Summary
Background
In the U.S. and globally, dominant metrics of contraceptive access focus on the use of certain contraceptive methods and do not address self-defined need for contraception; therefore, these metrics fail to attend to person-centeredness, a key component of healthcare quality. This study addresses this gap by presenting new data from the U.S. on preferred contraceptive method use, a person-centered contraceptive access indicator. Additionally, we examine the association between key aspects of person-centered healthcare access and preferred contraceptive method use.
Methods
We fielded a nationally representative survey in the U.S. in English and Spanish in 2022, surveying non-sterile 15-44-year-olds assigned female sex at birth. Among current and prospective contraceptive users (unweighted n = 2119), we describe preferred method use, reasons for non-use, and differences in preferred method use by sociodemographic characteristics. We conduct logistic regression analyses examining the association between four aspects of person-centered healthcare access and preferred contraceptive method use.
Findings
A quarter (25.2%) of current and prospective users reported there was another method they would like to use, with oral contraception and vasectomy most selected. Reasons for non-use of preferred contraception included side effects (28.8%), sex-related reasons (25.1%), logistics/knowledge barriers (18.6%), safety concerns (18.3%), and cost (17.6%). In adjusted logistic regression analyses, respondents who felt they had enough information to choose appropriate contraception (Adjusted Odds Ratio [AOR] 3.31; 95% CI 2.10, 5.21), were very (AOR 9.24; 95% CI 4.29, 19.91) or somewhat confident (AOR 3.78; 95% CI 1.76, 8.12) they could obtain desired contraception, had received person-centered contraceptive counseling (AOR 1.72; 95% CI 1.33, 2.23), and had not experienced discrimination in family planning settings (AOR 1.58; 95% CI 1.13, 2.20) had increased odds of preferred contraceptive method use.
Interpretation
An estimated 8.1 million individuals in the U.S. are not using a preferred contraceptive method. Interventions should focus on holistic, person-centered contraceptive access, given the implications of information, self-efficacy, and discriminatory care for preferred method use.
Funding
Arnold Ventures.
Keywords: Contraception, Health care quality, Health care access, Family planning, Unmet need, Person-centeredness, United States
Research in context.
Evidence before this study
In the U.S., common metrics of contraceptive access do not attend to self-defined need for contraception; therefore, these metrics neglect person-centeredness, a key component of healthcare quality, and the preference-sensitive nature of contraceptive decision-making.
We searched PubMed for relevant publications until June 7, 2023 using the search terms (contracept∗ OR birth control OR family planning) AND (preferred method) AND (United States). We also identified relevant publications in the grey literature. One key study, a 2022 report of nationally representative survey data from Frederiksen and colleagues, found that 25% of female contraceptive users in the U.S. were not using their preferred contraceptive method. Another analysis by Legasse and colleagues of nationally representative survey data from 2015 to 17 found that 22% of 15–44-year-old women who had “heterosexual intercourse” in the last three months and were not pregnant or trying to become pregnant would use a different contraceptive method if cost was not a consideration.
Added value of this study
This study advances a new person-centered metric of contraceptive access: use of preferred contraceptive method. Unlike previous research, we include prospective contraceptive users—individuals not currently using a method but who indicated there was a method they would like to use, as well as people who may use contraception for reasons outside pregnancy prevention. We developed this metric through a collaborative process that engaged stakeholders from sectors including reproductive justice, advocacy, research, and healthcare provision.
We use nationally representative data to describe the level of preferred method use among current and prospective contraceptive users and investigate its association with key aspects of person-centered healthcare access. The analysis includes 15-44-year-olds who were assigned female sex at birth and are not known to be sterile. We find that, while most current and prospective contraceptive users in the U.S. are using their preferred method, a quarter would rather use a(nother) method, translating to an estimated 8.1 million individuals. Those who preferred another method were most frequently interested in oral contraception and vasectomy. In regression analyses, we found strong relationships between preferred contraceptive method use and four components of person-centered healthcare access: having enough information to decide about the best contraception, confidence in one's ability to obtain desired contraception, receipt of person-centered contraceptive counseling, and never experiencing discrimination in family planning settings.
Implications of all the available evidence
Use of preferred contraceptive method captures one aspect of person-centered contraceptive access, attending to individual preferences and the dynamic nature of contraceptive use. These data, along with the extant research, demonstrate the value of focusing on preferred method use as a metric of contraceptive access and highlight the need to intervene upon barriers to preferred method use among over 8 million individuals in the U.S. Our study suggests the need for strategies to expand access to oral contraception and vasectomy. This analysis also underscores the importance of a holistic, person-centered approach to conceptualizing healthcare access, given the strong relationships between preferred method use and information, self-efficacy, person-centered contraceptive counseling, and non-discriminatory care.
Introduction
Being able to manage one's fertility in an acceptable, desired, and dignified manner is a key component of sexual and reproductive health equity (SRHE), defined as systems ensuring that all individuals have what they need to attain their highest level of sexual and reproductive health, including reproductive self-determination (the ability to decide if, when, and how to become pregnant and parent).1 The importance of SRHE in the U.S. has been elevated since the overturning of Roe v. Wade in 2022 and the loss of a constitutional right to abortion, as well as the prominence of broader threats to reproductive and bodily self-determination.2 Meanwhile, increasing misinformation about contraception and efforts to restrict access to certain methods under the false claim that they are abortifacients may further hinder contraceptive access.3, 4, 5
Contraceptive use is a preference-sensitive decision, as most individuals have multiple medically appropriate options6; yet policy conversations regarding contraceptive access often fail to center the extremely personal nature of contraceptive decision-making and instead focus on increasing access to and use of specific methods.1 In recent years, policies and programs have prioritized long-acting reversible contraceptives (LARC), such as intrauterine devices (IUDs) and contraceptive implants, given their long duration of use and high effectiveness rates in preventing pregnancy. These efforts, however, can undermine reproductive self-determination by neglecting prospective users’ preferences.7
Likewise, current approaches to defining and tracking contraceptive access in the U.S. tend to focus narrowly on contraceptive method use and services provided, often constrained by typically available data. For example, performance measures for facility-based “healthcare quality” include clinic-level reports of the proportion of women aged 15–44 years at risk of unintended pregnancy who are provided a most effective (i.e., permanent contraception, LARC) or moderately effective (i.e., injectables, pills, patch, ring, or diaphragm) contraceptive method.8 These performance measures do not shed light on the extent to which individuals requested or desired the methods that they received. Similarly, a Healthy People 2030 national public health goal is to increase the proportion of women at risk for unintended pregnancy who use effective birth control.9 Both metrics also focus on risk of unintended pregnancy, which is increasingly seen as an unhelpful and potentially harmful measure because of the ways that it perpetuates normative values about appropriate reproduction and its poor conceptualization and measurement.1,10 Further, conventional metrics of contraceptive access and quality also exclude the many people who use contraception for reasons other than pregnancy prevention,11 as well as people who use or would like to use vasectomy, reinforcing gendered norms around pregnancy prevention.12 Finally, like much of the existing research, these metrics do not define who is included in the population of “women,” nor do they specify whether and how gender identity is assessed, communicating a presumed focus on cisgender women.
Focusing on use of certain methods in quality and access metrics neglects that users may want to switch or stop using methods, since method discontinuation and switching are inherently part of the dynamic journey of contraceptive use.13, 14, 15 In a 2022 nationally representative survey of adult U.S. women, 25% of contraceptive users indicated a preference for a different method.16 The most recent National Survey of Family Growth asked respondents what method they would use if cost was not a worry; in 2015–17, 22% of U.S. women who had “heterosexual intercourse” in the last three months and were not pregnant or trying to become pregnant would use a different method, with the highest level of unsatisfied preferences among Black and Latinx women and low-income women.17 Understanding preferred method use is also critical for appropriate inclusion of people not using contraception in metrics. Given the many reasons for using or not using contraception, automatic classification of people as being in “need” of contraception based on demographic characteristics (e.g., reproductive age, marital status, gender identity) or risk of unintended pregnancy results in an inaccurate understanding of who “needs” contraception and related healthcare.
Given the lack of attention to self-defined contraceptive needs, current contraceptive access metrics and public health goals neglect one of the six key domains of healthcare quality according to the Institute of Medicine—person-centeredness.18 Implicitly, they also overlook the related domains of equity (given that historically marginalized communities may be considered “at-risk” and therefore designated as having greater need for more effective contraceptive methods,7 as well as receive lower-quality care19) and efficiency (in that contraceptive access efforts may waste resources if they are based on external assumptions about who “needs” contraception). Self-defined needs are also key to conceptualizing contraceptive access. In their framework for patient-centered healthcare access, Levesque and colleagues (2013) define access as “the opportunity to reach and obtain appropriate health care services in situations of perceived need for care.”20 As relevant to the current paper, the framework highlights appropriateness of healthcare as a key dimension of person-centered access, particularly related to the ability to engage with healthcare. Important factors related to the ability to engage include the interpersonal quality of care, health literacy, and self-efficacy.20 This framework—and others specific to contraception11,21,22—highlight self-defined needs as a key component of person-centered healthcare access, particularly relevant in the context of preference-sensitive contraceptive decision-making. In contrast to the previously described metrics that focus on use of “effective” methods, measuring whether a person is using a preferred contraceptive method captures a key aspect of person-centered contraceptive access.
This analysis sought to advance a person-centered approach to tracking contraceptive access. The aims of the study were: (1) to describe the use of preferred contraceptive method among a nationally representative sample of current and prospective contraceptive users in the U.S.; and (2) to examine the relationship between aspects of person-centered healthcare access (information to support choosing a method, confidence in being able to obtain contraception, interpersonal quality of contraceptive counseling, and experiences of discrimination in family planning settings) and use of preferred method of contraception.20 In centering preferred method use, this study also responds to a recent call to use and develop indicators measuring fulfillment of method preferences as a way to center reproductive self-determination and high-quality care.23
Methods
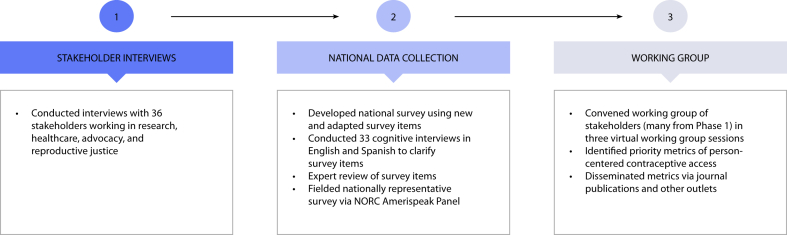
This project utilized a three-phase process that sought to disrupt norms in knowledge production that prioritize the perspective of traditional academic researchers (see Fig. 1).24 In contraceptive research, this paradigm has resulted in the previously described measures that fail to attend to the needs of those most affected by contraceptive access barriers.11 First, we interviewed 36 individuals working across sectors, including research, healthcare provision, advocacy, and reproductive justice. We asked interviewees to define contraceptive need and preferences, what issues they saw with existing measurement approaches, and for recommendations for alternative measures. Second, using insights from interviews and the existing literature, we developed new and modified existing survey questions to quantify key aspects of person-centered contraceptive access.20 We conducted 33 cognitive interviews in English and Spanish to understand how survey respondents would make sense of the questions and whether they captured the intended constructs. We fielded refined questions in a nationally representative survey. Finally, we convened a working group with individuals representing multiple sectors (many of whom participated in the first phase) to select priority metrics. Members of the working group participated in the project as co-researchers, shaping the formulation of metrics, identifying how each metric advanced SRHE, and collaborating on dissemination efforts. This paper reports data from the national survey phase of the project, with a focus on one priority metric identified by the working group: use of preferred contraceptive method. The Committee for the Protection of Human Subjects at the University of California, Berkeley and the Institutional Review Board at NORC at the University of Chicago approved the study protocol.
Fig. 1.
Person-centered contraceptive access metrics project overview.
Data source
Between January 13th and March 14th, 2022, we collected nationally representative survey data through NORC's AmeriSpeak Panel. AmeriSpeak covers an estimated 97% of U.S. households and includes 54,001 members from over 43,000 households.25 We completed a power analysis to determine a target sample size with sufficient statistical power for primary descriptive analyses to detect differences between the largest racial/ethnic groups, as well as within other subgroups, such as age groups. Eligibility criteria included being between the ages 15 and 44; assigned female sex at birth; not known to be sterile; and able to complete the survey in English or Spanish. To assess sex-related eligibility, we included a screening question, “What was your sex assigned at birth, on your original birth certificate?” (female; male). To assess sterility, we asked two questions: 1) Have you had a hysterectomy or sterilization procedure (a tubal ligation, “getting your tubes tied,” or Essure)? (yes; no); 2) Has a doctor or other healthcare provider ever told you that you are infertile (cannot get pregnant) or that you might have difficulty getting pregnant? (yes, a doctor/healthcare provider told me that I am infertile and cannot get pregnant; yes, a doctor/healthcare provider told me that I might have difficulty getting pregnant; no).
NORC invited active AmeriSpeak panelists meeting the age and sex criteria to complete survey screening. Prior to beginning the screening survey, panelists read an online informed consent form and indicated their consent by clicking “yes.” Eligible panelists proceeded to the full survey. For panelists ages 15–17, NORC first obtained parental consent before inviting their children to participate. These 15-17-year-old panelists then indicated their informed assent before screening. Among eligible panelists completing screening, 97.1% of 18–44-year-olds and 97.6% of 15–17-year-olds completed the survey. The median survey completion time was 25 min. NORC provided participant remuneration in the form of their cash equivalent “AmeriPoints” system. Participants received the equivalent of $8 for survey completion.
Measures
Our primary measure of interest is use of preferred contraceptive method; per the person-centered healthcare access framework, the ability to realize one's contraceptive preferences represents a successful outcome in the cumulative process of navigating contraceptive access (from information seeking to contraceptive use).20 The numerator of this measure captures a desire to maintain use of a current method(s)—that is, respondents do not prefer to use a different method and do not desire to stop using their current method(s). We asked respondents, “Is there a method of birth control that you would like to use but you are not currently using?” (yes; no; I don't know). We first categorized “no” responses as using a preferred method and “yes” responses as not using a preferred method. We classified responses of “I don't know” as “uncertain.” We then refined the classification of preferred method use by looking at an additional question about desire to discontinue current contraceptive method use. We asked current contraceptive users, “Do you want to stop using [current method] in the next year?” (yes; no; maybe) for each method they were using. We asked those answering “yes” to indicate when they wanted to stop using that method (as soon as possible; sometime in the next 6 months; sometime in the next year; I'm not sure). Current contraceptive users who (1) did not indicate there was another method they would like to use; and (2) reported they wanted to stop using any current method as soon as possible were recategorized as “uncertain,” as their desire to discontinue their method(s) made it unclear whether they were using a preferred method, and yet we also did not have enough information to categorize them as not using a preferred method. This recategorization included multiple method users who wanted to stop using at least one method being classified as uncertain; wanting to stop using one method as soon as possible suggested that users did not meet the criteria of desire to maintain their current mix of contraceptive methods. We asked respondents not using a preferred method what method(s) they would rather be using and reasons for non-use of preferred method (See Supplementary Material for survey questions.)
We assessed four aspects of person-centered healthcare access in relation to preferred contraceptive method use: two measures that represented self-efficacy to access preferred methods and two that captured interpersonal quality of past contraceptive care. For the domain of self-efficacy, we asked all respondents: 1) “Do you feel like you currently have enough information to make a decision about the birth control method(s) that is best for you?” (yes; no; I'm not sure); and 2) “In general, how confident are you that you can get the birth control that you want, when you want it?” (not confident; somewhat confident; very confident).
For interpersonal quality of care, we included measures of discrimination and quality of contraceptive counseling. We asked respondents who had ever discussed contraception with a healthcare provider about nine types of discrimination in family planning settings during their lifetimes, using an existing measure.26 The measure asks individuals if, while receiving birth control or family planning services, they had ever experienced the following because of their race, ancestry, or national origin: 1) You were treated with less courtesy than other people; 2) You were treated with less respect than other people; 3) You received poorer service than other people; 4) You felt like a doctor or nurse was not listening to what you were saying; 5) A doctor or nurse assumed you were on welfare; 6) A doctor or nurse made assumptions about the number of children you have; 7) A doctor or nurse assumed you had multiple sexual partners; 8) A doctor or nurse strongly encouraged you to use one method of birth control when you preferred another; 9) A doctor or nurse assumed you had a sexually transmitted disease, such as chlamydia, gonorrhea, genital warts, herpes, or HIV. We created a categorical variable describing the number of types of discrimination ever experienced (0, 1–4, 5–9). We also used the Person-Centered Contraceptive Counseling (PCCC) Measure, in which respondents rate their most recent contraceptive care provider on four aspects of person-centered counseling: 1) Respecting you as a person; 2) Letting you say what mattered to you about your birth control; 3) Taking your preferences about your birth control seriously; 4) Giving you enough information to make the best decision about your birth control method.27 Following PCCC scoring conventions, we constructed a binary variable indicating receipt of person-centered contraceptive counseling (“excellent” ratings on all four items).
The dataset included sociodemographic items and sexual and reproductive health characteristics, including sexual and pregnancy history, experience with contraception, and parenting status. NORC provided respondents’ previously collected race/ethnicity data using the following six categories: white, non-Hispanic; Black, non-Hispanic; other, non-Hispanic; Hispanic; 2+ races, non-Hispanic; Asian/Pacific Islander, non-Hispanic. To ascertain current gender, we asked, “What is your current gender identity?” (woman; man; transgender man; genderqueer; non-binary; another gender identity); respondents could select multiple response options. Within the survey, we defined birth control as “anything a person might take, do, or use to prevent pregnancy, prevent sexually transmitted infections (STIs), OR other reasons people might use birth control, like regulating their menstrual cycle or treating medical conditions.” We also noted that birth control includes “things you need a prescription for, condoms, permanent surgeries, not having sex at all, and other things.” We defined current contraceptive use as any method used in the past month; respondents could indicate use of multiple methods.
Sample
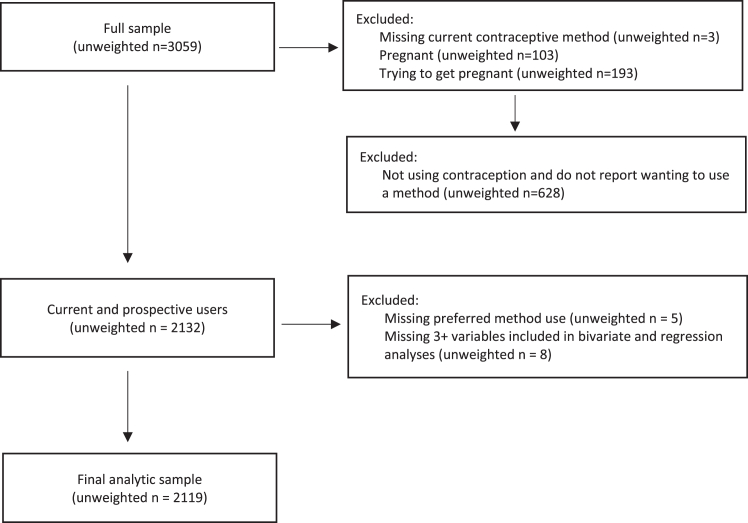
3059 people completed the survey. In contrast to existing approaches that classify individuals as needing contraception based on demographic characteristics and sexual behavior rather than their preferences, the working group determined that the most appropriate sample within which to examine use of preferred method was current and prospective contraceptive users who were not currently pregnant or trying to become pregnant (unweighted n = 2132). Current contraceptive users (unweighted n = 1988) were using any method, including prescription methods, condoms, partner's vasectomy, and other methods (e.g., fertility-awareness-based methods). Prospective contraceptive users (unweighted n = 144) were not using contraception at the time of the survey but indicated there was a method they would like to use. We excluded five current contraceptive users missing data on preferred method use and an additional eight current and prospective users missing data on three or more variables included in bivariate and regression analyses. NORC constructed survey weights using the following raking dimensions for adults: age, education, race/ethnicity, marital status, number of children in household, and age by race/ethnicity. Survey weights account for differences between the U.S. population and the sample on these characteristics. The final sample (unweighted n = 2119; see Fig. 2) includes 69.3% of individuals who completed the survey and is representative of an estimated 32,395,624 individuals in the U.S.
Fig. 2.
Analytic sample construction.
Analytic approach
We generated descriptive statistics for preferred contraceptive method use, sociodemographic and reproductive health characteristics, and contraceptive experiences and preferences. Using the population sample weights constructed by NORC, we present 95% confidence intervals (CIs) and generated the estimated population size for each category of preferred contraceptive method use (using, not using, uncertain). In bivariate analyses, we examined the association between preferred method use and key sociodemographic characteristics. Bivariate associations are presented for variables with at least five respondents in each cell using the Rao-Scott corrected chi-squared test.28, 29, 30 Because we did not correct for multiple comparisons, we present the full range of p-values; however to account for the concern that multiple comparisons increase the risk of Type 1 error, we focus our discussion on relationships with p-values <0.01. We conducted logistic regression analyses to investigate the association between aspects of person-centered healthcare access and use of preferred method.20 Regression analyses focused on having enough information to choose the most appropriate contraceptive method and level of confidence in obtaining contraception, as well as receipt of person-centered contraceptive counseling and lifetime experiences of discrimination in family planning settings among those who had ever discussed contraception with a healthcare provider. To explicitly examine how these aspects of person-centered healthcare access are associated with use of preferred method, we focused on a binary version of this variable: affirmative use of preferred method compared to the other two responses (not using and uncertain). Regression analyses adjusted for age, race/ethnicity, relationship status, pregnancy history, educational attainment, insurance, employment status, and largest affordable emergency expense. We conducted all analyses using Stata statistical analysis software (version 17.0), applying svy commands to account for weighting and complex survey design. All reported proportions are weighted. Unweighted n's are included in the tables.
Role of the funding source
The funder did not have a role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Results
Characteristics of the sample are presented in Table 1 (sociodemographic) and 2 (reproductive health and healthcare experiences). Regarding key aspects of person-centered healthcare access, 77.9% of respondents felt they currently had sufficient information for contraceptive decision-making, while 56.4% felt very confident and 38.4% somewhat confident about being able to obtain desired contraception when they wanted it (Table 2). Less than half (44.5%) reported no lifetime experiences of discrimination in family planning settings, while about a third (35.1%) had experienced person-centered contraceptive counseling the last time they discussed contraception with a healthcare provider.
Table 1.
Sociodemographic characteristics of current & prospective contraceptive users (ages 15–44) in a 2022 U.S. national sample.
| Weighted % | Unweighted n | |
|---|---|---|
| Age | ||
| 15–17 | 8.0 | 89 |
| 18–24 | 28.1 | 223 |
| 25–29 | 21.7 | 467 |
| 30–34 | 19.0 | 515 |
| 35–39 | 13.1 | 474 |
| 40–44 | 10.1 | 351 |
| Current gender identity | ||
| Woman | 96.9 | 2066 |
| Man | 0.3 | 7 |
| Transgender man | 0.0 | 0 |
| Genderqueer, non-binary, fluid, non-conforming, agender, or another gender | 1.2 | 23 |
| More than one gender | 1.2 | 14 |
| Missing | 0.4 | 9 |
| Current sexual orientation | ||
| Straight/heterosexual | 80.5 | 1806 |
| Gay/lesbian | 1.2 | 18 |
| Bisexual | 14.7 | 224 |
| Queer | 1.9 | 42 |
| Something else | 1.4 | 21 |
| Missing | 0.3 | 8 |
| Race/ethnicity | ||
| White only | 54.9 | 1210 |
| Black only | 12.7 | 253 |
| Latinx/Hispanic | 22.2 | 388 |
| Asian/Pacific Islander only | 6.3 | 139 |
| Another race/ethnicity only | 0.6 | 25 |
| Multiracial, not including Latinx/Hispanic | 3.4 | 104 |
| Relationship status | ||
| Married, engaged, or in a serious relationship | 54.8 | 1412 |
| In another type of relationship | 24.9 | 380 |
| Not in a relationship (including divorcing/separating) | 19.8 | 319 |
| Missing | 0.5 | 8 |
| Highest education completed | ||
| Less than high school | 14.5 | 149 |
| High school or equivalent | 19.4 | 246 |
| Vocational or technical school, some college, or associates degree | 33.0 | 754 |
| Bachelor's degree | 23.0 | 642 |
| Post graduate study or professional degree | 10.1 | 328 |
| Born in the United States | 87.8 | 1856 |
| Language of survey | ||
| English | 98.0 | 2078 |
| Spanish | 2.0 | 41 |
| Insurance type | ||
| Commercial (e.g., employer-based, direct purchase, health insurance exchange) | 65.0 | 1488 |
| State Medicaid or CHIP | 20.5 | 358 |
| Other public insurance (including Medicare, military/VA, IHS) | 4.4 | 83 |
| None | 6.1 | 128 |
| Don't know | 3.8 | 56 |
| Missing | 0.2 | 6 |
| Employment status | ||
| Working full time | 49.7 | 1161 |
| Working part time | 18.9 | 366 |
| Not working for pay | 30.6 | 580 |
| Other | 0.5 | 8 |
| Missing | 0.3 | 4 |
| Household income | ||
| Less than $30,000 | 21.7 | 387 |
| $30,000–$49,000 | 26.9 | 528 |
| $50,000–$74,999 | 18.9 | 420 |
| $75,000–$99,999 | 21.3 | 529 |
| $100,000 or more | 11.2 | 255 |
| Largest affordable emergency expense | ||
| I could not pay for any emergency expense | 18.8 | 311 |
| $1–99 | 13.2 | 233 |
| $100–399 | 22.0 | 416 |
| Over $400 | 45.2 | 1140 |
| Missing | 0.8 | 19 |
Notes: Unweighted n = 2119.
Table 2.
Reproductive health and healthcare experiences of current & prospective contraceptive users (ages 15–44) in a 2022 U.S. national sample.
| Weighted % | Unweighted n | |
|---|---|---|
| Ever had penile-vaginal sex | 89.2 | 1966 |
| Ever been pregnant | 47.8 | 1310 |
| Parent | 41.9 | 1224 |
| Ever used a contraceptive method | 97.4 | 2087 |
| Currently using multiple contraceptive methods | 32.3 | 596 |
| Current contraceptive method use | ||
| No method | 8.1 | 144 |
| Withdrawal/pulling out | 34.3 | 633 |
| Oral contraceptive pill | 29.4 | 544 |
| External condoms | 24.4 | 475 |
| Hormonal IUD | 14.3 | 330 |
| Fertility awareness | 9.0 | 205 |
| Implant | 6.1 | 108 |
| Vasectomy | 6.0 | 220 |
| Copper IUD | 3.0 | 77 |
| Shot | 2.7 | 50 |
| Ring | 1.8 | 39 |
| Emergency contraception | 1.8 | 35 |
| Internal condoms | 0.9 | 12 |
| Patch | 0.7 | 14 |
| Spermicide | 0.3 | 10 |
| Phexxi | 0.2 | 4 |
| Diaphragm | <0.1 | 2 |
| Cervical cap | 0.0 | 0 |
| Sponge | <0.1 | 1 |
| Currently feels they have enough information to make a decision about the birth control method(s) that are best for them | ||
| Yes | 77.9 | 1707 |
| No | 9.4 | 164 |
| Not sure | 12.2 | 237 |
| Missing | 0.5 | 11 |
| Confidence they can get the birth control method they want when they want it | ||
| Very confident | 56.4 | 1301 |
| Somewhat confident | 38.4 | 718 |
| Not confident | 4.8 | 88 |
| Missing | 0.5 | 12 |
| Number of types of discrimination ever experienced in a family planning setting | ||
| 0 types | 44.5 | 992 |
| 1–4 types | 26.0 | 564 |
| 5–9 types | 20.6 | 424 |
| Did not report ever discussing contraception with a healthcare provider | 6.6 | 91 |
| Missing | 2.3 | 48 |
| Received person-centered contraceptive counseling from most recent healthcare provider seen for birth control | ||
| Yes | 35.1 | 847 |
| No | 57.8 | 1169 |
| Did not report ever discussing contraception with a healthcare provider | 6.6 | 91 |
| Missing | 0.5 | 12 |
Notes: Unweighted n = 2119.
Among current and prospective contraceptive users, 59.3% (95% CI 56.3, 62.2%) were using a preferred method (Table 3). Approximately 1 in 4 (25.2%; 95% CI 22.6, 27.9%) were not using a preferred method, while 15.6% (95% CI 13.7, 17.7%) were in the uncertain category. Among those not using a preferred method (unweighted n = 475), nearly a third (32.1%) were not currently using contraception. The most commonly used methods among those not using a preferred method included withdrawal (32.2%), external condoms (24.4%), and oral contraceptive pills (23.2%). The methods most frequently desired included oral contraceptive pills (19.4%), followed by vasectomy (14.2%), the hormonal IUD (10.4%), and the implant (10.0%). Most frequently reported reasons for non-use of preferred method included concerns related to side effects (28.8%); sex-related reasons, including impact on pleasure or infrequent sex (25.1%); logistics and knowledge barriers (18.6%); safety concerns (18.3%); and cost-related reasons (17.6%). About half (52.8%) selected only one reason for non-use (data not shown).
Table 3.
Preferred contraceptive method use and reasons for non-use among current & prospective contraceptive users (ages 15–44) in a 2022 U.S. national sample.
| Weighted % | (95% CI) | Unweighted n | Population Estimate | |
|---|---|---|---|---|
| Using preferred contraceptive method | ||||
| Yes | 59.3 | (56.3, 62.2) | 1291 | 19,200,886 |
| No | 25.2 | (22.6, 27.9) | 475 | 8,147,499 |
| Uncertain | 15.6 | (13.7, 17.7) | 353 | 5,043,999 |
| Among those not using a preferred contraceptive method | ||||
|
Weighted % |
Unweighted n |
Weighted % |
Unweighted n |
|
| First choice method respondent would rather be using | Method(s) currently usinga | |||
| No method | 2.1 | 7 | 32.1 | 144 |
| Oral contraceptive pill | 19.4 | 75 | 24.4 | 103 |
| Vasectomy | 14.2 | 99 | 1.5 | 9 |
| Hormonal IUD | 10.4 | 41 | 5.7 | 34 |
| Implant | 10.0 | 39 | 3.7 | 17 |
| Shot | 6.4 | 33 | 1.9 | 5 |
| Copper IUD | 6.3 | 34 | 1.5 | 9 |
| Patch | 6.2 | 24 | 0.8 | 3 |
| Tubal ligation or other permanent method | 5.6 | 40 | 0.0 | 0 |
| Ring | 3.5 | 17 | 0.6 | 5 |
| Fertility awareness | 2.6 | 11 | 6.4 | 38 |
| External condoms | 2.3 | 12 | 23.2 | 112 |
| Cervical cap | 1.3 | 1 | 0.0 | 0 |
| Phexxi | 1.0 | 6 | 0.0 | 0 |
| Spermicide | 0.4 | 1 | 0.3 | 2 |
| Withdrawal/pulling out | 0.3 | 2 | 32.2 | 139 |
| Internal condoms | 0.2 | 1 | 0.1 | 1 |
| Diaphragm | 0.1 | 1 | 0.0 | 0 |
| Another method | 0.2 | 2 | 0.0 | 0 |
| Sponge | 0.0 | 0 | 0.0 | 0 |
| Emergency contraception | 0.0 | 0 | 2.6 | 11 |
| Don't know what method they'd like to use | 5.6 | 24 | – | – |
| Missing | 2.0 | 5 | – | – |
| Reason not using preferred methodb | ||||
| Concerns about side effects | 28.8 | 116 | ||
| Sex-related reasons (type, frequency, pleasure) | 25.1 | 110 | ||
| Logistics and knowledge barriers (can't get to location, not available, don't know where to get, problems when tried to obtain) | 18.6 | 95 | ||
| Concerns about safety | 18.3 | 68 | ||
| Cost-related reasons (can't afford it, another method is cheaper) | 17.6 | 93 | ||
| Interpersonal reasons (partner or family acceptability, secrecy) | 11.4 | 70 | ||
| Provider-related reasons (no trusted provider, provider suggestion) | 15.7 | 71 | ||
| Wants to get pregnant, have more children, or was recently pregnant | 2.3 | 15 | ||
| Concerns about effectiveness | 1.5 | 3 | ||
| Another reason | 11.6 | 61 | ||
| Not sure | 5.9 | 26 | ||
| Missing | 10.4 | 37 | ||
Note: Unweighted n = 2119. Subsample of those not using preferred method unweighted n = 475.
29.2% of respondents were currently using more than one contraceptive method.
Respondents may have provided multiple reasons for not using their preferred method.
In Table 4, we present the distribution of use of preferred contraceptive method by key sociodemographic characteristics. Notably, the youngest respondents (15–17- and 18-24-year-olds) comprised a larger proportion of those not using a preferred method (45.5% collectively) compared to those using a preferred method (34.1%) or uncertain (28.4%). In terms of educational attainment, respondents with less than high school education comprised a larger proportion of those not using a preferred method (19.3%) compared to those using their preferred method (12.7%) or uncertain (13.6%). Similiarly, those with some college/vocational or technical training comprised higher proportions of those not using a preferred method (40.9%) or uncertain (40.8%) compared to using a preferred method (27.5%). Among those using a preferred method, 23.6% had a high school degree or equivalent, which was higher than the prevelance of high school degree among those not using a preferred method (13.0%) or uncertain (13.8%).
Table 4.
Bivariate analyses of sociodemographic characteristics and preferred contraceptive method use among current & prospective contraceptive users (ages 15–44) in a 2022 U.S national sample.
| Using preferred method |
Total unweighted n | p value | ||||||
|---|---|---|---|---|---|---|---|---|
| Yes |
No |
Not sure |
||||||
| Weighted % | Unweighted n | Weighted % | Unweighted n | Weighted % | Unweighted n | |||
| Age | 2119 | 0.0018 | ||||||
| 15–17 | 6.6 | 40 | 11.8 | 33 | 7.1 | 16 | ||
| 18–24 | 27.5 | 121 | 33.7 | 67 | 21.3 | 35 | ||
| 25–29 | 20.5 | 258 | 20.7 | 122 | 27.7 | 87 | ||
| 30–34 | 19.2 | 309 | 17.5 | 113 | 21.0 | 93 | ||
| 35–39 | 14.8 | 325 | 10.0 | 83 | 12.0 | 66 | ||
| 40–44 | 11.5 | 238 | 6.4 | 57 | 10.8 | 56 | ||
| Race/ethnicity | 2094 | 0.026 | ||||||
| White only | 58.2 | 789 | 47.9 | 232 | 55.8 | 189 | ||
| Black only | 12.8 | 151 | 11.9 | 60 | 14.1 | 42 | ||
| Latinx/Hispanic | 19.6 | 203 | 30.0 | 116 | 20.3 | 69 | ||
| Asian/Pacific Islander only | 5.9 | 76 | 7.4 | 39 | 6.0 | 24 | ||
| Multiracial, not including Latinx/Hispanic | 3.6 | 62 | 2.8 | 24 | 3.8 | 18 | ||
| Relationship status | 2111 | <0.0001 | ||||||
| Married, engaged, or in a serious relationship | 59.7 | 910 | 42.3 | 269 | 58.6 | 233 | ||
| In another type of relationship | 24.2 | 222 | 25.5 | 82 | 27.2 | 76 | ||
| Not in a relationship (including divorcing/separating) | 16.1 | 156 | 32.3 | 124 | 14.2 | 39 | ||
| Ever been pregnant | 2114 | 0.018 | ||||||
| Yes | 49.9 | 833 | 40.9 | 257 | 51.7 | 220 | ||
| No | 50.1 | 455 | 59.2 | 217 | 48.3 | 132 | ||
| Highest education completed | 2119 | <0.0001 | ||||||
| Less than high school | 12.7 | 72 | 19.3 | 50 | 13.6 | 27 | ||
| High school or equivalent | 23.6 | 160 | 13.0 | 45 | 13.8 | 41 | ||
| Vocational or technical school, some college, or associates degree | 27.5 | 420 | 40.9 | 189 | 40.8 | 145 | ||
| Bachelor's degree | 25.0 | 426 | 18.5 | 124 | 22.8 | 92 | ||
| Post graduate study or professional degree | 11.2 | 213 | 8.3 | 67 | 9.1 | 48 | ||
| Born in the United States | 2111 | 0.30 | ||||||
| Yes | 89.0 | 1144 | 88.5 | 416 | 85.1 | 296 | ||
| No or prefer not to say | 11.0 | 143 | 11.5 | 58 | 14.9 | 54 | ||
| Insurance type | 2113 | 0.95 | ||||||
| Commercial (e.g., employer-based, direct purchase, health insurance exchange) | 65.0 | 953 | 66.5 | 312 | 63.4 | 223 | ||
| State Medicaid or CHIP | 20.5 | 196 | 20.8 | 92 | 20.6 | 70 | ||
| Other public insurance (including Medicare, military/VA, IHS) | 4.7 | 45 | 2.9 | 16 | 5.6 | 22 | ||
| None | 6.0 | 62 | 6.1 | 41 | 6.8 | 25 | ||
| Don't know | 3.8 | 29 | 3.7 | 14 | 3.7 | 13 | ||
| Employment status | 2107 | 0.81 | ||||||
| Working full time | 50.5 | 738 | 47.2 | 239 | 53.1 | 184 | ||
| Working part time | 18.9 | 206 | 20.3 | 87 | 17.9 | 73 | ||
| Not working for pay | 30.6 | 341 | 32.6 | 147 | 28.9 | 92 | ||
| Largest affordable emergency expense | 2100 | 0.015 | ||||||
| I could not pay for any emergency expense | 16.5 | 163 | 21.4 | 77 | 24.2 | 71 | ||
| $1–99 | 11.6 | 116 | 16.0 | 64 | 15.6 | 53 | ||
| $100–399 | 22.0 | 237 | 24.3 | 105 | 19.3 | 74 | ||
| Over $400 | 49.9 | 760 | 38.4 | 225 | 41.0 | 155 | ||
Notes: Total unweighted n varies due to missingness (as shown in Tables 1 and 2) and because categories for which there were fewer than five respondents in a cell (“another race” category in the race/ethnicity variable and “other” employment type in the employment variable) were excluded from bivariate analyses.
In unadjusted and adjusted logistic regression analyses (Table 5), we investigated the relationship between four aspects of person-centered healthcare access and use of preferred contraceptive method. After controlling for sociodemographic characteristics, we found increased adjusted odds of use of preferred method among those who currently felt they had enough information to decide about the best contraception for them (Adjusted Odds Ratio [AOR] 3.31; 95% CI 2.10, 5.21) compared to those who did not. Likewise, those who were very confident (AOR 9.24; 95% CI 4.29, 19.91) or somewhat confident (AOR 3.78; 95% CI 1.76, 8.12) they could obtain desired contraception when desired had much higher odds of preferred method use compared to those who were not confident. Among the subsample of respondents who had ever discussed contraception with a healthcare provider, those who had received person-centered contraceptive counseling had nearly twice the odds of preferred method use (AOR 1.72; 95% CI 1.33, 2.23) compared to those who had not. Those who had experienced no discrimination in family planning settings had 1.58 (95% CI 1.13, 2.20) times the adjusted odds of preferred contraceptive method use compared those who had ever experienced 5–9 types of discrimination.
Table 5.
Associations between aspects of person-centered healthcare access and preferred contraceptive method use among current & prospective contraceptive users (ages 15–44) in a 2022 U.S. national sample.
| Unadjusted Odds Ratio (95% CI) | Adjusted Odds Ratio (95% CI) | |||
|---|---|---|---|---|
| Model 1: Currently feels they have enough information to make a decision about the birth control method(s) that are best for them | ||||
| Has enough information | 3.17 | (1.97, 5.10) | 3.31 | (2.10, 5.21) |
| Not sure if they have enough information | 1.08 | (0.60, 1.93) | 1.17 | (0.66, 2.07) |
| Does not have enough information | Reference | Reference | ||
| Model 2: Confidence they can get the birth control method they want when they want it | ||||
| Very confident | 10.27 | (4.73, 22.30) | 9.24 | (4.29, 19.91) |
| Somewhat confident | 4.24 | (1.93, 9.29) | 3.78 | (1.76, 8.12) |
| Not confident | Reference | Reference | ||
| Model 3: Person-centered contraceptive counseling from most recent healthcare provider seen for birth control | ||||
| Received person-centered contraceptive counseling | 1.71 | (1.33, 2.21) | 1.72 | (1.33, 2.23) |
| Did not receive person-centered contraceptive counseling | Reference | Reference | ||
| Model 4: Number of types of discrimination ever experienced in a family planning setting | ||||
| 0 types | 1.72 | (1.25, 2.37) | 1.58 | (1.13, 2.20) |
| 1–4 types | 1.32 | (0.96, 1.96) | 1.30 | (0.90, 1.88) |
| 5–9 types | Reference | Reference | ||
Notes: Models 1 and 2, unweighted n = 2096. Models 3 and 4, unweighted n = 1972 (including respondents who had ever discussed contraception with a healthcare provider). The following variables were included in adjusted logistic regression analyses: age, race, relationship status, ever being pregnant, educational attainment, insurance, employment status, and largest affordable emergency expense.
Discussion
Among current and prospective contraceptive users in the U.S., one in four are not using a preferred contraceptive method, translating to an estimated 8.1 million people. We find that reasons for not using preferred methods extend beyond administrative, informational, and time barriers to the characteristics of the methods themselves (particularly side effects and sex-related reasons). Importantly, regression analyses highlight the importance of key aspects of person-centered healthcare access, including information, self-efficacy, and the long arm of low-quality and discriminatory contraceptive care, to preferred contraceptive method use. This sample of current and prospective users, representing an estimated 32.4 million individuals, reflects the minimum population that needs access to contraceptive methods and services. This access is critical for all three categories of preferred method use, as all may need services to start, switch, or discontinue contraceptive use (and those needs will change over time, given the dynamic nature of the contraceptive journey13).
Prior research has found similar levels of preference for use of a different contraceptive method among nationally representative U.S. samples, though these studies may focus only on current contraceptive users16 or those who had recent “heterosexual intercourse,”17 neglecting the unfulfilled preference to use contraception among those not currently using a method, excluding contraceptive use for reasons beyond pregnancy prevention, and including individuals who do not have a self-defined need for contraception. There has been limited exploration to understand why individuals are not using preferred contraception. One analysis of population-based data from Ohio found that affordability was the most frequent reason for not using a preferred method; the study did not report on side effects, safety concerns, and impact on sexual pleasure as reasons for non-use.31 A study using nationally representative data collected in 2013 found that cost was the top reason for non-use of preferred method, followed by lack of perceived/actual need and fear of side effects and health concerns.32 More recent research from 2022 also found that the most reported reason for not using a preferred method was side effects.16
In the present analysis, we found that some respondents simultaneously selected a method they would rather be using but later indicated they were not using this method due to concerns about side effects or for sex-related reasons. Taken together, our findings and the extant literature suggest the need for future research, especially using qualitative approaches, to explore this dynamic and whether concerns may be addressed by high-quality information and counseling or if this phenomenon reflects ambivalence between the desire to use specific contraceptive methods and the anticipated reality of use. Another possibility is that individuals would like to use an abstract contraceptive method that is not currently available; some research identifying ideal characteristics of contraceptive methods notes that people's ideals do not necessarily align with currently available methods.12,33 Notably, the data presented here represent one moment in time. Understanding where respondents are in the process of decision-making around contraception may be helpful, as someone could indicate that they would rather use a different method but be at one of several phases of contemplating this decision.32
This study centers on the concept of person-centered healthcare access,20 highlighting dimensions of contraceptive access that are important to track and address with interventions. Notably, this analysis revealed that low-quality care is pervasive among current and prospective users. Only 35% of respondents received person-centered contraceptive counseling from their most recent contraceptive care provider, while 26% reported experiencing 1–4 types and 20% 5–9 types of discrimination in family planning settings during their lifetimes. Though data from clinical settings focused on specific, recent clinical encounters generally finds the majority of patients receive person-centered contraceptive counseling,34 other population-based research has found lower levels, ranging from 30 to 51%.16,19,35 While receipt of person-centered contraceptive counseling is now being implemented as a metric of facility-level healthcare quality,27 public health metrics such as those utilized in the Healthy People 2030 national goals have yet to integrate aspects of the ability to engage in healthcare.20 Specifically, the strong relationships between having enough information and confidence about obtaining contraception with preferred method use signal the importance of these concepts in person-centered contraceptive access.
Further, with the focus on current and prospective users, this metric is helpful for capturing contraceptive autonomy.11 By excluding non-users who do not want to use contraception from the sample (a group that Sendorwicz (2020) describes as “autonomous non-users”), our metric thereby does not suggest that these individuals “need” contraception, as is implied by existing public health and quality metrics. Person-centered approaches to tracking contraceptive access, such as use of preferred method among prospective and current contraceptive users, are aligned with calls to advance SRHE through a focus on reproductive well-being and shift away from the widely critiqued measure of unintended pregnancy.1 Given that public health metrics and goals currently rely on individual-level survey data for tracking, we suggest the adoption of use of preferred method as an indicator of contraceptive access in the U.S. Potential improvement on this metric include adding the phrase “right now” to the primary question, asking follow-up questions to clarify whether uncertain participants desire use of a different method, and determining whether respondents who want to stop using a method as soon as possible should be classified as not using a preferred method rather than uncertain.
Strengths of this study include use of a nationally representative sample, which allows generalization to the U.S. population of prospective and current contraceptive users who had not obtained a permanent contraceptive method and were assigned female sex at birth. We used cognitive interviews to refine our measure of preferred method use and collaborated with a working group including researchers, advocates, and providers to define the contours of the metric of preferred method use, ensuring that the denominator is appropriate, and data are most useful. Further, by including prospective and current contraceptive users in this metric and not linking it to data collected in a healthcare setting, this study offers a holistic, national portrait of an important aspect of person-centered contraceptive access neglected by current access and quality measurement approaches.
Limitations
Limitations of this study include the broad shortcoming of survey research in its lack of detail to truly contextualize findings, even with the use of follow-up questions to identify why respondents were not using preferred methods. Additionally, we categorized current contraceptive users who wanted to stop using any of their methods as soon as possible in the “uncertain” category of preferred method use. Future research should investigate the contraceptive preferences of those in the uncertain category, including exploring why some were uncertain about whether there was another method they would like to use or if current users who wanted to discontinue use would prefer to use no method. While the AmeriSpeak sample is nationally representative, the subsample of current and prospective contraceptive users trends more educated and insured than the general population. If this sample represents more advantaged individuals, it may overestimate use of preferred method, as research has documented lower access to and experiences of quality care among under-resourced populations.17,19,36,37 Additionally, while we did not rely on cisgender or heterosexual identification for eligibility or inclusion in the denominator, we lacked sufficient sample sizes for consideration of differences in preferred method use by sexual orientation and gender identity. While inclusion criteria based on sex assignment at birth avoids equating identification as a woman with reproductive capacity, asking respondents to complete a body part checklist would provide more accurate data on pregnancy capacity; this is particularly important since transgender and nonbinary individuals have noted the harm of centering assigned sex at birth.38 Additionally, given the high interest in vasectomy, it is important to include cisgender men and other individuals with the capacity to produce sperm in future research about preferred method use. Likewise, we excluded people who had undergone permanent contraception procedures or were otherwise infecund; including them in future research will provide the most accurate estimate of preferred contraceptive method use and the population who may need contraception, as individuals and their partners use contraception for reasons beyond pregnancy prevention.
Conclusion
These data highlight the need for contraceptive access strategies that center the needs and preferences of current contraceptive users, as well as those interested in use. While many efforts over the last 15 years have focused on increasing access to LARC,7,39 these data reveal that other methods, including oral contraception and vasectomy, are also among those most frequently desired but not used. This suggests that a greater diversity of policy solutions than those that have facilitated increased access to LARC must be tested and adopted. For example, those not using a preferred method most frequently selected oral contraception as their most desired method; expanding service delivery approaches, including telehealth, pharmacist prescribing, and over-the-counter availability, and ensuring these options are covered by health insurance could facilitate greater access. Meanwhile, 14% of those not using a preferred method desired vasectomy, a method for which there are a host of different barriers to access, including knowledge among men40 and the financial burden of cost-sharing.41 This study also highlights the need for high-quality information about contraception (particularly important as misinformation and disinformation have been identified as key threats to contraceptive access in the U.S.3), as well as the significance of person-centered, non-discriminatory healthcare in reproductive self-determination. Our work points to the need to continue to innovate in measurement related to contraception and reproductive health more broadly, with the goal of optimizing knowledge generation that informs policy, programmatic, and clinical efforts to support people in actualizing the sexual and reproductive lives they wish to live.
Contributors
All authors contributed to the conceptualization of the manuscript and development of the preferred method use metric. AMG, JA, and CM conceptualized the study and designed the methodology. AMG and CM acquired funding. AMG supervised the study. AMG, AHB, and JA provided project administration. AHB and JA collected data. AMG, AHB, and JA conducted the data analysis. AMG and AHB accessed and verified the underlying data in the manuscript. AMG, AHB, JA, and CM interpreted the data. AMG and AHB wrote the original draft of the manuscript, and all authors contributed to writing by reviewing and editing the manuscript. AMG had final responsibility for the decision to submit the study for publication.
Data sharing statement
The data and codebook will be publicly available from the Open Science Framework at https://osf.io/wvb5m/.
Declaration of interests
AMG, AHB, JA, and CM received support for this work from a grant from Arnold Ventures. DC, AC, CL, WSR, and ESV received honoraria from the University of California, Berkeley for participation in the Person-Centered Contraceptive Access Metrics Working Group for this project. AMG has received funding the Robert Wood Johnson Foundation; consulting fees from the Coalition to Expand Contraceptive Access (CECA), and the Guttmacher Institute; and honoraria from the University of Kansas Medical Center, the University of Minnesota, and Elsevier. She is on the Board of Directors of Ibis Reproductive Health. JA has been a paid consultant for Medicines360, Insight Metrics, and Population Services International and received honoraria from the Society of Family Planning (SFP). LS has been a paid consultant for the University of California, San Francisco and JSI Research and Training Institute, and received honoraria from the University of Missouri, Kansas City. JB was a public board member of the ACOG Executive Board; she has received support from her employer for work-related travel; and her organization receives a Title X grant, private foundation funds, and a stipend for participation in CECA workgroups. CD receives royalties from Wolters Kluwer; has been a paid consultant for Modern Fertility; has received payments from Planned Parenthood Federation of America (PPFA), JSI, SFP, and Elsevier; and support for meetings/travel from PPFA. WSR has received funding from the Robert Wood Johnson Foundation, an anonymous foundation, and the Collaborative for Gender and Reproductive Equity; honoraria from CECA and SFP; support for meetings/travel from Power to Decide and the SFP Research Fund; and has served on the Feminist Women's Health Center Board of Directors. LD, BF, RM, TBS, and MLK declare no competing interests.
Acknowledgements
This research was supported by Arnold Ventures. The authors thank additional members of the Person-Centered Contraceptive Access Metrics Working Group for sharing their expertise, time, and insights to help conceptualize and prioritize this metric, including: Angela D. Aina, Sheila Desai, Elizabeth Jones, Alicia Luchowski, Sue Moskosky, Antoinette Nguyen, Ellen Pliska, and Kari White. Thank you to Jamie Hart from CECA for support in designing and facilitating the working group meetings. We acknowledge Brenda Mathias, Mayra Cazares-Minero, and Alex Schulte for supporting data collection and analysis and Ashley Nguyen for assisting with the design of the Project Overview figure.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lana.2023.100662.
Appendix A. Supplementary data
References
- 1.Hart J., Crear-Perry J., Stern L. US sexual and reproductive health policy: which frameworks are needed now, and next steps forward. Am J Public Health. 2022;112:S518–S522. doi: 10.2105/AJPH.2022.306929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maril R.S. 2023. From liberation to (re)criminalization: Dobbs v. Jackson Women's Health Organization, bodily autonomy, and the expansion of state rights. [DOI] [Google Scholar]
- 3.Malcolm N., Desai S., Stern L., Hart J. Coalition to Expand Contraceptive Access; Washington, D.C.: 2023. Developing a post-Roe contraceptive access strategy: environmental scan report.https://www.contraceptionaccess.org/post-roe-strategy [Google Scholar]
- 4.Mostafa A., Butler K., Mieszkowski K. The long campaign to turn birth control into the new abortion. http://revealnews.org/podcast/the-long-campaign-to-turn-birth-control-into-the-new-abortion
- 5.Stock N., Blum D. 2022. Is birth control still legal in the U.S.? The New York Times.https://www.nytimes.com/2022/06/24/us/birth-control-plan-b-roe-abortion.html [Google Scholar]
- 6.Dehlendorf C., Grumbach K., Schmittdiel J.A., Steinauer J. Shared decision making in contraceptive counseling. Contraception. 2017;95:452–455. doi: 10.1016/j.contraception.2016.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gómez A.M., Fuentes L., Allina A. Women or LARC first? Reproductive autonomy and the promotion of long-acting reversible contraceptive methods. Perspect Sex Reprod Health. 2014;46:171–175. doi: 10.1363/46e1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Office of Population Affairs, U.S, Department of Health and Human Services . 2017. Performance measures: contraceptive care measures.https://www.hhs.gov/opa/performance-measures/index.html [Google Scholar]
- 9.U.S. Department of Health and Human Services . 2020. Healthy People 2030: family planning.https://health.gov/healthypeople/objectives-and-data/browse-objectives/family-planning [Google Scholar]
- 10.Aiken A.R.A., Borrero S., Callegari L.S., Dehlendorf C. Rethinking the pregnancy planning paradigm: unintended conceptions or unrepresentative concepts? Perspect Sex Reprod Health. 2016;48:147–151. doi: 10.1363/48e10316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Senderowicz L. Contraceptive autonomy: conceptions and measurement of a novel family planning indicator. Stud Fam Plann. 2020;51:161–176. doi: 10.1111/sifp.12114. [DOI] [PubMed] [Google Scholar]
- 12.Littlejohn K.E. University of California Press; Oakland, California: 2021. Just get on the pill: the uneven burden of reproductive politics. [Google Scholar]
- 13.Downey M.M., Arteaga S., Villaseñor E., Gómez A.M. More than a destination: contraceptive decision making as a journey. Womens Health Issues. 2017;27:539–545. doi: 10.1016/j.whi.2017.03.004. [DOI] [PubMed] [Google Scholar]
- 14.Simmons R.G., Baayd J., Waters M., Diener Z., Turok D.K., Sanders J.N. Assessing contraceptive use as a continuum: outcomes of a qualitative assessment of the contraceptive journey. Reprod Health. 2023;20:33. doi: 10.1186/s12978-023-01573-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Darney B.G., Biel F.M., Oakley J., Coleman-Minahan K., Cottrell E.K. Contraceptive method switching and long-acting reversible contraception removal in U.S. Safety net clinics, 2016–2021. Obstet Gynecol. 2023;142:669–678. doi: 10.1097/AOG.0000000000005277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Frederiksen B., Ranji U., Long M., Diep K. KFF; 2022. 2022. Contraception in the United States: a closer look at experiences, preferences, and coverage.https://www.kff.org/report-section/contraception-in-the-united-states-a-closer-look-at-experiences-preferences-and-coverage-findings/ [Google Scholar]
- 17.Burke K.L., Potter J.E., White K. Unsatisfied contraceptive preferences due to cost among women in the United States. Contracept X. 2020;2 doi: 10.1016/j.conx.2020.100032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Institute of Medicine . The National Academies Press; Washington, DC: 2001. Crossing the quality chasm: a new health system for the 21st century.https://www.nap.edu/catalog/10027/crossing-the-quality-chasm-a-new-health-system-for-the [PubMed] [Google Scholar]
- 19.Welti K., Manlove J., Finocharo J., Faccio B., Kim L. Women's experiences with person-centered family planning care: differences by sociodemographic characteristics. Contracept X. 2022;4 doi: 10.1016/j.conx.2022.100081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Levesque J.-F., Harris M.F., Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. 2013;12:18. doi: 10.1186/1475-9276-12-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Holt K., Reed R., Crear-Perry J., Scott C., Wulf S., Dehlendorf C. Beyond same-day long-acting reversible contraceptive access: a person-centered framework for advancing high-quality, equitable contraceptive care. Am J Obstet Gynecol. 2020;222:S878.e1–S878.e6. doi: 10.1016/j.ajog.2019.11.1279. [DOI] [PubMed] [Google Scholar]
- 22.Contraceptive Justice Coalition . EverThrive Illinois; Chicago, IL: 2019. EverThrive Illinois. Contraceptive justice: policy and community assessment report.https://everthriveil.org/wp-content/uploads/2021/01/2019_ContraceptiveJusticePolicyandCommunityAssessmentReport.pdf [Google Scholar]
- 23.Burke K.L., Potter J.E. Meeting preferences for specific contraceptive methods: an overdue indicator. Stud Fam Plann. 2023;54:281–300. doi: 10.1111/sifp.12218. [DOI] [PubMed] [Google Scholar]
- 24.Bhakuni H., Abimbola S. Epistemic injustice in academic global health. Lancet Glob Health. 2021;9:e1465–e1470. doi: 10.1016/S2214-109X(21)00301-6. [DOI] [PubMed] [Google Scholar]
- 25.NORC . NORC at the University of Chicago; Chicago, IL: 2022. Technical overview of the AmeriSpeak panel, NORC's probability-based household panel.https://amerispeak.norc.org/Documents/Research/AmeriSpeak%20Technical%20Overview%202019%2002%2018.pdf [Google Scholar]
- 26.Bird S.T., Bogart L.M. Birth control conspiracy beliefs, perceived discrimination, and contraception among African Americans: an exploratory study. J Health Psychol. 2003;8:263–276. doi: 10.1177/1359105303008002669. [DOI] [PubMed] [Google Scholar]
- 27.Partnership for Quality Measurement . Partnership for Quality Measurement; 2020. Person-centered contraceptive counseling (PCCC) measure.https://p4qm.org/measures/3543 [Google Scholar]
- 28.StataCorp . StataCorp LLC; College Station, TX: 2021. Stata survey data reference manual: release 17. [Google Scholar]
- 29.Rao J.N.K., Scott A.J. The analysis of categorical data from complex sample surveys: chi-squared tests for goodness of fit and independence in two-way tables. J Am Stat Assoc. 1981;76:221–230. [Google Scholar]
- 30.Rao J.N.K., Scott A.J. On chi-squared tests for multiway contingency tables with cell proportions estimated from survey data. Ann Stat. 1984;12:46–60. [Google Scholar]
- 31.Chakraborty P., Gallo M.F., Nawaz S., et al. Use of nonpreferred contraceptive methods among women in Ohio. Contraception. 2021;103:328–335. doi: 10.1016/j.contraception.2021.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.He K., Dalton V.K., Zochowski M.K., Hall K.S. Women's contraceptive preference-use mismatch. J Womens Health. 2017;26:692–701. doi: 10.1089/jwh.2016.5807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Judge-Golden C.P., Wolgemuth T.E., Zhao X., Mor M.K., Borrero S. Agreement between self-reported “ideal” and currently used contraceptive methods among women veterans using the Veterans Affairs healthcare system. Womens Health Issues. 2020;30:283–291. doi: 10.1016/j.whi.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dehlendorf C., Vittinghoff E., Silverstein I., et al. Prioritizing patient experience: validation of the person-centered contraceptive counseling measure as a performance measure. Contraception. 2023;123 doi: 10.1016/j.contraception.2023.110010. [DOI] [PubMed] [Google Scholar]
- 35.Kavanaugh M.L., Zolna M.R. Where do reproductive-aged women want to get contraception? J Womens Health. 2023;32:657–669. doi: 10.1089/jwh.2022.0406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Barber J.S., Ela E., Gatny H., et al. Contraceptive desert? Black-white differences in characteristics of nearby pharmacies. J Racial Ethn Health Disparities. 2019;6:719–732. doi: 10.1007/s40615-019-00570-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Key K., Wollum A., Asetoyer C., et al. Challenges accessing contraceptive care and interest in over-the-counter oral contraceptive pill use among Black, Indigenous, and people of color: an online cross-sectional survey. Contraception. 2023;120 doi: 10.1016/j.contraception.2023.109950. [DOI] [PubMed] [Google Scholar]
- 38.Moseson H., Zazanis N., Goldberg E., et al. The imperative for transgender and gender nonbinary inclusion: beyond women's health. Obstet Gynecol. 2020;135:1059–1068. doi: 10.1097/AOG.0000000000003816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Committee on Gynecologic Practice Long-Acting Reversible Contraception Working Group Committee opinion no. 642: increasing access to contraceptive implants and intrauterine devices to reduce unintended pregnancy. Obstet Gynecol. 2015;126:e44–e48. doi: 10.1097/AOG.0000000000001106. [DOI] [PubMed] [Google Scholar]
- 40.White K., Martínez Órdenes M., Turok D.K., Gipson J.D., Borrero S. Vasectomy knowledge and interest among U.S. men who do not intend to have more children. Am J Mens Health. 2022;16 doi: 10.1177/15579883221098574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.U.S. Centers for Medicare & Medicaid Services Birth control benefits and reproductive health care options in the Health Insurance Marketplace. HealthCare.gov. n.d. https://www.healthcare.gov/coverage/birth-control-benefits/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.