Abstract
Purpose
The aim of this study was to identify potential risk factors for myocardial infarction immediately following total hip arthroplasty.
Methods
The 2016–2019 Nationwide Inpatient Sample database was used to identify patients who underwent primary total hip arthroplasty (THA) and suffered a myocardial infarction (MI). Patient data including demographics, admission, and comorbidities were recorded. Univariate analysis and subsequent multivariate logistic regression were performed to determine which circumstances affected the odds of MI.
Results
A total of 367,890 patients were identified for THA with 142 of those also having a myocardial infarction. Those who experienced an MI had increased length of stay, total charges, and generally negative dispositions compared to their non-MI counterparts (p < 0.001). Through regression analysis, factors that increased the odds of MI included older age [odds ratio (OR) 1.59, 95 % confidence interval (CI) 1.49–1.70], a female sex (OR 1.46, 95 % CI 1.37–1.55), previous coronary artery bypass graft (OR 1.20, 95 % CI 1.01–1.43), obesity (OR 1.12, 95 % CI 1.04–1.21), colostomy (OR 2.07, 95 % CI 1.21–3.56), and Parkinson's disease (OR 1.48, 95 % CI 1.13–1.95). Factors that decreased that risk included elective admission (OR 0.21, 95 % CI 0.19–0.22) and a tobacco related disorder (OR 0.69, 95 % CI 0.63–0.76).
Conclusions
Patient risk for myocardial infarction following total hip arthroplasty varies in part based on their background and comorbidities. These findings can be used to better recognize those who should receive further precautions and tailor proper treatment strategies for THA.
Keywords: Total hip arthroplasty, Myocardial infarction, Risk, In-patient
1. Introduction
Myocardial infarctions (MI) can alter a person's life significantly, leading to death, lifestyle changes, or other extreme health complications.1, 2, 3, 4, 5 MI is increasingly widespread in society, as it has been found to affect close to three million people per year, with one million deaths in the United States alone.6 Prior to onset, preventative measures include controlling diet and monitoring alcohol, nicotine, and drug consumption.7
Total hip arthroplasty (THA) is a highly successful surgical procedure and is estimated to increase upwards of 469 % by 2060, making it increasingly prevalent in orthopaedics.8 Although many advances have occurred in THA design, efficiency, and safety; postoperative complications, such as MI, still occur. Being incredibly dangerous, recent literature recognizes MI as the most common cause of death after THA.9,10
Previous studies have compared the timing of MI after THA and risk factors of it after total knee and hip arthroplasties however, there have been few comprehensive studies of the factors that increase risk of MI after THA.11,12 Lack of comprehensive understanding regarding patient factors that affect post-THA risk of MI affects the ability to counsel patients and plan for THA. The purpose of this study was to utilize a national database to investigate the prevalence of pre-operative patient factors associated with MI after THA.
2. Methods
2.1. Data acquisition
This is a retrospective review of the Nationwide Inpatient Sample (NIS) database. The NIS database was queried for all patients who underwent primary or complex primary THA from 2016 to 2019 using the International Classification of Disease, Tenth Revision, Clinical Modification/Procedure coding System [ICD-10-CM/PCS]. Patients were further selected into those who did and those who did not sustain an MI following THA, as the MI group (n = 142) and non-MI group (n = 367,748) respectively. MI data was captured up until discharge as the NIS contains strictly inpatient information. Patient demographics (age, sex, and race) were recorded. Admission related data such as length of stay, total charges, and disposition (DISP) at discharge (routine, short term hospital stay, alternate facility, death, etc.) were documented. Additional medical comorbidities were identified using ICD -10 – CM codes [Appendix A]. The study was exempt from IRB approval since the data were publicly available and de-identified.
2.2. Statistical analysis
Statistical analyses were performed using SPSS Statistics software version 27.0 (IBM Armonk, New York). Student's t tests were used to analyze numerical variables, and chi-squared analyses were used for categorical variables between groups. Fisher's exact tests were used when incidence values were less than 5. Statistical significance was specified as two-sided, p < 0.05 with unequal variances. Multivariate logistic regression analysis was conducted to assess the association between potential risk factors and the occurrence of MI after THA. Odds ratios (OR) with 95 % confidence intervals (CI) were calculated.
3. Results
A total of 367,890 patients who underwent total hip arthroplasty from 2016 to 2019 were identified in the NIS database. Of this population, 142 patients (0.039 %) suffered in-hospital MI following THA. Mean age was 65.86 years (SD = 11.39), and the myocardial infarction group was 75.55 (SD = 11.16) (p < 0.001). Gender and race did not vary significantly between the groups (p = 0.540). (Table 1 describes patient demographics).
Table 1.
Patient Demographics
a Race based on NIS Race/ethnicity.
| Factor | Non-MI Group N = 367,748 | MI Group N = 142 | P Value |
|---|---|---|---|
| Mean age (years) | 65.86 (SD = 11.39) | 75.55 (SD = 11.16) | <0.001 |
| Number of females (%) | 205,666 (55.9 %) | 76 (53.5 %) | 0.563 |
| Race | |||
| Caucasian | 302,978 (82.39 %) | 124 (87.32 %) | 0.540 |
| African American | 27,557 (7.50 %) | * (3.52 %) | |
| Hispanic | 13,029 (3.54 %) | * (3.52 %) | |
| Asian | 3409 (0.93 %) | * (0.70 %) | |
| Native American | 1122 (0.31 %) | 0 (0.00 %) | |
| Other | 6020 (1.64 %) | * (2.11 %) | |
Numbers between 1 and 10 were not reported per the healthcare cost and utilization project data agreement.
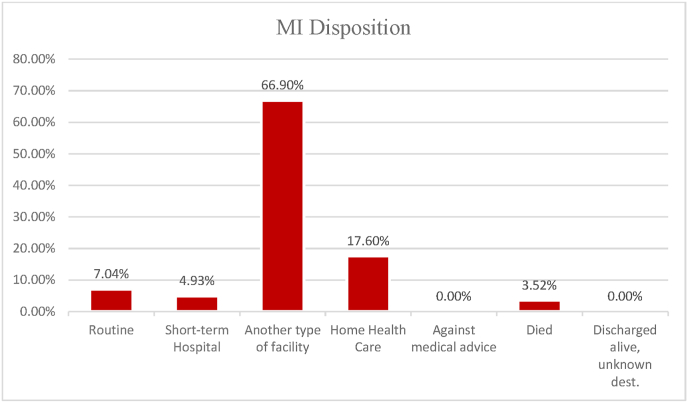
Patients that sustained an in-hospital MI had a significantly longer length of stay at 9.00 days (SD = 6.38) compared to non-MI patients at 2.32 days (SD = 2.52) (p < 0.001). MI patients also incurred higher total charges (167,755.19 USD, SD = 134,047.12) than non-MI patients (66,841.15 USD, SD = 47,739.07 (p < 0.001). On the other hand, non-MI patients were much more likely to have an elective admission (91.22 %) than MI patients (56.34 %) (p < 0.001). Fig. 1, Fig. 2 categorize patients based on discharge disposition for non-MI and MI patients respectively. Most non-MI patients were sent to home health care (42.3 %), while the majority of MI-patients were discharged to another type of facility (66.9 %). Mortality was 3.52 % in the MI group and 0.089 % in the non-MI group. (Table 2 illustrates disposition data).
Fig. 1.
Disposition for patients without MI following THA
Bar graph representing the percentage different disposition categories in patients without acute inpatient myocardial infarction (MI) following total hip arthroplasty (THA).
Fig. 2.
Disposition for patients with MI following THA
Bar graph representing the percentage different disposition categories in patients who sustained acute inpatient myocardial infarction (MI) following total hip arthroplasty (THA).
Table 2.
Patient Admission-Related Data a
a Disposition based on NIS DISP: 1 = Routine; 2 = Short-term hospital; 5 = Another type of facility; 6 = Home Health Care; 7 = Against medical advice; 20 = Died; 99 = Discharged alive, destination unknown.
| Factor | Non-MI Group N = 367,748 | MI Group N = 142 | P Value |
|---|---|---|---|
| Length of stay (days) | 2.32 (SD = 2.52) | 9.00 (SD = 6.38) | <0.001 |
| Total charges ($) | 66,841.15 (SD = 47,739.07) | 167,755.19 (SD = 134,047.12) | <0.001 |
| Elective Admission | 335,473 (91.22 %) | 80 (56.34 %) | <0.001 |
| Disposition | |||
| 1 | 143,228 (38.9 %) | 10 (7.04 %) | <0.001 |
| 2 | 863 (0.234 %) | * (4.93 %) | |
| 5 | 67,403 (18.3 %) | 95 (66.9 %) | |
| 6 | 155,539 (42.3 %) | 25 (17.6 %) | |
| 7 | 253 (0.069 %) | 0 (0.00 %) | |
| 20 | 327 (0.089 %) | * (3.52 %) | |
| 99 | 0 (0.00 %) | 0 (0.00 %) | |
Numbers between 1 and 10 were not reported per the healthcare cost and utilization project data agreement.
Table 3 contains univariate analysis for patient factors and comorbidities between MI and non-MI patients. The patients who had MI were associated with higher incidence of chronic kidney disease (9.86 % vs 5.88 %) (p = 0.044), coronary artery bypass graft (CABG) (9.15 % vs 2.47 %) (p < 0.001), cardiac stent (14.08 % vs 3.60 %) (p = 0.002), obesity (14.79 % vs 21.73 %) (p = 0.045), and Parkinson's (28.17 % vs 0.52 %) (p = 0.007) when compared to control. However, the MI group had a significantly decreased prevalence of tobacco related disorders than the non-MI group (3.52 % vs 17.32 %) (p < 0.001).
Table 3.
Comorbidities in Non-MI and MI groups (univariate)a.
| Factor | Non-MI Group (N = 367,748) | MI Group (N = 142) | P Value |
|---|---|---|---|
| HIV | 504 (0.14 %) | 0 (0.00 %) | 1 |
| Cirrhosis | 1133 (0.31 %) | * (0.70 %) | 0.355 |
| Dialysis | 383 (0.10 %) | 0 (0.00 %) | 1 |
| CKD | 21,612 (5.88 %) | 14 (9.86 %) | 0.044 |
| Colostomy | 444 (0.12 %) | *(0.70 %) | 0.158 |
| Down Syndrome | 129 (0.035 %) | 0 (0.00 %) | 1 |
| Pacemaker | 5552 (1.51 %) | * (3.52 %) | 0.065 |
| CABG | 9078 (2.47 %) | 13 (9.15 %) | <0.001 |
| Cardiac Stent | 13,244 (3.60 %) | 20 (14.08 %) | 0.002 |
| Heart Valve | 3119 (0.85 %) | * (1.41 %) | 0.335 |
| Blind | 322 (0.088 %) | 0 (0.00 %) | 1 |
| Ankylosing Spondylitis | 500 (0.14 %) | *(0.70 %) | 0.176 |
| Obesity | 79,898 (21.73 %) | 21 (14.79 %) | 0.045 |
| Morbid Obesity | 28,069 (7.63 %) | *(6.34 %) | 0.561 |
| Super Obesity | 1644 (0.45 %) | *(1.41 %) | 0.133 |
| Diabetes Without Complications | 36,280 (10.01 %) | *(5.63 %) | 0.082 |
| Diabetes With Complications | 713 (0.19 %) | 0 (0.00 %) | 1 |
| Tobacco Related Disorder | 63,703 (17.32 %) | *(3.52 %) | <0.001 |
| Sickle Cell | 655 (0.18 %) | 0 (0.00 %) | 1 |
| SLE | 1684 (0.46 %) | 0 (0.00 %) | 1 |
| Organ Transplant | 812 (0.22 %) | 0 (0.70 %) | 0.27 |
| Parkinson's | 1923 (0.52 %) | 40 (28.17 %) | 0.007 |
Abbreviations: HIV—human immunodeficiency virus; CKD – Chronic Kidney Disease; CABG – Coronary Artery Bypass Graft; SLE – Systemic Lupus Erythematosus.
Numbers between 1 and 10 were not reported per the healthcare cost and utilization project data agreement.
Table 4 summarizes the multivariate analysis for patient factors between MI and non-MI patients following THA. Those who underwent an elective admission were 0.21 times less likely to suffer a myocardial infarction (CI 0.19, 0.22) (p < 0.001). Similarly, those who had a tobacco related disorder were 0.69 times less likely to have an MI (CI 0.63, 0.76) (p < 0.001). Conversely, variables independently associated with increased risk for MI included: female sex with an OR of 1.46 (CI 1.37, 1.55) (p < 0.001), Parkinson's with an OR of 1.48 (CI 1.13, 1.95) (p = 0.005), obesity with OR of 1.12 (CI 1.04, 1.21) (p = 0.003), increasing age with OR of 1.59 (CI 1.49, 1.70) (p < 0.001), colostomy with OR of 2.07 (CI 1.21, 3.56) (p = 0.008) and CABG with OR of 1.2 (CI 1.01, 1.43) (p = 0.036).
Table 4.
Multivariate analysis of risk factors for MIa.
| Factor | Exp (B) Odds Ratio | Odds Ratio 95 % Confidence Interval | P Value |
|---|---|---|---|
| Elective Admission | 0.21 | (0.19, 0.22) | <0.001 |
| Indicator of sex | 1.46 | (1.37, 1.55) | <0.001 |
| Tobacco Related Disorder | 0.69 | (0.63, 0.76) | <0.001 |
| CKD | 1.00 | (0.89, 1.12) | 0.997 |
| Parkinson's | 1.48 | (1.13, 1.95) | 0.005 |
| Obesity | 1.12 | (1.04, 1.21) | 0.003 |
| Age (Nominal) | 1.59 | (1.49, 1.70) | <0.001 |
| Colostomy | 2.07 | (1.21, 3.56) | 0.008 |
| CABG | 1.20 | (1.01, 1.43) | 0.036 |
| Cardiac Pacemaker | 0.85 | (0.68, 1.06) | 0.154 |
| Cardiac Stent | 1.03 | (0.88, 1.20) | 0.758 |
Abbreviations: CKD – Chronic Kidney Disease; CABG – Coronary Artery Bypass Graft.
4. Discussion
Though THA is considered a relatively safe procedure with increasing volume, serious complications such as MI will continue to occur - highlighting the need for continued characterization of patient population and analysis for MI risk following THA.8,13 While older age and a history of heart conditions are well-established risk factors for MI after joint replacement surgeries, other factors like diabetes, obesity, and gender show varying significance.14 This study expands on the knowledge of known risk factors and sheds light on less scrutinized preoperative conditions for THA.
The majority of THA research focuses on elective procedures, as that is the normal consideration; however, the NIS represents a more comprehensive outlook, including emergent cases that we know are linked to worse outcomes.15 Additionally, the majority of post-THA MIs occur within 3 days from surgery - as much as 83 % - supporting use of a large, relevant inpatient sample (2016–2019).16 Our study observed a total MI incidence of 0.04 % after THA with 142 cases, comparable to a prospective cohort study by Peterson et al. that noted a 30-day occurrence of MI in both total hip and total knee arthroplasty at 0.12 % with 31 cases combined.
Examining patient demographics and admission, we observed several trends for MI groups. In agreement with other studies, the patients who experienced postoperative MI after THA tended to be older with a group average age of 75 rather than the non-MI's 65. Wood et al., retrospectively observed that the frequency of myocardial infarction increased markedly with older age (p < 0.001), and complications were highest in those 70 or older. This was further cemented in our multivariate analysis and an OR of 1.59 for increasing age. However, this same Wood et al. study noted that the frequency of MI was higher in male patients than in female patients – where we recorded an insignificant difference.17 Surprisingly, our multivariate logistic regression uncovered that female gender was significantly associated with increased risk of MI (OR 1.49) (p < 0.001) when holding other pertinent variables constant. A 2019 meta-analysis found that in 2 of 6 studies incorporating gender risks for TJA MI, male gender was associated with increased risk – but in the other 4 no significant differences were elucidated. While our finding represents an important departure from certain literature, it is not unsupported in the literature following other procedures.14 A prospective study examined lower extremity bypass grafting postoperative outcomes between genders and found that women had increased MI rates compared to men (9.8 % vs 2 %).18 They concluded that women may be at higher risk for a ‘silent’ cardiac disease which contributed to the result. While perhaps not necessarily a cardiac disease, it could be other conditions such as diabetes, or hypertension that have been shown to be risk factors but were not selected for against other variables.19 This is important finding should be further explored to best assess risk for MI.
As MI is a life-threatening complication, it is of no surprise that the THA patients who suffered from them had increased length of stay, total charges, and negative dispositions as part of their adverse outcomes. Aside from recognition as a primary cause of death following THA, sustaining an MI has been shown to lead to a mean LOS up to 17.5 days ± 12.7 in total joint arthroplasty.20 This, along with a myriad of complications, would subsequently add to increased costs of care.
Our disposition data point to troubled stays, being sent to other healthcare facilities at a much higher rate (66.9 %), and even death (3.52 %) compared to those without MI. The non-MI cohort saw the majority sent to home health care (42.30 %) with significantly less mortality (0.09 %). Ghandi and colleagues similarly found increased incidence of poor discharge outcomes in their analysis of MI following total joint arthroplasty – 58.7 % of their MI cohort went to home health care vs 94.3 % of the non-MI control.20 Part of the reasoning for these outcomes can be attributed to the MI category including a substantial amount of emergent procedures compared to the non-MI cohort, 43.66 % vs 8.78 % respectively. Instances of elective admission were shown to have protective effects by 0.21-fold; or about an 80 % decrease in MI odds. The sharp difference in outcome makes this an important distinction when evaluating for potential postoperative complication risk.
Numerous comorbidities were found to be significantly associated with MI following THA – in univariate analysis this included prior chronic kidney disease, coronary artery bypass graft, heart stent, obesity, tobacco use disorders and Parkinson's. These, alongside increasing age, gender, elective admission, obesity, prior pacemaker and colostomy were analyzed under multivariate logistic regression (selected for relevance and proximity to significance). Surprisingly, prior pacemaker, chronic kidney disease, and stent histories did not show significant impact. On the other hand, CABG, obesity, tobacco use disorders, colostomy and Parkinson's were found to significantly affect the odds of MI.
As mentioned, cardiac disease history has been recorded in several instances as a risk factor for TJA MI; Feng et al. went as far as to determine that even coronary artery revascularization therapies for treating heart disease did not significantly reduce risk of adverse cardiac outcomes.18,21 This may explain why CABG had an increased odds ratio, but more research would need to be done on other cardiac interventions and their effects e.g., pacemaker implantation which did not increase the MI rate.
Other studies have marked obesity as a risk factor for poor THA outcomes, including cardiac complications.22 In agreement, we found that obesity increased the odds of MI by 1.12-fold. There is association between obesity and myocardial infarction in the general population as well, where BMI>30 (kg/m2) so carryover is not unexpected.23
Patients with a colostomy are typically older and found to be at increased risk of periprosthetic dislocation and periprosthetic infection24 Further data surrounding this comorbidity are scarce, and here our study revealed that it can raise the odds of an MI by 2.07-fold. With age factored in, this supports their “high-risk” status for THA.
Neurocognitive comorbidities, such as Parkinson's Disease, are often referenced for generally negative results including higher wound infection rate, inferior functional scores, and longer, challenged hospital stays following THA.25 While data regarding MI after THA is lacking, one prior NIS study found no significance in “neurological disorders” in MI risk with an OR of 1.1 (95 % CI 1.0–1.2).26 Alternatively, we report Parkinson's specifically as an independent risk factor for myocardial infarction (OR 1.48) (95 % CI 1.13–1.95). Beyond these results, future studies should examine this relationship and subsequently other neurological disorders to see if this is a unique finding or can be more broadly applied.
This study is not without limitations. Interestingly, tobacco users had a decreased risk of MI following THA – OR was 0.69, meaning that this disorder had a potentially protective effect. This finding is surprising given research regarding increased complications and myocardial infarction in smokers in general or THA alike.27,28 This would have to be further explored – a known limitation of the NIS database is inadequate reporting of tobacco use.26 There are addition database related limitations. The coverage of only inpatient data and short-term complications restricts the study's insight into longer-term occurrences after discharge like delayed heart attacks. A transfer to a nonparticipating hospital or other type of facility may have resulted in an outcome not registered. However, as previously mentioned, most MIs occur within days following surgery. The NIS also does not report on the duration of each procedure, ambulation delays postoperatively, or skill level of the surgeon operating (attending, fellow, resident, etc.), and therefore their potential effects on MI outcomes were not included in this study. Revisional procedures were not included but a patient could contribute to multiple should they have required a contralateral THA. Despite this slim occurrence, our study is strengthened by the comprehensive nature of NIS database, including a large, national sample size as well as inclusion of more urgent THA cases.
5. Conclusion
As the volume of THA continues to rise, the necessity for identifying risk factors for adverse outcomes should increase as well. For a complication as severe as MI, it is imperative to characterize patient populations and those at greater risk. This study identified older age, a female sex, CABG, obesity, colostomy and Parkinson's as leading to greater chance of MI and in turn, increased LOS, cost of care, and mortality. Elective admission decreased the risk. These findings can be used as a basis for further research in the field and to better counsel patient care.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors; no funds, or other support were received during preparation and construction of this manuscript.
Ethical approval
The UTSW Institutional Review Board has confirmed that no ethical approval is required, exempt.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Ethical statement
The UTSW Institutional Review Board has confirmed that no ethical approval is required, and the study is exempt due to use of publicly available, deidentified information (NIS Database).
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors; no funds, or other support were received during preparation and construction of this manuscript.
Guardian/patient's consent
Not applicable.
CRediT authorship contribution statement
Enzo C. Mesarick: Conceptualization, Formal analysis, Writing – original draft. Terrul L. Ratcliff: Methodology, Writing – original draft. Jonathan Jose: Data curation, Writing – original draft. Senthil Sambandam: Supervision, Investigation, Writing – review & editing.
Declaration of competing interest
The authors have no relevant financial or non-financial conflicts of interest to disclose.
Acknowledgements
None.
Contributor Information
Enzo C. Mesarick, Email: enzo.mesarick@utsouthwestern.edu.
Terrul L. Ratcliff, Email: terrul.ratcliff@utsouthwestern.edu.
Jonathan Jose, Email: jonmjose21@gmail.com.
Senthil Sambandam, Email: senthil.sambandam@utsouthwestern.edu.
Appendix A. ICD Codes
| Comorbidities | Hip | Complication | |
|---|---|---|---|
| Diabetes without complications | Cardiac Arrest and VF | Hip replacement | Acute Myocardial Infarction |
| E119 | I4901 | 0SR9019, 0SR901A, 0SR901Z, 0SR9029, 0SR902A, 0SR902Z, 0SR9039, 0SR903A, 0SR903Z, 0SR9049, 0SR904A, 0SR904Z, 0SR9069, 0SR906A, 0SR906Z, 0SR907Z, 0SR90EZ, 0SR90J9, 0SR90JA, 0SR90JZ, 0SR90KZ, 0SRB019, 0SRB01A, 0SRB01Z, 0SRB029, 0SRB02A, 0SRB02Z, 0SRB039, 0SRB03A, 0SRB03Z, 0SRB049, 0SRB04A, 0SRB04Z, 0SRB069, 0SRB06A, 0SRB06Z, 0SRB07Z, 0SRB0EZ, 0SRB0J9, 0SRB0JA, 0SRB0JZ, 0SRB0KZ | I219 |
| Diabetes with complications | Heart failure | ||
| E1169 | I509 | ||
| Tobacco-related disorder | Cerebral Infarction | ||
| Z87891 | I639 | ||
| Type 1 Diabetes | Thromboembolism | ||
| E109 | I744 | ||
| Type 2 Diabetes | Immunity Disorders | ||
| E11 | D899 | ||
| Secondary Diabetes | Intestinal Obstruction | ||
| E09 | K56609 | ||
| Alcohol-related Disorder | Hepatic failure | ||
| F1099 | K7290 | ||
| Opioid-related disorder | Epilepsy | ||
| F11288 | G40909 | ||
| Cannabis-related disorder | Diverticulosis | ||
| F12988 | K5709 | ||
| Stimulant-related disorder | HIV | ||
| F1520 | B20 | ||
| Inhalant-related disorder | Hepatitis | ||
| F18980 | K739 | ||
| Obesity | Sickle Cell Disease | ||
| E66 | D571, D572, D573, D574, D575, D576, D577, D578, D5700 | ||
| Colostomy | Conduction Disorder | ||
| Z93.3 | I459 | ||
| Dialysis | Cardiac Arrythmia | ||
| Z992 | I49 | ||
| Chronic Kidney Disease | Ulcerative Collitis | ||
| N181, N182, N183, N184, N185, N186, N189 | K5190 | ||
| Parkinson's | Systemic Lupus Erythematosus | ||
| G20 | M3210, M3211, M3212, M3213, M3214, M3215, M3219, M328, M329, M32, M320, M321 | ||
| Other connective tissue | |||
| M3589 | |||
| Organ transplant | |||
| Z940, Z941, Z942, Z943, Z944 | |||
References
- 1.Bajaj A., Sethi A., Rathor P., Suppogu N., Sethi A. Acute complications of myocardial infarction in the current era: diagnosis and management. J Invest Med. 2015;63:844–855. doi: 10.1097/jim.0000000000000232. [DOI] [PubMed] [Google Scholar]
- 2.Damluji A.A., et al. Mechanical complications of acute myocardial infarction: a scientific statement from the American heart association. Circulation. 2021;144:e16–e35. doi: 10.1161/cir.0000000000000985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Everson S.A., et al. Hostility and increased risk of mortality and acute myocardial infarction: the mediating role of behavioral risk factors. Am J Epidemiol. 1997;146:142–152. doi: 10.1093/oxfordjournals.aje.a009245. [DOI] [PubMed] [Google Scholar]
- 4.Capes S.E., Hunt D., Malmberg K., Gerstein H.C. Stress hyperglycaemia and increased risk of death after myocardial infarction in patients with and without diabetes: a systematic overview. Lancet. 2000;355:773–778. doi: 10.1016/s0140-6736(99)08415-9. [DOI] [PubMed] [Google Scholar]
- 5.Condon C., McCarthy G. Lifestyle changes following acute myocardial infarction: patients perspectives. Eur J Cardiovasc Nurs. 2006;5:37–44. doi: 10.1016/j.ejcnurse.2005.06.005. [DOI] [PubMed] [Google Scholar]
- 6.Mechanic O.J., Gavin M., Grossman S.A. StatPearls. StatPearls Publishing; 2023. Acute myocardial infarction. [Google Scholar]
- 7.Lu L., Liu M., Sun R., Zheng Y., Zhang P. Myocardial infarction: symptoms and treatments. Cell Biochem Biophys. 2015;72:865–867. doi: 10.1007/s12013-015-0553-4. [DOI] [PubMed] [Google Scholar]
- 8.Shichman I., et al. Projections and epidemiology of primary hip and knee arthroplasty in medicare patients to 2040-2060. JBJS Open Access. 2023;8 doi: 10.2106/jbjs.oa.22.00112. e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berstock J.R., Beswick A.D., Lenguerrand E., Whitehouse M.R., Blom A.W. Mortality after total hip replacement surgery: a systematic review. Bone Jt. Res. 2014;3:175–182. doi: 10.1302/2046-3758.36.2000239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aynardi M., Pulido L., Parvizi J., Sharkey P.F., Rothman R.H. Early mortality after modern total hip arthroplasty. Clin Orthop. 2009;467:213–218. doi: 10.1007/s11999-008-0528-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lalmohamed A., et al. Timing of acute myocardial infarction in patients undergoing total hip or knee replacement: a nationwide cohort study. Arch Intern Med. 2012;172:1229–1235. doi: 10.1001/archinternmed.2012.2713. [DOI] [PubMed] [Google Scholar]
- 12.Belmont P.J.J., et al. Postoperative myocardial infarction and cardiac arrest following primary total knee and hip arthroplasty: rates, risk factors, and time of occurrence. JBJS. 2014;96:2025. doi: 10.2106/jbjs.n.00153. [DOI] [PubMed] [Google Scholar]
- 13.Turan O., et al. 30-day to 10-year mortality rates following total hip arthroplasty: a meta-analysis of the last decade (2011–2021) HIP Int. 2023;11207000231151235 doi: 10.1177/11207000231151235. [DOI] [PubMed] [Google Scholar]
- 14.Elsiwy Y., Jovanovic I., Doma K., Hazratwala K., Letson H. Risk factors associated with cardiac complication after total joint arthroplasty of the hip and knee: a systematic review. J Orthop Surg. 2019;14:15. doi: 10.1186/s13018-018-1058-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anis H.K., et al. A comparison of peri-operative outcomes between elective and non-elective total hip arthroplasties. Ann Transl Med. 2019;7:78. doi: 10.21037/atm.2019.01.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gandhi R., et al. Incidence and timing of myocardial infarction after total joint arthroplasty. J Arthroplasty. 2006;21:874–877. doi: 10.1016/j.arth.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 17.Wood M., et al. Frequency of myocardial infarction, pulmonary embolism, deep venous thrombosis, and death following primary hip or knee arthroplasty. Anesthesiology. 2002;96:1140–1146. doi: 10.1097/00000542-200205000-00017. [DOI] [PubMed] [Google Scholar]
- 18.Feng B., et al. The effect of previous coronary artery revascularization on the adverse cardiac events ninety days after total joint arthroplasty. J Arthroplasty. 2018;33:235–240. doi: 10.1016/j.arth.2017.08.011. [DOI] [PubMed] [Google Scholar]
- 19.Schulte, K. J. & Mayrovitz, H. N. Myocardial Infarction Signs and Symptoms: Females vs. Males. Cureus 15, e37522. 10.7759/cureus.37522. [DOI] [PMC free article] [PubMed]
- 20.Gandhi R., et al. Incidence and timing of myocardial infarction after total joint arthroplasty. J Arthroplasty. 2006;21:874–877. doi: 10.1016/j.arth.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 21.Curtis G.L., et al. Perioperative outcomes and complications in patients with heart failure following total knee arthroplasty. J Arthroplasty. 2018;33:36–40. doi: 10.1016/j.arth.2017.07.043. [DOI] [PubMed] [Google Scholar]
- 22.Onggo J.R., Onggo J.D., Steiger R. de, Hau R. Greater risks of complications, infections, and revisions in the obese versus non-obese total hip arthroplasty population of 2,190,824 patients: a meta-analysis and systematic review. Osteoarthritis Cartilage. 2020;28:31–44. doi: 10.1016/j.joca.2019.10.005. [DOI] [PubMed] [Google Scholar]
- 23.Zhu J., et al. The incidence of acute myocardial infarction in relation to overweight and obesity: a meta-analysis. Arch. Med. Sci. AMS. 2014;10:855–862. doi: 10.5114/aoms.2014.46206. 10.5114%2Faoms.2014.46206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang K., Sambandam S. Total hip arthroplasty in patients with colostomy: impact on inpatient complications, hospital costs, and length of stay. Arch Orthop Trauma Surg. 2023 doi: 10.1007/s00402-023-05060-0. 10.1007/s00402-023-05060-0. [DOI] [PubMed] [Google Scholar]
- 25.McCormack D., Boksh K., Sheikh N. Total hip arthroplasty in Parkinson's disease – a systematic review of the current evidence. J Orthop. 2021;24:284–290. doi: 10.1016/j.jor.2021.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Menendez M.E., Memtsoudis S.G., Opperer M., Boettner F., Gonzalez Della Valle A. A nationwide analysis of risk factors for in-hospital myocardial infarction after total joint arthroplasty. Int Orthop. 2015;39:777–786. doi: 10.1007/s00264-014-2502-z. [DOI] [PubMed] [Google Scholar]
- 27.Matharu G.S., et al. The effect of smoking on outcomes following primary total hip and knee arthroplasty: a population-based cohort study of 117,024 patients. Acta Orthop. 2019;90:559–567. doi: 10.1080/17453674.2019.1649510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Elkhader B.A., Abdulla A.A., Ali Omer M.A. Correlation of smoking and myocardial infarction among Sudanese male patients above 40 Years of age. Pol J Radiol. 2016;81:138–140. doi: 10.12659/PJR.894068. 10.12659%2FPJR.894068. [DOI] [PMC free article] [PubMed] [Google Scholar]