Abstract
Background
Mpox, one of the most serious threats to global health, is now being seen in small but rising numbers in Beijing, China. Our study aimed to investigate healthcare workers’ (HCWs) knowledge of Mpox and to explore reasons associated with their hesitancy to vaccinate against Mpox in Beijing, China.
Methods
A cross-sectional study was conducted among HCWs in Beijing from July 24 to August 2, 2023, through an online questionnaire. Participants answered questions about sociodemographic characteristics, Mpox information sources, Mpox knowledge, perception of vaccines, and attitudes toward Mpox vaccination. We used Chi-squared test to compare difference in Mpox vaccination hesitancy between different groups. Multivariable logistic regression models were applied to analyze correlates of vaccination hesitancy among HCWs.
Results
A total of 2331 HCWs completed the questionnaire, with an effective response rate of 92.45 % (2155/2331). Most of the HCWs in this study worked at tertiary hospitals (89.65 %), with a mean age of 36.69 ± 9.08 years. Among the 2155 participants, 52.99 % had over ten years of working experience, and 16.66 % were from high-risk departments relevant to Mpox treatment. Approximately 84.41 % knew about Mpox before this study, 80.79 % exhibited a high level of knowledge about Mpox, whereas 42.37 % were hesitant to be vaccinated against Mpox. Moreover, the hesitancy rate of HCWs in high-risk departments (47.91 %) was higher than in lower-risk departments (41.26 %). Higher educational level (aOR = 1.75, 95 %CI: 1.17–2.62), longer working years (1.71, 1.32–2.22), working at high-risk departments (1.34, 1.05–1.71), and lower level of knowledge about Mpox (1.78, 1.13–2.85) appeared as the most significant determinants of Mpox vaccination hesitancy among HCWs who knew about Mpox. For the HCWs who did not know about Mpox, longer working years (1.96, 1.02–3.78) were significant factors associated with their hesitancy. The predominant reason for hesitancy toward Mpox vaccination among HCWs encompassed apprehensions about vaccine side effects.
Conclusion
HCWs had good knowledge of Mpox, whereas their Mpox vaccination hesitancy was also relatively high in Beijing, China. Increasing HCWs’ vaccination confidence and knowledge level about Mpox, especially for those working in high-risk departments, may be an essential way of reducing their hesitancy.
Keywords: Mpox, Vaccines hesitancy, Healthcare workers, Knowledge, China
1. Introduction
Mpox caused by orthopoxvirus, a double-stranded DNA virus, has become one of the most noticeable threats to global health [1]. The first Mpox case was detected in the Democratic Republic of the Congo in 1970 [2]. Recently, cases of Mpox have been reported frequently from countries where the disease is not endemic [3]. This phenomenon may be related to the cessation of smallpox vaccination, which provided some cross-protection against Mpox, leading to increased human-to-human transmission [4], [5]. Since the eradication of smallpox was announced by the World Health Assembly in 1980, routine vaccination against smallpox has not been mandated, and immunity to the orthopoxvirus in young people has continuously waned over time [6], [7]. With the spread of the Mpox virus, two cases were released in June 2023 [8]. It was the first report from Beijing. According to the surveillance data, a total of 80 new cases of Mpox were reported on the Chinese mainland during November of 2023, with Beijing contributing 10 cases, the second-highest reported cases [9]. As of 1 December 2023, a total of 1513 confirmed cases of Mpox have been reported in China [10].
Emerging evidence suggests vaccines are an effective adjunct to other public health interventions in the context of the Mpox outbreak response [5], [11], [12], [13]. Judicious use of vaccines can protect vulnerable groups at risk of severe Mpox disease and minimize zoonotic transmission of Mpox virus. Based on assessed risks and benefits, WHO recommends taking primary preventive vaccination and post-exposure prophylaxis for individuals with high Mpox risk [5]. Laboratory personnel working with orthopoxviruses, clinical laboratory and health care personnel performing diagnostic testing for Mpox, and outbreak response team members were classified as high-risk individuals by WHO [5].
HCWs play an instrumental role in primary prevention and health promotion. Although the transmission of Mpox may be a rare event in the HCWs [14], [15], maintaining vigilance about the risk of occupational exposure to the Mpox virus is essential. According to the Statistical Yearbook of Beijing (2023) [16], there were 276,717 staff working in medical institutions in Beijing, including 83,996 clinicians, 111,841 nurses, and 20,309 medical technicians. Currently, there are three vaccines have been approved in a number of countries/territories for the prevention of Mpox. Unfortunately, none of the available Mpox vaccines have been approved for use in the Chinese mainland, and there are no available Mpox vaccines for HCWs in Beijing. As more and more cases of Mpox are reported in Beijing, proactive investigation of the HCWs' knowledge of Mpox and their attitude toward Mpox vaccination is necessary. Our study aimed to investigate HCWs' knowledge of Mpox and to explore reasons associated with their hesitancy to vaccinate against Mpox in Beijing, China.
2. Methods
2.1. Subjects and inclusion criteria
A cross-sectional study was conducted among HCWs from July 24 to August 2, 2023, through an online questionnaire powered by Wenjuanxing (an online survey platform). Wenjuanxing is a program for questionnaire designing with similar functions to Amazon Mechanical Turk (Survey Monkey, Survey Gizmo). The target population was all the employees in medical institutions, including clinicians, nurses, medical technicians (such as inspection, imaging, ultrasound, electrocardiogram, pharmacy), interns (such as medical students), and other administrative staff. The inclusion criteria for this survey were HCWs who worked in Beijing, were 18 years or older, and volunteered to participate. Snowball sampling methods were used to recruit HCWs. We sent the questionnaire link or QR code to the HCWs who keeping close contact with us in daily work. These close-knit HCWs forwarded the link or QR code to their colleagues through their work groups. HCWs who received the questionnaire could also forward it to another, but each participant was only allowed to submit the questionnaire once. No incentives of any kind are involved in the selection of participants.
2.2. Sample size
The sample size was estimated by the calculation formula of simple random samples, N = [ (Zα/2)2P (1-P)/ d2], and the primary outcome was the hesitancy to vaccinate against Mpox among HCWs in China. The estimated sample size was 973 according to previous Chinese studies among HCWs (9.88 %-35.10 %) [17], [18], α = 0.05, the allowable error was 3 %, and Zα/2 = 1.96. Considering the possible nonconforming feedback, the sample size should be at least 1071, with a margin of 10 %.
2.3. Study variable
The questionnaire was designed according to published studies on Mpox vaccination among HCWs and other studies related to the theme of Mpox [17], [18], [19], [20], [21], [22]. At the same time, we also discussed with experts and conducted a pilot survey before the release of the questionnaire. Our questionnaire for this study consisted of 30 closed-ended items divided into six aspects: a) Sociodemographic characteristics, b) Mpox information sources, c) Mpox knowledge, d) Perception of vaccines, e) Attitudes toward Mpox vaccination, and f) Quality control.
Sociodemographic characteristics included age, sex, educational level, marital status, monthly income, type of medical institution, occupation, professional title, working years, and department. We classified the departments that are involved in the diagnosis, treatment, and management of suspected or confirmed Mpox cases or are at potential risk of contracting the Mpox virus as high-risk departments. These high-risk departments include the infectious diseases department, dermatology department, venereal diseases department, anorectal diseases department, and urology/andrology department.
The awareness of Mpox information was measured by asking whether they knew about Mpox before this survey. Participants who didn't know about Mpox before the survey could skip the rest items of the Mpox information and knowledge. HCWs who knew about Mpox were asked to recall their Mpox information source (digital news portals and social media, traditional media, attending training meetings organized by school/ hospital/ CDC, attending academic conferences, communication with colleagues/ friends, neighborhood committee/ community organizations publicity, etc.) and how often did they get Mpox information every week (daily attention, frequent attention, occasional attention, little attention, and never attention).
Assessment of HCWs’ Mpox knowledge using the subsequent 14 items was only undertaken for the participants who knew about Mpox before this survey. With reference to other research [22], the following Mpox knowledge items were included: 1) Mpox is an infectious disease (TRUE), 2) Mpox is caused by a virus (TRUE), 3)People can get Mpox by close contact with an infected person or animal (TRUE), 4) People are generally susceptible to Mpox (TRUE), 5) There are currently no specific treatments for Mpox (TRUE), 6) There is a vaccine that protects against Mpox (TRUE), 7) Mpox can cause fever (TRUE), 8) Mpox can cause headaches (TRUE), 9) Mpox can cause fatigue or exhaustion (TRUE), 10) Mpox can cause swollen lymph nodes (TRUE), 11) Mpox can cause a body rash (TRUE), 12) Mpox can cause back and muscle aches (TRUE), 13)Selecting the correct transmission routes of Mpox, 14)Which of the following pictures is the Mpox rash.
For items 1–12, there were three options: right, wrong, and don't know. Choosing “right” was recategorized as the correct answer, and other options (including “wrong” and “don't know”) were recategorized as the incorrect answer. For item 13, which was a multiple-choice question, participants should choose at least one correct option and must not include any incorrect options. A correct answer to 8 or more out of 14 items was considered a high level of mpox knowledge.
The perception of vaccines among HCWs was assessed by asking “Do you think it is important to get vaccinated?” This item used a five-point Likert scale ranging from strongly important to strongly unimportant, and the data were recategorized as important (1–2), neutrality (3), and unimportant (4–5) when analyzing the results. Follow up with items like “Do you think vaccination is safe?” and “Do you think vaccination is effective?” We also used a five-point Likert scale ranging from strongly safe/effective to strongly unsafe/ineffective, and the data were recategorized as safe/effective (1–2), neutral (3), and unsafe/ineffective (4–5) when analyzing the results. Respectively, we also asked them about their attitudes toward the safety and effectiveness of domestic and foreign vaccines. Participants were allowed to choose one of three options: domestic vaccines were as good as foreign vaccines, domestic vaccines were better, and foreign vaccines were better.
The Mpox vaccination hesitancy was assessed by asking “Would you like to be vaccinated against Mpox?” All participants (including HCWs who indicated that they did not know about mpox at the start of the survey) need to answer the question about Mpox vaccination hesitancy, and they could choose one of the three options: willing, unwilling, or unsure. Participants who selected “unsure” or “unwilling” were further asked, “Would you like to get the Mpox vaccine if it were free?” Those who were still selected “unsure” or “unwilling” to receive the Mpox vaccine under the condition of free vaccination were classified as the group of Mpox vaccination hesitancy. The questions about the reasons for Mpox vaccine hesitancy were answered only by the participants of the hesitancy group.
To identify the unseriously questionnaires, we also set the following two common sense questions: “Where is the capital of China” and “Which direction does the sun rise in the morning”. The questionnaires with the wrong answer will be excluded.
2.4. Statistics analysis
We removed the questionnaires containing missing values and low quality while cleaning the data. We used Chi-squared test to compare difference in Mpox vaccination hesitancy between different groups. Continuous variables were expressed as mean and standard deviation (SD), and categorical variables were presented with frequency and percentage. Multivariate logistic regression was used to analyze correlates of Mpox vaccination hesitancy among HCWs. In the logistic regression, we adopted the stepwise regression method and calculated the aOR and 95 % confidence interval (95 %CI). All analyses were conducted using R 4.2.3 (R Foundation for Statistical Computing, Vienna, Austria).
2.5. Ethics approval
All procedures contributing to this work comply with the ethical standards of relevant national and institutional committees on human experimentation and with the Helsinki Declaration. Online informed consent will be obtained from all participants before any procedure of this study. The study (including online informed consent) was approved by the Human Research Ethics Committee of the School of Public Health (Shenzhen), Sun Yat-sen University (approval number SYSU-PHS[2022]051).
3. Results
3.1. Demographic characteristics
A total of 2331 questionnaires were received, with an effective response rate of 92.45 % (2155/2331). Among the 2155 participants, the mean age was 36.69 ± 9.08 years, 80.19 % were females, 70.86 % were married, and 80.14 % had a bachelor's degree or above. A large proportion of participants worked at tertiary hospitals (89.65 %), had over ten years of working experience (52.99 %), and exhibited a high level of Mpox knowledge (80.79 %). In addition, 16.66 % of participants in this study were recruited from the high-risk departments where HCWs were most likely to be exposed to patients with Mpox. Characteristics of HCWs were presented in Table 1.
Table 1.
Characteristics of HCWs in Beijing, China (N = 2155).
| Characteristics | Category | Frequency | Percentage (%) |
|---|---|---|---|
| Age | 18∼ | 607 | 28.17 |
| 31∼ | 874 | 40.56 | |
| 41∼ | 451 | 20.93 | |
| ≥51 | 223 | 10.34 | |
| Sex | Male | 427 | 19.81 |
| Female | 1728 | 80.19 | |
| Educational level | Junior college or below | 428 | 19.86 |
| Undergraduate | 1174 | 54.48 | |
| Master | 387 | 17.96 | |
| Doctor degree or higher | 166 | 7.70 | |
| Marital status | Unmarried | 628 | 29.14 |
| Married | 1527 | 70.86 | |
| Monthly income (CNY) | <3000 | 77 | 3.57 |
| 3000–5999 | 298 | 13.83 | |
| 6000–9999 | 938 | 43.53 | |
| 10000–19999 | 762 | 35.36 | |
| ≥20000 | 80 | 3.71 | |
| Type of medical institution | Tertiary hospitals | 1932 | 89.65 |
| Secondary hospitals | 191 | 8.86 | |
| Community health service centers/ private hospitals | 32 | 1.49 | |
| Occupation | Nurses | 1171 | 54.34 |
| Clinicians | 807 | 37.45 | |
| Medical technicians a | 138 | 6.40 | |
| Administrative/ nonclinical support | 39 | 1.81 | |
| Professional title | Junior or below | 952 | 44.18 |
| Intermediate | 901 | 41.81 | |
| Senior | 302 | 14.01 | |
| Working years | ≤5 | 489 | 22.69 |
| 6 ∼ | 524 | 24.32 | |
| ≥11 | 1142 | 52.99 | |
| Department | Low-risk departments | 1796 | 83.34 |
| High-risk departments b | 359 | 16.66 | |
| Mpox knowledge level | Low level | 414 | 19.21 |
| High level c | 1741 | 80.79 |
a: Medical technicians include inspection, imaging, ultrasound, electrocardiogram, pharmacy, etc.
b: High-risk departments include the infectious diseases department, dermatology department, venereal diseases department, anorectal diseases department, urology/andrology department.
c: A correct answer to 8 or more out of 14 questions about Mpox knowledge was considered a high level of knowledge.
3.2. Mpox information and knowledge
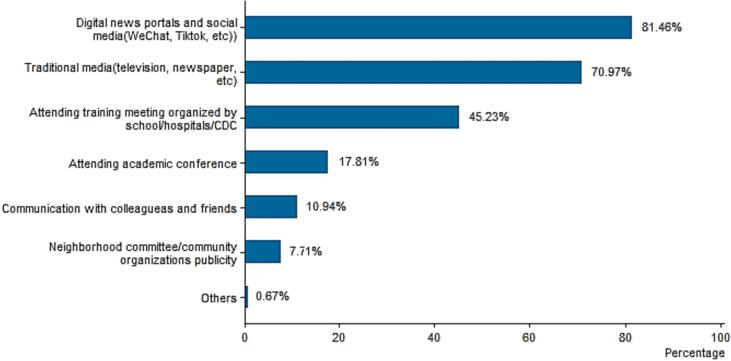
Approximately 1819 (84.41 %) of HCWs indicated that they knew about Mpox before this study. The weekly frequency of getting Mpox information was divided into five levels: daily attention, frequent attention, occasional attention, little attention, and never attention, and the percentages were 5.44 % (n = 99), 27.98 % (n = 509), 55.20 % (n = 1004), 9.84 % (n = 179), and 1.54 % (n = 28) respectively. Digital news portals and social media (i.e. WeChat, TikTok, and other internet media) were the main access for HCWs to get the Mpox information, followed by traditional media (i.e. television, newspaper, radio, etc.). Fig. 1 shows the access way to obtain the Mpox information among HCWs who attention to Mpox.
Fig. 1.
Sources to access Mpox information among HCWs in Beijing, China (n = 1791).
Results indicated that the proportion of participants of young, low educational level, unmarried, worked in low-level hospitals, had low professional titles, had short working years, worked as nurses or medical technicians, and worked in low-risk departments in the group did not know about Mpox were higher than that in the group of knew about Mpox. Table 2 shows the differences in HCWs’ characteristics between those who knew and did not know about Mpox.
Table 2.
Comparison of HCWs’ characteristics between those who knew and did not know about Mpox in Beijing, China.
| Characteristics |
Knew about Mpox before the investigation No. (%) |
Did not know about Mpox before the investigation No. (%) |
χ2 | P |
|---|---|---|---|---|
| Age | 34.35 | <0.01 | ||
| 18∼ | 477 (26.22) | 130 (38.69) | ||
| 31∼ | 734 (40.35) | 140 (41.67) | ||
| 41∼ | 412 (22.65) | 39 (11.61) | ||
| ≥51 | 196 (10.78) | 27 (8.04) | ||
| Sex | 1.11 | 0.29 | ||
| Male | 368 (20.23) | 59 (17.56) | ||
| Female | 1451 (79.77) | 277(82.44) | ||
| Educational level | 14.39 | <0.01 | ||
| Junior college or below | 342 (18.80) | 86 (25.60) | ||
| Undergraduate | 987 (54.26) | 187 (55.65) | ||
| Master | 345 (18.97) | 42 (12.50) | ||
| Doctor degree or higher | 145 (7.97) | 21 (6.25) | ||
| Marital status | 7.24 | <0.01 | ||
| Unmarried | 509 (27.98) | 119 (35.42) | ||
| Married | 1310 (72.02) | 217 (64.58) | ||
| Monthly income (CNY) | 3.73 | 0.44 | ||
| <3000 | 65 (3.57) | 12 (3.57) | ||
| 3000–5999 | 243 (13.36) | 55 (16.37) | ||
| 6000–9999 | 803 (44.15) | 135 (40.18) | ||
| 10000–19999 | 638 (35.07) | 124 (36.90) | ||
| ≥20000 | 70 (3.85) | 10 (2.98) | ||
| Type of medical institution | 12.68 | <0.01 | ||
| Tertiary hospitals | 1649 (90.65) | 283 (84.23) | ||
| Secondary hospitals | 146 (8.03) | 45 (13.39) | ||
| Community health service centers /private hospitals | 24 (1.32) | 8 (2.38) | ||
| Occupation | 27.79 | <0.01 | ||
| Nurses | 947 (52.06) | 224 (66.67) | ||
| Clinicians | 722 (39.69) | 85 (25.30) | ||
| Medical technicians a | 115 (6.32) | 23 (6.85) | ||
| Administrative/ nonclinical support | 35 (1.92) | 4 (1.19) | ||
| Professional title | 20.42 | <0.01 | ||
| Junior or below | 766 (42.11) | 186 (55.36) | ||
| Intermediate | 786 (43.21) | 115 (34.23) | ||
| Senior | 267 (14.68) | 35 (10.42) | ||
| Working years | 19.89 | <0.01 | ||
| ≤5 | 391 (21.50) | 98 (29.17) | ||
| 6 ∼ | 427 (23.47) | 97 (28.87) | ||
| ≥11 | 1001 (55.03) | 141 (41.96) | ||
| Department b | 12.83 | <0.01 | ||
| High-risk departments | 326 (17.92) | 33 (9.82) | ||
| Low-risk departments | 1493 (82.08) | 303 (90.18) |
The results for each knowledge item were shown in Fig. 2. Only three out of the 14 Mpox knowledge items had correct rates below 80 %, while six items had correct rates above 95 %. In this study, the lowest correct rate was the question about the transmission route of Mpox. Nearly 52.37 %(n = 938) of the HCWs chose the wrong option, followed by “There is a vaccine that protects against Mpox” and “Select the correct picture of Mpox”, with error rates of 39.36 % and 38.02 % respectively.
Fig. 2.
Knowledge about Mpox among HCWs in Beijing, China (n = 1819) Notes: For items 1–12, there were three options: right, wrong, and don't know. The answer “don't know” was recategorized as an incorrect answer. For item 13, which was a multiple-choice question, participants should choose at least one correct option and must not include any incorrect options.
3.3. Perception of vaccines
Approximately 67.52 % and 66.31 % of the HCWs had a positive attitude toward the safety and effectiveness of vaccines respectively, and 77.87 % considered that vaccination was important. Among the 2155 participants, nearly 59.68 % believed domestic and foreign vaccines had similar safety, 22.46 % believed foreign vaccines were safer, and 17.86 % believed domestic vaccines were safer. In addition, almost 58.75 % of the HCWs thought the effectiveness of domestic and foreign vaccines were comparable, 24.32 % thought foreign vaccines were more effective, and 16.93 % chose domestic vaccines.
3.4. Mpox vaccination hesitancy
Approximately 44.18 % (n = 952) of the participants did not support the promotion of Mpox vaccination among HCWs, and 42.37 % (n = 913) were hesitant to get the vaccines against Mpox. Chi-squared test results showed that age, educational level, marital status, monthly income, occupation, professional title, working years, hospital department, perceived Mpox, and Mpox knowledge level were significantly associated with Mpox vaccination hesitant among HCWs (Table 3).
Table 3.
Attitude of Mpox vaccination among HCWs in Beijing, China (N = 2155).
| Characteristics |
Hesitant to vaccinate No. (%) |
Willing to vaccinate No. (%) |
χ2 | P |
|---|---|---|---|---|
| Age | 49.21 | <0.01 | ||
| 18∼ | 193 (31.80) | 414 (68.20) | ||
| 31∼ | 377 (43.14) | 497 (56.86) | ||
| 41∼ | 223 (49.45) | 228 (50.55) | ||
| ≥51 | 120 (53.81) | 103 (46.19) | ||
| Sex | 0.02 | 0.88 | ||
| Male | 179 (41.92) | 248 (58.08) | ||
| Female | 734 (42.48) | 994 (57.52) | ||
| Educational level | 16.26 | <0.01 | ||
| Junior college or below | 153 (35.75) | 275 (64.25) | ||
| Undergraduate | 499 (42.50) | 675 (57.50) | ||
| Master | 173 (44.70) | 214 (55.30) | ||
| Doctor degree or higher | 88 (53.01) | 78 (46.99) | ||
| Marital status | 15.14 | <0.01 | ||
| Unmarried | 225 (35.83) | 403 (64.17) | ||
| Married | 688 (45.06) | 839 (54.94) | ||
| Monthly income (CNY) | 14.51 | <0.01 | ||
| <3000 | 23 (29.87) | 54 (70.13) | ||
| 3000–5999 | 112 (37.58) | 186 (62.42) | ||
| 6000–9999 | 386 (41.15) | 552 (58.85) | ||
| 10000–19999 | 353 (46.33) | 409 (53.67) | ||
| ≥20000 | 39 (43.75) | 41 (51.25) | ||
| Type of medical institution | 1.66 | 0.44 | ||
| Tertiary hospitals | 808 (42.08) | 1112 (57.92) | ||
| Secondary hospitals | 88 (43.35) | 115 (56.65) | ||
| Community health service centers /private hospitals | 17 (53.13) | 15 (46.87) | ||
| Occupation | 11.20 | 0.01 | ||
| Nurses | 459 (39.20) | 712 (60.80) | ||
| Clinicians | 368 (45.60) | 439 (54.40) | ||
| Medical technicians a | 68 (29.28) | 70 (50.72) | ||
| Administrative/ nonclinical support | 18 (46.15) | 21 (53.85) | ||
| Professional title | 27.79 | <0.01 | ||
| Junior or below | 346 (36.34) | 606 (63.66) | ||
| Intermediate | 413 (45.84) | 488 (54.16) | ||
| Senior | 154 (50.99) | 148 (49.01) | ||
| Working years | 35.02 | <0.01 | ||
| ≤5 | 163 (33.33) | 326 (66.67) | ||
| 6 ∼ | 201 (38.36) | 323 (61.64) | ||
| ≥11 | 549 (48.07) | 593 (51.93) | ||
| Department b | 5.15 | 0.02 | ||
| High-risk departments | 172 (47.91) | 187 (52.09) | ||
| Low-risk departments | 741 (41.26) | 1055 (58.74) | ||
| Whether know about Mpox before this survey | 5.86 | 0.02 | ||
| Know | 750 (82.15) | 1069 (86.07) | ||
| Unknow | 163 (17.85) | 173 (13.93) | ||
| Mpox knowledge level c | 9.67 | <0.01 | ||
| Low | 204 (49.28) | 210 (50.72) | ||
| High | 709 (40.72) | 1032 (59.28) |
a: Medical technicians include inspection, imaging, ultrasound, electrocardiogram, pharmacy, etc.
b: High-risk departments include the infectious diseases department, dermatology department, venereal diseases department, anorectal diseases department, urology/andrology department.
c: A correct answer to 8 or more out of 14 questions about Mpox knowledge was considered a high level of knowledge.
The results of multivariable logistic regression indicated that factors such as higher educational level (aOR = 1.75, 95 %CI:1.17–2.62), longer working years (1.71, 1.32–2.22), working at high-risk departments (1.34, 1.05–1.71), lower Mpox knowledge (1.78, 1.13–2.85) were associated with a high hesitancy for Mpox vaccine among HCWs who knew about Mpox before the investigation. For the HCWs who did not know about Mpox before the investigation, longer working years (1.96, 1.02–3.78) were significant factors associated with their hesitancy to vaccinate against Mpox (Table 4).
Table 4.
Correlates of Mpox vaccination hesitancy among HCWs in Beijing, China.
| Variables | Knew about Mpox before the investigation | Did not know about Mpox before the investigation | |||
|---|---|---|---|---|---|
| Adjusted OR (95 %CI) | P | Adjusted OR (95 %CI) | P | ||
| Educational level | |||||
| Junior college or below | Ref | ||||
| Undergraduate | 1.16 (0.88–1.52) | 0.29 | |||
| Master | 1.34 (0.97–1.84) | 0.07 | |||
| Doctor degree or higher | 1.75 (1.17–2.62) | <0.01 | |||
| Marital status | |||||
| Unmarried | Ref | ||||
| Married | 1.65 (0.94–2.92) | 0.08 | |||
| Working years | |||||
| ≤5 | Ref | Ref | |||
| 6 ∼ | 1.09 (0.81–1.46) | 0.59 | 1.59 (0.86–2.97) | 0.14 | |
| ≥11 | 1.71 (1.32–2.22) | <0.01 | 1.96 (1.02–3.78) | 0.05 | |
| Department | |||||
| Low-risk departments | Ref | ||||
| High-risk departments a | 1.34 (1.05–1.71) | 0.02 | |||
| Mpox knowledge level | |||||
| High level b | Ref | ||||
| Low level | 1.78 (1.13–2.85) | 0.01 | |||
Data were stratified according to whether knew about Mpox before this study. Statistically significant variables in the chi-squared test were included in the logistic regression model, such as education level, marital status, monthly income, occupation, professional title, working years, departments, and knowledge level. Due to strong collinearity with other variables, age was not included in the model.
a: High-risk departments include the infectious diseases department, dermatology department, venereal diseases department, anorectal diseases department, urology/andrology department.
b: A correct answer to 8 or more out of 14 questions about Mpox knowledge was considered a high level of knowledge.
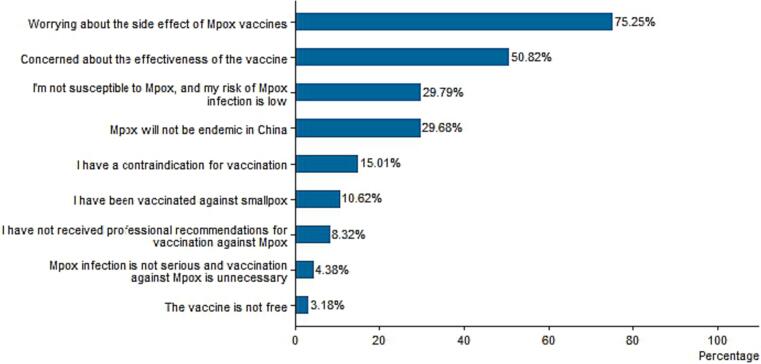
Fig. 3 shows the reasons for HCWs’ hesitancy to be vaccinated against Mpox. According to the results, a total of 913 (42.37 %) HCWs reported they were hesitant to be vaccinated against Mpox. The main reasons for this were that HCWs were worried about the side effects (75.25 %), lacked confidence in the effectiveness of the Mpox vaccines (50.82 %), and believed that their risk of infecting Mpox was low (29.79 %). The first two reasons for hesitation to receive the Mpox vaccine among HCWs working in high-risk departments and low-risk departments were both worried about side effects and lack of confidence in the effectiveness of the Mpox vaccines. However, the third reason among the two groups is different. HCWs working in the high-risk department chose “I'm not susceptible to Mpox, and my risk of Mpox infection is low”, while others working in the low-risk department chose “Mpox will not be endemic in China”.
Fig. 3.
Reasons for HCWs’ hesitancy to get vaccinated against Mpox in Beijing, China (n = 913).
4. Discussion
Our study demonstrated high Mpox knowledge among HCWs in Beijing, whereas their hesitancy towards Mpox vaccination was also relatively high. Higher educational levels, longer working years, working at high-risk departments, and lower Mpox knowledge were significantly associated with Mpox vaccination hesitancy among HCWs. The confidence in the safety and effectiveness of Mpox vaccines among HCWs, especially for HCWs working in high-risk departments, needs to be further increased.
Similar to a previous study conducted in China [17], we found that HCWs in Beijing had good Mpox knowledge. Approximately 80.79 % of the HCWs could correctly answer 8 or more out of 14 Mpox knowledge questions, and only three out of the 14 Mpox knowledge items had correct rates below 80 %. This result seems to be more encouraging than surveys conducted in other countries [17], [18], [19], [23], [24], [25]. A survey conducted in Jordan found that only 60 % of the HCWs have a high level of knowledge about Mpox [23]. At the same time, we also found some HCWs believed that the Mpox virus can be transmitted by insect vectors or the digestive tract. It indicates a potential knowledge gap about the transmission route of Mpox in HCWs. Consistent with studies conducted in other countries [25], digital news portals and social media (i.e. WeChat, TikTok, etc.) were some of the most utilized sources of information about Mpox while more credible sources (i.e. training organized by schools/hospitals/CDC, attending the academic conference) were relied on by a considerably much less percentage of participants. The gaps in Mpox knowledge among HCWs may be addressed by providing correct knowledge and training through digital news portals and social media. Increasing the frequency of training organized by schools/hospitals/CDC and encouraging HCWs to attend academic conferences are also effective ways to improve their knowledge.
We found higher Mpox vaccination hesitancy among HCWs in Beijing. Approximately 42.37 % were hesitant to be vaccinated against Mpox among the HCWs, which is higher than two existing surveys conducted in China [17], [18], but similar to other study results conducted in other countries [26], [27]. Existing surveys found that the Mpox vaccination hesitancy among Chinese HCWs ranged from 35.1 % and 9.9 % [17], [18]. The reasons for the different results between our study and previous studies may be the inconsistency in methods to measure HCW's Mpox vaccination hesitancy and distribute the questionnaire, and the geographical areas of the participants also vary. Furthermore, Mpox vaccination hesitancy among HCWs who have the potential risk for direct or indirect exposure to patients or infectious materials was even higher than among other HCWs. Besides worrying about side effects and lack of confidence about the effectiveness, the third reason for hesitant to be vaccinated against Mpox among HCWs working in high-risk departments was that they do not consider themselves as vulnerable crowd and believe that their risk of infecting Mpox is low. One possible explanation for this finding is that HCWs working in high-risk departments have sufficient knowledge of Mpox and are less worried about Mpox. Another possibility is that HCWs who work in low-risk departments also believe they are more susceptible to Mpox because they may not have access to the same level of personal protective equipment as their colleagues working in the high-risk departments, and therefore, were more willing to vaccinate against the Mpox [28].
In this study, the Mpox vaccination hesitancy among HCWs was significantly associated with educational level, working years, hospital department, and Mpox knowledge level. Similar to previous studies [17], we found that HCWs with higher educational levels, longer working years, lower Mpox knowledge, and worked at high-risk departments were less likely to get the Mpox vaccines. HCWs with higher educational levels and longer working years might have more chances to get information about vaccine adverse events, which increases their vaccine hesitancy. Whereas, Mahameed et al [23] showed the significant role of psychological factors and vaccine conspiracy beliefs. Different from what we found, some scholars also showed that Mpox vaccine acceptance was significantly associated with previous vaccination behavior, while Mpox knowledge was not correlated with Mpox vaccination intention [29].
Meanwhile, we found that HCWs’ confidence in the importance (77.87 %), safety (67.52 %), and effectiveness (66.31 %) of vaccines need to be further improved. The predominant reason for hesitancy toward Mpox vaccination among HCWs was worry about vaccine side effects. A survey in the Czech found that HCWs’ perceived barriers related to Mpox vaccine safety and effectiveness were significantly associated with Mpox vaccine acceptance [19]. Although Mpox transmission is likely a rare event in the provision of medical services, data from investigations of the Mpox virus and other related orthopoxviruses suggested that occupational exposure could occur [30], [31], [32]. To curb the spread of the Mpox virus, some countries have or are developing policies to promote vaccination among those who may be at risk such as laboratory personnel and health workers [12], [33]. Addressing vaccination hesitancy among HCWs can not only facilitate the achievement of public health strategies that aim to protect high-risk groups and individuals, but it may also improve public confidence in vaccines [34], [35].
Our study has several limitations. First, our study was a cross-sectional survey, causality cannot be identified. Second, convenience sampling may lead to section biases, we might lose the information from participants who refuse to participate in the survey or are unconcern about the situation of Mpox, and the HCWs from the basic-level hospitals account for relatively few. HCWs who received the questionnaire could forward it to their colleagues, but it was difficult to calculate the response rate. Third, given that this study relied on a single item to measure vaccination hesitancy as the primary outcome measure, measurement bias may exist. Fourth, the results may be influenced by possible social desirability bias. Finally, we did not test the validity and reliability of the questionnaire. To mitigate this we designed the questionnaire based on questions used in published studies on Mpox vaccination among HCWs and organized a panel of experts to discuss and finalize the questionnaire.
5. Conclusion
Mpox knowledge and Mpox vaccination hesitancy were both high among HCWs in Beijing, China. Increasing HCWs’ vaccination confidence and knowledge level about Mpox, especially for those working in high-risk departments, may be an essential way of reducing their hesitancy.
Funding
This study was supported by the 2021 Beijing Key Specialty Program for Major Epidemic Prevention and Control.
CRediT authorship contribution statement
Yuan Yang: Writing – original draft, Data curation, Investigation. Weijie Zhang: Writing – original draft. Baihui Han: Investigation, Writing – original draft. Han Meng: Conceptualization. Jiaqi Wang: Writing – original draft. Ke Wu: Writing – review & editing. Leiwen Fu: Writing – review & editing. Bingyi Wang: Writing – original draft. Xiaohong Jiang: Writing – review & editing. Qian Li: Writing – review & editing. Zhiyuan Xu: Writing – review & editing. Ye Zhang: Conceptualization. Xiao Qi: Conceptualization, Methodology. Huachun Zou: Conceptualization, Methodology.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We thank our partners, including thirteen hospitals that participated in this survey. We thank all HCWs who helped us forward the questionnaire to their colleagues. We thank all participants who made this research possible.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jvacx.2024.100434.
Contributor Information
Xiao Qi, Email: cyqwjwcdcqx@bjchy.gov.cn.
Huachun Zou, Email: zouhuachun@fudan.edu.cn.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Data availability
Data will be made available on request.
References
- 1.World Health Organization. Responding to the global mpox outbreak: ethics issues and considerations: a policy brief, 19 July 2023[EB/OL]. (https://www.who.int/publications/i/item/ WHO-Mpox-Outbreak_response-Ethics-2023.1); [Accessed 2023/8/27].
- 2.Ladnyj ID, Ziegler P, Kima E. A human infection caused by monkeypox virus in Basankusu Territory, Democratic Republic of the Congo. PMID: 4340218. [PMC free article] [PubMed]
- 3.Guarner J., Del R.C., Malani P.N. Monkeypox in 2022-what clinicians need to know. JAMA. 2022;328(2):139–140. doi: 10.1001/jama.2022.10802. [DOI] [PubMed] [Google Scholar]
- 4.Bunge E.M., Hoet B., Chen L., et al. The changing epidemiology of human monkeypox-A potential threat? A systematic review. PLoS Negl Trop Dis. 2022;16(2):e10141. doi: 10.1371/journal.pntd.0010141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. Vaccines and immunization for monkeypox: Interim guidance, 16 November 2022[EB/OL]. (https://www.who.int/publications/i/item/WHO-MPX-Immunization); [Accessed 2023/8/27].
- 6.Shah H.H., Molani M.K., Shabbir N. Human monkeypox - After 40 years, an unintended consequence of smallpox eradication. Front Public Health. 2022;10:1082586. doi: 10.3389/fpubh.2022.1082586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rimoin A.W., Mulembakani P.M., Johnston S.C., et al. Major increase in human monkeypox incidence 30 years after smallpox vaccination campaigns cease in the Democratic Republic of Congo. Proc Natl Acad Sci U S A. 2010;107(37):16262–16267. doi: 10.1073/pnas.1005769107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beijing Center for Disease Control and Prevention. Two cases of monkeypox were found in Beijing and their health implications[EB/OL]. (https://www.bjcdc.org/cdcmodule/jkdt/bsxw/2023/ 103589.shtml); [Accessed 2023/8/27].
- 9.Chinese Center for Disease Control and Prevention. Surveillance of Monkeypox in mainland China in November, 2023[EB/OL]. (https://www.chinacdc.cn/jkzt/crb/zl/szkb_13037/gnyq/202312/t20231213_271328.html); [Accessed 2023/8/27].
- 10.US. Centers for Disease Control and Prevention. 2022-2023 Mpox Outbreak Global Map [EB/OL]. (https://www.cdc.gov/poxvirus/mpox/response/2022/world-map.html); [Accessed 2023/12/21].
- 11.Fahrni M.L., Priyanka S.A., et al. Monkeypox: Prioritizing public health through early intervention and treatment. Int J Surg. 2022;104 doi: 10.1016/j.ijsu.2022.106774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Choudhary O.P., Priyanka F.ML., et al. Ring vaccination for monkeypox containment: Strategic implementation and challenges. Int J Surg. 2022;105 doi: 10.1016/j.ijsu.2022.106873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saadh M.J., Ghadimkhani T., Soltani N., et al. Progress and prospects on vaccine development against monkeypox infection. Microb Pathog. 2023;180 doi: 10.1016/j.micpath.2023.106156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fleischauer A.T., Kile J.C., Davidson M., et al. Evaluation of human-to-human transmission of monkeypox from infected patients to health care workers. Clin Infect Dis. 2005;40(5):689–694. doi: 10.1086/427805. Evaluation of human-to-human transmission of monkeypox from infected patients to health care workers. [DOI] [PubMed] [Google Scholar]
- 15.Choi Y., Jeon E.B., Kim T., et al. Case Report and Literature Review of Occupational Transmission of Monkeypox Virus to Healthcare Workers, South Korea. Emerg Infect Dis. 2023;29(5):997–1001. doi: 10.3201/eid2905.230028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beijing Municipal Bureau of Statistics. Statistical Yearbook of Beijing (2023) [EB/OL]. (https://nj.tjj.beijing.gov.cn/nj/main/2023-tjnj/zk/indexch.htm); [Accessed 2023/12/27].
- 17.Peng X., Wang B., Li Y., et al. Perceptions and worries about monkeypox, and attitudes towards monkeypox vaccination among medical workers in China: A cross-sectional survey. J Infect Public Health. 2023;16(3):346–353. doi: 10.1016/j.jiph.2023.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hong J., Pan B., Jiang H.J., et al. The willingness of Chinese healthcare workers to receive monkeypox vaccine and its independent predictors: A cross-sectional survey. J Med Virol. 2023;95(1):e28294. doi: 10.1002/jmv.28294. [DOI] [PubMed] [Google Scholar]
- 19.Riad A., Drobov A., Rozmarinova J., et al. Monkeypox knowledge and vaccine hesitancy of czech healthcare workers: a health belief model (HBM)-based study. Vaccines (Basel) 2022;10(12) doi: 10.3390/vaccines10122022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ghazy R.M., Okeh D.U., Sallam M., et al. Psychological antecedents of healthcare workers towards monkeypox vaccination in Nigeria. Vaccines (Basel) 2022;10(12) doi: 10.3390/vaccines10122151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miraglia D.G.G., Della P.G., Folcarelli L., et al. Knowledge and attitudes of health care workers about monkeypox virus infection in Southern Italy. Front Public Health. 2023;11:1091267. doi: 10.3389/fpubh.2023.1091267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ren F., Liu J., Miao J., et al. Public awareness, specific knowledge, and worry about mpox (monkeypox): A preliminary community-based study in Shenzhen, China. Front Public Health. 2023;11:1077564. doi: 10.3389/fpubh.2023.1077564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mahameed H., Al-Mahzoum K., AlRaie L.A., et al. Previous vaccination history and psychological factors as significant predictors of willingness to receive mpox vaccination and a favorable attitude towards compulsory vaccination. Vaccines (Basel) 2023;11(5) doi: 10.3390/vaccines11050897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alhasan K., Sallam M., Aljamaan F., et al. Mpox perceptions and vaccine advocacy among the healthcare workers of solid organ transplant centers: A multicenter, cross-sectional survey in Saudi Arabia. Healthcare (Basel) 2023;11(4) doi: 10.3390/healthcare11040603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sallam M., Al-Mahzoum K., Al-Tammemi A.B., et al. Assessing healthcare workers' knowledge and their confidence in the diagnosis and management of human monkeypox: a cross-sectional study in a middle eastern country. Healthcare (Basel) 2022;10(9) doi: 10.3390/healthcare10091722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ulloque-Badaracco J.R., Alarcon-Braga E.A., Hernandez-Bustamante E.A., et al. Acceptance towards monkeypox vaccination: a systematic review and meta-analysis. Pathogens. 2022;11(11) doi: 10.3390/pathogens11111248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lounis M., Riad A. Monkeypox (MPOX)-related knowledge and vaccination hesitancy in non-endemic countries. Concise Literature Review Vaccines (Basel) 2023;11(2) doi: 10.3390/vaccines11020229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kuter B.J., Browne S., Momplaisir F.M., et al. Perspectives on the receipt of a COVID-19 vaccine: A survey of employees in two large hospitals in Philadelphia. Vaccine. 2021;39(12):1693–1700. doi: 10.1016/j.vaccine.2021.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ricco M., Ferraro P., Camisa V., et al. When a neglected tropical disease goes global: knowledge, attitudes and practices of italian physicians towards monkeypox, preliminary results. Trop Med Infect Dis. 2022;7(7) doi: 10.3390/tropicalmed7070135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vaughan A., Aarons E., Astbury J., et al. Human-to-human transmission of monkeypox virus, United Kingdom, October 2018. Emerg Infect Dis. 2020;26(4):782–785. doi: 10.3201/eid2604.191164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Le Pluart D., Ruyer-Thompson M., Ferre V.M., et al. A healthcare-associated infection with monkeypox virus of a healthcare worker during the 2022 outbreak. Open Forum Infect Dis. 2022;9(10) doi: 10.1093/ofid/ofac520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sah R., Mohanty A., Singh P., et al. Monkeypox and occupational exposure: Potential risk toward healthcare workers and recommended actions. Front Public Health. 2022;10:1023789. doi: 10.3389/fpubh.2022.1023789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Health Organization. Vaccines and immunization for monkeypox: Updated interim guidance, 24 August 2022[EB/OL]. (https://www.who.int/news/item/24-08-2022-vaccines-and-immunization-for-monkeypox--interim-guidance--14-june-2022); [Accessed 2023/8/27].
- 34.Svartstein A.W., Knudsen A.D., Heidari S.L., et al. Mpox incidence and vaccine uptake in men who have sex with men and are living with HIV in Denmark. Vaccines (Basel) 2023;11(7) doi: 10.3390/vaccines11071167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.de Figueiredo A., Simas C., Karafillakis E., et al. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: a large-scale retrospective temporal modelling study. Lancet. 2020;396(10255):898–908. doi: 10.1016/S0140-6736(20)31558-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.