Abstract
Introduction and importance
Despite the chance of a complete cure that surgery offers for patients seen early, the management of some complicated forms of chronic pyothorax with calcified pleural pockets of tuberculosis origin is risky, if not impossible. In these conditions, thoracomyoplasty with complete effacement of the pleural pocket is an effective alternative in the surgical management of these pockets.
Case presentation
We report the case of a 37-year-old male African Arab who was treated for a chronic, calcified pleural pocket of tuberculous origin and in whom low thoracomyoplasty was performed because of the impossibility of performing a left pleuropneumonectomy. The operating courses were uneventful with full pocket closures. Review: 1 year later, the patient reported having resumed his active professional life.
Clinical discussion
Pleural decortication associated or not with a pulmonary resection is the main surgical procedure used to manage chronic pyothorax. However, this procedure remains difficult with the risk of death, if not impossible, in cases of long-term chronicity with calcification of the pleural poche wall. In these cases, thoracomyoplasty constitutes a viable alternative in the surgical management of these pleural pockets.
Conclusion
In the context of tuberculosis and chronic pleural empyema, thoracomyoplasty can be an alternative with satisfactory results when performed by an experienced team using this technique.
Keywords: Tuberculosis, Pyothorax, Thoracic drainage, Thoracoplasty, Myoplasty, Case report
Highlights
-
•
The resurgence of tuberculosis and the HIV/AIDS pandemic are accompanied by the resistance of the BAAR to drugs.
-
•
Chronic pyothorax with calcified pleural pockets is a dreadful complication of tuberculosis.
-
•
Pleuropneumonectomy in this condition is risky, if not impossible.
-
•
Thoracomyoplasty constitutes a real alternative in the surgical management of these pleural pockets.
1. Introduction
The 1980s were marked by a resurgence of tuberculosis worldwide, especially in low-income countries. This is accompanied by an increasing resistance of the bacillus acido-alcohol resistant (BAAR) to anti-bacillary drugs. These phenomena are linked to the HIV/AIDS pandemic, migration of populations, the precarity of certain population groups (unemployment, poverty, drug addiction, etc.), and problems related to the conduct of treatments [1]. The principle of surgical treatment of chronic pyothorax is pleural decortication associated with or not with pulmonary resection. This procedure remains difficult with a risk of death, if not impossible, in cases of long-term chronicity with calcification of the pleural poche wall. In these conditions, thoracomyoplasty, which results in complete effacement, constitutes a real alternative in the surgical management of these pleural pockets [2]. This article has been reported in line with the SCARE criteria [3].
2. Presentation of the case
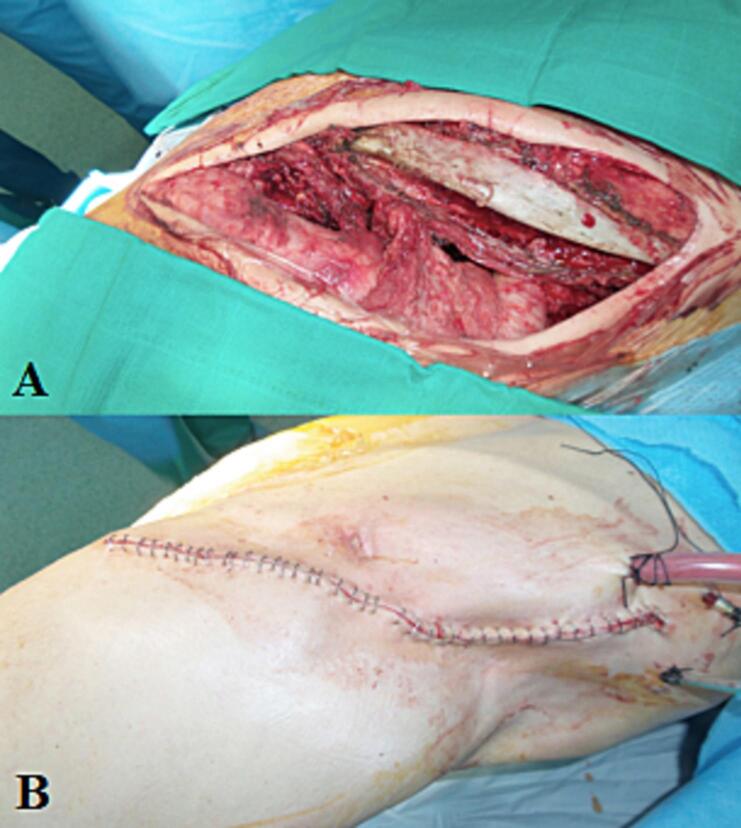
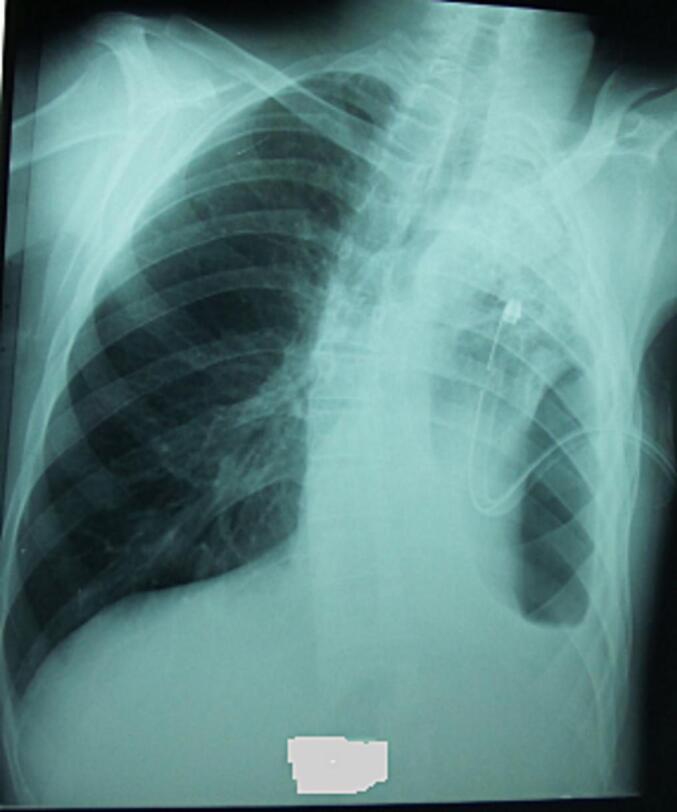
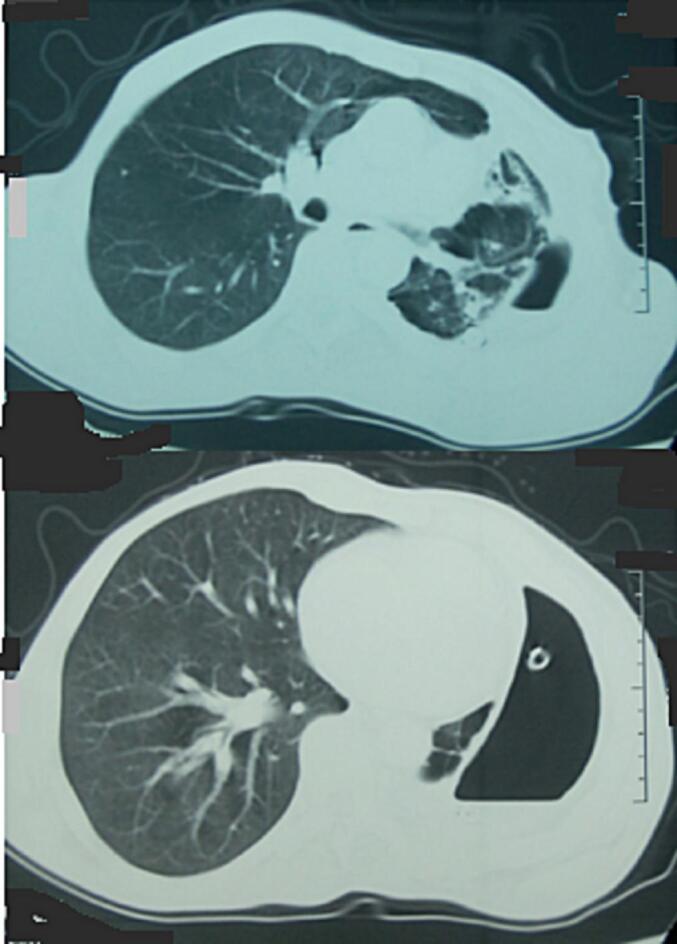
A 37-year-old male African Arab, treated for pulmonary tuberculosis at the age of 16, was admitted for dyspnea with left basithoracic pain for 8 months. He also complained of fever, general condition deterioration, and weight loss of 10 kg in 4 months. Clinical examination revealed a thoracic asymmetry due to retraction of the left hemithorax associated with left basal dullness, topped by a tympany. Blood examination found hemoglobin decreased to 9.7 g/dl, a normal platelet rate of 278,000 U/mm3, hyperleukocytosis at 13,000 U/mm3, a correct prothrombin level of 76 %, hypoalbuminemia at 26 g/l, hypoproteinemia at 55 g/l, AST at 97 U/l (2 times normal), ALT at 110 U/l (2 times normal), and CRP increased to 78 mg/l. The renal function and ionogram were correct. Frontal chest radiography (Fig. 1) revealed a left axillo-basal chronic pleural pocket with large pachypleuritis and pinching of the intercostal spaces. Computed tomography (CT) scan of the chest (Fig. 2) revealed the above-mentioned lesions, particularly the characteristics of the pocket and its impact on the remaining lung. There were no obvious lesions in the contralateral lung. Given the endemic context and the result of the clinical and radiological examination, the diagnosis of a pleural pocket of tuberculosis origin was evoked, and the assessment was supplemented by BK's search in sputum with pus culture obtained following the pleural puncture, which had all returned positive. Thoracic drainage associated with antibacillary chemotherapy for 6 months was instituted, and the patient was followed for 7 months with a preparation consisting of respiratory kinesitherapy, which allowed the discharge of the pleural cavity and adapted nutrition, allowing him to gain 7 kg in 5 months. It was then decided to perform a left pleuropneumonectomy, given the CT scan appearance. The approach was conservative left posterolateral thoracotomy through the bed of the sixth rib, which was resected. Exploration revealed a chronic pleural pocket with enormous pachypleuritis, making any attempt to dissect the pulmonary pedicle, which was the site of significant chronic inflammatory remodeling, dangerous. Given this context associated with the quality of the preparation, a low thoracoplasty (resection of a row of six ribs) with myoplasty using the latissimus dorsi and serratus simultaneously was performed (Fig. 3A, B). The postoperative courses were uneventful, with pocket plugging (Fig. 4). Review: 1 year later, the patient reported having resumed his socio-professional activities.
Fig. 1.
thoracic radiography of the front showing a drained left axillobasal pleural pocket, pinching of intercostal spaces, pachypleurite and contralateral lung hyperinflation.
Fig. 2.
Thoracic CT objectivating a pleural pouch with enormous pachypleuritis and a parenchymal destruction appearance of the upper left lobe.
Fig. 3.
surgical view showing the closure of the pouch by introducing the muscles after a prior thoracoplasty.
Fig. 4.
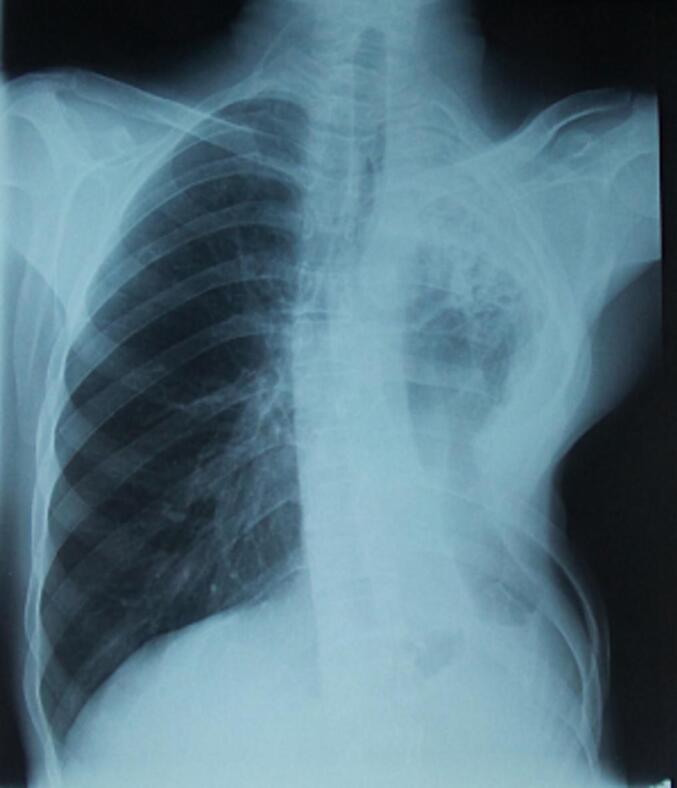
postoperative thoracic X-ray showing the closure of the pouch.
3. Discussion
Chronic pleural pockets are indeed a condition whose diagnosis and treatment principles were laid down more than 2400 years ago by Hippocrates. Nevertheless, it remains a topical issue in all latitudes, although the stage at the time of management and the underlying terrain vary significantly [2]. In High income countries with an appropriate management system, post-tuberculosis pleural empyema has become rare and reflects the failure of well-coordinated medical treatment based on early diagnosis and management with appropriate antibiotic therapy, puncture/drainage, and appropriate use of intrapleural antifibrinolytics. In low-income countries, the lack of organization of care upstream of hospital structures leads to a high frequency of tuberculosis pleural pockets, which evolve for several months and can only be treated surgically. In this context, the main principles of surgical treatment most often allow the performance of a pleural decortication associated or not with a pulmonary resection, a gesture that remains difficult and risky, if not impossible, because of the chronicity of the lesion and calcifications. In cases where the patient has been debilitated by months of septic evolution, salvage procedures may be useful, such as percutaneous drainage in front of the pocket, which can thus be evacuated as completely as possible. Follow-up will be conditioned by effective medical and nutritional care, combined with daily respiratory kinesitherapy, as part of the preparation for secondary surgery [4]. Despite adequate preparation for our patient, it was impossible to perform a left pleuropneumonectomy. Considering the risk of injuring the elements of the pulmonary pedicle that can kill the patient on the table, we resolved to remove this pocket in the same operative time through a low thoracoplasty followed by a myoplasty along with the latissimus dorsi and serratus muscles. This technique aims to clear the pocket by removing the residual cavity (already washed by chest drainage and respiratory Kinesistherapy) through the collapse of the chest wall by thoracoplasty, followed by filling myoplasty with muscle flaps of adequate volume and vitality. The latissimus dorsi and serratus muscles are better suited in this context; hence, there is an interest in preserving them during thoracotomies, as we systematically do in all our patients. In the case of this patient, the surgical procedures were simple, with satisfactory long-term results from the resumption of his socio-professional activities.
4. Conclusion
Despite the evolution of tuberculosis management, chronic pyothorax with a calcified pleural pocket remains common in low-income countries. Surgery to dissect and resect the lung is often risky or even impossible, given the chronic nature of the lesion. In this context, thoracomyoplasty can be an alternative with satisfactory results when performed by an experienced team using this technique.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Ethical approval
Ethical approval for this study (Ethical Committee N° NAC 28) was provided by the Ethical Committee NAC of our Hospital, on 25 November 2023.
Funding
This article did not receive fund.
Author contribution
SR, AZ,ML, YO and MS treated the patient during his hospitalization. SR wrote the case report. All authors read and approved the final manuscript.
Guarantor
SANI Rabiou.
Research registration number
Not applicable.
Conflict of interest statement
All authors declare that they have no conflicts of interest.
Acknowledgments
No
References
- 1.Botianu P.V., Botianu A.M. Thoracomyoplasty in the treatment of empyema: current indications, basic principles, and results. Pulm Med. 2012;2012 doi: 10.1155/2012/418514. (Epub 2012 May 14. PMID: 22666583; PMCID: PMC3361311) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Molnar T.F. Current surgical treatment of thoracic empyema in adults. Eur. J. Cardiothorac. Surg. 2007;32:422–430. doi: 10.1016/j.ejcts.2007.05.028. [DOI] [PubMed] [Google Scholar]
- 3.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A. The SCARE 2023 guideline: updating consensus surgical case report (SCARE) guidelines. Int J Surg Lond Engl. 2023;109(5):1136. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sakakura N., Mizuno T., Kuroda H., Sakao Y., Uchida T. Surgical treatment of empyema after pulmonary resection using pedicle skeletal muscle plombage, thoracoplasty, and continuous cavity ablution procedures: a report on three cases. J. Thorac. Dis. 2016;8(6):1333–1339. doi: 10.21037/jtd.2016.04.04. [DOI] [PMC free article] [PubMed] [Google Scholar]