171 | −0.0491 | −0.112 | 0.186*** | 0.0117 |
| (0.0625) | (0.0511) | (0.0760) | (0.0865) | (0.0407) | (0.0669) | |
| Post × ln(CalPERS exposure) | −0.0376 | −0.0147 | −0.0628 | 0.00992 | −0.104*** | −0.0181 |
| (0.0363) | (0.0245) | (0.0395) | (0.0255) | (0.0225) | (0.0215) | |
| 2010 | 0.0152 | 0.0844*** | 0.0141 | 0.0891*** | 0.0235*** | 0.0744*** |
| (0.0126) | (0.00881) | (0.0129) | (0.00866) | (0.00719) | (0.0100) | |
| 2011 | 0.111*** | 0.152*** | 0.0421* | 0.159*** | 0.0579*** | 0.140*** |
| (0.0176) | (0.0106) | (0.0244) | (0.0107) | (0.0108) | (0.0125) | |
| 2012 | 0.165*** | 0.228*** | 0.102*** | 0.190*** | 0.190*** | 0.232*** |
| (0.0373) | (0.0311) | (0.0371) | (0.0305) | (0.0264) | (0.0220) | |
| 2013 | 0.203*** | 0.271*** | 0.150** | 0.249*** | 0.228*** | 0.252*** |
| (0.0343) | (0.0319) | (0.0636) | (0.0338) | (0.0274) | (0.0267) | |
| Observations | 46,696 | 21,880 | 20,065 | 5845 | 224,469 | 86,586 |
| Number of providers | 325 | 246 | 239 | 158 | 414 | 275 |
| Number of markets | 108 | 108 | 110 | 79 | 117 | 114 |
| Adjusted R2 | 0.259 | 0.212 | 0.185 | 0.284 | 0.259 | 0.177 |
| Mean price | 4409 | 7893 | 1882 | 6560 | 1067 | 2772 |
This table presents the results from Eq. (13) and estimates provider price responses to the CalPERS reference pricing program based on both the market-level exposure to CalPERS and the market-level change in market shares between HOPDs and ASCs. The odd-numbered columns restrict the sample to ASC providers and the even-numbered columns restrict the sample to HOPD providers. The dependent variable inall columns is ln(priceijtk) and each regression is estimated using OLS. Controls for month, patient age, gender, Charlson comorbidity score, indicators for 17 chronic conditions, and patient HRR fixed effects are included but not reported. Robust standard errors clustered at the Hospital Service Area level are in parentheses.
p < 0.01.
p < 0.05.
p < 0.1.
Because the -types are less price sensitive than the -types, and . In other words, while HOPD market share decreases for both populations, there is a larger decrease in HOPD market share for the price sensitive, -type, population. Correspondingly, the increase in ASC market share for the -type population is larger than the increase for the -type population. More formally, and thus, .
These market shares inform each provider’s profit maximization optimization by entering into both revenues and costs. Each provider faces aggregate patient demand equal to the share of the and -type consumers that receive care at that provider:
| (9) |
The relative composition of the provider’s aggregate demand is important because consumers differ by their price sensitivity. As shown above, the HOPD will have a larger proportion of -type consumers under reference pricing than under traditional coverage, while the ASC will have a larger proportion of -type consumers. Increasing the share of the -type consumers decreases the aggregate price sensitivity facing the provider, while increasing the relative share of -type consumers increases the provider’s average price sensitivity.
If we assume constant marginal costs that are the same for each provider type, and let C denote costs, provider profit is given by
| (10) |
Taking first order conditions gives optimal prices as
| (11) |
For a given provider, the difference in prices in the traditional insurance coverage () and reference pricing () periods can be given by
| (12) |
Applying the above conditions implies that for HOPDs, and . Conversely, for ASCs, and . Thus, and .
Because optimal prices depend on each provider’s market share among each consumer type, increasing the share of -type consumers increases the aggregate price sensitivity faced by the provider while increasing the -type consumers makes the provider’s aggregate demand less price sensitive. Because the reference pricing program shifts a larger share of the -types to ASCs than the types, the reference pricing program increases the relative share of the -types at the ASC and types at the HOPD. Thus, the reference pricing increase equilibrium prices for the HOPD but decreases equilibrium prices for the ASC.
The results of this model suggest that one potential explanation for why price changes are observed only for ASC providers is that the reference pricing program segments the market. If price-sensitive consumers disproportionately respond to the program by switching to from HOPDs to ASCs, then the remaining population that receives care at HOPDs is less price sensitive. In such a case, standard insurer-provider bargaining models detail how lower consumer price sensitivities can lead to changes in negotiated prices (Capps et al., 2003; Ho, 2009; Gowrisankaran et al., 2015).
C.1. Empirical support of market segmentation
As an additional test of the market-segmentation model, we measure the market-level shift in patient demand from HOPDs to ASCs that is induced by the CalPERS programs. For each Hospital Referral Region (HRR) , we calculate the change in HOPD market share as
We separately calculate the change in HOPD market share for each procedure. We then estimate a triple-differences regression that interacts the change in HOPD market share with the post-implementation and CalPERS exposure variables:
| (13) |
As shown in Table C.1, we find that for colonoscopies, which account for 77% of the total procedure volume, the coefficient for ASCs is negative and statistically significant. The coefficient is negative, but not statistically significant for arthroscopy ASCs. We do not find economically or statistically significant coefficients for HOPD providers. These results support the market segmentation hypothesis that an increased consumer shift from HOPDs to ASCs increases price competition among ASCs.
Appendix D. Quality outcomes
We use the following algorithms to identify surgical complications related to each procedure. Complications related to joint arthroscopy are analyzed at both the 30-day and 90-day periods following the index arthroscopy procedure. Complications measured only for 30 days after the procedure will consist of bleeding (ICD-9 codes 998.1, 719.10, 719.16, 719.17, 39.98), post-operative deep vein thrombosis (ICD-9 codes 453.40–453.42, 453.50–453.52, 453.9), and pulmonary embolism (ICD-9 code 415.1). Complications measured for the full 90 days after the procedure will consist of mechanical failure (ICD-9 codes 996.40, 996.4, and 996.49), wound infection 682.1–682.9, 686.9, 998.6, 998.7, 998.83, 998.3, 998.5, 996.66, 996.67 and CPT codes 86.22, 86.28, 86.04, 81.53, 81.55, 81.59, 00.70, 00.71, 00.72, 00.73, 00.80, 00.81, 00.82, 00.84, 80.05, 80.06, 80.09), and postoperative nerve injury (ICD-9 codes 955, 956, 957.8, 957.9).
Complications for cataract surgery are identified following French et al. (2012) by using secondary surgeries as surrogate markers for complications of cataract surgery. Secondary surgeries must be performed within 90 days of the primary cataract surgery and must be separate in time from the primary cataract surgery. Current procedural terminology codes are linked to the site (right or left eye) of cataract surgery through CPT code modifiers, which identify the right and the left eye. The following procedures codes are used: repositioning of IOL (insertion of ocular lens) (66825), removal of IOL (65920), exchange of IOL (66986), repair of wound or iris (66250, 66680, 66682), therapeutic paracentesis of anterior chamber (65805), removal of anterior chamber blood or clot (65815, 65930), re-inflation of anterior chamber (66020), repair of retinal detachment (67101–67110), vitrectomy and related procedures (65810, 67005, 67010, 67015, 67025, 67036, 67039), removal of IOL posterior segment (67121), intravitreal injection (67028), drainage of choroid (67015), anterior orbitotmy (67400), and removal of eye, evisceration, or enucleation (65091, 65093, 65101, 65103, 65105).
Colonoscopy complications are classified as any procedural complication among three categories in the 30-days following the index colonoscopy: cardiovascular, serious gastrointestinal, or non-serious gastrointestinal. Cardiac complications include arrhythmia (427.0–427.4, 427.6–427.9), congestive heart failure (428.0–428.9), cardiac or respiratory arrest (427.5, 799.1, 997.1), and syncope, hypotension, or shock (453.29, 458.8–458.9, 639.5, 780.2, 785.50–785.51, 998.0, 995.4). Serious gastrointestinal complications include perforation (ICD-9 codes 569.83, 998.2), lower gastrointestinal bleeding (ICD-9 codes 558.9, 578.1, 995.2, 995.89, 998.1–998.13, 286.5, 459, 562.02–562.03, 562.12, 562.13, 569.3, 569.84–569.86, 578.9, 792.1), and infection (CPT codes 78066, 790.7, 424.9–424.99). Non-serious gastrointestinal complications include paralytic ileus (560.1), nausea, vomiting, dehydration (276.5, 536.2, 787.0–02), abdominal pain (789.0), diverticulitis (562.01, 562.03, 562.11, and 562.13), and enterocolitis (555–556).
Footnotes
We empirically test and confirm this assumption in Section 5.1.
In this paper, we do not examine knee and hip replacement surgery due to insufficient sample sizes.
Most medical claims for surgical services include a two price components. A price that covers the costs of the facility, the “facility fee,” and a price that covers the costs of the provider, the “professional fee.”
For example, a patient with a 20% coinsurance who receives a colonoscopy at a HOPD with a $2000 price is responsible for 20% × $1500 + ($2000 − $1500) = $800.
For colonoscopy services, a further consideration is the Affordable Care Act’s (ACA) requirement that cancer screening services be offered without patient cost sharing. The US Department of Health and Human Services and the US Department of the Treasury have ruled that reference pricing programs do not violate the ACA’s requirement if appropriately implemented and patients are given access to a sufficient number of facilities below the reference price (Department of Labor, 2014). Thus, CalPERS use of reference pricing for screening colonoscopies is compliant with the ACA.
For knee and hip replacements, which are not covered in this paper due to lack of sample size, the reference pricing program shifts patient volume from high-cost to fully covered providers by 15.0 percentage points, which leads to aper-procedure cost reduction of by 13.2% and a $2.8 million reduction in CalPERS spending (Robinson and Brown, 2013).
We combine hip, knee, shoulder, and wrist arthroscopies into a single procedure but exclude ankle, elbow, and wrist arthroscopies services because few patients receive these services.
Our prices measure the actual negotiated price between the insurer and the provider and not the billed “chargemaster” prices.
Because lies within [0,1], we calculate this as .
In Appendix A.1, we plot the non log-transformed distribution of exposure to the program. While the distribution of exposure varies, it is highly skewed. The regression results are similar when using the non-logged measure of exposure.
References
- Aouad M, Brown TT, Whaley C, 2018a. Quantile Treatment Effects of Reference Pricing. Working Paper. University of California, Berkeley. [Google Scholar]
- Aouad M, Brown T, Whaley C, 2018b. Reference Pricing - The Case of Screening Colonoscopies. Working Paper. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barro JR, Huckman RS, Kessler DP, 2006. The effects of cardiac specialty hospitals on the cost and quality of medical care. J. Health Econ. 25 (4), 702–721. [DOI] [PubMed] [Google Scholar]
- Beeuwkes Buntin M, Haviland AM, McDevitt R, Sood N, 2011. Health-care spending and preventive care in high-deductible and consumer-directed health plans. Am. J. Manag. Care 17 (3), 222–230. [PubMed] [Google Scholar]
- Blume-Kohout ME, Sood N, 2013. Market size and innovation: effects of Medicare part D on pharmaceutical research and development. J. Public Econ. 97 (Jan), 327–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brot-Goldberg ZC, et al. , 2017. What does a deductible do? The impact of cost-sharing on health care prices, quantities, and spending dynamics. Q. J. Econ. 132.3, 1261–1318. [Google Scholar]
- Brown TT, Robinson JC, 2016. Reference pricing with endogenous or exogenous payment limits: impacts on insurer and consumer spending. Health Econ. 25 (6), 740–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buntin MB, Damberg C, Haviland A, Kapur K, Lurie N, McDevitt R, Marquis MS, 2006. Consumer-directed health care: early evidence about effects on cost and quality. Health Aff. 25 (6). [DOI] [PubMed] [Google Scholar]
- Capps C, Dranove D, Satterthwaite M, 2003. Competition and market power in option demand markets. RAND J. Econ. 34 (4), 737–763. [PubMed] [Google Scholar]
- Carey K, Burgess JF Jr., Young GJ, 2011. Hospital competition and financial performance: the effects of ambulatory surgery centers. Health Econ. 20 (5), 571–581. [DOI] [PubMed] [Google Scholar]
- Casalino LP, Devers KJ, Brewster LR, 2003. Focused factories? Physician-owned specialty facilities. Health Aff. 22 (6), 56–67, 00197. [DOI] [PubMed] [Google Scholar]
- Charlson ME, Pompei P, Ales KL, MacKenzie CR, 1987. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J. Chronic Dis. 40 (5), 373–383. [DOI] [PubMed] [Google Scholar]
- Clemens J, Gottlieb JD, 2014. Do physicians’ financial incentives affect medical treatment and patient health? Am. Econ. Rev. 104 (4), 1320–1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtemanche C, Plotzke M, 2010. Does competition from ambulatory surgical centers affect hospital surgical output? J. Health Econ. 29 (5), 765–773. [DOI] [PubMed] [Google Scholar]
- Cromwell J, Mitchell JB, 1986. Physician induced demand for surgery. J. Health Econ. 5 (4), 293–313. [DOI] [PubMed] [Google Scholar]
- Dafny LS, 2005. How do hospitals respond to price changes? Am. Econ. Rev. 95 (5), 1525–1547. [DOI] [PubMed] [Google Scholar]
- Duggan M, Morton FS, 2010. The effect of Medicare part D on pharmaceutical prices and utilization. Am. Econ. Rev. 100 (1), 590–607. [DOI] [PubMed] [Google Scholar]
- Finkelstein A, 2007. The aggregate effects of health insurance: evidence from the introduction of Medicare. Q. J. Econ. 122 (1), 1–37. [Google Scholar]
- Freedman S, Lin H, Simon K, 2015. Public health insurance expansions and hospital technology adoption. J. Public Econ. 121 (Jan), 117–131. [Google Scholar]
- French DD, Margo CE, Campbell RR, 2012. Comparison of complication rates in veterans receiving cataract surgery through the veterans health administration and Medicare. Med. Care 50 (7), 620–626. [DOI] [PubMed] [Google Scholar]
- Frost A, Newman D, Quincy L, 2016. Health care consumerism: can the tail wag the dog? Health Aff. Blog (Mar). [Google Scholar]
- Gowrisankaran G, Nevo A, Town R, 2015. Mergers when prices are negotiated: evidence from the hospital industry. Am. Econ. Rev. 105 (1), 172–203. [Google Scholar]
- Gruber J, McKnight R, 2016. Controlling health care costs through limited network insurance plans: evidence from Massachusetts state employees. Am. Econ. J.: Econ. Policy 8 (2), 219–250. [Google Scholar]
- Gruber J, Owings M, 1996. Physician financial incentives and cesarean section delivery. RAND J. Econ. 27 (1), 99–123. [PubMed] [Google Scholar]
- Haviland AM, Eisenberg MD, Mehrotra A, Huckfeldt PJ, Sood N, 2015. Do Consumer-Directed Health Plans Bend the Cost Curve Over Time? Working Paper 21031. National Bureau of Economic Research, Mar. [DOI] [PubMed] [Google Scholar]
- Ho K, 2009. Insurer-provider networks in the medical care market. Am. Econ. Rev. 99 (1), 393–430. [DOI] [PubMed] [Google Scholar]
- Kim H, Norton EC, 2015. Practice patterns among entrants and incumbents in the home health market after the prospective payment system was implemented. Health Econ. 24 (Mar), 118–131. [DOI] [PubMed] [Google Scholar]
- Naseri A, Brown T, Robinson J, Whaley C, Guo C, 2016. Reference-Based Pricing for Cataract Surgery: Consumer Choices, Insurer and Consumer Spending, and Procedural Complications. Tech. Rept. University of California, Berkeley. [Google Scholar]
- Parente ST, Feldman R, Christianson JB, 2004. Evaluation of the effect of a consumer-driven health plan on medical care expenditures and utilization. Health Serv. Res. 39 (42), 1189–1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Regan TL, 2008. Generic entry, price competition, and market segmentation in the prescription drug market. Int. J. Ind. Organ. 26 (4), 930–948. [Google Scholar]
- Robinson JC, Brown TT, 2013. Increases in consumer cost sharing redirect patient volumes and reduce hospital prices for orthopedic surgery. Health Aff. 32 (8), 1392–1397. [DOI] [PubMed] [Google Scholar]
- Robinson J, Brown T, Whaley C, Bozic K, 2015a. Consumer choice between hospital-based and freestanding facilities for arthroscopy. J. Bone Joint Surg. 16 (97). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson JC, Brown TT, Whaley C, Finlayson E, 2015b. Association of reference payment for colonoscopy with consumer choices, insurer spending, and procedural complications. JAMA Intern. Med. (Sept), 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson JC, Brown T, Whaley C, 2015c. Reference-based benefit design changes consumers choices and employers payments for ambulatory surgery. Health Aff. 34 (3), 415–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson J, Brown T, Whaley C, 2017. Reference pricing changes the consumer choice architecture of health care. Health Aff. (Mar). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scherer FM, 1993. Pricing, profits, and technological progress in the pharmaceutical industry. J. Econ. Perspect. 7 (3), 97–115, 00364. [Google Scholar]
- Sood N, Wagner Z, Huckfeldt P, Haviland AM, 2013. Price shopping in consumer-directed health plans. Forum Health Econ. Policy 16 (1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whaley CM, Guo C, Brown TT, 2017. The moral hazard effects of consumer responses to targeted cost-sharing. J. Health Econ. 56 (Supplement C), 201–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yip WC, 1998. Physician response to Medicare fee reductions: changes in the volume of coronary artery bypass graft (CABG) surgeries in the Medicare and private sectors. J. Health Econ. 17 (6), 675–699. [DOI] [PubMed] [Google Scholar]


